ABSTRACT
Background
Functional status assessment is the cornerstone of heart failure management and trials. The New York Heart Association (NYHA) classification and 6‐minute walk distance (6MWD) are commonly used tools; however, the correlation between them is not well understood.
Hypothesis
We hypothesised that the relationship between the NYHA classification and 6MWD might vary across studies.
Methods
A systematic literature search was performed to identify all studies reporting both NYHA class and 6MWD. Two reviewers independently assessed study eligibility and extracted data. Thirty‐seven studies involving 5678 patients were included.
Results
There was significant heterogeneity across studies in 6MWD within all NYHA classes: I (n = 16, Q = 934.2; P < 0.001), II (n = 25, Q = 1658.3; P < 0.001), III (n = 30, Q = 1020.1; P < 0.001), and IV (n = 6, Q = 335.5; P < 0.001). There was no significant difference in average 6MWD between NYHA I and II (420 m vs 393 m; P = 0.416). There was a significant difference in average 6MWD between NYHA II and III (393 m vs 321 m; P = 0.014) and III and IV (321 m vs 224 m; P = 0.027). This remained significant after adjusting for region of study, age, and sex.
Conclusions
Although there is an inverse correlation between NYHA II–IV and 6MWD, there is significant heterogeneity across studies in 6MWD within each NYHA class and overlap in 6MWD between NYHA I and II. The NYHA classification performs well in more symptomatic patients (NYHA III/IV) but less so in asymptomatic/mildly symptomatic patients (NYHA I/II). Nonetheless, the NYHA classification is an easily applied first‐line tool in everyday clinical practice, but its potential subjectivity should be considered when performing comparisons across studies.
Introduction
The New York Heart Association (NYHA) classification system was first developed in 1928 and has since undergone several revisions.1 The ease of application of this classification based on patients' reported symptoms has resulted in widespread use in many heart failure (HF) studies2, 3 and international guidelines.4, 5 The NYHA classification is often used as inclusion or exclusion criteria for therapy as well as for prognostication and assessment of outcomes.2, 3, 4, 5 Contrary to its extensive use, the actual objectivity of the NYHA is unclear. The NYHA classification is based on patient and physician assessment of cardiac symptoms including dyspnea, angina, and fatigue at different levels of physical activity, and its reliability and validity have been widely debated.6, 7, 8
Studies have evaluated the usefulness and reliability of more objective measures of HF severity, such as cardiopulmonary exercise testing (CPET) and bicycle and treadmill testing.9 Although CPET is regarded as the gold standard for assessment of aerobic functional capacity,10 there are significant financial and logistical costs involved. A viable alternative is the 6‐minute walk distance (6MWD), where the distance ambulated on a level surface within 6 minutes is used as a simple and inexpensive yet objective grading of HF severity and prognosis.11, 12, 13 Many studies have shown the objectivity and added prognostic value of the 6MWD in predicting outcomes.11, 12, 13
To date, there has not been any comprehensive literature review on the correlation between NYHA class and 6MWD. We aimed to assess the correlation between NYHA class and 6MWD by conducting a systematic review of all studies reporting both NYHA class and 6MWD.
Methods
Literature Search Strategy
A comprehensive search of the MEDLINE, Embase, and Cochrane Library databases was performed from January 1980 to Decemebr 2013 by 2 independent reviewers. The search terms used included “heart failure,” “congestive cardiac failure,” “New York Heart Association,” “six minute walk test,” and “six minute walk distance.” In addition, the references of the included studies and the bibliographies of review articles were searched for additional articles. There was no language restriction. The investigation conformed with the principles outlined in the Declaration of Helsinki. Because the study was based on review of existing literature with no active participation from study subjects, no approval from an ethics committee was required locally.
Inclusion and Exclusion Criteria
Only studies that provided the average 6MWD and its distribution for each individual class of NYHA were included. Studies that did not report the number of patients in each class, or where there were <5 patients in each class, were excluded. Studies that reported average 6MWD for combined NYHA classes (eg, combined class I–II) were also excluded. Figure 1 describes the study selection process.
Figure 1.
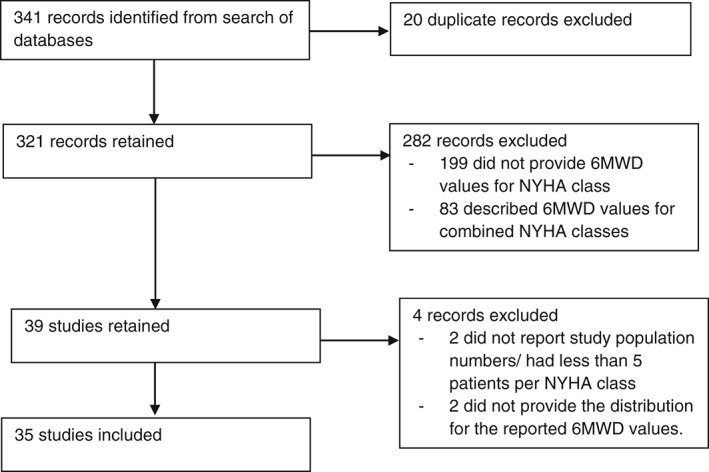
Flowchart of study selection. Abbreviations: 6MWD, 6‐minute walk distance; NYHA, New York Heart Association.
Data Extraction and Study Characteristics
Two reviewers (F.Y.L., L.L.T.) independently assessed the eligibility of the studies and performed data extraction on a prespecified data‐collection form. Discrepancies were resolved by consensus and consultation with a third investigator (J.Y.). Study characteristics collected included the date and type of study; region of study; number, age, and sex of study population; and average 6MWD and its distribution per NYHA class.
Statistical Analysis
For the pooled mean of the 6MWD, we used a random‐effects model based on the DerSimonian and Laird method. 14, 15 Random‐effect models methodology was selected as it was anticipated that systematic differences between studies (heterogeneity) would be likely. A Q statistic and corresponding P value was calculated using χ2 test to quantify the heterogeneity among combined results. Inconsistency was calculated using an I2 index to determine the impact of heterogeneity.
For each of the 4 NYHA classes, a separate meta‐analysis was performed to estimate the pooled mean of the 6MWD. Forest plots were produced to illustrate mean of 6MWD and its 95% confidence interval (CI). The studies are ordered by the size of the study, from the largest to smallest. In studies where median and interquartile range (IQR) of 6MWD were reported instead of mean and SD, estimation of the mean using IQR was determined within each of the NYHA classes. In these imputations, we assumed the distribution of 6MWD was similar to the normal distribution as the estimated average of 6MWD was close to the reported median.
To identify the association between 6MWD and NYHA, we further undertook study‐level meta‐regression analysis to assess the effects of NYHA, controlling for region, age, and sex (% of male sex). In this analysis, we compared the mean of the 6MWD for one class of NYHA to the next (adjacent) class, such as I vs II, II vs III, and III vs IV. Average age of each NYHA class was used as a continuous variable. Due to small numbers in the subgroups, region was categorized to 3 groups (North America, Europe, Others) in the meta‐regression analysis. The predicted 6MWD with multiple linear model of NYHA class, region, age, and sex was shown in the scatter plot. Stata software version 13 (StataCorp, Ltd., College Station, TX) was used for all analyses.
Results
Out of 321 studies, 35 studies involving 5422 patients met the study criteria and were included. Ten (29%) studies were from North America, 20 (57%) were from Europe, and 5 (14%) were from other regions (eg, South America, Asia). Table 1 describes the characteristics of the included studies. Sixteen studies reported data on NYHA class I, 24 on NYHA class II, 29 on NYHA class III, and 7 on NYHA class IV.
Table 1.
Summary of Included Studies
| Study | Country (Region) | Study Type | No. of Patients | Age, years, (SD/Range) | Male Sex, % | LVEF, %, SD (Range) | Data on NYHA Class(es) |
|---|---|---|---|---|---|---|---|
| Goode et al 20087 | UK (Europe) | Case–control | 1139 | 71 (64–77) | – | <40 | I, II |
| Rostagno et al 200313 | Italy (Europe) | Cohort | 146 | 64 (10) | – | 46 | I, II |
| Alahdab et al 200918 | US (North America) | Cohort | 198 | 55.7 (12.9) | 63.1 | 29 (40) | I, II, III, IV |
| Forman et al 201220 | US (North America) | Cohort | 2054 | 59 (51–68) | 71.0 | ≤35 | II, III |
| Zugck et al 200021 | Germany (Europe) | Cohort | 113 | 54 (12) | 79.646 | 19 | I, II, III |
| Radke et al 200524 | US (North America) | Cohort | 17 | – | 52.9 | – | I |
| Gary et al 200425 | US (North America) | RCT | 32 | – | 0 | 55 | II, III |
| Ingle et al 200826 | UK (Europe) | Case–control | 186 | – | – | – | I, II |
| Boşnak Guçlu et al 201127 | Turkey (Other) | Cohort | 34 | 69 (10) | 82 | 34 (8) | II, III |
| Karavidas et al 201028 | Greece (Europe) | Case–control | 18 | 62 (10) | 77.8 | <35 | II |
| Jankowska et al 200829 | Poland (Europe) | Cohort | 10 | 70 (6) | 90 | 30 (5) | II, III |
| Ates et al 201330 | Turkey (Other) | Cohort | 29 | 64 (7) | 52 | 32 (3) | II |
| Keast et al 201331 | Canada (North America) | RCT | 27 | 62.5 (11.4) | 81.5 | 27 (5) | III |
| Pepera et al 201232 | UK (Europe) | Case–control | 10 | – | 80 | 46 | I |
| Zaidi et al 201333 | US (North America) | Cohort | 5 | 35.5 (25–42) | – | 48 (9) | II |
| Jaski et al 201134 | US (North America) | Cohort | 39 | 60.5 (11.4) | 87.2 | 22 | III |
| Leszek et al 201035 | Poland (Europe) | Cohort | 34 | 61.5 (9.0) | 61.8 | 57 (12) | II, III |
| Jehn et al 200936 | Germany (Europe) | Cohort | 50 | 60.9 (14.0) | 76 | 39 (16) | I, II, III |
| Goscinska‐Bis et al 200837 | Poland (Europe) | RCT | 23 | 64.7 (7.0) | 87.0 | 30 (3) | III |
| Miller et al 200738 | US (North America) | Cohort | 25 | 50.1 (13.1) | – | 16 (6) | IV |
| Freimark et al 200739 | Israel (Other) | Case–control | 56 | – | 76.8 | – | II |
| Román et al 200640 | Spain (Europe) | Cohort | 22 | 45.4 (19–77) | 18.2 | – | II |
| Torre‐Amione et al 200541 | US (North America) | RCT | 37 | – | 70 | 22 | II |
| Ince et al 200442 | Germany (Europe) | RCT | 6 | – | 100 | 28 (9) | III |
| Guimãraes et al 200243 | Brazil (South America) | Cohort | 12 | 45 (12) | 100 | 23 (7) | III |
| Lellamo et al 201044 | Italy (Europe) | RCT | 32 | 69 (8) | 0 | 33 (6) | III |
| Rostagno et al 200045 | Italy (Europe) | Cohort | 140 | 45.4 (29–70) | – | 35 | I, II, III, IV |
| Rostagno et al 200046 | Italy (Europe) | Cohort | 33 | 57.3 (31–72) | – | 38 | I |
| Faggiano et al 199747 | Italy (Europe) | Cohort | 26 | 56 (11) | 92 | 22 (6) | II, III, IV |
| Bagur et al 201148 | Canada (North America) | Cohort | 46 | 56 (8) | – | 53 (15) | I, II, III |
| Tay et al 201149 | UK (Europe) | Cohort | 12 | 80 (10) | 17 | ≥40 | II, III |
| Jehn et al 201050 | Switzerland (Europe) | Cohort | 97 | 34 (13) | 76 | 40 (18) | I, II, III |
| Vrtovec et al 201351 | Slovenia (Europe) | RCT | 40 | 61 (10) | 85 | 26 (4) | III |
| Deuschle et al 201152 | Germany (Europe) | Cohort | 95 | 56 (25–80) | – | 60 (22–77) | I, II, III, IV |
| Souza et al 200753 | Brazil (South America) | Cohort | 38 | 37 (2) | – | – | I, II, III, IV |
Abbreviations: LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; RCT, randomized controlled trial; SD, standard deviation; UK, United Kingdom; US, United States.
Analysis Within Each New York Heart Association Class
An analysis of the reported 6MWD by NYHA classes showed a pooled estimate of 358 m (P < 0.0001; Q = 5580.1) and higher 6MWD associated with lower NYHA functional class (Table 2). There was significant heterogeneity between studies seen in each of NYHA classes (all P < 0.0001; Q = 934.2, 1657.6, 964.0, and 248.4 for NYHA classes I, II, III, and IV, respectively; Table 2 and Figure 2).
Table 2.
Heterogeneity Within Each NYHA Class
| NYHA Class | No. of Studies | No. of Patients | Pooled Average 6MWD, m (95% CI) | I 2, % | Q | P Value |
|---|---|---|---|---|---|---|
| I | 16 | 984 | 420 (379 to 462) | 98.4 | 934.2 | <0.0001 |
| II | 24 | 2769 | 393 (362 to 424) | 98.6 | 1657.6 | <0.0001 |
| III | 29 | 1530 | 325 (296 to 354) | 97.1 | 964.0 | <0.0001 |
| IV | 7 | 139 | 225 (115 to 336) | 97.6 | 248.4 | <0.0001 |
| Overall | 35 | 5422 | 358 (338 to 379) | 98.7 | 5580.1 | <0.0001 |
Abbreviations: 6MWD, 6‐minute walk distance; CI, confidence interval; NYHA, New York Heart Association.
Figure 2.
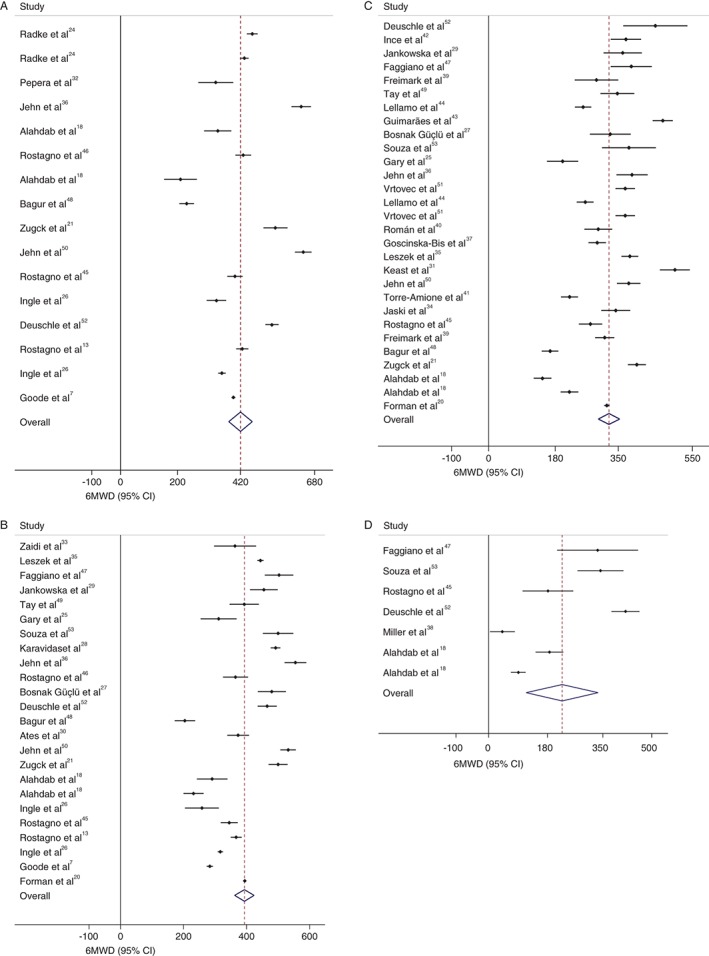
Distribution of 6MWD within NYHA, (A) class I, (B) class II, (C) class III, and (D) class IV. Abbreviations: 6MWD, 6‐minute walk distance; CI, confidence interval; NYHA, New York Heart Association.
Analysis Across New York Heart Association Classes
When adjacent classes of NYHA are compared, the smallest difference between 6MWD was seen in patients with class I and II (420 m vs 393 m) and the largest difference was in patients with classes III and IV (325 m vs 225 m). Meta‐regression analyses were used to assess the associations between 6MWD and NYHA functional class (Table 3). Significant difference between studies was present between class II and III (coefficient 67.4; 95% CI: 10.1 to 124.7, P = 0.022) and between class III and IV (coefficient 102.7; 95% CI: 13.0 to 192.4, P = 0.026). There was no significant difference between class I and II (coefficient 27.1; 95% CI: −39.8 to 93.9, P = 0.422). Adjusting for region, age, and sex did not change these associations. The estimated variance (τ2) between studies was reduced from 10 480 to 7239 when all these variables were combined in the model (Table 3, Figure 3).
Table 3.
Comparison of 6MWD by NYHA Class
| Coefficient (95% CI) | P Value | Coefficient (95% CI)a | P Valuea | |
|---|---|---|---|---|
| NYHA I vs II | 27.1 (−39.8 to 93.9) | 0.422 | 49.8 (−9.1 to 108.8) | 0.096 |
| NYHA II vs III | 67.4 (10.1 to 124.7) | 0.022 | 70.5 (21.6 to 119.3) | 0.005 |
| NYHA III vs IV | 102.7 (13.0 to 192.4) | 0.026 | 105.0 (25.5 to 184.5) | 0.010 |
Abbreviations: 6MWD, 6‐minute walk distance; CI, confidence interval; NYHA, New York Heart Association.
Corrected for region, age, and sex.
Figure 3.
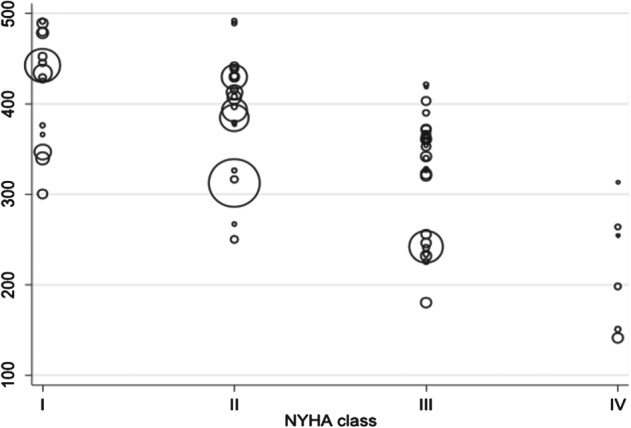
Comparison of 6MWD by NYHA class. Abbreviations: 6MWD, 6‐minute walk distance; NYHA, New York Heart Association.
Discussion
This is the first study to systemically analyze the correlation between NYHA class and 6MWD. It demonstrates the subjectivity of the NYHA classification when compared with a more objective measure like the 6MWD, with the 6MWD in all NYHA classes showing significant heterogeneity across different studies. Despite this heterogeneity, worsening NYHA class status appears to correlate well with decreasing 6MWD between class II and III, and between class III and IV.
The basis of the NYHA classification stems from a patient's perceived and reported cardiac symptoms, as well the physician's assessment of these symptoms. This easy availability has resulted in its extensive use in numerous trials as well as guidelines. Some studies have shown the NYHA classification to be subjective. Surveys among physicians assessing NYHA class showed only about 54% to 56% concordance, giving a result little better than chance.6, 8 There was also no consistent method used to assess NYHA class with criteria ranging from self‐reported walking distance to difficulty climbing stairs.8 Self‐reported walking distance has been shown to neither correlate with formally measured exercise capacity nor have any prognostic relevance.8 Goode et al found significant difference in physician‐rated and patient‐rated NYHA class in a study of >1000 HF patients.7 Severo et al also found discrepant interobserver thresholds of NYHA classification.16
In contrast, the 6MWD is a more objective test of a patient's functional capacity, requiring the patient to walk in a reproducible environment. The 6MWD has been shown in studies to have good prognostic value in the different subsets of HF patients. In a study of about 200 patients with mild to moderate HF, 6MWD was a strong predictor of mortality.13 Castel et al showed that in patients with moderate to severe HF receiving cardiac resynchronization therapy, 6MWD was found to be an independent predictor of mortality.17 Six‐minute walk distance also strongly predicted mortality and HF rehospitalisations in patients hospitalized for acute HF.18 However, the 6MWD is not without limitations. The test does not provide insight into the mechanisms of exercise limitation, and its results can be affected by a variety of factors unrelated to cardiopulmonary status, including age, sex, height, and weight. Some studies have shown that the change in 6MWD after the onset of therapy does not appear to predict outcomes in HF.19 Other than 6MWD, cardiopulmonary exercise testing has often been used as the gold standard for functional assessment,10 but this test requires appropriate equipment, trained staff, and logistical support and is relatively expensive. Several studies have shown the 6WMD to have similar utility and prognostic predictive value as CPET in patients with HF.20, 21 The appeal of the 6MWD stems from its reproducibilty, simplicity, and cost‐effectiveness. However, the limitations of this test, as mentioned above, have to be considered.
In this study, the variation between NYHA class and 6MWD was comprehensively analyzed in 2 distinct ways: within each NYHA class and between 2 adjacent NYHA classes. Comparing the different studies reporting 6MWD within each NYHA class, there was significant heterogeneity of 6MWD reported within all of the NYHA classes. Comparing the average 6MWD by NYHA class, there was no significant difference between class I and II, although there was a difference noted between class II vs III and class III vs IV. In this analysis, NYHA class appears useful for discriminating between mild and severe HF, but it may be more subjective in differentiating between mild and moderate HF. This has potential implications. Currently, various major guidelines, like the European4 and American guidelines22, 23 for device therapy (eg, implantable cardioverter‐defibrillator and cardiac resynchronization therapy), base their recommendations on the NYHA functional class. For example, implantable cardioverter‐defibrillator therapy is recommended as a class I indication for primary prevention in NYHA II/III patients with impaired ejection fraction (EF), but it is not recommended for those with poor functional status.22 Cardiac resynchronisation therapy is also recommended as a class I indication in suitable NYHA II/III and ambulatory NYHA IV patients, but not to those in NYHA I.4, 23 Differences in interpretation of NYHA class can result in a change in strength of indication for therapy from a class I recommendation to a lesser one. This conclusion appears mostly relevant for the group of patients who are asymptomatic/mildly symptomatic (NYHA I/II) and less so in more symptomatic HF patients (NYHA III/IV). Although NYHA classification is to some degree subjective, it is still an easily applied first‐line tool in everyday clinical practice to assess patients' functional limitation. Moreover, in more symptomatic patients (NYHA III/IV), the NYHA classification appears to be a well‐performing, accurate clinical tool to estimate these patients' functional limitation and guide therapy.
Study Limitations
Limitations of this study include the potential influence of other variables such as age, sex, comorbidities, and ethnicity on both NYHA class and 6MWD. Age and sex were corrected for in the analyses. For differences in ethnicity, an attempt to correct for this was made by considering the region of study. As data on comorbidities were not uniformly available in these reports, these could not be accounted for during the analysis. Differences between patients with reduced and preserved EF may exist. In the included studies that reported data on preserved EF,24, 25, 26 these were not higher than those with reduced EF. Ingle et al reported similar 6MWD between both groups of patients.26 Second, we would ideally have liked to compare both NYHA and 6MWD to cardiopulmonary exercise testing or clinical outcomes, but these were not available in all studies. Other limitations included lack of information on clinical significance of repeated measurements within each study.
Conclusion
Although there is an inverse correlation between NYHA class II to IV and 6MWD, there is significant heterogeneity across studies in reported 6MWD within each NYHA class and overlap in reported 6MWD between NYHA I and II. The NYHA classification appears to perform well in more symptomatic patients (NYHA III/IV) but less so in asymptomatic/mildly symptomatic patients (NYHA I/II). Nonetheless, the NYHA is an easily applied first‐line tool in everyday clinical practice, but its potential subjectivity should be considered when performing comparisons across studies.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Criteria Committee of the New York Heart Association . Diseases of the heart and blood vessels In: Harvey RM, et al, eds. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels 7th ed Boston, MA: Little, Brown & Co; 1973:286. [Google Scholar]
- 2. Castel MA, Magnani S, Mont L, et al. Survival in New York Heart Association class IV heart failure patients treated with cardiac resynchronization therapy compared with patients on optimal pharmacological treatment. Europace. 2010;12:1136–1140. [DOI] [PubMed] [Google Scholar]
- 3. Muntwyler J, Abetel G, Gruner C, et al. One‐year mortality among unselected outpatients with heart failure. Eur Heart J. 2002;23:1861–1866. [DOI] [PubMed] [Google Scholar]
- 4. Brignole M, Auricchio A, Baron‐Esquivias G, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on Cardiac Pacing and Resynchronization Therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013;15:1070–1118. [DOI] [PubMed] [Google Scholar]
- 5. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC [published correction appears in Eur J Heart Fail. 2013;15:361–362]. Eur J Heart Fail. 2012;14:803–869. [DOI] [PubMed] [Google Scholar]
- 6. Goldman L, Hashimoto B, Cook EF, et al. Comparative reproducibility and validity of systems for assessing cardiovascular functional class: advantages of a new specific activity scale. Circulation. 1981;64:1227–1234. [DOI] [PubMed] [Google Scholar]
- 7. Goode KM, Nabb S, Cleland JG, et al. A comparison of patient and physician‐rated New York Heart Association class in a community‐based heart failure clinic. J Cardiac Fail. 2008;14:379–387. [DOI] [PubMed] [Google Scholar]
- 8. Raphael C, Briscoe C, Davies J, et al. Limitations of the New York Heart Association functional classification system and self‐reported walking distances in chronic heart failure. Heart. 2007;93:476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fedele F, Severino P, Calcagno S, et al. Heart failure: TNM‐like classification. J Am Coll Cardiol. 2014;63:1959–1960. [DOI] [PubMed] [Google Scholar]
- 10. Balady GJ, Arena R, Sietsema K, et al. Clinician's guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:191–225. [DOI] [PubMed] [Google Scholar]
- 11. Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6‐minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 12. Lee R, Chan YH, Wong J, et al. The 6‐minute walk test predicts clinical outcome in Asian patients with chronic congestive heart failure on contemporary medical therapy: a study of the multiracial population in Singapore. Int J Cardiol. 2007;119:168–175. [DOI] [PubMed] [Google Scholar]
- 13. Rostagno C, Olivo G, Comeglio M, et al. Prognostic value of 6‐minute walk corridor test in patients with mild to moderate heart failure: comparison with other methods of functional evaluation. Eur J Heart Fail. 2003;5:247–252. [DOI] [PubMed] [Google Scholar]
- 14. Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta‐analysis In: Egger M, Smith GD, Altman DG, eds. Systematic Reviews in Health Care: Meta‐analysis in Context London, UK: BMJ Publishing Group; 2001:285–312. [Google Scholar]
- 15. DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 16. Severo M, Gaio R, Lourenço P, et al. Indirect calibration between clinical observers—application to the New York Heart Association functional classification system. BMC Res Notes. 2011;4:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Castel MA, Méndez F, Tamborero D, et al. Six‐minute walking test predicts long‐term cardiac death in patients who received cardiac resynchronization therapy. Europace. 2009;11:338–342. [DOI] [PubMed] [Google Scholar]
- 18. Alahdab MT, Mansour IN, Napan S, et al. Six minute walk test predicts long‐term all‐cause mortality and heart failure rehospitalization in African‐American patients hospitalized with acute decompensated heart failure. J Cardiac Fail. 2009;15:130–135. [DOI] [PubMed] [Google Scholar]
- 19. Shah MR, Hasselblad V, Georghiade M, et al. Prognostic usefulness of the six‐minute walk in patients with advanced congestive heart failure secondary to ischemic or nonischemic cardiomyopathy. Am J Cardiol. 2001;88:987–993. [DOI] [PubMed] [Google Scholar]
- 20. Forman DE, Fleg JL, Kitzman DW, et al. 6‐min walk test provides prognostic utility comparable to cardiopulmonary exercise testing in ambulatory outpatients with systolic heart failure. J Am Coll Cardiol. 2012;60:2653–2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zugck C, Krüger C, Dürr S, et al. Is the 6‐minute walk test a reliable substitute for peak oxygen uptake in patients with dilated cardiomyopathy? Eur Heart J. 2000;21:540–549. [DOI] [PubMed] [Google Scholar]
- 22. Epstein AE, Dimarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device‐based therapy of cardiac rhythm abnormalities: executive summary [published correction appears in Heart Rhythm. 2009;6:e1]. Heart Rhythm. 2008;5:934–955. [DOI] [PubMed] [Google Scholar]
- 23. Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device‐based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2013;61:e6–e75. [DOI] [PubMed] [Google Scholar]
- 24. Radke KJ, King KB, Blair ML, et al. Hormonal responses to the 6‐minute walk test in women and men with coronary heart disease: a pilot study. Heart Lung. 2005;34:126–135. [DOI] [PubMed] [Google Scholar]
- 25. Gary RA, Sueta CA, Dougherty M, et al. Home‐based exercise improves functional performance and quality of life in women with diastolic heart failure. Heart Lung. 2004;33:210–218. [DOI] [PubMed] [Google Scholar]
- 26. Ingle L, Cleland JG, Clark AL. Perception of symptoms is out of proportion to cardiac pathology in patients with “diastolic heart failure.” Heart. 2008;94:748–753. [DOI] [PubMed] [Google Scholar]
- 27. Boşnak Guçlu M, Inal İnce D, Arıkan H, et al. A comparison of pulmonary function, peripheral and respiratory muscle strength and functional capacity in the heart failure patients with different functional classes [article in Turkish]. Anadolu Kardiyol Derg. 2011;11:101–106. [DOI] [PubMed] [Google Scholar]
- 28. Karavidas A, Parissis JT, Matzaraki V, et al. Functional electrical stimulation is more effective in severe symptomatic heart failure patients and improves their adherence to rehabilitation programs. J Cardiac Fail. 2010;16:244–249. [DOI] [PubMed] [Google Scholar]
- 29. Jankowska EA, Wegrzynowska K, Superlak M, et al. The 12‐week progressive quadriceps resistance training improves muscle strength, exercise capacity and quality of life in patients with stable chronic heart failure. Int J Cardiol. 2008;130:36–43. [DOI] [PubMed] [Google Scholar]
- 30. Ates I, Yavuz AH, Doğru M, et al. Effects of ivabradine on 6‐minute walk test and quality of life in patients with previously implanted CRT‐D. J Investig Med. 2013;61:1013–1017. [DOI] [PubMed] [Google Scholar]
- 31. Keast ML, Slovinec D'Angelo ME, Nelson CR, et al. Randomized trial of Nordic walking in patients with moderate to severe heart failure. Can J Cardiol. 2013;29:1470–1476. [DOI] [PubMed] [Google Scholar]
- 32. Pepera GK, Sandercock GR, Sloan R, et al. Influence of step length on 6‐minute walk test performance in patients with chronic heart failure. Physiotherapy. 2012;98:325–329. [DOI] [PubMed] [Google Scholar]
- 33. Zaidi AN, White L, Holt R, et al. Correlation of serum biomarkers in adults with single ventricles with strain and strain rate using 2D speckle tracking. Congenit Heart Dis. 2013;8:255–265. [DOI] [PubMed] [Google Scholar]
- 34. Jessup M, Greenberg B, Mancini D, et al. Calcium Upregulation by Percutaneous Administration of Gene Therapy in Cardiac Disease (CUPID): a phase 2 trial of intracoronary gene therapy of sarcoplasmic reticulum Ca2 + −ATPase in patients with advanced heart failure. Circulation. 2011;124:304–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Leszek P, Klisiewicz A, Janas J, et al. Usefulness of 6‐minute walk test, plasma neurohumoral and cytokine activation in the assessment of symptomatic patients with left ventricle dysfunction caused by chronic severe mitral valve regurgitation. Acta Cardiol. 2010;65:43–51. [DOI] [PubMed] [Google Scholar]
- 36. Jehn M, Schmidt‐Trucksäss A, Schuster T, et al. Accelerometer‐based quantification of 6‐minute walk test performance in patients with chronic heart failure: applicability in telemedicine. J Cardiac Fail. 2009;15:334–340. [DOI] [PubMed] [Google Scholar]
- 37. Goscinska‐Bis K, Bis J, Krejca M, et al. Totally epicardial cardiac resynchronization therapy system implantation in patients with heart failure undergoing CABG. Eur J Heart Fail. 2008;10:498–506. [DOI] [PubMed] [Google Scholar]
- 38. Miller LW, Pagani FD, Russell SD, et al; HeartMate II Clinical Investigators. Use of a continuous‐flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357:885–896. [DOI] [PubMed] [Google Scholar]
- 39. Freimark D, Shechter M, Schwamenthal E, et al. Improved exercise tolerance and cardiac function in severe chronic heart failure patients undergoing a supervised exercise program. Int J Cardiol. 2007;116:309–314. [DOI] [PubMed] [Google Scholar]
- 40. Román A, Gispert P, Monforte V, et al. Long‐term outcomes of treatment with bosentan in pulmonary hypertension [article in Spanish]. Arch Bronconeumol. 2006;42:616–620. [DOI] [PubMed] [Google Scholar]
- 41. Torre‐Amione G, Sestier F, Radovancevic B, et al. Broad modulation of tissue responses (immune activation) by celacade may favorably influence pathologic processes associated with heart failure progression. Am J Cardiol. 2005;95:30C–40C. [DOI] [PubMed] [Google Scholar]
- 42. Ince H, Petzsch M, Rehders TC, et al. Transcatheter transplantation of autologous skeletal myoblasts in postinfarction patients with severe left ventricular dysfunction. J Endovasc Ther. 2004;11:695–704. [DOI] [PubMed] [Google Scholar]
- 43. Guimãraes GV, Bellotti G, Bacal F, et al. Can the cardiopulmonary 6‐minute walk test reproduce the usual activities of patients with heart failure? [article in English, Portuguese]. Arq Bras Cardiol. 2002;78:553–560. [PubMed] [Google Scholar]
- 44. Iellamo F, Volterrani M, Caminiti G, et al. Testosterone therapy in women with chronic heart failure: a pilot double‐blind, randomized, placebo‐controlled study. J Am Coll Cardiol. 2010;56:1310–1316. [DOI] [PubMed] [Google Scholar]
- 45. Rostagno C, Galanti G, Comeglio M, et al. Comparison of different methods of functional evaluation in patients with chronic heart failure. Eur J Heart Fail. 2000;2:273–280. [DOI] [PubMed] [Google Scholar]
- 46. Rostagno C, Galanti G, Felici M, et al. Prognostic value of baroreflex sensitivity assessed by phase IV of Valsalva manoeuvre in patients with mild‐to‐moderate heart failure. Eur J Heart Fail. 2000;2:41–45. [DOI] [PubMed] [Google Scholar]
- 47. Faggiano P, D'Aloia A, Gualeni A, et al. Assessment of oxygen uptake during the 6‐minute walking test in patients with heart failure: preliminary experience with a portable device. Am Heart J. 1997;134(2 part 1):203–206. [DOI] [PubMed] [Google Scholar]
- 48. Bagur R, Rodés‐Cabau J, Dumont E, et al. Performance‐based functional assessment of patients undergoing transcatheter aortic valve implantation. Am Heart J. 2011;161:726–734. [DOI] [PubMed] [Google Scholar]
- 49. Tay EL, Papaphylactou M, Diller GP, et al. Quality of life and functional capacity can be improved in patients with Eisenmenger syndrome with oral sildenafil therapy. Int J Cardiol. 2011;149:372–376. [DOI] [PubMed] [Google Scholar]
- 50. Jehn M, Schmidt‐Trucksäss A, Schuster T, et al. Pedometer accuracy in patients with chronic heart failure. Int J Sports Med. 2010;31:186–191. [DOI] [PubMed] [Google Scholar]
- 51. Vrtovec B, Poglajen G, Lezaic L, et al. Comparison of transendocardial and intracoronary CD34+ cell transplantation in patients with nonischemic dilated cardiomyopathy. Circulation. 2013;128(11 suppl 1):S42–S49. [DOI] [PubMed] [Google Scholar]
- 52. Deuschle K, Weinert K, Becker MO, et al. Six‐minute walk distance as a marker for disability and complaints in patients with systemic sclerosis. Clin Exp Rheumatol. 2011;29(2 suppl 65):S53–S59. [PubMed] [Google Scholar]
- 53. Souza R, Jardim C, Julio Cesar Fernandes C, et al. NT‐proBNP as a tool to stratify disease severity in pulmonary arterial hypertension. Respir Med. 2007;101:69–75. [DOI] [PubMed] [Google Scholar]


