Abstract
Reports of increasing methamphetamine use among vulnerable populations may be attributed in part to the adaptive use of stimulants in response to the loss of stable housing through residential eviction. We employed multivariable recurrent event extended Cox regression to examine the independent association between recent evictions and initiation of or relapse into crystal methamphetamine use among people who inject drugs in Vancouver, Canada enrolled in two prospective cohort studies. In a multivariable analysis, eviction remained independently associated with methamphetamine initiation or relapse (adjusted hazard ratio = 1.90; 95% confidence interval: 1.31–2.75). Findings demonstrate the need to secure tenancies for drug-using populations to reduce harms.
Keywords: Cox regression, drug use, eviction, housing, initiation, methamphetamine
Background
While overall trends in methamphetamine use may be stabilizing in the general North American population,1 widespread and increasing methamphetamine use has been reported among members of vulnerable and marginalized populations, including those who are homeless and unstably housed2–4 and people who inject drugs.4–6 Longitudinal cohort studies of people who inject drugs have reported high levels of methamphetamine use that appear to be increasing in some urban settings in Australia, the United States and Canada.5,7,8 Furthermore, methamphetamine use among people who inject drugs has been shown to be associated with a number of severe harms, including hepatitis C infection,9 psychosis10 and cerebrovascular complications, including stroke.11 Therefore, identifying factors associated with relapse or initiation into methamphetamine use among people who inject drugs should inform policy and programmatic efforts to reduce harms associated with drug use.
A possible contributing cause to increasing methamphetamine use among people who inject drugs is its adaptive use in response to changes in housing status. The social adaptation model of the etiology of substance use among homeless and unstably housed populations characterizes substance use as a means of coping with the trauma, stress, and uncertainty of homelessness.12 For example, methamphetamine use has a long history of functional use as a means to stay awake and alert.13,14 Indeed, homelessness has been independently associated with the initiation of methamphetamine use among people who inject drugs,4,5 in part because of its perceived benefits in improving concentration and productivity.15 For people who inject drugs, homelessness and unstable housing have been found to significantly increase the risk of early mortality,16 exposure to violence,17 drug-related risk behavior18 and difficulty in accessing treatment for drug or alcohol use.19
Concurrent with reported increases in methamphetamine use among people who inject drugs,5 a growing epidemic of residential evictions has been documented in the wake of a widespread housing affordability crisis in cities around the world.20,21 Evictions have been found to be an increasingly common22–25 and distinctively harmful pathway into homelessness.21,26,27 Studies have shown that evictions have become commonplace among people living in poverty, particularly those living in high crime communities and those connected to disadvantaged social networks.20 While little research is available on pathways into eviction among people who inject drugs, the ongoing criminalization of illicit drug use, poverty and social stigma faced by people who inject drugs likely elevates the risk of eviction within this group.19,28
Qualitative research has characterized evictions as precipitating a period of intense stress, uncertainty and intensifying material hardship.26,29 Evictions have been shown to significantly increase the risk of suicide,21,30 exposure to violence,31 depression32 and psychological distress.33 In a study of HIV-positive people who inject drugs in a setting with no-cost antiretroviral therapy, evictions were associated with detectable HIV viral load, mediated through poor adherence to antiretroviral therapy.34 These findings suggest that evictions are more than just a pathway into homelessness—they are a distinctively consequential life event associated with intense adverse health outcomes. While, to the best of our knowledge, no research has explored the effect of evictions on drug use related risk, we hypothesized that residential evictions would increase the likelihood that people who inject drugs initiated or relapsed into methamphetamine use. To test this hypothesis, we longitudinally examined the relationship between evictions and initiation of or relapse into methamphetamine use among people who inject drugs in Vancouver, Canada.
Methods
Study sample
The Vancouver Injection Drug Users Study (VIDUS) and the AIDS Care Cohort to evaluate Exposure to Survival Services (ACCESS) are two open prospective cohort studies of people who use drugs operating in Vancouver, Canada. Participants have been recruited through self-referral, snowball sampling, and street outreach in the Greater Vancouver region since May 1996. These cohorts have been described in detail previously.35,36 In brief, VIDUS enrolls HIV-negative adults (≥18 years of age) who injected illicit drugs at least once in the previous month at enrollment. ACCESS enrolls HIV-positive adults who used illicit drugs other than or in addition to cannabis in the previous month. VIDUS participants who seroconverted to HIV following recruitment have been transferred into the ACCESS study. All eligible participants provided written informed consent. The studies have been approved by the University of British Columbia/Providence Health Care Research Ethics Board.
The follow-up procedures for each study have been harmonized to allow for combined analyses. At baseline and semi-annually, all study participants completed a harmonized interviewer-administered questionnaire that elicited socio-demographic information, drug use and other behavioral patterns, and social and structural exposures. In addition, participants also provided blood samples for HIV and hepatitis C testing, and HIV disease monitoring as appropriate. At the conclusion of each visit, study participants received a $30 CDN honorarium. Questions regarding experiences of eviction were added to the study instrument in June 2007; therefore, we restricted our analyses to individuals who completed at least two study visits between June 2007 and May 2015, reported a history of injection drug use at baseline, and did not report crystal methamphetamine use in the past 6 months at their first visit during the study period. Ultimately, our sample consisted of 1257 participants.
Measures
The primary outcome for this analysis was self-reported initiation of or relapse into crystal methamphetamine use by injection or non-injection in the past 6 months (yes versus no). We defined initiation or relapse to mean having used crystal methamphetamine at least once in the past 6 months during follow-up. Because we did not ask about a history of crystal methamphetamine use by non-injection at baseline, the first report of crystal methamphetamine use during follow-up could have been the initiation of or relapse into crystal methamphetamine use. The primary explanatory variable of interest was a residential eviction in the past 6 months, defined as answering yes to the question, ‘Have you been evicted in the last 6 months?’
In order to examine the extent to which evictions contribute to methamphetamine initiation or relapse we examined a set of potential confounding variables that were previously found to increase the risk of methamphetamine use.37–39 The potential confounders considered in this analysis were sex (male versus female), age (per 10 years older), ethnicity/ancestry (white versus other), education (high school or higher versus less than high school), sexual orientation (non-heterosexual versus heterosexual), childhood emotional abuse, history of sexual abuse, being in a stable relationship, homelessness, HIV status (positive versus negative), employment (regular or temporary job, or self-employed), police or court imposed warrant or area restriction, any drug or alcohol treatment, drug dealing, incarceration, sex work involvement, heavy alcohol use and benzodiazepine use. Area restrictions referred to police or court imposed conditions of release, typically attached to judicial interim release orders, colloquially called ‘bail orders’, as an optional condition aimed at reducing the likelihood of recidivism. Other drug use behaviors considered included: daily non-injection crack use, daily heroin injection, and daily cocaine injection. Unless otherwise indicated, all behavioral variables referred to the 6-month period preceding the date of the interview and were treated as time-varying variables.
Analysis
First, we calculated the incidence density of crystal methamphetamine initiation or relapse using person-time methods. We estimated the time to the first report of crystal methamphetamine use by taking the midpoint between the date of the first interview during which crystal methamphetamine use was reported and the preceding interview in which the participant did not report crystal methamphetamine use. Then, we compared the baseline sample characteristics between those who reported initiation of or relapse into methamphetamine use at least once during follow-up with those who did not, using Pearson’s χ2 test for categorical variables and Wilcoxon rank sum test for continuous variables.
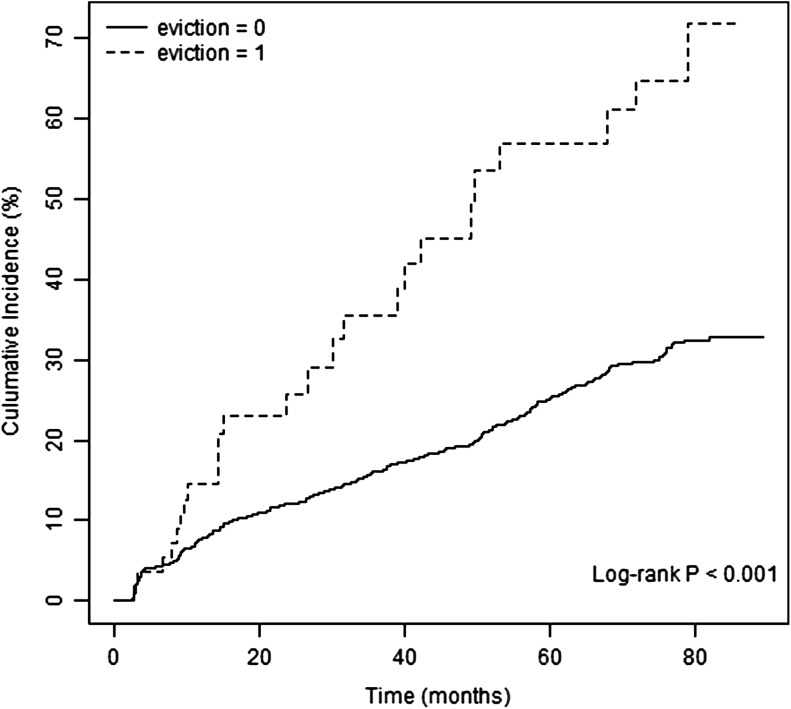
Next we used Kaplan–Meier methods40 to determine the cumulative incidence of crystal methamphetamine initiation or relapse during follow-up, stratifying the sample by those who did and did not report eviction at baseline. We used the log-rank test to compare the survival distributions of those two groups.
Because some participants reported initiating or relapsing into methamphetamine use more than once during follow-up, we constructed a recurrent event survival model to examine the relationship between evictions and the outcome of interest. We used a proportional rates-means model described by Lin et al.41 to account for correlation among the length of individuals’ repeated time at risk for crystal methamphetamine initiation or relapse. In this model, we specified a counting process framework to define time to repeated events, such that individuals were considered to be at risk from time zero to the first event, from the subsequent study visit when no crystal methamphetamine use was reported in the previous 6 months to the second event, and so forth. As in the case of the Cox proportional hazards regression, the model assumed proportional means.41 We assessed this assumption for each variable of interest by visual inspection of the Schoenfeld residuals plots42 and by examining time-by-covariate interactions.43
We first computed hazard ratios representing the bivariable associations between eviction and potential confounders with repeated crystal methamphetamine initiation or relapse. We then examined the independent effect of evictions by fitting a multivariable model that included all variables that were significantly associated with crystal methamphetamine initiation or relapse at the P < 0.05 level in bivariable analyses.
We also inspected a potential interaction between homelessness and eviction. At baseline, the phi coefficient (mean square contingency coefficient)44 between these two variables was 0.26, and the P-value of the baseline association using logistic regression was <0.01. In order to examine the effect of the interaction between homelessness and eviction, we re-ran our multivariable models including main effects and the interaction term. The interaction resulted in P = 0.95, showing that this interaction did not have any effect on the result. Then, we re-ran our model excluding the homelessness variable, and the eviction variable remained significantly associated with the outcome (P < 0.01). Therefore, we concluded that the association has not been driven by the possible interaction between homelessness and eviction. We conducted all statistical analyses with R software version 3.2.4 ,45 and all P values were two-sided.
Results
In total, 1257 people who inject drugs were eligible for the present study. These individuals completed a median of 9 (interquartile range [IQR]: 5–13) study visits and contributed 11 069 observations and 31 539 person-years. The median age at baseline was 45 years (IQR = 38–50), and 806 (64.1%) were male. During the study period, 280 (22.3%) participants reported one or more reports of recent evictions. Of those who had been evicted, 52 (16.6%) had been evicted more than once, with 12 (4.3%) participants reporting three or more evictions. In total, 339 (27.0%) participants initiated or relapsed into crystal methamphetamine use during follow-up, with an incidence density of 1.13 (95% confidence interval [CI]: 1.02–1.26) per 100 person-years. Among those who initiated or relapsed 234 (69.0%) did so on one occasion during follow-up, 79 (23.3%) on two occasions, and 26 (7.7%) on three or more occasions. Self-reported crystal methamphetamine use at the time of re-initiation tended towards more infrequent patterns of use. A considerable proportion of events (50%) involved using crystal methamphetamine less than once a month, while only 11% reported using everyday. Stratified by the number of re-initiation events these patterns remain stable, except for the two participants who reported five re-initiation events during the study period and described more frequent crystal methamphetamine use. The baseline sample characteristics stratified by crystal methamphetamine initiation or relapse during follow-up are shown in Table 1.
Table 1.
Baseline characteristics of people who inject drugs who did and did not report crystal methamphetamine initiation or relapse at least once during follow-up in Vancouver, Canada (n = 1257)
| Characteristic | Total (%) n = 1257 | Meth usea | P value | |
|---|---|---|---|---|
| No (%) n = 918 | Yes (%) n = 339 | |||
| Evictionb | ||||
| Yes | 82 (6.5) | 51 (5.6) | 31 (9.1) | 0.022 |
| No | 1175 (93.5) | 867 (94.4) | 308 (90.9) | |
| Sex | ||||
| Male | 806 (64.1) | 589 (64.2) | 217 (64.0) | 0.961 |
| Female | 451 (35.9) | 329 (35.8) | 122 (36.0) | |
| Age | ||||
| Median (IQR) | 44.5 (38.2–50.3) | 45.6 (39.4–51.3) | 41.3 (36.0–46.8) | <0.001c |
| Ethnicity/ancestry | ||||
| Other | 545 (43.4) | 406 (44.2) | 139 (41.0) | 0.306 |
| White | 712 (56.6) | 512 (55.8) | 200 (59.0) | |
| Education | ||||
| High school or higher | 617 (49.1) | 472 (51.4) | 145 (42.8) | 0.012 |
| Less than high school | 617 (49.1) | 433 (47.2) | 184 (54.3) | |
| Sexual orientation | ||||
| Non-heterosexual | 133 (10.6) | 85 (9.3) | 48 (14.2) | 0.013 |
| Heterosexual | 1114 (88.6) | 825 (89.9) | 289 (85.3) | |
| Childhood emotional abuse | ||||
| Yes | 501 (39.9) | 361 (39.3) | 140 (41.3) | 0.172 |
| No | 660 (52.5) | 499 (54.4) | 161 (47.5) | |
| Sexual abuse in lifetime | ||||
| Yes | 596 (47.4) | 426 (46.4) | 170 (50.1) | 0.238 |
| No | 661 (52.6) | 492 (53.6) | 169 (49.9) | |
| In a stable relationship | ||||
| Yes | 366 (29.1) | 272 (29.6) | 94 (27.7) | 0.574 |
| No | 874 (69.5) | 636 (69.3) | 238 (70.2) | |
| Homelessb | ||||
| Yes | 379 (30.2) | 230 (25.1) | 149 (44.0) | <0.001 |
| No | 875 (69.6) | 687 (74.8) | 188 (55.5) | |
| Employmentb | ||||
| Yes | 301 (23.9) | 226 (24.6) | 75 (22.1) | 0.358 |
| No | 956 (76.1) | 692 (75.4) | 264 (77.9) | |
| HIV seropositiveb | ||||
| Yes | 516 (41.1) | 355 (38.7) | 161 (47.5) | 0.005 |
| No | 741 (58.9) | 563 (61.3) | 178 (52.5) | |
| ≥Daily crack cocaine useb | ||||
| Yes | 457 (36.4) | 292 (31.8) | 165 (48.7) | <0.001 |
| No | 800 (63.6) | 626 (68.2) | 174 (51.3) | |
| ≥Daily heroin injectionb | ||||
| Yes | 221 (17.6) | 148 (16.1) | 73 (21.5) | 0.025 |
| No | 1036 (82.4) | 770 (83.9) | 266 (78.5) | |
| ≥Daily cocaine injectionb | ||||
| Yes | 91 (7.2) | 57 (6.2) | 34 (10.0) | 0.020 |
| No | 1166 (92.8) | 861 (93.8) | 305 (90.0) | |
| Heavy alcohol useb | ||||
| Yes | 170 (13.5) | 129 (14.1) | 41 (12.1) | 0.368 |
| No | 1087 (86.5) | 789 (85.9) | 298 (87.9) | |
| Benzodiazepine useb | ||||
| Yes | 16 (1.3) | 13 (1.4) | 3 (0.9) | 0.579d |
| No | 1241 (98.7) | 905 (98.6) | 336 (99.1) | |
| Area restrictionb | ||||
| Yes | 112 (8.9) | 70 (7.6) | 42 (12.4) | 0.007 |
| No | 1100 (87.5) | 817 (89.0) | 283 (83.5) | |
| Any drug or alcohol treatmentb | ||||
| Yes | 705 (56.1) | 510 (55. 6) | 195 (57.5) | 0.511 |
| No | 550 (43.8) | 407 (44.3) | 143 (42.2) | |
| Sex work involvementb | ||||
| Yes | 146 (11.6) | 95 (10.3) | 51 (15.0) | 0.020 |
| No | 1109 (88.2) | 822 (89.5) | 287 (84.7) | |
| Drug dealingb | ||||
| Yes | 323 (25.7) | 207 (22.5) | 116 (34.2) | <0.001 |
| No | 934 (74.3) | 711 (77.5) | 223 (65.8) | |
| Incarcerationb | ||||
| Yes | 173 (13.8) | 117 (12.7) | 56 (16.5) | 0.085 |
| No | 1084 (86.2) | 801 (87.3) | 283 (83.5) | |
aRefers to reporting crystal methamphetamine use in the previous 6 months at least once during follow-up.
bRefers to 6 months prior to an interview.
cWilcoxon Rank-Sum test.
dFisher’s exact test.
As shown in Fig. 1, 80 months after recruitment into the study the Kaplan–Meier cumulative incidence of the first self-reported methamphetamine initiation or relapse was 71.8% among those who reported being evicted at baseline, compared to 32.7% among those who did not (log-rank P < 0.001). Kaplan–Meier curves for other significant covariates are also shown in Appendix 1.
Fig. 1.
Cumulative incidence of first self-reported crystal methamphetamine initiation or relapse, stratified by recent eviction at baseline among 1257 PWID in Vancouver, Canada (2007–15).
Table 2 depicts the unadjusted and adjusted hazard ratios of eviction and other covariates with repeated methamphetamine initiation or relapse. In the multivariable model, after adjusting for various potential confounders, eviction (adjusted hazard ratio [AHR] = 1.90; 95% CI = 1.31, 2.75) was independently and positively associated with higher hazard of methamphetamine initiation or relapse, as were age (per 10 years older; HR = 0.72; 95% CI = 0.62, 0.83), homelessness (AHR = 1.46; 95% CI = 1.12, 1.89), HIV seropositivity (AHR = 1.78; 95% CI = 1.40, 2.25), daily injection heroin use (AHR = 1.57; 95% CI = 1.16, 2.13), daily injection cocaine use (AHR = 1.79; 95% CI = 1.32, 2.41), sex work (AHR = 1.73; 95% CI = 1.26, 2.38) and drug dealing (AHR = 1.71; 95% CI = 1.32, 2.20).
Table 2.
Unadjusted and adjusted hazard ratios for crystal methamphetamine initiation or relapse among people who inject drugs in Vancouver, Canada (2007–15)
| Characteristic | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| Hazard Ratio (95% CI) | P-value | Hazard Ratio (95% CI) | P-value | |
| Eviction* | ||||
| (yes versus no) | 2.79 (1.97–3.95) | <0.001 | 1.90 (1.31–2.76) | 0.001 |
| Age | ||||
| (per 10 years older) | 0.60 (0.53–0.68) | <0.001 | 0.72 (0.62–0.83) | <0.001 |
| Gender | ||||
| (male versus female) | 0.91 (0.71–1.17) | 0.468 | – | – |
| Ethnicity/ancestry | ||||
| (White versus other) | 1.02 (0.80–1.30) | 0.873 | – | – |
| Education | ||||
| (high school or higher versus less than high school) | 0.81 (0.63–1.04) | 0.099 | – | – |
| Sexual orientation | ||||
| (non-heterosexual versus heterosexual) | 1.77 (1.26–2.47) | 0.001 | 1.36 (0.98–1.89) | 0.069 |
| Childhood emotional abuse | ||||
| (yes versus no) | 1.17 (0.91–1.51) | 0.222 | – | – |
| Sexual abuse in lifetime | ||||
| (yes versus no) | 1.19 (0.94–1.51) | 0.154 | – | – |
| In a stable relationship | ||||
| (yes versus no) | 0.93 (0.73–1.20) | 0.587 | – | – |
| Homeless* | ||||
| (yes versus no) | 2.27 (1.81–2.85) | <0.001 | 1.46 (1.13–1.90) | 0.004 |
| Employment* | ||||
| (yes versus no) | 0.67 (0.52–0.87) | 0.002 | 0.92 (0.70–1.20) | 0.529 |
| HIV seropositive* | ||||
| (yes versus no) | 1.67 (1.31–2.12) | <0.001 | 1.79 (1.41–2.27) | <0.001 |
| ≥Daily non-injection crack use* | ||||
| (yes versus no) | 1.54 (1.23–1.93) | <0.001 | 0.80 (0.61–1.04) | 0.101 |
| ≥Daily injection heroin use* | ||||
| (yes versus no) | 2.46 (1.91–3.19) | <0.001 | 1.59 (1.17–2.14) | 0.003 |
| ≥Daily injection cocaine use* | ||||
| (yes versus no) | 2.40 (1.78–3.23) | <0.001 | 1.79 (1.33–2.43) | <0.001 |
| Heavy alcohol use* | ||||
| (yes versus no) | 1.07 (0.79–1.44) | 0.673 | – | – |
| Benzodiazepine use* | ||||
| (yes versus no) | 1.36 (0.74–2.50) | 0.316 | – | – |
| Area restriction* | ||||
| (yes versus no) | 2.12 (1.57–2.87) | <0.001 | 1.39 (0.99–1.95) | 0.057 |
| Any drug or alcohol treatment* | ||||
| (yes versus no) | 1.36 (1.08–1.72) | 0.094 | 1.25 (0.99–1.58) | 0.065 |
| Sex work involvement* | ||||
| (yes versus no) | 2.78 (2.05–3.78) | <0.001 | 1.73 (1.25–2.39) | 0.001 |
| Drug dealing* | ||||
| (yes versus no) | 2.50 (1.99–3.14) | <0.001 | 1.71 (1.32–2.21) | <0.001 |
| Incarceration* | ||||
| (yes versus no) | 2.28 (1.71–3.04) | <0.001 | 1.27 (0.90–1.79) | 0.178 |
*Refers to activities in the past 6 months
Discussion
Main finding of this study
In this community-recruited cohort of 1257 people who inject drugs, more than one in five participants reported one or more evictions over the course of the 8-year study period. After adjusting for a range of potential confounders including homelessness, evictions maintained an independent positive association with an increased hazard of crystal methamphetamine initiation or relapse. In our sample HIV status was also associated with increased likelihood of re-initiation of crystal methamphetamine alongside a set of other risk factors. While this interaction has been noted in past research,4 its persistence is disconcerting as methamphetamine use may enhance viral replication and accelerate HIV disease progression.45 This finding suggests that evictions represent a uniquely consequential moment with regard to initiating methamphetamine use among people who inject drugs. Significantly, this persisted after controlling for the effects of homelessness on initiation, suggesting that evictions play a uniquely consequential role in drug use related risk behavior.
What is already known on this topic?
Contemporary research has characterized a widespread ‘epidemic of evictions’ in cities cross North America.20,46 Evictions are associated with a range of severe health related harms.16–21,23,26 A small but growing literature has documented the unique effects of evictions on the health and well being of people who inject drugs.31,34 This growing body of research characterizes eviction as an important but heretofore under-studied risk factor in the lives of people who inject drugs.
In addition to the already documented harms associated with eviction, people who inject drugs are at elevated risk for a range of drug-use related harms. The association between the ‘binge’ use of methamphetamine type substances and severe physical and mental harms1,9–11 is a prominent example of the unique drug-use related harms that people who inject drugs are vulnerable too. Studies have documented relatively high rates of methamphetamine use among vulnerable people who inject drugs.1–3 Qualitative research has characterized people who use methamphetamine as falling into social and functional sub-groups.47 Functional users were described as initiating methamphetamine use in the context of stressful work environments, such as long haul truckers,48 rural oil and gas workers,49 and air force pilots.50 Given the qualitative description of the material hardship associated with eviction,29 the use of methamphetamine among people who inject drugs as a functional response to eviction seems possible, as individuals are forced to contend with the sequelae of eviction.
What does this study adds?
The association documented in this article between residential evictions and initiation or relapse into methamphetamine use among people who inject drugs suggests that an eviction is a critical transition event associated with a range of methamphetamine-related harms.51 This association may well be explained by the functional or adaptive use of methamphetamine by the recently evicted as they attempt to manage the unique stresses and uncertainties that accompany an eviction.26,29 The widespread use of methamphetamine among people who inject drugs might be an extension of amphetamine-type substances’ long history of use as a tool to, in the words of Murakawa,13 ‘speed up to keep up’ (p. 224). In the context of homelessness, crystal methamphetamine’s stimulating effect may help people who inject drugs navigate the many challenges people facing homelessness face.15 Further, given the social and economic costs associated with eviction,26,29 and given that crystal methamphetamine is considerably less expensive than other commonly used drugs,8 it is possible that crystal methamphetamine use post eviction is related with fewer resources. Understanding the exact mechanisms at work in people who inject drugs’s transition into methamphetamine use is necessary in order to pin point micro and meso level environmental risk factors that can, in turn, be directly targeted with policy and programmatic interventions. While widespread concern about methamphetamine use has contributed to a predominately punitive drug law enforcement-based approach to preventing the sale and use of methamphetamine,13 these findings signal a need to incorporate housing-focused approaches to efforts aimed at reducing stimulant use and drug-related harms. Our findings support broader structural interventions aimed at ensuring the stability of tenancies of people who inject drugs.
Limitations of this study
This study has several limitations. Both VIDUS and ACCESS cohorts consist of non-random samples of people who inject drugs, and therefore our findings may not be generalizable to people who inject drugs locally or in other settings. The data were also self-reported and may be subject to reporting bias. As with all observational research, unmeasured confounders may exist although we sought to reduce this bias through a multivariable model with an extensive covariate adjustment. For example, our data set did not include longitudinal measures of mental health disorders, which may have acted as an unmeasured confounder.
Further research should investigate how best to prevent evictions among drug-using populations, such as better access to legal advocates, housing subsidies and supportive housing programs, including those that provide support immediately following eviction and during housing transitions. In addition, future research should explore the contribution of eviction to the risk of experiencing other forms of drug-related harm. Interventional studies should also be considered, potentially modeled after public health focused eviction prevention strategies at work in other jurisdictions.51
In summary, more than one-fifth of our sample of 1257 people who inject drugs were evicted at least once during the study period, and more than one-fourth initiated or relapsed into crystal methamphetamine use during follow-up. Residential eviction independently predicted methamphetamine initiation/relapse after controlling for a number of potential confounders that might be associated with methamphetamine initiation, even including homelessness. These findings support the exploration of policy and programmatic interventions focused on housing as a means to reduce methamphetamine use.
Supplementary Material
Acknowledgements
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff.
Supplementary data
Supplementary data are available at the Journal of Public Health online.
Funding
The study was supported by the US National Institutes of Health (U01DA038886, R01DA021525) and Vancouver Foundation. This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports Dr Evan Wood (Director, Urban Health Research Initiative, BC Centre for Excellence in HIV/AIDS and Professor, Department of Medicine, University of British Columbia). Dr Kanna Hayashi is supported by a Canadian Institutes of Health Research (CIHR) New Investigator Award (MSH-141971) and a Michael Smith Foundation for Health Research (MSFHR) Scholar Award. Dr M.-J. Milloy is supported in part by the United States National Institutes of Health (R01DA021525), a New Investigator award from the CIHR, and a Scholar Award from the MSFHR. Ryan McNeil is supported by a CIHR New Investigator Award and MSFHR Scholar Award.
References
- 1. Colfax G, Santos G-M, Chu P et al. Amphetamine-group substances and HIV. Lancet 2010;376:458–74. 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- 2. Das-Douglas M, Colfax G, Moss AR et al. Tripling of methamphetamine/amphetamine use among homeless and marginally housed persons, 1996–2003. J Urban Health 2008;85:239–49. 10.1007/s11524-007-9249-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sara G, Burgess P, Harris M et al. Stimulant use disorders: characteristics and comorbidity in an Australian population sample. Aust N Z J Psychiatry 2012;46:1173–81. 10.1177/0004867412461057. [DOI] [PubMed] [Google Scholar]
- 4. Marshall BD, Wood E, Shoveller JA et al. Individual, social, and environmental factors associated with initiating methamphetamine injection: implications for drug use and HIV prevention strategies. Prev Sci 2011;12:173–80. 10.1007/s11121-010-0197-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Degenhardt L, Roxburgh A, Black E et al. The epidemiology of methamphetamine use and harm in Australia. Drug Alcohol Rev 2008;27:243–52. 10.1080/09595230801950572. [DOI] [PubMed] [Google Scholar]
- 6. Stafford J, Breen C, Burns L, 2016. Australian drug trends 2016: findings from the Illicit Drugs Reporting System (IDRS). NDARC Annual Research Symposium. NDARC Annual Research Symposium, Sydney.
- 7. Inglez-Dias A, Hahn JA, Lum PJ et al. Trends in methamphetamine use in young injection drug users in San Francisco from 1998 to 2004: the UFO Study. Drug Alcohol Rev 2008;27:286–91. 10.1080/09595230801914784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Urban Health Research Initiative The Drug Situation in Vancouver (No. 2). Vancouver, B.C: British Columbia Centre for Excellence in HIV/AIDS, 2013. [Google Scholar]
- 9. Cunningham EB, Jacka B, DeBeck K et al. Methamphetamine injecting is associated with phylogenetic clustering of hepatitis C virus infection among street-involved youth in Vancouver, Canada. Drug Alcohol Depend 2015;152:272–6. 10.1016/j.drugalcdep.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Grelotti DJ, Kanayama G, Pope HG. Remission of persistent methamphetamine-induced psychosis after electroconvulsive therapy: presentation of a case and review of the literature. AJP 2010;167:17–23. 10.1176/appi.ajp.2009.08111695. [DOI] [PubMed] [Google Scholar]
- 11. Ho EL, Josephson SA, Lee HS et al. Cerebrovascular complications of methamphetamine abuse. Neurocrit Care 2009;10:295–305. 10.1007/s12028-008-9177-5. [DOI] [PubMed] [Google Scholar]
- 12. Johnson TP, Fendrich M. Homelessness and drug use: evidence from a community sample. Am J Prev Med 2007;32:S211–218. 10.1016/j.amepre.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 13. Murakawa N, 2011. TOOTHLESS: The Methamphetamine ‘Epidemic,’ ‘Meth Mouth,’ and the Racial Construction of Drug Scares [WWW Document] Bois Rev. Soc. Sci. Res. Race. /core/journals/du-bois-review-social-science-research-on-race/article/toothless/C481A540F514BE3E688F8C47826DAB95/core-reader (11 October 2016, date last accessed).
- 14. Rasmussen N. On Speed: The Many Lives of Amphetamine. New York: New York University Press, 2008. [Google Scholar]
- 15. Fast D, Kerr T, Wood E et al. The multiple truths about crystal meth among young people entrenched in an urban drug scene: a longitudinal ethnographic investigation. Soc Sci Med 2014;1982(110):41–8. 10.1016/j.socscimed.2014.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zivanovic R, Milloy M, Hayashi K et al. Impact of unstable housing on all-cause mortality among persons who inject drugs. BMC Public Health 2015;15:106 10.1186/s12889-015-1479-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Padgett DK, Struening EL. Victimization and traumatic injuries among the homeless: associations with alcohol, drug, and mental problems. Am J Orthopsychiatry 1992;62:525–34. [DOI] [PubMed] [Google Scholar]
- 18. Topp L, Iversen J, Baldry E, Maher L, Collaboration of Australian NSPs . Housing instability among people who inject drugs: results from the Australian needle and syringe program survey. J Urban Health Bull N Y Acad Med 2013;90:699–716. 10.1007/s11524-012-9730-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Neale J. Homelessness amongst drug users: a double jeopardy explored. Int J Drug Policy 2001;12:353–69. 10.1016/S0955-3959(01)00097-4. [DOI] [Google Scholar]
- 20. Desmond M, Gershenson C. Who gets evicted? Assessing individual, neighborhood, and network factors. Soc Sci Res 2016;62:362–77. 10.1016/j.ssresearch.2016.08.017. [DOI] [PubMed] [Google Scholar]
- 21. Rojas Y, Stenberg S-Å. Evictions and suicide: a follow-up study of almost 22 000 Swedish households in the wake of the global financial crisis. J Epidemiol Commun Health 2015;70(4):409–13. 10.1136/jech-2015-206419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Burt MR. Homeless families, singles, and others: findings from the 1996 national survey of homeless assistance providers and clients. Hous Policy Debate 2001;12:737–80. 10.1080/10511482.2001.9521428. [DOI] [Google Scholar]
- 23. Crane M, Warnes AM. Evictions and prolonged homelessness. Hous Stud 2000;15:757–73. 10.1080/02673030050134592. [DOI] [Google Scholar]
- 24. Desmond M, Shollenberger T. Forced displacement from rental housing: prevalence and neighborhood consequences. Demography 2015;52:1751–72. 10.1007/s13524-015-0419-9. [DOI] [PubMed] [Google Scholar]
- 25. Desmond M. Eviction and the reproduction of urban poverty. Am J Sociol 2012;118:88–133. 10.1086/666082. [DOI] [Google Scholar]
- 26. Desmond M, Kimbro RT. Eviction’s fallout: housing, hardship, and health. Soc Forces 2015;94(1):295–324. 10.1093/sf/sov044. [DOI] [Google Scholar]
- 27. Qvarfordt Eisenstein C, 2016. Depression in the aftermath of eviction: a one-year follow-up study of a disruptive housing life event. Master’s Thesis Available online at: http://www.diva-portal.org/smash/record.jsf?pid=diva2%3A940068&dswid=mainwindow
- 28. Dickson-Gomez J, Convey M, Hilario H, Corbett AM, Weeks M. Structural and personal factors related to access to housing and housing stability among urban drug users in Hartford, Connecticut. Contemp Drug Probl 2008;35:115–52. [Google Scholar]
- 29. Desmond M. Evicted: Poverty and Profit in the American City. New York: Crown/Archetype, 2016. [Google Scholar]
- 30. Fowler KA, Gladden RM, Vagi KJ, Barnes J, Frazier L. Increase in suicides associated with home eviction and foreclosure during the US housing crisis: findings from 16 national violent death reporting system states, 2005–2010. Am J Public Health 2015;105:311–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kennedy MC, McNeil R, Milloy MJ, Dong H, Kerr T, Hayashi K. Residential eviction and exposure to violence among people who inject drugs in Vancouver, Canada. Int J Drug Policy 2017;41:59–64. https://www.researchgate.net/publication/312587665_Residential_eviction_and_exposure_to_violence_among_people_who_inject_drugs_in_Vancouver_Canada. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Osypuk TL, Caldwell CH, Platt RW, Misra DP. The consequences of foreclosure for depressive symptomatology. Ann Epidemiol 2012;22:379–87. 10.1016/j.annepidem.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Manzo LC, Kleit RG, Couch D. ‘Moving three times is like having your house on fire once’: the experience of place and impending displacement among public housing residents. Urban Stud 2008;45:1855–78. 10.1177/0042098008093381. [DOI] [Google Scholar]
- 34. Kennedy MC, Kerr T, McNeil R, Parashar S, Montaner J, Wood E, Milloy M-J. Residential eviction and risk of detectable plasma HIV-1 RNA viral load among HIV-positive people who use drugs. AIDS Behav 2016;21:678–87. 10.1007/s10461-016-1315-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Strathdee SA, Patrick DM, Currie SL, Cornelisse PG, Rekart ML, Montaner JS, Schechter MT, O’Shaughnessy MV. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS 1997;11(8):F59–65. [DOI] [PubMed] [Google Scholar]
- 36. Tyndall MW, Currie S, Spittal P, Li K, Wood E, O’Shaughnessy MV, Schechter MT. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. [Miscellaneous Article]. AIDS 2003;17:887–93. [DOI] [PubMed] [Google Scholar]
- 37. Milloy M-J, Kerr T, Buxton J, Montaner J, Wood E. Methamphetamine use and rates of incarceration among street-involved youth in a Canadian setting: a cross-sectional analysis. Subst Abuse Treat Prev Policy 2009;4:17 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Werb D, Kerr T, Buxton J, Shoveller J, Richardson C, Montaner J, Wood E. Crystal methamphetamine and initiation of injection drug use among street-involved youth in a Canadian setting. Can Med Assoc J 2013;185:1569–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wood E, Stoltz J-A, Zhang R, Strathdee SA, Montaner JSG, Kerr T. Circumstances of first crystal methamphetamine use and initiation of injection drug use among high-risk youth. Drug Alcohol Rev 2008;27:270–6. 10.1080/09595230801914750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–81. 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 41. Lin DY, Wei LJ, Yang I, Ying Z. Semiparametric regression for the mean and rate functions of recurrent events. J R Stat Soc Ser B Stat Methodol 2000;62:711–30. 10.1111/1467-9868.00259. [DOI] [Google Scholar]
- 42. Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994;81:515–26. 10.1093/biomet/81.3.515. [DOI] [Google Scholar]
- 43. Hess KR. Assessing time-by-covariate interactions in proportional hazards regression models using cubic spline functions. Stat Med 1994;13:1045–62. 10.1002/sim.4780131007. [DOI] [PubMed] [Google Scholar]
- 44. Guilford J. Psychometric Methods. New York: McGraw–Hill Book Company, Inc, 1936. [Google Scholar]
- 45. R Core Team R: A Language and Environment for Statistial Computing. Vienna, Austria: R Foundation for Statistical Computing, 2016. [Google Scholar]
- 46. Raymond E, Duckworth R, Miller B, Lucas M, Pokharel S. 2016. Corporate Landlords, Institutional Investors, and Displacement: Eviction Rates in Single Family Rentals. Federal Reserve Bank of Atlanta, Community and Economic Development Discussion Paper 04–16 https://www.frbatlanta.org/-/media/documents/community-development/publications/discussion-papers/2016/04-corporate-landlords-institutional-investors-and-displacement-2016-12-21.pdf
- 47. Blue Moon Research and Planning , 2008. Patterns of use and harms associated with specific populations of methamphetamine users in Australia: exploratory research. Prepared for Department of Health and Ageing—Market Research Unit.
- 48. Malta M, Bastos FI, Pereira-Koller EM, Cunha MD, Marques C, Strathdee SA. A qualitative assessment of long distance truck drivers’ vulnerability to HIV/AIDS in Itajai, southern Brazil. AIDS Care 2006;18:489–96. 10.1080/09540120500235241. [DOI] [PubMed] [Google Scholar]
- 49. Bowen A, Moring J, Williams M, Hopper G, Daniel C. An investigation of bioecological influences associated with first use of methamphetamine in a rural state. J Rural Health 2012;28:286–95. 10.1111/j.1748-0361.2011.00391.x. [DOI] [PubMed] [Google Scholar]
- 50. Emonson DL, Vanderbeek RD. The use of amphetamines in U.S. Air Force tactical operations during Desert Shield and Storm. Aviat Space Environ Med 1995;66:260. [PubMed] [Google Scholar]
- 51. Panenka WJ, Procyshyn RM, Lecomte T, MacEwan GW, Flynn SW, Honer WG, Barr AM. Methamphetamine use: a comprehensive review of molecular, preclinical and clinical findings. Drug Alcohol Depend 2013;129:167–79. 10.1016/j.drugalcdep.2012.11.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.