ABSTRACT
Despite the paucity of evidence, it is often presumed, and is physiologically plausible, that sudden, acute elevations in blood pressure may transiently increase the risk of recurrent aortic dissection (AD) or rupture in patients with a prior AD, because a post‐dissection aorta is almost invariably dilated and may thus experience greater associated wall stress as compared with a nondilated aorta. Few data are available regarding the specific types and intensities of exercise that may be both safe and beneficial for this escalating patient population. The purpose of this editorial/commentary is to further explore this conundrum for clinicians caring for and counseling AD survivors. Moderate‐intensity cardiovascular activity may be cardioprotective in this patient cohort. It is likely that severe physical activity restrictions may reduce functional capacity and quality of life in post‐AD patients and thus be harmful, underscoring the importance of further exploring the role of physical activity and/or structured exercise in this at‐risk patient population.
Introduction
Aortic dissection (AD) is due to disruption of the aortic‐wall integrity and architecture, most often related to underlying genetic disorders (eg, Marfan syndrome), abnormal shear stress, inflammatory disease, trauma, or combinations thereof. It is a life‐threatening medical emergency that, with immediate intervention, is now associated with improved rates of survival.1 Currently, there is an ∼ 90% survival rate to hospital discharge for patients with type B AD. The 1‐ and 3‐year survival rates in patients with type A acute AD treated surgically approximate 96% ± 2% and 91% ± 4%, respectively.1 Whereas progressive acute management (ie, inclusive of use of medical therapies, open surgical, or endovascular approaches) has contributed to the improved survival, this patient subset maintains a heightened risk of aortopathy and associated cardiovascular events that may be favorably or unfavorably modulated by regular exposure to exercise.
Some case reports have described acute aortic syndromes that were identified after unusual or unaccustomed vigorous physical exertion, such as strenuous weightlifting or lifting heavy objects, suggesting that the trigger for the acute aortic syndrome was a transient excessive rise in blood pressure (BP).2, 3, 4, 5, 6 Despite the paucity of evidence, it is often presumed, and is physiologically plausible, that sudden, acute elevations in BP may transiently increase the risk of recurrent AD or rupture in patients with a prior AD, because a post‐dissection aorta is almost invariably dilated and may thus experience greater associated wall stress as compared with a nondilated aorta.7 Consequently, it seems reasonable for post‐AD patients to minimize physical activities that evoke a transient, disproportionate increase in BP to decrease the risk for future aortic dilatation, dissection, and/or rupture.7
On the other hand, because physical conditioning lowers the heart rate (HR) and systolic blood pressure (SBP) response at rest and at any given level of exercise, it is feasible that structured exercise programs might lower lifelong recurrent aortic risk during exertion‐related and non–exertion‐related (eg, emotional) stresses. Because β‐blockers are associated with improved survival in both type A and type B acute AD, most likely due to their HR‐ and SBP‐lowering effects, it is plausible that regular exercise may also serve as a cardioprotective intervention for the AD patient, improving clinical outcomes by attenuating hemodynamic responses at rest and during any given level of exercise.8 Furthermore, exercise, in contrast to medications, may also have the added benefits of improving quality of life, mental health, and functional capacity, making it a complementary intervention to the pharmacotherapeutic armamentarium of the AD patient.
Despite the potential benefits of exercise in the AD population, few data are available regarding the specific types and intensities of exercise that may be both safe and beneficial for this escalating patient population. The purpose of this editorial/commentary is to further explore this conundrum for clinicians caring for and counseling AD survivors.
Clinician's Perspective
Several years ago, we surveyed cardiovascular specialists (n = 26) who participate in the International Registry of Aortic Dissection (IRAD) regarding physical‐activity recommendations for this patient cohort. For aerobic activities, 63% recommended moderate exercise, 26% recommended low‐impact exercise, and 10% had no restrictions. Many aortic disease specialists advised against weightlifting or resistance training (92%), competitive sports (46%), isometric exercise (46%), and participation in contact sports (54%). A majority (65%) reported that their recommendations were independent of the initial treatment intervention. Although most (58%) asked their patients to monitor SBP and HR during exercise, when asked to define safe upper limits for these hemodynamic responses during exercise, there was considerable variability in cutpoints among the IRAD clinician‐investigators. These survey results further highlight the current ambiguity regarding structured exercise/physical activity recommendations for post‐AD patients.
Post–Aortic Dissection Patient Practices
More recently, we sent a lifestyle survey to 82 AD survivors. Most respondents reported that they engaged in leisure‐time walking before and after AD, 49 (60%) and 47 patients (57%), respectively. However, the number of survivors who engaged in no structured physical activity increased from 14 patients (17%) before AD to 20 patients (24%) after AD, with many citing fear as the limiting factor. Furthermore, prior to AD, 31 patients (38%) engaged in sexual activity, whereas after AD, only 9 patients (11%) reported sexual activity, once again due to the perceived cardiac demands and the potential for recurrent cardiovascular events.
Physical Activity and Exercise
Hatzaras et al4 reviewed 65 patients (24 women, 41 men) with an average aortic diameter of 5.6 cm prior to AD, detailing specific triggers for the events. Of these patients, 27% and 40% reported strenuous physical activity and severe emotional stress, respectively, immediately prior to dissection. In another series by Hatzaras et al,3 31 patients (30 men, 1 woman; mean age, 47.3 years) were identified (mean aortic diameter of 4.6 cm on initial imaging) who were engaged in weight training or heavy lifting at dissection onset. Despite these case series, the relationship between a triggering exercise exposure and acute AD is often not known, as selective patient recall (patients who do not suffer AD after vigorous exercise will not be reported) and publication bias (authors would have little incentive to report a series of “safe exercise encounters with no adverse outcomes” and editors would likely consider this a low priority) render calculations of the true relative or absolute risk tenuous at best.
Most, but not all, patients with Marfan syndrome have aortic root dilatation. High‐intensity dynamic and isometric exertion, as well as contact sports, are contraindicated for this vulnerable patient subset (the Marfan Foundation physical activity recommendations are listed in Table 1).8 However, these exercise and physical‐activity restrictions are largely based on opinion and empiric experience, rather than scientific/clinical evidence. Although the listed prescriptions and proscriptions seem reasonable, the limited knowledge base substantiating these recommendations served as the rationale for this editorial.
Table 1.
The Marfan Foundation Physical Activity Recommendations
| Noncompetitive, isokinetic activity performed at a nonstrenuous aerobic pace, minimizing sudden stops, rapid changes in direction, or contact with other players, equipment, or the ground. |
|---|
| Performing aerobic activity at a moderate intensity (∼50% of aerobic capacity) and maintaining heart rate <100 bpm or <110 bpm for patients on and off β‐blockers, respectively. |
| Avoiding exercise involving a substantial isometric component, such as weightlifting, climbing steep inclines, gymnastics, and pull‐ups. |
| Avoiding activities that are associated with rapid changes in atmospheric pressure (scuba diving, flying in unpressurized aircraft). |
| For resistance training, higher repetitions at lower weights are recommended as opposed to lower repetitions with heavier weight, stopping before muscle fatigue. |
Abbreviations: bpm, beats per minute.
To our knowledge, only 1 study to date has evaluated the safety and efficacy of exercise‐based cardiac rehabilitation in post‐AD patients. Corone et al9 reported on 33 French patients (25 men, 8 women) with type 1 DeBakey AD (mean age, 55.1 years) who underwent cardiac rehabilitation soon after surgical repair (mean, 27 days). Average resting SBP at hospital discharge was 120 mm Hg; most of the patients (97%) were taking β‐blockers. Patients with poorly controlled SBP at rest were excluded. The intervention group was followed up at 6 and 12 months. During cardiac rehabilitation, exercise training was performed on a cycle ergometer, using a moderate intensity (11.3 or “fairly light” on the Borg 6 to 20 scale). Systolic BP during exercise remained <150 mm Hg in 25% of the patients, was between 150 and 160 mm Hg in half of the patients, and averaged 160 to 170 mm Hg in the remaining patients. The mean baseline maximum physical work capacity increased from 62.7 W/min to 91.6 W/min at the conclusion of the intervention (P = 0.002). Follow‐up was for 1 year and in total there were 3 complications, including 2 patients that required additional thoracic aortic surgery. These data suggest that moderate intensity, noncontact aerobic activity is likely safe and effective for selected post‐AD patients. Accordingly, moderate‐intensity exercise training is currently used in post‐AD patients referred to cardiac rehabilitation centers in France.
Activity Recommendations
Few data are available regarding exercise tolerance and physical‐activity recommendations for patients who have survived an AD. Most of the limited number of available reports pertain to patients with a history of thoracic aortic aneurysm prior to dissection. Unaccustomed vigorous physical activity, acute emotional stress, and heavy lifting have been suggested as triggers for AD in patients with preexisting aortic aneurysm.3, 4 According to the Law of LaPlace, the aortic wall experiences greater stress at a given SBP as aortic size increases. In contrast, even near‐maximal to maximal levels of physical exertion do not appear to result in dangerous elevations of wall stress in normal, nondilated aortas.10 Thus, for patients with known aortic dilatation or underlying aortopathy, high‐intensity aerobic and isometric activity is most likely contraindicated.
Regular aerobic exercise lowers resting SBP over time, on average, by a modest amount (3–8 mm Hg), with moderate‐intensity exertion being more effective than high‐intensity training.11 Moreover, a lower resting SBP is associated with a reduced risk of future aortic complications.12, 13, 14, 15, 16 Dynamic aerobic activity is typically categorized by intensity level, using the relative HR response, estimated metabolic equivalents (METs; 1 MET = 3.5 mL O2/kg/min), and the percent of maximal voluntary contraction (MVC) for young, middle‐aged, and older adults (Table 2).17 The general public‐health recommendation is to engage in moderate‐intensity aerobic activity (3–5 METs) for ≥30 minutes on most days of the week, for a minimum of 150 minutes per week.17 This suggests that high‐intensity exercise is not necessary to provide the hemodynamic benefits of exercise. Thus, for many post‐AD patients, age‐adjusted light to moderate dynamic exercise, such as comfortable to brisk walking and/or cycling at a perceived exertion of “fairly light” to “somewhat hard,” should be reasonably safe and well‐tolerated. A light to moderate weight‐training program limiting the amount of weight utilized per set, and stopping well short of volitional fatigue and Valsalva, has been suggested as potentially beneficial in selected patients and should be encouraged.17 Sexual activity, which approximates an aerobic requirement of 2 to 3 METs, is most likely safe and should not be discouraged in this patient cohort.18
Table 2.
Exercise Intensity, METs, and MVC Based on Agea
| Intensity | Maximal Heart Rate, % | METs in Healthy Adults (Age 28–39) | METs in Healthy Adults (Age 40–64) | METs in Healthy Adults (Age 65–79) | MVC, % |
|---|---|---|---|---|---|
| Very light | <35 | <2.4 | <2.0 | <1.6 | <30 |
| Light | 35–54 | 2.4–4.7 | 2.0–3.9 | 1.6–3.1 | 30–49 |
| Moderate | 55–69 | 4.8–7.1 | 4.0–5.9 | 3.2–4.7 | 50–69 |
| Hard | 70–89 | 7.2–10.1 | 6.0–8.4 | 4.8–6.7 | 70–84 |
| Very hard | ≥90 | ≥10.2 | ≥8.5 | ≥6.8 | ≥85 |
| Maximal | 100 | 12.0 | 10.0 | 8.0 | 100 |
Abbreviations: METs, metabolic equivalents; MVC, maximal voluntary contraction.
Adapted from the American College of Sports Medicine Position Stand.17
Role of Antihypertensive Agents
β‐Blockers, calcium channel blockers, angiotensin‐converting enzyme inhibitors, and angiotensin receptor blockers are commonly prescribed to lower SBP in patients with AD. β‐Blockers, by reducing HR, myocardial contractility, and abrupt increases in ventricular pressure (dP/dt), are particularly therapeutic post‐dissection.1 Patients taking antihypertensive medications may safely tolerate greater intensities of exertion as a lower resting SBP leads to attenuated average and peak SBPs during physical activity as compared with uncontrolled hypertensive individuals. β‐Blockers also limit the magnitude of SBP increase during activity, suggesting greater efficacy in attenuating the exertion‐related SBP rise as compared with other antihypertensives.19, 20, 21, 22, 23, 24, 25, 26, 27, 28 This suggests that the same activity restrictions do not apply to patients taking BP medications compared with those not taking BP medications, and that post‐AD patients with uncontrolled hypertension should markedly limit their physical exertion. However, varied SBP responses to progressive levels of physical activity may occur in any given patient, depending on superimposed environmental, circadian, and emotional stressors.
Conclusion
Although there are few data regarding safe exercise practices in AD survivors, numerous studies now suggest that usual gait speed, distance covered during walk performance tests, and weekly walking distance/time are powerful predictors of mortality and future cardiovascular events in patients with and without heart disease, including those with heart failure.29, 30 Potential triggers of AD and cardioprotective interventions are shown in the Figure 1. It appears that varied exercise doses can both protect against and provoke acute cardiac events, including AD, especially when the exertion is unaccustomed.
Figure 1.
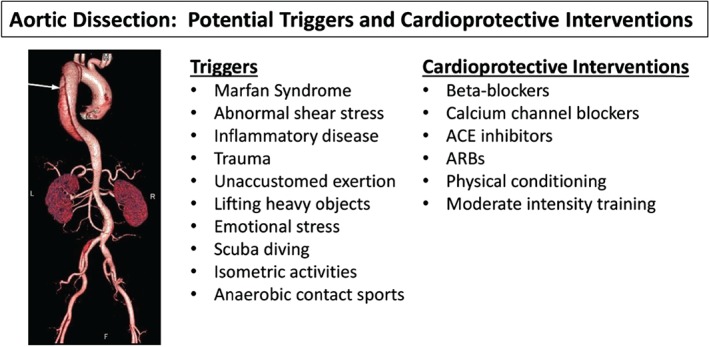
Potential triggers and cardioprotective interventions for acute AD. Abbreviations: ACE, angiotensin‐converting enzyme; AD, aortic dissection; ARB, angiotensin II receptor blocker.
The post‐AD patient's functional capacity and habitual physical activity should be regularly assessed. Exercise testing may be performed to identify adverse exertional signs/symptoms (eg, chest pain, dyspnea, threatening ventricular arrhythmias, hypo‐hypertension) and perceived exertion and chronotropic responses at progressive MET levels. These data should be used to develop a safe and effective exercise prescription and to adjust antihypertensive medication dosages to permit a higher exercise intensity to be achieved with reduced cardiac demands (eg, rate‐pressure‐product). Moreover, the exercise prescription should be reevaluated on a serial basis. A trained physiologist, exercise therapist, or nurse clinician should be available for counseling and supervision, at least during the initial training sessions, and ideally thereafter. In summary, it is likely that severe physical activity restrictions may reduce functional capacity and quality of life in post‐AD patients and thus be harmful, underscoring the importance of further exploring the role of physical activity and/or structured exercise in this at‐risk patient population.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Tsai TT, Evangelista A, Nienaber CA, et al; International Registry of Acute Aortic Dissection (IRAD). Long‐term survival in patients presenting with type a acute aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006;114(1 suppl):I350–I356. [DOI] [PubMed] [Google Scholar]
- 2. de Virgilio C, Nelson RJ, Milliken J, et al. Ascending aortic dissection in weight lifters with cystic medial degeneration. Ann Thorac Surg. 1990;49:638–642. [DOI] [PubMed] [Google Scholar]
- 3. Hatzaras I, Tranquilli M, Coady M, et al. Weight lifting and aortic dissection: more evidence for a connection. Cardiology. 2007;107:103–106. [DOI] [PubMed] [Google Scholar]
- 4. Hatzaras IS, Bible JE, Koullias GJ, et al. Role of exertion or emotion as inciting events for acute aortic dissection. Am J Cardiol. 2007;100:1470–1472. [DOI] [PubMed] [Google Scholar]
- 5. Ragucci MV, Thistle HG. Weight lifting and type II aortic dissection: a case report. J Sports Med Phys Fitness. 2004;44:424–427. [PubMed] [Google Scholar]
- 6. Schor JS, Horowitz MD, Livingstone AS. Recreational weight lifting and aortic dissection: case report. J Vasc Surg. 1993;17:774–776. [DOI] [PubMed] [Google Scholar]
- 7. Koullias G, Modak R, Tranquilli M, et al. Mechanical deterioration underlies malignant behavior of aneurysmal human ascending aorta. J Thorac Cardiovasc Surg. 2005;130:677–683. [DOI] [PubMed] [Google Scholar]
- 8. Braverman AC. Exercise and the Marfan syndrome. Med Sci Sports Exerc. 1998;30(10 suppl):S387–S395. [DOI] [PubMed] [Google Scholar]
- 9. Corone S, Iliou MC, Pierre B, et al; Cardiac Rehabilitation Working Group of the French Society of Cardiology. French registry of cases of type I acute aortic dissection admitted to a cardiac rehabilitation center after surgery. Eur J Cardiovasc Prev Rehabil. 2009;16:91–95. [DOI] [PubMed] [Google Scholar]
- 10. Mayerick C, Carré F, Elefteriades J. Aortic dissection and sport: physiologic and clinical understanding provide an opportunity to save young lives. J Cardiovasc Surg (Torino). 2010;51:669–681. [PubMed] [Google Scholar]
- 11. Brook RD, Appel LJ, Rubenfire M, et al; American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61:1360–1383. [DOI] [PubMed] [Google Scholar]
- 12. Albrecht F, Eckstein F, Matt P. Is close radiographic and clinical control after repair of acute type A aortic dissection really necessary for improved long‐term survival? Interact Cardiovasc Thorac Surgery. 2010;11:620–625. [DOI] [PubMed] [Google Scholar]
- 13. Melby SJ, Zierer A, Damiano RJ Jr, et al. Importance of blood pressure control after repair of acute type A aortic dissection: 25‐year follow‐up in 252 patients. J Clin Hypertens (Greenwich). 2013;15:63–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zierer A, Voeller RK, Hill KE, et al. Aortic enlargement and late reoperation after repair of acute type A aortic dissection. Ann Thorac Surg. 2007;84:479–487. [DOI] [PubMed] [Google Scholar]
- 15. Palmieri V, Bella JN, Arnett DK, et al. Aortic root dilatation at sinuses of Valsalva and aortic regurgitation in hypertensive and normotensive subjects: the Hypertension Genetic Epidemiology Network Study. Hypertension. 2001;37:1229–1235. [DOI] [PubMed] [Google Scholar]
- 16. Onitsuka S, Akashi H, Tayama K, et al. Long‐term outcome and prognostic predictors of medically treated acute type B aortic dissections. Ann Thorac Surg. 2004;78:1268–1273. [DOI] [PubMed] [Google Scholar]
- 17. American College of Sports Medicine Position Stand . The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. [DOI] [PubMed] [Google Scholar]
- 18. Nemec ED, Mansfield L, Kennedy JW. Heart rate and blood pressure responses during sexual activity in normal males. Am Heart J. 1976;92:274–277. [DOI] [PubMed] [Google Scholar]
- 19. Pickering TG, Case DB, Sullivan PA, et al. Comparison of antihypertensive and hormonal effects of captopril and propranolol at rest and during exercise. Am J Cardiol. 1982;49:1566–1568. [DOI] [PubMed] [Google Scholar]
- 20. Lund‐Johansen P, Omvik P. Long‐term haemodynamic effects of enalapril (alone and in combination with hydrochlorothiazide) at rest and during exercise in essential hypertension. J Hypertens Suppl. 1984;2:S49–S56. [PubMed] [Google Scholar]
- 21. Ekelund LG, Ekelund C, Rössner S. Antihypertensive effects at rest and during exercise of a calcium blocker, nifedipine, alone and in combination with metoprolol. Acta Med Scand. 1982;212:71–75. [DOI] [PubMed] [Google Scholar]
- 22. Lund‐Johansen P. Blood pressure and heart rate responses during physical stress in hypertension: modifications by drug treatment. Eur Heart J. 1999;1(suppl B):B10–B17. [Google Scholar]
- 23. Virtanen K, Jänne J, Frick MH. Response of blood pressure and plasma norepinephrine to propranolol, metoprolol and clonidine during isometric and dynamic exercise in hypertensive patients. Eur J Clin Pharmacol. 1982;21:275–279. [DOI] [PubMed] [Google Scholar]
- 24. Sklar J, Johnston GD, Overlie P, et al. The effects of a cardioselective (metoprolol) and a nonselective (propranolol) β‐adrenergic blocker on the response to dynamic exercise in normal men. Circulation. 1982;65:894–899. [DOI] [PubMed] [Google Scholar]
- 25. Crawford MH, Lindenfeld J, O'Rourke RA. Effects of oral propranolol on left ventricular size and performance during exercise and acute pressure loading. Circulation. 1980;61:549–554. [DOI] [PubMed] [Google Scholar]
- 26. Koch G. Haemodynamic adaptation at rest and during exercise to long‐term antihypertensive treatment with combined α‐ and β‐adrenoreceptor blockade by labetalol. Br Heart J. 1979;41:192–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Johnsson G. Influence of metoprolol and propranolol on hemodynamic effects induced by adrenaline and physical work. Acta Pharmacol Toxicol (Copenh). 1975;36(suppl 5):59–68. [DOI] [PubMed] [Google Scholar]
- 28. Franz IW, Behr U, Ketelhut R. Resting and exercise blood pressure with atenolol, enalapril and a low‐dose combination. J Hypertens Suppl. 1987;5:S37–S41. [PubMed] [Google Scholar]
- 29. Lo AX, Donnelly JP, McGwin G Jr, et al. Impact of gait speed and instrumental activities of daily living on all‐cause mortality in adults ≥65 years with heart failure. Am J Cardiol. 2015;115:797–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Franklin BA, Brinks J, Sacks R, et al. Reduced walking speed and distance as harbingers of the approaching Grim Reaper. Am J Cardiol. 2015;116:313–317. [DOI] [PubMed] [Google Scholar]


