ABSTRACT
The incidence of acute coronary syndromes (ACS) is high in the elderly. Despite a high prevalence of frailty and other aging‐related variables, little information exists about the optimal clinical management in patients with coexisting geriatric syndromes. The aim of the LONGEVO‐SCA registry (Impacto de la Fragilidad y Otros Síndromes Geriátricos en el Manejo y Pronóstico Vital del Anciano con Síndrome Coronario Agudo sin Elevación de Segmento ST) is to assess the impact of aging‐related variables on clinical management, prognosis, and functional status in elderly patients with ACS. A series of 500 consecutive octogenarian patients with non–ST‐segment elevation ACS from 57 centers in Spain will be included. A comprehensive geriatric assessment will be performed during the admission, assessing functional status (Barthel Index, Lawton‐Brody Index), frailty (FRAIL scale, Short Physical Performance Battery), comorbidity (Charlson Index), nutritional status (Mini Nutritional Assessment–Short Form), and quality of life (Seattle Angina Questionnaire). Patients will be managed according to current recommendations. The primary outcome will be the description of mortality and its causes at 6 months. Secondary outcomes will be changes in functional status and quality of life. Results from this study might significantly improve the knowledge about the impact of aging‐related variables on management and outcomes of elderly patients with ACS. Clinical management of these patients has become a major health care problem due to the growing incidence of ACS in the elderly and its particularities.
Introduction
The progressive aging of the population and the high incidence of acute coronary syndromes (ACS) in the elderly point to a marked increase in the number of elderly patients admitted for ACS in the coming years.1, 2 In addition, comorbidities and frailty are common in this clinical setting and are associated with higher rates of complications and consumption of health care resources.3, 4, 5 Non–ST‐segment elevation ACS (NSTEACS) is the most common form of presentation in the elderly. Clinical evidence on the optimal management of NSTEACS in the elderly is scarce.6 These patients are underrepresented in clinical trials,7, 8 and the few elderly patients included in these trials have significantly different characteristics from the real‐life elderly population. Moreover, information on the impact of aging‐related conditions on management and prognosis in elderly patients with ACS is scarce.
Therefore, the purpose of the LONGEVO‐SCA registry (Impacto de la Fragilidad y Otros Síndromes Geriátricos en el Manejo y Pronóstico Vital del Anciano con Síndrome Coronario Agudo sin Elevación de Segmento ST) is to assess the characteristics of an unselected cohort of elderly patients with NSTEACS, performing a comprehensive geriatric assessment during hospitalization and assessing the association between these factors and clinical management, mid term mortality and functional outcomes of these patients.
Methods
Design and Study Population
This is a prospective, multicenter, and observational registry to be conducted at 57 Spanish hospitals. This initiative has been endorsed by the Geriatric Cardiology Section of the Spanish Society of Cardiology. This registry will be coordinated by the team of Bellvitge University Hospital (L'Hospitalet de Llobregat, Barcelona, Spain). This registry will include consecutive patients age ≥80 years admitted for NSTEACS, defined as the presence of chest pain consistent with ACS and 1 or both of the following conditions: (1) electrocardiographic (ECG) changes suggestive of myocardial ischemia (appearance of negative T‐wave or ST‐segment depression), and (2) elevated markers of myocardial damage (troponin or CK‐MB above the reference value of each laboratory). Signed informed consent by the patient (or a representative in cases of cognitive impairment) will be required. Patients fulfilling the inclusion criteria will be included regardless the area of the hospital where they are admitted and the clinical specialist assigned to their management. Patient refusal to participate in the registry and the impossibility of obtaining the geriatric tests will be considered exclusion criteria. Although distinguishing this situation in routine clinical practice may be sometimes difficult, patients with severe comorbidities will only be excluded if symptoms of myocardial ischemia are clearly triggered only by other conditions such as acute anemia, severe decompensated respiratory insufficiency, active infectious diseases, or severe coexisting valvular disease (type 2 myocardial infarction).
Antithrombotic treatment and performance of coronary angiography will be up to each medical team according to current recommendations. If coronary angiography is performed, vascular access, antithrombotic drugs, and the choice of stents and other devices will be left to the operator's decision.
The primary endpoint of the study will be the description of the contribution of frailty and other geriatric syndromes to all‐cause mortality at 6 months, as well as its specific causes and associated factors. Secondary objectives will be the description of the evolution of functional capacity and quality of life at 6 months (Figure 1).
Figure 1.
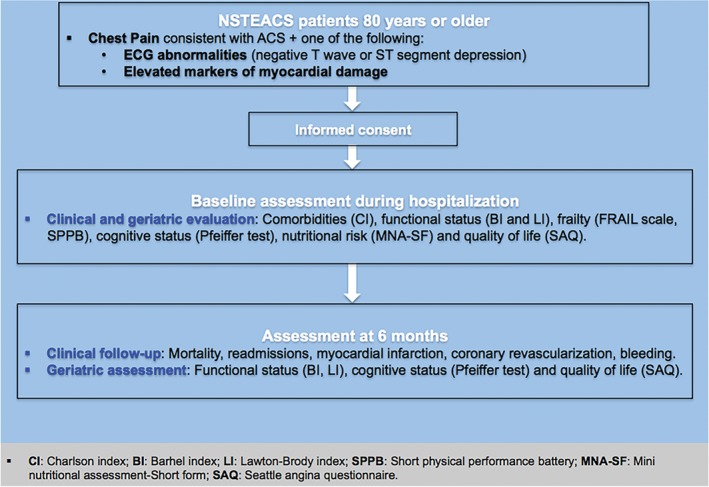
Design of the LONGEVO‐SCA Registry. Abbreviations: ACS, acute coronary syndrome; BI, Barthel Index; CI, Charlson Comorbidity Index; ECG, electrocardiography; LI, Lawton‐Brody Index; LONGEVO‐SCA, Impacto de la Fragilidad y Otros Síndromes Geriátricos en el Manejo y Pronóstico Vital del Anciano con Síndrome Coronario Agudo sin Elevación de Segmento ST; MNA‐SF, Mini Nutritional Assessment–Short Form; NSTEACS, non–ST‐segment elevation acute coronary syndrome; SAQ, Seattle Angina Questionnaire; SPPB, Short Physical Performance Battery.
Data Collection
Data will be recorded prospectively by local investigators during the admission (for a list of study investigators, see Supporting Information, Appendix, in the online version of this article) using standardized case‐report forms. Demographics, baseline clinical features, ECG data, and echocardiographic, laboratory, and angiographic parameters will be collected. In‐hospital clinical outcome will be also collected, such as the need for invasive procedures and in‐hospital complications (bleeding and its location, need for blood transfusion, need for surgery, infectious complications requiring antibiotics, reinfarction, mechanical and arrhythmic complications, delirium, and hospital mortality).
Inclusion in the study will not imply any change in patients' clinical management. All patients or their representatives will give written informed consent before inclusion in the study. The design of this study has been approved by the Clinical Research Ethics Committee of Bellvitge University Hospital (IRB00005523).
Baseline Geriatric Assessment
The baseline geriatric assessment will be made during admission in all patients through interview with the patient and/or family/caregivers and referring to the patient's status prior to admission.
The functional capacity for basic activities of daily living will be assessed by the Barthel Index (BI).9, 10 This is an ordinal scale with a total score of 0 to 100, where the intermediate ranges help evaluate the different degrees of dependency: total (0–20), severe (21–40), moderate (41–60), light (61–90), and independent (>90). Instrumental activities will be evaluated with the Lawton‐Brody Index (LI).11 Cognitive status will be evaluated with the Pfeiffer test.12 Previous frailty will be assessed by the FRAIL scale,13 which includes the evaluation of fatigue, resistance, ambulation, concomitant diseases, and weight loss. After the acute clinical phase (once the patient is stabilized), the Short Physical Performance Battery will be carried out.14 This test includes balance in 3 positions (feet together, semi‐tandem, and tandem), walking speed (4 meters along), and getting up and sitting in a chair 5 times. The score is the sum of the 3 subtests, ranging from 0 (worst) to 12 (best). A score <10 indicates frailty and an increased risk of disability and falls.
For the evaluation of comorbidity, the Charlson Comorbidity Index15 will be applied, with a maximum score of 37 points. The number of medications with chronic prescription taken by the patient before admission also will be collected.
The nutritional risk assessment will be carried out with the Mini Nutritional Assessment–Short Form,16 whose value ranges from 0 to 14 points; scores <11 identify patients at risk of malnutrition.
Quality of life will be analyzed by the Seattle Angina Questionnaire (SAQ),17 designed for patients with stable ischemic heart disease but also applied in patients with acute coronary syndromes.18 It consists of 19 items assessing 5 key areas: frequency of episodes of angina, stability of angina, physical limitations, satisfaction with treatment, and disease perception. This questionnaire has shown adequate validity, reproducibility, and relationship with prognosis. The SAQ values range from 0 to 100; higher values indicate a lower burden of symptoms and higher quality of life.
Study Endpoints
The primary endpoint will be mortality and its causes after 6 months of follow‐up. The assignment of the cause of death will be based on clinical judgment of the physician taking care of the patient at the time of death. In cases of coexistence of ≥2 possible causes, the assignment will be performed taking into account the clinical relevance of each of those conditions and their contribution at the time of death. Death will be deemed cardiac when it is due to myocardial infarction, heart failure, or sudden death. All deaths will be centrally reviewed by the coordinating team in consensus with local researchers. The secondary endpoints will include: (1) rehospitalization and its causes, reinfarction, and the need for coronary revascularization; (2) bleeding complications, the requirement for blood transfusion, or stopping antithrombotic treatment during follow‐up; and (3) functional capacity (Barthel Index), instrumental activities (Lawton‐Brody Index), cognitive capacity (Pfeiffer), and quality of life (SAQ) at 6 months. Clinical follow‐up will be carried out by local investigators at 6 months, by medical visit, review of medical history, or telephone contact with the patient, family, or referring physician. The coordinating team will supervise the geriatric assessment during the recruitment period and assess the quality of data.
Sample‐Size Calculation
Little information exists about the impact of frailty and other geriatric syndromes on the clinical course of these patients, thus lacking enough data to allow precise measurement of sample size. Preliminary data from elderly ACS patients from our setting showed a 6‐month mortality of about 20%. Assuming these data, a sample size of 500 patients will enable a sufficient number of events to study the primary outcome of the study.
Statistical Analysis
Categorical variables will be expressed as numbers and percentages. Quantitative variables will be expressed as mean and SD. Quantitative variables with normal distribution will be expressed as median and interquartile range (25%–75%). Normal distribution of quantitative variables will be assessed by the Kolmogorov‐Smirnov test. For reference variables, the t test will be used for comparison of quantitative variables and the χ2 or Fisher exact test, as appropriate, will be used for categorical variables. The software used for the analysis is PASW Statistics, version 18 (SPSS Inc., Chicago, IL).
The relationship between geriatric variables and target variables will be assessed by Cox regression method, using mortality and secondary endpoints at 6 months as dependent variables, and each of the indexes specified as covariates along with other cardiac variables that have shown a statistical association with mortality with P < 0.20.
Exploratory analysis of mortality will also be made by means of Kaplan‐Meier curves for different values of the functional, cognitive, nutritional assessment, and comorbidity indexes mentioned previously.
In addition, a predictive model for 6‐month mortality will be also developed using the Cox regression method, trying to elucidate the predictive capacity of each of these indexes regarding the global model.
Furthermore, a descriptive analysis of possible changes in functional capacity and quality of life of patients in this clinical scenario will be performed. Finally, we will also perform exploratory analysis of baseline characteristics of patients suffering a significant functional decline or significant loss of quality of life during the study period.
Discussion
Cardiovascular disease is a major cause of morbidity and mortality in elderly patients. The incidence of ACS increases with age and is particularly high in the elderly.1 Furthermore, the presence of comorbidities and frailty is associated with higher rates of complications, prolonged hospital stay, and increased use of health care resources.3 Therefore, ACS in the elderly is becoming a major public health problem.
The most common form of presentation of ACS in the elderly is NSTEACS. Clinical practice guidelines recommend an early invasive stratification in most patients at intermediate to high risk. However, available information about the benefits of this strategy in the elderly is scarce.6 The elderly are underrepresented in clinical trials. Therefore, current recommendations19 emphasize the need to individualize patient treatment, taking into account their medical condition and comorbidities. It also emphasizes the importance of collecting information on conditions such as frailty, cognitive impairment, functional capacity, and quality of life.
Frailty is an emerging concept defined by vulnerability and functional impairment. During the last few years, different scales for the assessment of frailty have been described. Recent data suggest a high prevalence of frailty in elderly patients undergoing percutaneous coronary intervention20, 21 and in patients with NSTEACS.22 Other geriatric syndromes such as cognitive impairment and severe dependence are common among elderly patients hospitalized for acute heart diseases.4, 5, 23, 24 Several registries have shown that elderly patients often undergo conservative management.22, 25, 26 The presence of frailty and other geriatric syndromes has been suggested as a possible cause for this conservative strategy. Moreover, recent data have shown an association between geriatric syndromes and a worse prognosis in elderly patients with NSTEACS,27, 28, 29 which could be independent of the most commonly used prognostic markers.30, 31
Ekerstad et al22 described a population of 307 patients age ≥75 years from 3 centers, defining frailty according to the Canadian Study of Health and Aging Clinical Frailty Scale. Of 307 patients, 149 (48.5%) were considered frail. Frailty was found to be independently associated with risk for in‐hospital mortality (odds ratio: 4.6) and 1‐month mortality (odds ratio: 4.7). Graham et al26 assessed 183 consecutive patients age ≥65 years with ACS admitted to a single center in Canada. Frailty was defined by the Edmonton Frail Scale (EFS). Patients with higher EFS scores were older, with more comorbidities, longer lengths of stay, and decreased procedure use. After adjusting for baseline risk differences using a “burden of illness” score, the hazard ratio (HR) for mortality for EFS ≥7 compared with EFS 0 to 3 was 3.49 (P = 0.002). Sanchis et al29 studied 342 patients with ACS age >65 years, evaluating 5 geriatric conditions at hospital discharge: frailty (Fried and Green scores), physical disability (Barthel Index), instrumental disability (Lawton‐Brody Index), cognitive impairment (Pfeiffer questionnaire), and comorbidity (Charlson and simple comorbidity indexes). The outcomes were mortality and the composite of death/myocardial infarction during a 30‐month median follow‐up. Seventy‐four (22%) patients died and 105 (31%) suffered from the composite endpoint.
All individual geriatric indexes were associated with outcomes, mainly mortality. Of all of them, frailty using the Green score had the strongest discriminative accuracy (area under the receiver operating characteristic curve 0.76 for mortality). The incremental predictive information was even greater over the Global Registry of Acute Coronary Events (GRACE) score. More recently, White et al31 analyzed the impact of frailty as defined by the Fried score in 4996 patients age >65 years from the Targeted Platelet Inhibition to Clarify the Optimal Strategy to Medically Manage Acute Coronary Syndromes (TRILOGY‐ACS), designed to compare prasugrel vs clopidogrel in patients planned for medical management. In that study, 72.3% of patients were classified as not‐frail (0 items), 23.0% as pre‐frail (1–2 items), and 4.7% as frail (≥3 items). After adjustment for baseline characteristics and GRACE covariates, frailty remained independently associated with the primary endpoint: pre‐frail vs not‐frail HR: 1.33, P < 0.001; frail vs not‐frail HR: 1.52, P = 0.002.
However, little information exists about the optimal management of ACS in elderly patients with geriatric syndromes and its prognostic impact in this clinical setting. Although several more‐complex tools to assess frailty and other aging‐related variables have been previously described, for the performance of this study we chose simple validated clinical tools to ensure its full completion for all the investigators and the success of this initiative.
Conclusion
The results of the LONGEVO‐SCA registry might contribute to a better understanding of the impact of aging‐related variables on the prognosis of elderly patients with ACS, help define the role of a comprehensive geriatric assessment32 in these patients, and help to identify the best clinical management in the presence of frailty and other aging‐related variables in this clinical scenario. Improving clinical management of elderly patients with ACS has become an essential health care issue for the upcoming years.
Supporting information
Appendix S1: Study organization
Appendix S2: Inclusion and exclusion criteria
This registry has received funding from the Spanish Society of Cardiology as a Clinical Research Project.
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Gabriel R, Alonso M, Reviriego B, et al. Ten‐year fatal and non‐fatal myocardial infarction incidence in elderly populations in Spain: the EPICARDIAN cohort study. BMC Public Health. 2009;9:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dégano IR, Elosua R, Marrugat J. Epidemiology of acute coronary syndromes in Spain: estimation of the number of cases and trends from 2005 to 2049. Rev Esp Cardiol (Engl Ed). 2013;66:472–481. [DOI] [PubMed] [Google Scholar]
- 3. Khandelwal D, Goel A, Kumar U, et al. Frailty is associated with longer hospital stay and increased mortality in hospitalized older patients. J Nutr Health Aging. 2012;16:732–735. [DOI] [PubMed] [Google Scholar]
- 4. Sánchez E, Vidán MT, Serra JA, et al. Prevalence of geriatric syndromes and impact on clinical and functional outcomes in older patients with acute cardiac diseases. Heart. 2011;97:1602–1606. [DOI] [PubMed] [Google Scholar]
- 5. Noriega FJ, Vidán MT, Sánchez E, et al. Incidence and impact of delirium on clinical and functional outcomes in older patients hospitalized for acute cardiac diseases. Am Heart J. 2015;170:938–944. [DOI] [PubMed] [Google Scholar]
- 6. Savonitto S, Cavallini C, Petronio AS, et al; Italian Elderly ACS Trial Investigators . Early aggressive versus initially conservative treatment in elderly patients with non–ST‐segment elevation acute coronary syndrome: a randomized controlled trial. JACC Cardiovasc Interv. 2012;5:906–916. [DOI] [PubMed] [Google Scholar]
- 7. Lee PY, Alexander KP, Hammill BG, et al. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708–713. [DOI] [PubMed] [Google Scholar]
- 8. Krumholz HM, Gross CP, Peterson ED, et al. Is there evidence of implicit exclusion criteria for elderly subjects in randomized trials? Evidence from the GUSTO‐1 study. Am Heart J. 2003;146:839–847. [DOI] [PubMed] [Google Scholar]
- 9. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Maryland State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 10. Formiga F, Ortega C, Cabot C, et al. Interobserver concordance in functional assessment by Barthel Index [article in Spanish]. Rev Clin Esp. 2006;206:230–232. [DOI] [PubMed] [Google Scholar]
- 11. Lawton MP, Brody EM. Assessment of older people: self‐maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 12. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. [DOI] [PubMed] [Google Scholar]
- 13. Abellan van Kan G, Rolland Y, Bergman H, et al. The I.A.N.A. Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12:29–37. [DOI] [PubMed] [Google Scholar]
- 14. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–M231. [DOI] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 16. Rubenstein LZ, Harker JO, Salvà A, et al. Screening for undernutrition in geriatric practice: developing the short‐form mini‐nutritional assessment. J Gerontol A Biol Sci Med Sci. 2001;56A:M366–M372. [DOI] [PubMed] [Google Scholar]
- 17. Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25:333–341. [DOI] [PubMed] [Google Scholar]
- 18. Maddox TM, Reid KJ, Rumsfeld JS, et al. One‐year health status outcomes of unstable angina versus myocardial infarction: a prospective, observational cohort study of ACS survivors. BMC Cardiovasc Disord. 2007;7:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Alexander KP, Newby LK, Cannon CP, et al; American Heart Association Council on Clinical Cardiology, Society of Geriatric Cardiology . Acute coronary care in the elderly, part I: non–ST‐segment elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115:2549–2569. [DOI] [PubMed] [Google Scholar]
- 20. Gharacholou SM, Roger VL, Lennon RJ, et al. Comparison of frail patients versus non frail patients ≥65 years of age undergoing percutaneous coronary intervention. Am J Cardiol. 2012;109:1569–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Murali‐Krishnan R, Iqbal J, Rowe R, et al. Impact of frailty on outcomes after percutaneous coronary intervention: a prospective cohort study. Open Heart. 2015;2:e000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ekerstad N, Swahn E, Janzon M, et al. Frailty is independently associated with short‐term outcomes for elderly patients with non–ST‐segment elevation myocardial infarction. Circulation. 2011;124:2397–2404. [DOI] [PubMed] [Google Scholar]
- 23. Vidán MT, Sánchez E, Fernández‐Avilés F, et al. FRAIL‐HF, a study to evaluate the clinical complexity of heart failure in nondependent older patients: rationale, methods and baseline characteristics. Clin Cardiol. 2014;37:725–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moretti C, Quadri G, D'Ascenzo F, et al. THE STORM (acute coronary Syndrome in paTients end Of life and Risk assesMent) study. Emerg Med J. 2016;33:10–16. [DOI] [PubMed] [Google Scholar]
- 25. Ferreira‐González I, Permanyer‐Miralda G, Marrugat J, et al; MASCARA study research team . MASCARA (Manejo del Síndrome Coronario Agudo. Registro Actualizado) study: general findings [article in English, Spanish; published correction appears in Rev Esp Cardiol. 2008;61:1228]. Rev Esp Cardiol. 2008;61:803–816. [PubMed] [Google Scholar]
- 26. Graham MM, Galbraith PD, O'Neill D, et al. Frailty and outcome in elderly patients with acute coronary syndrome. Can J Cardiol. 2013;29:1610–1615. [DOI] [PubMed] [Google Scholar]
- 27. Landi F, Cruz‐Jentoft AJ, Liperoti R, et al. Sarcopenia and mortality risk in frail older persons aged 80 years and older: results from iISIRENTE study. Age Ageing. 2013;42:203–209. [DOI] [PubMed] [Google Scholar]
- 28. Singh M, Rihal CS, Lennon RJ, et al. Influence of frailty and health status on outcomes in patients with coronary disease undergoing percutaneous revascularization. Circ Cardiovasc Qual Outcomes. 2011;4:496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sanchis J, Bonanad C, Ruiz V, et al. Frailty and other geriatric conditions for risk stratification of older patients with acute coronary syndrome. Am Heart J. 2014;168:784–791. [DOI] [PubMed] [Google Scholar]
- 30. Sanchis J, Núñez E, Ruiz V, et al. Usefulness of clinical data and biomarkers for the identification of frailty after acute coronary syndromes. Can J Cardiol. 2015;31:1462–1468. [DOI] [PubMed] [Google Scholar]
- 31. White HD, Westerhout CM, Alexander KP, et al; TRILOGY ACS Investigators . Frailty is associated with worse outcomes in non–ST‐segment elevation acute coronary syndromes: insights from the Targeted Platelet Inhibition to Clarify the Optimal Strategy to Medically Manage Acute Coronary Syndromes (TRILOGY ACS) trial. Eur Heart J Acute Cardiovasc Care. 2015;pii:2048872615581502. [DOI] [PubMed] [Google Scholar]
- 32. Ariza‐Solé A, Formiga F, Vidán MT, et al. Impact of frailty and functional status on outcomes in elderly patients with ST‐segment elevation myocardial infarction undergoing primary angioplasty: rationale and design of the IFFANIAM study. Clin Cardiol. 2013;36:565–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Study organization
Appendix S2: Inclusion and exclusion criteria


