Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- AFD
alcoholic foamy degeneration
- AFLJ
alcoholic fatty liver with jaundice
- AH
alcoholic hepatitis
- ALT
alanine aminotransferase
- AST
aspartate aminotransferase
- GGT
gamma‐glutamyltranspeptidase
Alcoholic liver disease manifests in a spectrum of clinical and histological patterns, including steatosis (fatty liver), alcoholic hepatitis (AH), and cirrhosis. Steatosis, usually consisting of macrovesicular (large droplet) fat, is seen in more than 90% of individuals with heavy alcohol consumption and is typically benign and asymptomatic.1 Uncommonly, fatty change, even in the absence of significant inflammation, causes acute episodes of jaundice, hepatomegaly, and hepatic decompensation that can mimic the clinical presentation of AH. Case reports of such episodes, which we refer to as alcoholic fatty liver with jaundice (AFLJ), have been published since the 1950s.2, 3, 4, 5, 6 Episodes of jaundice have also been reported in patients whose liver biopsies showed diffuse microvesicular steatosis, an entity termed alcoholic foamy degeneration (AFD) by Uchida et al.7 in 1983. Despite similarities in their clinical presentations, AFLJ and AFD are often overlooked in the differential diagnosis of AH.
Histological Features
AFLJ and AFD are both defined by significant steatosis often involving more than 75% of hepatocytes. The histology of AFLJ consists of macrovesicular steatosis that is similar to that seen in simple alcoholic fatty liver, except that the former condition may have more diffuse fatty change, as well as the presence of cholestasis in some cases1 (Fig. 1). The histological diagnosis of AFLJ requires exclusion of AH (i.e., the absence of significant sinusoidal collagen deposition, neutrophilic inflammation, or Mallory‐Denk bodies). It is not known whether the mechanism of cholestasis in AFLJ is distinct from that seen in severe AH. AFD is defined by the presence of significant microvesicular, foamy‐appearing steatosis that mainly involves the perivenular and often midzonal hepatocytes1 (Fig. 2). Concomitant macrovesicular fat is almost always present to a variable degree. The histology of AFD is similar to that seen in several nonalcoholic liver injuries with abnormal mitochondrial fatty acid oxidation, such as Reye syndrome, tetracycline‐induced liver injury, and acute fatty liver of pregnancy.1, 7 Multiple hepatic mitochondrial DNA deletions have been correlated with AFD,8 and affected hepatocytes have damaged mitochondria and endoplasmic reticulum on electron microscopy,7 consistent with a degenerative process accompanying microvesicular but not macrovesicular fatty change. In its pure form, AFD lacks the inflammatory features of AH; however, coexisting, usually focal, microvesicular steatosis can be found in some cases of AH7, 9 (Fig. 3). As in AH, portal fibrosis in cases of AFLJ and AFD can be mild to moderate, or there can be underlying cirrhosis.1, 7 The histological features of AFLJ, AFD, AH, and AH with coexisting AFD are summarized in Table 1.
Figure 1.
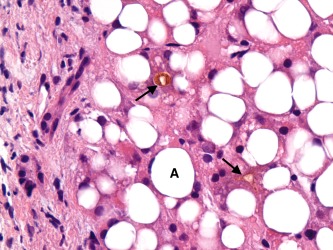
AFLJ. Diffuse macrovesicular steatosis is present (A). Cholestasis is also apparent (arrows). No liver cell ballooning, Mallory‐Denk bodies, or lobular necroinflammatory changes are seen.
Figure 2.
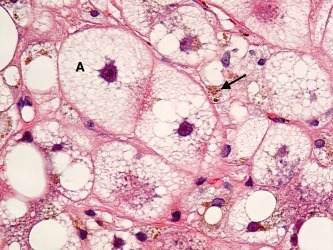
AFD. The hepatocytes show diffuse microvesicular steatosis having a “foamy” cytoplasmic appearance (A). The liver cell nuclei are located within the center of the cell without the displacement that commonly occurs with macrovesicular steatosis. Cholestasis is also apparent (arrow).
Figure 3.
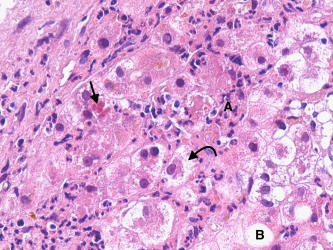
AH with coexisting AFD. This field shows the characteristic features of AH, with liver cell ballooning (curved arrow), Mallory‐Denk body formation (straight arrow), and neutrophilic infiltrates (A). Macrovesicular steatosis is present (B) but involves only a few hepatocytes. Microvesicular foamy hepatocytes were present in other fields of the biopsy.
Table 1.
Typical Histological Features of Alcoholic Fatty Liver With Jaundice, Alcoholic Foamy Degeneration, Alcoholic Hepatitis, and Alcoholic Hepatitis With Coexisting Alcoholic Foamy Degeneration1, 4, 5, 7
| AFLJ | AFD | AH | AH‐AFD | |
|---|---|---|---|---|
| Macrovesicular fatty change | ++ | + | + | + |
| Microvesicular fatty change | − | ++ | − | + |
| Portal fibrosis | − to ++ | − to ++ | + to ++ | + to ++ |
| Neutrophilic lobular inflammation | − | − | ++ | ++ |
| Mallory‐Denk bodies | − | − | + | + |
| Sinusoidal collagen deposition | − | − | + | + |
++, prominent; +, present, −, absent or minimal.
Epidemiology
Among alcoholic patients who underwent liver biopsy, the reported prevalence rate of AFD has ranged from 0.8% to 14%.7, 9, 10 No previous studies reported the prevalence or incidence of AFLJ among alcoholic patients. In not yet published results from our retrospective study of 95 alcoholic patients hospitalized at the Los Angeles County‐University of Southern California Medical Center between 2008 and 2012 and who underwent liver biopsy because of jaundice and suspicion for severe AH, 9 patients (9.5%) were diagnosed with AFD and 8 patients (8.4%) were diagnosed with ALFJ without AH. Nine of the patients with AFD or AFLJ were noncirrhotic. In addition, of the 74 patients in our study with biopsy‐proven severe AH, 5 (6.8%) had evidence of coexisting AFD. The true prevalence of AFD and ALFJ among alcoholic patients is likely underestimated, because patients may not undergo liver biopsy if they remain asymptomatic or have only mild liver test abnormalities.
Clinical features
Patients who experience development of AFLJ or AFD have a history of chronic and heavy alcohol consumption, usually at least 100 g ethanol per day.6, 7, 9, 11 They often report increased alcohol consumption in the weeks to months before being diagnosed,5, 11 but this may be followed by a 1‐ to 2‐week period of abstinence immediately before biopsy after symptom onset.9 When symptomatic, patients may present with jaundice and hepatomegaly, as well as other nonspecific symptoms such as fatigue, malaise, anorexia, weight loss, nausea, vomiting, or abdominal pain.2, 3, 4, 5, 6, 7, 9, 10, 11, 12, 13 Uncommonly, patients may be febrile.3, 4, 7 Manifestations of portal hypertension, including spider angiomas, splenomegaly, ascites, peripheral edema, esophageal varices, and encephalopathy, can occur; rarely, these can be seen even in the absence of underlying cirrhosis.3, 4, 5, 6, 7 These presenting symptoms and signs are clinically indistinguishable from those of AH.
Laboratory findings in patients with AFLJ or AFD include elevations in serum levels of alkaline phosphatase, bilirubin, gamma‐glutamyltranspeptidase (GGT), and aminotransferases,6, 7, 9, 10, 11, 12, 13 often with a ratio of the aspartate aminotransferase (AST) level to the alanine aminotransferase (ALT) level of greater than 2. Liver synthetic dysfunction as indicated by decreased serum albumin and prolonged prothrombin time is variable.6, 7, 9, 10, 11, 12, 13 Unlike AH, leukocytosis is usually absent in patients with AFLJ or AFD,4, 7, 9 and in AFD, the AST level can be greater than 300 IU/L7, 11, 12, 13 and even exceed 1000 IU/L.11, 13 Cases of AFD with markedly elevated GGT levels greater than 3000 IU/L have also been reported.11, 12 Hypercholesterolemia is not infrequent3, 4, 5, 6, 7, 9 among patients with AFLJ or AFD, and a subset of these patients has a triad of hypercholesterolemia, jaundice, and transient hemolytic anemia that is known as Zieve syndrome.3 Some patients with AFD have severe hypertriglyceridemia as well.9, 11 The typical initial laboratory features reported for cases of AFLJ, AFD, and AH are summarized in Table 2.
Table 2.
Typical Initial Laboratory Features of Patients With Alcoholic Fatty Liver With Jaundice, Alcoholic Foamy Degeneration, and Alcoholic Hepatitis1, 2, 3, 4, 5, 6, 7, 9, 10, 12
| AFLJ | AFD | AH | |
|---|---|---|---|
| Leukocyte count | Normal | Normal | ↑ to ↑↑ |
| Total bilirubin | ↑ to ↑↑ | ↑ to ↑↑ | ↑ to ↑↑ |
| Prothrombin time | Normal to ↑ | Normal to ↑↑ | ↑ to ↑↑ |
| Alkaline phosphatase | ↑ to ↑↑ | ↑ to ↑↑ | ↑ |
| AST | ↑ | ↑↑ | ↑ |
| ALT | ↑ | ↑ to ↑↑ | ↑ |
| Cholesterol | Normal to ↑↑ | Normal to ↑↑ | Normal |
↑↑, markedly elevated; ↑, elevated.
Diagnosis
The differential diagnosis for AFLJ and AFD includes AH, decompensation of alcoholic cirrhosis (such as secondary to infection, portal vein thrombosis, or hepatocellular carcinoma), and various nonalcoholic causes of liver disease. Patients should be screened for bacterial infections, and abdominal ultrasonography should be performed to rule out biliary obstruction or portal vein thrombosis and to evaluate for underlying cirrhosis. Nonalcoholic causes of liver disease including nonalcoholic steatohepatitis, acute or chronic viral hepatitis, autoimmune liver disease, and drug‐induced liver injury must be excluded based on the clinical history and appropriate laboratory markers. Although certain laboratory or radiological features in patients may be more suggestive of AFLJ or AFD than AH, there is substantial overlap in the clinical features of these three alcoholic liver diseases. Similarly, although a normal hepatic venous pressure gradient, normal liver stiffness by transient elastography, and heterogeneous distribution of radioactivity on liver‐spleen scintigraphy have been reported for cases of AFD,11, 13 none of these findings have been shown to reliably distinguish among AFD, AFLJ, and AH, and may instead reflect the absence of cirrhosis and portal hypertension in the reported cases. Therefore, liver biopsy remains the gold standard for diagnosis. We believe that exclusion of AH based on liver biopsy is essential for any patients with significant laboratory abnormalities to guide the need for medical therapy.
Prognosis and Management
Unlike patients with severe AH who have a high short‐term mortality if untreated,14 almost all patients with AFLJ and AFD, including those with markedly abnormal initial liver test abnormalities, have a favorable clinical course, with rapid recovery with alcohol abstinence.3, 4, 5, 9, 10, 11, 12, 13 In a study of 124 patients who died of alcohol‐related liver disease, 51 (35%) had autopsy evidence of AH, whereas only 5 (4%) had AFD. Although Morgan et al.6 reported death from hepatic failure in two of three patients with AFD, the biopsies of both deceased patients showed evidence of acute inflammation that may have represented coexisting AH. Specific therapies such as corticosteroids or pentoxifylline have not been studied in patients with AFLJ or AFD and are not indicated.
Summary
AFLJ and AFD are patterns of acute liver injury in alcoholic patients with macrovesicular and microvesicular fatty change, respectively, but little, if any, necroinflammatory changes. AFD appears to be caused by alcohol‐induced mitochondrial DNA damage leading to impaired fatty acid oxidation. The pathogenesis of cholestasis in AFLJ is not known, and it is uncertain whether it is different from that seen in AH. Both AFLJ and AFD can mimic the clinical presentation of AH, causing jaundice, hepatomegaly, and hepatic decompensation, but generally they have a good prognosis. Laboratory and radiological features can aid in making the diagnosis, but there is diagnostic overlap with AH. Liver biopsy is useful to exclude AH if specific medical therapy such as prednisolone is being considered.
Potential conflict of interest: Nothing to report.
References
- 1. Kanel GC, Korula J. Alcoholic and non‐alcoholic fatty liver diseases In: Atlas of Liver Pathology. 3rd ed Philadelphia, PA: Saunders; 2011:71‐92. [Google Scholar]
- 2. Popper H, Szanto PB. Fatty liver with hepatic failure in alcoholics. J Mt Sinai Hosp 1957;24:1121‐1131. [PubMed] [Google Scholar]
- 3. Zieve L. Jaundice, hyperlipidemia and hemolytic anemia: a heretofore unrecognized syndrome associated with alcoholic fatty liver and cirrhosis. Ann Intern Med 1958;48:471‐496. [DOI] [PubMed] [Google Scholar]
- 4. Sataline LR, Matre WJ. Significance of hyperphosphatasemia in alcoholics with liver disease. An analysis of fifty‐eight cases, with histologic diagnoses. Am J Med 1963;35:323‐342. [DOI] [PubMed] [Google Scholar]
- 5. Ballard H, Bernstein M, Farrar JT. Fatty liver presenting as obstructive jaundice. Am J Med 1971;30:196‐201. [DOI] [PubMed] [Google Scholar]
- 6. Morgan MY, Sherlock S, Scheuer PJ. Acute cholestasis, hepatic failure, and fatty liver in the alcoholic. Scand J Gastroenterol 1978;13:299‐303. [DOI] [PubMed] [Google Scholar]
- 7. Uchida T, Kao H, Quispe‐Sjogren M, Peters RL. Alcoholic foamy degeneration – a pattern of acute alcoholic injury of the liver. Gastroenterology 1983;84:683‐692. [PubMed] [Google Scholar]
- 8. Mansouri A, Fromenty B, Berson A, Robin M, Grimbert S, Beaugrand M, et al. Multiple hepatic mitochondrial DNA deletions suggest premature oxidative aging in alcoholic patients. J Hepatol 1997;27:96‐102. [DOI] [PubMed] [Google Scholar]
- 9. Montull S, Parés A, Bruguera M, Caballeria J, Uchida T, Rodés J. Alcoholic foamy degeneration in Spain. Prevalence and clinico‐pathological features. Liver 1989;9:79‐85. [DOI] [PubMed] [Google Scholar]
- 10. Flejou JF, Degott C, Kharsa G, Soulier A, Rueff B, Potet F. La steatose spongiocytaire alcoolique: etude de trois cas. Gastroenterol Clin Biol 1987;11:165‐168. [PubMed] [Google Scholar]
- 11. Ruiz P, Michelena J, Altamirano J, Miquel R, Moreira L, Cárdenas A, et al. Hepatic hemodynamics and transient elastography in alcoholic foamy degeneration: report of 2 cases. Ann Hepatol 2012;3:399‐403. [PubMed] [Google Scholar]
- 12. Suri S, Mitros FA, Ahluwalia JP. Alcoholic foamy degeneration and a markedly elevated GGT. A case report and literature review. Dig Dis Sci 2003;48:1142‐1146. [DOI] [PubMed] [Google Scholar]
- 13. Shiomi S, Sasaki N, Yokogawa T, Kawada N, Sakaguchi H, Nakajima S, et al. Usefulness of scintigraphy with Tc‐99m phytate for the diagnosis of alcoholic foamy degeneration. Clin Nucl Med 1998;23:302‐304. [DOI] [PubMed] [Google Scholar]
- 14. Lucey MR, Mathurin P, Morgan TR. Alcoholic hepatitis. N Engl J Med 2009;360:2758‐2769. [DOI] [PubMed] [Google Scholar]


