Abstract
Background
A Class II division 2 malocclusion is characterised by upper front teeth that are retroclined (tilted toward the roof of the mouth) and an increased overbite (deep overbite), which can cause oral problems and may affect appearance.
This problem can be corrected by the use of special dental braces (functional appliances) that move the upper front teeth forward and change the growth of the upper or lower jaws, or both. Most types of functional appliances are removable and this treatment approach does not usually require extraction of any permanent teeth. Additional treatment with fixed braces may be necessary to ensure the best result.
An alternative approach is to provide space for the correction of the front teeth by moving the molar teeth backwards. This is done by applying a force to the teeth from the back of the head using a head brace (headgear) and transmitting this force to part of a fixed or removable dental brace that is attached to the back teeth. The treatment may be carried out with or without extraction of permanent teeth.
If headgear use is not feasible, the back teeth may be held in place by bands connected to a fixed bar placed across the roof of the mouth or in contact with the front of the roof of the mouth. This treatment usually requires two permanent teeth to be taken out from the middle of the upper arch (one on each side).
Objectives
To establish whether orthodontic treatment that does not involve extraction of permanent teeth produces a result that is any different from no orthodontic treatment or orthodontic treatment involving extraction of permanent teeth, in children with a Class II division 2 malocclusion.
Search methods
Cochrane Oral Health's Information Specialist searched the following electronic databases: Cochrane Oral Health's Trials Register (to 13 November 2017), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2017, Issue 10), MEDLINE Ovid (1946 to 13 November 2017), and Embase Ovid (1980 to 13 November 2017). To identify any unpublished or ongoing trials, the US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch) were searched. We also contacted international researchers who were likely to be involved in any Class II division 2 clinical trials.
Selection criteria
Randomised controlled trials (RCTs) and controlled clinical trials (CCTs) of orthodontic treatments to correct deep bite and retroclined upper front teeth in children.
Data collection and analysis
Two review authors independently screened the search results to find eligible studies, and would have extracted data and assessed the risk of bias from any included trials. We had planned to use random‐effects meta‐analysis; to express effect estimates as mean differences for continuous outcomes and risk ratios for dichotomous outcomes, with 95% confidence intervals; and to investigate any clinical or methodological heterogeneity.
Main results
We did not identify any RCTs or CCTs that assessed the treatment of Class II division 2 malocclusion in children.
Authors' conclusions
There is no evidence from clinical trials to recommend or discourage any type of orthodontic treatment to correct Class II division 2 malocclusion in children. This situation seems unlikely to change as trials to evaluate the best management of Class II division 2 malocclusion are challenging to design and conduct due to low prevalence, difficulties with recruitment and ethical issues with randomisation.
Plain language summary
Orthodontic treatment for deep bite and retroclined upper front teeth in children
Background
Orthodontics is concerned with growth of the jaws and face, development of the teeth, and the way teeth and jaws bite together. Ideally, the lower front teeth bite in the middle of the back surface of the upper front teeth. When the lower front teeth bite further behind the upper front teeth than ideal, this is known as a Class II malocclusion. A Class II division 2 malocclusion is characterised by upper front teeth that are retroclined (tilted toward the roof of the mouth) and an increased overbite (vertical overlap of the front teeth), which can cause oral problems and may affect appearance.
This problem can be corrected by the use of special dental braces (functional appliances) that move the upper front teeth forward and change the growth of the upper or lower jaws, or both. These braces can be removed from the mouth and this approach does not usually require removal of any permanent teeth. Additional treatment with fixed braces may be necessary to ensure the best result.
An alternative approach is to provide space for the correction of the front teeth by moving the molar teeth backwards. This is done by applying a force to the teeth from the back of the head using a head brace (headgear) and transmitting this force to part of a fixed or removable dental brace that is attached to the back teeth. The treatment may be carried out with or without extraction of permanent teeth.
If headgear use is not feasible, the back teeth may be held in place by bands connected to a fixed arch placed across the roof of the mouth or in contact with the front of the roof of the mouth. This treatment usually requires two permanent teeth to be taken out from the middle of the upper arch (one on each side).
Aim
We carried out this Cochrane Review to find out if orthodontic treatment without the removal of permanent teeth had different effects than no orthodontic treatment or orthodontic treatment involving the removal of permanent teeth, in children with a Class II division 2 malocclusion.
Method
We searched the scientific literature up to 13 November 2017 and found no relevant studies to include in this review.
Results
There are no clinical trials that evaluate whether orthodontic treatment, carried out without the removal of permanent teeth, is better or worse than no orthodontic treatment or orthodontic treatment that involves taking out permanent teeth, in children with Class II division 2 malocclusion.
Author conclusions
There is no evidence from clinical trials to recommend or discourage any type of orthodontic treatment to correct the teeth of children whose bite is deep and whose upper front teeth are tilted towards the roof of the mouth. It seems unlikely that trials will be carried out to evaluate this treatment as they are challenging to design and conduct.
Summary of findings
Summary of findings for the main comparison. Orthodontic treatment for deep bite and retroclined upper front teeth in children.
| Orthodontic intervention (without extraction) compared with extraction or no orthodontic intervention for treating deep bite and retroclined upper front teeth in children | ||||||
|
Patient or population: children with deep bite and retroclined upper front teeth Settings: orthodontic clinic Intervention: orthodontic treatment Comparison: extraction or no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Extraction or no treatment | Orthodontic treatment | |||||
| Dento‐occlusal results of treatment, measured with the PAR index | No data are available as no RCTs or CCTs have been conducted. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; RCT: randomised controlled trial; CCT: controlled clinical trial | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Background
Orthodontics is the branch of dentistry concerned with the growth of the jaws and face, the development of the teeth, and the way the teeth and jaws bite together. It also involves treatment of the teeth and jaws when they are irregular or bite in an abnormal way, or both. Teeth may not bite together correctly due to any combination of problems in the positioning of the teeth, jaws, lips, tongue or cheeks; these can be affected in some cases by a habit, such as thumb sucking, or by the way in which people breathe (Shaw 1991). The need for orthodontic treatment can be determined by looking at the effect any particular tooth position has on the life expectancy of the teeth or by the effect that the appearance of the teeth has on how people feel about themselves, or both (Shaw 1991).
Description of the condition
Ideally the lower front teeth bite in the middle of the back surface of the upper front teeth. When the lower front teeth bite further behind the upper front teeth than ideal, this is known as a Class II malocclusion. The upper jaw can be too far forward or, more usually, the lower jaw is too far back. The upper front teeth may stick out (Class II division 1 malocclusion) if the lower lip catches behind them or as a result of a habit, such as thumb‐sucking (Shaw 1980). Management of prominent upper front teeth (Class II division 1 malocclusion) in children is the subject of a separate systematic review (Thiruvenkatachari 2013).
A Class II division 2 malocclusion is a type of orthodontic problem characterised by retroclined (tilted toward the roof of the mouth) upper front teeth and an increased overbite (vertical overlap of the front teeth), although there is variation in the severity of each of these (Millett 2012; Bilgic 2015; Dimberg 2015). Aesthetic impairments and trauma to the palatal or lower labial gingivae are frequently reported by people with this problem. Sometimes the deep overbite is so severe that the front teeth bite into the gums either behind the upper front teeth or in front of the lower front teeth producing damage (traumatic overbite) (Wragg 1990). The incidence of Class II division 2 malocclusion is reported to be about 10% within the UK population (Houston 1996), but prevalence of 18% has been reported in the Croatian population (Legovic 1999). Recent Swedish and Turkish studies have reported lower prevalence, from 1.8% to 4.7% (Bilgic 2015; Dimberg 2015). This type of malocclusion has a strong genetic link (Markovic 1992; Mossey 1999).
The appearance of the upper front teeth and the deep bite of the upper and lower front teeth are reasons why people with this type of problem seek orthodontic treatment (O'Brien 1993). Class II division 2 malocclusion is also associated with a greater percentage of upper permanent canines failing to erupt as a result of them following an abnormal pathway towards the palate/roof of the mouth (Mossey 1999; Al‐Nimri 2005).
Correction of the Class II division 2 malocclusion may be carried out using several types of orthodontic (dental brace) treatment, but the evidence regarding management is weak and highly biased (Millett 2012). People with severe Class II division 2 malocclusions may require surgery to the jaws in combination with orthodontics.
Description of the intervention
In growing children, treatment may sometimes be carried out using special upper and lower dental braces (functional appliances) that can be removed from the mouth (Dyer 2001). They usually work by correcting the position of the upper and lower front teeth and modifying the growth of the upper or lower jaws, or both (growth modification). In many cases this treatment does not involve taking out any permanent teeth but often further treatment is needed with fixed braces to get the best result; such braces are glued to the teeth.
In other cases, treatment aims to move the molar teeth backwards to provide space for the correction of the front teeth. This may be carried out by applying a force to the teeth and jaws from the back of the head using a head brace (headgear) and transmitting this force to part of a fixed or removable dental brace that is attached to the back teeth (Litt 1984). This treatment may or may not involve the removal of permanent teeth.
Other options do exist and may include fixed brace treatment without extraction of permanent teeth, with neither functional appliances nor headgear (Selwyn‐Barnett 1996).
As an alternative to headgear, the back teeth can be held back in other ways such as with an arch across the roof of the mouth or in contact with the front of the roof of the mouth which links the two back teeth. Often in these cases, two permanent teeth are taken out from the middle of the upper arch (one on each side) to provide room to correct the position of the upper front teeth (Paquette 1992).
In severe cases, particularly in adults, treatment may require a combination of dental braces and surgery to the jaws to correct the position of the teeth and the bite (Arvystas 1979). Our review does not evaluate this treatment option, which is not generally used for children.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were considered most clinically important to maintain on the Cochrane Library (Worthington 2015). The orthodontic expert panel identified this review as a priority title (Cochrane Oral Health priority review portfolio).
It is important for orthodontists to establish whether orthodontic treatment alone, carried out without the removal of permanent teeth, in children with a Class II division 2 malocclusion, produces a result that is any different from no orthodontic treatment or orthodontic treatment involving extraction of permanent teeth.
We did not consider combined orthodontic treatment and surgery to the jaws in this review.
Objectives
To evaluate the effectiveness of:
(1) orthodontic treatment only for Class II division 2 malocclusion in children (aged ≤ 16 years) versus no treatment in terms of:
dento‐occlusal results of treatment, measured with the Peer Assessment Rating (PAR) index;
cephalometric measurements (A Point‐Nasion‐B Point (ANB) change and front teeth inclination changes);
participant discomfort;
gingival and temporomandibular joint (TMJ) symptoms;
side effects;
quality of life;
(2) orthodontic treatment only for Class II division 2 malocclusion in children (aged ≤ 16 years) that does not involve extraction of permanent teeth versus orthodontic treatment involving extraction of permanent teeth in terms of:
dento‐occlusal results of treatment, measured with the PAR index;
number of visits to complete treatment;
duration of treatment;
cephalometric measurements (ANB change and front teeth inclination changes);
participant discomfort;
gingival and TMJ symptoms;
side effects;
quality of life.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and controlled clinical trials (CCTs) of orthodontic treatments to correct deep bite and retroclined upper front teeth in children.
Types of participants
We planned to include trials that recruited participants (80% aged ≤ 16 years) receiving orthodontic treatment to correct deep bite and retroclined upper front teeth.
We planned to exclude trials of participants with a cleft lip or palate, or both, or other craniofacial deformity/syndrome, and trials in which participants had received surgical treatment for their Class II malocclusion.
Types of interventions
Active interventions: orthodontic braces (removable, fixed, functional) or head braces with or without extraction of permanent teeth.
Control: no treatment or delayed treatment.
Types of outcome measures
Primary outcomes
Dento‐occlusal results of treatment, measured with the PAR index
Secondary outcomes
Number of visits required to complete treatment and the duration of treatment (for objective 2)
Cephalometric measurements (ANB change and front teeth inclination changes)
Participant discomfort
Gingival and TMJ symptoms
Side effects
Quality of life
Where appropriate, we planned to group outcome data into those measured post‐phase I (growth modification phase) and post‐phase II (fixed brace phase), to record and report post‐retention outcomes and to consider examining outcome data reported at other time points.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for RCTs and CCTs:
Cochrane Oral Health's Trials Register (searched 13 November 2017) (see Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 10) in the Cochrane Library (searched 13 November 2017) (see Appendix 2);
MEDLINE Ovid (1946 to 13 November 2017) (see Appendix 3);
Embase Ovid (1980 to 13 November 2017) (see Appendix 4).
No language, publication year or publication status restrictions were imposed.
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, we combined these strategies with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying RCTs and CCTs, as described in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
Searching other resources
The following resources were searched for ongoing trials:
US National Institutes of Health Trials Register (ClinicalTrials.gov; searched 13 November 2017) (see Appendix 5);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 13 November 2017) (see Appendix 6).
We planned to contact all first authors of trials in an attempt to identify any unpublished studies and clarify information about published trials (including missing data, method of randomisation, blinding and withdrawals). We intended to screen the references cited in the included studies for any further trials. We wrote to international researchers potentially involved in Class II division 2 malocclusion clinical trials in an attempt to identify unpublished/ongoing RCTs or CCTs.
A separate search for the adverse effects of interventions used was not performed.
Data collection and analysis
Selection of studies
Two review authors (DTM and CMO or SC) independently scanned the titles and abstracts (when available) of all reports identified. When studies appeared to meet the inclusion criteria, or there was insufficient information in the title and abstract to make a decision, we obtained the full report and two review authors assessed it independently to establish whether the inclusion criteria were met or not. We planned to resolve any disagreements by discussion, consulting a third review author if necessary. We had planned to carry out 'Risk of bias' assessments of all studies meeting the inclusion criteria, to extract relevant data and to record all studies rejected at this or subsequent stages in a table of excluded studies, together with the reasons for exclusion. The review authors were not to be blinded to author(s), institution or site of publication.
Data extraction and management
For each trial, we planned to enter the following information on a customised data collection form.
Year of publication, country of origin, setting and source of study funding.
Details on the type of interventions including appliance type.
Details of the participants including demographic characteristics, criteria for inclusion and exclusion, and sample size by study group.
Details of the outcomes reported, including method of assessment and time intervals.
Details of withdrawals by study group.
Details of outcomes, including measures and timepoints.
Assessment of risk of bias in included studies
We planned for two review authors to independently assess random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and 'other issues' for each study, using the 'Risk of bias' tool recommended for Cochrane Reviews (Higgins 2011). For blinding, we would have noted any outcomes where participants self‐assessed. We would have categorised the overall risk of bias for each study as follows.
| Risk of bias | Interpretation | Within a study | Across studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |
Measures of treatment effect
We planned to calculate risk ratios, the number needed to treat for an additional beneficial/harmful outcome and corresponding 95% confidence intervals, for dichotomous data, and the mean difference and 95% confidence intervals for continuous data. We would have used the fixed‐effect model for all meta‐analyses unless there were more than three trials included, in which case we would have used a random‐effects model.
Assessment of heterogeneity
We planned to assess heterogeneity using Cochran's test and the I2 statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than chance. We planned to assess clinical heterogeneity by examining the types of participants and interventions for all outcomes in each study.
Data synthesis
We planned to follow Cochrane statistical guidelines. We would have included only studies of similar comparisons reporting the same outcome measures in meta‐analyses. We planned to analyse the data using Review Manager software (RevMan 2014).
Subgroup analysis and investigation of heterogeneity
We planned a subgroup analysis based on the age (stage of dental development) at which treatment was undertaken.
Sensitivity analysis
We planned to conduct sensitivity analysis based on risk of bias (i.e. including studies at low risk of bias only).
Results
Description of studies
Results of the search
Through our searches and enquiries, we identified 928 references that were potentially relevant to our review. Two review authors (DTM and CMO or SC) screened these records and rejected them all. We were involved in a trial that we mentioned in a previous version of this review, but this was discontinued due to difficulties with patient recruitment (Cunningham 2011). Therefore, we have been unable to identify any RCTs or CCTs for inclusion in this review (Figure 1).
1.
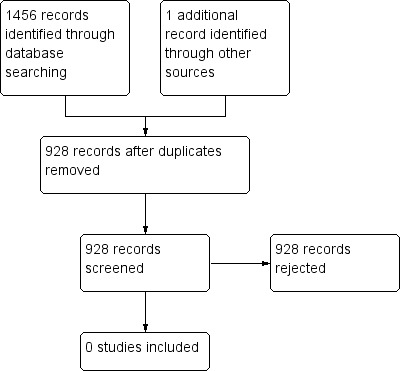
Study flow diagram
Risk of bias in included studies
No RCTs or CCTs were included in this review.
Effects of interventions
See: Table 1
No RCTs or CCTs were included in this review (Table 1).
Discussion
We found no RCTs or CCTs assessing i) orthodontic treatment without the removal of permanent teeth versus no treatment or ii) orthodontic treatment involving removal of permanent teeth versus treatment without the removal of permanent teeth. There is no evidence from clinical trials to guide the management of this malocclusion in children. It is unlikely that this situation will change as no trials have been conducted since we first identified the need for trials in the original version of this review, which was published in 2006.
Authors' conclusions
Implications for practice.
There is no evidence from clinical trials to establish whether orthodontic treatment that does not involve the removal of permanent teeth is better or worse than no orthodontic treatment or orthodontic treatment involving extraction of permanent teeth, in children with Class II division 2 malocclusion.
Implications for research.
The need for randomised controlled trials to investigate the management of Class II division 2 malocclusion in children is unlikely to be fulfilled. Design and conduct of a randomised trial is complicated by a number of factors including low prevalence, difficulties with recruitment, even in multicentre studies (Cunningham 2011; Millett 2012), and ethical issues with randomisation to different modes of treatment or to a control group. As recommended previously in a review of cohort studies and case series, standardised criteria with regard to the definition of Class II division 2 malocclusion should be specified in any study (Millett 2012). Future trials now seem unlikely, but If any are to be carried out, they should be designed, conducted and reported according to the criteria of the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
What's new
| Date | Event | Description |
|---|---|---|
| 8 March 2018 | Review declared as stable | There are no controlled trials that evaluate orthodontic treatment for deep bite and retroclined upper front teeth in children. The review is now considered 'stable' and will not be updated. |
History
Protocol first published: Issue 2, 2006 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 31 January 2018 | New citation required but conclusions have not changed | Search updated to 13 November 2017. This review has been updated several times and no controlled trials for orthodontic treatment for deep bite and retroclined upper front teeth in children have been identified. The review is now considered 'stable' and will not be updated. |
| 13 November 2017 | New search has been performed | Search updated ‐ no relevant studies identified |
| 3 July 2017 | New citation required but conclusions have not changed | No studies are included in this review |
| 10 January 2017 | New search has been performed | New search conducted |
| 28 November 2011 | New search has been performed | Methods updated. Electronic searches updated November 2011. No new trials identified for inclusion. |
| 5 January 2009 | Amended | Minor addition to Discussion. |
| 12 September 2008 | New search has been performed | Electronic searches updated to June 2008. |
| 12 September 2008 | Amended | Converted to new review format. |
Notes
This review is stable and will not be updated as no relevant studies have been identified in any search conducted since its first publication in 2006.
Acknowledgements
We wish to thank Sylvia Bickley and Anne Littlewood (Cochrane Oral Health) for their assistance with literature searching, and Luisa Fernandez Mauleffinch (Cochrane Oral Health) for help with the preparation of the review and Laura MacDonald (Cochrane Oral Health) for help with the preparation of updates. Thanks to Fang Hua for editorial comments and Gill Gummer for copy editing.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
From March 2014, searches of Cochrane Oral Health’s Trials Register were undertaken using the Cochrane Register of Studies and the search strategy below:
1 orthodontic*:ti,ab 2 (function* and appliance*):ti,ab 3 (remova* and appliance*):ti,ab 4 (fix* and appliance*):ti,ab 5 (orthodontic* and (extract* or remov*)):ti,ab 6 (band* or brace* or wire*):ti,ab 7 (function* and device*):ti,ab 8 (remova* and device*):ti,ab 9 (fix* and device*):ti,ab 10 ((intraoral or "intra oral" or intra‐oral or extraoral or "extra oral" or extra‐oral) AND (device* or appliance*)):ti,ab 11 "activator appliance*":ti,ab 12 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 13 "deep bite*":ti,ab 14 (increase* and bite*):ti,ab 15 (overbite* or over‐bite* or "over bite*" or overjet* or over‐jet* or "over jet*"):ti,ab 16 (("class 2" or "class II" and malocclusion) and ("division 2" or "division II")):ti,ab 17 ((teeth or tooth) AND (retro‐clin* or retroclin*)):ti,ab 18 ("short face syndrome*"):ti,ab 19 #13 or #14 or #15 or #16 or #17 or #18 20 #12 and #19
Previous searches of Cochrane Oral Health's Trials Register were performed using the Procite software and the search strategy below:
(orthodontic* or (function* and appliance*) or (remova* and appliance*) or (fix* and appliance*) or (orthodontic* and (extract* or remov*)) or (band* or brace* or wire*) or (function* and device*) or (remova* and device*) or (fix* and device*) or ((intraoral or "intra oral" or intra‐oral or extraoral or "extra oral" or extra‐oral) AND (device* or appliance*)) or "activator appliance*") AND ("deep bite*" or (increase* and bite*)) or (overbite* or over‐bite* or "over bite*" or overjet* or over‐jet* or "over jet*") or (("class 2" or "class II" and malocclusion) and ("division 2" or "division II")) or ((teeth or tooth) AND (retro‐clin* or retroclin*)) or ("short face syndrome*")
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor Orthodontics explode all trees #2 ((appliance* in All Text near/5 function* in All Text) or (appliance* in All Text near/5 remova* in All Text) or (appliance* in All Text near/5 fix* in All Text)) #3 (orthodontic* in All Text and (band* in All Text or brace* in All Text or wire* in All Text)) #4 (orthodontic* in All Text and (extract* in All Text or remov* in All Text)) #5 (orthodontic* in All Text and (headgear* in All Text or "head gear*" in All Text or head‐gear* in All Text or facemask* in All Text or "face mask*" in All Text or face‐mask* in All Text or chin‐cap* in All Text or chincap* in All Text or "chin cap*" in All Text or "face bow*" in All Text or facebow* in All Text or face‐bow* in All Text)) #6 ((device* in All Text near/5 function* in All Text) or (device* in All Text near/5 remova* in All Text) or (device* in All Text near/5 fix* in All Text)) #7 ((intraoral in All Text near/5 appliance* in All Text) or (intra‐oral in All Text near/5 appliance* in All Text) or ("intra oral" in All Text near/5 appliance* in All Text) or (extraoral in All Text near/5 appliance* in All Text) or ("extra oral" in All Text near/5 appliance* in All Text) or (extra‐oral in All Text near/5 appliance* in All Text) or (intraoral in All Text near/5 device* in All Text) or (intra‐oral in All Text near/5 device* in All Text) or ("intra oral" in All Text near/5 device* in All Text) or (extraoral in All Text near/5 device* in All Text) or ("extra oral" in All Text near/5 device* in All Text) or (extra‐oral in All Text near/5 device* in All Text)) #8 "activator appliance*" in All Text #9 (#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8) #10 ((deep in All Text near/3 bite* in All Text) or (increas* in All Text near/3 bite* in All Text)) #11 (overbite* in All Text or over‐bite* in All Text or "over bite*" in All Text or overjet* in All Text or over‐jet* in All Text or "over jet*" in All Text) #12 (("class II" in All Text near/3 malocclusion* in All Text) or (("class 2" in All Text near/3 malocclusion* in All Text) and ("division II" in All Text or "division 2" in All Text))) #13 ((teeth in All Text near/3 retro‐clin* in All Text) or (teeth in All Text near/3 retroclin* in All Text) or (incisor* in All Text near/3 retro‐clin* in All Text) or (incisor* in All Text near/3 retroclin* in All Text)) #14 "short face syndrome*" in All Text #15 (#10 or #11 or #12 or #13 or #14) #16 (#9 and #15)
Appendix 3. MEDLINE Ovid search strategy
1. exp Orthodontics/ 2. (appliance$ adj5 (function$ or remova$ or fix$)).mp. 3. (orthodontic$ and (brace$ or band$ or wire$)).mp. 4. (orthodontic$ and (extract$ or remov$)).mp. 5. (orthodontic$ and (headgear$ or "head gear$" or head‐gear$ or facemask$ or "face mask$" or face‐mask$ or chincap$ or "chin cap$" or chin‐cap$ or "face bow$" or face‐bow$ or facebow$)).mp. 6. (device$ adj5 (function$ or remova$ or fix$)).mp. 7. ((appliance$ or device$) adj5 (intraoral or "intra oral" or intra‐oral or extraoral or "extra oral" or extra‐oral)).mp. 8. (activator adj appliance$).mp. 9. or/1‐8 10. ((deep or increase$) adj3 bite$).mp. 11. (overbite$ or over‐bite$ or "over bite$" or overjet$ or over‐jet$ or "over jet$").mp. 12. ((("class II" or "class 2") adj3 malocclusion$) and ("division 2" or "division II")).mp. 13. ((teeth or incisor$) adj3 (retro‐clin$ or retroclin$)).mp. 14. "short face syndrome$".mp. 15. or/10‐14 16. 9 and 15
The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity‐maximising version (2008 revision), as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. exp Orthodontics/ 2. (appliance$ adj5 (function$ or remova$ or fix$)).mp. 3. (orthodontic$ and (brace$ or band$ or wire$)).mp. 4. (orthodontic$ and (extract$ or remov$)).mp. 5. (orthodontic$ and (headgear$ or "head gear$" or head‐gear$ or facemask$ or "face mask$" or face‐mask$ or chincap$ or "chin cap$" or chin‐cap$ or "face bow$" or face‐bow$ or facebow$)).mp. 6. (device$ adj5 (function$ or remova$ or fix$)).mp. 7. ((appliance$ or device$) adj5 (intraoral or "intra oral" or intra‐oral or extraoral or "extra oral" or extra‐oral)).mp. 8. (activator adj appliance$).mp. 9. or/1‐8 10. ((deep or increase$) adj3 bite$).mp. 11. (overbite$ or over‐bite$ or "over bite$" or overjet$ or over‐jet$ or "over jet$").mp. 12. ((("class II" or "class 2") adj3 malocclusion$) and ("division 2" or "division II")).mp. 13. ((teeth or incisor$) adj3 (retro‐clin$ or retroclin$)).mp. 14. "short face syndrome$".mp. 15. or/10‐14 16. 9 and 15
The above subject search was linked to adapted version of the Cochrane Embase Project filter for identifying RCTs in Embase Ovid (see http://www.cochranelibrary.com/help/central‐creation‐details.html for information):
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. US National Institutes of Health Trials Register (ClinicalTrials.gov) search strategy
(orthodontic and ("deep bite" or overbite or overjet or "over bite" or "over jet")) (orthodontic and ("class II division II" or "class 2 division 2”))
Appendix 6. WHO International Clinical Trials Registry Platform search strategy
orthodontic and “deep bite” or orthodontic and overbite or orthodontic and overjet or orthodontic and “over bite” or orthodontic and “over jet” orthodontic and class II division II orthodontic and class 2 division 2
Differences between protocol and review
The methods section of this review has been updated from the protocol in line with the latest version of the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) (Higgins 2011). 'Quality assessment' of included studies has been changed to 'Assessment of risk of bias of included studies'.
Contributions of authors
This review was conceived by Declan Millett (DTM), Kevin O'Brien (KOB) and Susan Cunningham (SC). The protocol was written by DTM, KOB and Cesar M de Oliveira (CMO). The review was co‐ordinated by DTM and CMO. DTM and CMO developed the search strategy with the help of Anne Littlewood (Sylvia Bickley in the original review), Information Specialist for Cochrane Oral Health, who undertook the electronic searches. DTM, SC, CMO, Philip E Benson (PEB), KOB and Alison Williams (AW). undertook handsearching. DTM and CMO or SC undertook screening of the search results. DTM, CMO, SC and KOB wrote the review.
Sources of support
Internal sources
University College Cork, Ireland.
University of London, UK.
The University of Manchester, UK.
University of Sheffield, UK.
External sources
-
Cochrane Oral Health Global Alliance, Other.
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships‐alliances). Contributors over the past year have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and NHS Education for Scotland, UK; Swiss Society of Endodontology, Switzerland.
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, the NIHR, the NHS or the Department of Health.
Declarations of interest
Declan T Millett: none known. Susan J. Cunningham: at the time of completing the update for this work (Jan 2018), Susan J Cunningham is a member of Council of the European Orthodontic Society and has just completed her term of office as a Trustee of the British Orthodontic Society. Kevin D O'Brien: none known. Philip E Benson: none known. Cesar M de Oliveira: none known.
Stable (no update expected for reasons given in 'What's new')
References
Additional references
Al‐Nimri 2005
- Al‐Nimri K, Gharaibeh T. Space conditions and dental and occlusal features in patients with palatally impacted maxillary canines: an aetiological study. European Journal of Orthodontics 2005;27(5):461‐5. [DOI] [PubMed] [Google Scholar]
Arvystas 1979
- Arvystas MG. Treatment of severe mandibular retrusion in class II, division 2 malocclusion. American Journal of Orthodontics 1979;76(2):149‐64. [DOI] [PubMed] [Google Scholar]
Bilgic 2015
- Bilgic F, Gelgor IE, Celebi AA. Malocclusion prevalence and orthodontic treatment need in central Anatolian adolescents compared to European and other nations' adolescents. Dental Press Journal of Orthodontics. 2015;20(6):75‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cunningham 2011
- Cunningham S, Bearn D, Benson P, Johal A, Millett D, O'Brien K, Luther F. In search of the sample: recent experiences of a trial team in orthodontics. Contemporary Clinical Trials 2011;32:530‐34. [DOI] [PubMed] [Google Scholar]
Dimberg 2015
- Dimberg L, Lennartsson B, Arnrup K, Bondemark L. Prevalence and change of malocclusions from primary to early permanent dentition: a longitudinal study. Angle Orthodontist 2‐15;85(5):728‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dyer 2001
- Dyer FM, McKeown HF, Sandler PJ. The modified twin block appliance in the treatment of Class II division 2 malocclusions. Journal of Orthodontics 2001;28(4):271‐80. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Houston 1996
- Houston WJB, Stephens CD, Tulley J. A Text Book of Orthodontics. Oxford (UK): Blackwell, 1996. [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. The Cochrane Collaboration, 2011.
Legovic 1999
- Legovic M, Mady L. Longitudinal occlusal changes from primary to permanent dentition in children with normal primary occlusion. Angle Orthodontist 1999;69(3):264‐6. [DOI] [PubMed] [Google Scholar]
Litt 1984
- Litt RA, Nielsen IL. Class II, division 2 malocclusion. To extract ‐ or not extract?. Angle Orthodontist 1984;54(2):123‐38. [DOI] [PubMed] [Google Scholar]
Markovic 1992
- Markovic M. At the crossroads of oral facial genetics. European Journal of Orthodontics 1992;14(6):469‐81. [DOI] [PubMed] [Google Scholar]
Millett 2012
- Millett DT, Cunningham SJ, O'Brien KD, Benson PE, Oliveira CM. Treatment and stability of class II division 2 malocclusion in children and adolescents: a systematic review. American Journal of Orthodontics and Dentofacial Orthopedics 2012;142(2):159‐69. [DOI: 10.1016/j.ajodo.2012.03.022] [DOI] [PubMed] [Google Scholar]
Mossey 1999
- Mossey PA. The heritability of malocclusion: part 2. The influence of genetics in malocclusion. British Journal of Orthodontics 1999;26(3):195‐203. [DOI] [PubMed] [Google Scholar]
O'Brien 1993
- O'Brien M. Children's Dental Health in the United Kingdom. London (UK): HMSO, 1993. [Google Scholar]
Paquette 1992
- Paquette DE, Beattie JR, Johnston LE Jr. A long‐term comparison of nonextraction and premolar extraction edgewise therapy in "borderline" Class II patients. American Journal of Orthodontics and Dentofacial Orthopedics 1992;102(1):1‐14. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager (RevMan) Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Selwyn‐Barnett 1996
- Selwyn‐Barnett BJ. Class II, division 2 malocclusion: a method of planning and treatment. British Journal of Orthodontics 1996;23(1):29‐36. [DOI] [PubMed] [Google Scholar]
Shaw 1980
- Shaw WC, Addy M, Ray C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dentistry and Oral Epidemiology 1980;8(1):36‐45. [DOI] [PubMed] [Google Scholar]
Shaw 1991
- Shaw WC, Richmond S, O'Brien KD, Brook P, Stephens CD. Quality control in orthodontics: indices of treatment need and treatment standards. British Dental Journal 1991;170(3):107‐12. [DOI] [PubMed] [Google Scholar]
Thiruvenkatachari 2013
- Thiruvenkatachari B, Harrison JE, Worthington HV, O'Brien KD, Worthington HV. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD003452.pub3] [DOI] [PubMed] [Google Scholar]
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision‐making. Evidence‐based Dentistry 2015;16(3):69‐71. [DOI] [PubMed] [Google Scholar]
Wragg 1990
- Wragg PF, Jenkins WM, Watson IB, Stirrups DR. The deep overbite: prevention of trauma. British Dental Journal 1990;168(9):365‐7. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Millett 2006
- Millett DT, Cunningham S, O'Brien KD, Benson PE, Oliveira CM. Orthodontic treatment for deep bite and retroclined upper front teeth in children. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD005972.pub2] [DOI] [PubMed] [Google Scholar]
Millett 2017
- Millett DT, Cunningham SJ, O'Brien KD, Benson PE, Oliveira CM. Orthodontic treatment for deep bite and retroclined upper front teeth in children. Cochrane Database of Systematic Reviews 2017, Issue 10. [DOI: 10.1002/14651858.CD005972.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]


