ABSTRACT
Background
The prognostic significance of right bundle branch block (RBBB) is inconsistent across studies. We aimed to assess the association between RBBB (in general population and patients with heart disease) and risk of all‐cause mortality, cardiac death, acute myocardial infarction (MI), and heart failure (HF).
Hypothesis
RBBB may be associated with increased risk of death.
Methods
PubMed, EMBASE, and the Cochrane Library up to February 2015 were searched for prospective cohort studies that reported RBBB at baseline and all‐cause mortality, cardiac death, MI, and HF at follow‐up. A meta‐analysis of published data was undertaken primarily by means of fixed‐effects models.
Results
Nineteen cohort studies including 201 437 participants were included with a mean follow‐up period ranging from 1 to 246 months. For general population with RBBB, the pooled adjusted hazard ratio (HR) for all‐cause mortality was 1.17 (95% confidence interval [CI]: 1.03–1.33) compared with no BBB. General population with RBBB had an increased risk of cardiac death (HR: 1.43, 95% CI: 1.17–1.74). For patients with RBBB and acute MI, the pooled risk ratio was 2.31 (95% CI: 2.13–2.49) for in‐hospital mortality, 2.85 (95% CI: 2.46–3.30) for 30‐day mortality, and 1.96 (95% CI: 1.59–2.42) for longer‐term mortality. For acute HF patients, the pooled risk ratio of all‐cause mortality was 1.11 (95% CI: 1.06–1.16), and for chronic HF patients it was 1.75 (95% CI: 1.38–2.22).
Conclusions
Right bundle branch block is associated with an increased risk of mortality in general population and patients with heart disease.
Introduction
Right bundle branch block (RBBB) is an intraventricular conduction disorder in which normal electrical activity in the His‐Purkinje system is disrupted and depolarization of the right ventricle is delayed. After the left ventricle depolarizes normally, the wave of depolarization spreads to the right ventricle through nonspecialized conducting tissue. Consequently, the electrocardiogram (ECG) reveals a QRS duration ≥0.12 seconds, a secondary R wave (R′) in V1 or V2, and a wide slurred S wave in leads I, V5, and V6, often with associated ST‐segment depression and T‐wave inversion in the right precordial leads.
Right bundle branch block occurs in 0.2% to 1.3% of general population and may be an incidental finding on ECG or a manifestation of occult or symptomatic heart disease (congenital, ischemic, inflammatory, rheumatic) and pulmonary disease (pulmonary embolism, cor pulmonale).1, 2, 3
The clinical relevance of RBBB is not only determined by its etiology, but also ultimately by its prognosis. However, recent studies have reported conflicting results on its association with clinical outcomes. For example, in general population, the Women's Health Initiative study of 53 197 women, free of cerebrovascular disease, did not identify RBBB as a predictor of a significant increase in either all‐cause mortality or cardiac death during 14 years of follow‐up.4 However, the Copenhagen City Heart Study of 18 441 participants without prior myocardial infarction (MI) or heart failure (HF) revealed that RBBB increased the risk for all‐cause mortality and cardiac death over 20 years of follow‐up.5 Furthermore, in patients with heart disease (MI and HF), several other studies have reported positive associations between RBBB and all‐cause mortality,6, 7, 8, 9, 10, 11 whereas others have reported no association.12, 13, 14
We hypothesized first that RBBB as a manifestation of heart disease (MI and HF) would be strongly associated with a poor prognosis (increased risk of mortality), and second that RBBB in an asymptomatic general population would have an occult, undeclared cardiopulmonary cause, and therefore would also be associated with a poor prognosis, albeit more weakly than in patients with RBBB due to symptomatic heart disease.
We performed a meta‐analysis of large observational studies to investigate the relationship between RBBB and the outcomes of all‐cause mortality and cardiac death among general population, MI patients, and HF patients, and the relationship between RBBB and the outcomes of MI and HF among general population.
Methods
Search Strategy
Published studies were identified through a computer‐based search (up to February 1, 2015) of PubMed and EMBASE for relevant literatures on the associations between RBBB and all‐cause mortality, cardiac death, MI, and HF by using the keywords “right bundle‐branch block*,” “right bundle branch block*,” “RBBB,” “right BBB,” “mortality,” “death,” “prognosis,” “outcome,” and “community,” and Medical Subject Headings (MeSH) terms “healthy volunteers,” “myocardial infarction,” and “heart failure.” The search was limited to human studies. In addition, the PubMed option “Related Articles” was used, and the references of identified studies were reviewed to search for potentially relevant papers. Only papers published in English were considered. No review protocol was available in the Cochrane Library.
Selection Criteria
Two reviewers (Y.X. and S.W.) independently reviewed the abstracts and titles identified by the database searches and together decided which articles should be retrieved. These retrieved articles were reviewed by both authors to identify suitable studies. Discrepancies were resolved by consensus. Reviewers were not blinded to study authors and results. Articles were considered for inclusion in this meta‐analysis if (1) the authors reported data from an original, peer‐reviewed study; (2) the study was a longitudinal cohort study consisting of subjects who had an ECG at baseline, a diagnosis of RBBB (or not) made at baseline according to standardized diagnostic criteria, and who could be classified as general population, acute MI, or HF (acute MI was established by the presence of 2 of the following 3 criteria: elevation of serum creatine kinase >2× upper limit of normal values, characteristic chest pain lasting ≥30 minutes, or ECG ST‐T changes with evolution of an abnormal Q wave; HF included acute congestive HF and chronic HF that was diagnosed by clinical manifestations and diagnostic tests, including echocardiography and/or biomarkers); (3) hazard ratio (HR), relative risk (RR), or odds ratio (OR) of RBBB for risk of all‐cause mortality, cardiac death, MI, or HF was available, or number of subjects with RBBB status and all‐cause mortality, cardiac death, MI, or HF were available, which can be used to calculate the RR; (4) subjects were adults age ≥18 years; and (5) the study was the most relevant and most recent if subjects/populations overlapped considering that many large sample studies were published in this area, we arbitrarily selected studies with >1000 subjects with ECG data to provide more powerful evidence. Exclusion criteria were (1) case report or cross‐sectional studies, (2) no or insufficient data, or (3) the same data overlapped another eligible larger or more recent study.
Data Extraction
All data were independently abstracted in duplicate by means of a standardized data‐collection form. Discrepancies were resolved by discussion and referencing the original publication. We also contacted authors to request additional information. The following information was extracted from the eligible articles: study characteristics (study title, authors, year of publication, journal, study site, follow‐up duration, and sample size), demographic characteristics (mean age or age range and sex), number of subjects with RBBB and no BBB (QRS duration <120 ms on ECG), main outcome at follow‐up (all‐cause mortality, cardiac death, MI, or HF), and analysis strategy (statistical models, covariates included in the models). Duration of follow‐up among participants with MI at baseline was categorized as in‐hospital (ie, inpatient), within 30 days of MI, and longer‐term (>1 month after MI). Quality assessment was performed with the Newcastle‐Ottawa Scale for assessing quality of cohort studies, and studies with ≥8 stars were considered high‐quality studies.
Data Synthesis and Analysis
Comparison groups were based on RBBB vs no BBB. Due to the long duration of follow‐up, adjusted HRs in multivariate Cox proportional hazard models were used to assess the relationship between RBBB and all‐cause mortality, cardiac death, MI, or HF in general population. Risk ratio was used to evaluate the relationship of RBBB with all‐cause mortality in MI or HF patients. If HRs were not reported, the numbers of different outcomes for both RBBB‐positive and RBBB‐negative groups were recorded for each study using 2 × 2 tables. Risk ratios and their 95% confidence intervals (CIs) were calculated individually for each study. Heterogeneity across studies was evaluated by means of Q and I2 statistics.15 I2 ≥ 50% was considered significant heterogeneity. Reasons for significant heterogeneity were explored. Fixed‐effects models were used to calculate the pooled HRs or RRs if the studies did not have significant heterogeneity. Otherwise, random‐effects models were utilized if the heterogeneity could not be explained or stratified analyses could not be performed. Sensitivity analyses were performed by excluding studies, one at a time, or only including high‐quality studies to evaluate the impact of selected studies on study results.
The potential for publication bias was investigated using visual assessment of the funnel plot calculated by Review Manager 5.2 software (the Nordic Cochrane Centre, Copenhagen, Denmark; http://ims.cochrane.org/revman). As publication bias may lead to asymmetrical funnel plots,16 we visually assessed publication bias based on funnel plots with a study number ≥5.
Results
Literature Search
The search process is presented in Figure 1. A total of 1018 potentially relevant citations were initially identified. After the first round of screening based on titles and abstracts, 45 articles remained for further evaluation. After examining those articles in more detail, 26 articles were excluded for reasons shown in Figure 1. In total, 19 articles were included into the meta‐analysis.
Figure 1.
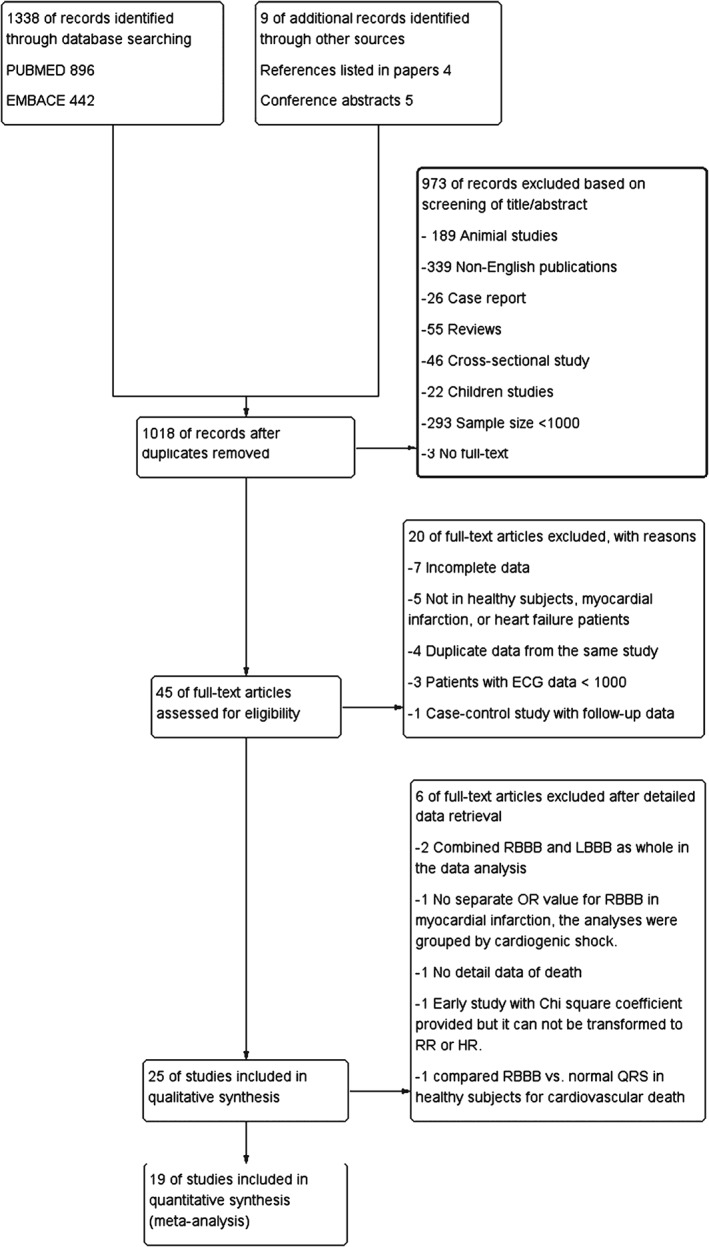
The flow chart of studies selection. Abbreviations: ECG, electrocardiographic; HR, hazard ratio; LBBB, left bundle branch block; OR, odds ratio; RBBB, right bundle branch block; RR, risk ratio.
Study Characteristics
Characteristics of the selected studies are shown in the Table 1. Of the 19 studies, 9 were conducted in Europe and 4 in the United States.
The diagnosis of RBBB was based on ECG in all studies; 17 studies only included complete RBBB, and 2 studies did not mention the definition of RBBB.
The total number of participants included in this meta‐analysis was 201 437, ranging from 1220 in the smallest study1 to 53 605 in the largest study.4 The study population in 15 studies consisted of men and women, 1 study consisted of only women, and 3 studies consisted of only men.
The studies varied with regard to follow‐up duration (1–246 months) and controlled variables in the multivariate models.
Eighteen studies reported all‐cause mortality, 5 studies reported cardiac death, and 2 studies reported MI and HF as clinical outcomes.
The quality of the studies included in the meta‐analysis was generally high; 13 studies had 8 or 9 stars, and 6 studies had 5 to 7 stars (see Supporting Information, Table 1, in the online version of this article).
Table 1.
Summary of the included studies
| Source | Study Participants | Sample size | RBBB types | Mean/median follow‐up duration, M | Follow‐up process | Outcome Assessment | Adjusted for multiple variables (Yes/No) | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Eriksson P, 20051 | General population‐men aged 52 y in Sweden | 7,392 | Complete | Mean unknown, follow‐up over 28 y | Hospital records, the Swedish National Register on death, stroke register and MI register | All‐cause mortality, cardiac death, acute MI, heart failure | Yes | In men with RBBB, there was no increased risk of MI, HF, cardiac death or all‐cause mortality. |
| Stein R, 20102 | General population‐ Veteran men aged 59 y in USA | 9,623 | Complete | 106 | The California Death Index and the Social Security Death Index | All‐cause mortality and cardiac death | Yes | Exercise‐induced RBBB was not associated with all‐cause mortality or cardiovascular mortality. |
| Zhang ZM, 20124 | General population‐women aged 62 y in the Women's Health Initiative in USA | 53,605 | Complete | 168 | Annual telephone follow‐up, vital records, and community surveillance of hospitalized and fatal events | All‐cause mortality and cardiac death | Yes | RBBB in women without CVD was not significant predictor for all‐cause mortality or cardiac death. |
| Bussink BE, 20135 | General population‐men and women aged ≥20 y in Copenhagen City Heart Study | 18,441 | Complete | 246 | Obtained from the National Patient Registry and the National Danish Causes of Death Register | All‐cause mortality, cardiac death, acute MI, heart failure | Yes | RBBB was associated with increased cardiovascular risk and all‐cause mortality. |
| Kleemann T, 20086 | Acute STEMI and NSTEMI men and women aged 69 y in Germany | 26,636 | Complete | 12 M for NSTEMI, 15.7 M for STEMI | Telephone follow‐up | All‐cause mortality | Yes | Unlike RBBB in STEMI, RBBB in NSTEMI was not an independent predictor of all‐cause mortality. |
| Wong CK, 20067 | Acute MI men and women aged 61 y in HERO‐2 trial | 17,073 | Complete | 1 | Hospital records, death certification | All‐cause mortality | Yes | RBBB accompanying anterior acute MI was independent predictor of high 30‐day mortality. |
| Widimsky P, 20128 | Acute MI men and women aged 65 y in Czech Republic | 6,742 | Complete | In‐hospital | Hospital records | All‐cause mortality | Unknown | In hospital mortality of patients with AMI and RBBB was highest from all ECG presentations of AMI. |
| McCullough PA, 20059 | Acute HF men and women aged 63 y in USA | 2,907 | Complete | 23.4 | Stae of Michigan Death Certificate Registry, record of a death within death identification service | All‐cause mortality | Yes | RBBB was associated with increase all‐cause mortality. |
| Cinca J, 201310 | Chronic HF men and women aged 66 y in Spain | 1,762 | Complete | 21 | Outpatient annual visits, readmission, or event reports | All‐cause mortality, cardiac death | Yes | RBBB was associated with increased all‐cause mortality and cardiac death. |
| Manzano L, 201111 | Chronic HF men and women aged 76 y in multicenter SENIORS trial | 2,128 | Not clearly stated | 21 | Clinical visits | All‐cause mortality | Yes | RBBB was significantly associated with all‐cause mortality but not in multivariate cox regression model. |
| Abdel‐Qadir HM, 201112 | Acute HF men and women aged 75 y in Canada | 9,082 | Complete | 60 | Registered Persons Database | All‐cause mortality | Unknown | RBBB was associated with increased all‐cause mortality |
| Archbold RA, 199813 | Acute MI men and women aged 60 y in London | 1,220 | Complete | 6 | Hospital records, general practitioner records or direct inquiry | All‐cause mortality | Unknown | RBBB was significantly associated with increased all‐cause mortality. |
| Haataja P, 201521 | Individuals from the Heath 2000 survey‐men and women aged over 30 y in Finnish | 6,299 | Complete | 98 | The Causes of the Death register maintained by Statistic Finland | Cardiac death | Yes | RBBB was not associated with the risk of cardiac death. |
| Hess B, 200122 | Subjects referred for symptom‐limited exercise nuclear exercise testing‐men and women aged 60 y in USA | 7,073 | Complete | 80 | Social Security Administration Death Master Files | All‐cause mortality | Yes | Complete RBBB and LBBB were independent predictors for all‐cause mortality risk even after adjustment for exercise capacity, nuclear perfusion defects, and other risk factors. |
| Taniguchi M, 200323 | Pilots men aged 53 y in Japan | 2,722 | Complete | 131 | Clinical visits | All‐cause mortality | N/A | No patient died and RBBB did not confer a poor prognosis. |
| Ahmadi A, 201424 | Acute MI men and women aged 61 y in Iran | 20,750 | No clearly stated | In‐hospital | Hospital records | All‐cause mortality | Yes | RBBB was associated with increased risk for in hospital mortality in acute MI patients. |
| Iwasaki J, 200925 | Acute MI men and women aged 70 y in Japan | 1,227 | Complete | In‐hospital | Hospital records | All‐cause mortality | Unknown | New permanent RBBB during inferior MI was a strong predictor for increased in‐hospital mortality. |
| Melgarejo‐Moreno A, 199726 | Acute MI men and women aged >50 y in Spain | 1,238 | Complete | 12 | Hospital records, unknown after discharge | All‐cause mortality | Yes | RBBB was an independent predictor for early and 1‐year mortality. |
| Baldasseroni S, 200327 | Acute HF men and women aged 70 y in Italy | 5,517 | Complete | 12 | Clinical visits, telephone interview using standardized questionnaire | All‐cause mortality | N/A | LBBB but not RBBB was an independent predictor of death in HF patients. |
MI, myocardial infarction; HF, heart failure; STEMI, ST elevation myocardial infarction; NSTEMI, non‐ST elevation myocardial infarction; SENIORS, Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure; ECG, electrocardiogram; LBBB, left bundle branch block; N/A, non‐applicable.
All‐Cause Mortality in General Population With Right Bundle Branch Block
In general population, 6 studies reported RBBB and all‐cause mortality. Nonsignificant heterogeneity (I 2 = 49%) was found across the studies. Right bundle branch block was associated with an increased risk of all‐cause mortality in general population, with an HR of 1.17 (95% CI: 1.03–1.33; Figure 2).
Figure 2.
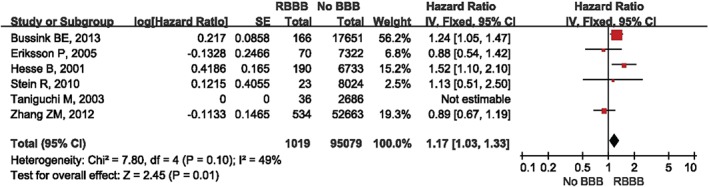
RBBB for all‐cause mortality in general population. Abbreviations: BBB, bundle branch block; CI, confidence interval; df, degrees of freedom; IV, inverse variance; LBBB, left bundle branch block; RBBB, right bundle branch block; SE, standard error.
Among the 6 studies, 4 studies evaluated RBBB for all‐cause mortality in men. Low heterogeneity was detected among these studies (I 2 = 9%), and the pooled HR for all‐cause mortality was 1.22 (95% CI: 1.03–1.45; see Supporting Information, Figure 1, in the online version of this article). Two studies reported the association between RBBB and all‐cause mortality in women, but there was significant heterogeneity (I 2 = 70%); the pooled HR was 1.09 (95% CI: 0.73–1.61).
All‐Cause Mortality in Patients With Acute Myocardial Infarction and Right Bundle Branch Block
In acute MI patients, the 5 studies that examined the association between RBBB and in‐hospital mortality each reported a doubling of risk, and the pooled RR was 2.31 (95% CI: 2.13–2.49; I2 = 44%; Figure 3). In the single study that reported the association between RBBB and 30‐day mortality, the association was also positive (RR: 2.85, 95% CI: 2.46–3.30). The 3 studies that examined the association between RBBB and longer‐term mortality (>1 month after MI) were characterized by significant heterogeneity (I 2 = 57%; Cochrane Q statistic: 4.68; P = 0.10) and a pooled RR from random‐effects model of 1.96 (95% CI: 1.59–2.42; Figure 3). A sensitivity analysis, in which each study in turn was omitted, showed that the study of Archbold et al13 had the largest influence on the heterogeneity. Without this study, heterogeneity was nonsignificant (I 2 = 48%; Cochrane Q statistic: 1.93; P = 0.16) and the pooled RR for longer‐term mortality was 1.97 (95% CI: 1.83–2.11).
Figure 3.
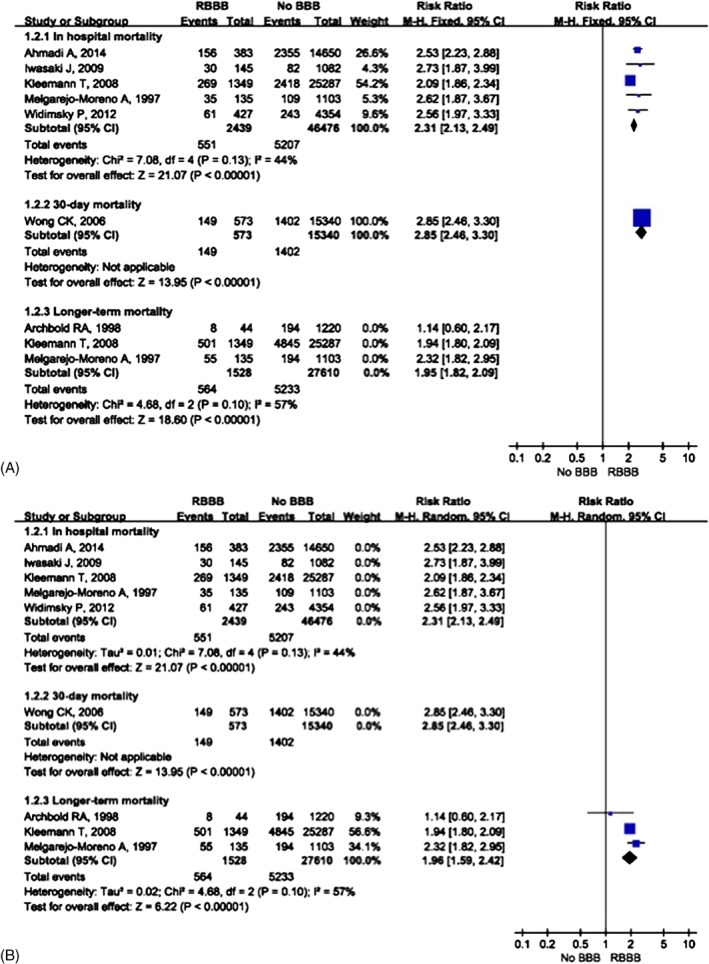
RBBB for all‐cause mortality in myocardial infarction. Abbreviations: BBB, bundle branch block; CI, confidence interval; df, degrees of freedom; M‐H, Mantel‐Haenszel; RBBB, right bundle branch block.
Further sensitivity analysis, which only included high‐quality studies, found similar results to all studies, with pooled RRs of 2.28 (95% CI: 2.10–2.47) and 1.97 (95% CI: 1.83–2.11) for in‐hospital mortality and longer‐term mortality, respectively. Subgroup analysis according to patient sex could not be performed because of a lack of relevant reported data in these 8 studies.
Overall, in patients with MI, RBBB was associated with an increased risk of all‐cause mortality in‐hospital, at 30 days, and in the longer term.
All‐Cause Mortality in Patients With Heart Failure and Right Bundle Branch Block
In acute HF patients, 3 studies reported a modest increase in risk of all‐cause mortality (pooled RR: 1.11, 95% CI: 1.06–1.16). Moderate, but nonsignificant, heterogeneity across the studies was present (I 2 = 46%).
In chronic HF patients, 2 studies reported a significant increase in risk of all‐cause mortality (pooled RR: 1.75, 95% CI: 1.38–2.22). No heterogeneity was observed (Figure 4). A sensitivity analysis with only high‐quality studies and omission of any single study did not change the overall result.
Figure 4.
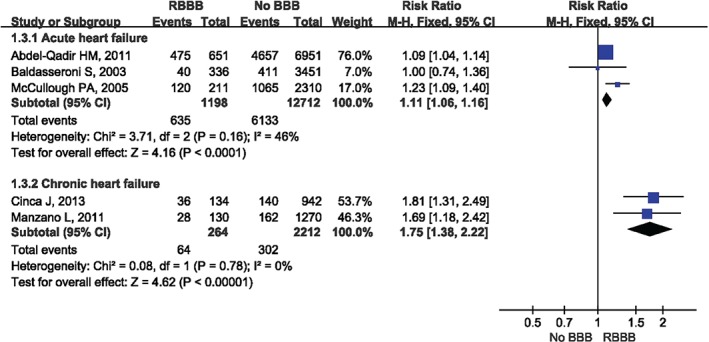
RBBB for all‐cause mortality in heart failure. Abbreviations: BBB, bundle branch block; CI, confidence interval; df, degrees of freedom; M‐H, Mantel‐Haenszel; RBBB, right bundle branch block.
Cardiac Death in General Population With Right Bundle Branch Block
In general population, 6 studies evaluated the association between RBBB and risk of cardiac death; the pooled HR was 1.43 (95% CI: 1.17–1.74) with no heterogeneity among the studies (see Supporting Information, Figure 2, in the online version of this article).
Four of these studies provided separate data for men and 2 studies for women. There was no significant heterogeneity among the studies (I 2 = 44% in men and I 2 = 13% in women) and the pooled HRs were 1.72 (95% CI: 1.34–2.22) for men and 1.63 (95% CI: 1.15–2.31) for women (see Supporting Information, Figure 3, in the online version of this article).
Cardiac Death in Heart Failure Patients With Right Bundle Branch Block
In HF patients, only 1 study reported the risk of cardiac death associated with RBBB.10 The HR was 1.89 (95% CI: 1.19–3.01).
Heart Failure and Myocardial Infarction in General Population With Right Bundle Branch Block
In general population, 2 studies reported RBBB and the risk for MI and HF. Very low heterogeneity was detected between the 2 studies, and RBBB was not associated with incident MI or HF (see Supporting Information, figures 4 and 5, in the online version of this article).
Analysis of Publication Bias
In general population, MI, and HF patients, no publication bias was evident upon graphical inspection of the funnel plots for studies of the association between RBBB and all‐cause mortality in general population and patients with MI and HF (see Supporting Information, figures 6–8, in the online version of this article), as well as RBBB and cardiac death in general population (see Supporting Information, Figure 9, in the online version of this article). Funnel plots were not constructed for studies of the association between RBBB in general population and MI and HF because of too few studies (<5).
Discussion
Several large epidemiological and cohort studies that have examined the effect of RBBB on the risk of all‐cause mortality, cardiac death, MI, and HF have provided inconsistent findings. Using a meta‐analysis of published large observational studies, we found that RBBB was associated with an increased risk of all‐cause mortality in general population, MI, and HF patients, and with an increased risk of cardiac death, but not MI or HF, in the general population.
Right bundle branch block was also significantly associated with an increased risk of all‐cause mortality and cardiac death in healthy men, and an increased risk for cardiac death in healthy women. It is very interesting to observe the sex differences on all‐cause mortality in our meta‐analysis. Although the pooled HR was not significant, it showed a positive trend for the association between RBBB and all‐cause mortality in women, but a strong conclusion could not be drawn based on 2 studies. More studies are warranted in future to evaluate whether women with RBBB hazard a high risk for all‐cause mortality.
The strengths of our meta‐analysis are that it included all published large‐cohort studies, the methodological quality of most studies was high, and the results of the associations between RBBB and all‐cause mortality, cardiac death, MI, and HF in the general population and patients with MI and HF are reasonably consistent and robust, allowing for clinically meaningful insights.
Study Limitations
There are several potential limitations also, however. First, our meta‐analysis was limited to English‐language publications, raising the possibility of publication bias by failing to include unidentified unpublished reports and reports in other languages. Second, data extraction and analyses were not blinded to the authors, journals, or institutions of the publications, raising the possibility of assessor bias. Nevertheless, the literature screening and data extraction were performed independently by 2 investigators. Third, substantial heterogeneity was present among some studies in some of the meta‐analyses. Moderate heterogeneity among studies of the association between RBBB and all‐cause mortality in general population was mainly due to the differences among the studies in their subjects (age, race, and sex), follow‐up duration, and covariates included in multivariate Cox regression models.4, 5 When heterogeneity was significant, random‐effects models were used in place of fixed‐effects models. Fourth, 2 studies did not clearly state how to define RBBB, only introduced RBBB as a variable in the analysis, and the presence of concomitant left fascicular block (anterior, posterior, or even septal LBBB) and atrioventricular block (mainly first degree), which may affect the prognosis, was not noted in most of the studies. Fifth, our results are prone to not only bias (publication bias, study‐quality bias, assessor bias), but also random error in areas where study numbers, patient numbers, and outcome events were few, and hence statistical power was limited. This was particularly evident in studies of the relation between RBBB and MI and HF in healthy individuals. Hence, more longitudinal studies with larger sample size are warranted to investigate the relationship of RBBB with MI and HF.
The underlying mechanism of how RBBB increased overall risk for all‐cause mortality and cardiac death in general population patients is still unknown. Pathologic and physiologic studies have indicated that RBBB is associated with fibrosis of the conduction system17, 18 and might contribute to bradyarrhythmias and tachyarrhythmias.19 In patients with MI, RBBB was more frequent in anterior MI, which may reflect larger infarct territories, or was associated with atrioventricular block and low left ventricular ejection fraction.6, 7 In patients with HF, RBBB was associated with diminishing left ventricular systolic function,9, 20 which is a strong predictor for mortality.
It is likely that inclusion of RBBB in future iterations of risk scores for general population and patients presenting with MI and acute HF will help refine the predictive ability of such risk scores to discriminate among relevant patients along a continuum of risk of adverse outcomes.
Conclusion
Right bundle branch block was associated with a modest but statistically significant increased risk for all‐cause mortality in general population and HF patients. A more pronounced increased risk was observed in MI patients. Results from this meta‐analysis support previous prospective cohort studies reporting that RBBB is not a benign finding, but portends a higher mortality risk.
Supporting information
Appendix S1
The project was supported by National Natural Science Foundation of China (nos. 81300244 and 81400898).
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Eriksson P, Wilhelmsen L, Rosengren A. Bundle‐branch block in middle‐aged men: risk of complications and death over 28 years. The Primary Prevention Study in Göteborg, Sweden. Eur Heart J. 2005;26:2300–2306. [DOI] [PubMed] [Google Scholar]
- 2. Stein R, Nguyen P, Abella J, et al. Prevalence and prognostic significance of exercise‐induced right bundle branch block. Am J Cardiol. 2010;105:677–680. [DOI] [PubMed] [Google Scholar]
- 3. Zimetbaum PJ, Buxton AE, Batsford W, et al. Electrocardiographic predictors of arrhythmic death and total mortality in the multicenter unsustained tachycardia trial. Circulation. 2004;110:766–769. [DOI] [PubMed] [Google Scholar]
- 4. Zhang ZM, Rautaharju PM, Soliman EZ, et al. Mortality risk associated with bundle branch blocks and related repolarization abnormalities (from the Women's Health Initiative [WHI]). Am J Cardiol. 2012;110:1489–1495. [DOI] [PubMed] [Google Scholar]
- 5. Bussink BE, Holst AG, Jespersen L, et al. Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur Heart J. 2013;34:138–146. [DOI] [PubMed] [Google Scholar]
- 6. Kleemann T, Juenger C, Gitt AK, et al. Incidence and clinical impact of right bundle branch block in patients with acute myocardial infarction: ST‐elevation myocardial infarction versus non–ST‐elevation myocardial infarction. Am Heart J. 2008;156:256–261. [DOI] [PubMed] [Google Scholar]
- 7. Wong CK, Stewart RA, Gao W, et al. Prognostic differences between different types of bundle branch block during the early phase of acute myocardial infarction: insights from the Hirulog and Early Reperfusion or Occlusion (HERO)‐2 trial. Eur Heart J. 2006;27:21–28. [DOI] [PubMed] [Google Scholar]
- 8. Widimsky P, Rohác F, Stásek J, et al. Primary angioplasty in acute myocardial infarction with right bundle branch block: should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy? Eur Heart J. 2012;33:86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McCullough PA, Hassan SA, Pallekonda V, et al. Bundle branch block patterns, age, renal dysfunction, and heart failure mortality. Int J Cardiol. 2005;102:303–308. [DOI] [PubMed] [Google Scholar]
- 10. Cinca J, Mendez A, Puig T, et al; Investigators of the Spanish Heart Failure Network . Differential clinical characteristics and prognosis of intraventricular conduction defects in patients with chronic heart failure. Eur J Heart Fail. 2013;15:877–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Manzano L, Babalis D, Roughton M, et al; SENIORS Investigators. Predictors of clinical outcomes in elderly patients with heart failure. Eur J Heart Fail. 2011;13:528–536. [DOI] [PubMed] [Google Scholar]
- 12. Abdel‐Qadir HM, Tu JV, Austin PC, et al. Bundle branch block patterns and long‐term outcomes in heart failure. Int J Cardiol. 2011;146:213–218. [DOI] [PubMed] [Google Scholar]
- 13. Archbold RA, Sayer JW, Ray S, et al. Frequency and prognostic implications of conduction defects in acute myocardial infarction since the introduction of thrombolytic therapy. Eur Heart J. 1998;19:893–898. [DOI] [PubMed] [Google Scholar]
- 14. Juárez‐Herrera U, Jerjes‐Sánchez C; RENASICA II Investigators. Risk factors, therapeutic approaches, and in‐hospital outcomes in Mexicans with ST‐elevation acute myocardial infarction: the RENASICA II multicenter registry. Clin Cardiol. 2013;36:241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med. 2002;21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 16. Egger M, Davey Smith G, Schneider M, et al. Bias in meta‐analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Krongrad E, Hefler SE, Bowman FO Jr, et al. Further observations on the etiology of the right bundle branch block pattern following right ventriculotomy. Circulation. 1974;50:1105–1113. [DOI] [PubMed] [Google Scholar]
- 18. Horowitz LN, Alexander JA, Edmunds LH Jr. Postoperative right bundle branch block: identification of three levels of block. Circulation. 1980;62:319–328. [DOI] [PubMed] [Google Scholar]
- 19. Denes P, Dhingra RC, Wu D, et al. H‐V interval in patients with bifascicular block (right bundle branch block and left anterior hemiblock): clinical, electrocardiographic and electrophysiologic correlations. Am J Cardiol. 1975;35:23–29. [DOI] [PubMed] [Google Scholar]
- 20. Ashley EA, Raxwal VK, Froelicher VF. The prevalence and prognostic significance of electrocardiographic abnormalities. Curr Probl Cardiol. 2000;25:1–72. [DOI] [PubMed] [Google Scholar]
- 21. Haataja P, Anttila I, Nikus K, et al. Prognostic implications of intraventricular conduction delays in a general population: the Health 2000 Survey. Ann Med. 2015;47:74–80. [DOI] [PubMed] [Google Scholar]
- 22. Hesse B, Diaz LA, Snader CE, et al. Complete bundle branch block as an independent predictor of all‐cause mortality: report of 7073 patients referred for nuclear exercise testing. Am J Med. 2001;110:253–259. [DOI] [PubMed] [Google Scholar]
- 23. Taniguchi M, Nakano H, Kuwahara K, et al. Prognostic and clinical significance of newly acquired complete right bundle branch block in Japan airline pilots. Intern Med. 2003;42:21–24. [DOI] [PubMed] [Google Scholar]
- 24. Ahmadi A, Soori H, Mehrabi Y, et al. Epidemiologic pattern of myocardial infarction and modelling risk factors relevant to in‐hospital mortality: the first results from the Iranian Myocardial Infarction Registry. Kardiol Pol. 2015;73:451–457. [DOI] [PubMed] [Google Scholar]
- 25. Iwasaki J, Kono K, Katayama Y, et al. Prognostic significance of right bundle branch block in patients with acute inferior myocardial infarction. Acta Med Okayama. 2009;63:25–33. [DOI] [PubMed] [Google Scholar]
- 26. Melgarejo‐Moreno A, Galcerá‐Tomás J, Garciá‐Alberola A, et al. Incidence, clinical characteristics, and prognostic significance of right bundle‐branch block in acute myocardial infarction: a study in the thrombolytic era. Circulation. 1997;96:1139–1144. [DOI] [PubMed] [Google Scholar]
- 27. Baldasseroni S, Gentile A, Gorini M, et al. Intraventricular conduction defects in patients with congestive heart failure: left but not right bundle branch block is an independent predictor of prognosis. A report from the Italian Network on Congestive Heart Failure (IN‐CHF database). Ital Heart J. 2003;4:607–613. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1


