Abstract
Annual increases in global travel have resulted in more individuals being exposed to varying environmental conditions abroad and, thereby, subject to air pollution related health risks. Individuals who travel abroad may be exposed to varying levels of air pollution within a matter of hours. We wish to consider whether exposure to air pollution could be a significant contributor to the risk of illness and death in travelers, particularly those who travel to highly polluted cities. We report the findings of a study in which the peak expiratory flow (PEF) of a traveler decreased in Shanghai relative to baseline in New York City; the decline in PEF correlated to concentration of particulate matter (PM2.5). We discuss the health implication of these results on global travel.
Keywords: Air pollution, travel abroad, exposure and health effects
Introduction
The adverse health effects of acute and long-term exposure to ambient air pollution are well known and include elevated risks for asthma, chronic obstructive pulmonary disease, cardiovascular disease and lung cancer. Several large epidemiological cohort studies have shown higher rates of relative risk for cardiovascular and respiratory health effects.1–3 Of the various air pollutants, particulate matter (PM), mainly fine PM (PM2.5), is the pollutant most strongly associated with adverse respiratory and cardiac impacts. Long-term PM exposures are most strongly associated with mortality attributable to ischemic heart disease, dysrhythmias, heart failure, and cardiac arrest.4 Each 10-μg/m3 increase in PM2.5, for example, has been associated with approximately a 4, 6 and 8% increased risk of all-cause, cardiopulmonary and lung cancer mortality, respectively.2 Outdoor ambient PM is one of the leading causes of global health burden and is associated with 3.2 million deaths and 76 million disability-adjusted-life-years lost per year.5, 6 However, almost all of such epidemiological studies have modeled study populations within a selected city, country or geographic area, which gives rise to the question whether the impacts are the same for travelers, who may be exposed to varying pollution levels within a matter of hours.
According to the World Health Organization’s (WHO) urban air quality databases, air pollution levels are rising in many of the world’s largest cities. The highest pollution levels have been recorded in low- and middle-income countries in WHO’s Eastern Mediterranean and South-East Asia Regions (annual mean levels often exceeding 5–10 times WHO guidelines), followed by low-income cities in the Western Pacific Region.7 Megacities in Asia such as New Delhi, Mumbai, Dhaka, Shanghai and Beijing rank amongst the most polluted cities, in terms of annual mean airborne PM concentrations.7 Travelers to these destinations may, therefore, be at increased risk from exposure to high levels of ambient air pollution, especially during certain seasons and weather conditions that result in major pollution episodes, as seen in New Delhi in late 2016 and 2017.
Myocardial infarctions (MIs) and cerebrovascular accidents (CVAs) are among the most common causes of deaths of international travelers. Some studies indicate that approximately half of all deaths of travelers is due to one of these two causes.8 Might some portion of travelers’ deaths due to MI, CVA and other cerebrovascular issues be attributable to air pollution? PM2.5 is linked to increased QT interval duration, a marker of ventricular repolarization and a risk factor for cardiac arrhythmia and sudden death.9 PM2.5 is also linked to ischemic heart disease and risk of pulmonary embolism (PE).10 Thus, a potential link between PM exposure and acute cardiovascular events could be an important health concern for susceptible travelers.
Case Report
Previous anecdotal comments from students and staff who traveled to Beijing and Shanghai, China showed that they experienced various respiratory symptoms during the days of elevated air pollution during their stay. To investigate this relationship of air pollution exposure and health impacts during travel, our laboratory launched a pilot study where we measured lung function and PM2.5 exposure levels in a healthy, non-smoking subject. This case report presents data from a female subject, 31 years old, who did not have respiratory illnesses and did not take any medication prior to or during travel. The subject traveled from NYC to Shanghai and was pre-trained in NYC to measure lung function—Peak Expiratory Flow (PEF) and Forced Expiratory Volume (FEV1) (Koko Pro 6, Ferraris Medical). PM2.5 concentrations were obtained from the central air pollution monitoring stations in Manhattan (US EPA) and at the US embassy in Shanghai. Daily pulmonary function measurements were recorded in the evening for 1 week in NYC before travel and during the 2 weeks abroad. The subject also recorded daily respiratory symptoms.
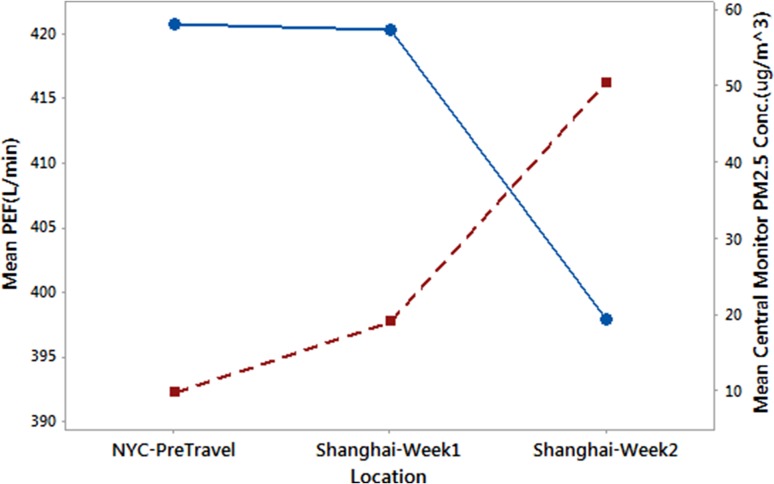
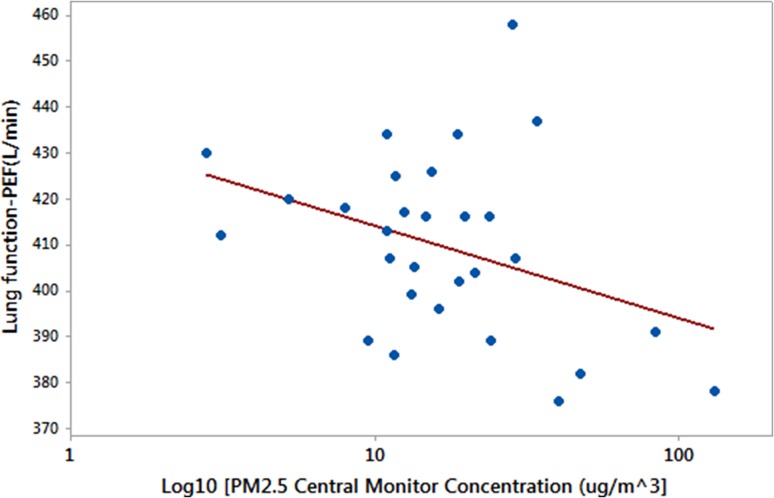
Compared with the pre-travel week in NYC, the mean PEF decreased by ~20 L/min when the average ambient PM2.5 levels increased during the last week of stay in Shanghai (Figure 1). This decrease was not seen during the first travel week when PM levels in Shanghai were similar to the pre-travel NYC levels. The average PM level in Shanghai during the last week of travel (50.4 ± 38.5 μg/m3; mean ± SD) was higher than the first travel week (19.0 ± 8.6 μg/m3), and in particular, 2 days within the highly polluted week had PM levels of 130 μg/m3. Lung function changes were negatively correlated with the ambient PM2.5 concentrations (Figure 2). The observed decrement in PEF was accompanied by an increase in respiratory symptoms, which included throat irritation, cough with phlegm, nasal irritation and congestion, and rhinorrhea, and a small but not statistically significant reduction in FEV1.
Figure 1.
The change in evening mean PEF in the study participant and mean ambient PM2.5 concentrations (obtained from respective central monitors), during the week-long baseline period in New York City and the 2-week travel abroad period in Shanghai, China
Figure 2.
Mean PEF vs. mean ambient PM2.5 concentration (μg/m3) recorded in the evening for the participant shown in Figure 1. Data include pre-travel NYC and Shanghai values
Discussion
This case presents an initial perspective of how short-term exposure to PM pollution, when traveling abroad, can impact pulmonary health. The subject did not report having a cold, wheeze or any respiratory illness during the stay in Shanghai. Therefore, we suggest that the lung function reduction and reported respiratory symptoms were due to the higher air pollution levels encountered during the second travel week in Shanghai. We are continuing to examine this phenomenon in more participants who travel to urban centers with higher air pollution, to varying degrees, than their resident city. We propose to supplement these pulmonary function data with blood pressure and heart rate. While studying the short-term acute impacts of air pollution on travelers is important, it is also impactful to examine whether this effect persists during a longer stay in high pollution urban centers. It is possible that long-term travelers may adapt to such conditions, as residents of those cities may have to a certain degree. Longer stays, of course, might also involve changes in living conditions, behavior and activities, thus altering the time a traveler spends indoors vs. outdoors.
Little to no research has investigated the potential health effects of traveling to a polluted travel destination, relative to the home site. Although not international travel, a study in China has demonstrated that lung function and blood pressure are changed in a study population that moved from a cleaner suburban area of Beijing to a more polluted urban area, and that specific components of PM were associated with these effects.11 Moreover, data from the Geosentinel study of travelers to China has shown that respiratory illnesses were the most common illness among travelers who visited China during the study period.12
Deaths in international travelers are relatively rare. Of every 100 000 people who visit a low-income country for a month, approximately one will die.13 Hence, a study that investigates whether travelers are more likely to die in polluted foreign cities, compared with foreign cities with relatively unpolluted air, would require a very large number of subjects. Thus, it is unclear the extent of contribution that air pollution makes to deaths in travelers to polluted destinations. One study found that cardiovascular causes account for 70% of the deaths of travelers to the USA, which has relatively low levels of ambient air pollution.14 This suggests that high air pollution levels are not prerequisite for cardiovascular causes to comprise the most common cause of deaths of travelers. However, data from the 2008 Beijing Olympics and the Chinese travel study show that acute changes in ambient air pollution are associated with adverse cardiopulmonary effects.11
There are statistical and logistical obstacles to demonstrating an elevated risk of adverse pulmonary or cardiac health effects, including sudden death, in international travelers to polluted cities. However, given the demonstrated association between elevated levels of pollutants (PM and ozone) and alterations in cardiopulmonary health shown in large time series studies, the link between air pollution and adverse health effects in international travelers is biologically plausible. If this issue is shown to be significant in further study, it may be reasonable for pre-travel clinicians to advise travelers with cardiovascular risk factors to minimize their duration of stay in urban areas with significant air pollution.
Funding
This pilot study was supported by the New York University – National Institute of Environmental Health Sciences (NIEHS) Core Center (ES000260) grant and the New York University College of Global Public Health grant.
Conflict of interest
The authors have declared no conflicts of interest.
References
- 1. American Thoracic Society (ATS) What constitutes an adverse health effect of air pollution? Am J Respir Crit Care Med 2000; 161: 665–73. [DOI] [PubMed] [Google Scholar]
- 2. Pope CA 3rd, Burnett RT, Thun MJ et al. . Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. J Am Med Assoc 2002; 287: 1132–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization Regional Office for Europe. Air Quality Guidelines Global Update 2005: Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide. Copenhagen: WHO Regional Office for Europe, 2006. [Google Scholar]
- 4. Pope CA 3rd, Burnett RT, Thurston GD et al. . Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004; 109: 71–7. [DOI] [PubMed] [Google Scholar]
- 5. Lim SS, Vos T, Flaxman AD et al. . A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thurston G, Lippmann M. Ambient particulate matter air pollution and cardiopulmonary diseases. Semin Respir Crit Care Med 2015; 36: 422–32. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organization (WHO) WHO Urban Ambient Air Pollution Database – Update 2016, version 0.2. http://www.who.int/phe/en/. [Google Scholar]
- 8. Hargarten SW, Baker TD, Guptill K. Overseas fatalities of United States citizen travelers: an analysis of deaths related to international travel. Ann Emerg Med 1991; 20: 622–6. [DOI] [PubMed] [Google Scholar]
- 9. Mordukhovich I, Kloog I, Coull B, Koutrakis P, Vokonas P, Schwartz J. Association between particulate air pollution and QT interval duration in an elderly cohort. Epidemiology 2016; 27: 284–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pun VC, Hart JE, Kabrhel C, Camargo CA Jr., Baccarelli AA, Laden F. Prospective study of ambient particulate matter exposure and risk of pulmonary embolism in the nurses’ health study cohort. Environ Health Perspect 2015; 123: 1265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wu S, Deng F, Wei H et al. . Association of cardiopulmonary health effects with source-appointed ambient fine particulate in Beijing, China: a combined analysis from the Healthy Volunteer Natural Relocation (HVNR) study. Environ Sci Technol 2014; 48: 3438–48. [DOI] [PubMed] [Google Scholar]
- 12. Davis XM, MacDonald S, Borwein S et al. . Health risks in travelers to China: the GeoSentinel experience and implications for the 2008 Beijing Olympics. Am J Trop Med Hyg 2008; 79: 4–8. [PubMed] [Google Scholar]
- 13. Steffen R, Amitirigala I, Mutsch M. Health risks among travelers—need for regular updates. J Travel Med 2008; 15: 145–6. [DOI] [PubMed] [Google Scholar]
- 14. Lawson CJ, Dykewicz CA, Molinari NA, Lipman H, Alvarado-Ramy F. Deaths in international travelers arriving in the United States, July 1, 2005 to June 30, 2008. J Travel Med 2012; 19: 96–103. [DOI] [PubMed] [Google Scholar]