Abstract
BACKGROUND:
Iatrogenic left main coronary artery dissection is a rare complication during invasive coronary procedures. Prompt action is needed avoiding acute pump failure followed with hemodynamic collapse and fatal results.
CASE REPORT:
We report a 48-year-old woman who underwent bail-out stenting.
CONCLUSION:
The best therapeutic strategy depends upon the prompt recognition of this complication, hemodynamic condition of the patient and operative skills. The therapeutic strategy by bail-out stenting should be performed in most cases of severe dissection toward good outcomes.
Keywords: Left main dissection, stenting
Introduction
Iatrogenic left main coronary artery dissection is a rare complication during coronary angiography or angioplasty. The incidence has been reported by about 0.07% [1]. Prompt action is needed because deterioration of antegrade coronary blood flow leads to acute pump failure resulting in hemodynamic collapse and fatal results [2]. Percutaneous coronary intervention (PCI) is considered as the best therapeutic option based on the type of dissection [3].
We report a case of a woman with iatrogenic left main coronary artery dissection treated by percutaneous coronary intervention (PCI).
Case Report
A 48-year-old woman was admitted to our hospital complaining of chest pain and palpitations. Her family history was positive for coronary artery disease. Physical examination was unremarkable while laboratory data showed no abnormal finding. There was no sign of cardiac ischemia on electrocardiography (ECG).
Transthoracic echocardiography demon-strated normal left ventricular function without wall motion abnormalities and no valvular disorder.
Coronary angiography was performed via the right transradial approach. During angiography to engaged the left coronary artery was used a diagnostic 6 Fr left Judkins 4.0 catheter (Medtronic, Inc.) and a diagnostic 6 Fr right Judkins 3.5 catheter (Medtronic, Inc.) for engaging right coronary artery. Angiography of the left coronary artery was normal in the first and last view (LAO caudal and LAO cranial view) (Figure 1A and 1B).
Figure 1.
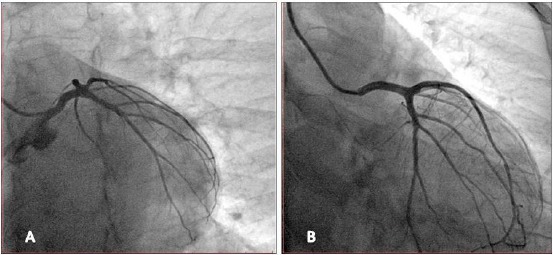
A) Normal left the coronary system in the left anterior oblique, caudal projection; B) Normal left the coronary system in the left anterior oblique, cranial projection
Angiography of the right coronary artery was normal (LAO view) but in the level of the left main (LM) was showed the presence of contrast (Figure 2).
Figure 2.

Normal right coronary artery with the presence of contrast in the level of the left main (LM).
Immediately, the patient complained of severe chest pain, accompanied by ST-segment elevation on the ECG and hemodynamic condition deteriorated.
A right femoral approach was chosen to perform the angiography of the left coronary artery with a 6 Fr 4 JL guiding catheter (Boston Scientific) showing an acute occlusion of the left anterior descending artery (LAD) (Type F) (LAO caudal view) (Figure 3A). A 0.014” choice floppy guidewire was advanced through LMCA into the true lumen of LAD, and a bare metal stent (BMS) 4.5 x 15 mm (Apolo 3, Balton) was placed in left main (LM), re-establishing TIMI 3 flow in LAD (Figure 3B, 3C and 3D).
Figure 3.

Left main dissection and stent placement; A) Left the main dissection followed with LAD occlusion; B) Stent position; C) Deploying stent; D) Left main stented
Post-dilatation was performed with a non-compliant balloon (NC-Quantum Apex, Boston Scientific) 4.5 x 15 mm (Figure 4A and 4B) (caudal view). Final angiography showed good results with TIMI 3 flow across the left coronary artery (Figure 4C, caudal view and 4D, RAO cranial view).
Figure 4.

Balloon post-dilation; A) Balloon position; B) Inflation of balloon; C) Angiography results in caudal view; D) Angiography results in RAO cranial view
The patient was in a stable condition without symptoms after the procedure. She was discharged three days later with optimal medical treatment. At 4-month clinical follow-up, she did not have any symptoms with a good clinical condition.
Discussion
Iatrogenic left main dissection as a life-threatening condition is a rare complication during coronary angiography or angioplasty. Risk factors for left main dissection include coronary artery anomalies, connective tissue disorders-Marfan syndrome, atherosclerotic changes-left main stenosis, arterial hypertension, bicuspid aortic valve, aortic root calcification and older age [4]. Iatrogenic left main dissection results from catheter manipulation, forceful injection of contrast medium, balloon dilatation and stenting [5], [6].
In our case, inappropriate position, deep intubation of the diagnostic catheter and vigorous hand-injection of contrast medium may have caused left the main dissection as a result of increased wall stress. The careful position of the catheter in co-axial alignment with the artery before any vigorous contrast injection cannot be stressed enough [2], [7].
Based on NHLBI classification (The National Heart, Lung and Blood Institute) dissection of the coronary artery is divided into six types (A-F) according to an appearance on coronary angiography [8]. Clinically benign are types A and B, whereas types C through F portend significant morbidity and mortality if untreated [9]. Dunning classification of coronary artery dissection is based on the retrograde extension into the aortic root as a class I-focal dissection restricted to the coronary cusp, class II-involves the cusp and extends up the ascending aorta but is less than 40mm and class III-extends from the coronary cusp up the ascending aorta greater than 40 mm [10]. Eshtehardi's simplified classification according to the extension of left main (LM) ostial dissection includes three types of iatrogenic aortocoronary dissection (IACD): type I-a localized dissection in the LM ostium, type II-extension of the dissection from the LM into the left anterior descending artery (LAD) or left circumflex artery (LCx) and type III-extension of the dissection flap into the aortic root [1].
Left main coronary artery (LMCA) dissection may be followed with different Thrombolysis in Myocardial Infarction (TIMI) grade flow determining hemodynamic stability and clinical picture.
The alternative strategies for the treatment of iatrogenic LMCA dissection are a percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG) and conservative therapy.
Percutaneous coronary intervention (PCI) is preferred in patients hemodynamically unstable in terms of time and technique [11], [12], [13]. The foremost is the successful wiring of the true lumen of the LMCA and its branches considering that the false lumen is usually larger and inadvertent stenting of the false lumen will completely occlude the coronary artery [14].
In an observational study of patients with iatrogenic LM dissection from 38 patients, 1 (3%) patient died before any therapeutic attempt was performed, 6 (16%) patients were treated conservatively, 14 patients were treated by bail-out stenting, and 17 patients were treated by coronary artery bypass grafting (CABG). There was no difference during the 5-year follow-up between bailout stenting and CABG [1]. A review of the literature with 54 patients, 50 patients was treated by bailout stenting, 4 patients were treated by CABG, and there was only 1 cardiac death [2]. In patients with iatrogenic left main coronary artery dissection hemodynamically unstable prompt management by bailout stenting is crucial determining favourable outcomes.
In conclusion, in patients with iatrogenic left main coronary artery dissection to choice, the best treatment strategy is required prompt recognition of this complication, hemodynamic condition of the patient and operative skills. The therapeutic strategy by bail-out stenting should be performed as promptly as possible in hemodynamically unstable patients toward acceptable results.
Authors’ Contributions
HÇ was contributed in the preparation of manuscript and literature analysis. XK was a major contributor in preparation of the manuscript, the design of manuscript and literature analysis. Authors read and approved the final manuscript.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics Approval and Consent to Participate
Approval from our local ethics committee was obtained for publication.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Eshtehardi P, Adorjan P, Togni M, Tevaearai H, Vogel R, Seiler C, Meier B, Windecker S, Carrel T, Wenaweser P, Cook S. Iatrogenic left main coronary artery dissection:incidence, classification, management, and long-term follow-up. American heart journal. 2010;159(6):1147–1153. doi: 10.1016/j.ahj.2010.03.012. https://doi.org/10.1016/j.ahj.2010.03.012 PMid:20569732. [DOI] [PubMed] [Google Scholar]
- 2.Onsea K, Kayaert P, Desmet W, Dubois CL. Iatrogenic left main coronary artery dissection. Netherlands Heart Journal. 2011;19(4):192–195. doi: 10.1007/s12471-011-0089-1. https://doi.org/10.1007/s12471-011-0089-1 PMid:22020998 PMCid:PMC3077877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Celik M, Yuksel UC, Yalcinkaya E, Gokoglan Y, Iyisoy A. Conservative treatment of iatrogenic left main coronary artery dissection:report of two cases. Cardiovascular diagnosis and therapy. 2013;3(4):244. doi: 10.3978/j.issn.2223-3652.2013.10.04. PMid:24400208 PMCid:PMC3878113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Awadalla H, Sabet S, El AS, Rosales O, Smalling R. Catheter-induced left main dissection incidence, predisposition and therapeutic strategies experience from two sides of the hemisphere. The Journal of invasive cardiology. 2005;17(4):233–236. PMid:15831980. [PubMed] [Google Scholar]
- 5.Kovac JD, De Bono DP. Cardiac catheter complications related to left main stem disease. Heart. 1996;76(1):76–78. doi: 10.1136/hrt.76.1.76. https://doi.org/10.1136/hrt.76.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyle AJ, Chan M, Dib J, Resar J. Catheter-induced coronary artery dissection:risk factors, prevention and management. Journal of Invasive Cardiology. 2006;18(10):500. PMid:17015916. [PubMed] [Google Scholar]
- 7.Antoniades D, Apostolakis S, Tzoras S, Lazaridis K. Iatrogenic right coronary artery dissection distal to a total occlusion:a case report. Cases journal. 2009;2(1):6797. doi: 10.4076/1757-1626-2-6797. https://doi.org/10.4076/1757-1626-2-6797 PMid:19829863 PMCid:PMC2740282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rogers JH, Lasala JM. Coronary artery dissection and perforation complicating percutaneous coronary intervention. The Journal of invasive cardiology. 2004;16(9):493–499. PMid:15353832. [PubMed] [Google Scholar]
- 9.Bittl JA, Ryan TJ, Keaney JF, Tcheng JE, Ellis SG, Isner JM, Sanborn TA. Coronary artery perforation during excimer laser coronary angioplasty. Journal of the American College of Cardiology. 1993;21(5):1158–1165. doi: 10.1016/0735-1097(93)90240-2. https://doi.org/10.1016/0735-1097(93)90240-2. [DOI] [PubMed] [Google Scholar]
- 10.Dunning DW, Kahn JK, Hawkins ET, O'Neill WW. Iatrogenic coronary artery dissections extending into and involving the aortic root. Catheterization and Cardiovascular Interventions. 2000;51(4):387–393. doi: 10.1002/1522-726x(200012)51:4<387::aid-ccd3>3.0.co;2-b. https://doi.org/10.1002/1522-726X(200012)51:4<387::AID-CCD3>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 11.Vatrano M, Dattilo G, Mandraffino G, Gangemi S, Ciconte VA, Quartuccio S, Ceravolo R, Imbalzano E. A quick bailout ongoing of cardiogenic shock and iatrogenic dissection of the left main coronary artery. International journal of cardiology. 2015;184:473–474. doi: 10.1016/j.ijcard.2015.03.001. https://doi.org/10.1016/j.ijcard.2015.03.001 PMid:25756567. [DOI] [PubMed] [Google Scholar]
- 12.Cheng CI, Wu CJ, Hsieh YK, Chen YH, Chen CJ, Chen SM, Yang CH, Hung WC, Yip HK, Chen MC, Fu M. Percutaneous coronary intervention for iatrogenic left main coronary artery dissection. International journal of cardiology. 2008;126(2):177–182. doi: 10.1016/j.ijcard.2007.03.125. https://doi.org/10.1016/j.ijcard.2007.03.125 PMid:17490760. [DOI] [PubMed] [Google Scholar]
- 13.Boukhris M, Tomasello SD, Marzà F, Azzarelli S, Galassi AR. Iatrogenic aortic dissection complicating percutaneous coronary intervention for chronic total occlusion. Canadian Journal of Cardiology. 2015;31(3):320–327. doi: 10.1016/j.cjca.2014.11.030. https://doi.org/10.1016/j.cjca.2014.11.030 PMid:25660151. [DOI] [PubMed] [Google Scholar]
- 14.Suarez-Mier MP, Merino JL. False lumen stent placement during iatrogenic coronary dissection. Cardiovascular Pathology. 2013;22(2):176–177. doi: 10.1016/j.carpath.2012.06.002. https://doi.org/10.1016/j.carpath.2012.06.002 PMid:23153587. [DOI] [PubMed] [Google Scholar]


