ABSTRACT
Background
Race and sex have been shown to affect management of myocardial infarction (MI); however, it is unclear if such disparities exist in contemporary care of ST‐segment elevation myocardial infarction (STEMI) and non‐ST‐segment elevation myocardial infarction (NSTEMI).
Hypothesis
Disparities in care will be less prevalent in more heavily protocol‐driven management of STEMI than the less algorithmic care of NSTEMI.
Methods
Data were collected from the ACTION Registry‐GWTG database to assess care differences related to race and sex of patients presenting with NSTEMI or STEMI. For key treatments and outcomes, adjustments were made including patient demographics, baseline comorbidities, and markers of socioeconomic status.
Results
Key demographic variables demonstrate significant differences in baseline comorbidities; black patients had higher incidences of hypertension and diabetes, and women more frequently had diabetes. With few exceptions, rates of acute and discharge medical therapy were similar by race in any sex category in both STEMI and NSTEMI populations. Rates of catheterization were similar by race for STEMI but not for NSTEMI, where both black men and women had lower rates of invasive therapy. Rates of revascularization were significantly lower for black patients in both the STEMI and NSTEMI groups regardless of sex. Rates of adverse events differed by sex, with disparities for death and major bleeding; after adjustment, rates were similar by race within sex comparisons.
Conclusions
In this contemporary cohort, although there are differences by race in presentation and management of MI, heavily protocol‐driven processes seem to show fewer racial disparities.
Keywords: Acute coronary syndrome, Gender, Disparities in Care, Race, STEMI, NSTEMI
1. INTRODUCTION
The past 2 decades have seen the development of evidence‐based guidelines for the management of acute ST‐segment elevation myocardial infarction (STEMI) and non–ST‐segment elevation myocardial infarction (NSTEMI).1, 2 In addition, increasing emphasis has been placed on quality‐improvement efforts to ensure adherence to such guidelines, with reimbursement often tied to performance metrics and the advent of quality‐improvement registries to track progress.3, 4, 5, 6, 7 However, despite these efforts, recent studies have demonstrated that broad and substantial adherence remains a challenge.8, 9 In particular, race and sex have previously been associated with discrepant management of NSTEMI, as black patients and women were less likely to receive novel, more costly therapies or undergo invasive procedures.9, 10, 11, 12, 13, 14, 15
Given the disparities in health care delivery, over recent years there have been national and global efforts to rectify such inequalities10, 16; however, the success of such efforts is still unknown. This has led to an Institute of Medicine report that ranked health care delivery and racial and ethnic disparities to be its top 2 recommended research priorities, underscoring the need to fully characterize and understand these problems facing the health care system.17
We examined the Acute Coronary Treatment and Intervention Outcomes Network Registry–Get With The Guidelines (ACTION Registry‐GWTG) database to assess racial and sex disparities in the management of myocardial infarction (MI) after adjusting for markers of socioeconomic status (SES) such as income, education, and geographic region. We hypothesize that such disparities may be of lesser prevalence in more heavily protocol‐driven management of STEMI as opposed to the less algorithmic care of NSTEMI.
2. METHODS
2.1. Data Source, Study Population, and Study Variables
The ACTION Registry‐GWTG is a national quality‐improvement database. The registry uses a standardized dataset with written definitions, has requirements in place to ensure uniform data entry and transmission, and is subject to data quality checks. For inclusion in this study, sites either received an institutional review board approval or the data were considered quality‐assurance data exempt from institutional review board approval per local standards.18 We examined records of consecutive patients presenting with STEMI or NSTEMI enrolled to 464 US hospitals from July 1, 2008, through March 31, 2011, for whom race information was available.
The study population included 289 322 STEMI and NSTEMI patients. As part of the ACTION Registry‐GWTG, demographic data and baseline characteristics were collected on all patients, including age, sex, race, insurance status, body mass index, medical history, signs and symptoms, and presentation. Race was self‐reported. Patients were excluded for any of the following: incomplete data (n = 21 717) because a short‐form data‐collection form was used; no zip code data provided (n = 77 129); patients were transferred out of an ACTION Registry‐GWTG hospital (n = 9029), resulting in incomplete outcome assessment; and patients self‐reported their race as neither white nor black (n = 5988) or checked multiple races (n = 89). After exclusions, 175 370 patients remained in the study.
The diagnosis of STEMI is defined for registry inclusion as new left bundle branch block or persistent ST‐segment elevation ≥1 mm in ≥2 contiguous electrocardiographic leads. Non–ST‐segment elevation myocardial infarction is defined as ischemic symptoms at rest, lasting ≥10 minutes, occurring within 24 hours before admission or up to 72 hours for STEMI, and positive cardiac markers associated with NSTEMI (creatine kinase‐MB or troponin I/T > local laboratory upper limit of normal values) within 24 hours after initial presentation. Patients are ineligible for the ACTION Registry‐GWTG if they meet the diagnostic criteria for STEMI or NSTEMI during hospitalization but their original admission was unrelated to STEMI or NSTEMI diagnosis.18
Medical and interventional therapeutics were collected during hospitalization and at discharge. Acute medical therapies were defined as given within 24 hours from the first medical contact. Also reported were procedures and tests during hospitalization, in‐hospital clinical events, discharge medications, and processes‐of‐care metrics, including door‐to‐balloon time for STEMI and use and timing of catheterization for NSTEMI.
Clinical events of interest include death and major bleeding. Major bleeding is defined as an event meeting ≥1 of the following criteria: (1) absolute hemoglobin (Hb) drop of ≥4 g/dL (baseline to nadir Hb ≥4 g/dL); (2) intracranial hemorrhage stroke; (3) retroperitoneal witnessed bleeding event; (4) baseline Hb ≥9 g/dL and red blood cell transfusion; or (5) baseline Hb < 9 g/dL and red blood cell transfusion and witnessed a bleeding event.
2.2. Statistical Analysis
Comparisons between black and white race were stratified by male or female sex. For select variables, the data were further stratified by patient‐presentation STEMI status (either STEMI or NSTEMI). Categorical variables were summarized using percentages and compared using Mantel‐Haenszel χ2 tests; continuous variables were presented using median and compared using Wilcoxon rank‐sum tests.
Multivariable logistic‐regression modeling was used to compare outcomes between black and white (reference group) stratified by sex and STEMI status. Because patients treated at the same hospital are more likely to have similar outcomes relative to patients treated at different hospitals, we used generalized estimating equations with exchangeable working correlation structure to account for within‐hospital clustering. For acute medications, discharge medications (aspirin, clopidogrel, statin, β‐blocker), procedures (catheterization and revascularization), and mortality, adjustments were made for all the covariates in previously validated ACTION Registry‐GWTG in‐hospital mortality model,19 which consisted of patient demographics (age, weight), medical history (prior peripheral arterial disease, dyslipidemia, prior percutaneous coronary intervention [PCI], prior stroke, current/recent smoker, diabetes mellitus [DM], prior coronary artery bypass grafting [CABG], prior MI, prior heart failure [HF], and hypertension); signs and symptoms at presentation (systolic blood pressure, heart rate, presentation with HF and/or cardiogenic shock); laboratory results (initial serum creatinine [Cr], baseline troponin ratio, baseline Hb); and insurance status. In addition, for acute‐specific medication or discharge‐specific medication, the specific medication used at home was also adjusted. Socioeconomic status variables abstracted based on patient zip code and Area Resource File, including rural vs urban community, college‐education attainment, and median household income, were added as covariates to the model. For major bleeding, these SES variables were also added to the adjustment model along with variables from the ACTION Registry‐GWTG major bleeding model, which consisted of age, heart rate, and systolic blood pressure on presentation, baseline Hb, baseline serum Cr, presentation with HF and/or cardiogenic shock, DM, prior peripheral arterial disease, weight, and home warfarin.20 Odds ratios along with 95% confidence intervals for outcomes were presented, where the reference is white race.
The percentages of missing data were rare, <5% for all covariates in the multivariate models. We did not impute main interested variable (such as race or sex), and those patients were excluded. For the covariates in multivariable modeling, missing values for weight, initial serum Cr, or baseline Hb were set to the sex‐specific median of the nonmissing values. Missing values of other continuous variables were imputed to median of the nonmissing values. Missing values of the categorical variables were imputed to their most common value. All analyses were conducted using SAS version 9.2 (SAS Institute, Inc., Cary, NC).
3. RESULTS
3.1. Patient Characteristics
Among 175 370 patients in our study, NSTEMI (60.4%) was more common than STEMI. Within in each sex category, black patients tended to be younger, have a higher body mass index, have DM, and be current or recent smokers (Tables 1 and 2). Despite being younger, black patients had a higher incidence of hypertension, DM, and prior stroke. Of those patients who underwent catheterization, black patients were more likely to have no evidence of significant coronary disease in both the STEMI and NSTEMI populations (Tables 1 and 2).
Table 1.
Demographic and Clinical Characteristics by Race and Sex Among ACTION Registry Participants (STEMI)
| White Men, n = 44 560 | Black Men, n = 3886 | Unadjusted P Value | White Women, n = 18 771 | Black Women, n = 2283 | Unadjusted P Value | |
|---|---|---|---|---|---|---|
| Patient characteristics | ||||||
| Median age, y | 59 | 55 | <0.0001 | 67 | 60 | <0.0001 |
| Median BMI, kg/m2 | 28 | 28 | <0.0001 | 28 | 30 | <0.0001 |
| Current/recent smoker | 45.5 | 55.2 | <0.0001 | 38.7 | 44.4 | <0.0001 |
| DM | 20.7 | 27.5 | <0.0001 | 26.2 | 40.7 | <0.0001 |
| HTN | 60.2 | 73.0 | <0.0001 | 69.4 | 82.5 | <0.0001 |
| Dyslipidemia | 54.1 | 48.0 | <0.0001 | 53.1 | 53.2 | 0.9842 |
| Prior stroke | 4.0 | 6.7 | <0.0001 | 6.8 | 11.1 | <0.0001 |
| Prior MI | 20.3 | 21.5 | 0.0558 | 16.5 | 19.6 | 0.0002 |
| Prior PCI | 21.7 | 20.3 | 0.0437 | 16.3 | 18.2 | 0.0219 |
| Prior CABG | 7.7 | 4.8 | <0.0001 | 5.8 | 3.9 | 0.0002 |
| Median symptom onset time to presentation (h; all) | 2.3 | 2.3 | 0.0546 | 2.6 | 2.4 | 0.0104 |
| Median time of symptom onset to presentation (h; direct arrival) | 1.5 | 1.6 | 0.0002 | 1.8 | 1.8 | 0.9112 |
| Signs, symptoms, and findings at presentation | ||||||
| HR on admission, bpm, median | 78 | 80 | <0.0001 | 80 | 83 | <0.0001 |
| Initial Cr, mg/dL, median (nondialysis) | 1.10 | 1.20 | <0.0001 | 0.90 | 1.00 | <0.0001 |
| No. of diseased vessels (among patients with cath) | <0.0001 | <0.0001 | ||||
| 1 | 34.55 | 38.34 | 37.83 | 40.62 | ||
| 2 | 33.50 | 29.84 | 31.99 | 27.30 | ||
| 3 | 30.01 | 26.48 | 25.86 | 26.26 | ||
| 0 | 1.51 | 4.85 | 3.64 | 5.17 | ||
| Signs of CHF | 7.5 | 8.7 | 0.0083 | 12 | 13 | 0.0659 |
| Cardiogenic shock | 7.5 | 7.6 | 0.7812 | 9.8 | 9.1 | 0.2792 |
| Insurance status | ||||||
| HMO/private | 59.8 | 39.9 | <0.0001 | 56.3 | 38.7 | <0.0001 |
| Medicare | 17.9 | 21.7 | 27.6 | 33.9 | ||
| Medicaid | 3.2 | 8.1 | 4.0 | 9.1 | ||
| Self/none | 16.1 | 25.5 | 10.9 | 16.6 | ||
| Hospital characteristics | ||||||
| No. of beds, median | 407 | 530 | <0.0001 | 403 | 550 | <0.0001 |
| Hospital type | <0.0001 | 0.0022 | ||||
| PCI and surgery | 92.1 | 91.6 | 92.9 | 91.1 | ||
| PCI, no surgery | 6.1 | 8.4 | 6.6 | 7.5 | ||
| Cath lab only | 0.4 | 0.1 | 0.6 | 0.0 | ||
| No services | 0.6 | 0.4 | 0.7 | 0.9 | ||
| Academic hospital | 25.6 | 39.8 | <0.0001 | 24.9 | 41.4 | <0.0001 |
| Socioeconomic status | ||||||
| Education (% of persons age ≥25 with ≥4 years of college, median) | 21.1 | 25.1 | <0.0001 | 21.0 | 25.3 | <0.0001 |
| HHI in 2004, $, median | 42 182 | 41 922 | <0.0001 | 42 122 | 41 922 | <0.0001 |
| Rural community | 27.9 | 17.9 | <0.0001 | 27.6 | 17.0 | <0.0001 |
Abbreviations: ACTION, Acute Coronary Treatment and Intervention Outcomes Network; BMI, body mass index; CABG, coronary artery bypass grafting; cath, catheterization; CHF, congestive heart failure; Cr, creatinine; DM, diabetes mellitus; HHI, household income; HMO, health maintenance organization; HR, heart rate; HTN, hypertension; MI, myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST‐segment elevation myocardial infarction.
Data are presented as % unless otherwise noted.
Table 2.
Demographic and Clinical Characteristics by Race and Sex Among ACTION Registry Participants (NSTEMI)
| White Men, n = 58 634 | Black Men, n = 6293 | Unadjusted P Value | White Women, n = 35 241 | Black Women, n = 5702 | Unadjusted P Value | |
|---|---|---|---|---|---|---|
| Patient characteristics | ||||||
| Median age, y | 65 | 59 | <0.0001 | 72 | 65 | <0.0001 |
| Median BMI, kg/m2 | 29 | 29 | 0.0296 | 28 | 30 | <0.0001 |
| Current/recent smoker | 32.3 | 44.5 | <0.0001 | 24.3 | 30.1 | <0.0001 |
| DM | 33.3 | 39.3 | <0.0001 | 36.7 | 49.5 | <0.0001 |
| HTN | 74.6 | 84.4 | <0.0001 | 80.2 | 90.1 | <0.0001 |
| Dyslipidemia | 66.5 | 59.0 | <0.0001 | 63.2 | 61.1 | 0.0018 |
| Prior stroke | 8.4 | 12.2 | <0.0001 | 10.6 | 15.5 | <0.0001 |
| Prior MI | 31.5 | 31.5 | 0.8918 | 26.0 | 28.7 | <0.0001 |
| Prior PCI | 29.0 | 26.2 | <0.0001 | 21.8 | 21.2 | 0.2722 |
| Prior CABG | 23.2 | 13.9 | <0.0001 | 14.6 | 12.1 | <0.0001 |
| Median symptom onset time to presentation (h; all) | 4.4 | 4.2 | 0.1854 | 4.4 | 3.9 | 0.0003 |
| Median time of symptom onset to presentation (h; among direct arrivals) | 2.4 | 2.4 | 0.1555 | 2.6 | 2.6 | 0.9195 |
| Signs, symptoms, and findings at presentation | ||||||
| Signs of CHF | 16.8 | 19.9 | <0.0001 | 24.2 | 24.7 | 0.4576 |
| Cardiogenic shock | 2.1 | 1.9 | 0.3937 | 2.0 | 2.1 | 0.7019 |
| HR on admission, bpm, median | 81 | 84 | <0.0001 | 86 | 86 | 0.1124 |
| Initial Cr, mg/dL, median (nondialysis) | 1.10 | 1.20 | <0.0001 | 1.00 | 1.00 | <0.0001 |
| No. of diseased vessels (among patients with cath) | ||||||
| 1 | 24.93 | 27.72 | <0.0001 | 29.10 | 28.69 | <0.0001 |
| 2 | 30.86 | 28.41 | 27.26 | 26.05 | ||
| 3 | 39.41 | 32.39 | 29.50 | 28.35 | ||
| 0 | 4.14 | 10.25 | 12.73 | 15.49 | ||
| Insurance status | ||||||
| HMO/private | 60.8 | 40.0 | <0.0001 | 56.7 | 38.1 | <0.0001 |
| Medicare | 25.4 | 32.2 | 32.8 | 42.8 | ||
| Medicaid | 2.5 | 7.7 | 3.6 | 8.9 | ||
| Self/none | 8.8 | 15.9 | 6.1 | 9.1 | ||
| Hospital characteristics | ||||||
| No. of beds, median | 402 | 562 | <0.0001 | 392 | 547 | <0.0001 |
| Hospital type | ||||||
| PCI and surgery | 92.9 | 93.5 | <0.0001 | 90.9 | 91.7 | <0.0001 |
| PCI, no surgery | 5.0 | 5.7 | 5.9 | 6.7 | ||
| Cath lab only | 1.1 | 0.2 | 1.5 | 0.6 | ||
| No services | 1.0 | 0.6 | 1.7 | 1.0 | ||
| Academic hospital | 25.1 | 37.3 | <0.0001 | 23.3 | 37.7 | <0.0ß001 |
| Socioeconomic status | ||||||
| Education (% of persons age ≥25 years with ≥4 of college, median) | 20.8 | 24.6 | <0.0001 | 21.4 | 25.3 | <0.0001 |
| HHI in 2004, $, median | 41 981 | 41 242 | <0.0001 | 42 239 | 41 767 | <0.0001 |
| Rural community | 28.2 | 17.4 | <0.0001 | 25.9 | 15.5 | <0.0001 |
Abbreviations: ACTION, Acute Coronary Treatment and Intervention Outcomes Network; BMI, body mass index; CABG, coronary artery bypass grafting; cath, catheterization; CHF, congestive heart failure; Cr, creatinine; DM, diabetes mellitus; HHI, household income; HMO, health maintenance organization; HR, heart rate; HTN, hypertension; MI, myocardial infarction; NSTEMI, non–ST‐segment elevation myocardial infarction; PCI, percutaneous coronary intervention.
Data are presented as % unless otherwise noted.
Black patients were more likely to present to an academic hospital and to be covered by Medicare, Medicaid, or to be self‐insured, whereas white patients were more likely to be covered by an HMO or private insurance (Tables 1 and 2). Although there were differences in the services available at individual hospitals, >90% of patients presented to a facility that provided both PCI and cardiac surgery. There were significant differences in markers of SES (Tables 1 and 2). White patients in the registry presenting with STEMI and NSTEMI were more likely to reside in a rural community, had nominally higher median income, and had lower levels of education attainment.
3.2. Acute Medical Therapy
3.2.1. ST‐Segment Elevation Myocardial Infarction–Men
Among men presenting with STEMI, there were few significant differences in acute medical therapies between races (Table 3). Unadjusted data demonstrated black men to be less likely to be placed on any heparin (unfractionated heparin or low‐molecular‐weight heparin) or anticoagulant (including bivalirudin, fondaparinux, argatroban, or lepirudin; see Supporting Information, Table 1A, in the online version of this article). However, after adjusting for baseline health and SES, these differences were no longer statistically significant.
Table 3.
In‐hospital Medications Administered (STEMI) (OR of Black vs White [Ref] in Specified Sex Category)
| Acute Medication Use (<24 Hours), % | White Men | Black Men | P Value | Adjusted OR (95% CI) | Adjusted P Value |
|---|---|---|---|---|---|
| Men | |||||
| Aspirin | 98.5 | 98.3 | 0.0905 | 1.05 (0.78‐1.40) | 0.766 |
| Clopidogrel | 82.4 | 81.9 | 0.3529 | 1.05 (0.97‐1.15) | 0.24 |
| β‐Blocker | 92.4 | 90.6 | 0.0001 | 1.06 (0.92‐1.22) | 0.44 |
| Statin | 73.0 | 72.3 | 0.3504 | 1.01 (0.93‐1.09) | 0.86 |
| White Women | Black Women | P Value | Adjusted OR (95% CI) | Adjusted P Value | |
|---|---|---|---|---|---|
| Women | |||||
| Aspirin | 98.2 | 97.7 | 0.2098 | 1.05 (0.76‐1.47) | 0.756 |
| Clopidogrel | 81.9 | 80.5 | 0.1267 | 0.96 (0.84‐1.09) | 0.508 |
| β‐Blocker | 90.3 | 90.6 | 0.7330 | 1.37 (1.11‐1.69) | 0.004 |
| Statin | 67.0 | 69.4 | 0.0234 | 1.09 (0.97‐1.21) | 0.151 |
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, reference; STEMI, ST‐segment elevation myocardial infarction.
3.2.2. ST‐Segment Elevation Myocardial Infarction–Women
Rates of acute medication use were overall similar between black and white women (Table 3; see also Supporting Information, Table 1A, in the online version of this article). After adjustment, black women were shown to be more likely to have received a β‐blocker compared with white women (Table 3).
3.2.3. Non–ST‐Segment Elevation Myocardial Infarction–Men
In the NSTEMI population, black men had numerically similar but statistically lower rates of aspirin, clopidogrel, β‐blocker, and statin use when compared with white men (Table 4). Black men had significantly lower overall rates of being prescribed any anticoagulant (see Supporting Information, Table 1B, in the online version of this article). After adjustment, only significant differences in statin use persisted (Table 4).
Table 4.
In‐hospital Medications Administered (NSTEMI) (OR of Black vs White [Ref] in Specified Sex Category)
| Acute Medication Use (<24 Hours), % | White Men | Black Men | P Value | Adjusted OR (95% CI) | Adjusted P Value |
|---|---|---|---|---|---|
| Men | |||||
| Aspirin | 97.2 | 96.2 | <0.0001 | 0.96 (0.84‐1.11) | 0.617 |
| Clopidogrel | 57.4 | 54.9 | 0.0001 | 0.94 (0.88‐1.00) | 0.051 |
| β‐Blocker | 87.8 | 86.6 | 0.0159 | 0.99 (0.91‐1.08) | 0.820 |
| Statin | 63.1 | 59.3 | <0.0001 | 0.92 (0.87‐0.98) | 0.013 |
| White Women | Black Women | P Value | Adjusted OR (95% CI) | Adjusted P Value | |
|---|---|---|---|---|---|
| Women | |||||
| Aspirin | 96.0 | 95.1 | 0.0011 | 0.93 (0.81‐1.08) | 0.356 |
| Clopidogrel | 52.5 | 52.0 | 0.4487 | 0.93 (0.87‐0.99) | 0.026 |
| β‐Blocker | 86.2 | 85.6 | 0.2291 | 1.09 (0.97‐1.21) | 0.151 |
| Statin | 56.2 | 57.2 | 0.1920 | 1.0 (0.94‐1.07) | 0.927 |
Abbreviations: CI, confidence interval; NSTEMI, non–ST‐segment elevation myocardial infarction; OR, odds ratio; Ref, reference.
3.2.4. Non–ST‐Segment Elevation Myocardial Infarction–Women
Acute medical therapies were similar among black and white women, with a nominally lower rate of aspirin use among black women. In adjusted analysis, only clopidogrel showed a marginal statistical difference, with white women shown to be significantly more likely to receive clopidogrel (Table 4).
3.3. Invasive Procedures and Processes of Care
3.3.1. ST‐Segment Elevation Myocardial Infarction–Men
Men presenting with STEMI showed no significant difference by race in the overall rate of catheterization or PCI within 90 minutes (Figure 1A) in either adjusted or unadjusted analyses. Interventional procedural use differed slightly by race, with white men having higher overall rates of CABG and revascularization than did black men (94% vs 87%, respectively). After adjustments for baseline comorbidities and SES, rates of overall reperfusion, catheterization, and primary PCI for STEMI were similar across race, whereas disparities in CABG and revascularization persisted (Figure 1A).
Figure 1.
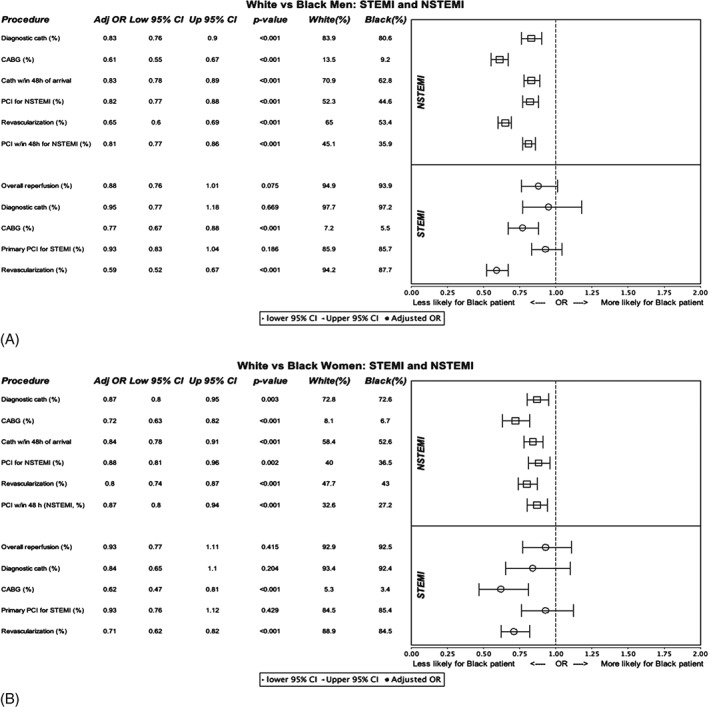
A (men) and B (women): Odds ratios for black vs white patients to undergo procedure by sex and type of MI. Overall, black patients are significantly less likely to undergo catheterization or revascularization. In the NSTEMI population, all such differences are statistically significant. Abbreviations: CABG, coronary artery bypass grafting; cath, catheterization; CI, confidence interval; MI, myocardial infarction; NSTEMI, non–ST‐segment elevation myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST‐segment elevation myocardial infarction.
3.3.2. ST‐Segment Elevation Myocardial Infarction–Women
Women presenting with STEMI also showed no significant difference by race in the overall rates of catheterization or PCI within 90 minutes (Figure 1B) in either adjusted or unadjusted analyses. After adjusting for baseline health status, rates of overall reperfusion, diagnostic catheterization, and primary PCI for STEMI were similar across race; however, white women had higher rates of CABG and revascularization (Figure 1B).
3.3.3. Non–ST‐Segment Elevation Myocardial Infarction–Men
Black men presenting with NSTEMI were less likely to have revascularization and CABG. Distinct from STEMI, black men with NSTEMI were significantly less likely to undergo catheterization (Figure 1A). Black men were also less likely to undergo PCI within 48 hours and had a longer median arrival‐to‐PCI time (Figure 1A). Across all variables, these differences persisted after adjustment for baseline health status and SES (Figure 1A). When patients were evaluated by risk status, significant differences were observed across categories in low‐ and intermediate‐risk patients. In the high‐risk population, catheterization and PCI rates were similar, whereas CABG and overall revascularization demonstrated a significantly lower rate among black men (Figure 2A).
Figure 2.
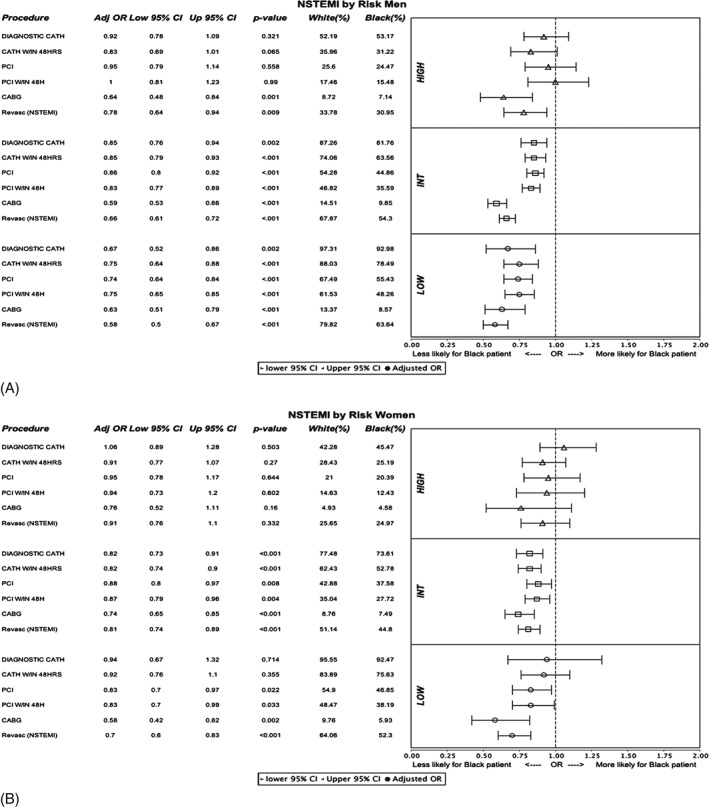
A (men) and B (women): Odds ratios for black vs white patients presenting with NSTEMI to undergo procedure by race. Data stratified by ACTION risk score into high‐, intermediate‐, and low‐risk groups. The high‐risk group demonstrated few disparities compared with the low‐ and intermediate‐risk groups. Abbreviations: ACTION, Acute Coronary Treatment and Intervention Outcomes Network; CABG, coronary artery bypass grafting; cath, catheterization; CI, confidence interval; int, intermediate; NSTEMI, non–ST‐segment elevation myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention; revasc, revascularization.
3.3.4. Non–ST‐Segment Elevation Myocardial Infarction–Women
Among women, although unadjusted rates of catheterization were similar by race, black women were less likely to undergo revascularization and CABG. There were also significant differences for process‐of‐care measures, with black women having longer median time to PCI (Figure 1B). After adjustments, there were significant differences in all key variables, with white women more likely to have interventional procedures and early invasive therapy (Figure 1B) than black women. When rates of procedure use were stratified by patient risk, statistically significant differences persisted across all variables for the intermediate‐risk group and for most variables in the low‐risk group. In the high‐risk population, there were no statistically significant differences (Figure 2B).
3.3.5. Discharge Therapy and Intervention
There were few disparities in the rates of discharge medications in both the STEMI and NSTEMI populations. Most of these lost statistical significance after adjusting for baseline comorbidities and SES. White men and women were more likely to be referred to cardiac rehabilitation at discharge (see Supporting Information, Tables 2A and 2B, in the online version of this article).
3.4. Major Clinical Events
3.4.1. ST‐Segment Elevation Myocardial Infarction
Among men and women presenting with STEMI, there were no statistically significant differences by race in rates of death or major bleed before and after baseline adjustments (Table 5).
Table 5.
Clinical Adverse Events (STEMI) (OR of Black vs White [Ref] in Specified Sex Category)
| White Men, % | Black Men, % | Unadjusted OR | Unadjusted P Value | Adjusted OR | Adjusted P Value | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Death | 4.7 | 5.5 | 1.12 | 0.127 | 1.04 | 0.642 |
| Major bleed | 8.7 | 9.1 | 0.96 | 0.61 | 0.88 | 0.086 |
| White Women, % | Black Women, % | Unadjusted OR | Unadjusted P Value | Adjusted OR | Adjusted P Value | |
|---|---|---|---|---|---|---|
| Women | ||||||
| Death | 8.5 | 9.3 | 1.08 | 0.314 | 1.04 | 0.693 |
| Major bleed | 15.9 | 17.4 | 1.06 | 0.360 | 1.00 | 0.995 |
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, reference; STEMI, ST‐segment elevation myocardial infarction.
3.4.2. Non–ST‐Segment Elevation Myocardial Infarction
White men presenting with NSTEMI had higher unadjusted rates of death, which did not persist after adjustment (Table 6). Women were observed to have similar rates of death and major bleed in the unadjusted data, but after baseline adjustments white women had higher rates of major bleed (Table 6).
Table 6.
Clinical Adverse Events (NSTEMI) (OR of Black vs White [Ref] in Specified Sex Category)
| White Men, % | Black Men, % | Unadjusted OR | Unadjusted P Value | Adjusted OR | Adjusted P Value | |
|---|---|---|---|---|---|---|
| Men | ||||||
| Death | 3.6 | 3.3 | 0.87 | 0.041 | 0.91 | 0.250 |
| Major bleed | 7.1 | 8.0 | 1.03 | 0.617 | 0.94 | 0.244 |
| White Women, % | Black Women, % | Unadjusted OR | Unadjusted P Value | Adjusted OR | Adjusted P Value | |
|---|---|---|---|---|---|---|
| Women | ||||||
| Death | 4.4 | 4.4 | 1.00 | 0.977 | 0.99 | 0.943 |
| Major bleed | 11.4 | 12.4 | 1.00 | 0.989 | 0.87 | 0.010 |
Abbreviations: CI, confidence interval; NSTEMI, non–ST‐segment elevation myocardial infarction; OR, odds ratio; Ref, reference.
4. DISCUSSION
We evaluated >175 000 patients with MI enrolled in the ACTION Registry‐GTWG to assess for differences by race. When comparing black and white patients stratified by sex, several patterns emerged. In general, the use of acute medical therapies and the rates of invasive or interventional procedures were similar for black and white STEMI patients. In the NSTEMI population, there were few differences in rates of acute medication use. Among the STEMI and NSTEMI populations, there were also no significant differences by race in the adjusted rates of in‐hospital mortality. In contrast, black patients of both sexes presenting with NSTEMI tended to have lower rates of invasive and interventional procedures and longer delays to therapy. These differences were more pronounced among subjects at low or intermediate risk and attenuated with high‐risk patients. Black patients tended to have less CABG, less overall revascularization, and lower rates of some key discharge therapies and counseling across both STEMI and NSTEMI.
Given the large sample size of this study, certain results reached statistical significance despite having a modest numerical difference. This was the case for medications administered acutely or prescribed at discharge. In comparison, the differences in procedural use and markers of timeliness of care were more pronounced. Moreover, although there were significant differences in the use of interventional therapies in all populations, these were more apparent for patients presenting with NSTEMI. When comparing white men with black women presenting with STEMI, the differences in rates of catheterization and revascularization were 5% and 10%, respectively. For NSTEMI care, these nearly doubled to 11% and 22%.
Previous studies of racial disparities in MI have shown that, although there may be decreased rates of interventional therapy use for black patients, there are few statistically or clinically significant differences in acute medication use.9, 10, 11, 15, 21, 22, 23, 24, 25, 26 Recent large database studies have shown that such trends persist in the modern era, with white patients and men being more likely to undergo invasive procedures (eg, angiography, PCI, CABG).27, 28 However, these investigations used insurance and national admissions databases in which clinical information such as type of MI, socioeconomic factors, inpatient medication use, and process‐of‐care metrics could not be assessed. This study significantly adds to the existing literature on racial and sex differences in care as a large, contemporary, nationwide study with the ability to assess management of both STEMI and NSTEMI populations. By including all patients presenting with MI, we are able to both investigate race disparities in care in the United States as well as assess how heavily protocol‐driven strategies may impact or eliminate disparate treatment. Another strength of this study is that it examines differences by race among a large sample of patients of both sexes. Finally, this is the first study of this scale to investigate race and sex differences while adjusting for socioeconomic markers accounting for income level, education, or geographic origin, all of which may track with race and sex.
It this study we observed similar adjusted outcomes by race and similar rates of acute medical and invasive therapies among patients presenting with STEMI and those NSTEMI patients with highest baseline risk. In our current era of national quality‐improvement initiatives, it is promising that rigorous guideline adherence is associated with few racial disparities in care.
For the observed disparities, it is uncertain why such inequalities in care exist or why they are more pronounced in management of NSTEMI. Some differences can be attributed to coronary artery disease burden, as black patients presenting with NSTEMI were more likely than their white counterparts to have no evidence of coronary artery disease found at the time of catheterization. This could account for some of the measured disparities in rates of PCI between black and white patients but would not explain differences in the overall rates or timeliness of diagnostic procedures. Care differences may also be attributed to variable baseline comorbidities, treatment variation by geographic region or hospital type, or presenting characteristics making a patient a nonideal candidate for interventional therapy.9, 10, 11, 15, 21, 22, 23, 24, 25, 26, 27, 28, 29 However, in this study, disparities persist even after adjusting for these variables.
It is possible that care differences may be related to biases within the medical system or unmeasured subtleties of disease process not captured in the database. In NSTEMI management, providers take on a larger role as gatekeepers of care delivery; as provider preference, judgment, and recommendations bear more weight, care may be more susceptible to subconscious biases.30, 31 This contrasts with management of STEMI, which is highly protocol driven, from care delivered in the field by emergency medical services and provision of acute care such as early medications and primary PCI. Such standardization of care may minimize the potential impact of clinician or health care–system bias.32
4.1. Study Limitations
A primary limitation of this study is that, as a database study, we can only detect associations between race and sex with treatments and metrics of care, but we cannot assess causality. Another limitation is that we cannot test for all potential confounders. Unmeasured or unmeasurable clinical characteristics and socioeconomic factors associated with race or sex may have contributed to the differences we observed. For instance, health literacy or routine access to primary care may impact a patient's ability to advocate for his or her own treatment. Although we have not directly accounted for all confounders, our adjustments for income, education, and geography may address many such issues. An additional limitation of this study is that it only reflects acute management and outcomes of patients presenting with acute coronary syndromes. Less care—for example, lower CABG rates—does not inherently mean worse care, and recent data suggests that long‐term survival may be similar by race despite differences in acute management.33 Moreover, we cannot determine if the care differences observed are attributable to under‐ or overtreatment in certain populations. In our study we observed that the adjusted rates of in‐hospital mortality were similar across groups.
5. CONCLUSION
In this contemporary cohort, many evidence‐based therapies and invasive treatment metrics were similar between black and white patients, particularly among patients with STEMI. Although differences in management of MI continue to exist by race among both sexes, these differences were more pronounced among patients with NSTEMI and among those at lower risk.
Supporting information
Appendix S1. Supporting Appendix Tables
Anstey DE, Li S, Thomas L, Wang TY, Wiviott SD.. Race and Sex Differences in Management and Outcomes of Patients After ST‐Elevation and Non–ST‐Elevation Myocardial Infarct: Results From the NCDR, Clin Cardiol 2016, 39, 585–595. DOI: 10.1002/clc.22570
SW reports grants and personal fees from AstraZeneca, grants and personal fees from Bristol Myers Squibb, grants from Eisai, grants and personal fees from Arena, grants from Merck, personal fees from Aegerion, personal fees from Angelmed, personal fees from Janssen, personal fees from Xoma, personal fees from ICON Clinical, personal fees from Boston Clinical Research Institute, grants and personal fees from Eli Lilly/Daiichi Sankyo, grants from Sanofi‐Aventis, personal fees from Boehringer Ingelheim. SW's spouse is an employee of Merck Research Labs. All fees are outside the submitted work.
REFERENCES
- 1. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST‐elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST‐Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine [published correction appears in Circulation. 2008;117:e180]. Circulation . 2007;116:e148–e304. [DOI] [PubMed] [Google Scholar]
- 2. Kushner FG, Hand M, Smith SC Jr, et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines [published corrections appear in J Am Coll Cardiol. 2009;54:2464 and 2010;55:612]. J Am Coll Cardiol . 2009;54:2205–2241. [DOI] [PubMed] [Google Scholar]
- 3. Hoekstra JW, Pollack CV, Roe MT, et al. Improving the care of patients with non–ST‐elevation acute coronary syndromes in the emergency department: the CRUSADE Initiative. Acad Emerg Med. 2002;9:1146–1155. [DOI] [PubMed] [Google Scholar]
- 4. Marciniak TA, Ellerbeck EF, Radford MJ, et al. Improving the quality of care for Medicare patients with acute myocardial infarction: results from the Cooperative Cardiovascular Project. JAMA. 1998;279:1351–1357. [DOI] [PubMed] [Google Scholar]
- 5. Spertus JA, Radford MJ, Every NR, et al. Challenges and opportunities in quantifying the quality of care for acute myocardial infarction: summary from the Acute Myocardial Infarction Working Group of the American Heart Association/American College of Cardiology First Scientific Forum on Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke. Circulation. 2003;107:1681–1691. [DOI] [PubMed] [Google Scholar]
- 6. Bradley EH, Nallamothu BK, Herrin J, et al. National efforts to Improve door‐to‐balloon time: results from the Door‐to‐Balloon Alliance. J Am Coll Cardiol. 2009;54:2423–2429. [DOI] [PubMed] [Google Scholar]
- 7. Bonow RO, Masoudi FA, Rumsfeld JS, et al. ACC/AHA classification of care metrics: performance measures and quality metrics: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2008;52:2113–2117. [DOI] [PubMed] [Google Scholar]
- 8. Tricoci P, Peterson ED, Roe MT; CRUSADE Quality Improvement Initiative. Patterns of guideline adherence and care delivery for patients with unstable angina and non–ST‐segment elevation myocardial infarction (from the CRUSADE Quality Improvement Initiative). Am J Cardiol . 2006;98:30Q–35Q. [DOI] [PubMed] [Google Scholar]
- 9. Sonel AF, Good CB, Mulgund J, et al. Racial variations in treatment and outcomes of black and white patients with high‐risk non–ST‐elevation acute coronary syndromes: insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?). Circulation. 2005;111:1225–1232. [DOI] [PubMed] [Google Scholar]
- 10. Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094–1100. [DOI] [PubMed] [Google Scholar]
- 11. Vaccarino V, Rathore SS, Wenger NK, et al; National Registry of Myocardial Infarction Investigators. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med . 2005;353:671–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non–ST‐segment elevation acute coronary syndromes: large‐scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. [DOI] [PubMed] [Google Scholar]
- 13. Jneid H, Fonarow GC, Cannon CP, et al; Get With the Guidelines Steering Committee and Investigators. Sex differences in medical care and early death after acute myocardial infarction. Circulation . 2008;118:2803–2810. [DOI] [PubMed] [Google Scholar]
- 14. Peterson ED, Shah BR, Parsons L, et al. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156:1045–1055. [DOI] [PubMed] [Google Scholar]
- 15. Graham G. Racial and ethnic differences in acute coronary syndrome and myocardial infarction within the United States: from demographics to outcomes. Clin Cardiol. 2016;39:299–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. US Department of Health and Human Services, Developing Healthy People 2020. The Secretary's Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020, Office of Disease Prevention & Health Promotion. https://www.healthypeople.gov/2020/topics‐objectives. Accessed March 10, 2011.
- 17. Institute of Medicine . Initial National Priorities for Comparative Effectiveness Research . Washington, DC: National Academies Press; 2002. [Google Scholar]
- 18. Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:491–499. [DOI] [PubMed] [Google Scholar]
- 19. Chin CT, Chen AY, Wang TY, et al. Risk adjustment for in‐hospital mortality of contemporary patients with acute myocardial infarction: the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry–Get With The Guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J . 2011;161:113.e2–122.e2. [DOI] [PubMed] [Google Scholar]
- 20. Mathews R, Peterson ED, Chen AY, et al. In‐hospital major bleeding during ST‐elevation and non–ST‐elevation myocardial infarction care: derivation and validation of a model from the ACTION Registry‐GWTG. Am J Cardiol. 2011;107:1136–1143. [DOI] [PubMed] [Google Scholar]
- 21. Stone PH, Thompson B, Anderson HV, et al. Influence of race, sex and age on management of unstable angina and non–Q‐wave myocardial infarction: the TIMI III registry. JAMA. 1996;275:1104–1112. [PubMed] [Google Scholar]
- 22. Chen J, Rathore SS, Radford MJ, et al. Racial differences in use of cardiac catheterization after acute myocardial infarction. N Engl J Med. 2001;344:1443–1449. [DOI] [PubMed] [Google Scholar]
- 23. Epstein AM, Weissman JS, Schneider EC, et al. Race and gender disparities in rates of cardiac revascularization: do they reflect appropriate use of procedures or problems in quality of care? Med Care. 2003;41:1240–1255. [DOI] [PubMed] [Google Scholar]
- 24. Weitzman S, Cooper L, Chambless L, et al. Gender, racial, and geographic differences in the performance of cardiac diagnostic and therapeutic procedures for hospitalized acute myocardial infarction in four states. Am J Cardiol. 1997;79:722–726. [DOI] [PubMed] [Google Scholar]
- 25. Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization [published correction appears in N Engl J Med. 1999;340:1130]. N Engl J Med . 1999;340:618–626. [DOI] [PubMed] [Google Scholar]
- 26. Giles WH, Anda RF, Casper ML, et al. Race and sex differences in rates of invasive cardiac procedures in US hospitals: data from the National Hospital Discharge Survey. Arch Intern Med. 1995;155:318–324. [PubMed] [Google Scholar]
- 27. Rodriguez F, Foody, JM , Wang Y, et al. Young Hispanic women experience higher in‐hospital mortality following an acute myocardial infarction. J Am Heart Assoc. 2015;4:e002089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Singh JA, Lu X, Ibrahim S, et al. Trends in and disparities for acute myocardial infarction: an analysis of Medicare claims data from 1992 to 2010. BMC Med. 2014;12:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pereira AC, Gomez LM, Bittencourt MS, et al. Age, gender, and race‐based coronary artery calcium score percentiles in the Brazilian Longitudinal Study of Adult Health (ELSA‐Brasil). Clin Cardiol. 2016;39:352–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Eisenberg JM. Sociologic influences on decision‐making by clinicians. Ann Intern Med. 1979;90:957–964. [DOI] [PubMed] [Google Scholar]
- 31. Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22:1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rhee MK, Ziemer DC, Caudle J, et al. Use of a uniform treatment algorithm abolishes racial disparities in glycemic control. Diabetes Educ. 2008;34:655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mathews R, Chen AY, Thomas L, et al. Differences in short‐term versus long‐term outcomes of older black versus white patients with myocardial infarction: findings from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of American College of Cardiology/American Heart Associations Guidelines (CRUSADE). Circulation. 2014;130:659–667. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Appendix Tables


