Abstract
Background
Obesity is increasingly recognized as an important risk factor for coronary artery disease (CAD).
Hypothesis
Patients with increased body mass index (BMI) present at a younger age with symptomatic CAD.
Methods
We analyzed data on 2137 consecutive patients admitted for treatment of CAD proven on angiography from 2010 to 2013, excluding those with prior coronary intervention or bypass surgery.
Results
Mean age was 64.1 ± 12.4 years; 75% were male; 43.6% were overweight (BMI 25–29.9 kg/m2) and 31.6% were obese (BMI ≥30 kg/m2). Patients with BMI ≥25 kg/m2 compared with <25 kg/m2 were more likely to have diabetes (24.5% vs 13.6%), hypertension (56.2% vs 45.5%), and hyperlipidemia (42.4% vs 31.6%; P < 0.0001 for all). On multivariate analysis adjusted for sex and cardiovascular risk factors, patients in higher BMI categories had lower mean age in a linear and stepwise fashion compared with those with normal BMI (P < 0.0001). For example, compared with patients with normal BMI, those with BMI of 35 to 39.9 kg/m2 were on average 9.2 years younger (P < 0.0001). Multivariate analysis examining the interaction between sex and BMI produced similar results for effect of BMI on age of presentation (P = 0.97 for interaction).
Conclusions
After multivariate adjustment, patients with increased BMI presented at an earlier age with symptomatic CAD compared with patients with normal BMI. Primary prevention efforts in those with increased BMI to reduce risk‐factor burden, including evidence‐based treatments for weight reduction, promise to reduce risk or delay onset of CAD.
Keywords: Preventive cardiology, Body mass index, Coronary artery disease, Risk factors, Obesity, Cardiac, rehabilitation
1. INTRODUCTION
Obesity and its complications are the most important chronic health problems that the world is facing in the 21st century. In recent reports, 26% of adults worldwide are overweight (body mass index [BMI] 25–29.9 kg/m2) and 13% are obese (BMI ≥30 kg/m2)1; whereas in the United States, 33.6% of adults are overweight and 34.9% are obese.2 Obesity has been recognized as an independent risk factor for coronary artery disease (CAD).3, 4, 5 In a large multicenter registry of patients without known CAD disease undergoing computed tomography (CT) coronary angiography, BMI was independently associated with presence of any CAD and obstructive CAD.6 Obesity is also associated with a clustering of other risk factors for CAD such as diabetes mellitus (DM), hyperlipidemia, and hypertension (HTN).4, 5 Although previous studies strongly suggest that obesity promotes CAD, the association between BMI and age of presentation with symptomatic CAD is not well understood. Better understanding of this association can lead to more patient‐specific strategies for primary and secondary prevention of CAD. It is well known that overweight men and women have a different body fat distribution, with abdominal obesity as measured by the waist‐to‐hip ratio (WHR) being more prevalent in men.7 However, it is unclear whether the effect of obesity as a risk factor for CAD is equally strong in both sexes. In this retrospective cohort study, we investigated the association between BMI and age of presentation in patients with symptomatic CAD and compared this association in men and women.
2. METHODS
Our patient population consisted of consecutive patients between 2010 and 2013 who required hospitalization and investigation with coronary angiography for treatment of suspected CAD. Patients with stable or unstable presentation of CAD at any age were included. Patients with prior percutaneous coronary intervention (PCI) or coronary artery bypass grafting surgery (CABG) were excluded. We also excluded patients with normal coronary arteries and those diagnosed with other cardiac disease such as valvular heart disease, endocarditis, or cardiomyopathy as their main diagnosis.
Our study was conducted at The Canberra Hospital, which is the main referral center for patients with CAD in the Australian Capital Territory and surrounding regions, serving several regional hospitals and a population of approximately 700 000 patients. Data were collected prospectively on consecutive patients including demographics, cardiovascular risk factors, angiographic findings, procedural variables, and type of treatment. Height and weight of each patient were measured with the patient wearing a hospital gown and no footwear.
Body mass index was defined as weight in kilograms divided by the square of the height in meters (kg/m2). Body mass index categories were defined according to the World Health Organization classification as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2), class I obesity (30–34.9 kg/m2), class II obesity (35–39.9 kg/m2), and class III obesity (>40 kg/m2).8 Age of presentation was defined as age at the time of coronary angiography. Cardiovascular risk factors such as DM, HTN, and hyperlipidemia were defined as reported by patients or by presence of medications to treat these conditions. Family history was defined as a history of CAD in first‐degree relatives age <65 years.
2.1. Statistical Analysis
Categorical data were analyzed with the χ2 test and continuous variables were analyzed by the Student t test or Wilcoxon rank‐sum test. Multivariate logistic regression analysis was performed to investigate the effect of BMI on the age of presentation with symptomatic CAD. Variables included in the model included sex, cardiovascular risk factors, and BMI categories. A forward likelihood ratio method was used to enter variables into the regression model. A separate multivariate analysis was performed to analyze the interaction between sex and BMI in relation to age of presentation. All analyses were 2‐tailed, and a P value of 0.05 was considered significant. Analyses were performed using SPSS version 22 software (IBM Corp., Armonk, NY).
3. RESULTS
We analyzed data on 2137 consecutive patients, admitted to hospital for management of CAD proven on angiography. Mean age for the total cohort was 64.1 ± 12.4 years (range, 24.4–99.7 years), and 75% were male. Mean BMI for the cohort was 28.5 ± 5.2 kg/m2 (range, 14.0–55.3 kg/m2). A normal BMI was present in 508 (23.8%) patients, 20 (0.9%) patients were underweight, 929 (43.6%) were overweight, and 675 (31.7%) patients were obese.
The cohort was divided into those with a BMI <25 kg/m2 and ≥25 kg/m2 for a preliminary analysis of the effect of BMI. Baseline characteristics for the 2 groups are shown in Table 1. Patients in the higher‐BMI group were on average 4.6 years younger (P < 0.0001), and there was a lower proportion of women in this group (24.2% vs 28.2%; P = 0.068). Patients with BMI ≥25 kg/m2 were more likely to have DM (24.5% vs 13.6%; P < 0.0001), HTN (56.2% vs 45.5%; P < 0.0001), and hyperlipidemia (42.4% vs 31.6%; P = 0.0001), but were less likely to be current smokers (22.5% vs 27.5%; P = 0.0204). Patients with a higher BMI presented significantly more frequently with a history of stable angina (18.2% vs 13.8%; P = 0.021), and less frequently with ST‐segment elevation myocardial infarction (36.4% vs 46.1%; P < 0.0001). There was no significant difference between the 2 groups with regard to use of radial access for catheterization or the severity of coronary disease found on coronary angiography.
Table 1.
Baseline Characteristics of Study Patients With BMI <25 kg/m2 or ≥25 kg/m2
| Variable | BMI <25 kg/m2, n = 528 | BMI ≥25 kg/m2, n = 1603 | P Value |
|---|---|---|---|
| Mean age, y | 67.6 ± 13.0 | 63.0 ± 12.0 | <0.0001 |
| Female sex | 149 (28.2) | 388 (24.2) | 0.068 |
| DM | 72 (13.6) | 392 (24.5) | <0.0001 |
| On oral hypoglycemics | 20 (3.8) | 123 (7.7) | 0.001 |
| On insulin | 8 (1.5) | 53 (3.3) | 0.022 |
| HTN | 240 (45.5) | 901 (56.2) | <0.0001 |
| Smoker | 145 (27.5) | 360 (22.5) | 0.0204 |
| Reformed smoker | 120 (22.7) | 460 (28.7) | 0.0068 |
| Hyperlipidemia | 167 (31.6) | 680 (42.4) | <0.0001 |
| Family history of IHD | 122 (23.1) | 494 (30.8) | 0.0006 |
| BMI | 22.8 ± 1.9 | 30.4 ± 4.6 | <0.0001 |
| Admission diagnosis | |||
| Stable angina | 71 (13.8) | 278 (18.2) | 0.021 |
| UA | 45 (8.8) | 164 (10.7) | 0.200 |
| NSTEMI | 161 (31.3) | 533 (34.8) | 0.149 |
| STEMI | 237 (46.1) | 557 (36.4) | <0.0001 |
| Radial access | 67 (14.1) | 227 (15.7) | 0.369 |
| Vessels diseased | |||
| 1 | 283 (53.6) | 849 (53.0) | 0.841 |
| 2 | 152 (28.8) | 482 (30.1) | 0.841 |
| 3 | 93 (17.6) | 272 (17.0) | 0.841 |
| Prasugrel/ticagrelor used | 75 (14.5) | 228 (14.7) | 0.898 |
| GP IIb/IIIa inhibitor used | 82 (17.4) | 227 (15.6) | 0.351 |
Abbreviations: BMI, body mass index; DM, diabetes mellitus; GP, glycoprotein; HTN, hypertension; IHD, ischemic heart disease; NSTEMI, non–ST‐segment elevation myocardial infarction; SD, standard deviation; STEMI, ST‐segment elevation myocardial infarction; UA, unstable angina.
Data are presented as n (%) or mean ± SD.
To investigate the impact of BMI on age of presentation with symptomatic CAD, we analyzed the distribution of mean age of presentation across defined BMI categories as shown in Figure 1. We observed a strong linear and inverse association between BMI and age of presentation with CAD (P < 0.0001). This was further investigated with a multivariate analysis, with age of presentation as the dependent variable. Factors entered in the analysis included sex, cardiovascular risk factors, and BMI categories. As seen in Table 2 and also Figure 2, patients in higher‐BMI categories had a lower mean age in a linear and stepwise fashion. Men, smokers, and those with a family history of CAD were significantly younger at the time of presentation, whereas patients with DM and HTN were on average significantly older at the time of presentation.
Figure 1.
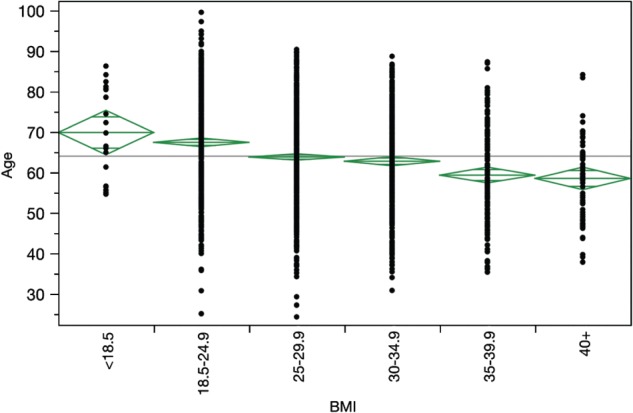
Mean age of presentation with symptomatic CAD with 95% CIs in different BMI categories. Abbreviations: BMI, body mass index; CAD, coronary artery disease; CI, confidence interval.
Table 2.
Multivariate Analysis of the Effect of Risk Factors on Age of Presentation for the Whole Cohort, Adjusted for Prior History of PCI and CABG
| Variables Compared | Difference in Age of Presentation | 95% CI | P Value |
|---|---|---|---|
| Male vs female sex | −4.9 | −6.1 to −3.8 | <0.0001 |
| Smoker vs nonsmoker | −7.6 | −8.8 to −6.4 | <0.0001 |
| DM vs no DM | 1.7 | 0.46 to 2.9 | 0.007 |
| HTN vs no HTN | 3.8 | 2.8 to 4.8 | <0.0001 |
| Previous smoker vs nonsmoker | 0.72 | −0.4 to 1.9 | 0.223 |
| Hyperlipidemia vs no hyperlipidemia | −0.35 | −1.4 to 0.7 | 0.50 |
| Family history present vs absent | −5.8 | −6.8 to −4.7 | <0.0001 |
| BMI, kg/m2 | |||
| 13–18.51 | 2.4 | −5.4 to 10.3 | 1.0 |
| 25.0–29.91 | −3.9 | −5.8 to −2.1 | <0.0001 |
| 30.0–34.91 | −5.7 | −7.9 to −3.6 | <0.0001 |
| 35.0–39.91 | −9.2 | −12.3 to −6.2 | <0.0001 |
| ≥40.01 | −12.6 | −16.7 to −8.4 | <0.0001 |
Abbreviations: BMI, body mass index; CABG, coronary artery bypass grafting; CI, confidence interval; DM, diabetes mellitus; HTN, hypertension; PCI, percutaneous coronary intervention.
Difference in age of presentation indicates average age differential in those with and without the variable, adjusted for other variables. For example, males were on average 4.9 years younger than females at the time of treatment.
Compared with those with a normal BMI (18.5–24.9 kg/m2).
Figure 2.
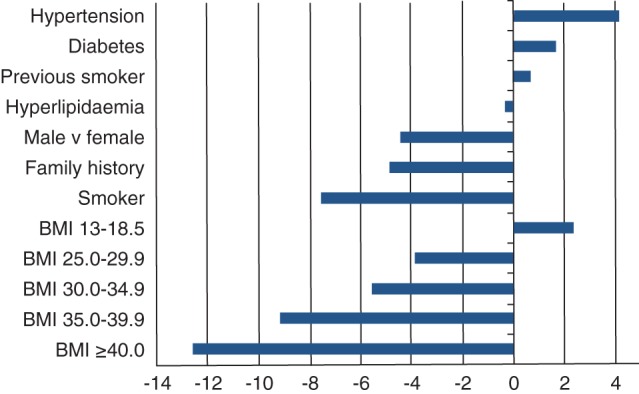
Effect of cardiac risk factors on age of presentation on multivariate analysis. The x‐axis represents the difference between mean age of presentation in patients with and without the risk factor. For example, patients with hypertension were on average approximately 4 years older at presentation compared with those without hypertension. BMI groups are compared with those with a normal BMI (18.5–24.9 kg/m2). Abbreviations: BMI, body mass index.
We also performed a multivariate analysis stratified by sex to examine the interaction between gender and BMI (Figure 3). The model produced similar results for the effect of BMI on age of presentation in males and females (P = 0.97 for interaction).
Figure 3.
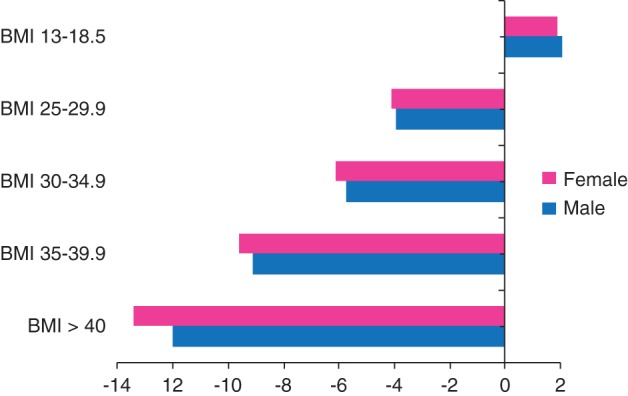
Multivariate analysis of effect of BMI on age of presentation in men and women in different BMI groups compared with those in the normal BMI group (18.5–24.9 kg/m2). The x‐axis represents the difference between mean age of presentation in men and women in different BMI groups compared with those with a normal BMI (P for interaction = 0.97). Abbreviations: BMI, body mass index.
4. DISCUSSION
This study highlights the impact of BMI on the age of presentation with symptomatic CAD. We found a strong and linear association between severity of obesity as measured by BMI and an earlier age of presentation with symptomatic CAD. This association was confirmed in a multivariate analysis, adjusting for all the common risk factors including sex, diabetes, hyperlipidemia, and hypertension. For example, patients with a BMI of 35 kg/m2 to 39.9 kg/m2 presented on average 9.2 years younger at the time of hospitalization than patients with a normal BMI. Eisenstein et al observed a similar trend for earlier age of presentation with coronary artery disease associated with higher BMI, although they did not adjust for presence of other risk factors.9 We believe our is the first study of the association between BMI and age of presentation with CAD in a multivariate analysis.
The above finding adds a new thread of evidence to support the hypothesis that higher BMI is associated with accelerated coronary atherosclerosis resulting in earlier presentation with symptomatic CAD. Data from the Dallas Heart Study showed increased WHR to be predictive of coronary artery calcium score on CT, suggesting that obesity contributes to CAD through promotion of atherosclerosis.7 In a registry of 13 874 patients undergoing CT coronary angiography, BMI was independently associated with presence of any CAD and obstructive CAD.6 After a systematic review of available research, the authors of the US guidelines on obesity concluded that in overweight and obese adults, higher BMI levels were associated with a higher risk of fatal and also combined fatal and nonfatal coronary heart disease.10 It is likely that the influence of higher BMI on the age of presentation is partly independent, as shown in our multivariate analysis, and partly mediated through clustering of risk factors as shown by a higher prevalence of DM, HTN, and hyperlipidemia. From analysis of pooled data of 97 prospective cohort studies, it is estimated that 46% of the excess risk of BMI for CAD is mediated by disorders of blood pressure, serum cholesterol, and blood glucose.5
Obesity in children and young adults has been found to be associated with a higher prevalence of cardiovascular risk factors including HTN, hyperlipidemia, and hyperglycemia.11 Moreover, epidemiologic studies have found that about a third (26% to 41%) of obese preschool children and about half (42% to 63%) of obese school‐age children grow up to be obese adults.12 A Danish study of 276 835 school children age 7 to 13 years found a significant linear association between childhood obesity and incidence of CAD events in adulthood.13 Therefore, It is likely that earlier presentation with CAD events in obese individuals, as in our study, is secondary to a relatively long period of obesity and exposure to metabolic risk factors.
Our study has indicated that cardiovascular risk factors vary with regard to their impact on age of presentation with CAD. Obesity, smoking, and a family history of CAD were associated with a younger age of presentation with CAD, whereas DM and HTN were associated with an older age of presentation. This may be explained by the observation that DM and HTN have their onset at a later age in life, and their effect on causing coronary atherosclerosis may take several years or decades to become manifest in clinical events. This is in contrast to obesity, which is present in 16.9% of children and adolescents ages 2 to 19 years2; and smoking, which is reported in 9% of high school children in the United States.14 Therefore, these are common risk factors in children and adolescents and can lead to clinical coronary events in their fourth or fifth decades of life.
Abdominal obesity has been reported to be more closely associated with insulin resistance and the metabolic syndrome.15 In the INTERHEART study, WHR was more closely associated with the risk of myocardial infarction than was BMI.16 In the Dallas Heart Study, mean WHR for men was 0.96 with a mean BMI of 29.0 kg/m2, compared with a WHR of 0.86 in women with a mean BMI of 31.3 kg/m2, indicating greater abdominal obesity in men.7 Because abdominal obesity is observed more often in men, it can be postulated that the risk of CAD due to obesity may be higher in men compared with women. In our study we found no significant interaction between sex and the effect of BMI on age of presentation with CAD across all of the BMI categories. Similarly, a recent analysis of pooled data from longitudinal population‐based studies did not find any sex difference in risk of CAD for obese patients across all BMI categories.17
Our study adds to the evidence for the importance of increased BMI as a major risk factor for CAD, especially in younger patients. In the primary‐care setting, the use of a lifetime‐risk calculator, as recommended by the American College of Cardiology/American Heart Association (ACC/AHA) and the UK National Institute for Health and Clinical Excellence (NICE) guidelines, is an appropriate way for clinicians to start a conversation about an individual's risk of CAD.18, 19 Following this, specific issues such as diet, lifestyle, and weight control as they relate to the individual can be explored. In overweight patients, focused attention to evidence‐based weight‐reduction strategies,10 in addition to control of traditional cardiovascular risk factors, is likely to be the most successful preventive strategy. The 2013 AHA/ACC/The Obesity Society (TOS) Guideline for the Management of Overweight and Obesity in Adults10 is an important resource and worthy of greater attention, given this report. Our study also highlights the importance of preventing and managing obesity in children and youth, as a significant proportion of these children will grow up to become obese adults and will be at a high risk of premature CAD.
4.1. Study Limitations
This is a single‐center, retrospective, observational study, although our center is a hub for several regional hospitals for treatment of CAD. Some studies have shown other measures of obesity to be better correlated with incident CAD.20, 21 We used BMI as it is the most commonly used and readily available metric for assessment of obesity. Several studies have shown only marginal difference between the predictive value of BMI and other measures of obesity.20, 21, 22, 23 The current US obesity guidelines support the use of BMI as a measure of obesity and provide evidence that higher BMI using the current cutpoints are associated with a higher risk of fatal and nonfatal coronary heart disease.10 It should be noted that the main outcome measure of our study was age of presentation with CAD and not age of first presentation, which was outside the scope of this retrospective study.
5. CONCLUSION
We have shown that obesity is an independent risk factor for earlier age of presentation with CAD and there is a strong linear association between increasing BMI with mean age of presentation. Patients with BMI of 35 kg/m2 to 39.9 kg/m2 presented on average 9.2 years earlier with symptomatic CAD than patients with a normal BMI. This association was equally strong in men and women. Primary prevention efforts in those with increased BMI to reduce risk‐factor burden, including evidence‐based treatments for weight reduction, have the promise of reducing the risk or delaying the onset of CAD.
Atique SM, Shadbolt B, Marley P, Farshid A. Association Between Body Mass Index and Age of Presentation With Symptomatic Coronary Artery Disease, Clin Cardiol 2016;39(11):653–657.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
REFERENCES
- 1. World Health Organization . Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World Health Organization; 2014:79–93. [Google Scholar]
- 2. Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26‐year follow‐up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. [DOI] [PubMed] [Google Scholar]
- 4. Wilson PW, D'Agostino RB, Sullivan L, et al. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002;162:1867–1872. [DOI] [PubMed] [Google Scholar]
- 5. Lu Y, Hajifathalian K, Ezzati M, et al; Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects). Metabolic mediators of the effects of body‐mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet . 2014;383:970–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Labounty TM, Gomez MJ, Achenbach S, et al. Body mass index and the prevalence, severity, and risk of coronary artery disease: an international multicentre study of 13–874 patients. Eur Heart J Cardiovasc Imaging. 2013;14:456–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. See R, Abdullah SM, McGuire DK, et al. The association of differing measures of overweight and obesity with prevalent atherosclerosis: the Dallas Heart Study. J Am Coll Cardiol. 2007;50:752–759. [DOI] [PubMed] [Google Scholar]
- 8. Poirier P, Giles TD, Bray GA, et al; American Heart Association. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation . 2006;113:898–918. [DOI] [PubMed] [Google Scholar]
- 9. Eisenstein EL, Shaw LK, Nelson CL, et al. Obesity and long‐term clinical and economic outcomes in coronary artery disease patients. Obes Res. 2002;10:83–91. [DOI] [PubMed] [Google Scholar]
- 10. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society [published correction appears in J Am Coll Cardiol. 2014;63(25 part B):3029–3030]. J Am Coll Cardiol . 2014;63(25 part B):2985–3023. [DOI] [PubMed] [Google Scholar]
- 11. Skinner AC, Perrin EM, Moss LA, et al. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373:1307–1317. [DOI] [PubMed] [Google Scholar]
- 12. Serdula MK, Ivery D, Coates RJ, et al. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22:167–177. [DOI] [PubMed] [Google Scholar]
- 13. Baker JL, Olsen LW, Sørensen TI. Childhood body‐mass index and the risk of coronary heart disease in adulthood. N Engl J Med. 2007;357:2329–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Arrazola RA, Singh T, Corey, CG et al; Centers for Disease Control and Prevention. Tobacco use among middle and high school students—United States, 2011–2014. MMWR Morb Mortal Wkly Rep . 2015;64:381–385. [PMC free article] [PubMed] [Google Scholar]
- 15. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement [published corrections appear in Circulation. 2005;112:e297–e298]. Circulation. 2005;112:2735–2752. [DOI] [PubMed] [Google Scholar]
- 16. Yusuf S, Hawken S, Ounpuu S, et al; INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet . 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 17. Mongraw‐Chaffin ML, Peters SA, Huxley RR, et al. The sex‐specific association between BMI and coronary heart disease: a systematic review and meta‐analysis of 95 cohorts with 1.2 million participants. Lancet Diabetes Endocrinol . 2015;3:437–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Goff DC Jr, Lloyd‐Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in J Am Coll Cardiol. 2014;63(25 part B):3026]. J Am Coll Cardiol . 2014;63:2935–2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rabar S, Harker M, O'Flynn N, et al. Lipid modification and cardiovascular risk assessment for the primary and secondary prevention of cardiovascular disease: summary of updated NICE guidance. BMJ. 2014;349:g4356. [DOI] [PubMed] [Google Scholar]
- 20. Kaess BM, Jozwiak J, Mastej M, et al. Association between anthropometric obesity measures and coronary artery disease: a cross‐sectional survey of 16 657 subjects from 444 Polish cities. Heart. 2010;96:131–135. [DOI] [PubMed] [Google Scholar]
- 21. Gruson E, Montaye M, Kee F, et al. Anthropometric assessment of abdominal obesity and coronary heart disease risk in men: the PRIME study. Heart. 2010;96:136–140. [DOI] [PubMed] [Google Scholar]
- 22. Gelber RP, Gaziano JM, Orav EJ, et al. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol. 2008;52:605–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Litwin SE. Which measures of obesity best predict cardiovascular risk? J Am Coll Cardiol. 2008;52:616–619. [DOI] [PubMed] [Google Scholar]


