Abstract
Background
Bronchiectasis is a long term respiratory condition with an increasing rate of diagnosis. It is associated with persistent symptoms, repeated infective exacerbations, and reduced quality of life, imposing a burden on individuals and healthcare systems. The main aims of therapeutic management are to reduce exacerbations and improve quality of life. Self‐management interventions are potentially important for empowering people with bronchiectasis to manage their condition more effectively and to seek care in a timely manner. Self‐management interventions are beneficial in the management of other airways diseases such as asthma and COPD (chronic obstructive pulmonary disease) and have been identified as a research priority for bronchiectasis.
Objectives
To assess the efficacy, cost‐effectiveness and adverse effects of self‐management interventions for adults and children with non‐cystic fibrosis bronchiectasis.
Search methods
We searched the Cochrane Airways Specialised Register of trials, clinical trials registers, reference lists of included studies and review articles, and relevant manufacturers’ websites up to 13 December 2017.
Selection criteria
We included all randomised controlled trials of any duration that included adults or children with a diagnosis of non‐cystic fibrosis bronchiectasis assessing self‐management interventions delivered in any form. Self‐management interventions included at least two of the following elements: patient education, airway clearance techniques, adherence to medication, exercise (including pulmonary rehabilitation) and action plans.
Data collection and analysis
Two review authors independently screened searches, extracted study characteristics and outcome data and assessed risk of bias for each included study. Primary outcomes were, health‐related quality of life, exacerbation frequency and serious adverse events. Secondary outcomes were the number of participants admitted to hospital on at least one occasion, lung function, symptoms, self‐efficacy and economic costs. We used a random effects model for analyses and standard Cochrane methods throughout.
Main results
Two studies with a total of 84 participants were included: a 12‐month RCT of early rehabilitation in adults of mean age 72 years conducted in two centres in England (UK) and a six‐month proof‐of‐concept RCT of an expert patient programme (EPP) in adults of mean age 60 years in a single regional respiratory centre in Northern Ireland (UK). The EPP was delivered in group format once a week for eight weeks using standardised EPP materials plus disease‐specific education including airway clearance techniques, dealing with symptoms, exacerbations, health promotion and available support. We did not find any studies that included children. Data aggregation was not possible and findings are reported narratively in the review.
For the primary outcomes, both studies reported health‐related quality of life, as measured by the St George's Respiratory Questionnaire (SGRQ), but there was no clear evidence of benefit. In one study, the mean SGRQ total scores were not significantly different at 6 weeks', 3 months' and 12 months' follow‐up (12 months mean difference (MD) ‐10.27, 95% confidence interval (CI) ‐45.15 to 24.61). In the second study there were no significant differences in SGRQ. Total scores were not significantly different between groups (six months, MD 3.20, 95% CI ‐6.64 to 13.04). We judged the evidence for this outcome as low or very low. Neither of the included studies reported data on exacerbations requiring antibiotics. For serious adverse events, one study reported more deaths in the intervention group compared to the control group, (intervention: 4 of 8, control: 2 of 12), though interpretation is limited by the low event rate and the small number of participants in each group.
For our secondary outcomes, there was no evidence of benefit in terms of frequency of hospital admissions or FEV1 L, based on very low‐quality evidence. One study reported self‐efficacy using the Chronic Disease Self‐Efficacy scale, which comprises 10 components. All scales showed significant benefit from the intervention but effects were only sustained to study endpoint on the Managing Depression scale. Further details are reported in the main review. Based on overall study quality, we judged this evidence as low quality. Neither study reported data on respiratory symptoms, economic costs or adverse events.
Authors' conclusions
There is insufficient evidence to determine whether self‐management interventions benefit people with bronchiectasis. In the absence of high‐quality evidence it is advisable that practitioners adhere to current international guidelines that advocate self‐management for people with bronchiectasis.
Future studies should aim to clearly define and justify the specific nature of self‐management, measure clinically important outcomes and include children as well as adults.
Plain language summary
Self‐management for non‐cystic fibrosis bronchiectasis
Background
Bronchiectasis is a respiratory condition that may occur in both children and adults and is being diagnosed with increasing frequency. It is a long‐term condition, where people have recurrent chest infections and symptoms that include cough, mucus production and recurrent flare‐ups (exacerbations) that reduce their quality of life. The main aims of management are to reduce the risk of flare‐ups using various treatments including antibiotics, inhalers and physiotherapy exercises. It is important for people/carers to stick to their treatments and self‐management strategies can help people to do this by teaching them about their condition, available treatments, exercise and what to do if their condition changes. The objective of the review is to assess the effectiveness and value for money of self‐management interventions for adults and children with non‐cystic fibrosis bronchiectasis.
Review question
We assessed the benefits and possible harms of self‐management strategies, including patient education, airway clearance techniques, education aimed at increasing adherence to medication, exercise (including pulmonary rehabilitation), and action plans for children and adults with bronchiectasis.
Study characteristics
We conducted a search on 13 December 2017 and found just two UK studies that included 84 participants, comparing a self‐management approach with normal care for adults with bronchiectasis. One study looked at the impact of an expert patient self‐management programme and the other, involving just a small number of participants with bronchiectasis, looked at self‐management in combination with exercises to improve lung function. Neither study included children.
Main results
Health‐related quality of life did not improve in either study. Although there were more deaths in the group receiving self‐management in one study, the numbers were very small and we do not know whether the difference is meaningful. The number of admissions to hospital, and lung function showed no benefit from self‐management. In one of the studies, people receiving self‐management felt more empowered to manage their condition. There was no information on the impact of self‐management on symptoms of bronchiectasis, adverse events or potential cost savings arising from more effective self‐management. There are no studies looking at self‐management in children.
Overall there is not enough information to assess whether strategies to support self‐management may help people with bronchiectasis and further studies are needed. Future studies will need to look at how often flare ups occur, how often antibiotics are prescribed, and how long for, whether people have a better quality of life, and the impact of self‐management on costs of care. It is also important to look at self‐management for bronchiectasis in children.
Quality of the results
This review is based on only two small trials and the quality of the studies is very poor. With only two studies looking at very specific approaches to self‐management we cannot say with any degree of certainty whether self‐management strategies work for people with bronchiectasis, but until further evidence is available we advocate adherence to current international guidelines that recommend self‐management for people with bronchiectasis.
Summary of findings
Background
Description of the condition
Bronchiectasis, also referred to as non‐cystic fibrosis (non‐CF) bronchiectasis, is a persistent respiratory condition characterised by abnormal dilation of the airways (Pasteur 2010; Chang 2015). Pathological processes include weakness and destruction of the structural components of the bronchial wall, which together with the loss of ciliated epithelium, and increase in number and hypertrophy of mucus‐secreting glands, causes mucus to accumulate, which in turn creates a conducive environment for bacteria and leads to a ‘vicious cycle’ of bacterial infection (Cole 1986), inflammatory mediator release, airway damage and further infection (Welsh 2015). Chronic infection is associated with a variety of pathogens (Martinez‐García 2007; Murray 2011; Chalmers 2012; Tunney 2013), contributing to persistent symptoms and repeated exacerbations (Murray 2011).
Causes of bronchiectasis include a wide range of factors such as damage by serious infection (including Mycobacterium tuberculosis), necrotising pneumonia, immune deficiency, allergic bronchopulmonary aspergillosis, and recurrent aspiration, although the majority of cases are idiopathic (Pasteur 2000; Goeminne 2012; Lonni 2015). Diagnosis is based on clinico‐radiographic assessments, requiring identification of one or more abnormally dilated bronchi using high‐resolution computerised tomography (HRCT) scanning and appropriate symptoms, including chronic productive or wet cough and recurrent lower respiratory tract infections, together with a range of other symptoms such as breathlessness, wheeze, chest pain (in stable patients) and lethargy (Pasteur 2010; Chang 2015). Factors associated with disease severity include frequency of hospital admissions and mortality, poor lung function, bacterial colonisation, high Medical Research Council (MRC) dyspnoea score and frequency of exacerbations (Chalmers 2014; Martinez‐García 2014). The impact on people's quality of life is significant and health status is poor with progressive deterioration. Severity may be assessed with tools such as the Bronchiectasis Severity Index (Chalmers 2014), or FACED (FEV1, Age, Chronic colonisation, Extension (number of lobes), Dyspnoea) (Martinez‐García 2014), to identify high‐risk individuals, though they have limited value as outcome measures because of the non‐modifiable nature of components such as lung function.
Estimates of the prevalence of bronchiectasis vary considerably. Although it has previously been considered a relatively rare disease (Kolbe 1996), more recent studies have suggested an increasing prevalence, particularly in those over 75 years (Weycker 2005), and higher prevalence rates in low‐income and middle‐income countries (Habesoglu 2011). Co‐morbidity may also influence detection and prevalence, with one UK study showing that 29% of people with COPD scanned by HRCT had bronchiectasis (O'Brien 2000). Prevalence rates per 100,000 were estimated at 0.5 in Finland and 3.7 in New Zealand though these data are more than 10 years old (European Lung White Book 2013). Higher prevalence rates have been observed in ethnic populations such as amongst indigenous Australians (up to 14 per 1000) and Native Alaskan children (up to 20.5 per 1000) (Singleton 2000; Chang 2002). Higher prevalence rates are also observed in women and people aged over 60 years (Chang 2003; Seitz 2012). Recent data suggest that incidence and prevalence in the UK may be higher than previously estimated (Quint 2016). Over a nine‐year period to 2013, point prevalence rates per 100,000 rose from 350.5 to 566.1 in women and from 301.2 to 485.5 in men. This reflects an increase of more than 60% with approximately 263,000 adults living with bronchiectasis in 2013. Similarly, the incidence rates per 100,000 person‐years rose from 21.2 to 35.2 in women and from 18.2 to 26.9 in men, a 63% increase in new cases to over 15,000 in 2013. However, these increases may be due to improved diagnosis resulting from easier access to high‐quality CT scanners, rather than a true rise in prevalence (Goeminne 2016).
Mortality rates for bronchiectasis in England and Wales rose by 3% per year between 2001 to 2007 (Roberts 2010), and hospitalisations also increased by 3% per year over a nine‐year period in the US (Seitz 2010). Average bronchiectasis mortality rates per 100,000 general population in Europe are estimated at 0.3 in 27 of the 28 countries in the EU (ranging from 0.01 in Germany to 1.18 in the UK) and 0.2 in nine non‐EU countries (ranging from 0.01 in Azerbaijan to 0.67 in Kyrgyzstan), based on 2005 to 2009 data (European Lung White Book 2013). The recent UK study reported higher age‐adjusted bronchiectasis mortality rates, with estimates 2.26 times higher in women and 2.14 times higher in men compared to the general population (Quint 2016).
The main aims of therapeutic management are: preservation of lung function, reduction of symptoms and exacerbations, minimising complications, and improvement in quality of life (Pasteur 2010; Saleh 2014; Chang 2015).
Description of the intervention
Taylor 2014 describes a taxonomy in which long‐term conditions are diagnosed and brought under control by professionals; thereafter the individual self‐manages the condition with support, to achieve stable maintenance. Self‐management support empowers the person with the condition by enabling them to modify treatment or behaviour, or to seek professional advice and has been defined as “increasing the capacity, confidence, and efficacy of the individual” (Kennedy 2013). Self‐management interventions are defined as structured programmes for individuals, designed to improve self‐health behaviours and self‐management skills (Lorig 2003). Self‐management programmes should ideally include training with feedback to improve problem solving, decision making, resource utilisation, formation of patient‐provider partnerships, action planning and self‐tailoring (Lorig 2003). People become more confident at managing their own health and this in turn supports the development and maintenance of beneficial health behaviours (Lorig 2003; Bourbeau 2004).
Self‐management support is delivered in a range of ways, all of which aim to equip the individual with knowledge, ability, and confidence, to take appropriate action. The support can take the form of specific techniques employed to help people choose healthy behaviours, but it can also be a fundamental alteration of the patient‐caregiver relationship into a collaborative partnership (de Silva 2011). Interventions can range from individualised support such as the provision of educational material, to larger but localised whole‐system approaches. An example of a whole‐system approach involved practitioners trained to offer a range of resources, such as a tool to assess the support needs of patients, guidebooks on self‐management, and a web‐based directory of local self‐management resources (Kennedy 2013). There are also extensive generic programmes such as the ‘Expert Patients Programme’ (Department of Health 2001).
Self‐management support increasingly includes a mutually agreed, individualised plan, which incorporates behavioural elements including goal setting and problem solving. Recent work conducted by the Richmond Group of Charities and The King's Fund suggests that clients and professionals should co‐create a personalised self‐management plan which could include patient and career education, medicines' management advice and support, use of telecare and telehealth to aid self‐monitoring, psychological interventions (e.g. coaching), telephone‐based health coaching, symptom management and patient access to their own records (Naylor 2015). Self‐management support and interventions can therefore vary significantly. All approaches aim to enable the individual to develop the knowledge and confidence to appropriately manage their long‐term condition, and to seek professional support when needed.
The components of self‐management programmes may need to be condition‐specific; for example, education may be particularly beneficial for diabetes, but cognitive and behavioural interventions may work well for people with depression (de Silva 2011). The principal aims of management in bronchiectasis are to maintain and improve pulmonary function and to improve quality of life by reducing symptoms and exacerbations (Pasteur 2010; Chang 2015). British Thoracic Society guidelines recommend a range of therapeutic strategies including physiotherapy for airway clearance, pulmonary rehabilitation for significant dyspnoea, bronchodilators for reversible airflow obstruction and a range of antibiotic therapy to reduce bacterial load. The latter may include short‐term courses for exacerbations, prophylactic therapy for frequent exacerbators (≥ 3 exacerbations requiring antibiotics per year) and combination therapy for people with multiple airway pathogens (Pasteur 2010). Recommendations are often based on a small number of short trials that are insufficient to draw firm conclusions about benefits and harms (Welsh 2015).
Bronchiectasis impacts upon physical and psychosocial well‐being and there is the potential to improve self‐management through self‐regulation of medication, adherence to airway clearance techniques and patient education about management of the condition (Wilson 1997; Lavery 2007). Current guidelines recommend airway clearance techniques, adherence to medication, action plans, exercise (including pulmonary rehabilitation), and patient education as potential components of self‐management interventions for bronchiectasis (Pasteur 2010; Chang 2015). The educational component focuses on understanding the basic principles of disease management and early recognition of an exacerbation to facilitate timely intervention (Pasteur 2010). In COPD, self‐management programmes that include action plans have been shown to accelerate appropriate treatment‐seeking behaviours (Walters 2010), and studies including action plans should therefore be considered separately.
How the intervention might work
Studies of long‐term chronic conditions suggest that self‐management support may improve self‐efficacy, health status, psychological well‐being, coping strategies and physical functioning (Farrell 2004; Griffiths 2005; Siu 2007; Challis 2010). Benefits may be attributable to enhanced adherence to medication, the adoption of appropriate behaviours, and reduced stress and anxiety, though this may also be associated with increased use of healthcare resources (Naylor 2015). Self‐management programmes for COPD, defined above, have improved quality of life and reduced breathlessness and hospital admissions (Zwerink 2014), though there is currently no consensus on the most effective components of self‐management interventions (Effing 2012). The evidence of effectiveness in cystic fibrosis is less clear, with interpretation of observed increases in knowledge and changes in behaviour hampered by small, poor‐quality trials (Savage 2014).
The objectives of care in bronchiectasis are to treat identifiable underlying causes, control symptoms, reduce the number of exacerbations, prevent deterioration in pulmonary function, improve quality of life and minimise complications (Pasteur 2010; Chalmers 2016). The potential benefits from self‐management in individuals with bronchiectasis may include: reduction in symptoms and subsequent improvement in quality of life; and reduction in the number and severity of exacerbations, together with potential reduction in hospital admissions, length of stay, and disease and health status decline.
Non‐adherence to therapy may be a significant problem in bronchiectasis with up to 50% of people with severe chest infections not completing prescribed courses of antibiotics, other medicines and airway clearance (McCullough 2014). People who do not adhere to therapy have a shorter time to first exacerbation (Haworth 2014); and a higher annual exacerbation rate compared to those who are adherent (McCullough 2014). Similar to reports from cystic fibrosis (Sawicki 2009), treatment burden may increase with the emergence of new treatments, which may in turn lead to more problems with adherence. Non‐adherence to antibiotic therapy and airway clearance procedures may be attributable to a range of factors including beliefs about their potential risks and benefits, a younger age and (for antibiotics) a higher number of prescribed medications (McCullough 2015). It is likely that patient self‐management programmes may help to improve adherence to prescribed therapy and reduce the negative consequences of poor adherence. With the rise of antimicrobial resistance, adherence to frontline antibiotic therapy may be particularly important for people with bronchiectasis (O'Neill 2016).
Why it is important to do this review
Bronchiectasis is a chronic disease which causes both persistent day‐to‐day symptoms such as cough and breathlessness, and intercurrent exacerbations. The long‐term management of bronchiectasis focuses on reducing these features of the disease.
Self‐management interventions have been shown to be beneficial in the management of other airways diseases associated with management of day‐to‐day respiratory symptoms and respiratory exacerbations such as asthma and COPD (Zwerink 2014; Peytremann‐Bridevaux 2015). Guidelines recommend self‐management plans for these diseases and patient education is one of the factors in bronchiectasis management recently prioritised by the European EMBARC group (Aliberti 2016).
This review aims to summarise the evidence for self‐management strategies for people with bronchiectasis and will seek to provide guidance for both current recommendations and possible future research needs.
Objectives
To assess the efficacy, cost‐effectiveness and adverse effects of self‐management interventions for adults and children with non‐cystic fibrosis bronchiectasis.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel and cluster‐randomised controlled trials (RCTs) of any duration. We included studies reported as full‐text, those published as abstract only, and unpublished data.
Types of participants
Adults (> 18 years) and children with a diagnosis of non‐cystic fibrosis bronchiectasis confirmed by plain film chest radiograph, bronchography or high‐resolution computed tomography with at least three months of daily sputum expectoration. We excluded participants with a diagnosis of cystic fibrosis (CF), sarcoidosis or active allergic bronchopulmonary aspergillosis. We also excluded studies of other long‐term health conditions unless results for people with bronchiectasis were reported separately.
Types of interventions
Self‐management interventions were defined as structured interventions for individuals with bronchiectasis designed to improve self‐health behaviours and self‐management skills. We specified that interventions should include collaborative interaction between participants and healthcare providers, involving goal setting and feedback, with at least two points of contact, and that specific programmes should include at least two of the following components: patient education, airway clearance techniques, adherence to medication, exercise (including pulmonary rehabilitation), and action plans (Pasteur 2010; Chang 2015). Self‐management interventions that included action plans were to be considered separately (Hagger 2014). We excluded interventions solely comprising participant education or those focused only on exercise, such as pulmonary rehabilitation delivered in a care setting. We included pulmonary rehabilitation interventions only when they explicitly included self‐management strategies within the programme. We included studies of self‐management interventions delivered in any form (e.g. Internet, mobile device, face‐to‐face, paper) with the following comparisons.
Self‐management versus usual care
Self‐management versus an alternate form of self‐management (e.g. paper‐based booklet versus mobile app)
For comparisons between different types of self‐management programmes we included co‐interventions, including types of exercise interventions, provided that they were evenly distributed between groups.
Types of outcome measures
We included all outcomes irrespective of follow‐up duration, but planned to evaluate the impact of follow‐up in subgroup analyses if sufficient data were available.
Primary outcomes
Health‐related quality of life using measures validated for people with bronchiectasis in a clinical setting (e.g. Bronchiectasis Severity Index (BSI; St. George's Respiratory Questionnaire (SGRQ))
Exacerbations (requiring antibiotic therapy) measured as frequency, proportion with one or more, or duration
Serious adverse events (i.e. any adverse even that results in death or is life‐threatening)
Secondary outcomes
Frequency of hospital admissions measured
Lung function (forced expiratory volume in one second (FEV1) litres or percent of predicted)
Symptoms (e.g. dyspnoea, cough, wheeze), for example using the Leicester Cough Questionnaire (LCQ)
Self‐efficacy (e.g. Chronic Disease Self‐Efficacy Scale)
Economic costs (e.g. direct: costs of care such as cost‐benefit or cost‐effectiveness; indirect: days lost from work or full‐time education)
Adverse events (e.g. pneumonia)
Reporting of one or more of the outcomes above was not an inclusion criterion for the review.
We recognise the limitation of using self‐efficacy as a primary outcome, and it may be viewed as an intermediate or process outcome. Research is needed to establish if, in bronchiectasis, improvements in self‐efficacy leads to long‐term improvements in clinically important endpoints (Lavery 2011).
Search methods for identification of studies
Electronic searches
We identified studies from the Cochrane Airways Trials Register, which is maintained by the Information Specialist for the Group. The Cochrane Airways Trials Register contains studies identified from several sources:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org);
weekly searches of MEDLINE Ovid SP 1946 to date;
weekly searches of Embase Ovid SP 1974 to date;
Monthly searches of PsycINFO Ovid SP 1967 to date;
Monthly searches of CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature) 1937 to date;
Monthly searches of AMED EBSCO (Allied and Complementary Medicine);
handsearches of the proceedings of major respiratory conferences.
Studies contained in the Trials Register are identified through search strategies based on the scope of Cochrane Airways. Details of these strategies, as well as a list of handsearched conference proceedings are in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We also conducted a search of ClinicalTrials.gov (www.ClinicalTrials.gov) and the World Health Organization (WHO) trials portal (www.who.int/ictrp/en/). We searched for studies in any language in all databases from their inception to November 2016.
Searching other resources
We examined the reference lists of all primary studies and review articles for additional references and searched relevant manufacturers' websites for trial information. We searched the ‘grey’ literature at OpenGrey (www.opengrey.eu/) and searched for errata or retractions from included studies published in full‐text on PubMed (www.ncbi.nlm.nih.gov/pubmed).
Data collection and analysis
Selection of studies
Two review authors (CK and SG) independently screened titles and abstracts for inclusion of all potential studies and classified them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. Two review authors (CK and S Grundy) independently screened the full‐text of retrieved studies to identify those for inclusion and record reasons for exclusion of the ineligible studies. We resolved disagreements through discussion or through a third review author (SS). We identified and excluded duplicates and collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram and a 'Characteristics of excluded studies' table (Moher 2009).
Data extraction and management
We used a data collection form, piloted on at least one study in the review, to record study characteristics and outcome data. One review author (DL) extracted the following characteristics from the included studies.
Methods: study design, total duration of study, details of any 'run in' period, number of study centres and location, study setting, withdrawals, and date of study
Participants: number, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria, and exclusion criteria
Interventions: intervention, comparison, concomitant medications, and excluded medications
Outcomes: primary and secondary outcomes specified and collected, and time points reported
Notes: funding for trial, and notable conflicts of interest of trial authors
Two review authors (DL and CK) independently extracted outcome data from the included studies. We noted outcome data that were not reported in a usable way in the 'Characteristics of included studies' table. We resolved disagreements by consensus or by involving a third review author (SS). One review author (DJWE) transferred data into the Review Manager 5 (RevMan 5) file (RevMan 2014). We validated data entry by comparing the data presented in the systematic review with the study reports. A second review author (CK) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (CK and DL) independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We resolved disagreements by discussion or by involving another review author (SS). We assessed the risk of bias according to the following domains.
Random sequence generation
Allocation concealment
Blinding of participants and personnel
Blinding of outcome assessment
Incomplete outcome data
Selective outcome reporting
Other bias
We graded each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for our judgement in the 'Risk of bias' table. We summarised the risk of bias judgements across different studies for each of the domains listed and considered blinding separately for different key outcomes where necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality may be very different than for a patient‐reported quality‐of‐life scale). Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for studies that contributed to that outcome.
Assessment of bias in conducting the systematic review
We conducted the review according to the published protocol and reported any deviations from it in the 'Differences between protocol and review' section of the systematic review.
Measures of treatment effect
We estimated intervention effects using odds ratios with 95% confidence intervals (CI) for dichotomous data and mean difference or standardised mean difference with 95% CI for continuous data. Where standard deviations (SD) were not reported but other measures of variance around mean differences, such as standard error, CIs, or P values were reported, we calculated these according to Section 7.3 in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). In this review it was likely that different scales may have been used to measure the same outcome (for example, Bronchiectasis‐Quality of Life (B‐QoL) and St. George's Respiratory Questionnaire (SGRQ)). In this case, we planned to use the standardised mean difference (SMD) and its 95% CI, ensuring a consistent direction of effect by reversing scaling where necessary, supported by a statement in the text on direction of interpretation.
We planned to undertake meta‐analyses only where this was meaningful, that is, where the treatments, participants and the underlying clinical question were similar enough for pooling to make sense. We planned to narratively describe skewed data reported as medians and interquartile ranges.
Unit of analysis issues
In this review the unit of analysis was the participant. For all dichotomous data, we reported the proportion of participants that contributed to each outcome compared with the total number of randomised participants.
Cross‐over trials
Cross‐over trials were not appropriate for this intervention as it was not possible to avoid carry‐over of knowledge acquisition from the first phase. However, if we had identified eligible cross‐over studies we planned to only include data from the first pre cross‐over phase.
Cluster‐randomised trials
Large‐scale trials are uncommon in bronchiectasis and it was therefore unlikely that we would identify eligible RCTs randomising at group level (e.g. by primary care practice). We planned to analyse eligible cluster‐RCTs in accordance with methods described in Section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c), using average cluster size and an estimate of the intraclass correlation coefficient (ICC) to adjust sample sizes to the 'effective sample size'. Where appropriate, we planned to combine single RCTs with cluster‐RCTs if we considered the designs and interventions sufficiently similar and the effect of the intervention was unlikely to be influenced by the method of randomisation.
Multiple‐arm trials
Where trials included multiple arms we planned to describe all study groups in the 'Characteristics of included studies' table, but to only include the arms that met our review criteria in the analyses. If multiple comparisons (e.g. self‐management A versus self‐management B versus self‐management C versus usual care) were combined in the same meta‐analysis, we planned to divide the usual care (control) group by the number of intervention arms to avoid 'double‐counting'.
Dealing with missing data
We contacted investigators of included studies to provide unreported data such as missing outcomes, missing data, means or SDs and noted differential dropout between study groups along with reasons for withdrawal. Where a particular outcome included substantial loss to follow‐up (≥ 50%), we planned to report this in the text and mark the data with an asterisk. We used available cases for data analysis and did not impute missing data. Where studies included analyses based on the imputation of missing values, we planned to include data at low risk of bias and report data separately for those at higher risk of bias in the text of the review. Multiple imputation methods that included sensitivity analyses pre‐specified in published protocols were considered at low risk of bias (Little 2012; Gewandter 2014). Imputation of missing data related to trial outcomes, using methods such as last observation carried forward, were not considered appropriate. For example, completion of missing data (e.g. relating to an efficacy outcome) following an intervention‐related death would be inappropriate (Gewandter 2014).
Where missing data were thought to introduce a high risk of bias (substantial loss to follow‐up or inappropriate imputation), we planned to explore the impact of including such studies using a sensitivity analysis.
Assessment of heterogeneity
In this review, the specific nature of the intervention, population, outcomes and methodological quality had the potential to vary considerably between studies. We therefore planned to assess potential sources of variability between studies in the following ways.
Clinical variability: to compare the distribution of participants, interventions, and outcomes across the included studies. To discuss and agree potential clinical heterogeneity by consensus.
Methodological variability: to compare study designs and study quality using 'Risk of bias' criteria.
-
Statistical heterogeneity (where variability in the effects of interventions is greater than expected by chance alone): to evaluate the statistical significance of heterogeneity using the Chi² test (P = 0.10 is significant). However, this test may be unreliable, lacking power to detect important heterogeneity with few or small studies and the potential to detect clinically insignificant heterogeneity with large numbers of studies. It is also possible for trials to show large consistent effects in the face of significant heterogeneity. Therefore, in addition to assessing evidence of heterogeneity using the Chi² test as above, we also planned to quantify the magnitude of heterogeneity using the Tau² (random‐effects model only), and I² statistics (Higgins 2003) with the following interpretation thresholds, based on recommendations in Section 9.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
We planned to report substantial heterogeneity (> 50%) and to explore possible causes by prespecified subgroup analysis.
Assessment of reporting biases
We planned to compare the results of data from published and unpublished studies as a direct test of publication bias and, if there were a sufficient number of studies (10 or more), to explore potential bias arising from small‐study effects using Egger’s method to test for asymmetry in funnel plots (Egger 1997). If smaller studies had shown larger intervention effects compared to larger studies, we planned to evaluate potential causes (for example, poor methodological quality; differences in populations or interventions) and to report studies at high risk of bias in the text of the review.
Data synthesis
We planned to include studies in meta‐analyses where the study designs, interventions and outcomes were similar. Where substantial heterogeneity (> 50%) was identified we planned to report outcomes in the text, giving direction and size of the effect along with the strength of the evidence (risk of bias). It was likely that included studies would vary by population, design and outcomes, therefore we considered meta‐analysis using a random‐effects model the most appropriate. However, where there are few studies or the effects of interventions across studies are not randomly distributed (for example, with publication bias), the random‐effects model estimates may be unreliable or biased. It was likely that this review would only include a small number of low‐powered studies and we therefore planned to use a fixed‐effect model and to evaluate the impact of model choice using a sensitivity analysis. We aimed to synthesise and report dichotomous and continuous data separately for a given outcome, should the need arise (e.g. exacerbation/no exacerbation or exacerbation duration). Where both end‐of‐study point estimates and change from baseline scores were reported we analysed these separately. We performed the analyses using RevMan 5 (RevMan 2014).
'Summary of findings' table
We created a 'Summary of findings' table using the following primary and secondary outcomes: health‐related quality of life, hospital admissions, serious adverse events, exacerbations, lung function, self‐efficacy and economic costs. We tabulated the quality of each outcome with the five GRADE criteria (study limitations, consistency of effect, imprecision, indirectness and publication bias) (GRADE 2004) using methods and recommendations described in Section 8.5 (Higgins 2011a) and Chapter 12 (Schünemann 2011) of the Cochrane Handbook for Systematic Reviews of Interventions and GRADEpro GDT software (GRADEpro GDT 2015). We justified all decisions to downgrade or upgrade the quality of studies using footnotes and we included comments to aid the reader's understanding where necessary.
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following subgroup analyses.
Age: adults (> 18 years) versus children
Duration of follow‐up (less than 12 months versus 12 months or longer)
We planned to use the following outcomes in subgroup analyses.
Health‐related quality of life
Hospital admissions
Adverse events
We planned to use the formal test for subgroup interactions in RevMan 5 (RevMan 2014).
Sensitivity analysis
We planned to carry out the following sensitivity analyses.
To exclude studies at high risk of selection bias
Analyses using a random‐effects model
Missing data (studies with > 50% or those using inappropriate imputation)
Results
Description of studies
Results of the search
Following comprehensive electronic searches of bibliographic databases we identified ninety‐two records and an additional eight records through searches of clinicaltrials.gov and the WHO trials portal. Of a total of sixty records (40 duplicates removed), forty‐three were excluded following screening of titles and abstracts. We examined the full‐text articles of 17 records (11 studies) and excluded 12 records (8 studies; see Excluded studies). The remaining five records reported the results of three studies; two studies were included in the review and one was an ongoing study (Characteristics of ongoing studies). The PRISMA flow diagram in Figure 2 shows the study selection process.
2.
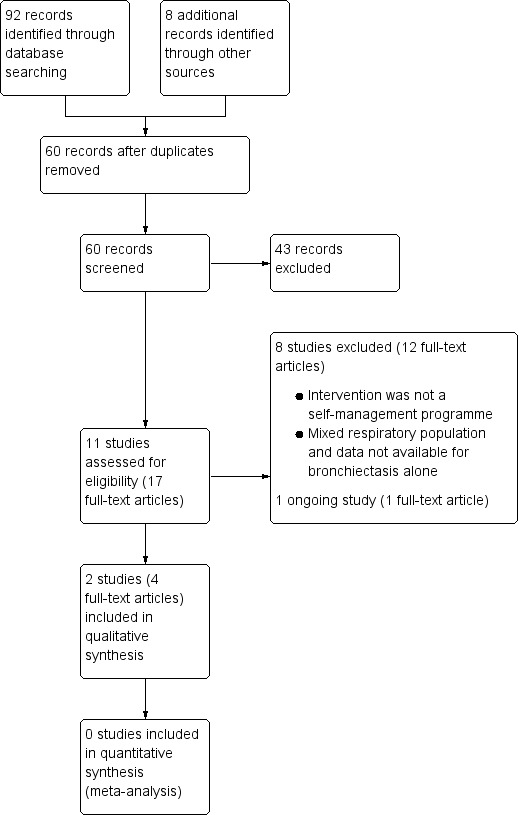
Study flow diagram
Included studies
Two studies met the inclusion criteria for this review and contributed data to the narrative synthesis (Lavery 2011; Greening 2014). The two studies randomised a total of 84 adult participants with bronchiectasis. Greening 2014 recruited and reported data for participants with any respiratory disease (n = 389), but the study authors kindly provided disaggregated data for the subset of participants with a primary diagnosis of bronchiectasis that are reported in the review. Both studies were reported as full‐text, peer‐reviewed articles. In Greening 2014 the complex rehabilitation intervention included a self‐management programme. As this component of the complex intervention was substantial, we have included the trial in this review; however, we are mindful that because the self‐management programme was included alongside other interventional components (described in Characteristics of included studies) the findings from this trial in relation to the predefined inclusion criteria for this review should be interpreted with caution.
Methods
Greening 2014 was a prospective, 12‐month RCT conducted in an acute cardiorespiratory unit in a teaching hospital and an acute medical unit in an affiliated teaching district general hospital, both located in England (UK) Characteristics of included studies.
Lavery 2011 was a proof‐of‐concept, six‐month RCT in a single regional respiratory centre in Northern Ireland (UK) Characteristics of included studies.
Participants
Greening 2014 enrolled adults with a diagnosis of chronic respiratory disease, aged 40 years or over (bronchiectasis group mean age = 72 (intervention = 78, control = 68) with self‐reported breathlessness on exertion (MRC dyspnoea grade 3 or worse). Individuals with concomitant acute cardiac events or more than four emergency admissions to hospital (any cause) during the previous 12 months were excluded. Eligible patients were enrolled within 48 hours of admission to hospital for an exacerbation of chronic respiratory disease. The study included people with COPD, chronic asthma, interstitial lung disease and bronchiectasis but the study authors kindly provided disaggregated data for the cohort of participants with bronchiectasis (n = 20); baseline characteristics are presented in the Characteristics of included studies.
In Lavery 2011 64 adult participants were randomised (with 32 participants in each arm of the study), and four were withdrawn before the study reached completion (two in each arm of the study). In both groups the mean age was 60 years, with an inclusion criterion of 18 years or over, and with a primary diagnosis of bronchiectasis based on respiratory physician assessment, including a computed tomographic scan Characteristics of included studies
Interventions
Greening 2014 randomised individuals on a 1:1 basis to receive early rehabilitation plus self‐management (six weeks' duration) and usual care, versus usual care alone. Early rehabilitation comprised supervised volitional (strength and aerobic training) and non‐volitional (neuromuscular electrical stimulation) techniques and a self‐management programme. The progressive exercise programme was individually tailored and delivered/supported by physiotherapists and nurses during the stay on an acute medical ward, and after discharge was supported by weekly telephone consultations with the pulmonary rehabilitation team, consisting of physiotherapists and nurses. The self‐management programme comprised the SPACE (Self management programme of Activity, Coping and Education) manual for COPD, a structured programme of exercise, education, and psychosocial support. Motivational interviewing techniques were used to familiarise participants with the manual, which was used throughout the participants’ inpatient stay and during telephone discussions. Usual care comprised standard care from the ward physiotherapy team, including physiotherapist‐delivered techniques for airway clearance, assessment and supervision of mobility and smoking cessation advice; usual care did not include a supervised progressive exercise programme during admission or immediately after discharge.
In Lavery 2011 the intervention was usual care plus an expert patient programme (EPP); disease‐specific EPP was delivered in group format during one session per week (2.5 hours) for eight weeks (two weeks of disease‐specific education; six weeks of standardised EPP). The disease‐specific component included causes of bronchiectasis, disease process, medical investigations, dealing with symptoms, airway clearance techniques, exacerbations, health promotion and available support. Participants in the control group received usual care; review at a specialist respiratory clinic on a three‐monthly basis to monitor spirometry, inflammatory blood markers, and sputum microbiologic assessment. Inhaled therapy and antibiotics were prescribed where required and treatment was adjusted to the needs of the participant as necessary, including hospital admission.
Outcomes
The primary outcome for the study reported by Greening 2014 was the readmission rate at 12 months. Secondary outcomes included number of hospital days, mortality, lung function, physical performance and health‐related quality of life, measured using the St George's Respiratory Questionnaire (SGRQ); secondary outcomes were assessed at baseline, discharge from hospital, six‐week, and three‐ and 12‐month follow‐up.
In Lavery 2011 the primary outcome was the Chronic Disease Self‐efficacy Scales (CDSS), which measures the confidence of an individual to perform items related to self‐management. Secondary outcomes included the Revised Illness Perception Questionairre (IPQ‐R), which explains health behaviour in terms of coping; SGRQ was used to measure quality of life; two standard EPP questionnaires relating to self‐rated health, ability to manage their condition and adherence to medication. Other outcome measures included FEV1, frequency of antibiotic therapy and sputum microbiology. Secondary measures were recorded at baseline, post‐intervention (eight weeks) and at three‐ and six‐month follow‐up.
Excluded studies
We excluded a total of eight studies (Newall 2005; Liaw 2011; Mandal 2012; Gurses 2013; Lee 2014; Mazzoleni 2014 ;Hester 2016; Aksamit 2017; ); three studies were excluded because both intervention and control groups received common self‐management components (Newall 2005; Mandal 2012; Lee 2014), resulting in a single component of difference between the two groups, which failed to meet our inclusion criteria of at least two elements in the self‐management component; the intervention in one study was solely an information resource, which also did not meet our criteria (Hester 2016); in three studies the intervention was not self‐management (Liaw 2011; Gurses 2013;Aksamit 2017; ); in one study with a mixed population of participants, data were not available for bronchiectasis participants alone (Mazzoleni 2014).
Risk of bias in included studies
'Risk of bias' assessments and supporting evidence are presented in the Characteristics of included studies. Figure 1 provides a summary of risk of bias judgements presented by study and domain. Figure 3 depicts the risk of bias for each domain, presented as percentage values across both included studies. Overall, the two included studies were well reported and of high methodological quality; we considered the studies to have a low risk of bias for the majority of domains (see below).
1.
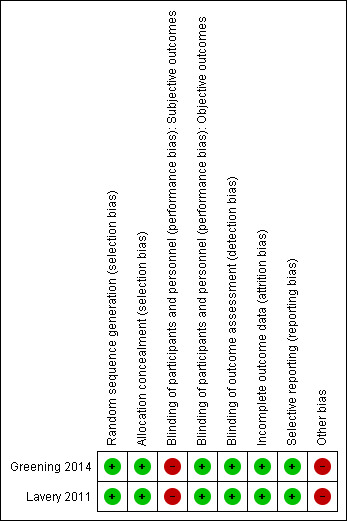
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
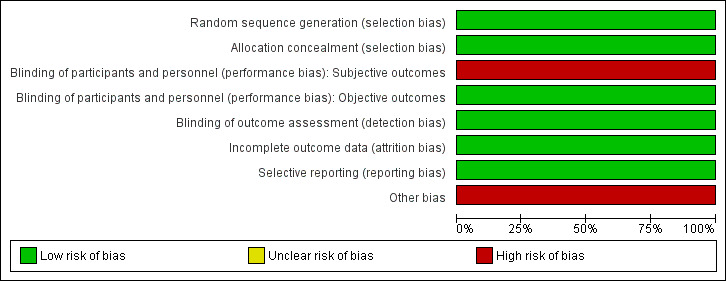
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Both studies used appropriate methods for random sequence generation and allocation concealment. We judged both studies to be at low risk of selection bias.
Blinding
Blinding of the participants and personnel (i.e. those delivering the intervention) to treatment allocation was not feasible due to the nature of the interventions. Thus, we considered both studies to be at low risk of performance bias for objective outcomes (i.e. exacerbations, serious adverse events, serious adverse events, lung function, frequency of hospital admissions, lung function, economic costs, adverse events) and at high risk of performance bias for subjective outcomes (i.e. health‐related quality of life; symptoms, self‐efficacy). In both studies, outcome assessors were blinded to treatment allocation; we considered the risk of detection bias to be low for both studies.
Incomplete outcome data
We considered both studies to have a low risk of attrition bias based on low and balanced rates of participant withdrawal, which were documented adequately in the study reports.
Selective reporting
Both studies were pre‐registered on appropriate clinical trials registries, where predefined outcomes of interest were listed. Both studies reported all pre‐defined outcomes of interest and were considered to be at low risk of reporting bias.
Other potential sources of bias
The study by Lavery 2011 was a proof‐of‐concept RCT that did not include a power calculation. There was therefore a risk that negative findings were influenced by an inadequate sample size and we considered this study at high risk of 'other bias', though this was not related to the methodological quality of the study.
The authors of Greening 2014 provided disaggregated data for participants with bronchiectasis. The number of participants with bronchiectasis was low (n = 20) and there appeared to be a baseline imbalance in disease severity; participants in the intervention group showed a trend towards higher MRC dyspnoea grades (baseline and stable state) and worse baseline lung function (lower FEV1); however, statistical comparisons were not available. In addition, mortality rates were imbalanced between groups in the subset of bronchiectasis participants. We therefore considered the study by Greening 2014 to be at high risk for 'other bias', although we would stress that this was not related to the methodological quality of the overall study, and likely a result of our use of disaggregated data with an insufficient sample size.
Effects of interventions
See: Table 1
Summary of findings for the main comparison. Self‐management compared to usual care for bronchiectasis.
| Self‐management compared to usual care for bronchiectasis | ||||||
| Patient or population: people with non‐cystic fibrosis bronchiectasis Setting: community Intervention: self‐management Comparison: usual care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with usual care | Risk with self‐management | |||||
| Health‐related quality of life assessed with: SGRQ Scale from: 0 to 100, lower score is better Follow‐up: range 6 weeks to 12 months | The mean health‐related quality of life was 56.02 points | MD 10.27 lower (45.15 lower to 24.61 higher) | ‐ | 20 (1 RCT) | ⊕⊝⊝⊝ Very low1, 2, 3 | No clear benefit or harm from self‐management (very low‐quality evidence) |
|
Health‐related quality of life
assessed with: SGRQ
Scale from: 0 to 100, lower score is better Follow up: range post‐intervention to 6 months |
The mean health‐related quality of life was 44.7 points | MD 3.2 higher (6.64 lower to 13.04 higher) | ‐ | 60 (1 RCT) | ⊕⊕⊝⊝ Low1, 3 | No clear benefit or harm from self‐management |
| Exacerbations requiring antibiotics | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Serious adverse events: mortality | ‐ | ‐ | not estimable | 20 (1 RCT) | ||
| Hospital admissions (number admitted at least once) Follow‐up: range 6 weeks to 12 months | ‐ | ‐ | not estimable | 20 (1 RCT) | ‐ | |
| Lung function assessed with: FEV1 L Follow‐up: discharge to 12 months | The mean FEV1 was 1.03 L | MD 0.3 higher (1.11 lower to 1.71 higher) | ‐ | 20 (1 RCT) | ⊕⊝⊝⊝ Very low1, 2, 3 | No clear benefit or harm from self‐management |
|
Self‐efficacy assessed with: CDSS
Scale from: 0 to 10 Follow‐up: postintervention to 6 months |
‐ | ‐ | not estimable | 60 (1 RCT) | ⊕⊕⊝⊝ Low1, 3 | Six out of ten scales showed significant improvements over time with the intervention. We elected not to include all 10 scales in the table but graded the evidence based on overall quality of the study |
| Economic costs | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CDSS: Chronic Disease Self‐efficacy Scale; CI: confidence interval; FEV1: forced expiratory volume in one second MD: mean difference; SGRQ: St George's Respiratory Questionnaire | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
1One point deducted for the unblinded nature of the comparison. 2One point deducted for baseline imbalances. 3One point deducted for risk of bias from an underpowered study. Figure 1
The different nature of the interventions in the two included studies (a complex rehabilitation intervention including self‐management and a single expert patient programme) meant that meta‐analysis of the data was not appropriate and the results were therefore included narratively.
Primary outcomes
Health‐related quality of life
The authors of Greening 2014 provided health‐related quality of life data for the subset of participants with bronchiectasis. Mean SGRQ Total scores in both groups improved over time but were not significantly different at six weeks', three and 12 months' follow‐up (6 weeks MD ‐12.70, 95% CI ‐30.39 to 4.99; 3 months MD ‐9.15, 95% CI ‐28.08 to 9.78; 12 months MD ‐10.27, 95% CI ‐45.15 to 24.61; Analysis 1.1). The mean difference between groups at each time point exceeds the minimum clinically important difference (MCID) of four units (Jones 2005) but confidence intervals indicate imprecision in the effect, potentially attributable to the low sample size (max n = 13). The study authors did not formally report the change from baseline to 12 months and it was not possible to calculate the change value as more than half of the participants withdrew during the study. However, results should be interpreted with caution due to the small sample size and unequal numbers of participants in each group (n = 20).
1.1. Analysis.
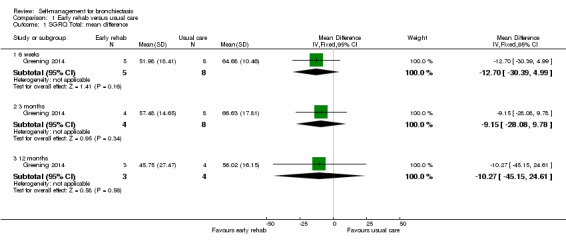
Comparison 1 Early rehab versus usual care, Outcome 1 SGRQ Total: mean difference.
In Lavery 2011 there were no differences in SGRQ Total scores between groups postintervention, or at three or six months' follow‐up (postintervention: MD ‐6.50, 95% CI ‐16.59 to 3.59; 3 months, MD ‐2.60, 95% CI ‐12.97 to 7.77, 6 months, MD 3.20, 95% CI ‐6.64 to 13.04; Analysis 2.1). The study authors reported marginal worsening in SGRQ Total scores over the six‐month follow‐up in the intervention group (from 46.9, 95% CI 40.2 to 53.6 to 47.9, 95% CI 40.7 to 55.1) and an improvement of 6.9 units in the control group (from 51.6, 95% CI 45.0 to 58.1 to 44.7, 95% CI 37.6 to 51.7).
2.1. Analysis.
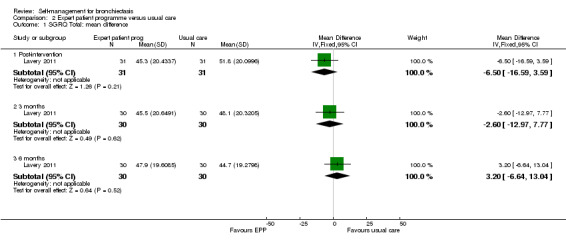
Comparison 2 Expert patient programme versus usual care, Outcome 1 SGRQ Total: mean difference.
There is therefore no indication of benefit in health‐related quality of life, based on SGRQ total scores, attributable to the intervention. Using GRADE criteria we judged the quality of the evidence for this outcome to be either low (Lavery 2011) or very low (Greening 2014) Table 1.
Exacerbations (requiring antibiotic therapy)
Neither of the included studies reported data on exacerbations requiring antibiotic therapy.
Serious adverse events
Greening 2014 provided mortality data for the subset of participants with bronchiectasis. During the 12 months of follow‐up, four of eight participants (50%) died in the early rehabilitation group and two of 12 participants (16.7%) died in the usual care group. However, results should be interpreted with caution due to the low event rate, unequal numbers of participants in each group and small sample size (n = 20).
Lavery 2011 did not evaluate serious adverse events.
It was not possible to assess this outcome using GRADE criteria.
Secondary outcomes
Frequency of hospital admissions
The study authors provided data on hospital admissions for the subset of participants with bronchiectasis. In the early rehabilitation group (n = 8), six participants (75%) were readmitted to hospital during 12 months of follow‐up; three were readmitted once; one was readmitted twice; and two were readmitted three times. In the usual care group (n = 12), six participants (50%) were readmitted to hospital during the 12 months of follow‐up; four were readmitted once; one was readmitted three times; and one was readmitted seven times. The mean (SD) number of admissions per participant per 12 months in the early rehabilitation group and usual care groups, respectively, were 1.38 (1.19) and 1.17 (2.04); there did not appear to be a significant difference between groups. However, results should be interpreted with caution due to the low event rate, unequal numbers of participants in each group and small sample size (n = 20).
Lavery 2011 did not evaluate the frequency of hospital admissions.
It was not possible to assess this outcome using GRADE criteria.
Lung function
The study authors provided data on FEV1 (L) for the subset of participants with bronchiectasis. Baseline measurements were recorded when individuals were in a stable state. There were no significant differences between groups at discharge, six weeks', three or 12 months' follow‐up (discharge MD ‐0.13, 95% CI ‐0.60 to 0.34; 6 weeks MD 0.07, 95% CI ‐0.55 to 0.69; 3 months MD 0.15, 95% CI ‐0.55 to 0.85; 12 months MD 0.30, 95% CI ‐1.11 to 1.71; Analysis 1.2). Change in lung function was not formally reported in the paper and it was not possible to calculate the change value as more than half of the participants withdrew during the study. The results should be interpreted with caution due the low sample size at each time point (n = 17 at discharge; n = 8 at one year), the unequal numbers of participants in each group (intervention = 8; control = 12) and the small size of the overall sample (n = 20).
1.2. Analysis.
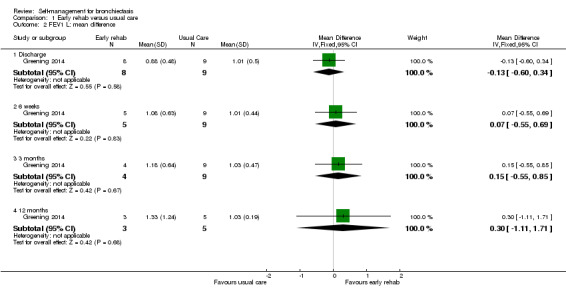
Comparison 1 Early rehab versus usual care, Outcome 2 FEV1 L: mean difference.
Lavery 2011 reported no significant differences between the control and intervention groups with regard to lung function (P > 0.05) but did not report further details.
Using GRADE criteria we judged the quality of the evidence for this outcome to be very low Table 1.
Symptoms
Neither of the included studies reported data on symptoms.
Self‐efficacy
Greening 2014 did not examine self‐efficacy.
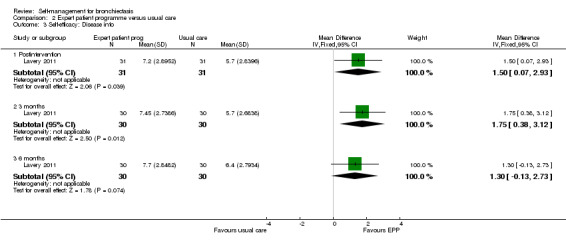
Lavery 2011 reported data on self‐efficacy using an outcome measure found to be valid and reliable when tested in individuals with long term‐health conditions. The Chronic Disease Self‐efficacy Scale (CDSS) measures the confidence of an individual to perform self‐management tasks on 10 component scales using 1 to 10 Likert responses. All scales showed significant benefit postintervention (exercise, MD 2.10, 95% CI 0.89 to 3.31, Analysis 2.2; disease information, MD 1.50, 95% CI 0.07 to 2.93, Analysis 2.3; obtaining help, MD 1.10, 95% CI 0.05 to 2.15, Analysis 2.4; communicating with physician, MD 1.10, 95% CI 0.14 to 2.06, Analysis 2.5; managing disease, MD 1.10, 95% CI 0.17 to 2.03, Analysis 2.6; doing chores, MD 2.00, 95% CI 0.78 to 3.22, Analysis 2.7; social activity, MD 2.00, 95% CI 0.84 to 3.16, Analysis 2.8; Managing symptoms, MD 1.90, 95% CI 0.78 to 3.02, Analysis 2.9; Managing breathlessness, MD 1.50, 95% CI 0.32 to 2.68, Analysis 2.10; Managing depression, MD 2.00, 95% CI 0.91 to 3.09, Analysis 2.11), but the effect was only sustained by the six‐month endpoint on the Managing Depression scale (6 months, MD 1.30, 95% CI 0.09 to 2.51, Analysis 2.11). The study authors report a significant improvement in self‐efficacy over time with the intervention on six of the 10 subscales of the CDSS (exercise, disease information, doing chores, social activity, managing symptoms and managing depression) though they acknowledge that the greatest impact was immediately postintervention. The authors report that four subscales did not show a significant difference between groups over time (managing the disease, obtaining help, communicating with physician, managing breathlessness). There is no Minimum Clinically Important Difference value for the CDSS.
2.2. Analysis.
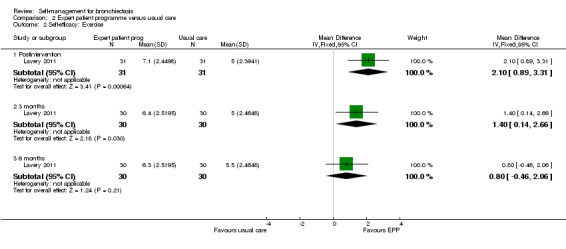
Comparison 2 Expert patient programme versus usual care, Outcome 2 Self‐efficacy: Exercise.
2.3. Analysis.
Comparison 2 Expert patient programme versus usual care, Outcome 3 Self‐efficacy: Disease info.
2.4. Analysis.
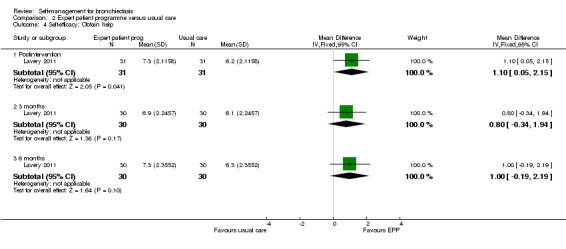
Comparison 2 Expert patient programme versus usual care, Outcome 4 Self‐efficacy: Obtain help.
2.5. Analysis.
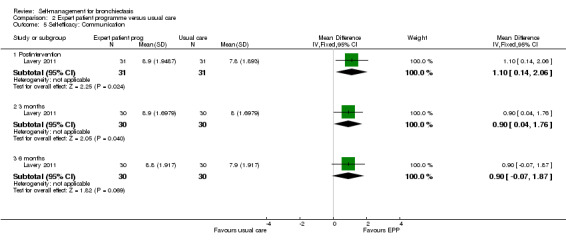
Comparison 2 Expert patient programme versus usual care, Outcome 5 Self‐efficacy: Communication.
2.6. Analysis.
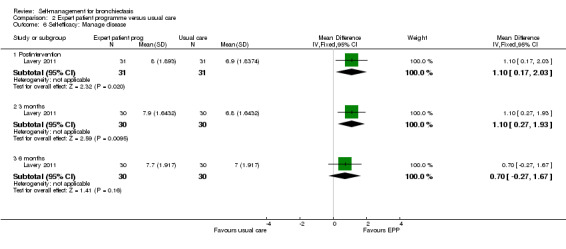
Comparison 2 Expert patient programme versus usual care, Outcome 6 Self‐efficacy: Manage disease.
2.7. Analysis.
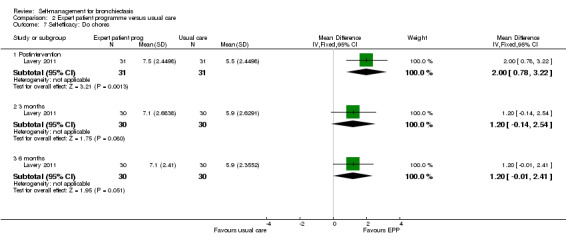
Comparison 2 Expert patient programme versus usual care, Outcome 7 Self‐efficacy: Do chores.
2.8. Analysis.
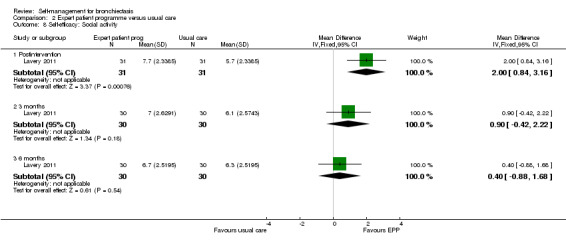
Comparison 2 Expert patient programme versus usual care, Outcome 8 Self‐efficacy: Social activity.
2.9. Analysis.
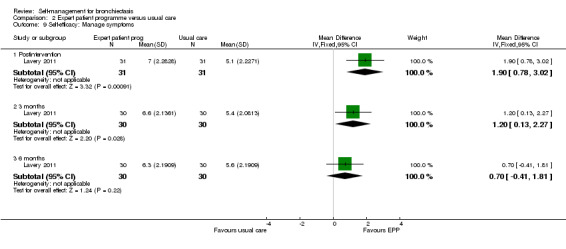
Comparison 2 Expert patient programme versus usual care, Outcome 9 Self‐efficacy: Manage symptoms.
2.10. Analysis.
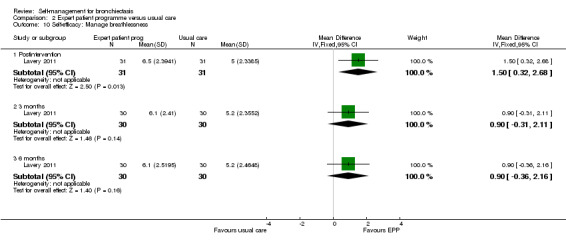
Comparison 2 Expert patient programme versus usual care, Outcome 10 Self‐efficacy: Manage breathlessness.
2.11. Analysis.
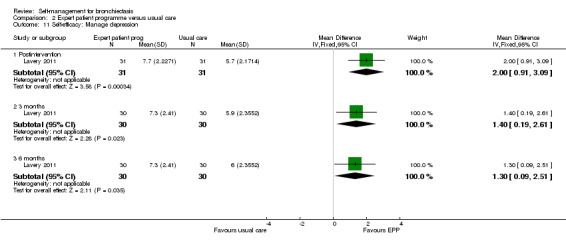
Comparison 2 Expert patient programme versus usual care, Outcome 11 Self‐efficacy: Manage depression.
As the CDSS comprises 10 component scales we opted not to include them in the 'Summary of findings' tables. However using GRADE criteria, we judged the quality of evidence for this outcome as very low, based on the overall quality of the study Table 1.
Economic costs
Neither of the included studies reported data on economic costs.
Adverse events
Neither of the included studies reported data on adverse events.
Discussion
Summary of main results
There is insufficient evidence to draw clear conclusions as to whether self‐management interventions for people with bronchiectasis have a significant impact on the primary outcomes of this review, namely: health‐related quality of life; frequency of exacerbations and serious adverse events.
Only two studies fulfilled the inclusion criteria for the review. The first evaluated the effect of a combined early rehabilitation and self‐management programme on 389 participants admitted to hospital with acute exacerbations of chronic respiratory disease (Greening 2014). However, we were only able to use a subset of 20 participants with bronchiectasis in the review. The second study evaluated the impact of an expert patient self‐management programme on 64 participants with bronchiectasis (Lavery 2011). It is important to note that the Greening study recruited participants at an exacerbation, whilst Lavery recruited participants in stable condition. Merging results of these two self‐management plans therefore is limited by the different clinical conditions of participants and should be considered as an additional limitation. Participants receiving self‐management did not show any significant benefit from the intervention in terms of health‐related quality of life by the endpoint in either study. There was a trend towards a higher mortality rate in one very small study but no clear difference was seen.. Neither of the included studies measured exacerbation frequency. In terms of our secondary outcomes, there was no impact on the frequency of hospital admissions in one study and no impact on lung function in either of our included studies. One study reported self‐efficacy using the CDSS and showed evidence of improvement following an expert patient programme in six of the ten scales that comprised the outcome measure. Neither of the included studies reported symptoms, adverse events and economic costs.
It is important to note that (Greening 2014) was a compound intervention incorporating a substantial self‐management component and we included it in the review for that reason. However, the findings from this trial in relation to the predefined inclusion criteria for this review should be interpreted with caution as we cannot isolate the effects of self‐management from the other intervention components. In addition, the self‐management component was based on a model used with people with COPD and was not specifically tailored to people with bronchiectasis. All of the results from this study should be interpreted with caution as the disaggregated data were not powered to detect differences and there were imbalances between groups.
Overall there is inadequate published data to establish with any degree of certainty whether self‐management strategies for people with bronchiectasis have either a positive or negative impact.
Overall completeness and applicability of evidence
The paucity of data available for inclusion in this review mandates caution when extrapolating the findings to similar populations or other settings. We identified only two adult studies in the review, looking at different interventions. We did not identify any trials of self‐management programmes for children, nor any trials comparing one type of self‐management strategy with another. Neither of the studies included in the review measured the frequency of exacerbations requiring antibiotics, an important marker of disease activity in bronchiectasis, symptoms, adverse events or economic costs. As an exercise component was included in the compound intervention in one of the studies, it would have been useful to have included exercise performance as an outcome measure in the review. As it stands, the evidence for the benefits and harms of self‐management interventions is incomplete and of limited applicability to clinical practice.
Quality of the evidence
With guidance from the GRADE criteria we considered the quality of the evidence, where data were available for formal comparison, to be low or very low, and where data were available for narrative inclusion we would draw similar conclusions. We are aware of the limitations of the two included studies, in particular the small amount of disaggregated data available for inclusion from Greening 2014, and have summarised them in Characteristics of included studies, Figure 2 and Figure 3. It was not possible to consider publication bias through the construction of a funnel plot due to the very small number of included studies.
Potential biases in the review process
We are aware of the potential for publication bias in this systematic review, as there is inevitably the concern that we may not have found relevant unpublished trials. However, we have received excellent support from Cochrane Airways, with comprehensive and systematic database searches, and we endeavoured to address any study selection bias with two review authors independently evaluating trials for inclusion. Throughout we were careful to ensure that this process was consistent with our predefined inclusion criteria.
Agreements and disagreements with other studies or reviews
The need for patient self‐management has been identified and included in bronchiectasis guidelines and research prioritisation (Pasteur 2010; Aliberti 2016). However, uptake remains unclear with a UK audit showing that only 33% of 97 institutions provided individualised self‐management plans, and a single‐centre UK audit suggesting that effective personal management was achievable without a formal self‐management plan (Hill 2013; Ali 2015). Aliberti 2016 suggest in their research priorities in bronchiectasis that future studies should be conducted to determine the effectiveness of patient self‐management and adherence to treatment; this review supports this by revealing how little evidence currently exists. Due to the limited data available from our review it is not possible to assess whether effects of self‐management may be observed in people with bronchiectasis but planned future studies may help to resolve the uncertainty (Hester 2016).
Authors' conclusions
Implications for practice.
There is inadequate published evidence to guide clinical decisions as to the potential benefits and risks of self‐management interventions for people with non‐cystic fibrosis bronchiectasis. The evidence was limited by a number of factors including potentially underpowered studies, complex interventions and limited reporting of important measures of clinical benefit. Overall, this review has been unable to identify sufficient evidence to resolve uncertainties regarding the benefits of self‐management in clinical practice. In the absence of high‐quality evidence it is advisable that practitioners adhere to current international guidelines that advocate self‐management for people with bronchiectasis Polverino 2017.
Implications for research.
Currently, self‐management for bronchiectasis is a broad term incorporating a diverse range of interventions, from complex multi‐component programmes to web‐based information systems. An international consensus statement defining the essential components of bronchiectasis self‐management is required in order to support research replication, data synthesis and the evaluation of efficacy. The international consensus‐based definition of self‐management will help to drive the standardisation of interventions in COPD (Effing 2016), but the definition is unsuitable for use in bronchiectasis. There is uncertainty about the potential overlap between COPD and bronchiectasis, but resolution of this issue may inform revision of the definition of self‐management used in future updates of the review. The taxonomy of self‐management support developed by Taylor and colleagues (Taylor 2014) may form the basis for development of a self‐management definition for bronchiectasis, with condition‐specific refinement informed by methods from the chronic obstructive pulmonary disease self‐management definition (Effing 2016). The review authors suggest that there is a clear need for a definition of self‐management in bronchiectasis that will provide a basis for future clinical trials with enhanced homogeneity that could be included in subsequent meta‐analysis.
There are very few clinical trials in this area and those available only include adults. Research is needed on the impact of self‐management programmes in children, in particular with a focus on the causes of bronchiectasis in children. The context of self‐management interventions may also vary from chest clinics to community settings and this should be taken into consideration when evaluating effectiveness. Likewise the clinical condition of the patient, with regards to severity and exacerbation versus stable state should be explicit in future studies. Statification of patients at risk of exacerbations, hospital admissions, and mortality using a validated tool such as the Bronchiectasis Severity Index (Chalmers 2014) or the FACED score (Martinez‐García 2014) can be considered vital for future research. Few clinically important outcomes were available for inclusion in this review and future studies should include measures of the frequency and duration of exacerbations, including those requiring antibiotic therapy, adherence to antibiotic therapy, other aspects of self‐management such as airway clearance techniques, adverse events and data on economic costs to inform policy and clinical commissioning.
All future trials should use a robust, high‐quality design, taking the above sources of variability into consideration and ensuring adequate sample sizes, potentially from multicentre studies, and populations that reflect the age range of people with bronchiectasis.
Acknowledgements
We would like to the thank Cochrane Airways for their support during preparation of the review. Julia Walters was the Editor for this review and commented critically on the protocol and review. The Background and Methods sections of this review are based on a standard template used by Cochrane Airways. This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to Cochrane Airways. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
We would like to thank Mrs Alison Clark and Mr Ian Kenworthy for their very valuable patient and parent career comments.
We also like to thank Dr Greening for providing additional information about one of the included studies.
Appendices
Appendix 1. Sources and search methods for the Cochrane Airways Group's Specialised Register (CAGR)
Electronic searches: core databases
| Database | Frequency of search |
| MEDLINE (Ovid) | Weekly |
| Embase (Ovid) | Weekly |
| CENTRAL (crso.cochrane.org) | Monthly |
| PsycINFO (Ovid) | Monthly |
| CINAHL (EBSCO) | Monthly |
| AMED (EBSCO) | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
MEDLINE search strategy used to identify trials for the CAGR
Bronchiectasis topic search
1. exp Bronchiectasis/
2. bronchiect$.mp.
3. bronchoect$.mp.
4. kartagener$.mp.
5. (bronchial$ adj3 dilat$).mp.
6. or/1‐5
Filter to identify RCTs
1. exp "clinical trial [publication type]"/
2. (randomised or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter (Lefebvre 2011) are adapted to identify trials in other electronic databases.
Appendix 2. Search strategy to identify relevant trials from the CAGR
#1 BRONCH:MISC1
#2 MeSH DESCRIPTOR Bronchiectasis Explode All
#3 bronchiect*
#4 #1 or #2 or #3
#5 MeSH DESCRIPTOR Self Care Explode All
#6 MeSH DESCRIPTOR Education
#7 MeSH DESCRIPTOR Patient Education as Topic
#8 educat*
#9 self‐manag*
#10 "self manag*"
#11 self‐car* or "self car*"
#12 train* or instruct*
#13 "patient cent*" or patient‐cent*
#14 patient‐focus* or "patient focus*"
#15 patient‐education or "patient education"
#16 "management plan" or management‐plan
#17 management* NEAR1 program*
#18 behavior* or behaviour*
#19 disease* NEAR2 management*
#20 self‐efficac*
#21 empower*
#22 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21
#23 #4 AND #22
[In search line #1, MISC1 denotes the field in the record where the reference has been coded for condition, in this case, bronchiectasis]
Data and analyses
Comparison 1. Early rehab versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SGRQ Total: mean difference | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 weeks | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | ‐12.70 [‐30.39, 4.99] |
| 1.2 3 months | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | ‐9.15 [‐28.08, 9.78] |
| 1.3 12 months | 1 | 7 | Mean Difference (IV, Fixed, 95% CI) | ‐10.27 [‐45.15, 24.61] |
| 2 FEV1 L: mean difference | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Discharge | 1 | 17 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐0.60, 0.34] |
| 2.2 6 weeks | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.55, 0.69] |
| 2.3 3 months | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.55, 0.85] |
| 2.4 12 months | 1 | 8 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐1.11, 1.71] |
| 3 Mortality | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.64, 39.06] |
1.3. Analysis.
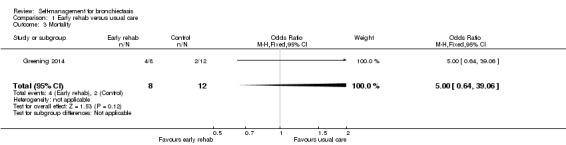
Comparison 1 Early rehab versus usual care, Outcome 3 Mortality.
Comparison 2. Expert patient programme versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 SGRQ Total: mean difference | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐6.5 [‐16.59, 3.59] |
| 1.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐12.97, 7.77] |
| 1.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 3.20 [‐6.64, 13.04] |
| 2 Self‐efficacy: Exercise | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.10 [0.89, 3.31] |
| 2.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.14, 2.66] |
| 2.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.46, 2.06] |
| 3 Self‐efficacy: Disease info | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [0.07, 2.93] |
| 3.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.75 [0.38, 3.12] |
| 3.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐0.13, 2.73] |
| 4 Self‐efficacy: Obtain help | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.05, 2.15] |
| 4.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.34, 1.94] |
| 4.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.19, 2.19] |
| 5 Self‐efficacy: Communication | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.14, 2.06] |
| 5.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [0.04, 1.76] |
| 5.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.07, 1.87] |
| 6 Self‐efficacy: Manage disease | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.17, 2.03] |
| 6.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.27, 1.93] |
| 6.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐0.27, 1.67] |
| 7 Self‐efficacy: Do chores | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.78, 3.22] |
| 7.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.14, 2.54] |
| 7.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.01, 2.41] |
| 8 Self‐efficacy: Social activity | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.84, 3.16] |
| 8.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.42, 2.22] |
| 8.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [‐0.88, 1.68] |
| 9 Self‐efficacy: Manage symptoms | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.90 [0.78, 3.02] |
| 9.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [0.13, 2.27] |
| 9.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐0.41, 1.81] |
| 10 Self‐efficacy: Manage breathlessness | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [0.32, 2.68] |
| 10.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.31, 2.11] |
| 10.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.36, 2.16] |
| 11 Self‐efficacy: Manage depression | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.91, 3.09] |
| 11.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.19, 2.61] |
| 11.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [0.09, 2.51] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Greening 2014.
| Methods |
Study design: prospective RCT (single blind, parallel group; trial identifier: ISRCTN05557928) Total duration of study: 12 months 'Run in' period: none Number of study centres and location: 2 centres; UK Study setting: an acute cardiorespiratory unit in a teaching hospital and an acute medical unit in an affiliated teaching district general hospital Date of study: January 2010‐September 2012 |
|
| Participants |
Note: This study recruited participants with any chronic respiratory condition; Dr Greening kindly provided disaggregated data for the participants with bronchiectasis reported here. Number randomised: 20 participants with bronchiectasis randomised (early rehabilitation: n = 8; usual care: n = 12) Number of withdrawals: none Number analysed: variable per outcome Mean age (SD), years: early rehabilitation: 78 (7.8); usual care: 68.8 (11.5) Gender, n (%) male: early rehabilitation: NA; usual care: NA Severity of condition Mean (SD) baseline MRC dyspnoea grade on admission: early rehabilitation: 4.9 (0.35); usual care: 4.4 (0.67) Mean (SD) stable state MRC dyspnoea grade: early rehabilitation: 4.3 (0.46); usual care: 3.5 (0.67) Mean (SD) stable state FEV1 (L): early rehabilitation: 0.84 (0.28); usual care: 1.18 (0.49) Diagnostic criteria: MRC dyspnoea score; spirometry was measured to British Thoracic Society standards. Baseline lung function: see severity of condition Smoking history: smoker, n yes/no/ex‐smoker/missing: early rehabilitation: 1/4/2/1 ; usual care: 1/5/6/0 Inclusion criteria: the study recruited patients with a diagnosis of chronic respiratory disease, including COPD; chronic asthma, bronchiectasis or interstitial lung disease); we have considered only the subset of participants with bronchiectasis. Participants had to be aged ≥ 40 years with self‐reported breathlessness on exertion when stable (MRC dyspnoea grade 3 or worse). Exclusion criteria: inability to provide informed consent; concomitant acute cardiac event; presence of musculoskeletal, neurological, or psychiatric comorbidities that would prevent the delivery of the rehabilitation intervention; and > 4 emergency admissions to hospital for any cause in the previous 12 months. |
|
| Interventions |
Intervention: early rehabilitation (6 weeks' duration), comprising usual care plus daily, supervised volitional (strength and aerobic training) and non‐volitional (neuromuscular electrical stimulation) techniques. This complex intervention also included a self‐management programme, described by the study authors as: "The intervention team delivered education using the SPACE (Self management programme of Activity, Coping and Education) manual for chronic obstructive pulmonary disease, a structured programme of exercise, education, and psychosocial support. Motivational interviewing techniques were used to introduce patients to the manual and to familiarise them with the content. The manual was used throughout the participants’ inpatient stay and in the subsequent discussions during telephone calls." As this component of the complex intervention was substantial we deemed the trial to be eligible for inclusion in this review; however, we are mindful that because SPACE was included alongside other components the findings from this trial in relation to the predefined inclusion criteria for this review should be interpreted with caution. It should also be noted that SPACE was primarily designed for COPD patients and is not specifically targeted for bronchiectasis. The pulmonary rehabilitation team, consisting of physiotherapists and nurses, delivered the intervention. The exercise programme was individually prescribed and progressed. Early rehabilitation was performed on the acute medical ward and by the participants’ bedside. After discharge, participants underwent an unsupervised home based programme, supported by telephone consultations. Those who were readmitted after the 6‐week intervention period did not receive a further early rehabilitation intervention. Comparison: usual care (standard care from the ward clinical physiotherapy team as directed by the responsible clinical team) including physiotherapist‐delivered techniques for airway clearance, assessment and supervision of mobility, and advice on smoking cessation. Nutritional status was assessed using the malnutrition universal screening tool score in all participants, and referral for dietetic advice and nutritional support was carried out if appropriate. No supervised or progressive exercise programme was provided during the admission or immediately after discharge, but outpatient pulmonary rehabilitation was offered to all participants 3 months after discharge as part of standard care. Concomitant medications: not stated Excluded medications: not stated |
|
| Outcomes |
Primary outcomes (pre‐specified): readmission rate at 12 months Secondary outcomes (pre‐specified): number of hospital days, mortality, physical performance and HRQoL. Secondary functional measures were recorded at baseline, at discharge from hospital, 6 weeks, 3 months and 12 months. Timepoints: 12 months Outcomes collected: 1ll specified outcomes were collected |
|
| Notes |
Funding: not stated Notable author conflicts of interest: none stated/identified |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The clinical trials unit at the University of Leicester coordinated randomisation by an automated internet based service (www.sealedenvelope.com)" |
| Allocation concealment (selection bias) | Low risk | Quote: "The clinical trials unit at the University of Leicester coordinated randomisation by an automated internet based service (www.sealedenvelope.com)" |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | It is not feasible to blind participants to the intervention. Knowledge of treatment group could influence self‐reporting of subjective outcomes by participants. |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote: "Single blind". It is not feasible to blind participants to the treatment group. However, knowledge of treatment group would be unlikely to influence objective outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “..all investigators performing the outcome measures were blinded to treatment allocation..” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | During trial: 14/196 withdrew from intervention group; 10/193 withdrew from control group. Missing data imputed |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Other bias | High risk | Baseline imbalances in age and disease severity in the subset of participants with bronchiectasis; participants in the control group appeared to have less severe disease. Higher mortality with intervention in bronchiectasis subgroup (intervention: 4/8; control: 2/12) |
Lavery 2011.
| Methods |
Study design: proof‐of‐concept RCT (NCT01117493). Total duration of study: 6 months 'Run in' period: none Number of study centres and location: single regional respiratory centre, Belfast, Northern Ireland, UK. Study setting: Tertiary care Date of study: September 2006‐October 2007 |
|
| Participants |
Number randomised: 64 (32/32) Number of withdrawals: 4 (2/2) Number analysed: 60 (30/30) Mean age (SD), years: intervention: 60 (9); control: 60 (8) Gender, % m/f: intervention: 44/56; control: 47/53 Diagnostic criteria: assessment by respiratory clinician Baseline lung function ‐ mean (SD) % predicted FEV1: intervention: 59 (20); control: 65 (23) Smoking history: not stated Inclusion criteria: adults (aged ≥ 18 years) with a primary diagnosis of bronchiectasis based on a respiratory physician’s assessment, including a CT scan Exclusion criteria: primary diagnosis of CF, MRSA infection, or a condition that would have an impact on the assessment procedures (e.g. sensory impairment, pregnancy, language barrier, or a factor that would prevent adherence to the self‐management programme) |
|
| Interventions |
Intervention: usual care plus EPP: disease‐specific EPP was delivered in a group format during 1 session/week (2.5 h) for 8 weeks in total (2 weeks of disease‐specific education; 6 weeks of standardised EPP). The disease‐specific component included causes of bronchiectasis, disease process, medical investigations, dealing with symptoms, airway clearance techniques, exacerbations, health promotion and support available. The format of the disease‐specific EPP was delivered by a physiotherapist and a nurse with specialist expertise in the management of bronchiectasis who were trained and followed a scripted manual to standardise delivery. The format of the EPP was developed and piloted before this RCT. Topics included general health education, education on self‐management treatment strategies, action planning, and problem solving. Comparison: usual care: reviews at a specialist respiratory clinic on a 3‐monthly basis to monitor spirometry results, inflammatory blood marker levels, and sputum microbiologic assessment. Inhaled therapy and antibiotics were prescribed if required, and treatment was adjusted to the needs of the participant as necessary, including hospital admission. Concomitant medications: not stated Excluded medications: not stated |
|
| Outcomes |
Primary outcomes (pre‐specified): CDSS ‐ comprises 10 scales as follows: exercise, disease information, obtaining help, communication with physician, managing disease, doing cores, social activity, managing symptoms, managing breathlessness, managing depression. Responses are measured using a 1‐10 Likert scale where higher scores indicate greater self‐efficacy. There is no Minimum Clinically Important Difference value for these scales. Secondary outcomes (pre‐specified): revised Illness Perception Questionnaire, SGRQ, FEV1, frequency of oral and/or intravenous antibiotic therapy prescribed at respiratory clinics Timepoints: baseline, post‐intervention (8 weeks), 3 and 6 months postintervention Outcomes collected: all specified outcomes were collected |
|
| Notes |
Funding: supported by the Health and Social Care Research and Development Division, Public Health Agency, Belfast, Northern Ireland Notable author conflicts of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “…computer generated concealed randomisation process conducted by an independent person...” |
| Allocation concealment (selection bias) | Low risk | Quote “..an envelope corresponding to the patient’s number was opened to reveal if they were assigned to the intervention or control group.” |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Not blinded and lack of blinding may have influenced outcome (1 withdrew who ‘wanted intervention’) |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | It is not feasible to blind participants or personnel to the intervention. However, knowledge of treatment group would be unlikely to influence objective outcomes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Data were collected by trained health professionals who were blinded to participants’ groups and had no other contact with the participants. Study participants were requested not to disclose their group assignment.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 months: 2/32 missing from intervention group (1 illness, 1 did not complete outcome measures); 2/32 missing from control group (1 wanted intervention, 1 disliked questionnaire). Even balance between groups |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported. Subjective outcomes were well‐reported but objective outcomes poorly reported. |
| Other bias | High risk | This was a proof‐of‐concept study so there was no power calculation. There is therefore a risk that negative findings were influenced by an inadequate sample size |
CDSS: Chronic Disease Self‐Efficacy Scale; CF: cystic fibrosis; COPD: chronic obstructive pulmonary disease; CT: computed tomographic; EPP: expert patient programme; FEV1: forced expiratory volume in one second; HRQoL: health‐related quality of life; MRC: medical research council; MRSA: methicillin‐resistant Staphylococcus aureus ;NA: not applicable; RCT: randomised controlled trial; SGRQ: St Georges Respiratory Questionnaire; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aksamit 2017 | The intervention was not self‐management |
| Gurses 2013 | Inspiratory muscle training was the sole intervention |
| Hester 2016 | Information resource was the sole intervention |
| Lee 2014 | Exercise programme plus airway clearance therapy (ACT) advice at baseline versus ACT advice at baseline alone. Therefore, the only intervention component was exercise and does not meet our criteria of at least 2 components in the intervention group alone |
| Liaw 2011 | Inspiratory muscle training was the sole intervention |
| Mandal 2012 | Pulmonary rehabilitation plus chest physiotherapy plus education plus self‐management plan versus chest physiotherapy plus education plus self‐management. Therefore, the only component in the intervention group alone is pulmonary rehabilitation and does not meet our criteria of at least 2 components in the intervention group alone |
| Mazzoleni 2014 | The study included 40 participants with a range of respiratory conditions, including 2 with bronchiectasis. We contacted the study authors for data on the bronchiectasis participants alone but did not receive a reply. |
| Newall 2005 | Inspiratory muscle training plus pulmonary rehabilitation plus education versus pulmonary rehabilitation plus education. Therefore, the only component in the intervention group alone is inspiratory muscle training and does not meet our criteria of at least 2 components in the intervention group alone |
Characteristics of ongoing studies [ordered by study ID]
NCT02179983.
| Trial name or title | Tayside Rehabilitation in Bronchiectasis Exacerbations (TRIBE) : a randomized controlled trial (TRIBE) |
| Methods | RCT of pulmonary rehabilitation after exacerbations of bronchiectasis |
| Participants | Inclusion Criteria
Exclusion Criteria
|
| Interventions |
|
| Outcomes | Primary Outcome Measures
Secondary Outcome Measures
|
| Starting date | June 2014 |
| Contact information | James D Chalmers, University of Dundee |
| Notes |
CF: cystic fibrosis; COPD: chronic obstructive pulmonary disorder; CT: computed tomographic; RCT: randomised controlled trial
Contributions of authors
SS, CK, DL and S Grundy drafted the protocol. For the review, CK and S Grundy selected studies for inclusion; DJWE and SS extracted data from the studies and assessed the risk of bias; SS and DJWE entered data into Review Manager 5 and performed the analyses; SS, CK, DL, SJM S Grundy and S Gudur drafted the final review. SS had overall responsibility for the review.
Sources of support
Internal sources
-
Postgraduate Medical Institute, Edge Hill University, UK.
Employer of Sally Spencer, Dave Lynes and Carol Kelly
-
Aintree University Hospitals NHS Foundation Trust, UK.
Employer of Seamus Grundy
-
Lancaster University, UK.
Employer of David JW Evans and Steve Milan
External sources
The authors declare that no such funding was received for this systematic review, Other.
Declarations of interest
Sally Spencer – none known
Carol Kelly – none known
Dave Lynes – none known
Seamus Grundy – none known
David Evans – none known
Stephen Milan – none known
Sharada Gudur‐ none know
New
References
References to studies included in this review
Greening 2014 {published data only}
- Greening NJ, Williams JEA, Hussain SF, Harvey‐Dunstan TC, Bankart MJ, Chaplin EJ, et al. An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: randomised controlled trial. BMJ (Clinical research ed.) 2014;349:4315. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lavery 2011 {published data only}
- Lavery K, O'Neill B, Elborn S, Bradley J. Self‐management in bronchiectasis. An exploratory randomised controlled trial of a disease specific expert patient programme compared to usual care in patients with bronchiectasis [Abstract]. Thorax. 2007; Vol. 62:A18.
- Lavery KA, O'Neill B, Parker M, Elborn JS, Bradley JM. Expert patient self‐management program versus usual care in bronchiectasis: A randomized controlled trial. Archives of physical medicine and rehabilitation 2011;92:1194‐201. [DOI] [PubMed] [Google Scholar]
- NCT01117493. Expert patient self‐management programme versus usual care in bronchiectasis. Clinicaltrials.gov 2006.
References to studies excluded from this review
Aksamit 2017 {published data only}
- Aksamit T, Bandel TJ, Criollo M, Soyza A, Elborn JS, Operschall E, et al. The RESPIRE trials: two phase III, randomized, multicentre, placebo‐controlled trials of ciprofloxacin dry powder for inhalation (diprofloxacin DPI) in non‐cystic fibrosis bronchiectasis. Contemporary Clinical Trials 2017;58:78‐85. [PUBMED: 28495619] [DOI] [PubMed] [Google Scholar]
Gurses 2013 {published data only}
- Gurses HN, Ayhan B, Demir R, Ozyilmaz S. The effects of inspiratory muscle training on respiratory muscle strength and pulmonary functions in children with bronchiectasis. European respiratory journal 2013;42:1074s [P5064]. [Google Scholar]
Hester 2016 {published data only}
- Hester KL, Newton J, Rapley T, Soyza A. Evaluation of a novel information resource for patients with bronchiectasis: study protocol for a randomised controlled trial. Trials 2016;17:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hester KLM, Newton J, Rapley T, Ryan V, Soyza A. M15 evaluation of a novel intervention for patients with bronchiectasis: the bronchiectasis information and education feasibility (brief) study. Thorax 2016;71(Suppl 3):A265‐A266. [DOI: 10.1136/thoraxjnl-2016-209333.457] [DOI] [Google Scholar]
Lee 2014 {published data only}
- Lee A L, Hill C J, Cecins N, Jenkins S, McDonald C F, Burge A T, et al. The short and long term effects of exercise training in non‐cystic fibrosis bronchiectasis‐‐a randomised controlled trial. Respiratory research 2014;15:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A, Hill C, Cecins N, Jenkins S, McDonald C, Burge A, et al. Exercise training is beneficial in patients with noncystic fibrosis bronchiectasis A multicentre, randomised controlled trial. European respiratory journal 2012;40:515s [P2834]. [Google Scholar]
- Lee AL, Cecins N, Hill CJ, Holland AE, Rautela L, Stirling RG, et al. The effects of pulmonary rehabilitation in patients with non‐cystic fibrosis bronchiectasis: protocol for a randomised controlled trial. BMC Pulmonary Medicine 2010;10:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liaw 2011 {published data only}
- Liaw MY, Wang YH, Tsai YC, Huang KT, Chang PW, Chen YC, et al. Inspiratory muscle training in bronchiectasis patients: a prospective randomized controlled study. Clinical Rehabilitation 2011;25:524‐36. [DOI] [PubMed] [Google Scholar]
Mandal 2012 {published data only}
- Mandal P, Sidhu MK, Kope L, Pollock W, Stevenson LM, Pentland JL, et al. A pilot study of pulmonary rehabilitation and chest physiotherapy versus chest physiotherapy alone in bronchiectasis. Respiratory Medicine 2012;106:1647‐54. [DOI] [PubMed] [Google Scholar]
Mazzoleni 2014 {published data only}
- Mazzoleni S, Montagnani G, Vagheggini G, Buono L, Moretti F, Dario P, et al. Interactive videogame as rehabilitation tool of patients with chronic respiratory diseases: preliminary results of a feasibility study. Respiratory Medicine 2014;108:1516‐24. [DOI] [PubMed] [Google Scholar]
Newall 2005 {published data only}
- Newall C, Henson M, McConnell AK, Stockley RA, Hill SL. The effect of inspiratory muscle training (IMT) on pulmonary function, exercise tolerance, and quality of life in patients with bronchiectasis (BE). European Respiratory Journal 2000;16:36s. [Google Scholar]
- Newall C, Stockley RA, Hill SL. Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax 2005;60:943‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT02179983 {published data only}
- NCT02179983. A randomized controlled trial of pulmonary rehabilitation after exacerbations of bronchiectasis. clinicaltrials.gov/ct2/show/NCT02179983 2014.
Additional references
Ali 2015
- Ali S, Duckers J, Lau D. Audit investigating self‐management of bronchiectasis at University Hospital Llandough, Wales. European Respiratory Journal 2015;46:PA362. [DOI: 10.1183/13993003.congress-2015.PA362] [DOI] [Google Scholar]
Aliberti 2016
- Aliberti S, Masefield S, Polverino E, Soyza A, Loebinger MR, Menendez R, et al. Research priorities in bronchiectasis: a consensus statement from the EMBARC Clinical Research Collaboration. European Respiratory Journal 2016;48(3):632.47. [DOI: 10.1183/13993003.01888-2015] [DOI] [PubMed] [Google Scholar]
Bourbeau 2004
- Bourbeau J, Nault D, Dang‐Tan T. Self‐management and behaviour modification in COPD. Patient Education and Counseling 2004;52(3):271‐7. [DOI] [PubMed] [Google Scholar]
Challis 2010
- Challis D, Hughes J, Berzins K, Reilly S, Abell J, Stewart K. Self‐care and case management in long‐term conditions: the effective management of critical interfaces. www.pssru.ac.uk/pdf/MCpdfs/SCCMfr.pdf Accessed 11th January 2017.
Chalmers 2012
- Chalmers JD, Smith MP, McHugh BJ, Doherty C, Govan JR, Hill AT. Short‐ and long‐term antibiotic treatment reduces airway and systemic inflammation in non–cystic fibrosis bronchiectasis. American Journal of Respiratory and Critical Care Medicine 2012;186(7):657‐65. [DOI] [PubMed] [Google Scholar]
Chalmers 2014
- Chalmers JD, Goeminne P, Aliberti S, McDonnell MJ, Lonni S, Davidson J, et al. The Bronchiectasis Severity Index: an international derivation and validation study. American Journal of Respiratory and Critical Care Medicine 2014;189(5):576‐85. [DOI: 10.1164/rccm.201309-1575OC] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chalmers 2016
- Chalmers JD, Aliberti S, Blasi F. Management of bronchiectasis in adults. European Respiratory Journal 2016;45(5):1446‐62. [DOI] [PubMed] [Google Scholar]
Chang 2002
- Chang AB, Grimwood K, Mulholland K, Torzillo P. Bronchiectasis in Indigenous children in remote Australian communities. Medical Journal of Australia 2002;177:200‐204. [DOI] [PubMed] [Google Scholar]
Chang 2003
- Chang AB, Masel JP, Boyce NC, Wheaton G, Torzillo PJ. Non‐CF bronchiectasis: clinical and HRCT evaluation. Pediatric Pulmonology 2003;35(6):477‐83. [DOI: 10.1002/ppul.10289] [DOI] [PubMed] [Google Scholar]
Chang 2015
- Chang AB, Bell SC, Torzillo PJ, King PT, Maguire GP, Byrnes CA, et al. Chronic suppurative lung disease and bronchiectasis in children and adults in Australia and New Zealand Thoracic Society of Australia and New Zealand guidelines. Medical Journal of Australia 2015;202(1):21‐3. [DOI: 10.5694/mja14.00287] [DOI] [PubMed] [Google Scholar]
Cole 1986
- Cole PJ. Inflammation: a two‐edged sword—the model of bronchiectasis. European Journal of Respiratory Diseases Supplement 1986;147:6‐15. [PubMed] [Google Scholar]
de Silva 2011
- Silva D. Helping People Help Themselves. London: The Health Foundation, 2011. [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Department of Health 2001
- Department of Health. The Expert Patient: A New Approach to Chronic Disease Management for the 21st Century. London: Department of Health, 2001. [Google Scholar]
Effing 2012
- Effing TW, Bourbeau J, Vercoulen J, Apter AJ, Coultas D, Meek P. Self‐management programmes for COPD: moving forward. Chronic Respiratory Disease 2012;9(1):27‐35. [DOI] [PubMed] [Google Scholar]
Effing 2016
- Effing TW, Vercoulen JH, Bourbeau J, Trappenburg J, Lenferink A, Cafarella P, et al. Definition of a COPD self‐management intervention: International Expert Group consensus. European Respiratory Journal 2016;48:46‐54. [DOI: 10.1183/13993003.00025-2016] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [PUBMED: 9310563] [DOI] [PMC free article] [PubMed] [Google Scholar]
European Lung White Book 2013
Farrell 2004
- Farrell K, Wicks MN, Martin JC. Chronic disease self‐management improved with enhanced self‐efficacy. Clinical Nursing Research 2004;13(4):289‐308. [DOI] [PubMed] [Google Scholar]
Gewandter 2014
- Gewandter JS, McDermott MP, McKeown A, Smith SM, Williams MR, Hunsinger M, et al. Reporting of missing data and methods used to accommodate them in recent analgesic clinical trials: ACTTION systematic review and recommendations. Pain 2014;155(9):1871‐7. [DOI: 10.1016/j.pain.2014.06.018] [DOI] [PubMed] [Google Scholar]
Goeminne 2012
- Goeminne PC, Scheers H, Decraene A, Seys S, Dupont LJ. Risk factors for morbidity and death in non‐cystic fibrosis bronchiectasis: a retrospective cross‐sectional analysis of CT diagnosed bronchiectatic patients. Respiratory Research 2012;13:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goeminne 2016
- Goeminne PC, Soyza A. Bronchiectasis: how to be an orphan with many parents?. European Respiratory Journal 2016;47(1):10‐3. [DOI] [PubMed] [Google Scholar]
GRADE 2004
- Grade Working Group. Education and debate: grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490‐4. [DOI: 10.1136/bmj.328.7454.1490] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- GRADE Working Group, McMaster University. GRADEpro GDT. Version accessed 28 April 2016. Hamilton (ON): GRADE Working Group, McMaster University, 2015.
Griffiths 2005
- Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay‐led self management programme for Bangladeshi patients with chronic disease. British Journal of General Practice 2005;55(520):831‐7. [PMC free article] [PubMed] [Google Scholar]
Habesoglu 2011
- Habesoglu MA, Ugurlu AO, Eyuboglu FO. Clinical, radiological, and functional evaluation of 304 patients with bronchiectasis. Annals of Thoracic Medicine 2011;6(3):131‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hagger 2014
- Hagger MS, Luszczynska A. Implementation intention and action planning interventions in health contexts: state of the research and proposals for the way forward. Applied Psychology: Health and Well‐Being 2014;6(1):1‐47. [DOI] [PubMed] [Google Scholar]
Haworth 2014
- Haworth CS, Foweraker JE, Wilkinson P, Kenyon RF, Bilton D. Inhaled colistin in patients with bronchiectasis and chronic Pseudomonas aeruginosa infection. American Journal of Respiratory and Critical Care Medicine 2014;189(8):975‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011c
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hill 2013
- Hill AT, Routh C, Welham S. National BTS bronchiectasis audit 2012: is the quality standard being adhered to in adult secondary care?. Thorax 2014;69(3):292‐4. [DOI: 10.1136/thoraxjnl-2013-203739; PUBMED: 23878159] [DOI] [PubMed] [Google Scholar]
Jones 2005
- Jones PW. St. George's Respiratory Questionnaire: MCID. COPD 2005;2(1):75‐9. [DOI] [PubMed] [Google Scholar]
Kennedy 2013
- Kennedy A, Peter P, Reeves D, Blakeman T, Bowen R, Chew‐Graham C, et al. Implementation of self management support for long term conditions in routine primary care settings: cluster randomised controlled trial. BMJ 2013;346:f2882. [doi: http://dx.doi.org/10.1136/bmj.f2882] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kolbe 1996
- Kolbe J, Wells AU. Bronchiectasis: a neglected cause of respiratory morbidity and mortality. Respirology 1996;1(4):221‐5. [DOI] [PubMed] [Google Scholar]
Lavery 2007
- Lavery K, O'Neill B, Elborn JS, Reilly J, Bradley JM. Self‐management in bronchiectasis: the patients’ perspective. European Respiratory Journal 2007;29(3):541‐7. [DOI: 10.1183/09031936.00057306] [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Little 2012
- Little RJ, D'Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, et al. The prevention and treatment of missing data in clinical trials. New England Journal of Medicine 2012;367(14):1355‐60. [DOI: 10.1056/NEJMsr1203730] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lonni 2015
- Lonni S, Chalmers JD, Goeminne PC, McDonnell MJ, Dimakou K, Soyza A, et al. Etiology of non–cystic fibrosis bronchiectasis in adults and its correlation to disease severity. Annals of the American Thoracic Society 2015;12(12):1764‐70. [DOI: 10.1513/AnnalsATS.201507-472OC] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lorig 2003
- Lorig KR, Holman HR. Self‐management education: history, definition, outcomes, and mechanisms. Annals of Behavioral Medicine 2003;26(1):1‐7. [DOI] [PubMed] [Google Scholar]
Martinez‐García 2007
- Martinez‐García MA, Soler‐Cataluña JJ, Perpiñá‐Tordera M, Román‐Sánchez P, Soriano J. Factors associated with lung function decline in adult patients with stable non‐cystic fibrosis bronchiectasis. Chest 2007;132(5):1565‐72. [DOI] [PubMed] [Google Scholar]
Martinez‐García 2014
- Martinez‐García MA, Gracia J, Vendrell Relat MV, Girón RM, Máiz Carro L, Rosa Carrillo D, et al. Multidimensional approach to non‐cystic fibrosis bronchiectasis: the FACED score. European Respiratory Journal 2014;43(5):1357‐67. [DOI: 10.1183/09031936.00026313] [DOI] [PubMed] [Google Scholar]
McCullough 2014
- McCullough AR, Tunney AM, Quittner A, Elborn J, Bradley J, Hughes C. Treatment adherence and health outcomes in patients with bronchiectasis. BMC Pulmonary Medicine 2014;14:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
McCullough 2015
- McCullough AR, Tunney MM, Elborn JS, Bradley JM, Hughes CM. Predictors of adherence to treatment in bronchiectasis. Respiratory Medicine 2015;109(7):838‐45. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 2011
- Murray M, Govan J, Doherty C, Simpson A, Wilkinson T, Chalmers J, et al. A randomized controlled trial of nebulized gentamicin in non–cystic fibrosis bronchiectasis. American Journal of Respiratory and Critical Care Medicine 2011;183(4):491‐9. [DOI] [PubMed] [Google Scholar]
Naylor 2015
- Naylor C, Imison C, Addicott R, Buck D, Goodwin N, Harrison T, et al. Transforming our health care system. www.kingsfund.org.uk/publications/articles/transforming‐our‐health‐care‐system‐ten‐priorities‐commissioners. London: Kings Fund, Accessed 11 January 2017. [http://www.kingsfund.org.uk/publications/articles/transforming‐our‐health‐care‐system‐ten‐priorities‐commissioners]
O'Brien 2000
- O'Brien C, Guest PJ, Hill SL, Stockley RA. Physiological and radiological characterization of patients diagnosed with chronic obstructive pulmonary disease in primary care. Thorax 2000;55(8):635–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Neill 2016
- O'Neill J. Tackling drug‐resistant infections globally: final report and recommendations. The review on antimicrobial resistance. amr‐review.org/ Accessed 11 January 2017.
Pasteur 2000
- Pasteur MC, Helliwell SM, Houghton SJ, Webb SC, Foweraker JE, Coulden RA, et al. An investigation into causative factors in patients with bronchiectasis. American Journal of Respiratory and Critical Care Medicine 2000;162(4 Pt 1):1277‐84. [DOI] [PubMed] [Google Scholar]
Pasteur 2010
- Pasteur MC, Bilton D, Hill AT, the British Thoracic Society Bronchiectasis (non‐CF) Guideline Group. British Thoracic Society Guidelines for non‐CF bronchiectasis. Thorax 2010;65(Suppl 1):i1‐i58. [DOI] [PubMed] [Google Scholar]
Peytremann‐Bridevaux 2015
- Peytremann‐Bridevaux I, Arditi C, Gex G, Bridevaux PO, Burnand B. Chronic disease management programmes for adults with asthma. Cochrane Database of Systematic Reviews 2015, Issue 5. [DOI: 10.1002/14651858.CD007988.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Polverino 2017
- Polverino E, Goeminne PC, McDonnell MJ, Aliberti S, Marshall SE, Loebinger MR, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. European Respiratory Journal 2017;50(3):pii: 1700629. [DOI: 10.1183/13993003.00629-2017] [DOI] [PubMed] [Google Scholar]
Quint 2016
- Quint JK, Millett ERC, Joshi M, Navaratnam V, Thomas SL, Hurst JR, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population‐based cohort study. European Respiratory Journal 2016;47(1):186‐93. [DOI: 10.1183/13993003.01033-2015] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roberts 2010
- Roberts HJ, Hubbard R. Trends in bronchiectasis mortality in England and Wales. Respiratory Medicine 2010;104(7):981‐5. [DOI] [PubMed] [Google Scholar]
Saleh 2014
- Saleh AD, Hurst JR. How to assess the severity of bronchiectasis. European Respiratory Journal 2014;43(5):1217‐9. [DOI: 10.1183/09031936.00226913] [DOI] [PubMed] [Google Scholar]
Savage 2014
- Savage E, Beirne PV, Ni Chroinin M, Duff A, Fitzgerald T, Farrell D. Self‐management education for cystic fibrosis. Cochrane Database of Systematic Reviews 2014, Issue 9. [DOI: 10.1002/14651858.CD007641.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sawicki 2009
- Sawicki DS, Sellers DE, Robinson WM. High treatment burden in adults with cystic fibrosis: challenges to disease self‐management. Journal of Cystic Fibrosis 2009;8(2):91‐6. [DOI: 10.1016/j.jcf.2008.09.007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Seitz 2010
- Seitz AE, Olivier KN, Steiner CA, Montes de Oca R, Holland SM, Prevots DR. Trends and burden of bronchiectasis‐associated hospitalizations in the United States. Chest 2010;138(4):944‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Seitz 2012
- Seitz AE, Olivier KN, Adjemian J, Holland SM, Prevots DR. Trends in bronchiectasis among Medicare beneficiaries in the United States, 2000‐2007. Chest 2012;142(2):432‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singleton 2000
- Singleton R, Morris A, Redding G, Poll J, Holck P, Martinez P, et al. Bronchiectasis in Alaska Native children: causes and clinical courses. Pediatric Pulmonology 2000;29(3):182‐7. [DOI] [PubMed] [Google Scholar]
Siu 2007
- Siu AMH, Chan CCH, Poon PKK, Chui DYY, Chan SCC. Evaluation of the chronic disease management programme in a Chinese population. Patient Education and Counseling 2007;65(1):42‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2014
- Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke HL, Schwappach A, et al. A rapid synthesis of the evidence on interventions supporting self‐management for people with long‐term conditions: PRISMS – Practical Systematic RevIew of Self‐Management Support for long‐term conditions. Health Services and Delivery Research 2014;2(53):1‐622. [PubMed] [Google Scholar]
Tunney 2013
- Tunney M. Lung microbiota and bacterial abundance in patients with bronchiectasis when clinically stable and during exacerbation. American Journal of Respiratory and Critical Care Medicine 2013;187(10):1118‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walters 2010
- Walters JA, Turnock AC, Walters EH, Wood‐Baker R. Action plans with limited patient education only for exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD005074.pub3] [DOI] [PubMed] [Google Scholar]
Welsh 2015
- Welsh EJ, Evans DJ, Fowler SJ, Spencer S. Interventions for bronchiectasis: an overview of Cochrane systematic reviews. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD010337.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Weycker 2005
- Weycker D, Edelsberg J, Oster G, Tino G. Prevalence and economic burden of bronchiectasis. Clinical Pulmonary Medicine 2005;12(4):205‐9. [Google Scholar]
Wilson 1997
- Wilson CB, Jones PW, O'Leary CJ, Cole PJ, Wilson R. Validation of the St. George's Respiratory Questionnaire in bronchiectasis. American Journal of Respiratory and Critical Care Medicine 1997;156(2):536‐41. [DOI] [PubMed] [Google Scholar]
Zwerink 2014
- Zwerink M, Brusse‐Keizer M, Valk PD, Zielhuis GA, Monninkhof EM, Palen J, et l. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2014, Issue 3. [DOI: 10.1002/14651858.CD002990.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]


