ABSTRACT
There is increasing evidence that mental stress can manifest as physical diseases. One such condition is mental stress–induced myocardial ischemia (MSIMI); a silent, transient, myocardial ischemic response to stressful conditions. We propose that the cardiac microvasculature may be an important site for the interplay between mental stress and MSIMI. This study is a review of the literature discussing the prevalence and emerging mechanisms underlying MSIMI. We identified several aspects underlying MSIMI, including psychological, genetic, and physiological causes. Several sources suggested that dysfunctional cardiac microvasculature might be a contributing factor in the development of stress‐induced myocardial ischemia. The literature also suggested that although MSIMI has distinct features and pathophysiology, its occurrence might indicate an increased future risk of cardiovascular events. We found that dysfunctional cardiac microvasculature may be the key point of interaction between mental stress and transient myocardial ischemia and that the development of MSIMI might be a “silent” indicator for future cardiac events.
Introduction
The prevalence of both stress‐related psychological conditions and cardiovascular disease (CVD) is high in many countries. In addition to traditional risk factors, there is evidence that elements of the modern city lifestyle may confer risk for CVD. Although these lifestyle factors are not well‐defined, and may also be related to healthcare provision, there is evidence for synergy between stress‐related psychological conditions and the development of vascular disease,1, 2 suggesting that stress is an independent risk factor. Understanding the interplay between these 2 conditions will be important in reducing overall morbidity and mortality in modern health care systems. This review describes what is currently known about the prevalence and mechanisms of mental stress–induced myocardial ischemia (MSIMI), a transient myocardial ischemic response to mental stress, with emphasis on evidence suggesting that the microvasculature is the key site of interplay between stressful emotions and CVD.
Incidence of Mental Stress–Induced Myocardial Ischemia
Mental stress–induced myocardial ischemia has strong clinical and prognostic similarities to exercise‐ or pharmacology‐induced myocardial ischemia during standard cardiac testing.3 Although observed in some patients with normal coronary angiograms,4 MSIMI is much more common among patients with coronary heart disease (CHD), both in obstructive and nonobstructive forms. Mental stress has been shown to closely correlate with myocardial ischemia measured in daily life by ambulatory monitoring, with MSIMI associated with a 2‐fold increased risk of future cardiac events independent of physical stress–induced ischemia in patients with stable CHD.5, 6 It has been demonstrated that MSIMI is predominantly related to the degree of microvascular constriction, and not the angiographic burden of CHD,7 strongly suggesting that the condition is related to the interplay between emotion and the microvasculature. A summary of our review is depicted in the Figure 1, with the details of key published papers in the Table 1.
Figure 1.
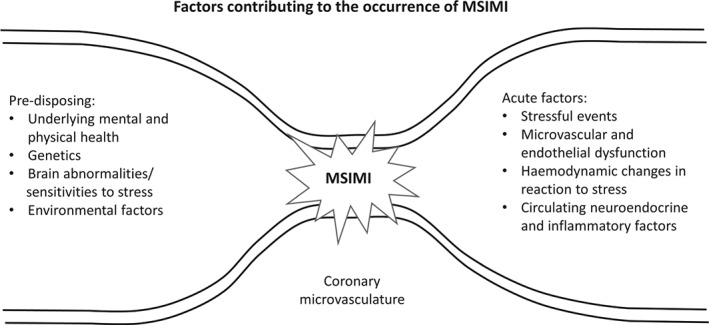
Factors contributing to the occurrence of MSIMI. Abbreviations: MSIMI, mental stress–induced myocardial ischemia.
Table 1.
Summary of Key Publications
| Publication | Study Design | Key Findings |
|---|---|---|
| Peix et al, 2006 | Tc‐99 m myocardial scintigraphy (exercise stress/mental stress protocol), brachial artery endothelial function measurement by ultrasonography, and 24‐hour ambulatory ECG recording (Holter) in 19 postmenopausal women with typical angina (n = 6) and normal coronary angiography (n = 10). | Patients with typical angina exhibited endothelial dysfunction more frequently than those without (83% vs 20%). |
| Exercise‐ and mental stress–induced ischemia was observed in 6 patients with angina. | ||
| Wei et al, 2014 | Systematic review and meta‐analysis of 5 prospective studies, examining the association between MSIMI and adverse outcome events in patients with stable CAD (n = 555). | MSIMI was associated with a 2× increased risk of a combined endpoint of cardiac events or total mortality (RR: 2.24, 95% CI: 1.59‐3.15). No heterogeneity was detected among the studies (Q = 0.39, I2 = 0.0%, P = 0.98). |
| Ramadan et al, 2013 | Tc‐99 m myocardial scintigraphy (exercise stress/mental stress protocol) and peripheral arterial tonometry in patients with CAD (n = 384). | Disease scores were not significantly associated with MSIMI. |
| Peripheral vascular tone was lower in those with MSIMI (0.55 ± 0.36 vs 0.76 ± 0.52; P = 0.009). | ||
| Multivariable analysis showed peripheral arterial tonometry ratio to be the only independent predictor of MSIMI (P = 0.009), whereas angiographic severity and extent of CAD independently predicted PSIMI. | ||
| Gale et al, 2014 | Interviews and historical registry data for 1 107 524 conscripted Swedish men. | Age‐adjusted HRs for CHD (95% CIs) at conscription were 1.30 (1.05‐1.62) for depressive disorders and 1.90 (1.58‐2.38) for alcohol‐related disorders. |
| Roest et al, 2013 | Secondary analysis on data from the ENRICHD trial comprising 1254 patients who had suffered an MI. | At 6 months, HR showed that positive changes (per 1‐point increase) in somatic depressive symptoms (0.95, 95% CI: 0.92‐0.98, P = 0.001) were related to a reduced risk of recurrent MI and mortality after adjustment for baseline depression scores. |
| Jiang et al, 2013 | Randomized, double‐blind, placebo‐controlled trial of 127 patients with clinically stable CHD and laboratory‐diagnosed MSIMI, receiving escitalopram (titrated to 20 mg/d) vs placebo treatment for 6 weeks. | 34.2% patients taking escitalopram vs 17.5% taking placebo had an absence of MSIMI during the 3 mental‐stressor tasks. (OR: 2.62, 95% CI: 1.06‐6.44) |
| Hassan et al, 2008 | Assessment of the association between β‐1 adrenergic receptor polymorphisms and perfusion defects in 148 patients with CAD | MSIMI occurred 3× more frequently among homozygous Ser49 allele carriers compared with the Gly49 allele carriers (P = 0.02). (Adjusted OR: 3.9, 95% CI: 1.2‐12.5, P = 0.02) |
| L'Abbate et al, 1991 | Assessment of MSIMI in 63 patients with a history of ischemia; 13 underwent angiography. | 44% of patients showed ECG indications of MSIMI; the majority experienced angina both at rest and during exercise. |
| Rate‐pressure product values suggested that ischemia was due to increased myocardial oxygen demand. | ||
| Lazzarino et al, 2013 | Salivary cortisol response to mental stress, plasma Tn concentration, and assessment of coronary calcification in 508 disease‐free participants. | Robust association between cortisol response and detectable Tn (OR: 3.98, 95% CI: 1.60‐9.92, P = 0.003). This association was independent of coronary calcification. |
| Lambert et al, 2010 | Pattern of sympathetic nervous firing in 8 women and 17 men with the metabolic syndrome and elevated BP in relation to their underlying psychological stress. | Single‐unit sympathetic nerve‐firing pattern correlated with anxiety state and trait and the affective component of the BDI score. In particular, higher trait anxiety score (OR: 0.557, P = 0.004) and higher affective depressive symptoms (0.517, P = 0.008). |
| Carroll et al, 2012 | Association between systolic and diastolic BP reactions to stress and CVD mortality in 431 Scottish participants followed for up to 16 years. | BP reactions were positively associated with future CVD mortality. |
| Kupper et al, 2015 | MSIMI assessment in 100 patients with systolic HF. | Over a median follow‐up period of 48.5 months, mortality rates were 2× higher (HR: 2.04, 95%CI: 1.15‐3.60, P = 0.014) among patients with the lowest diastolic responses (mean = −2.4 ± 5.4 mm Hg) to mental stress than among those patients with an intermediate diastolic BP response (mean = 7.3 ± 2.5 mm Hg). High diastolic responses were not related to mortality. |
| Similar results were observed for systolic BP but were not significant. | ||
| High heart rate response (≥6.3 bpm) to acute mental stress was associated with a reduced mortality risk (0.40, 95% CI: 0.16‐1.00, P = 0.051) compared with patients with intermediate responses. | ||
| Gulati et al, 2009 | Comparison of 540 symptomatic women with obstructive CAD from the WISE study and 100 matched asymptomatic women with no history of heart disease from the St. James WTH Project. | 5‐year annualized event rates for cardiovascular events were 16.0% in WISE women with nonobstructive CAD, 7.9% in WISE women with normal coronary arteries, and 2.4% in asymptomatic WTH women (P ≤ 0.002). |
Abbreviations: BDI, Beck Depression Inventory; BP, blood pressure; CAD, coronary artery disease; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; ECG, electrocardiographic; ENRICHD, Enhancing Recovery in Coronary Heart Disease; HF, heart failure; HR, hazard ratio; MI, myocardial infarction; MSIMI, mental stress–induced myocardial ischemia; OR, odds ratio; RR, relative risk; Tc, technetium; Tn, troponin; WISE, Women's Ischemia Syndrome Evaluation; WTH, Women Take Heart.
As most MSIMI is silent, most research is conducted using provoked events, similar to the more commonly used exercise testing but instead using mental challenges (including psychological testing scales and mental stress tests such as mental arithmetic testing, memories of public speaking, mirror drawing tests). The characteristic transient ischemia of MSIMI is then assessed using electrocardiograms, echocartography, radionuclide ventriculography, or positron emission tomography.
Causes of Mental Stress–Induced Myocardial Ischemia
Psychological Causes
The acute effects of emotion on physiology are clearly experienced by all; however, the longer‐term implications for chronic‐disease pathophysiology are not so well known. In the past 40 years, more than 60 clinical studies and meta‐analyses have established a strong link between depression and increased cardiovascular morbidity and mortality.8 Several epidemiological surveys have shown that patients with chronic mental disorders are at increased risk of CVD,2, 9 suggesting that other emotions may also confer cardiovascular risk. Most mental conditions are associated with increased stress. Individuals have different thresholds for expressing emotions, and for experiencing stress, so that the risk of a cardiovascular event may depend on a combination of the scenario, the individual's cardiovascular health, and on his or her unique mental outlook.
Antidepressant therapy has been suggested as a potential way to improve the long‐term prognosis for patients with CHD,10 but it also prevents approximately 40% of MSIMI,11 suggesting a link between mental and physical health. Equipping patients with better mental coping mechanisms may therefore reduce the cardiovascular risk associated with stressful scenarios without the need for pharmacological interventions.
Genetic Causes
When challenged by the same stimuli, some people might react strongly and others might not react at all. One of the possible mechanisms that underlies different reactions is genetics. For example, patients with a specific polymorphism of the β‐1 adrenergic receptor have been shown to be 3× more likely to have MSIMI than those carrying an alternative allele,12 and expression of a specific serotonin receptor allele in the brain has been shown to increase an individual's reactivity to emotional stress.13
Pathology and Clinical Manifestations of Mental Stress–Induced Myocardial Ischemia
Hemodynamic Changes Associated With Mental Stress
We have all experienced the hemodynamic response associated with mental stress. This typically involves increases in heart rate, blood pressure, systemic vascular resistance, or cardiac output, but it can also lead to damages to vagal tone, impaired endothelial function, and exaggerated peripheral microvascular and coronary artery tone.7, 14 Because myocardial ischemia can be caused by either a reduction in oxygen supply or an increase in demand, one possibility is that MSIMI is sustained by the same hemodynamic mechanisms that underlie physical stress–induced ischemia (ie, elevated myocardial oxygen demand and raised levels of toxic byproducts). However, there are fundamental differences in the mental and exercise‐induced hemodynamic responses. Mental stress is associated with elevated epinephrine in the blood and increased peripheral resistance, whereas responses initiated during exercise have no relationship with catecholamine levels and conversely feature a reduction in systemic resistance.15 Furthermore, many studies have demonstrated that MSIMI occurs at a lower rate‐pressure product than exercise‐induced ischemia in the same individual patient, whereas others show left ventricular ejection fraction depression to be greater with MSIMI than with exercise‐induced ischemia, which was inversely correlated with systemic resistance.16
Proposed Mechanisms Contributing to Mental Stress–Induced Myocardial Ischemia
Hyperactivity of the Hypothalamic‐Pituitary‐Adrenocortical Axis
The hypothalamic‐pituitary‐adrenocortical (HPA) axis is an important region of the brain for initiating the fight‐or‐flight response. Mental stress causes the release of corticotrophin releasing factors from the hypothalamus, initiating cortisol release from the adrenal glands into the systemic circulation. Cortisol and corticotrophin releasing factors both have numerous systemic effects, including modulation of the inflammatory response and platelet function, as well as increases in blood pressure.17 Hyperactivity of the HPA axis is one of the most consistently proposed links between brain abnormalities and MSIMI.18, 19 Antonio et al20 found that heightened cortisol responses to mental stress were associated with detectable levels of cardiac troponin T in the plasma of healthy people, suggesting that damage to cardiac muscle can be caused by stress. Additionally, another study showed that stress‐related endothelial dysfunction and impairment of baroreceptor pressure sensitivity can both be prevented by blocking cortisol production, demonstrating a direct role for cortisol in stress‐related changes in cardiovascular functions of relevance to MSIMI.21 Furthermore, in healthy older participants, without history or objective signs of CHD, heightened cortisol reactivity is associated with a greater extent of coronary artery calcification score,22 supporting the notion that heightened HPA activity is also a risk factor for the future development of CHD.
Sympathetic Nervous System Stimulation
Mental stress is associated with activation of the sympathetic nervous system. Through sympathetic nerve actions and the release of catecholamines, the sympathetic‐adrenal system is largely responsible for the increases in heart rate, blood pressure, ventricular contractility, vascular resistance, and the increased risk of arrhythmias during periods of acute mental stress.23 Interestingly, in patients with metabolic syndrome and hypertension thought to be due to underlying psychological stress, a higher incidence of multiple sympathetic nerve firing was associated with an increased incidence of affective depressive symptoms, suggesting a link between depression and increased autonomic tone.24 Other studies have suggested that higher autonomic reactivity in response to stress stimuli is a risk factor for the development of hypertension and other cardiovascular diseases.25
The hyperactivation of the sympathetic nervous system during mental stress also plays an important pro‐inflammatory role, working through α‐2 receptors to increase production of TNF‐α, which can further provoke the release of endothelin‐1 from macrophages and synergistically promote vasoconstriction.26 Inflammation is also a contributor toward atherosclerotic plaque rupture, coronary artery vasospasm, and ischemic injury.27
Microcirculatory Dysfunction
The systemic biological responses to mental stress are coordinated largely through neuroendocrine signals. The heart itself possesses endocrine functions,28 secreting various peptides including atrial natriuretic peptides, brain natriuretic peptides, troponins, and others, upon stimulation. These substances can regulate many aspects of circulatory and metabolic systems. The microvasculature expresses many receptors for neuroendocrine signals, such as for angiotensin II, natriuretics, cytokines, endothelin, and other vasoactive peptides such as catecholamines. The function of myocardial arterioles is to regulate blood flow to the capillaries, and their tone can be modulated by numerous blood‐borne factors. Serotonin is one such substance, which also has strong links to mental health, being altered in depression and by therapies for depression, and a vasoconstrictor in myocardial arterioles.
In 2013, the European Society of Cardiology (ESC) guidelines noted that stable CHD not only included patients with atherosclerotic stenosis, but must also consider those with chest symptoms induced by exercise or mental stress resulting from microvascular dysfunction and coronary artery spasm.29 Therefore, MSIMI can exist in both obstructive CHD and nonobstructive CHD. Some patients experiencing chest pain but with no abnormal coronary angiography findings may have slow blood flow resulting from microvascular dysfunction. In these patients, microvasculature dysfunction may be the first sign of developing CHD, occurring before structural changes in the coronary arteries.30, 31
Endothelial Dysfunction
The endothelium plays an important role in the control of vascular tone. Endothelial dysfunction is a potential mechanism linking mental stress to end‐organ damage and CVD. Stress‐related endothelial dysfunction is a risk factor for cardiovascular disorders, with recent studies supporting the idea that acute mental stress negatively affects endothelial function.32 The degree of mental stress–induced endothelial dysfunction correlates with changes in the systemic vascular resistance response,33 which in turn correlates with decreases in ejection fraction and myocardial ischemia.15 Thus, endothelial dysfunction can be considered to be proportional to mental stress. Impaired endothelial function has been transiently observed for up to 1.5 hours following mental stress, and such periods of impairment could accumulate to become clinically relevant over the long term.32
Although the action of adrenaline on β‐2 receptors usually drives nitric oxide–mediated coronary vasodilation, during endothelial dysfunction this response can be diminished, leading to inadequate coronary perfusion.34 Stress hormones such as glucocorticoids, pro‐inflammatory cytokines, and endothelin‐1 are systemically liberated in response to mental stress and may participate in the development of endothelial dysfunction. The main features of endothelial dysfunction are impaired vasodilation, impaired inhibition of platelet aggregation, and thrombus formation.15 A possible mechanism may be via chronic catecholamine‐ or corticotropin‐releasing hormone–induced blood pressure elevation and downregulation of endothelial nitric oxide production and vasodilator sensitivity.23, 24 Increased microvessel tone can directly lead to myocardial ischemia through vessel narrowing and reduced perfusion. Systemic vasoconstriction (an increase in systemic vascular resistance) also increases afterload, therefore increasing myocardial activity and oxygen demand. Uninhibited platelet aggregation and thrombosis can also precipitate myocardial ischemia or myocardial infarction. An example of the acute effects of mental stress could be following the 1995 Hanshin‐Awaji earthquake, when a higher incidence of elevated blood pressure, endothelial injury, and increased blood viscosity due to high hematocrit and fibrinogen levels coincided with increased rates of myocardial infarction and cardiovascular deaths.16 As endothelial dysfunction can be a progressive condition, associated with coronary artery atherosclerosis, this may help to explain the greater impact of dramatic sporting events on older individuals with known CHD.
Clinical Implications
Studies suggest that pronounced hemodynamic responses to mental stress are linked to poorer patient prognosis. For example, Carroll et al35 examined the association between the magnitude of systolic and diastolic blood pressure reactions to mental arithmetic stress and cardiovascular disease mortality in 431 Scottish participants. Both systolic and diastolic blood pressure reactions were positively associated with CVD mortality. This association could reflect the long‐term erosive effects of exaggerated hemodynamic reactivity on the vasculature, as well as its short‐term capacity to trigger acute cardiovascular events. However, Kupper et al36 conversely reported that limited diastolic blood pressure reactivity to mental stress is independently associated with all‐cause mortality in patients with heart failure. Other studies have failed to find associations between MSIMI, blood pressure, or heart rate responses to mental stressors in patients with CHD or healthy volunteers.
Mental Stress and Nonobstructive Coronary Heart Disease
Nonobstructive CHD also involves myocardial ischemia; however, its ischemic features are different from those of obstructive CHD. Nonobstructive disease mainly consists of downstream microvascular changes. Microvascular dysfunction results in slowing of the blood flow in coronary arteries and reductions, in the intraluminal pressure. A particular feature of ischemia of nonobstructive coronary heart disease is punctate ischemia,37 which was also one of the main characteristics of MSIMI. Nonobstructive CHD also carries high risks for cardiovascular events, as demonstrated by comparison of cardiovascular events between 540 cases of female patients with suspected ischemia but without obstruction evidence from coronary angiography with 1000 cases of age‐matched asymptomatic females.38 It is noteworthy that although some study participants may not have had a coronary obstruction sufficient to cause left ventricular dysfunction with exercise stress or to warrant percutaneous intervention, they nonetheless developed left ventricular dysfunction with mental stress. Other studies have demonstrated significant decreases in myocardial blood flow during mental stress in coronary vessels without flow‐limiting atherosclerotic plaques, as well as significant coronary vasoconstriction in coronary segments with only minor obstruction.39, 40 Stress‐induced heart injury might therefore be a consequence of slow blood flow in coronary arteries, a phenomenon that is also called left ventricular ballooning syndrome or stress‐induced heart disease. These findings indicate that the nature of stress‐induced coronary obstruction is dynamic and occurs due to unique pathophysiological mechanisms. Future awareness of these mechanisms will be important for improving patient care, with stress‐coping techniques and mental‐stress tests having potential clinical value.
Conclusion
Mental stress affects the brain like a stressor, causing systemic release of signaling molecules. The response from the body is acutely beneficial; however, episodes of MSIMI can occur, and over the longer term they can work alongside other CVD risk factors to cause serious cardiovascular pathology. Few studies have described the mechanisms underlying MSIMI. Reviewing the evidence, we suggest that cardiac microcirculation is a key point of interaction between mental stress and cardiac ischemia. Pathological changes in the microcirculation likely act synergistically to those which occur systemically, further increasing the risk of MSIMI. In addition, patients with nonobstructive coronary artery diseases may experience MSIMI and transient coronary obstruction as a result of this microvascular and endothelial dysfunction. Further investigations are required to fully characterize the MSIMI phenomenon and its implications for cardiovascular health.
This work was supported by grant from Guangdong Provincial Department of Science and Technology, Guangdong Provincial Academy of Medicine joint research projects, Guangdong, People's Republic of China (grant number: 2011B032200006).
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Ormel J, von Korff M, Burger H, et al. Mental disorders among persons with heart disease—results from World Mental Health surveys. Gen Hosp Psychiatry. 2007;29:325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scott KM, de Jonge P, Alonso J, et al. Associations between DSM‐IV mental disorders and subsequent heart disease onset: beyond depression. Int J Cardiol. 2013;168:5293–5299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Strike PC, Steptoe A. Systematic review of mental stress–induced myocardial ischaemia. Eur Heart J. 2003;24:690–703. [DOI] [PubMed] [Google Scholar]
- 4. Peix A, Trápaga A, Asen L, et al. Mental stress–induced myocardial ischemia in women with angina and normal coronary angiograms. J Nucl Cardiol. 2006;13:507–513. [DOI] [PubMed] [Google Scholar]
- 5. Wei J, Rooks C, Ramadan R, et al. Meta‐analysis of mental stress–induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease. Am J Cardiol. 2014;114:187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Blumenthal JA, Jiang W, Waugh RA, et al. Mental stress–induced ischemia in the laboratory and ambulatory ischemia during daily life: association and hemodynamic features. Circulation. 1995;92:2102–2108. [DOI] [PubMed] [Google Scholar]
- 7. Ramadan R, Sheps D, Esteves F, et al. Myocardial ischemia during mental stress: role of coronary artery disease burden and vasomotion. J Am Heart Assoc. 2013;2:e000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zellweger MJ, Osterwalder RH, Langewitz W, et al. Coronary artery disease and depression. Eur Heart J. 2004;25:3–9. [DOI] [PubMed] [Google Scholar]
- 9. Gale CR, Batty GD, Osborn DP, et al. Mental disorders across the adult life course and future coronary heart disease: evidence for general susceptibility. Circulation. 2014;129:186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roest AM, Carney RM, Freedland KE, et al. Changes in cognitive versus somatic symptoms of depression and event‐free survival following acute myocardial infarction in the Enhancing Recovery In Coronary Heart Disease (ENRICHD) study. J Affect Disord. 2013;149:335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jiang W, Velazquez EJ, Kuchibhatla M, et al. Effect of escitalopram on mental stress‐induced myocardial ischemia: results of the REMIT trial. JAMA. 2013;309:2139–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hassan M, York KM, Li H, et al. Association of beta1‐adrenergic receptor genetic polymorphism with mental stress–induced myocardial ischemia in patients with coronary artery disease. Arch Intern Med. 2008;168:763–770. [DOI] [PubMed] [Google Scholar]
- 13. Hariri AR, Mattay VS, Tessitore A, et al. Serotonin transporter genetic variation and the response of the human amygdala. Science. 2002;297:400–403. [DOI] [PubMed] [Google Scholar]
- 14. Arrighi JA, Burg M, Cohen IS, et al. Myocardial blood‐flow response during mental stress in patients with coronary artery disease. Lancet. 2000;356:310–311. [DOI] [PubMed] [Google Scholar]
- 15. Goldberg AD, Becker LC, Bonsall R, et al. Ischemic, hemodynamic, and neurohormonal responses to mental and exercise stress: experience from the Psychophysiological Investigations of Myocardial Ischemia Study (PIMI). Circulation. 1996;94:2402–2409. [DOI] [PubMed] [Google Scholar]
- 16. L'Abbate A, Simonetti I, Carpeggiani C, et al. Coronary dynamics and mental arithmetic stress in humans. Circulation. 1991;83(4 suppl):II94–II99. [PubMed] [Google Scholar]
- 17. Wilbert‐Lampen U, Straube F, Trapp A, et al. Effects of corticotropin‐releasing hormone (CRH) on monocyte function, mediated by CRH‐receptor subtype R1 and R2: a potential link between mood disorders and endothelial dysfunction? J Cardiovasc Pharmacol. 2006;47:110–116. [DOI] [PubMed] [Google Scholar]
- 18. Inoue N. Stress and atherosclerotic cardiovascular disease. J Atheroscler Thromb. 2014;21:391–401. [DOI] [PubMed] [Google Scholar]
- 19. Neylon A, Canniffe C, Anand S, et al. A global perspective on psychosocial risk factors for cardiovascular disease. Prog Cardiovasc Dis. 2013;55:574–581. [DOI] [PubMed] [Google Scholar]
- 20. Lazzarino AI, Hamer M, Gaze D, et al. The association between cortisol response to mental stress and high‐sensitivity cardiac troponin T plasma concentration in healthy adults. J Am Coll Cardiol. 2013;62:1694–1701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Broadley AJ, Korszun A, Abdelaal E, et al. Inhibition of cortisol production with metyrapone prevents mental stress‐induced endothelial dysfunction and baroreflex impairment. J Am Coll Cardiol. 2005;46:344–350. [DOI] [PubMed] [Google Scholar]
- 22. Hamer M, O'Donnell K, Lahiri A, et al. Salivary cortisol responses to mental stress are associated with coronary artery calcification in healthy men and women. Eur Heart J. 2010;31:424–429. [DOI] [PubMed] [Google Scholar]
- 23. Kloner RA. Natural and unnatural triggers of myocardial infarction. Prog Cardiovasc Dis. 2006;48:285–300. [DOI] [PubMed] [Google Scholar]
- 24. Lambert E, Dawood T, Straznicky N, et al. Association between the sympathetic firing pattern and anxiety level in patients with the metabolic syndrome and elevated blood pressure. J Hypertens. 2010;28:543–550. [DOI] [PubMed] [Google Scholar]
- 25. Garafova A, Penesova A, Cizmarova E, et al. Cardiovascular and sympathetic responses to a mental stress task in young patients with hypertension and/or obesity. Physiol Res. 2014;(63 suppl 4):S459–S467. [DOI] [PubMed] [Google Scholar]
- 26. Woods M, Mitchell JA, Wood EG, et al. Endothelin‐1 is induced by cytokines in human vascular smooth muscle cells: evidence for intracellular endothelin‐converting enzyme. Mol Pharmacol. 1999;55:902–909. [PubMed] [Google Scholar]
- 27. Mizia‐Stec K, Gasior Z, Zahorska‐Markiewicz B, et al. Serum tumour necrosis factor‐alpha, interleukin‐2 and interleukin‐10 activation in stable angina and acute coronary syndromes. Coron Artery Dis. 2003;14:431–438. [DOI] [PubMed] [Google Scholar]
- 28. McGrath MF, de Bold ML, de Bold AJ. The endocrine function of the heart. Trends Endocrinol Metab. 2005;16:469–477. [DOI] [PubMed] [Google Scholar]
- 29. Montalescot G, Sechtem U, Achenbach S, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology [published correction appears in Eur Heart J. 2014;35:2260–2261]. Eur Heart J. 2013;34:2949–3003. [DOI] [PubMed] [Google Scholar]
- 30. Camici PG, d'Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. 2015;12:48–62. [DOI] [PubMed] [Google Scholar]
- 31. Kassab GS. Functional hierarchy of coronary circulation: direct evidence of a structure‐function relation. Am J Physiol Heart Circ Physiol. 2005;289:H2559–H2565. [DOI] [PubMed] [Google Scholar]
- 32. Poitras VJ, Pyke KE. The impact of acute mental stress on vascular endothelial function: evidence, mechanisms and importance. Int J Psychophysiol. 2013;88:124–135. [DOI] [PubMed] [Google Scholar]
- 33. Sherwood A, Johnson K, Blumenthal JA, et al. Endothelial function and hemodynamic responses during mental stress. Psychosom Med. 1999;61:365–370. [DOI] [PubMed] [Google Scholar]
- 34. Barbato E. Role of adrenergic receptors in human coronary vasomotion. Heart. 2009;95:603–608. [DOI] [PubMed] [Google Scholar]
- 35. Carroll D, Ginty AT, Der G, et al. Increased blood pressure reactions to acute mental stress are associated with 16‐year cardiovascular disease mortality. Psychophysiology. 2012;49:1444–1448. [DOI] [PubMed] [Google Scholar]
- 36. Kupper N, Denollet J, Widdershoven J, et al. Cardiovascular reactivity to mental stress and mortality in patients with heart failure. JACC Heart Fail. 2015;3:373–382. [DOI] [PubMed] [Google Scholar]
- 37. Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation. 2010;121:2317–2325. [DOI] [PubMed] [Google Scholar]
- 38. Gulati M, Cooper‐DeHoff RM, McClure C, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med. 2009;169:843–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yeung AC, Vekshtein VI, Krantz DS, et al. The effect of atherosclerosis on the vasomotor response of coronary arteries to mental stress. N Engl J Med. 1991;325:1551–1556. [DOI] [PubMed] [Google Scholar]
- 40. Kop WJ, Krantz DS, Howell RH, et al. Effects of mental stress on coronary epicardial vasomotion and flow velocity in coronary artery disease: relationship with hemodynamic stress responses. J Am Coll Cardiol. 2001;37:1359–1366. [DOI] [PubMed] [Google Scholar]


