Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- ESLD
end‐stage liver disease
- LT
liver transplantation
- PC
palliative care
The debilitating complications of end‐stage liver disease (ESLD) are associated with substantial symptom burden. These symptoms are often suboptimally controlled, resulting in poor quality of life among those with ESLD (Fig. 1).1, 2
Figure 1.
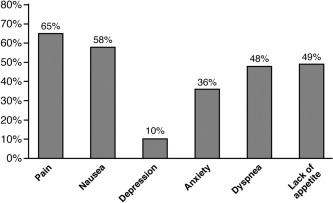
Symptomatology in patients with palliative cirrhosis according to (revised) Edmonton Symptom Assessment System (ESAS)..2
What Is Palliative Care?
Palliative care (PC) is defined as “patient and family‐centered care that optimizes quality of life by anticipating, preventing, and treating suffering” and should be considered for patients with advanced chronic illness, at any point in disease trajectory.3 In contrast, hospice, which is a component of PC, is appropriate for those whose life expectancy is less than 6 months. Addressing end‐of‐life issues through PC or hospice referral provides improved communication between patients, their caregivers, and their healthcare team; reduces symptom burden; and enhances quality of life.4 In other diseases (non–small cell lung cancer, pancreatic cancer, congestive heart failure), PC and hospice can prolong life as well.5, 6 From an institutional perspective, PC consultation can also be cost‐saving (Fig. 22).7 Despite all of this, end‐of‐life issues for patients with cirrhosis are often not addressed until too late, if at all.8
Figure 2.

Mean direct costs per day for palliative care (PC) patients (with any chronic condition) who were (A) discharged alive or (B) died before and after PC consultation. The solid line and dotted lines represent 2 different ways of estimating costs if PC consultation had not occurred.7
Utilization of PC in ESLD
A recent study by Poonja et al. demonstrated that, among patients with decompensated cirrhosis with no curative options (ie, removed from the liver transplantation < waiting list or declined for transplant), only 11% were referred for PC.2 Of those, only 28% had documented do not resuscitate (DNR) status. Our group demonstrated a similarly low utilization rate of PC services among veterans with cirrhosis who died within 1 year of cirrhosis diagnosis: only 7.5% received PC services and, when they did, it was very late in their disease trajectory (median of 32 days from PC consultation to death) (Rakoski, unpublished data).
Barriers to PC
There is little literature that has explored barriers to PC utilization among patients with ESLD. The following are potential barriers (Table 1).
Table 1.
Potential Barriers to Utilization of PC Services
| Barrier | Mechanism |
|---|---|
| Disease | Unpredictable episodes of decompensation |
| Patient |
Lack of knowledge of disease severity Uncertainty about prognosis Focus on liver‐saving interventions Distrust and misperception of PC (“death panels”) |
| Physician |
Overestimation of life expectancy Misperception of PC Discomfort with end‐of‐life discussions Poor prognosis communication with patient Focus on liver‐saving interventions Confusion regarding indications for PC referral |
| Access | Improving, but potentially inadequate, access to PC services |
Disease Factors
Unlike the progressive decline that occurs with cancer, ESLD is characterized by periods of relative stability interposed with episodes of hepatic decompensation that can result in rapid decline and death.
Patient Factors
Patients may have poor understanding of liver disease severity and prognosis, due to inadequate physician communication or poor health literacy. When faced with life‐limiting illness, some patients may also refuse to accept prognosis. For some patients and their families, the prospect of a life‐saving intervention such as LT precludes consideration of any treatment focus that does not offer prolongation of life or cure. Misperception of PC (“death panels”) and its association with “giving up” may also contribute to underutilization.9 All of these issues may be further exacerbated by hepatic encephalopathy and the associated uncertainty about decisional capacity.
Physician Factors
In a web‐based survey of intensive care nurses, house officers, and attendings at a large liver transplant center, 84% of respondents indicated that the greatest barrier to PC involvement in patients with ESLD was the attending physician.10 Potential physician‐related barriers are multiple and well described in other diseases: overestimation of life expectancy, misperception of or unfavorable attitudes towards PC services, discomfort with end‐of‐life discussions.11, 12 This discomfort with end‐of‐life discussions can be particularly challenging for a hepatologist who is working with their patient toward a mutual curative goal such as LT. Suboptimal end‐of‐life physician communication can result in patients being unaware of their prognosis as well as physicians being unaware of their patient's end‐of‐life preferences.13 Uncertainty and confusion about how and when to integrate PC into standard ESLD management may also result in under‐referral,10 indicating the need for guidelines to help guide timely and appropriate referral.
Access to PC
Although the number of PC programs is increasing and the field of hospice and palliative medicine has recently been granted subspecialty status, there remains a discrepancy between the need for PC services and access to these subspecialists. In 2012, only two‐thirds of hospitals with more than 50 beds had PC programs, and access remains limited in smaller community hospital settings.14
Indications for PC in Patients with ESLD
A PC referral may be helpful for any patient with a life‐limiting illness who is experiencing suffering of any kind (physical, emotional, spiritual, intrafamily conflict). The following are conditions for which a PC referral for a patient with ESLD could be considered:
Uncontrolled physical symptoms related to ESLD (eg, pain, cramping, nausea, anorexia)
Patient emotional or spiritual distress (eg, fear of dying; guilt about prior behaviors like alcohol abuse that led to ESLD)
Family/caregiver emotional or spiritual distress (eg, financial distress from taking off from work to care for patient; strain associated with fluctuating mental status and unpredictable hospitalizations15)
Intrafamily conflict about goals of care (eg, patient has severe hepatic encephalopathy or is intubated and family is uncertain of patient's desire for LT)
Accelerating need for medical care or hospitalizations (eg, refractory ascites requiring weekly paracenteses)
Medical team has declined curative or life‐sustaining treatment (eg, patient denied LT listing or removed from the transplant list)
Patient has declined life‐sustaining treatments
Physician distress about caring for this patient (eg, difficulty communicating a grim prognosis or lack of curative options)
PC and LT: Divergent or Complementary?
For some, LT and PC seem like divergent treatment philosophies, especially among those who equate PC with end‐of‐life care.16 When pursuing life‐saving interventions such as transplantation, transplant physicians may feel compelled to use medical innovation to its fullest extent in order to prolong life, even when these efforts become increasingly futile. The typical role of PC in LT involves consultation at the time when a patient's medical condition deteriorates to the point that LT is no longer an option, which is often only weeks to days before death. These barriers lead to denial of valuable PC services for those who need it most. Another way to view PC in this setting is as a tool to help patients and families cope with the fear, uncertainty, and loss of control inherent in the transplant waiting process.17 When viewed in this light, PC may be seen as a valuable addition to LT services. This viewpoint is consistent with the National Consensus Project for Quality Palliative Care Clinical Practice Guidelines,3 which advocates for PC across the illness trajectory, and has been successfully implemented in some programs.18
Future Directions
Several possible avenues exist to improve the provision of PC to patients with ESLD. One would be to enhance training in PC skills (eg, communication, pain management) among gastroenterology and hepatology fellows, as well as practicing hepatologists. This approach would allow continued patient‐physician relationships with a hepatology provider that has familiarity with disease trajectory. However, constraints of managing multiple medical issues during each encounter would likely preclude adequate time for comprehensive PC. For this reason, PC consultation may enhance this important aspect of patient care, ideally in close partnership with hepatology. In addition to such novel clinical programs, more research is needed about the unmet needs and barriers/facilitators to PC in this population.
Potential conflict of interest: Nothing to report.
References
- 1. Rakoski MO, McCammon RJ, Piette JD, Iwashyna TJ, Marrero JA, Lok AS, et al. Burden of cirrhosis on older Americans and their families: Analysis of the health and retirement study. Hepatology 2012;55:184‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Poonja Z, Brisebois A, van Zanten SV, Tandon P, Meeberg G, Karvellas CJ. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clin Gastroenterol Hepatol 2014;12:692‐698. [DOI] [PubMed] [Google Scholar]
- 3.The National Consensus Project for Quality Palliative Care Clinical Practice Guidelines for Quality Palliative Care, 3rd edition. 2013. (www.nationalconsensusproject.org/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf). Accessed March 12, 2015.
- 4. Manfredi PL, Morrison RS, Morris J, Goldhirsch SL, Carter JM, Meier DE. Palliative care consultations: how do they impact the care of hospitalized patients. J Pain Symptom Manage 2000;20:166‐173. [DOI] [PubMed] [Google Scholar]
- 5. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non‐small‐cell lung cancer. N Engl J Med 2010;363:733‐742. [DOI] [PubMed] [Google Scholar]
- 6. Connor SR, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and nonhospice patient survival among patients who die within a three year window. J Pain Symptom Manage 2007;33:238‐246. [DOI] [PubMed] [Google Scholar]
- 7. Morrison RS, Penrod JD, Cassel JB, Caust‐Ellenbogen M, Litke A, Spragens L, et al; Palliative Care Leadership Centers’ Outcomes Group. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 2008;168:1783‐1790. [DOI] [PubMed] [Google Scholar]
- 8. Larson AM, Curtis JR. Integrating palliative care for liver transplant candidates: “Too well for transplant, too sick for life.” JAMA 2006;295:2168‐2176. [DOI] [PubMed] [Google Scholar]
- 9. Cagle JG, Van Dussen DJ, Culler KL, Carrion I, Hong S, Guralnik J, Zimmerman S. Knowledge about hospice: Exploring misconceptions, attitudes, and preferences for care. Am J Hosp Palliat Care 2014; doi: 10.1177/1049909114546885. [DOI] [PubMed] [Google Scholar]
- 10. Beck K, O'Riordan D, Peters M, Pantilat S. Expanding access to palliative care consultation for patients with end‐stage liver disease: survey of liver transplant service providers. J Pain Symptom Manage 2014:47;468‐469. [Google Scholar]
- 11. Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ 2000;320:469‐473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brickner L, Scannell K, Marquet S, Ackerson L. Barriers to hospice care and referrals: survey of physicians' knowledge, attitudes, and perceptions in a health maintenance organization. J Palliat Med 2004;7:411‐418. [DOI] [PubMed] [Google Scholar]
- 13. Puntillo KA, McAdam JL. Communication between physicians and nurses as a target for improving end‐of‐life care in the intensive care unit: challenges and opportunities for moving forward. Crit Care Med 2006;34:S332‐S340. [DOI] [PubMed] [Google Scholar]
- 14.Center to Advance Palliative Care. Growth of palliative care in U.S. hospitals: 2014 snapshot. https://www.capc.org/media/filer_public/6d/db/6ddbbaa1‐0c03‐4e34‐9186‐696bbc158950/capc_growth_snapshot_2014.pdf Accessed February 1, 2015.
- 15. Bajaj JS, Wade JB, Gibson DP, Heuman DM, Thacker LR, Sterling RK, et al. The multi‐dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol 2011;106:1646‐1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Potosek J, Curry M, Buss M, Chittenden E. Integration of palliative care in end‐stage liver disease and liver transplantation. J Palliat Med 2014;17:1271‐1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brown J, Sorrell JH. Waiting for a liver transplant. Qual Health Res 2006;16:119‐136. [DOI] [PubMed] [Google Scholar]
- 18. Rossaro L, Troppmann C, McVicar JP, Sturges M, Fisher K, Meyers FJ. A strategy for the simultaneous provision of pre‐operative palliative care for patients awaiting liver transplantation. Transpl Int 2004;17:473‐475. [DOI] [PubMed] [Google Scholar]


