Abstract
Introduction
African Americans (AAs) have the highest risk of developing heart failure (HF) among all ethnicities in the United States and are associated with higher rates of readmissions and mortality. This study aims to determine the prevalence and relationship of common psychiatric conditions to outcomes of patients hospitalized with HF.
Hypothesis
Psychiatric conditions lead to worse outcomes in HF patients.
Methods
This single‐center retrospective study enrolled 611 AA patients admitted to an urban teaching community hospital for HF from 2010 to 2013. Patient demographics, clinical variables, and history of psychiatric disorders were obtained. Cox proportional hazards regression was used to assess impact of psychiatric disorders on readmission rates and mortality.
Results
The mean age was 66 ± 15 years; 53% were men. Median follow‐up time from index admission for HF was 3.2 years. Ninety‐seven patients had a psychiatric condition: 46 had depression, 11 had bipolar mood disorder (BMD), and 40 had schizophrenia. After adjustment of known risk factors and clinical metrics, our study showed that AA HF patients with a psychiatric illness were 3.84× more likely to be admitted within 30 days for HF, compared with those without (P < 0.001). Individually, adjusted Cox multivariable logistic regression analysis also showed that, for 30‐day readmission, schizophrenia had a hazard ratio (HR) of 4.92 (P < 0.001); BMD, an HR of 3.44 (P = 0.02); and depression, an HR 3.15 (P = 0.001). No associations were found with mortality.
Conclusions
Psychiatric conditions of schizophrenia, BMD, and depression were significantly associated with a higher 30‐day and overall readmission rate for HF among AA patients.
Keywords: African American, Bipolar Mood Disorder, Depression, Heart Failure, Mortality, Readmission Rate, Schizophrenia
1. INTRODUCTION
Heart failure (HF) is the leading cause of hospitalization and readmissions in the United States.1, 2 HF accounted for >$30 billion in healthcare costs in 2012. This is projected to increase by 127% through 2030, amounting to >$70 billion, due to an estimated increase of 46% in prevalence of HF.3 African Americans (AAs) have the highest risk of developing HF among all ethnicities, occurring in about 4.6 per 1000 person‐years.4 AAs are also more likely to be hospitalized and readmitted for HF compared with other races.5 Although the overall rate of hospitalization for HF has declined substantially from 1998 to 2008, the rate reduction is much lower for AA males.6
Research both at the national and community level has focused on efforts to predict which patients with HF are likely to be readmitted and to devise novel strategies to prevent such readmissions. Socioeconomic factors have been implicated in this racial disparity. Living alone and/or being unmarried resulted in higher readmissions and mortality in the AA population.7 The impact of psychological factors on cardiac function has been studied extensively in areas such as coronary artery diseases (CAD) and myocardial infarction,8 but not as much in HF patients. Depression is associated with worse outcomes in HF patients, and the relationship is strong and consistent across multiple clinical outcomes including rehospitalization and mortality, according to one meta‐analysis.9 However, the association of other psychiatric disorders and these outcomes still remains unclear. This study aims to determine whether AA HF patients with a psychiatric disorder have higher readmissions and mortality following hospitalization for acute decompensated heart failure (ADHF) compared with those without any psychiatric illness.
2. METHODS
The study sample was retrospectively selected from a cohort of adult AA patients (age > 20 years) who were hospitalized at Einstein Medical Center in Philadelphia between January 1, 2011, and February 28, 2013, with a primary discharge diagnosis of ADHF. Patients who had end‐stage renal disease on dialysis and those with life‐limiting disease such as malignancy were excluded from the study. A total of 611 AA patients were included in the study. Baseline demographic characteristics at the time of first admission, risk factors for cardiovascular disease (CVD), and other comorbidities were abstracted from electronic medical records. Chronic medical conditions were defined by either physician documentation of the condition or treatment with appropriate medical therapy. Psychiatric disease was defined as having a documented history of schizophrenia, depression, and/or bipolar mood disorder (BMD). Mortality was determined at the end date of this study (August 31, 2015) via query of the Social Security Death Index and review of hospital records.
The primary endpoint was 30‐day readmission, specifially for ADHF only. A 30‐day readmission was defined as a subsequent hospital admission within 30 days after discharge day of index admission. The secondary endpoints were any readmission during the study period and all‐cause mortality. This project was approved by the institutional review board of the Einstein Healthcare Network.
2.1. Statistical analysis
Demographic and clinical characteristics were summarized using descriptive statistics. Continuous variables were expressed as mean ± SD and compared using the Student t test (with Welch's approximation in case of unequal variances). Categorical variables were expressed as percentages and compared using the χ2 or Fisher exact test. Cox proportional hazards regression was used to evaluate the association between the presence of major psychiatric illnesses and 30‐day readmission. Time to first 30‐day readmission was used as the time to event variable. Data was right censored at 30 days or at the day of death, whichever occurred earlier. Psychiatric illness was analyzed as a binary (presence or absence) and a categorical variable (no psychiatric illness, schizophrenia, anxiety/depression, BMD), in separate models. Patient characteristics at the time of first admission (eg, age, sex, peak troponin I [TnI], left ventricular ejection fraction [LVEF], B‐type natriuretic peptide [BNP], and major comorbidities such as hypertension [HTN], diabetes mellitus [DM], chronic kidney disease [CKD], and CAD) and social characteristics (eg, living situation and marital status) were included as covariates in the model to provide an adjusted hazard ratio (HR). Similar analysis was also conducted for secondary outcomes. A P value <0.05 was considered statistically significant. All statistical analyses were performed using Stata version 13.0 (StataCorp LP, College Station, TX).
3. RESULTS
3.1. Patient demographics
A total of 611 AA patients were included in the study. Clinical characteristics of the study population are reported in Table 1. The mean age of the cohort was 66 ± 15 years (median, 67 years); 53% were male. The median follow‐up time from the index admission for ADHF was 3.2 years (maximum follow‐up, 4.6 years). Sixteen percent of the subjects (n = 97) had a psychiatric illness: 40 patients had schizophrenia of various types, 11 had BMD, and 46 patients carried a diagnosis of depression. As shown in Table 1, baseline demographics and comorbidities such as HTN, DM, dyslipidemia, CKD, and obstructive sleep apnea were similar in the 2 groups. There was no statistically significant difference in LVEF, peak serum TnI, and BNP measurement between the 2 groups.
Table 1.
Baseline characteristics of patients
| No Psychiatric Illness, n = 514 | With Psychiatric Illness, n = 97 | P Value | |
|---|---|---|---|
| Demographics | |||
| Age, y | 65.8 (15.2) | 63.9 (15.3) | 0.27 |
| Male sex | 52.5 | 54.6 | 0.70 |
| BMI, kg/m2 | 30.5 (10.4) | 29.5 (8.9) | 0.39 |
| General medical history | |||
| Medication compliance | 62.6 | 64.9 | 0.65 |
| HTN | 93.9 | 94.9 | 0.73 |
| DM | 55.5 | 53.6 | 0.74 |
| Dyslipidemia | 46.1 | 43.3 | 0.61 |
| CKD | 35.6 | 35.1 | 0.92 |
| OSA | 13 | 18.6 | 0.15 |
| CAD | 39.2 | 35.1 | 0.44 |
| Clinical metrics | |||
| LVEF, % | 32.4 (16.5) | 29.3 (14.6) | 0.09 |
| BNP, pg/mL | 1126.9 (987.5) | 1032.4 (945.9) | 0.39 |
| Peak Tn level, ng/mL | 0.19 (1.1) | 0.26 (0.8) | 0.53 |
| Length of stay, d | 5.6 (5.9) | 4.9 (3.8) | 0.21 |
Abbreviations: BNP, B‐type natriuretic peptide; CAD, coronary artery disease; CKD, chronic kidney disease; DM, diabetes mellitus; HTN, hypertension; LVEF, left ventricular ejection fraction; OSA, obstructive sleep apnea; SD, standard deviation; Tn, troponin.
Data are reported as % or mean (SD).
3.2. Thirty‐day readmission
Approximately 32% of the patients who had a psychiatric illness were readmitted within 30 days (n = 32), as compared with only 11% of those without any psychiatric illness (n = 53). After adjusting for known risk factors and clinical metrics, our study showed that AA HF patients who carry a diagnosis of psychiatric illness were 3.84× more likely (HR: 3.84, 95% confidence interval [CI]: 2.32‐6.35, P < 0.00) to be readmitted within 30 days for ADHF compared with their normal counterparts. The Kaplan–Meier curve for 30‐day readmission stratified according to the presence or absence of major psychiatric illness is shown in section A of the Figure.
Psychiatric illness was also analyzed as a categorical variable, with no psychiatric illness being the reference category. After adjusting for age, sex, peak TnI, LVEF, BNP, and traditional risk factors (such as HTN, DM, hyperlipidemia, and CAD), the factors independently associated with an increased hazard of 30‐day readmission, compared with patients with no psychiatric illness, were schizophrenia (HR: 4.92, 95% CI: 2.49‐9.71, P < 0.001), BMD (HR: 3.44, 95% CI: 1.19‐10.00, P = 0.02), and depression (HR: 3.15, 95% CI: 1.55‐6.39, P = 0.001; Table 2).
Table 2.
Results of multivariate Cox proportional hazards model examining the relationship between individual psychiatric disorders (schizophrenia, depression, and BMD) with 30‐day readmission for ADHF
| HR | 95% CI | P Value | |
|---|---|---|---|
| Patient demographics | |||
| Age | 1.01 | 0.99‐1.03 | 0.28 |
| Make sex | 1.37 | 0.81‐2.30 | 0.24 |
| Comorbidities | |||
| HTN | 0.71 | 0.25‐2.00 | 0.58 |
| DM | 1.15 | 0.69‐1.93 | 0.69 |
| CKD | 1.11 | 0.66‐1.85 | 0.64 |
| CAD | 1.55 | 0.94‐2.56 | 0.09 |
| Clinical Metrics | |||
| LVEF | 1.01 | 1.00‐1.00 | 0.12 |
| BNP | 1.00 | 1.00‐1.00 | 0.06 |
| Peak Tn level | 0.95 | 0.76‐1.19 | 0.76 |
| Living situation | |||
| Lives alone | Ref | ||
| Living with family | 0.34 | 0.18‐0.64 | 0.001 |
| Nursing home resident | 0.50 | 0.23‐1.13 | 0.096 |
| Psychiatric disorders | |||
| No major psychiatric illness | Ref | ||
| Depression | 3.15 | 1.55‐6.39 | 0.001 |
| BMD | 3.44 | 1.19‐10.00 | 0.02 |
| Schizophrenia | 4.92 | 2.49‐9.71 | <0.001 |
Abbreviations: ADHF; acute decompensated heart failure; BMD, bipolar mood disorder; BNP, B‐type natriuretic peptide; CAD, coronary artery disease; CI, confidence interval; CKD, chronic kidney disease; DM, diabetes mellitus; HR, hazard ratio; HTN, hypertension; LVEF, left ventricular ejection fraction; Ref, referent; Tn, troponin.
3.3. Readmission over the entire study period
Over the mean follow‐up time of 3.2 years, 77% of patients (n = 75) who carried a diagnosis of psychiatric illness were readmitted at least once, as compared with 57% (n = 293) of those who did not have any psychiatric disease. After adjusting for age, sex, peak TnI, LVEF, BNP, and traditional risk factors (HTN, DM, hyperlipidemia, and CAD), presence of a psychiatric illness was independently associated with an increased risk of rehospitalization for ADHF (HR: 1.94, 95% CI: 2.32‐6.35, P < 0.001). This association remained significant even when the psychiatric illnesses were taken separately (Table 3). The Kaplan–Meier curve for hospital‐free survival stratified according to the presence or absence of major psychiatric illness is shown in section B of the Figure.
Table 3.
Results of the multivariable Cox proportional hazards model examining the relation of the presence of schizophrenia, depression, and BMD to readmission for ADHF
| HR | 95% CI | P Value | |
|---|---|---|---|
| Patient demographics | |||
| Age | 1.00 | 0.99‐1.00 | 0.93 |
| Male sex | 1.05 | 0.83‐1.33 | 0.67 |
| Comorbidities | |||
| HTN | 1.18 | 0.71‐1.98 | 0.58 |
| DM | 1.18 | 0.93‐1.50 | 0.69 |
| CKD | 1.43 | 1.12‐1.83 | 0.64 |
| CAD | 1.39 | 1.10‐1.765 | 0.09 |
| Clinical metrics | |||
| LVEF | 1.00 | 0.99‐1.01 | 0.12 |
| BNP | 1.00 | 1.00‐1.00 | 0.06 |
| Peak Tn level | 0.97 | 0.86‐1.10 | 0.76 |
| Living situation | |||
| Lives alone | Ref | ||
| Living with family | 0.73 | 0.56‐0.95 | 0.02 |
| Nursing home resident | 0.70 | 0.46‐1.07 | 0.10 |
| Psychiatric disorders | |||
| No major psychiatric illness | Ref | ||
| Depression | 1.69 | 1.15‐2.47 | 0.007 |
| BMD | 2.08 | 1.05‐4.11 | 0.03 |
| Schizophrenia | 2.33 | 1.51‐3.61 | <0.001 |
Abbreviations: ADHF; acute decompensated heart failure; BMD, bipolar mood disorder; BNP, B‐type natriuretic peptide; CAD, coronary artery disease; CI, confidence interval; CKD, chronic kidney disease; DM, diabetes mellitus; HR, hazard ratio; HTN, hypertension; LVEF, left ventricular ejection fraction; Ref, referent; Tn, troponin.
3.4. Mortality
A total of 175 subjects died during the study period. In our multivariate Cox proportional hazards analysis, having psychiatric illness was not associated with increased all‐cause mortality (HR: 1.27, 95% CI: 0.82‐1.97, P = 0.28). The variables that were associated with increased all‐cause mortality were age, with a HR of 1.04 for every 1‐year increment in age (95% CI: 1.02‐1.05, P = 0.001) and having CAD (HR: 1.52, 95% CI: 1.09‐2.15, P = 0.01).
4. DISCUSSION
The major findings of our study are as follows: AA HF patients with psychiatric conditions had significantly higher readmission rates, particularly 30‐day readmission, than did those without any psychiatric condition. AA HF patients with schizophrenia were 4.9× more likely to be readmitted within 30 days than were those without any psychiatric illness. AA HF patients with BMD were 3.4× and those with depression were 3.1× more likely to be readmitted within 30 days for ADHF after their index admission. Of note, living with family was significantly associated with a lower 30‐day readmission risk compared with patients living alone. This result has already been previously reported in a study done by the authors.7 Lastly, having any psychiatric condition was not associated with a significant increase in all‐cause mortality. Our study is one of the first to show an association between major psychiatric disorders and worse outcomes among AA patients with HF.
Figure 1.
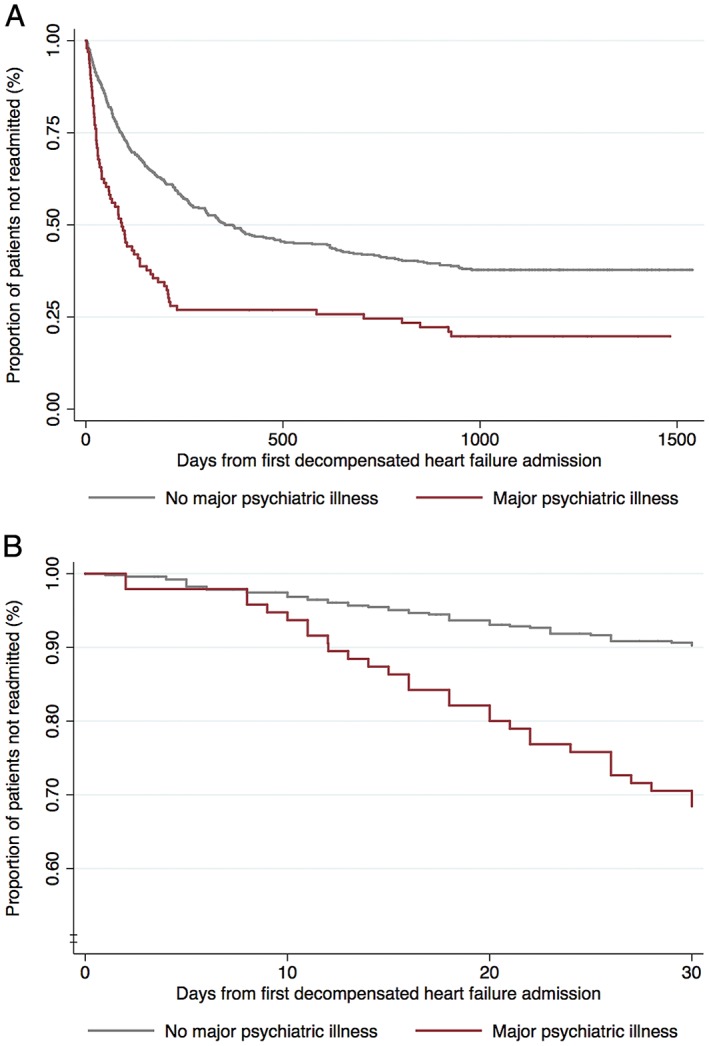
(A) Kaplan–Meier survival analysis demonstrating 30‐day hospital‐free survival for patients stratified by presence of psychiatric illness. (B) Kaplan–Meier survival analysis demonstrating hospital‐free survival for patients stratified by presence of psychiatric illness
This study builds on previous studies regarding the impact of depression among HF patients. Depression has been demonstrated to have worse outcomes, such as increased mortality and readmissions, and poorer prognosis, in HF patients.9, 10, 11, 12, 13, 14, 15 The higher risk of readmissions in patients with depression is also seen in other chronic medical conditions such as chronic obstructive pulmonary disease.16 Mortality seems to increase in a graded fashion with increasing severity of depression.11 The mechanism for these poorer outcomes in depressed HF patients may involve several factors. Studies have shown that they have higher rates of medication nonadherence,13 impaired self‐care ability,15 poor intimate social support,17 poor perceived quality of life,18 and limited ability to learn and retain educational content, such as understanding discharge instructions.19 In our study, depression in the AA population was significantly associated with increased 30‐day readmission rate and overall readmission rate, with HRs of 3.15 and 1.69, respectively, and was comparable with the general population.10
Studies done on the effects of having BMD on HF outcomes are scarce, and most of the available literature focuses on the relationship of this psychiatric disease with CVD in general. In our study, patients with BMD were 2.08× more likely to be readmitted for ADHF than were those without any psychiatric disorder. They also had a significantly higher hazard of 30‐day readmission, with an HR of 3.44, compared with their counterparts. Our study is the first to show an association between BMD in HF patients and increased readmission rate. The exact reasons for such a high readmission risk remain unclear but may be due to poor compliance and outpatient follow‐up. Cradock‐O'Leary et al. demonstrated that patients with BMD have been shown to have poor outpatient follow‐up even when access to medical care is readily available, using the Veterans Affairs health system data.20
Patients with schizophrenia have a lower life expectancy than the general population, secondary to a higher prevalence of CVD.21 However, no studies have examined the impact of schizophrenia on HF morbidity and mortality. In our study, HF patients with schizophrenia had the highest risk of 30‐day readmission, with a HR of 4.92. However, we found no association between schizophrenia and all‐cause mortality.
Research on psychotropic medications suggest they could play a role in cardiovascular risks in patients on therapy. Antipsychotics such as quetiapine and most tricyclic antidepressants have potent α‐1 blockade activity and can cause significant orthostatic hypotension and intolerance to diuretics.22 An in vitro study found that tricyclic antidepressants decrease myocardial contractility in a dose‐dependent manner.23 Outcomes data, however, fail to support these claims. A review of randomized controlled trials found that tricyclic antidepressants and selective serotonin reuptake inhibitors were associated with similar rates of major adverse cardiovascular events (such as HF, myocardial infarction, stroke, or cardiovascular death).24 However, that systematic review could not determine whether these medications were associated with risk of cardiovascular adverse effects, due to the rarity of the serious adverse effects and the scarcity of large trials concerning these patients. In another cohort, depression, but not antidepressant or selective serotonin reuptake inhibitor use, was independently associated with increased mortality.25
It would be interesting to understand whether intensive outpatient psychiatric rehabilitation would significantly impact readmission. The 2013 American College of Cardiology Foundation/American Heart Association HF guidelines already recommend scheduling an early follow‐up visit within 7 to 14 days of hospital discharge for ADHF.26 However, written instructions alone may not be sufficient in this group of patients. According to a study published in the Journal of the American Medical Association, one of the best strategies to decrease hospital readmission is to focus and identify unrecognized high‐risk groups and to match the intensity of interventions, both pharmacologic and nonpharmacologic, to the risk of readmission.27 We believe that patients with high psychiatric‐disease burden are part of the “unrecognized high‐risk” patients. They should be identified early during the index admission to create post‐discharge support systems, such as home‐health services, to make sure they have appropriate outpatient follow‐up. Multiple phone calls and home visits may be necessary to make sure that they are compliant with diet and guideline‐directed medical therapy. Caution should be exercised in the reconciliation of cardiac and psychotropic medications because of the potential interactions. A consult to a psychiatrist can be sought when necessary. The role of a psychiatrist and psychiatric rehabilitation may be more significant than originally anticipated. Social support may also be a key factor in reducing morbidity and mortality of these patients. Our findings reinforce the importance of psychosocial research in HF populations. We have included these issues in our discussion.
4.1. Study limitations
This is a retrospective study, and as such it is possible that not all clinically relevant data were collected. Among such unavailable relevant data were compliance with diet and appointments with the primary‐care provider and cardiologist, type of insurance, annual income, and homelessness. We relied on accurate documentation and record‐keeping of a history of psychiatric disease. Being a single‐center study, we were only able to capture readmissions to our institution. The Social Security Death Index database is only publicly available for deaths before or during 2011 annd could have significantly impacted our study results. Our study sample is homogenously AA, and the results of this study may not be generalizable to other patient populations. Our study also did not include information regarding compliance with or use of psychiatric medications. It would be interesting to determine whether compliance would make a positive impact on decreasing readmission rate.
5. CONCLUSION
Psychiatric conditions of schizophrenia, BMD, and depression were significantly associated with a higher 30‐day and overall readmission rate for ADHF among AA patients. Our findings reinforce the importance of psychosocial research in HF populations. Treating these patients' psychiatric diseases could lead to a lower readmission rate and better outcomes.
Conflicts of interest
The authors declare no potential conflicts of interest.
Lu MLR, De Venecia TA, Goyal A, et al. Psychiatric conditions as predictors of rehospitalization among African American patients hospitalized with heart failure. Clin Cardiol. 2017;40:1020–1025. 10.1002/clc.22760
REFERENCES
- 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for service program [published correction appears in N Engl J Med. 2011;364:1582]. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 2. Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation. 2012;126:501–506. [DOI] [PubMed] [Google Scholar]
- 3. Heidenreich PA, Albert NM, Allen LA, et al; on behalf of the American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council . Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bahrami H, Kronmal R, Bluemke DA, et al. Differences in the incidence of congestive heart failure by ethnicity: the Multi‐Ethnic Study of Atherosclerosis. Arch Intern Med. 2008;168:2138–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mitchell JE, Ferdinand KC, Watson KE, et al. Treatment of heart failure in African Americans—a call to action. J Natl Med Assoc. 2011;103:86–98. [DOI] [PubMed] [Google Scholar]
- 6. Chen J, Normand SL, Wang Y, et al. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. JAMA. 2011;306:1669–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lu ML, Davila CD, Shah M, et al. Marital status and living condition as predictors of mortality and readmissions among African Americans with heart failure. Int J Cardiol. 2016;222:313–318. [DOI] [PubMed] [Google Scholar]
- 8. Friedman M, Thorensen CE, Gill JJ, et al. Alteration of type A behavior and its effect on cardiac recurrences in post–myocardial infarction patients: summary results of the Recurrent Coronary Prevention Project. Am Heart J. 1986;112:653–665. [DOI] [PubMed] [Google Scholar]
- 9. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure: a meta‐analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. [DOI] [PubMed] [Google Scholar]
- 10. Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. [DOI] [PubMed] [Google Scholar]
- 11. Jiang W, Kuchibhatla M, Clary GL, et al. Relationship between depressive symptoms and long‐term mortality in patients with heart failure. Am Heart J. 2007;154:102–108. [DOI] [PubMed] [Google Scholar]
- 12. Riegel B, Moser DK, Anker SD, et al. State of the science: promoting self‐care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141–1163. [DOI] [PubMed] [Google Scholar]
- 13. Morgan AL, Masoudi FA, Havranek EP, et al; Cardiovascular Outcomes Research Consortium . Difficulty taking medications, depression, and health status in heart failure patients. J Card Fail. 2006;12:54–60. [DOI] [PubMed] [Google Scholar]
- 14. Lesman‐Leegte I, van Veldhuisen DJ, Hillege HL, et al. Depressive symptoms and outcomes in patients with heart failure: data from the COACH study. Eur J Heart Fail. 2009;11:1202–1207. [DOI] [PubMed] [Google Scholar]
- 15. Holzapfel N, Löwe B, Wild B, et al. Self‐care and depression in patients with chronic heart failure. Heart Lung. 2009;38:392–397. [DOI] [PubMed] [Google Scholar]
- 16. Chatterjee K, Goyal A, Joshi M. Thirty‐day readmissions in adults hospitalized for COPD or bronchiectasis: findings from the Nationwide Readmission Database 2013. Chest. 2017;151:943–945. [DOI] [PubMed] [Google Scholar]
- 17. Murberg TA, Bru E, Svebak S, et al. Depressed mood and subjective symptoms as predictors of mortality in patients with congestive heart failure: a two‐year follow‐up study. Int J Psychiatry Med. 1999;29(3):311–326. [DOI] [PubMed] [Google Scholar]
- 18. Dracup K, Walden JA, Stevenson LW, et al. Quality of life in patients with advanced heart failure. J Heart Lung Transplant. 1992;11(2 part 1):273–279. [PubMed] [Google Scholar]
- 19. Moser DK, Doering LV, Chung ML. Vulnerabilities of patients recovering from an exacerbation of chronic heart failure. Am Heart J. 2005;150:984. [DOI] [PubMed] [Google Scholar]
- 20. Cradock‐O'Leary J, Young AS, Yano EM, et al. Use of general medical services by VA patients with psychiatric disorders. Psychiatr Serv. 2002;53:874–878. [DOI] [PubMed] [Google Scholar]
- 21. Hennekens CH, Hennekens AR, Hollar D, et al. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150:1115–1121. [DOI] [PubMed] [Google Scholar]
- 22. McLaren KD, Marangell LB. Special considerations in the treatment of patients with bipolar disorder and medical comorbidities. Ann Gen Hosp Psychiatry. 2004;3:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Heard K, Cain BS, Dart RC, et al. Tricyclic antidepressants directly depress human myocardial mechanical function independent of effects on the conduction system. Acad Emerg Med. 2001;8:1122–1127. [DOI] [PubMed] [Google Scholar]
- 24. Swenson JR, Doucette S, Fergusson D. Adverse cardiovascular events in antidepressant trials involving high‐risk patients: a systematic review of randomized trials. Can J Psychiatry. 2006;51:923–929. [DOI] [PubMed] [Google Scholar]
- 25. O'Connor CM, Jiang W, Kuchibhatla M, et al. Antidepressant use, depression, and survival in patients with heart failure. Arch Intern Med. 2008;168:2232–2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810–1852. [DOI] [PubMed] [Google Scholar]
- 27. Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost‐effectiveness. JAMA Intern Med. 2013;173:695–698. [DOI] [PubMed] [Google Scholar]


