Watch a video presentation of this article
Watch the interview with the author
Ocular changes are associated with a wide spectrum of liver diseases. The early identification of ocular changes may provide clues to the presence of liver disease and lead to early diagnosis, which is particularly important in liver disorders where effective treatments can prevent hepatic injury. Ophthalmic examinations also can be useful in monitoring response to treatment of underlying liver disease. Many ocular manifestations of liver disease can be seen on physical examination without using a slit lamp. A careful history and eye examination can reveal these often subtle findings and aid in the diagnosis or treatment of hepatobiliary disease. This article presents the more common ocular manifestations of liver diseases, the pathology associated with each finding, and the role of the eye examination in clinical medicine.
Xanthelasma
Xanthelasma is a physical examination finding that can be classified both as a dermatological and as an ocular manifestation of liver disease. Xanthelasmas are characterized as soft yellow plaques and can be seen along the medial canthal regions of the eyelids (Fig. 1).
Figure 1.

Xanthelasma evident along the upper and lower portions of the medial eyelid.
Histologically, xanthelasmas are composed of foamy histiocytes or lipid‐laden macrophages.1 They are often bilateral and are not pathognomic for liver disease, because they also can be found in healthy individuals. Typically, xanthelasmas are associated with hyperproteinemias, cholestasis, and primary biliary cholangitis.1 They are benign growths and do not require treatment unless desired for cosmetic reasons. Treatment can include surgical excision, laser, or cryotherapy, although lesions often recur.2
Conjunctival Icterus
The term scleral icterus is a commonly used medical term to describe jaundice present in the eyes, but this is actually a misnomer.3, 4 It is the conjunctiva, not the sclera, that takes on the characteristic yellow hue when plasma bilirubin levels rise. Conjunctival icterus becomes most apparent when bilirubin levels are greater than 2 mg/dL (Fig. 2).3 In patients with dark skin, conjunctival icterus may be the only sign of jaundice on physical examination.
Figure 2.
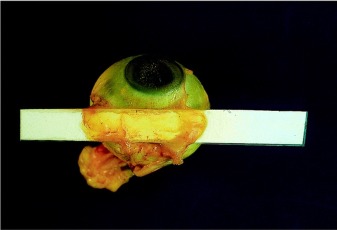
Postmortem photograph of an eye from a patient whose serum bilirubin concentration at the time of death was 374 μmol/L (21.9 mg/dL). A white plastic band has been inserted between the conjunctiva and sclera; sclera at the right margin is free of covering conjunctiva. Reproduced with permission from Annals of Internal Medicine.4 Copyright 2001, American College of Physicians.
Keratoconjunctivitis Sicca (Dry Eye Disease)
Secondary Sjögren syndrome can lead to keratoconjunctivitis sicca, or dry eye disease, and can be caused by primary biliary cholangitis and chronic hepatitis C virus infection.5, 6 Prolonged dry eye can result in a multitude of symptoms including grittiness or foreign body sensation, blurred vision, redness, eyelid crusting, and potentially vision‐threatening epithelial erosions and corneal infections (Fig. 3).5 Keratoconjunctivitis sicca can be treated conservatively with artificial tears but referral to an ophthalmologist or optometrist is necessary if symptoms persist.
Figure 3.
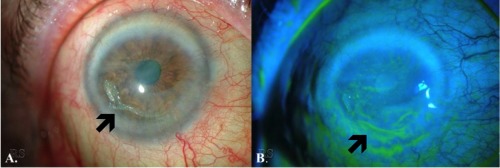
Slit‐lamp photos of a patient with severe, complex surface disease secondary to keratoconjunctivitis sicca. (A) Conjunctival injection, diffuse haze throughout the cornea, corneal neovascularization, and epithelial erosions are evident. (B) Note the epithelial erosions and irregularity shown with fluorescein staining.
Kayser‐Fleischer Rings
Kayser‐Fleischer rings are often thought to be pathognomonic for Wilson's disease and, when observed in a patient, should be considered secondary to Wilson's disease until proved otherwise. Despite their strong association with Wilson's disease, there have been documented cases of Kayser‐Fleischer rings in non‐Wilson's liver disease.7 Kayser‐Fleischer rings rarely can be seen in primary biliary cirrhosis and primary sclerosing cholangitis.6
Kayser‐Fleischer rings are due to copper deposition in Descemet membrane, the basement membrane of the cornea. They are seen in the peripheral cornea and may appear as several different colors, notably ruby red, dark brown, or green. Kayser‐Fleischer rings first occur superiorly and gradually spread circumferentially and inferiorly (Fig. 4).6 Kayser‐Fleischer rings do not affect vision or the health of the cornea. The pigment will gradually resolve with copper‐lowering therapy, and therefore can be used to monitor response to treatment.
Figure 4.
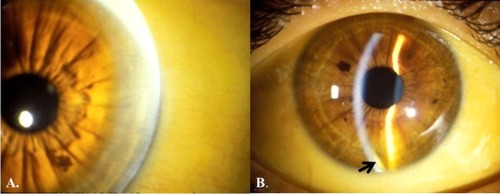
(A) Kayser‐Fleischer rings evident along the peripheral cornea are shown as small, golden granular deposits. (B) In the slit‐lamp photo, the beam on the left is focused on the outer surface of the cornea, whereas the beam on the right is focused more posteriorly along the iris and pupil. Note the golden hue and corneal thickening evident on the inferior aspect of the left beam (arrow).
Cataract
Sunflower cataracts are secondary to copper deposition in the eye and, therefore, another ocular manifestation of Wilson's disease. The appearance of the sunflower cataract actually represents copper deposition in the anterior and posterior lens capsule, not within the lens cortex or nucleus itself.8 Sunflower cataracts, like Kayser‐Fleischer rings, will improve with copper‐lowering therapy and do not have any lasting effects on vision.
Several other liver diseases can cause lens opacities and cataracts, although these are less common. Specific causes of lens opacities include galactosemia, Zellweger hepatocerebrorenal syndrome, neonatal adrenoleukodystrophy, and neonatal hemolytic jaundice syndrome.9
Posterior Embryotoxon
Alagille syndrome is an autosomal dominant cholestatic liver disease associated with multiple ocular abnormalities including keratoconus, refractive errors, band keratopathy, chorioretinal changes, and anomalous optic discs. Although the syndrome is rare, its ocular manifestation, posterior embryotoxon, is present in 95% of patients with Alagille and is therefore a common ocular manifestation of this liver disease.10 Posterior embryotoxon is a corneal finding and represents a thickened and anteriorly displaced termination of Descemet membrane.1 This can be seen on slit‐lamp examination but is not noticeable on general examination with the naked eye.
Any child with prolonged neonatal cholestatic jaundice should be referred to an ophthalmologist for slit‐lamp biomicroscopy to look for the nearly ubiquitous posterior embryotoxon of Alagille syndrome. Screening for Alagille syndrome in these patients could facilitate an early diagnosis and eliminate the need for more extensive testing.10
Cranial Nerve Abnormalities
Liver disease can cause cranial nerve abnormalities that present as gaze palsies or nystagmus. Wilson's disease can cause a horizontal gaze palsy. Wernicke encephalopathy, caused by thiamine deficiency, may be seen with alcoholic liver disease. Wernicke encephalopathy is associated with ocular cranial nerve palsies, ataxia, and nystagmus. Nystagmus is a repetitive, involuntary eye oscillation, which can be either physiological or pathological.11 It is often characterized by a slow phase in which the eyes deviate away from the object of fixation and then a fast, correcting phase. The abnormal eye movement is in the direction of the slow phase, whereas the fast phase represents the eyes correcting to maintain fixed gaze.
Supporting Video 1 shows upbeat nystagmus in a patient with Wernicke encephalopathy. Note the patient also has xanthelasma around the medial eyelids.
A. A. Tooley acquired the data and drafted the manuscript; S. Sweetser critically revised the manuscript for important intellectual content.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Ophthalmic Pathology and Intraocular Tumors. Basic and Clinical Science Course. Ed. Rosa Robert H. San Francisco: American Academy of Ophthalmology, 2015:205‐227. [Google Scholar]
- 2. Bowling B, Kanski JJ. Eyelids In: Kanski's Clinical Ophthalmology: A Systematic Approach, 8th ed. Sydney: Elsevier; 2016. [Google Scholar]
- 3. Tripathi RC. “Conjunctival icterus” not “scleral icterus.” JAMA 1979;242:2558. [PubMed] [Google Scholar]
- 4. Kuiper JJ. Conjunctival icterus. Ann Intern Med 2001;134:345‐346. [DOI] [PubMed] [Google Scholar]
- 5. Bowling B, Kanski JJ. Cornea In: Kanski's Clinical Ophthalmology: A Systematic Approach, 8th ed. Sydney: Elsevier; 2016. [Google Scholar]
- 6. External Disease and Cornea. Basic and Clinical Science Course. Ed. Weisenthal Robert W. San Francisco: American Academy of Ophthalmology, 2015. [Google Scholar]
- 7. Fleming CR, Dickson ER, Wahner HW, Hollenhorst RW, McCall JT. Pigmented corneal rings in non‐Wilsonian liver disease. Ann Intern Med 1977;86:285‐288. [DOI] [PubMed] [Google Scholar]
- 8. Tso MO, Fine BS, Thorpe HE. Kayser‐Fleischer ring and associated cataract in Wilson's disease. Am J Ophthalmol 1975;79:479‐488. [DOI] [PubMed] [Google Scholar]
- 9. O'Neill DP. The eye and liver disorders. Eye 1992;6:366‐370. [DOI] [PubMed] [Google Scholar]
- 10. Hingorani M, Nischal KK, Davies A, Bentley C, Vivian A, Baker AJ, et al. Ocular abnormalities in Alagille syndrome. Ophthalmology 1999;106: 330‐337. [DOI] [PubMed] [Google Scholar]
- 11. Bowling B, Kanski JJ. Neuro‐ophthalmology In: Kanski's Clinical Ophthalmology: A Systematic Approach, 8th ed. Sydney: Elsevier; 2016. [Google Scholar]


