Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- MHE
minimal hepatic encephalopathy
- OHE
overt hepatic encephalopathy
Current Knowledge in MHE
Minimal hepatic encephalopathy (MHE) is a mild disturbance in brain functioning caused by liver cirrhosis. It affects approximately half of cirrhosis patients, deeply affects daily functioning, and must by definition be diagnosed by means of psychometric tests.1 There have been several recent advances in the subject of MHE testing, and the pros and cons of testing and management are summarized in Table 1. The current status is that only a few highly specialized clinics routinely offer psychometric testing, although there is a profusion of tests for MHE diagnosis with increasing consensus on “gold standards”. Apart from driving, there are several other important aspects of daily function that are affected by MHE, which gives additional reason to increase diagnosis. There are treatment options available, but long‐term studies to evaluate clinically relevant outcomes are awaited. Further, it has become evident that a significant proportion of patients with MHE are dangerous drivers with poor navigation skills and reaction times.2, 3, 4, 5 Driving under the influence of MHE is hazardous, and therefore, fitness to drive is a key issue when discussing MHE management. A special concern in case of MHE and other mild cognitive impairments is to which extent patients' autonomy should be respected when they may not be fully aware of the extent of the impairment.
Table 1.
Pros and Cons to Screening for Minimal Hepatic Encephalopathy
| Pros | Cons |
|---|---|
| Simple and fast screening tests are available | Screening in any form is time consuming |
| A handful of well‐validated tests are recommended | No gold‐standard test exists |
| Quality of life may improve | The patients will feel labeled as “impaired” |
| Several safe treatment options are possible | Lactulose causes frequent bowel movements |
| Patients and especially caregivers will be grateful that a doctor addresses issues important to daily living | The patient‐doctor relationship can be harmed if the patient is unaware of and doesn't recognize the cognitive impairment |
| MHE patients are more likely to be in a traffic accident | Patient's freedom/autonomy could be limited by driving restrictions |
| Episodes of overt hepatic encephalopathy can be prevented, and this could ease the burden on the healthcare system | MHE screening requires dedicated resources |
Pros and Cons to Diagnosing and Treating MHE
Ethics has to do with moral principles and practices, and in medical literature, the term “unethical” often refers to professional conduct that fails to conform to moral standards. In medicine, the level of knowledge, availability of technology, and financial resources set moral and practice standards.6 Good ethics encompasses patients' autonomy, beneficence to patients and society, as well as nonmaleficence (Table 2). The clinician must balance the desire to maintain the fiduciary relationship with the patient, while at the same time protecting both the patient and the community from harm (ethical balance between autonomy and beneficence). In general, the doctor should serve the patient's best interest. In most countries, patient‐doctor confidentiality can be overridden if the patient poses a direct threat to himself or others. This is sometimes relevant when recommending driving restrictions (see below).
Table 2.
Ethical Aspects of MHE Screening Adapted from Beauchamp and Childress
| Principle | Potential harm |
|---|---|
| Beneficence |
• Finding and treating HE at an early stage could prevent episodes of OHE • Even without treatment, identifying patients at risk will raise awareness, and caregivers will know what to expect • Accidents can be prevented by advising selected MHE patients against driving and working heavy machinery |
| Non‐malfeasance |
• Screening tests pose no harm to patients • First‐line treatment (nonabsorbable disaccharides) have only a few and well‐known side effects • Screening tests are nonspecific but sensitive, so a number of false positives must be expected |
| Justice | • Screening is still not uniformly performed, and it is an ethical concern that some patients are screened and counseled whereas others are left unaware |
| Autonomy | • Patients participating in screening could end up being deemed unfit to drive or work machinery, and by restricting driving the patient may be asked to forgo his/her ability to decide their own best course of action |
There are benefits of diagnosing and potentially treating MHE. A growing body of evidence demonstrates that it is possible to identify a group of patients who are likely to have poor quality of life, a higher risk of OHE, falls, and death. Treatment is recommended on a case‐by‐case basis. Studies have shown that cheap and safe treatment with lactulose can improve quality of life and reduce episodes of OHE and mortality, but patient acceptability may be an issue.7, 8
However, important possible cons to MHE diagnostics need to be addressed. When driving restrictions are necessary, patients' autonomy and confidentiality is violated to protect patient and community from harm. Hence, recommending driving restrictions is a balancing act and calls for careful consideration. First, it should be considered that the legal responsibility for withdrawal of driver's licenses or ensuing driving lies with the local traffic authority. However, doctors in their role as healthcare professionals have an ethical responsibility to recommend driving restriction for potentially dangerous drivers and should notify authorities if necessary. When making this decision, clinicians should remember that many other factors besides MHE could affect driving skills; therefore, an automatic assumption that MHE diagnosis will equal loss of driving privileges is false (Fig. 1). Also, no single psychometric test is accurate enough to predict future crashes. This means that relying on a single psychometric test inherently will cause MHE patients who will never have an accident to be deemed unfit to drive (Fig. 1A) (type I error), when in reality the fraction of MHE patients who will prove to be dangerous drivers is smaller (Fig. 2B). This implies that focus should be on the MHE patient with advanced liver disease and poor driving history, because they may be more likely to be involved in crashes, rather than focusing on all MHE patients. Currently, only very few physicians routinely use psychometric tests or discuss driving issues with their patients, in part due to the lack of uniform public recommendations.9 The ethical principles of autonomy versus justice and social beneficence will be tested in all subjects with MHE who ultimately have the potential to harm others or themselves while driving, operating heavy machinery, and so forth. However, none of the currently available tests have the power to clearly differentiate between those who are safe or unsafe drivers. Therefore, a balance between these two major ethical principle thoughts are needed whenever recommending driving restrictions.
Figure 1.
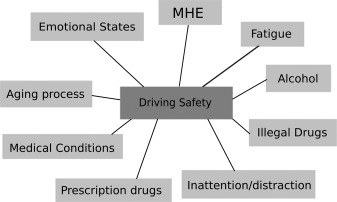
Many factors affect driving skills in patients with cirrhosis, not just minimal hepatic encephalopathy.
Figure 2.
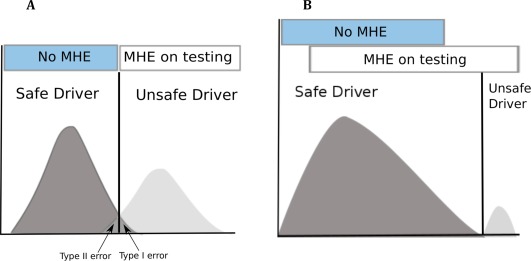
Issues with MHE tests and driving: Far from all MHE patients are dangerous drivers. (A) When relying blindly on a cognitive test, safe drivers will in some cases be deemed unfit to drive (type I error) and vice versa (type II error). (B) In reality, only a few MHE patients will prove to be unfit to drive.
Another drawback to MHE diagnostics is the issue of time resources. Dealing with MHE inevitably takes time and resources that in the short‐term could reduce the focus on other disorders. However, finding and treating MHE, especially from a societal perspective, is thought to be cost‐effective.10, 11 In addition, diagnostic efforts can be individually tailored to suit the resource and expertise level in each clinic (Fig. 3). Therefore, it should be possible to find resources (medical assistants, technicians, and so forth) to perform basic cognitive testing.
Figure 3.
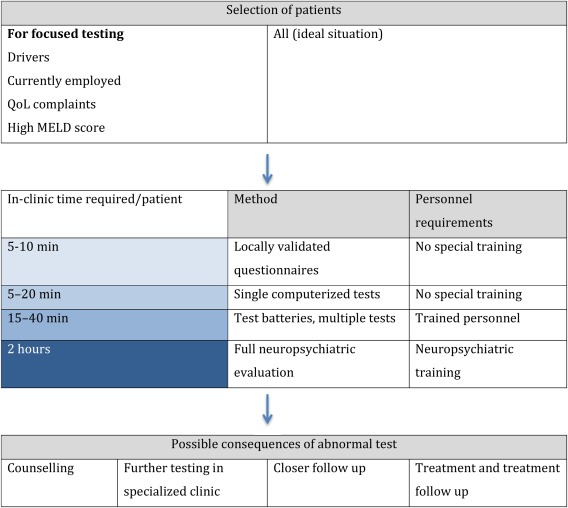
MHE Screening Procedure Can Be Tailored to the Clinic's Resource and Expertise Level.
We believe it is ethical to screen and treat MHE on a case‐by‐case basis for a multitude of reasons, including driving impairment. However, a diagnosis of MHE does not necessarily mean that the subject is a dangerous driver. Driving restrictions should, however, be discussed in MHE patients with advanced liver disease who actually drive and who have prior poor driving history.
Funding: This study was partly supported by RO1DK089713 and VA Merit Review CX10076 awarded to JSB.
Potential conflict of interest: Nothing to report.
References
- 1. Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014;60:715‐735. [DOI] [PubMed] [Google Scholar]
- 2. Bajaj JS, Hafeezullah M, Hoffmann RG, Saeian K. Minimal hepatic encephalopathy: a vehicle for accidents and traffic violations. Am J Gastroenterol 2007;102:1903‐1909. [DOI] [PubMed] [Google Scholar]
- 3. Wein C, Koch H, Popp B, Oehler G, Schauder P. Minimal hepatic encephalopathy impairs fitness to drive. Hepatology 2004;39:739‐745. [DOI] [PubMed] [Google Scholar]
- 4. Bajaj JS, Thacker LR, Heuman DM, Gibson DP, Sterling RK, Stravitz RT, et al. Driving simulation can improve insight into impaired driving skills in cirrhosis. Dig Dis Sci 2012;57:554‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bajaj JS, Hafeezullah M, Hoffmann RG, Varma RR, Franco J, Binion DG, et al. Navigation skill impairment: Another dimension of the driving difficulties in minimal hepatic encephalopathy. Hepatology 2008;47:596‐604. [DOI] [PubMed] [Google Scholar]
- 6. Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 6th edition New York, NY: Oxford University Press; 2009. [Google Scholar]
- 7. Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R. Lactulose improves cognitive functions and health‐related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology 2007;45:549‐559. [DOI] [PubMed] [Google Scholar]
- 8. Luo M, Li L, Lu CZ, Cao WK. Clinical efficacy and safety of lactulose for minimal hepatic encephalopathy: a meta‐analysis. Eur J Gastroenterol Hepatol 2011;23:1250‐1257. [DOI] [PubMed] [Google Scholar]
- 9. Lauridsen MM, Bajaj JS. Hepatic encephalopathy treatment and its effect on driving abilities: a continental divide. J Hepatol 2015;63:287‐288. [DOI] [PubMed] [Google Scholar]
- 10. Andersen MM, Aunt S, Jensen NM, Homann C, Manniche J, Svendsen S, et al. Rehabilitation for cirrhotic patients discharged after hepatic encephalopathy improves survival. Dan Med J 2013;60:A4683. [PubMed] [Google Scholar]
- 11. Bajaj JS, Pinkerton SD, Sanyal AJ, Heuman DM. Diagnosis and treatment of minimal hepatic encephalopathy to prevent motor vehicle accidents: a cost‐effectiveness analysis. Hepatology 2012;55:1164‐1171. [DOI] [PMC free article] [PubMed] [Google Scholar]


