Watch a video presentation of this article
Abbreviations
- PBC
primary biliary cirrhosis
Hepatic granulomas are localized collections of inflammatory cells, which are found in 2% to 10% of patients who undergo a liver biopsy.1 They can be associated with a variety of systemic conditions or may be an incidental finding on an otherwise normal liver biopsy. Although the granulomas themselves rarely cause structural liver damage, their detection may be the first indication of an underlying systemic disease. Careful assessment for associated clinical symptoms, targeted laboratory and radiological investigations, and characterization of the morphology and localization of granulomas will usually lead to a definitive diagnosis and appropriate treatment.
Causes of Hepatic Granulomas
Hepatic granulomas are associated with a wide range of disorders (Table 1). The most common causes in the West are sarcoidosis, drug‐induced, tuberculosis, neoplastic disease, and primary biliary cholangitis [formerly primary biliary cirrhosis (PBC)].2 Infectious causes are summarized in Table 2.
Table 1.
Causes of Hepatic Granuloma
| Autoimmune Disorders |
| Sarcoidosis |
| Cholestatic liver disease, e.g., primary biliary cholangitis |
| Polymyalgia rheumatica |
| Vasculitides |
| Granulomatosis with polyangiitis |
| Polyarteritis nodosa |
| Churg‐Strauss syndrome |
| Infections |
| Bacterial, fungal, viral, parasitic (Table 2) |
| Drugs |
| Nitrofurantoin, allopurinol, phenytoin (Table 3) |
| Allopurinol, Bacillus Calmette‐Guérin, carbamazepine, chlorpropamide, diltiazem, gold, halothane, hydralazine, interferon‐α, mebendazole, methyldopa, nitrofurantoin, phenylbutazone, phenytoin, procainamide, quinidine, sulfa drugs |
| Malignancy |
| Hodgkin's lymphoma and non‐Hodgkin's lymphoma |
| Renal cell carcinoma |
| Hepatic metastases |
| Inherited |
| Chronic granulomatous disease |
| Chronic Gastrointestinal Disease |
| Crohn's disease |
| Postoperative Appearance |
| Jejunoileal bypass |
| Metal Toxicity |
| Copper toxicity |
| Berylliosis |
| Ingestion of Foreign Materials |
| Mineral oil, talc, starch |
| Toxins |
| Intravesical administration of Bacillus Calmette‐Guérin |
| Idiopathic |
Table 2.
Infectious Causes of Hepatic Granuloma
| Bacterial |
| Tuberculosis |
| Brucellosis |
| Listeriosis |
| Mycobacterium avium complex |
| Disseminated Bacillus Calmette‐Guérin infection |
| Rickettsia (typhus fever and Boutonneuse fever) |
| Coxiella burnetii (Q fever) |
| Spirochetal (Lyme disease) |
| Secondary syphilis |
| Lepromatous leprosy |
| Yersiniosis |
| Psittacosis |
| Tropheryma whipplei (Whipple disease) |
| Melioidosis |
| Tularemia |
| Catch scratch fever |
| Viral |
| Cytomegalovirus |
| Epstein‐Barr virus |
| Hepatitis A, B and C |
| Fungal |
| Histoplasmosis |
| Coccidioidomycosis |
| Cryptococcus |
| Candidiasis |
| Nocardiosis |
| Parasitic |
| Schistosomiasis |
| Toxoplasmosis |
| Visceral larva migrans |
| Visceral leishmaniasis |
Isolated granulomas may also be an incidental finding on a normal liver biopsy or in patients with known liver disease, such as viral hepatitis, with no relationship to the clinical presentation or response to treatment.3 Indeed, between 10% and 36% of granulomas are reported to have no discoverable cause after extensive evaluation.4 Granulomatous hepatitis is a syndrome with a prolonged febrile illness, myalgias, hepatosplenomegaly, and arthralgia of unknown cause.
Histopathology
Granulomas are circumscribed lesions that form as a result of an inflammatory reaction and are characterized by a central accumulation of macrophages, with a surrounding rim consisting of lymphocytes and fibroblasts (Figure 1). There are four main histological variants of hepatic granulomas, which are summarized in Table 3. Noncaseating granulomas are often seen in sarcoidosis, caseating granulomas in tuberculosis, fibrin‐ring variants in infections and vasculitis, and lipogranulomas in the context of ingested mineral oil or hepatic steatosis.5
Figure 1.
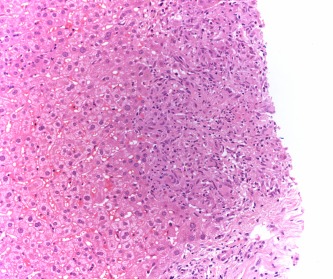
Large, noncaseating granuloma from patient with sarcoid.
Table 3.
Histological Variants of Hepatic Granulomas
| Variant | Description | Causes |
|---|---|---|
| 1. Noncaseating | Nonnecrotic | Sarcoidosis |
| 2. Caseating | Area of central necrosis |
Tuberculosis Vasculitis, e.g., GPA |
| 3. Fibrin‐ring | Epithelioid cells surround a vacuole within an encircling fibrin ring | Q fever, Hodgkin's lymphoma, Leishmaniasis, cytomegalovirus, hepatitis A, Toxoplasmosis, giant cell arteritis, Q fever, Boutonneuse fever, allopurinol |
| 4. Lipogranulomas | Contain a central lipid vacuole | Ingestion of mineral oil, hepatic steatosis |
The morphology and location of granulomas can help with a differential diagnosis. Important morphological features include the presence or absence of necrosis, the nature of the infiltrate and surrounding biopsy specimen, and the presence of organisms or foreign material, for example, schistosome eggs or fungal organisms.6 Although granulomas can be located throughout the hepatic lobule, most occur in the parenchyma. Certain locations are associated with specific disease processes, such as portal granulomas in PBC.
Special stains for microorganisms (acid‐fast and fungal staining) and polarizing light microscopy (foreign body talc granulomas) are also invaluable.7 However, it may be difficult, if not impossible, to determine the significance and cause, based on histology alone.
Clinical Features and Investigations
The observation of granulomata in a liver biopsy specimen warrants thorough workup to identify a possible cause. Clues may be obtained from the medical history, physical examination, specific blood tests, or radiological studies (Table 4).
Table 4.
Laboratory Investigations for Hepatic Granuloma
| Cause | Investigation |
|---|---|
| Sarcoidosis and tuberculosis | Chest radiograph |
| Tuberculosis | Tuberculin skin test |
| Acid‐fast stains on liver biopsy | |
| Sarcoidosis | Serum angiotensin‐converting enzyme |
| Primary biliary cholangitis | Serum antimitochondrial antibodies and immunoglobulin M |
| Bacterial, fungal, viral infections | Blood cultures |
| Fungal | Fungal stains on liver biopsy |
| Virus | Virology: cytomegalovirus, Epstein‐Barr virus, human immunodeficiency virus serology |
| Parasites | Assess for schistosome eggs |
| Infection, e.g., Brucella, syphilis, Coxiella | Brucella, syphilis, Coxiella serology |
Granulomas themselves are typically asymptomatic. Clinical features reflect the underlying systemic disease and its severity. Constitutional symptoms such as fever, night sweats, and weight loss are the most common, especially in tuberculosis, sarcoidosis, and infectious causes. Hepatosplenomegaly may be present in schistosomiasis.8 Progressive hepatic fibrosis with portal hypertension and cirrhosis is infrequent and is associated with extensive sarcoidosis, primary biliary cholangitis, and schistosomiasis.9
From a biochemical perspective, the most common abnormalities are elevations in serum alkaline phosphatase and gamma‐glutamyltransferase. However, these are nonspecific and rarely helpful in diagnosis.10 Hepatocellular dysfunction may also occur when part of a broader inflammatory reaction, for example, a drug reaction. Imaging including plain radiographs, ultrasound, computed tomography, and magnetic resonance imaging may show calcification in chronic granulomas, lymphadenopathy in sarcoidosis (hilar) or lymphoma (generalized), or filling defects, particularly with confluent lesions, but are generally nondiagnostic.11
Other tests such as blood cultures, viral serology, skin tests, and tissue specimens from multiple sites are often needed to guide diagnosis (Table 4). Fresh biopsy specimens can be sent for culture, and special stains for acid‐fast bacilli, fungi, and other organisms, to increase diagnostic sensitivity for infections in those with constitutional symptoms.
Treatment
Treatment is directed at the underlying disorder. In asymptomatic idiopathic incidental granuloma, treatment is usually withheld and monitoring undertaken with regular clinical assessment and liver function. In patients with symptomatic idiopathic granulomatous hepatitis, immunosuppression with corticosteroids should be considered once tuberculosis has been excluded. Corticosteroids are started with careful evaluation for symptomatic or biochemical response, or both, in the first 3 months.12 Evaluation of those who do not respond to immunosuppression is important given the differential diagnosis of lymphoma, solid‐organ malignancies, and atypical infections.13
Because immunosuppression will exacerbate tuberculosis, an empiric course of antituberculous therapy is justified in the presence of fever and other nonspecific symptoms, or if presentation is suggestive of underlying tuberculosis and a specific diagnosis cannot be made.14 If there is no clinical or radiological response after 1 to 2 months, empiric corticosteroids are considered. In the case of tuberculosis, medications used to treat may themselves be associated with granulomas, such as sulfonamides and isoniazid.
The majority of patients with sarcoidosis are asymptomatic; however, corticosteroids may benefit patients with progressive hepatic sarcoidosis, although whether this prevents hepatic fibrosis is unclear.15 Ursodeoxycholic acid may be beneficial for pruritus caused by cholestatic jaundice in sarcoidosis and PBC.
Relapse can occur when any treatment is discontinued. Repeat courses of corticosteroids may be required in those responsive to an initial course of immunosuppression. Methotrexate is effective in patients who relapse, are steroid intolerant, or refuse corticosteroid treatment with symptomatic improvement and histological regression in case series.16
Prognosis
Hepatic granulomas caused by drugs or infection regress with appropriate treatment. Sarcoid granulomas may disappear spontaneously or persist for years, usually without causing clinically important liver disease. However, progressive fibrosis, portal hypertension, and cirrhosis can rarely develop.17 In schistosomiasis, progressive portal scarring “pipestem fibrosis” is typical; liver function is usually preserved, but marked splenomegaly and variceal hemorrhage can occur.18
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Lamps L. Hepatic granulomas: a review with an emphasis on infectious causes. Arch Path Lab Med 2015;139:867‐875. [DOI] [PubMed] [Google Scholar]
- 2. Lagana SM, Moreira RK, Lefkowitch JH. Hepatic granulomas: pathogenesis and differential diagnosis. Clin Liver Dis 2010;14:605‐617. [DOI] [PubMed] [Google Scholar]
- 3. Tahan V, Ozaras R, Lacevic N, et al. Prevalence of hepatic granulomas in chronic hepatitis B. Dig Dis Sci 2004;49:1575. [DOI] [PubMed] [Google Scholar]
- 4. Zakim, D , Boyer, TD . Hepatology, A Textbook of Liver Diseases. Vol. 3 3rd ed Philadelphia: WB Saunders; 1996:1472. [Google Scholar]
- 5. Maddrey WC. Granulomas of the liver In: Schiff ER, Sorrell MF, Maddrey WC, eds. Schiff's Diseases of the Liver. 8th ed Philadelphia: Lippincott‐Raven; 1989:1572. [Google Scholar]
- 6. Klatskin G. Hepatic granulomata: problems in interpretation. Mt Sinai J Med 1977;44:798. [PubMed] [Google Scholar]
- 7. Drebber U, Kasper HU, Ratering J, et al. Hepatic granulomas: histological and molecular pathological approach to differential diagnosis‐a study of 442 cases. Liver Int 2008;28:828. [DOI] [PubMed] [Google Scholar]
- 8. Hams E, Aviello G, Fallon PG. The Schistosoma Granuloma: Friend or Foe? Front Immunol 2013;4:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Devaney K, Goodman ZD, Epstein MS, et al. Hepatic sarcoidosis: clinic‐pathologic features in 100 patients. Am J Surg Pathol 1993;17:1272‐1280. [PubMed] [Google Scholar]
- 10. Shimizu Y. Liver in systemic disease. World J Gastroenterol 2008;14:4111‐4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tuncer CA, Gezer NS, Secil M. Radiologic features of granulomatous hepatitis. Eur Soc Radiol 2014;1‐16. [Google Scholar]
- 12. Sartin JS, Walker RC. Granulomatous hepatitis: a retrospective review of 88 cases at the Mayo Clinic. Mayo Clin Proc 1991;66:914‐918. [DOI] [PubMed] [Google Scholar]
- 13. Lagana SM, Moreria RK, Lefkowitch JH. Hepatic granulomas: pathogenesis and differential diagnosis. Clin Liver Dis 2010;14:605‐617. [DOI] [PubMed] [Google Scholar]
- 14. Gaya DR, Thorburn D, Oien KA. Hepatic granulomas: a 10 year single centre experience. J Clin Pathol 2003;56:850‐853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ebert EC, Kierson M, Hagspiel KD. Gastrointestinal and hepatic manifestations of sarcoidosis. Am J Gastroenterol 2008;103:3184‐3192; quiz 3193. [DOI] [PubMed] [Google Scholar]
- 16. Knox TA, Kaplan MM, Gelfand JA, Wolff SM. Methotrexate treatment of idiopathic granulomatous hepatitis. Ann Intern Med 1995;122:592. [DOI] [PubMed] [Google Scholar]
- 17. Valla D, Pessegueiro‐Miranda H, Degott C, Lebrec D, Rueff B, Benhamou JP. Hepatic sarcoidosis with portal hypertension.A report of seven cases with a review of the literature. Q J Med 1987;63:531‐544. [PubMed] [Google Scholar]
- 18. Shaker Y, Samy N, Ashour E. Hepatobiliary schistosomiasis. J Clin Transl Hepatol 2014;2:212‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]


