Abstract
Background
Approximately one‐third of individuals with interstitial lung disease (ILD) have associated connective tissue disease (CTD). The connective tissue disorders most commonly associated with ILD include scleroderma/systemic sclerosis (SSc), rheumatoid arthritis, polymyositis/dermatomyositis, and Sjögren's syndrome. Although many people with CTD‐ILD do not develop progressive lung disease, a significant proportion do progress, leading to reduced physical function, decreased quality of life, and death. ILD is now the major cause of death amongst individuals with systemic sclerosis.
Cyclophosphamide is a highly potent immunosuppressant that has demonstrated efficacy in inducing and maintaining remission in autoimmune and inflammatory illnesses. However this comes with potential toxicities, including nausea, haemorrhagic cystitis, bladder cancer, bone marrow suppression, increased risk of opportunistic infections, and haematological and solid organ malignancies.
Decision‐making in the treatment of individuals with CTD‐ILD is difficult; the clinician needs to identify those who will develop progressive disease, and to weigh up the balance between a high level of need for therapy in a severely unwell patient population against the potential for adverse effects from highly toxic therapy, for which only relatively limited data on efficacy can be found. Similarly, it is not clear whether histological subtype, disease duration, or disease extent can be used to predict treatment responsiveness.
Objectives
To assess the efficacy and adverse effects of cyclophosphamide in the treatment of individuals with CTD‐ILD.
Search methods
We performed searches on CENTRAL, MEDLINE, Embase, CINAHL, and Web of Science up to May 2017. We handsearched review articles, clinical trial registries, and reference lists of retrieved articles.
Selection criteria
We included randomised controlled parallel‐group trials that compared cyclophosphamide in any form, used individually or concomitantly with other immunomodulating therapies, versus non‐cyclophosphamide‐containing therapies for at least six months, with follow‐up of at least 12 months from the start of treatment.
Data collection and analysis
We imported studies identified by the search into a reference manager database. We retrieved the full‐text versions of relevant studies, and two review authors independently extracted data. Primary outcomes were change in lung function (change in forced vital capacity (FVC) % predicted and diffusing capacity of the lung for carbon monoxide (DLCO) % predicted), adverse events, and health‐related quality of life measures. Secondary outcomes included all‐cause mortality, dyspnoea, cough, and functional exercise testing. When appropriate, we performed meta‐analyses and subgroup analyses by severity of lung function, connective tissue disease diagnosis, and radiological pattern of fibrosis. We assessed the evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach and created 'Summary of findings' tables.
Main results
We included in the analysis four trials with 495 participants (most with systemic sclerosis). We formed two separate comparisons: cyclophosphamide versus placebo (two trials, 195 participants) and cyclophosphamide versus mycophenolate (two trials, 300 participants). We found evidence to be of low quality, as dropout rates were high in the intervention groups, and as we noted a wide confidence interval around the effect with small differences, which affected the precision of results.
The data demonstrates significant improvement in lung function with cyclophosphamide compared with placebo (post‐treatment FVC % mean difference (MD) 2.83, 95% confidence interval (CI) 0.80 to 4.87; P = 0.006) but no significant difference in post‐treatment DLCO (% MD ‐1.68, 95% CI ‐4.37 to 1.02; P = 0.22; two trials, 182 participants).
Risk of adverse effects was increased in the cyclophosphamide treatment groups compared with the placebo groups, in particular, haematuria, leukopenia, and nausea, leading to a higher rate of withdrawal from cyclophosphamide treatment. The data demonstrates statistically significant improvement in one‐measure of quality of life in one trial favouring cyclophosphamide over placebo and clinically and statistically significant improvement in breathlessness in one trial favouring cyclophosphamide compared with placebo, with no significant impact on mortality.
Trialists reported no significant impact on lung function when cyclophosphamide was used compared with mycophenolate at 12 months (FVC % MD ‐0.82, 95% CI ‐3.95 to 2.31; P = 0.61; two trials, 149 participants; DLCO % MD ‐1.41, 95% CI ‐10.40 to 7.58; P = 0.76; two trials, 149 participants).
Risk of side effects was increased with cyclophosphamide versus mycophenolate, in particular, leukopenia and thrombocytopenia.
The data demonstrates no significant impact on health‐related quality of life, all‐cause mortality, dyspnoea, or cough severity in the cyclophosphamide group compared with the mycophenolate group. No trials reported outcomes associated with functional exercise tests.
We performed subgroup analysis to determine whether severity of lung function, connective tissue disease diagnosis, or radiological pattern had any impact on outcomes. One trial reported that cyclophosphamide protected against decreased FVC in individuals with worse fibrosis scores, and also showed that cyclophosphamide may be more effective in those with worse lung function. No association could be made between connective tissue disease diagnosis and outcomes.
Authors' conclusions
This review, which is based on studies of varying methodological quality, demonstrates that overall, in this population, small benefit may be derived from the use of cyclophosphamide in terms of mean difference in % FVC when compared with placebo, but not of the difference in % DLCO, or when compared with mycophenolate. Modest clinical improvement in dyspnoea may be noted with the use of cyclophosphamide. Clinical practice guidelines should advise clinicians to consider individual patient characteristics and to expect only modest benefit at best in preserving FVC. Clinicians should carefully monitor for adverse effects during treatment and in the years thereafter.
Further studies are required to examine the use of cyclophosphamide; they should be adequately powered to compare outcomes within different subgroups, specifically, stratified for extent of pulmonary infiltrates on high‐resolution computed tomography (HRCT) and skin involvement in SSc. Studies on other forms of connective tissue disease are needed. Researchers may consider comparing cyclophosphamide (a potent immunosuppressant) versus antifibrotic agents, or comparing both versus placebo, in particular, for those with evidence of rapidly progressive fibrotic disease, who may benefit the most.
Plain language summary
Cyclophosphamide for interstitial lung disease associated with connective tissue disease
Background
People with connective tissue disease such as rheumatoid arthritis and systemic sclerosis may develop a group of lung diseases called interstitial lung disease. This can affect breathing and quality of life, and can lead to a reduced life span. A drug called cyclophosphamide has been useful in treating other illnesses, but it has side effects.
Review question
We wanted to know if cyclophosphamide helped preserve lung function in people with interstitial lung disease due to connective tissue disease. We also wanted to look at whether the drug causes side effects, and if it helps improve peoples' quality of life, length of life, breathing, and ability to exercise.
Study characteristics
We searched for studies up to May 2017, and we included four studies involving a total of 495 people with interstitial lung disease due to connective tissue disease. Some people were given cyclophosphamide, and others were given other drugs or a placebo. We compared these different groups to look for differences.
Key findings
We found some low‐quality evidence showing small benefit of using cyclophosphamide compared with placebo in terms of lung function and symptoms of breathlessness. No clear evidence shows that people who took cyclophosphamide had better lung function than people who took a different drug (mycophenolate mofetil). Some people experienced low blood counts, blood in their urine, and nausea.
Quality of the evidence
We rated the quality of the evidence using one of the following grades: very low, low, moderate, or high. A rating of very low‐quality evidence means that we are uncertain about the results. A rating of high‐quality evidence means that we are very certain about the results. For this Cochrane review, we found evidence of low quality. We included randomised controlled trials that were blinded, which means that participants and those people who assessed study results did not know whether participants had received cyclophosphamide or a placebo. However, the trials mostly included people with systemic sclerosis, so these results may not apply to all people with interstitial lung disease with connective tissue disease.
Summary of findings
Background
Description of the condition
Connective tissue disease (CTD) can affect any component of the respiratory tract, causing a diverse range of disorders. When it is associated with interstitial lung disease (ILD), CTD is classified within the current American Thoracic Society (ATS)/European Respiratory Society (ERS) consensus statement as one of the forms of diffuse parenchymal lung disease of known cause (ATS/ERS Consensus Statement). Approximately 30% of individuals with ILD have associated CTD, which presents subsequent to the development of ILD in about 15% of these individuals (Mittoo 2009).
Various approaches have been used to define connective tissue disease–associated interstitial lung disease (CTD‐ILD). The most rigorous approach includes only people with features that clearly meet published diagnostic criteria for systemic autoimmune disease. However, many people with ILD display one or more features of CTD clinically or serologically, without meeting diagnostic criteria. Amongst the definitions that have so far been applied to this cohort, significant heterogeneity in disease behaviour has been displayed, suggesting that further refinement is required to distinguish persons in this group with CTD‐ILD from those with idiopathic interstitial pneumonia (Corte 2012).
The connective tissue disorders most commonly associated with ILD include scleroderma/systemic sclerosis (SSc), rheumatoid arthritis, polymyositis/dermatomyositis, and Sjögren's syndrome. Each may be associated with progressive and fatal disease, but survival data in general are better than those reported for idiopathic forms of ILD (Fischer 2008; Park 2007). As an example, five‐year survival for people with systemic sclerosis–related ILD has been reported to be approximately 85%, as opposed to 50% for idiopathic disease (Wells 1994). It remains to be elucidated what features are the principal determinants of progression among people with CTD‐ILD. Histologically, non‐specific interstitial pneumonia, usual interstitial pneumonia (UIP), organising pneumonia, and lymphocytic interstitial pneumonia all may occur. Although for idiopathic interstitial pneumonia, UIP carries a significantly worse prognosis than other histological forms, with the exception of rheumatoid arthritis, a histological impact on prognosis is not seen in CTD‐ILD (Bongartz 2010; Bouros 2002; Kim 2010).
Despite resulting in better survival than its idiopathic counterparts, ILD is the major cause of death amongst individuals with systemic sclerosis (Ferri 2002). When present, ILD contributes to reduced physical function and quality of life (Baron 2008). Correlation has been demonstrated between extent of ILD and degree of disability, and this correlation serves as a predictor of disease behaviour. Radiological and physiological extent of ILD in cohorts with diagnoses of CTD and systemic sclerosis has been demonstrated to adversely affect prognosis (Goh 2008; Park 2007). Presence of greater than 20% disease extent on high‐resolution computed tomography (HRCT) and baseline forced vital capacity (FVC) < 70% have been demonstrated to predict mortality (Goh 2008). A greater rate of decline in physiological values such as FVC is a predictor of mortality in people with systemic sclerosis (Assassi 2010). A rate of decline > 10% in FVC or a 5% to 9% decline with a > 15% decline in diffusing capacity of the lung for carbon monoxide (DLCO) is predictive of mortality (Goh 2017).
Description of the intervention
Cyclophosphamide is a highly potent immunosuppressant that has demonstrated efficacy in inducing and maintaining remission in a range of autoimmune and inflammatory illnesses (Gourley 1996; Hoffman 1992). Its immunosuppressant activity may occur in a number of ways. Through its action as an alkylating agent, cyclophosphamide causes cross‐linkage of a variety of macromolecules, including DNA, producing cell death amongst resting and dividing lymphocytes. Additionally, it produces impaired humoral and cellular immune responses (Hall 1992).
Cyclophosphamide is associated with a range of significant toxicities that make its usage problematic, limiting its prescription to a specialist setting. Most patients experience nausea and hair thinning. Haemorrhagic cystitis and bladder cancer are produced by exposure of the bladder to acrolein, a metabolite of cyclophosphamide. The risk of each is related to total cumulative dose, with a total dosage greater than 100 grams most strongly associated with bladder cancer. To reduce total dosage, duration of cyclophosphamide usage is often limited to periods shorter than 12 months.
Cyclophosphamide causes bone marrow suppression with associated risks of bacterial and opportunistic infections, as well as reactivation of dormant infections such as tuberculosis. It is associated with gonadal toxicity with the potential to cause premature ovarian failure and oligospermia or azoospermia. It is teratogenic and should be avoided throughout pregnancy. Cyclophosphamide has been shown to increase risks of haematological malignancy, skin cancer, and solid organ malignancy.
Cyclophosphamide is administered in daily oral and intermittent intravenous protocols; intravenous regimens are preferred because they allow a reduction by up to two‐thirds of total cumulative dose, thereby reducing risks of malignancy and bladder toxicity (Boumpas 1992). The standard oral dosage for patients with normal renal function is 2 mg/kg/d, and intravenous doses range between 500 and 1000 mg/m2 body surface area administered every four to six weeks. Therapy generally is provided for at least six months and is followed by treatment with a less toxic alternative immunosuppressant.
How the intervention might work
On radiological grounds, fibrotic lung disease associated with CTD is similar to that seen in idiopathic interstitial pneumonia (Hwang 2009). Similar pathways have been suggested in their causation, with elevated levels of a range of similar pro‐inflammatory and pro‐fibrotic cytokines such as transforming growth factor (TGF)‐beta signalling pathways, along with growth factors and chemokines, involved in connective tissue deposition (Mathai 2010; Murray 2011; Peng 2011).
Despite these similarities, recent research has highlighted genetic differences in the MUC5‐B (mucin 5B, oligomeric mucus/gel‐forming gene) promoter region between idiopathic pulmonary fibrosis (IPF) and systemic sclerosis‐related ILD (Stock 2013). Histological differences are apparent, with CTD‐ILD demonstrating an increase in germinal centre density and inflammation and reduced numbers of fibroblastic foci (Song 2009). These differences suggest an alternative "inflammatory" pathogenesis that is likely crucial in providing any basis for improved natural history and responsiveness to immunosuppressant therapy amongst those with CTD‐ILD. Various immunosuppressant approaches have been used to treat people with IPF, and each has demonstrated a disappointing lack of efficacy (Raghu 2012). Only limited data can be found for most of the immunosuppressant therapies used in CTD‐ILD, but supportive case series data are available for several of them, including prednisolone, methotrexate, azathioprine, cyclosporine, and mycophenolate mofetil (Fischer 2013). Cyclophosphamide has significantly greater literature exploring its use, including several placebo‐controlled trials in CTD‐ILD (Hoyles 2006; Tashkin 2006).
Why it is important to do this review
Decision‐making in the treatment of people with CTD‐ILD is difficult, and the clinician must balance a high level of need for therapy in a severely unwell patient population against the potential for adverse effects from highly toxic therapy, for which only relatively limited data on efficacy can be found. Research in this field has been limited, with publications frequently representing case reports or case series. It is not clear whether evidence of efficacy in one CTD subtype can be extrapolated to all forms. Similarly, it is not clear whether histological subtype, disease duration, or disease extent can be used to predict responsiveness. Although these issues cannot currently be addressed in the absence of sufficient clinical studies, improved understanding of the strength of the treatment effect of cyclophosphamide in CTD‐ILD, as well as the extent to which adverse effects can be expected, would be of great assistance in clinical decision‐making.
Objectives
To assess the efficacy and adverse effects of cyclophosphamide in the treatment of individuals with CTD‐ILD.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled parallel‐group trials.
Types of participants
We included all adults (18 to 80 years of age) with a diagnosis of CTD‐ILD. We included only individuals with definitive connective tissue disease as defined by accepted diagnostic criteria at the time studies were identified. We included the connective tissue diseases commonly associated with interstitial lung disease: systemic sclerosis, rheumatoid arthritis, polymyositis/dermatomyositis, Sjögren's syndrome, systemic lupus erythematosus (SLE), and mixed connective tissue disorders.
Types of interventions
We included comparisons of cyclophosphamide, intravenous or oral, used individually or concomitantly with other immunomodulating or immunosuppressant therapies for periods of at least six months and for follow‐up periods of at least 12 months. Comparator groups provided non–cyclophosphamide‐containing therapies.
Types of outcome measures
Primary outcomes
Change in lung function (forced vital capacity (FVC) % predicted and diffusing capacity of the lung for carbon monoxide (DLCO) % predicted)
Adverse events
Health‐related quality of life, as measured by validated questionnaires
Secondary outcomes
Survival and mortality (all‐cause)
Dyspnoea
Cough
Functional exercise tolerance (e.g. six‐minute walk test)
Search methods for identification of studies
Electronic searches
We identified trials by conducting searches of the following databases up to May 2017.
Cochrane Airways Register of Trials (all years to 2 May 2017).
Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library (May 2017).
MEDLINE (Ovid) (1946 to 2 May 2017).
Embase (Ovid) (1974 to 2 May 2017).
ClinicalTrials.gov and World Health Organization (WHO) trials portal to 2 May 2017.
We searched for grey literature through the Airways Register of Trials and the CENTRAL database. We have detailed our database search strategies in Appendix 1. We applied no restrictions on language of publication. When data were missing, we contacted trial investigators.
Searching other resources
We checked reference lists of all primary studies and review articles for additional references.
Data collection and analysis
Selection of studies
Two review authors (ING and HB) independently screened all abstracts to determine if they met the inclusion criteria. We sought full‐text publications of articles that potentially or definitely met review criteria. Two review authors (ING and HB) then reviewed these full‐text articles to determine eligibility. We resolved disagreements by discussion and consensus. We included in the review a Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) study flow diagram to document the screening process, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Data extraction and management
Two review authors (ING and HB) independently extracted data from the included studies. When appropriate, we imported data and pooled them in the Cochrane statistical software, Review Manager 5 (RevMan) for further analysis.
We documented study characteristics and outcome data by using a data collection form that we had piloted on one study included in the review.
We extracted the following data.
Methods: study design, duration of the study, study setting, and date of study.
Participants: number, mean age and age range, gender, and inclusion and exclusion criteria.
Intervention: intervention, dose, mode of administration, concomitant medications, and exclusions.
Outcomes: primary and secondary outcomes as specified, type of scale used, and time points collected.
Notes: funding for trials and any conflicts of interest for trial authors.
'Risk of bias' summary.
We extracted mean and standard deviation (SD) values from each study. When included studies reported standard error or confidence intervals (CIs), we converted these to SD values according to recommendations provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of risk of bias in included studies
Two independent review authors (ING and HB) assessed the included studies for risk of bias using the Cochrane 'Risk of bias' assessment tool (Higgins 2011). We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
We scored each of these domains separately as introducing low risk of bias, unclear risk of bias (insufficient information to make a judgement), or high risk of bias.
Measures of treatment effect
Continuous data
When possible, we pooled data from all studies. We presented results from continuous variables, such as FVC, using a random‐effects model, and calculated mean differences (MDs) with corresponding 95% CIs.
Dichotomous data
We presented dichotomous data, including adverse events, as Peto odds ratios (ORs) or risk differences (RDs) (to account for zero cells in analyses) when we could pool the data. When we were unable to pool data, we included these results in a descriptive analysis.
Unit of analysis issues
We analysed treatment effect measured 12 months post initiation of therapy and at other shared time points, depending on available data.
Dealing with missing data
We utilised data as presented in published articles and in their supplementary appendices, and we contacted trial investigators to request further data.
Assessment of heterogeneity
We used the I² statistic to measure heterogeneity among the trials in each analysis. When we identified substantial heterogeneity (i.e. I² statistic > 50%), we explored between‐trial differences by performing subgroup analyses and removing potentially substantially different studies.
Assessment of reporting biases
We planned to perform funnel plot analysis to assess for reporting bias; however, given that only four studies were available, this was not possible.
Data synthesis
We performed a pooled quantitative analysis when possible. We synthesised a summary of findings table for change in FVC % predicted and DLCO % predicted, adverse events, and health‐related quality of life using the methods and recommendations described in the Cochrane Handbook for Systematic Reviews of Interventions, along with GRADEpro software (GradePro GDT 2015).
Subgroup analysis and investigation of heterogeneity
We had planned to analyse data according to the following subgroups.
FVC < 70% predicted.
Analysis by connective tissue disease diagnosis: systemic sclerosis, rheumatoid arthritis, polymyositis/dermatomyositis.
Analysis by radiological pattern: usual interstitial pneumonia (UIP), non‐UIP.
CTD symptom onset date within two years.
We planned to use the following parameters.
Change in lung function (FVC and DLCO).
Adverse events.
Health‐related quality of life.
However, data were insufficient for review authors to perform such meta‐analyses.
Sensitivity analysis
We planned to perform sensitivity analyses by excluding studies that did not use an intention‐to‐treat analysis or that had high risk of bias. However, given only two studies per comparison group, we found that data were insufficient for this approach.
Results
Description of studies
This review is based on a previously published protocol (Glaspole 2014).
Results of the search
We identified 1149 citations in the initial search, and after screening abstracts, we selected 39 studies for full‐text review. We included four trials with 495 participants in the final meta‐analysis; this included 26 separate citations, including protocols, early abstracts, and further analyses of other secondary outcomes (see Figure 1). We also noted two ongoing studies (see Characteristics of ongoing studies).
1.
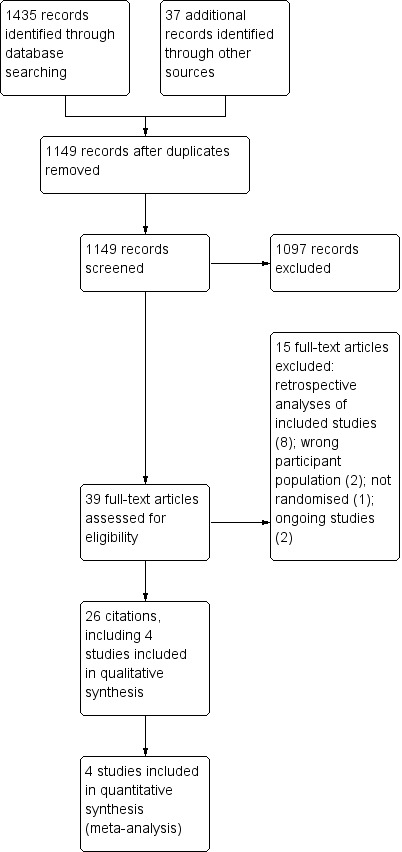
Study flow diagram.
Included studies
We included four trials with 495 participants in the final meta‐analysis (see Characteristics of included studies). All four included studies were randomised, parallel trials involving adults with a diagnosis of connective tissue disease according to accepted criteria, and with evidence of interstitial lung disease according to high‐resolution computed tomography (HRCT), lung biopsy, or evidence of active alveolitis on bronchoalveolar lavage. Three studies included only participants with systemic sclerosis (Hoyles 2006; Tashkin 2006; Tashkin 2016), and one study included participants with systemic sclerosis, dermatomyositis/polymyositis, systemic lupus erythematosus (SLE), and rheumatoid arthritis (RA) (Zhang 2015); however, we did not analyse these subgroups separately. Two studies included only participants with impaired lung function (FVC 45% to 85%), and two studies included participants with any lung function (Hoyles 2006; Zhang 2015). Zhang 2015 further analysed outcomes according to forced expiratory volume in one second (FEV1) > 75% and ≤ 75% in subgroup analyses.
Intervention protocols varied across trials. Tashkin 2006 compared oral cyclophosphamide daily (dosed by weight according to standard protocols) versus placebo for 12 months. Tashkin 2016 compared daily oral cyclophosphamide (dosed by weight), followed by oral placebo, for 12 months, versus oral mycophenolate (500 mg twice daily up‐titrated to 1.5 mg twice daily) for 24 months. Hoyles 2006 compared prednisolone (20 mg alternate daily) plus six cycles of IV cyclophosphamide four‐weekly, then oral azathioprine for 12 months, versus placebo, for 12 months. Zhang 2015 compared intravenous (IV) cyclophosphamide for 12 months versus oral mycophenolate (1.5 g daily) for 12 months; in addition, all participants in intervention and control groups received prednisolone, with the starting dose titrated according to disease severity (as deemed by trial doctors) and all participants weaned to 10 mg daily within four weeks.
All four trials included the primary outcome of change in lung function (FVC % predicted and DLCO % predicted). One study reported both change from baseline and post‐treatment change at 12 months (Tashkin 2006), another study reported this as change from baseline at 12 months (Tashkin 2016), and two studies reported post‐treatment change at 12 months (Hoyles 2006; Zhang 2015).
All four studies reported adverse events.
Tashkin 2006 and Tashkin 2016) reported health‐related quality of life outcomes using the Health Assessment Questionnaire (HAQ‐DI: a disease‐specific musculoskeletal targeted measure designed to test functional ability, where 0 = no disability and 3 = severe disability, with mean clinically important difference (MCID) for systemic sclerosis = 0.10 to 0.14 (Khanna 2006)), and Tashkin 2006 used Short Form (SF)‐36 (a generic measure of health‐related quality of life with both physical and mental components; higher score indicates less disability; MCID = 2.5 to 5.0 with different types of arthritis (Khanna 2009)).
In terms of secondary outcomes, all four studies reported mortality at 12 months. Three trials reported dyspnoea; Hoyles 2006 used a modified American Thoracic Society (ATS) respiratory questionnaire (0 = breathlessness after 30 minutes of vigorous activity, 20 = breathlessness after minimal activity; MCID not available); Tashkin 2006 and Tashkin 2016 used Mahlers Dyspnoea Index, renamed the Transition Dyspnoea Index (12‐point scale from ‐9 to +9; lower score indicates worse dyspnoea; MCID = 1.5 (Khanna 2009)).
Two trials reported cough using the modified cough index (0 to 3, with 3 = most severe) (Tashkin 2006; Tashkin 2016).
No studies reported functional exercise tolerance.
Excluded studies
We excluded 15 studies for the following reasons: retrospective analyses of data from studies already included (8); wrong participant population (2); only a protocol of an included study (2); not a randomised trial (1); and ongoing studies (2) (see Characteristics of excluded studies).
Risk of bias in included studies
We assessed risk of bias in the included studies using the Cochrane 'Risk of bias' assessment tool (Higgins 2011), including the domains of allocation, blinding, incomplete outcome data, selective reporting, and other bias. Please see Figure 2 and Figure 3 for a summary of 'Risk of bias' findings.
2.
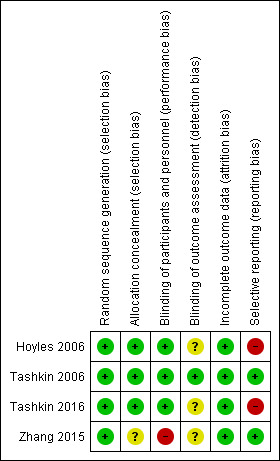
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
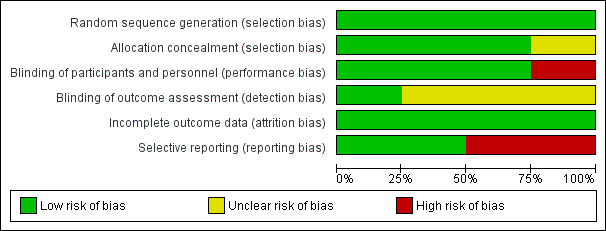
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
We assessed random sequence generation as low risk for four studies. We assessed allocation concealment as low risk for three studies ‐ Hoyles 2006; Tashkin 2006; and Tashkin 2016 ‐ and as unclear risk for one study ‐ Zhang 2015 ‐ as trial authors did not report allocation concealment.
Blinding
We assessed blinding of participants as low risk in three studies ‐ Hoyles 2006; Tashkin 2006; and Tashkin 2016 ‐ and as high risk for one study ‐ Zhang 2015 ‐ as one intervention was intravenous and control was oral, and trial authors did not mention blinding, so it was likely participants knew what intervention they were receiving. When IV and oral preparations were used in Hoyles 2006, researchers specifically used a placebo IV and oral formulation to reduce risk of bias. We assessed blinding of outcome assessors as low risk in Tashkin 2006 and as unclear risk in Hoyles 2006, Tashkin 2016, and Zhang 2015, as trial authors did not provide a clear statement.
Incomplete outcome data
We assessed attrition bias as low risk in all four studies. Tashkin 2006 and Tashkin 2016 reported more withdrawals in the intervention group than in the control group, and this may have introduced bias or affected the 'real‐world' tolerability of the intervention. In Tashkin 2006, a total of 20 of 79 participants in the cyclophosphamide group and 13 of 79 participants in the placebo group withdrew within 12 months after randomisation, most because of adverse events or serious adverse events. In Tashkin 2016, a total of 15 of 73 participants in the cyclophosphamide group and 7 of 69 participants in the mycophenolate group withdrew within 12 months after randomisation owing to serious adverse events. However in Tashkin 2006, investigators fitted a generalised estimating equation regression model for participants who withdrew prematurely, and imputed data missing at 12 months for the primary outcome; analysis included 73 participants in the treatment group and 72 in the control group. Tashkin 2016 performed a modified intention‐to‐treat analysis by using an inferential joint model consisting of a mixed‐effects model for longitudinal outcomes and a survival model to handle non‐ignorable missing data due to study dropout, treatment failure, or death (i.e. likely related to disease or treatment, and therefore not random). Hoyles 2006 and Zhang 2015 completely reported outcomes and a low withdrawal rate showing similar numbers distributed across intervention and control groups.
Selective reporting
We assessed selective reporting bias as low risk in Tashkin 2006 and Zhang 2015, as trial authors reported all prespecified outcomes. We assessed reporting bias as high risk in Hoyles 2006 and Tashkin 2016, as some prespecified quality of life outcomes reported as measured were not reported in the final manuscript (Tashkin 2016), and as some outcomes were recorded at more regular intervals than were reported (Hoyles 2006).
Effects of interventions
Summary of findings for the main comparison. Cyclophosphamide compared with placebo for connective tissue disease–associated interstitial lung disease.
| Cyclophosphamide compared with placebo for connective tissue disease–associated interstitial lung disease | |||||
| Patient or population: people with connective tissue disease‐associated interstitial lung disease Setting: community Intervention: cyclophosphamide Comparison: placebo | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) Follow‐up | Quality of the evidence (GRADE) | |
| Risk with placebo | Risk difference with cyclophosphamide | ||||
| Change in lung function (FVC % predicted) 12‐month follow‐up |
‐ | MD in FVC was 2.83% higher (0.80 lower to 4.87 higher) | ‐ | 182 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Change in lung function (diffusing capacity of the lung for carbon monoxide (DLCO) % predicted) 12‐month follow‐up |
‐ | MD in DLCO was 1.66% lower (4.39 lower to 1.07 higher) | ‐ | 182 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Adverse events: pneumonia 12‐month follow‐up |
49 per 1000 | 32 more per 1000 (21 fewer to 166 more) | OR 1.70 (0.55 to 5.32) | 203 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Adverse events: haematuria 12‐month follow‐up |
88 per 1000 | 113 more per 1000 (10 more to 280 more) | OR 2.60 (1.12 to 6.03) | 203 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Health‐related quality of life (HAQ‐DI) 12‐month follow‐up |
MD in HAQ‐DI was 0.27 lower (0.42 lower to 0.12 lower) | ‐ | 158 (1 RCT) | ⊕⊕⊕⊝ MODERATEa | |
| All‐cause mortality 12‐month follow‐up |
34 per 1000 | 2 fewer per 1000 (28 fewer to 111 more) | OR 0.94 (0.19 to 4.77) | 179 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DLCO: diffusing capacity of the lung for carbon monoxide; FVC: forced vital capacity; HAQ‐DI: Health‐Related Quality of Life Index; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect, Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | |||||
aThe study population included well, stable participants, and results may not be directly applicable to the general patient population.
bConfidence intervals are wide, and the population size is small.
Summary of findings 2. Cyclophosphamide compared with mycophenolate for connective tissue disease–associated interstitial lung disease.
| Cyclophosphamide compared with mycophenolate for connective tissue disease–associated interstitial lung disease | |||||
| Patient or population: people with connective tissue disease‐associated interstitial lung disease Setting: community Intervention: cyclophosphamide Comparison: mycophenolate | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) Follow‐up | Quality of the evidence (GRADE) | |
| Risk with mycophenolate | Risk difference with cyclophosphamide | ||||
| Change in lung function (FVC % predicted) 12‐month follow‐up |
‐ | MD 0.82% lower (3.95 lower to 2.31 higher) |
‐ | 149 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Change in lung function (diffusing capacity of the lung for carbon monoxide (DLCO) % predicted) 12‐month follow‐up |
‐ | MD 1.41% lower (10.4 lower to 7.58 higher) | ‐ | 145 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Adverse events: leukopenia 12‐month follow‐up |
27 per 1000 | 135 more per 1000 (56 more to 264 more) | OR 6.86 (3.23 to 14.58) | 300 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Adverse events: pneumonia 12‐month follow‐up |
103 per 1000 | 1 more per 1000 (51 fewer to 94 more) | OR 1.01 (0.48 to 2.14) | 300 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Adverse events: anaemia 12‐month follow‐up |
55 per 1000 | 32 more per 1000 (18 fewer to 138 more) | OR 1.63 (0.65 to 4.11) | 300 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| Adverse events: thrombocytopenia 12‐month follow‐up |
0 per 1000 | 30 more per 1000 (0 to 60 more) |
RD 0.03 (0.00 to 0.06) |
300 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b,c |
| Health‐related quality of life (HAQ‐DI) 12‐month follow‐up |
‐ | MD for HAQ‐DI was 0.05 lower (0.17 lower to 0.07 higher) |
‐ | 142 (1 RCT) | ⊕⊕⊝⊝ LOWa,b |
| All‐cause mortality 12‐month follow‐up |
88 per 1000 | 46 more per 1000 (29 fewer to 188 more) | OR 1.60 (0.65 to 3.95) | 187 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DLCO: diffusing capacity of the lung for carbon monoxide; FVC: forced vital capacity; HAQ‐DI: Health‐Related Quality of Life Index; MD: mean difference; OR: odds ratio; RCT: randomised controlled trial; RD: risk difference; RR: risk ratio. | |||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | |||||
aThe study population included well, stable participants, and results may not be directly applicable to the general patient population.
bConfidence intervals are wide, and the population size is small.
cSubstantial statistical heterogeneity detected; I2 = 81%, but not downgraded as no heterogeneity when analysed as a ratio.
Cyclophosphamide versus placebo
Primary outcomes
Change in lung function
Two trials reported change in lung function when comparing cyclophosphamide versus placebo at 12 months (Hoyles 2006; Tashkin 2006). Tashkin 2006 reported percent change from baseline and mean post‐treatment values and performed a prespecified Huber covariance analysis to assess treatment effects, which was adjusted for baseline values of FVC, as the data were not normally distributed and included extreme values. Hoyles 2006 reported mean post‐treatment values and the mean treatment effect in FVC, using a covariance analysis adjusted for baseline values of FVC and treatment centre. Treatment effects were combined via the generic inverse method in Review Manager 5.
The mean difference in post‐treatment FVC % predicted between cyclophosphamide and placebo was 2.83 (95% CI 0.80 to 4.87; P = 0.006; two studies, 182 participants; see Figure 4), favouring cyclophosphamide. Studies showed no significant heterogeneity (I² = 0; P = 0.54). The mean difference in post‐treatment DLCO % predicted was ‐1.68 (95% CI ‐4.37 to 1.02; P = 0.22; two studies, 182 participants; see Figure 5). We noted no significant heterogeneity between studies (I² = 0%; P = 0.88).
4.
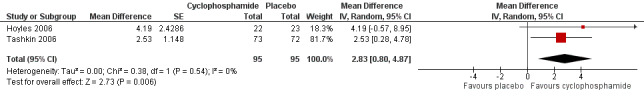
Forest plot of comparison: 1 Cyclophosphamide versus placebo, outcome: 1.1 FVC % predicted.
5.
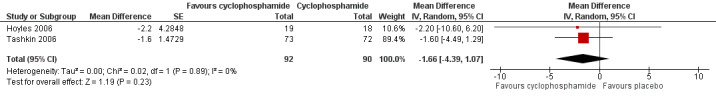
Forest plot of comparison: 1 Cyclophosphamide versus placebo, outcome: 1.2 DLCO % predicted.
Tashkin 2006 also reported outcomes at 24 months by performing a non‐parametric analysis using a modified Wilcoxon score test, in which FVC at 12 months and time to death were combined as a composite endpoint, and an extension of the covariance analysis in which the baseline score for fibrosis was accounted for. In this model, the adjusted mean absolute difference in FVC at 12 months between the two groups was 2.97% greater (95% CI 0.75 to 5.19), favouring cyclophosphamide (P = 0.009).
Adverse events
Two studies reported adverse events upon comparing cyclophosphamide with placebo at 12 months (Hoyles 2006; Tashkin 2006).
Risk of haematuria was significantly increased in the cyclophosphamide group compared with the placebo group at 12 months (Peto OR 2.60, 95% CI 1.12 to 6.03; P = 0.03; two studies, 195 participants) in the pooled meta‐analysis. Data show no significant difference in the risk of pneumonia (Peto OR 1.70, 95% CI 0.55 to 5.32; P = 0.27; two studies, 195 participants), but confidence intervals were wide.
Hoyles 2006 reported further adverse events at 12 months. Nausea was 11 times more likely in the cyclophosphamide group than in the placebo group (Peto OR 11.39, 95% CI 2.51 to 51.63; P = 0.002; 45 participants). Data show no significant differences in liver function disturbance (Peto OR 8.11, 95% CI 0.49 to 133.96; P = 0.14; 45 participants), but the effect estimate was highly imprecise.
Tashkin 2006 reported further adverse events. Leukopenia at 12 months was 10 times more likely in the cyclophosphamide group than in the placebo group (Peto OR 9.57, 95% CI 3.68 to 24.90; P < 0.00001; 158 participants). Data show no further events at 24 months. Neutropenia was eight times more likely at 12 months in the cyclophosphamide group than in the placebo group (Peto OR 8.00, 95% CI 1.77 to 36.24; P = 0.007; 158 participants). Trial authors reported no further events of neutropenia at 24 months.
Data show no significant differences in haematuria at 24 months (Peto OR 2.08, 95% CI 0.72 to 6.00; P = 0.18; 158 participants), nor in anaemia at 12 months (Peto OR 7.48, 95% CI 0.46 to 120.72; P = 0.16; 158 participants) or at 24 months (Peto OR 3.43, 95% CI 0.58 to 20.23; P = 0.17; 158 participants). However, events were rare, and results are uncertain.
In Tashkin 2006, 20 of 79 participants in the cyclophosphamide group and 13 of 79 participants in the placebo group withdrew within 12 months after randomisation, most because of adverse events or serious adverse events.
In Hoyles 2006, 2 of 22 participants in the cyclophosphamide group and 0 of 23 participants in the placebo group withdrew within 12 months after randomisation owing to adverse events.
Health‐related quality of life
Only one study with 158 participants reported health‐related quality of life when comparing cyclophosphamide versus placebo using the health assessment questionnaire (Tashkin 2006): Researchers used the disability index (HAQ‐DI), whereby lower score indicates less disability. The mean difference in change from baseline scores was clinically and statistically significant, with a mean difference of ‐0.27 favouring the cyclophosphamide group (95% CI ‐0.42 to ‐0.12; P < 0.0006; one trial, 158 participants). However, at baseline, data show a significantly lower score in the placebo group (indicating better health) than in the cyclophosphamide group.
Tashkin 2006 also reported change from baseline in the Short Form health survey (SF‐36; the lower the score, the greater the disability). Data show no significant differences in the change from baseline in the physical component of the SF‐36 between cyclophosphamide and placebo groups (MD 2.60, 95% CI ‐0.46 to 5.66; P = 0.10; 158 participants) and no significant differences in the mental component of the SF‐36 between cyclophosphamide and placebo groups (MD 2.09, 95% CI ‐2.07 to 6.25; P = 0.32; 158 participants).
Secondary outcomes
All‐cause mortality
Researchers reported no significant difference in all‐cause mortality between cyclophosphamide and placebo groups (Peto OR 0.94, 95% CI 0.19 to 4.77; P = 0.94; two trials, 179 participants), although the confidence interval does not rule out possible harm or benefit from the intervention.
Furst 2010 followed up the Sclerorderma Lung Study (SLS) I cohort for five years with respect to overall mortality and was able to follow‐up with 138 of 158 (87%) participants. Trial authors reported no significant differences between cyclophosphamide and placebo groups; 24 of 66 (36.4%) participants treated with cyclophosphamide had died compared with 22 of 72 placebo‐treated participants (30.6%; P = 0.46). This study did not report specific causes of death and adverse events (Furst 2010).
Dyspnoea
Tashkin 2006 reported dyspnoea outcomes, initially using the Mahler Dyspnoea Index, then using the Transitional Dyspnoea Index (TDI) (the lower the score, the worse the dyspnoea). Data show a significant difference in post‐treatment values favouring cyclophosphamide (MD 2.90, 95% CI 2.79 to 3.01; P < 0.00001; one study, 158 participants).
Cough
Tashkin 2006 reported cough as a percentage of participants affected. The percentage of participants with cough decreased in the cyclophosphamide group, from 71% at baseline to 56% at 12 months, but the percentage of participants in the placebo group with cough remained the same (68%) at both baseline and 12 months. This effect was lost at 24 months, correlating with loss of effect on FVC.
Functional exercise tests
No studies reported any outcome associated with functional exercise tests.
Cyclophosphamide versus mycophenolate
Primary outcomes
Change in lung function
Two trials reported change in lung function upon comparing cyclophosphamide versus mycophenolate (Tashkin 2016; Zhang 2015). Tashkin 2016 treated participants with cyclophosphamide for 12 months and with mycophenolate for 24 months, and Zhang 2015 treated participants with both cyclophosphamide and mycophenolate for 12 months. We reported change in lung function at both 12‐month follow‐up and end of study follow‐up. Tashkin 2016 reported adjusted outcomes using an inferential joint model consisting of a mixed‐effects model for longitudinal outcomes and a survival model to handle non‐ignorable missing data (due to study dropout, treatment failure, or death). Zhang 2015 reported post‐treatment outcomes but did not report baseline characteristics, so it was not clear whether they were similar across both groups. We combined treatment effects using the generic inverse method in Review Manager 5.
Data show no significant differences in FVC % predicted at 12 months (MD ‐0.82, 95% CI ‐3.95 to 2.31; P = 0.61; two trials, 149 participants; see Figure 6), or at end of study (MD ‐0.68, 95% CI ‐5.44 to 4.08; P = 0.78; two trials, 149 participants; see Figure 6). Data show no significant heterogeneity between trials (I² = 16%; P = 0.28 at 12 months; I² = 39%; P = 0.20, at end of study).
6.
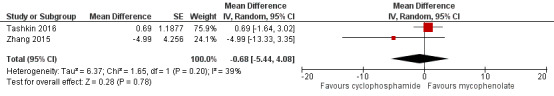
Forest plot of comparison: 2 Cyclophosphamide versus mycophenolate, outcome: 2.2 FVC % predicted at end of study.
Data show no significant differences in DLCO % predicted at 12 months (MD ‐1.41, 95% CI ‐10.40 to 7.58; P = 0.76; two trials, 149 participants), or at end of study (MD 2.04, 95% CI ‐1.11 to 5.19; P = 0.20; see Figure 7). We noted significant heterogeneity between trials at 12 months (I² = 76%; P = 0.006), whereby Tashkin 2016 reported a better effect with mycophenolate than with cyclophosphamide, but by 24 months, the effect favoured cyclophosphamide (I² = 0%; P = 0.60).
7.
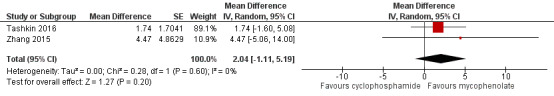
Forest plot of comparison: 2 Cyclophosphamide versus mycophenolate, outcome: 2.4 DLCO % predicted at end of study.
Adverse events
Two trials reported adverse events upon comparing cyclophosphamide versus mycophenolate at 12 months (Tashkin 2016; Zhang 2015).
Data show significantly more cases of leukopenia (Peto OR 6.86, 95% CI 3.23 to 14.58; P < 0.00001; two trials, 300 participants) and more cases of thrombocytopenia (RD 0.03, 95% CI ‐0.00 to 0.06; P = 0.10; two trials, 300 participants; I² = 81%) in the cyclophosphamide group than in the mycophenolate group in the pooled meta‐analysis. However, the confidence interval for thrombocytopaenia includes no difference, and we detected substantial statistical heterogeneity when analysing the outcome as a risk difference rather than as a ratio. Investigators reported no significant difference for risk of pneumonia (Peto OR 1.01, 95% CI 0.48 to 2.14; p = 0.97; two trials, 300 participants) or anaemia (Peto OR 1.63, 95% CI 0.65 to 4.11; two trials, p = 0.30; 300 participants) in the pooled meta‐analysis. Data show no significant difference in haematuria at 12 months (Peto OR 1.27, 95% CI 0.28 to 5.78; p = 0.76; one trial, 142 participants). However, as in other analyses, effect estimates for pneumonia, anaemia, and haematuria are imprecise.
Health‐related quality of life
Tashkin 2016 reported health‐related quality of life upon comparing cyclophosphamide versus mycophenolate using the health assessment questionnaire disability index (HAQ‐DI), whereby lower scores indicate less disability. Data show no significant difference in the change from baseline at 12 months between cyclophosphamide and mycophenolate (MD ‐0.05, 95% CI ‐0.17 to 0.07; P = 0.41; one trial, 142 participants).
Secondary outcomes
All‐cause mortality
Data show no significant differences in all‐cause mortality at 12 months between cyclophosphamide and mycophenolate (Peto OR 1.60, 95% CI 0.65 to 3.95; P = 0.31; two trials, 187 participants), but results are imprecise.
Dyspnoea
Tashkin 2016 reported Transition Dyspnoea Index change from baseline to 24 months (the lower the score, the worse the dyspnoea). Data show no significant differences between the cyclophosphamide group and the mycophenolate group (MD 0.39, 95% CI ‐0.68 to 1.46; P = 0.48; one trial, 142 participants).
Cough
Tashkin 2016 and Tashkin 2017 reported change in cough severity score from 6 to 18 months (the higher the score, the better the quality of life). They noted no significant differences between the cyclophosphamide group and the mycophenolate group (MD ‐0.17, 95% CI ‐0.39 to 0.05; P = 0.13; one trial, 142 participants).
Functional exercise tests
No studies reported any outcome associated with functional exercise tests.
Subgroup analysis
Severity of lung function (FVC < 70% predicted)
It was not possible to pool data to perform subgroup analysis based on severity of lung function owing to heterogeneity between trials.
Tashkin 2006 performed post hoc subgroup analysis using the joint longitudinal model, and noted that more severe restriction at baseline (FVC < 70% predicted) was associated with a greater difference in % FVC predicted at 12 months between cyclophosphamide and placebo (4.62% higher FVC % predicted in the cyclophosphamide group; P = 0.007) than was observed when the entire cohort was included in the analysis; and the cyclophosphamide treatment effect was even greater at 18 months (6.8% higher FVC % predicted; P = 0.006).
Zhang 2015 performed subgroup analysis for people who had FEV1 and FVC less than 75% predicted and found no significant differences between groups.
Hoyles 2006 did not perform subgroup analysis based on lung function.
Analysis by connective tissue disease diagnosis
Three studies recruited only participants with systemic sclerosis (Hoyles 2006; Tashkin 2006; Tashkin 2016). Zhang 2015 included participants with other connective tissue diseases but did not perform subgroup analysis. We contacted trial authors to request individual data; however, these data were not available at the time of review publication.
Analysis by radiological pattern
Tashkin 2006 performed baseline and post‐treatment fibrosis analysis using a Likert scale (0 = absent, 1 = 1% to 25%, 2 = 26% to 50%, 3 = 51% to 75%, and 4 = 76% to 100%) for extent of four categories of parenchymal abnormality, as indicated by:
pure ground glass opacity (pure GGO: hazy parenchymal opacity in the absence of reticular opacity or architectural distortion);
lung fibrosis (reticular opacification, traction bronchiectasis, and bronchiolectasis);
honeycombing (clustered air‐filled cysts with dense walls); and
emphysema (lucencies or cysts without walls).
Researchers performed scoring in each of three lung zones.
Upper (lung apex to aortic arch).
Middle (aortic arch to inferior pulmonary veins).
Lower (inferior pulmonary veins to diaphragm).
Regression analysis was performed to evaluate the effect of the baseline fibrosis score on FVC at 12 months. The regression slope in the placebo group was significantly negative (‐2.01% of predicted FVC per unit score of fibrosis; P = 0.006), indicating a greater decline in FVC over 12 months for those with a worse baseline fibrosis score. In the cyclophosphamide group, data show no relationship between fibrosis score and FVC progression. The difference between regression slopes in the two groups was significant (P < 0.009), suggesting that cyclophosphamide protected against the decrease in FVC seen in patients with more severe fibrosis.
No other study analysed changes in outcomes by radiological pattern subgroups.
Analysis by time of onset of CTD
Tashkin 2006 using SLS I data divided participants into three groups, depending on their duration of SSc (0 to 2 years, 2 to 4 years, > 4 years). Researchers used a mixed‐effects model to analyse the rate of decline in FVC% predicted over one year. Data show no significant differences in terms of the change in FVC between cyclophosphamide and placebo groups based on duration of SSc (P = 0.85) (Khanna 2011).
Sensitivity analysis
Data were insufficient for review authors to perform sensitivity analyses.
Discussion
Summary of main results
This Cochrane review has found that a small benefit may be derived from use of cyclophosphamide in people with connective tissue disease‐associated interstitial lung disease (CTD‐ILD) in mean difference in % forced vital capacity (FVC) when compared with placebo, but not in the difference in % diffusing capacity of the lung for carbon monoxide (DLCO) or mortality. Researchers have found no significant impact on lung function or mortality when compared with mycophenolate.
One trial reported a clinically and statistically significant improvement in breathlessness favouring cyclophosphamide compared with placebo (Tashkin 2006). Another trial found a statistically significant improvement in one measure of quality of life favouring cyclophosphamide compared with placebo (Tashkin 2006). Data show increased risk of side effects in the cyclophosphamide treatment groups, in particular, leukopenia, neutropenia, thrombocytopenia, and anaemia, leading to a higher rate of withdrawal from cyclophosphamide treatment.
This review, based on studies of varying methodological quality, demonstrates that overall, in the population studied, cyclophosphamide may provide a small benefit in terms of mean difference in % FVC when compared with placebo, but not in terms of the difference in % DLCO, or when compared with mycophenolate. Clinical improvement in dyspnoea may be seen with the use of cyclophosphamide.
Overall completeness and applicability of evidence
The conclusions drawn from this review are limited by the small number of trials, the small number of participants involved, and the imprecision of many effect estimates. Further high‐quality trials comparing cyclophosphamide versus placebo and other therapies are required.
In clinical practice, the decision to commence immunosuppression depends on factors that suggest risk of increased mortality, including the severity of disease at presentation and the presence of disease progression. Severity of CTD‐ILD can be derived by the degree of reduction in FVC and the extent of fibrosis evident on high‐resolution computed tomography (HRCT) (Goh 2017). Although two of the included studies included participants with moderately severe impairment in baseline FVC of 65% to 68% (Tashkin 2006; Tashkin 2016), the other two studies included participants with % FVC baseline of 80% (or not specified) (Hoyles 2006; Zhang 2015) ‐ above the threshold associated with increased mortality risk. Risk of mortality in CTD‐ILD is also increased by a recent decline in lung function over time (Goh 2017; Wells 2014). Although this is difficult to depict within the limitations of a clinical trial, the addition or augmentation of immunosuppression could be taken as evidence of recent disease progression. Each of the analysed studies excluded patients with a recent course of high‐dose immunosuppression, and it is probable that they included relatively stable or mildly impaired participants, as stated by Hoyles 2006. This also potentially blunts signals for efficacy, making it difficult to determine the applicability of our findings to a more progressive group, for whom immunosuppression is most likely to be considered.
At the other end of the spectrum, for patients with minor or subclinical disease, these studies suggest that the benefit of using cyclophosphamide compared with no therapy to reduce progression of disease is small and is associated with risk of adverse events. However, the effect is equivalent to that demonstrated by mycophenolate, although mycophenolate demonstrated has fewer adverse effects, suggesting that mycophenolate may be the preferable agent for these patients. Evidence extrapolated from this review is not clear on whether use of mycophenolate would be sufficient in rapidly progressive patients. The included trials involved mostly people with systemic sclerosis, so it is difficult to extrapolate these findings to people with CTD‐ILD from other causes.
Intervention protocols varied across trials, in terms of route of administration of cyclophosphamide used and co‐interventions. Tashkin 2006 and Tashkin 2016 used oral and Hoyles 2006 and Zhang 2015 used intravenous (IV) cyclophosphamide. Although IV cyclophosphamide is believed to have a better safety profile compared with oral cyclophosphamide, the data provided in this review do not address this issue, nor is it able to address whether one formulation is more efficacious than the other. Zhang 2015 and Hoyles 2006 added prednisolone for four weeks in both groups, which may have affected the treatment difference between cyclophosphamide and control groups. Hoyles 2006 utilised maintenance therapy with azathioprine, but the other trials did not. Zhang 2015 also included participants with a variety of different connective tissue diseases, which may have resulted in differences in clinical course and corticosteroid responsiveness compared with systemic sclerosis, making those findings potentially less applicable to individuals with systemic sclerosis.
A large number of participants withdrew from the included trials (25.3% in the cyclophosphamide group and 20.2% in the placebo group of Tashkin 2006 at one year, 43.8% in the cyclophosphamide group and 27.5% in the mycophenolate group of Tashkin 2016 at two years, 50% in each group in Hoyles 2006, and 15% in each group in Zhang 2015). Causes for withdrawal included adverse events, treatment failure, and participant preference.
The conclusions of this review are limited by the outcome measures used. None of the included trials used the six‐minute walk test or measured any other exercise capacity parameters, although musculoskeletal involvement in systemic sclerosis (SSc) may limit performance on exercise tests. It may have been useful to quantify use of rescue immunosuppression therapy or transplantation as other efficacy outcomes. Symptom and health‐related quality of life measurements were limited among the included studies, although we note that these data were collected in the Tashkin 2006 and Tashkin 2016 trials and may be published in future studies. The use of such patient‐reported outcomes has been recognised by the Food and Drug Administration (FDA) and OMERACT as of high clinical utility, and further trials should use well‐validated instruments to measure such outcomes, when available (Tugwell 2007). Quality of life data were limited and future trials should include these in their outcomes.
The primary outcome for most of these trials included change in FVC or DLCO. Some prospective studies have demonstrated that a greater rate of decline in FVC is a predictor of mortality among people with systemic sclerosis (Assassi 2010; Goh 2017). However, evidence regarding the clinical utility and reproducibility of FVC and DLCO is mixed. The British Thoracic Society (BTS) Interstitial Lung Diseases Guideline notes that pulmonary function testing is widely variable, particularly at the milder end of the spectrum, and that variable factors in connective tissue disease‐associated interstitial lung disease, including coexisting pulmonary vascular, muscular, and pleural disease, may render interpretation of pulmonary function testing and its true impact on the patient difficult (Wells 2008). Considerable intersubject and intrasubject variability may be observed in the rate of decline in lung function. Hence, FVC % as a predictor of mortality may not always correlate as a predictor of therapeutic response (Goh 2017; Nathan 2016).
The conclusions of this review are limited by the time points at which outcomes were measured. Tashkin 2006 demonstrated a small but significant effect with 12‐month treatment with cyclophosphamide compared with placebo at 12 months, which increased to 18 months, but this effect had largely dissipated by 24 months. Longer duration of benefit has been suggested by the Scleroderma Lung Study (SLS) II trial; however, owing to lack of placebo groups, it is difficult to draw definitive conclusions. In light of these results, different outcomes may be ascertained depending on which time points are utilised to measure outcomes. The duration of treatment with cyclophosphamide has been limited to 12 months owing to concerns about adverse events (Tashkin 2007). No studies have considered a second course of treatment for responders to cyclophosphamide to assess for further benefit or added risks. The cohort of SLS I was followed up to five years for mortality (Furst 2010); however, other trials have provided very limited follow‐up for efficacy and adverse events ‐ only to 12 months. When possible, the included trials should continue to monitor long‐term outcomes in these patients, and future trials should consider long‐term follow‐up.
We aimed to perform subgroup analysis to determine whether severity of lung function, connective tissue disease diagnosis, or radiological pattern had any impact on outcomes. Tashkin 2006 demonstrated that cyclophosphamide protected against decreased FVC among patients with worse fibrosis scores. Tashkin 2006 found that more severe restriction demonstrated on lung function tests (baseline FVC < 70% predicted) was associated with a greater difference in % FVC predicted at 12 months. Previous studies have found that the best predictors of disease progression and long‐term mortality correspond to the extent of reticular change seen on HRCT (> 20% involvement) and to impact on pulmonary function (< 70% FVC) (Goh 2008). Further publications on the SLS I data have examined subgroup analyses and found that those with worse pulmonary infiltrates on HRCT and those with greater skin involvement showed greater improvement in FVC. Duration of SSc appeared to have no correlation.
Quality of the evidence
Overall we found the evidence to be of low quality. We noted limitations in the directness of evidence, in terms of the population studied and outcomes used. Trials included participants with relatively stable disease, baseline lung function of 66% to 80% FVC, and no recent exacerbations or rescue immunosuppression therapy. None of the included trials used the six‐minute walk test or measured any other exercise capacity parameters, and symptom and health‐related quality of life measurements were limited. We also noted in many analyses a wide confidence interval around a small effect estimate, indicating imprecision.
Except for Zhang 2015 (in which risk of bias was unclear), included studies revealed no significant limitations in the way trials were conducted. We detected substantial heterogeneity in only one analysis (Analysis 2.8) but did not downgrade for inconsistency, as when data are analysed as a ratio heterogeneity is not a factor.
2.8. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 8 Thrombocytopenia.
Potential biases in the review process
We conducted this review in accordance with established Cochrane standards. Two review authors independently screened search results and resolved discrepancies by discussion and consensus. We did not restrict the literature search by language, and we translated one study into English to determine suitability for inclusion. Publication bias is possible, whereby failure to identify unpublished negative trials could have led to an overestimation of effect.
Agreements and disagreements with other studies or reviews
Evidence on long‐term treatment to reduce progression of disease is conflicting, is modest at best, and is based on small numbers of clinical, mostly non‐randomised controlled trials. Corticosteroids are commonly used, but little evidence supports their benefit (Mathai 2016). Azathioprine has demonstrated no significant benefit in randomised trials (Hoyles 2006). Cyclosporine and tacrolimus have demonstrated small benefit in retrospective studies on antisynthetase syndrome (Labirua‐Iturburu 2013). Retrospective studies have demonstrated benefit for oral cyclophosphamide followed by mycophenolate mofetil for treatment of inflammatory myopathies (Mira‐Avendano 2013). At present, few other treatments have demonstrated significant benefit in CTD‐ILD. Ongoing studies are examining the use of rituximab (Daoussis 2012; Jordan 2015; Maher 2015), nintedanib (NCT02597933), pirfenidone (NCT02808871), tocilizumab (Khanna 2015), abituzumab (NCT02745145), and autologous stem cell transplantation (van Laar 2014); these results remain to be published.
Authors' conclusions
Implications for practice.
This review, based on studies of varying methodological quality, demonstrates that overall, in the population studied, small benefit may be derived from the use of cyclophosphamide in terms of mean difference in % forced vital capacity (FVC) when compared with placebo, but not in terms of the difference in % diffusing capacity of the lung for carbon monoxide (DLCO), or when compared with mycophenolate. Mycophenolate may be as good as cyclophosphamide, although the evidence remains uncertain. Clinical improvement in dyspnoea may be seen with the use of cyclophosphamide. Clinical practice guidelines should advise clinicians to consider individual patient characteristics, and to expect only a modest benefit in slowing progression of FVC decline. Clinicians should carefully monitor for adverse effects during treatment and during the years thereafter.
Implications for research.
It is not clear whether evidence of efficacy in one connective tissue disease (CTD) subtype can be extrapolated to all forms. Similarly, it is not clear whether histological subtype, disease duration, or disease extent can be used to predict responsiveness to treatment. Further studies are required to consider which patient factors and future biomarkers might predict response to treatment. Although these issues cannot currently be answered in the absence of sufficient clinical studies, improved understanding of the strength of the treatment effect of cyclophosphamide in CTD‐interstitial lung disease (ILD), as well as the extent to which adverse effects can be expected, would be of great assistance in clinical decision‐making.
Further studies are required to examine the use of cyclophosphamide; they should be adequately powered to compare outcomes within different subgroup analyses, specifically, extent of pulmonary infiltrates seen on high‐resolution computed tomography (HRCT) and skin involvement in systemic sclerosis (SSc). Additional studies are also needed to examine other connective tissue disease not including SSc. Future studies may consider comparing cyclophosphamide (a potent immunosuppressant) with antifibrotic agents, or comparing both with either cyclophosphamide alone or placebo alone (although these studies may be limited by ethical implications). Given that the evidence presented in this review was derived mostly from well participants, future studies must examine treatments in those with evidence of progressive fibrotic disease, who may benefit the most.
Researchers should continue to monitor progress of lung disease by using respiratory function tests, HRCT, and patient‐centred outcomes, even after treatment has ceased, to determine whether these therapies have any long‐term impact in halting the progression of fibrosis. They should aim to determine the optimal treatment duration of such induction therapies, as well as the optimal combination and duration of maintenance therapies.
Future studies of predictors of disease behaviour across the spectrum of CTD‐ILD are vital not only to guide timely introduction of potentially toxic therapies but also to guide the optimal duration of therapies. These include not only currently used modalities of respiratory function tests and HRCT of the chest, but also patient factors, peripheral biomarkers, and genetic markers. Researcers must explore the effectiveness and safety of maintenance therapy following induction therapy with a relatively short course of a toxic agent, such as cyclophosphamide. Long‐term outcome studies (5 to 10 years), incorporating patient‐centred outcomes, following initiation of treatment are also important.
One of the challenges of doing research in this area is the small number of potential participants. This could be overcome by having national registries that would serve as an important conduit for identifying sufficient numbers of well‐characterised patients who are willing to participate in trials of treatment for rare lung diseases.
Acknowledgements
We thank the Cochrane Airways Team, including Rebecca Normansell, Emma Dennett, Christopher Cates, and Elizabeth Stovold, for their input in this review. Chris Cates was the Contact Editor for this review.
We thank Dr Jarrel Seah for his translations for the Zhang study.
We thank Professor Tashkin, who provided us with further unpublished data for the SLS I and SLS II trials.
We thank the Peer Reviewers for providing comments on this review.
The Background and Methods sections of this review are based on a standard template used by Cochrane Airways.
This project was supported by a generous grand from the Lung Foundation/Cochrane Airways Australia Scholarship.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health.
Appendices
Appendix 1. Database search strategies
Cochrane Airways Register
#1 ILD:MISC1 #2 MeSH DESCRIPTOR Lung Diseases, Interstitial Explode All #3 ILD:ti,ab #4 (pulmonary* or lung*) NEAR3 (fibros* or fibrot*) #5 sarcoidosis* or alveolitis* #6 #1 or #2 or #3 or #4 or #5 #7 MeSH DESCRIPTOR Cyclophosphamide Explode All #8 cyclophosphamide* #9 endoxan* #10 cytoxan* #11 Neosar #12 Procytox #13 Sendoxan #14 Clafen #15 #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 #16 #6 and #15 #17 (#16) AND (INREGISTER)
CENTRAL
#1 MeSH descriptor: [Lung Diseases, Interstitial] explode all trees #2 interstitial* near/3 (lung* or pulmonary* or pneumon*) #3 (pulmonary* or lung*) near/3 (fibros* or fibrot*) #4 sarcoidosis* #5 alveolitis* #6 ILD:ti,ab #7 {or #1‐#6} #8 MeSH descriptor: [Connective Tissue Diseases] explode all trees #9 (connective near/3 tissue near/3 (disorder* or disease*)) #10 scleroderma* #11 sclerosis* #12 systemic lupus erythematosus #13 Libman‐Sacks #14 rheumatoid arthritis #15 polymyositis #16 dermatomyositis #17 myositis #18 Sjogren's syndrome #19 {or #8‐#18} #20 MeSH descriptor: [Cyclophosphamide] explode all trees #21 cyclophosphamide* #22 endoxan* #23 cytoxan* #24 Neosar #25 Procytox #26 Sendoxan #27 Clafen #28 {or #20‐#27} #29 #7 and #19 and #28
MEDLINE (Ovid)
1. exp Lung Diseases, Interstitial/
2. (interstitial$ adj3 (lung$ or pulmonary$ or pneumon$)).tw.
3. ILD.ti,ab.
4. ((pulmonary$ or lung$) adj3 (fibros$ or fibrot$)).tw.
5. sarcoidosis$.tw.
6. alveolitis$.tw.
7. or/1‐6
8. exp Connective Tissue Diseases/
9. (connective adj3 tissue adj3 (disorder$ or disease$)).tw.
10. scleroderma.tw.
11. sclerosis.tw.
12. systemic lupus erythematosus.tw.
13. Libman‐Sacks.tw.
14. rheumatoid arthritis.tw.
15. polymyositis.tw.
16. dermatomyositis.tw.
17. myositis.tw.
18. Sjogren's syndrome.tw.
19. or/8‐18
20. 7 and 19
21. exp Cyclophosphamide/
22. cyclophosphamide.tw.
23. Endoxan.tw.
24. Cytoxan.tw.
25. Neosar.tw.
26. Procytox.tw.
27. Sendoxan.tw.
28. Clafen.tw.
29. or/21‐28
30. 20 and 29
31. (clinical trial or controlled clinical trial or randomised controlled trial).pt.
32. (randomised or randomised).ab,ti.
33. placebo.ab,ti.
34. dt.fs.
35. randomly.ab,ti.
36. trial.ab,ti.
37. groups.ab,ti.
38. or/31‐37
39. Animals/
40. Humans/
41. 39 not (39 and 40)
42. 38 not 41
43. 30 and 42
Embase (Ovid)
1. exp interstitial lung disease/ 2. (interstitial$ adj3 (lung$ or pulmonary$ or pneumon$)).tw. 3. ILD.ti,ab. 4. ((pulmonary$ or lung$) adj3 (fibros$ or fibrot$)).tw. 5. sarcoidosis$.tw. 6. alveolitis$.tw. 7. or/1‐6 8. exp connective tissue disease/ 9. (connective adj3 tissue adj3 (disorder$ or disease$)).tw. 10. scleroderma.tw. 11. sclerosis.tw. 12. systemic lupus erythematosus.tw. 13. Libman‐Sacks.tw. 14. rheumatoid arthritis.tw. 15. polymyositis.tw. 16. dermatomyositis.tw. 17. myositis.tw. 18. Sjogren's syndrome.tw. 19. or/8‐18 20. 7 and 19 21. exp cyclophosphamide/ 22. cyclophosphamide.tw. 23. Endoxan.tw. 24. Cytoxan.tw. 25. Neosar.tw. 26. Procytox.tw. 27. Sendoxan.tw. 28. Clafen.tw. 29. or/21‐28 30. 20 and 29 31. Randomized Controlled Trial/ 32. randomization/ 33. controlled clinical trial/ 34. Double Blind Procedure/ 35. Single Blind Procedure/ 36. Crossover Procedure/ 37. (clinica$ adj3 trial$).tw. 38. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (mask$ or blind$ or method$)).tw. 39. exp Placebo/ 40. placebo$.ti,ab. 41. random$.ti,ab. 42. ((control$ or prospectiv$) adj3 (trial$ or method$ or stud$)).tw. 43. (crossover$ or cross‐over$).ti,ab. 44. or/31‐43 45. exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 46. human/ or normal human/ or human cell/ 47. 45 and 46 48. 45 not 47 49. 44 not 48 50. 30 and 49
Data and analyses
Comparison 1. Cyclophosphamide versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 FVC % predicted | 2 | 190 | Mean Difference (Random, 95% CI) | 2.83 [0.80, 4.87] |
| 2 DLCO % predicted | 2 | 182 | Mean Difference (Random, 95% CI) | ‐1.66 [‐4.39, 1.07] |
| 3 Haematuria | 2 | 203 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.60 [1.12, 6.03] |
| 4 Pneumonia | 2 | 203 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.70 [0.55, 5.32] |
| 5 HAQ‐DI | 1 | Mean Difference (Fixed, 95% CI) | ‐0.27 [‐0.42, ‐0.12] | |
| 6 SF‐36: physical component | 1 | 158 | Mean Difference (IV, Fixed, 95% CI) | 2.60 [‐0.46, 5.66] |
| 7 SF‐36: mental component | 1 | 158 | Mean Difference (IV, Fixed, 95% CI) | 2.09 [‐2.07, 6.25] |
| 8 All‐cause mortality | 2 | 179 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.94 [0.19, 4.77] |
| 9 Breathlessness: Mahler Dyspnoea Index | 1 | 158 | Mean Difference (IV, Fixed, 95% CI) | 2.9 [1.95, 3.85] |
1.1. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 1 FVC % predicted.
1.2. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 2 DLCO % predicted.
1.3. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 3 Haematuria.
1.4. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 4 Pneumonia.
1.5. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 5 HAQ‐DI.
1.6. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 6 SF‐36: physical component.
1.7. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 7 SF‐36: mental component.
1.8. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 8 All‐cause mortality.
1.9. Analysis.
Comparison 1 Cyclophosphamide versus placebo, Outcome 9 Breathlessness: Mahler Dyspnoea Index.
Comparison 2. Cyclophosphamide versus mycophenolate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 FVC % predicted at 12 months | 2 | 149 | Mean Difference (IV, Random, 95% CI) | ‐0.82 [‐3.95, 2.31] |
| 2 FVC % predicted at end of study | 2 | Mean Difference (Random, 95% CI) | ‐0.68 [‐5.44, 4.08] | |
| 3 DLCO % predicted at 12 months | 2 | 154 | Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐10.40, 7.58] |
| 4 DLCO % predicted at end of study | 2 | Mean Difference (Random, 95% CI) | 2.04 [‐1.11, 5.19] | |
| 5 Leukopenia | 2 | 300 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 6.86 [3.23, 14.58] |
| 6 Pneumonia | 2 | 300 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.01 [0.48, 2.14] |
| 7 Anaemia | 2 | 300 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.63 [0.65, 4.11] |
| 8 Thrombocytopenia | 2 | 300 | Risk Difference (M‐H, Fixed, 95% CI) | 0.03 [‐0.00, 0.06] |
| 9 Health‐related quality of life | 1 | 142 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.17, 0.07] |
| 10 All‐cause mortality | 2 | 187 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.60 [0.65, 3.95] |
| 11 Dyspnoea: TDI | 1 | Mean Difference (Fixed, 95% CI) | 2.9 [2.79, 3.01] | |
| 12 Cough severity score | 1 | 142 | Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.39, 0.05] |
2.1. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 1 FVC % predicted at 12 months.
2.2. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 2 FVC % predicted at end of study.
2.3. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 3 DLCO % predicted at 12 months.
2.4. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 4 DLCO % predicted at end of study.
2.5. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 5 Leukopenia.
2.6. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 6 Pneumonia.
2.7. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 7 Anaemia.
2.9. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 9 Health‐related quality of life.
2.10. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 10 All‐cause mortality.
2.11. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 11 Dyspnoea: TDI.
2.12. Analysis.
Comparison 2 Cyclophosphamide versus mycophenolate, Outcome 12 Cough severity score.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Hoyles 2006.
| Methods | Participants recruited from 5 centres in the United Kingdom Participants allocated to the active treatment group (prednisolone and CYC followed by AZA) or the placebo group via the minimisation method, with balancing for the following known prognostic factors: age, baseline HRCT pattern and extent of disease, and autoantibody profile |
|
| Participants | Ambulatory participants aged 18 to 75 years, who fulfil American College of Rheumatology (ACR; formerly, the American Rheumatism Association) preliminary criteria for a diagnosis of SSc, have SSc‐associated pulmonary fibrosis, as indicated by high‐resolution computed tomography (HRCT) or thoracoscopic lung biopsy, and comply with therapy and with regular specialty centre attendance Participants excluded from the study if they had previous AZA or CYC therapy for 3 months, had previous high‐dose oral corticosteroid therapy (30 mg of prednisolone or equivalent daily) for 3 months, had oral corticosteroid therapy (prednisolone dosage 10 mg daily) in the 3 months before study entry, had contraindications to oral corticosteroids such as poorly controlled diabetes or severe osteoporosis, were likely to require lung transplantation within 1 year, had a history of or laboratory data suggestive of other serious systemic or psychological disease unrelated to SSc, were pregnant or lactating, exhibited evidence of alcohol or drug abuse, or were unable to give written informed consent No significant differences in baseline characteristics between intervention and control groups Baseline FVC 80% |
|
| Interventions | Participants in the active treatment group received therapy with 20 mg oral prednisolone on alternate days and 6 IV infusions of CYC at a dose of 600 mg/m² (mean dose 1050 mg) at 4‐week intervals, followed by oral AZA at 2.5 mg/kg/d (maximum 200 mg/d) as maintenance therapy. Patients in the placebo group received placebo formulations that matched the active treatment. |
|
| Outcomes | Tests of lung function were performed at 3, 6, and 12 months. Pulmonary function testing was performed according to the guidelines of the British Thoracic Society. Tests of lung volume and airway resistance were conducted via a constant volume body plethysmograph. Single‐breath diffusing capacity for carbon monoxide (DLCO) was tested with a conventional carbon monoxide/helium gas mixture and corrected for haemoglobin (corrected DLCO) and alveolar volume (coefficient of gas transfer, Kco). Spirometry
was performed using flow‐volume loops. All results were expressed as a percentage of normal predicted values based on age, sex, and height. A modified American Thoracic Society respiratory questionnaire was used to determine a baseline dyspnoea score; the minimum score of 0 represented breathlessness after 30 minutes of vigorous activity, and the maximum score of 20 represented breathlessness with minimal activity. Arterial blood gases were performed at 3, 6, and 12 months. HRCT (1.5‐mm cuts at 20‐mm intervals from lung apex to base in the supine position) was repeated at 1 year. |
|
| Notes | Other immunosuppressive agents, including colchicine, methotrexate, and D‐penicillamine, which might influence the course of lung fibrosis, were not permitted. Both groups continued to receive standard therapy for non‐pulmonary disease. Participants with early (not defined) pulmonary fibrosis including new referrals and existing patients were recruited. Early is not defined in the entry criteria. Many patients with severe or deteriorating disease were inevitably excluded. How patients were selected by investigators or referring physicians for entry is not clearly described. The bias is likely to affect both arms towards a lack of treatment effect. Supported by the Arthritis Research Campaign |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used stratified sampling (minimisation method) for known prognostic factors: age, baseline HRCT pattern and extent of disease, and autoantibody profile |
| Allocation concealment (selection bias) | Low risk | Investigators were blinded to treatment allocation. Randomisation was undertaken at the Royal Brompton Hospital by members of the Clinical Trials and
Evaluation Unit, who were not involved in the analysis of data. However, selection of participants for entry consideration was not clearly described. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants in the placebo group received placebo formulations that matched the active treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Radiologists were blinded to treatment category, but it was not explicitly stated whether other outcome assessors were blinded. It is not clear if study personnel managed adverse events and potentially would have been unblinded by the presence or lack of outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Eight of 45 participants (18%) were lost to follow‐up but had already been withdrawn from the study. Intention‐to‐treat analysis was used. |
| Selective reporting (reporting bias) | High risk | Prespecified outcomes were reported. Post hoc subgroup analysis for weight was included. Tests of lung function and arterial blood gases were performed at 3, 6, and 12 months. Only baseline and 12‐month data are compared. |
Tashkin 2006.
| Methods | Ambulatory participants recruited from 13 centres Parallel placebo‐controlled double‐blind trial |
|
| Participants | Participants with limited or diffuse systemic scleroderma, if they had evidence of active alveolitis on examination of bronchoalveolar‐lavage (BAL) fluid (defined as neutrophilia ≥ 3%, eosinophilia ≥ 2%, or both), or on thoracic high‐resolution computed tomography (CT), any ground‐glass opacity, onset of the first symptom of scleroderma other than Raynaud's phenomenon within the previous 7 years, FVC between 45% and 85% of predicted value, and grade 2 exertional dyspnoea according to the baseline instrument of the Mahler Dyspnea Index (as measured via the magnitude‐of‐task component) Primary exclusion criteria included a single‐breath carbon monoxide diffusing capacity (DLCO) that was < 30% of predicted value, a history of smoking within preceding 6 months, other clinically significant pulmonary abnormalities, or clinically significant pulmonary hypertension requiring drug therapy. Patients taking prednisone at a dose > 10 mg/d, those who had previously been treated for longer than 4 weeks with oral cyclophosphamide or had received ≥ 2 intravenous doses, and those who had recently received other potentially disease‐modifying medications were also excluded. Data show no significant differences between groups except that scores for the HAQ disability index were significantly lower (indicating greater health) in the placebo group than in the cyclophosphamide group. Baseline FVC 68% |
|
| Interventions | Cyclophosphamide and placebo were formulated into matching gelcaps at a dose of 25 mg, and treatment was initiated with a dose of 1 mg per kilogram of body weight per day (to the nearest 25 mg). Doses were increased monthly by 1 capsule up to 2 mg per kilogram. Prednisolone up to 10 mg per day was permitted as a co‐intervention. |
|
| Outcomes | Measurements were made at baseline and at 3‐month intervals throughout the study, except the Mahler Dyspnoea Index. Primary outcome: FVC (expressed as a percentage of predicted value) at 12 months Lung volume measurements were repeated at 6‐month intervals. Prespecified secondary outcomes included values for total lung capacity (expressed as a percentage of predicted value), DlCO (diffusing capacity adjusted for alveolar volume (Dl:Va)), the disability index of the Health Assessment Questionnaire (HAQ), and the Medical Outcomes Study 36‐item Short‐Form General Health Survey (SF‐36). Mahler Transitional Dyspnoea Index (scale from −9 to +9, with the plus sign indicating improvement and the minus sign indicating worsening) Post hoc: skin thickness Cough is reported in a separate manuscript as part of this trial. |
|
| Notes | Professor Tashkin provided unpublished data for subgroup analyses. Funded by NIH and University grants. Medication supplied free of charge by Bristol‐Myers Squibb. Trial authors state that funders had no influence on the trial or the publication. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned with the use of a permuted‐block design and 1:1 allocation (in blocks of 4 to 6 participants per centre). |
| Allocation concealment (selection bias) | Low risk | Cyclophosphamide and placebo were formulated into matching gelcaps. To preserve blinding of investigators, an independent medication control officer assessed adverse events and regulated all doses of study medication, in accordance with the study protocol. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Cyclophosphamide and placebo were formulated into matching gelcaps. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The primary outcome (FVC) was determined by trained, project‐certified hospital‐based pulmonary function technologists. As these technicians were unaware of changes in study medication or results of other outcomes, it is unlikely that they could have become unintentionally unblinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of a total of 158 patients, 3 assigned to placebo and 1 assigned to cyclophosphamide withdrew before starting study treatment and were not included in the analysis. A total of 20 participants in the cyclophosphamide group and 13 in the placebo group withdrew within 12 months after randomisation, most because of adverse events or serious adverse events. Many participants who withdrew were available for endpoint measurement at 12 months; however some 12‐month data were extrapolated from 6‐ or 9‐month data. For remaining participants who withdrew prematurely, a generalised estimating‐ equation regression model was fitted, and data missing at 12 months were imputed. Intention‐to‐treat analysis was used. |
| Selective reporting (reporting bias) | Low risk | Post hoc skin thickness was added. Otherwise all prespecified outcomes were reported. Cough index is reported in a separate manuscript. |
Tashkin 2016.
| Methods | Randomised double‐blind parallel‐group trial performed at 14 US medical centres | |
| Participants | Ambulatory adults with defined systemic sclerosis with limited cutaneous or diffuse cutaneous involvement; age 18 to 75 years; screening forced vital capacity (FVC) < 80% but at least 45% of predicted value and reproducible within 10% at the baseline visit (but 85% or less predicted); exertional dyspnoea grade 2 or higher on the Magnitude of Task component of the Mahler Baseline Dyspnea Index; any ground‐glass opacity on HRCT, whether associated with reticulations (fibrosis) or not; and onset of the patient's first non‐Raynaud's symptom of systemic sclerosis within the past 7 years. Exclusion criteria were FVC < 45% predicted, ratio of FEV1 to FVC < 65%, evidence of substantial airflow obstruction, pulmonary hypertension according to echocardiography or right heart catheterisation and judged by the investigator to be clinically significant and warranting drug therapy; a single‐breath diffusing capacity of the lung for carbon monoxide (DLCO) < 40% predicted (30% to 39% predicted allowed if echocardiography or right heart catheterisation, or both, did not show evidence of pulmonary hypertension); clinically significant abnormalities on HRCT not attributable to systemic sclerosis; smoking within the past 6 months; persistent unexplained haematuria (> 10 red blood cells per high power field); persistent leukopenia (white blood cell count < 4·0 × 109 per L) or thrombocytopenia (platelet count < 150 × 109 per L); clinically significant anaemia (haemoglobin < 100 g/L); baseline liver function test (alanine aminotransferase and aspartate aminotransferase) or bilirubin > 1·5 times the upper normal limit; concomitant and present use of captopril; serum creatinine > 176.8 μmol/L; uncontrolled congestive heart failure; pregnancy (documented by urine pregnancy test) or breastfeeding; prior use of oral MMF or cyclophosphamide for longer than 8 weeks or receipt of more than 2 intravenous doses of cyclophosphamide in the past; use of MMF or cyclophosphamide, or both, in the 30 days before randomisation; active infection (lung or elsewhere) whose management would be compromised by MMF or cyclophosphamide; other serious concomitant medical illness (e.g. cancer), chronic debilitating illness (other than systemic sclerosis), unreliability, or drug abuse that might compromise the patient's participation in the trial; if of childbearing potential (a female participant aged < 55 years who has not been postmenopausal for ≥ 5 years and who has not had a hysterectomy or oophorectomy), failure to use 2 reliable means of contraception; use of contraindicated medications; use of medications with putative disease‐modifying properties within the past 30 days (e.g. D‐penicillamine, azathioprine, methotrexate, Potaba) before randomisation; and prednisone in doses > 10 mg/d. Data show no significant differences in baseline characteristics between control and intervention groups. Baseline FVC 66% |
|
| Interventions | Cyclophosphamide was administered once daily (morning dose active drug and evening dose placebo) for 12 months, with an initial dose of 50 to 150 mg (based on weight) titrated up to a maximum dose of 1.8 to 2.3 mg/kg according to a defined protocol. During the second 12 months, participants assigned to the cyclophosphamide group received only placebo. MMF was initiated at a dose of 500 mg twice daily increased over time to a maximum dose of 1·5 g twice daily according to a defined protocol, and continued for a total of 2 years. |
|
| Outcomes | Primary outcome: % FVC Secondary outcome variables: course from 3 months to 24 months of % predicted DLCO, TDI, and mRSS scores, and change from baseline in quantitative HRCT scores for lung fibrosis and total interstitial lung disease at 24 months St Georges Respiratory Questionnaire for cough and Leichester Cough Questionnaire scores collected but not reported in any final manuscripts |
|
| Notes | Funded by NIH, medication supplied by Roche. Trial authors state funders had no role in development and publication of this trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned via a double‐blind, double‐dummy, centre‐blocked design. |
| Allocation concealment (selection bias) | Low risk | Masking was done by the UCLA Pharmacy Core, which formulated all study drugs (250 mg MMF, 25 mg cyclophosphamide, or placebo) into matching 250‐mg gel capsules. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study drugs were masked in matching gelcaps. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not explicitly stated Blinding of PFT technologists not made clear, although likely to be that of other local study staff PROs self‐reported and likely to be unbiased |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In the cyclophosphamide group, 36 participants prematurely stopped drug treatment (2 deaths, 2 treatment failures, and 32 other withdrawals), whereas only 20 participants in the MMF group prematurely stopped drug treatment (1 death, no treatment failures, 19 other withdrawals). A modified intention‐to‐treat analysis was performed, using an inferential joint model consisting of a mixed‐effects model for longitudinal outcomes and a survival model to handle non‐ignorable missing data due to study dropout, treatment failure, or death (i.e. likely related to disease or treatment and therefore not random). |
| Selective reporting (reporting bias) | High risk | St Georges Respiratory Questionnaire for cough and Leichester Cough Questionnaire scores collected but not reported in any final manuscripts |
Zhang 2015.
| Methods | Single‐blind parallel controlled trials at 5 centres | |
| Participants | Inclusion criteria: 18‐ to 80‐year‐olds with a diagnosis of connective tissue disease according to the International Guidelines for Rheumatic Disease (included systemic sclerosis, rheumatoid arthritis, polymyositis/dermatomyositis, SLE), with symptoms suggestive of and an HRCT confirming interstitial lung disease (with 1 of 7 criteria for ILD according to ATS/ERS 2002 criteria). All types of lung function were included. Exclusion criteria: interstitial lung disease not from connective tissue disease, pregnant or lactating women, those with chronic liver failure, diarrhoea, infection, cancer, pulmonary hypertension, creatinine > 170, LFTs > 2 times the upper limit of normal, obstructive liver function tests Participant numbers and sex distribution were oddly balanced. |
|
| Interventions | IV cyclophosphamide for 12 months Compared with oral mycophenolate (1.5 grams daily) for 12 months In addition, all participants in intervention and control groups received prednisolone, with the starting dose titrated according to disease severity (as deemed by trial doctors), then weaned to 10 mg daily within 4 weeks. |
|
| Outcomes | FVC, FEV1, TCLCO HRCT scores of interstitial lung disease Liver and kidney function Adverse events All‐cause mortality No patient‐reported outcomes. Outcomes measured at 0, 3, 6, and 12 months. Change from baseline scores were reported, but SDs were not included, so post‐treatment scores with SDs were used in the analysis. |
|
| Notes | Per‐protocol analysis Trial authors were contacted in Chinese to request further details about the conduct of the trial and to obtain individual data to calculate change from baseline standard deviations, but at the time of publication, review authors had received no reply. Funding source was not stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Predetermined random numbers used |
| Allocation concealment (selection bias) | Unclear risk | Methods of allocation concealment not clearly stated. Participant numbers and sex distribution oddly balanced between groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not clearly stated. One group received intravenous medication, and one group received oral medication, with no mention of blinding, so it is possible participants were aware of the intervention they received. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not clearly stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdrawals accounted for but very low dropout numbers compared with other included papers. Appears to be per‐protocol analysis rather than ITT analysis |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
ACR: American College of Rheumatology.
ATS: American Thoracic Society.
AZA: azathioprine.
BAL: bronchoalveolar lavage.CT: computed tomography.
CYC: cyclophosphamide.
DLCO: diffusing capacity of the lung for carbon monoxide.
ERS: European Respiratory Society.
FVC: forced vital capacity.
HAQ: Health Assessment Questionnaire.
HRCT: high‐resolution computed tomography.
ITT: intention‐to‐treat.
IV: intravenous.
Kco: coefficient of gas transfer.
LFTs: liver function tests.
MMF: mycophenolate mofetil.
mRSS: modified Rodnan skin score.
NIH: National Institutes of Health.
PFT: pulmonary function test.
PRO: patient‐reported outcome.
SD: standard deviation.
SLE: systemic lupus erythematosus.
SSc: systemic sclerosis.
TLCO: transfer factor for carbon monoxide.
TDI: Transition Dyspnoea Index.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Au 2010 | Wrong participant population |
| Choudhury 2013 | Not randomised |
| Goldin 2008 | Post hoc analysis of data from SLS I study |
| Highland 2005 | Post hoc analysis of data from SLS I study |
| Khanna 2005 | Post hoc analysis of data from SLS I study |
| Khanna 2009 | Post hoc analysis of data from SLS I study |
| Kim 2008 | Post hoc analysis of data from SLS I study |
| Kim 2011 | Post hoc analysis of data from SLS I study |
| Roth 2011 | Post hoc analysis of data from SLS I study |
| Strange 2008 | Post hoc analysis of data from SLS I study |
| Tashkin 2009 | Post hoc analysis of data from SLS I study |
SLS I: Scleroderma Lung Study I.
Characteristics of ongoing studies [ordered by study ID]
Maher 2015.
| Trial name or title | Rituximab Versus Cyclophosphamide in Connective Tissue Disease‐ILD (RECITAL) |
| Methods | Randomised parallel double‐blind controlled trial |
| Participants | Adults over 18 years with a diagnosis of connective tissue disease, based on internationally accepted criteria, in one of the following categories:
• Systemic sclerosis
• Idiopathic interstitial myopathy (including polymyositis/dermatomyositis)
• Mixed connective tissue disease With severe and/or progressive interstitial lung disease associated with underlying connective tissue disease |
| Interventions | Experimental: rituximab: 1 gram given at baseline and at 2 weeks Active comparator: cyclophosphamide: intravenous dose of 600 mg/m2 body surface area. 6 doses given 4‐weekly |
| Outcomes | Primary outcome measures • Absolute change in FVC at 48 weeks Secondary outcome measures • Change from baseline in diffusing capacity for carbon monoxide (DLCO) at 48 weeks • Change from baseline in health‐related quality of life scores at 48 weeks • Change from baseline in global disease activity score at 48 weeks • Progression‐free survival at 48 weeks • Composite endpoint of mortality, transplant, treatment failure, or decline in FVC > 10% compared with baseline • Adverse and serious adverse events (as defined in GCP) at 48 weeks |
| Starting date | May 2013 |
| Contact information | Toby M Maher: Royal Brompton and Harefield Foundation NHS Trust |
| Notes |
Mouthon 2016.
| Trial name or title | Cyclophosphamide Systemic Sclerosis Associated Interstitial Lung Disease (SCLEROCYC) |
| Methods | Randomised placebo‐controlled trial |
| Participants | Adults > 18 years with systemic sclerosis fulfilling ACR (American College of Rheumatology) diagnostics criteria with worsening ILD (interstitial lung disease) identified on a high‐resolution chest CT scan and by worsening of forced vital capacity (FVC) and/or total lung capacity (TLC) ≥ 10% and/or worsening of DLCO ≥ 15% as compared with values obtained within the 3 to 18 months preceding inclusion (for DLCO, in the absence of pulmonary arterial hypertension upon echocardiography) |
| Interventions | Prednisone 15 mg/d + monthly pulse cyclophosphamide 700 mg/m² diminished to 600 mg/m² in patients over 65 years or with creatinine clearance < 30 mL/min for 12 months vs Prednisone 15 mg/d + monthly pulse of placebo |
| Outcomes | Primary outcome measures
• Forced vital capacity at 12 months Secondary outcome measures • Mortality at 12 months • Progression‐free survival at 12 months • Progression‐free survival • Carbon monoxide diffusing capacity (DLCO) at 12 months • Treatment failure at 12 months • Failure of cyclophosphamide or placebo • Walk test distance at 12 months • Six‐minute walk test distance, O2 desaturation, and gradient between maximal and minimal SaO2 during the test • Dyspnoea at 12 months • NYHA (New York Heart Association Classification), BDI (Beck Depression Inventory), and Borg index • Health Assessment Questionnaire at 12 months • Quality of life at 12 months • Saint Georges; SF‐36 • Chest CT (computed tomography) scan at 12 months • CT scan abnormalities |
| Starting date | January 2013 |
| Contact information | Principal Investigator: Luc Mouthon, Cochin Hospital |
| Notes |
ACR: American College of Rheumatology.
BDI: Beck Depression Inventory.
CT: computed tomography.
DLCO: diffusing capacity of the lung for carbon monoxide.
FVC: forced vital capacity.
GCP: good clinical practice.
ILD: interstitial lung disease.
NHS: National Health Service.
NYHA: New York Heart Association.
O2: oxygen.
SaO2: oxygen saturation.
SF‐36: Short Form‐36.
TLC: total lung capacity.
Differences between protocol and review
We added all‐cause mortality to the 'Summary of findings' table.
We removed the following exclusion criteria in response to peer referee comments on the draft review: "Studies that included people with clinically unstable disease, respiratory sepsis or coexistent obstructive lung disease were excluded from the analysis". However, we identified no such eligible studies for this review.
Contributions of authors
ING drafted the protocol with assistance from GPW, NSLG, and AEH.
HB and ING screened the abstracts and full‐text articles for inclusion, extracted the data, and drafted the review. AEH, GPW, and NLSSLG provided comments and revisions of the review. HB will be responsible for updating this Cochrane review.
Sources of support
Internal sources
Lung Foundation Australia/Cochrane Airways Australia Scholarship 2017, Australia.
External sources
The review authors declare that no such funding was received for this systematic review, Other.
Declarations of interest
HB: none known.
AEH: none known.
GPW: none known.
NSLGG: none known.
ING: none known.
New
References
References to studies included in this review
Hoyles 2006 {published data only}
- Herrick AL. A clinical trial of treatment for lung disease in scleroderma fibrosing alveolitis in scleroderma (FAST study). National Research Register (UK) 2005. [Google Scholar]
- Hoyles R, Ellis R, Herrick A, Foley N, McHugh N, Pearson S, et al. Fibrosing alveolitis in scleroderma trial (FAST): a multicentre prospective randomised double blind placebo controlled trial [Abstract]. British Thoracic Society Winter Meeting; 2005 December 7‐9; London. 2005; Vol. 2:ii48.
- Hoyles RK, Ellis RW, Wellsbury J, Lees B, Newlands P, Goh NS, et al. A multicenter, prospective, randomized, double‐blind, placebo‐controlled trial of corticosteroids and intravenous cyclophosphamide followed by oral azathioprine for the treatment of pulmonary fibrosis in scleroderma. Arthritis and Rheumatism 2006;54(12):3962‐70. [DOI] [PubMed] [Google Scholar]
Tashkin 2006 {published data only}
- Clements PJ, Tashkin D, Roth M, Khanna D, Furst DE, Tseng CH, et al. The scleroderma lung study II (SLS II) shows that both oral cyclophosphamide (CYC) and mycophenolate mofetil (MMF) are efficacious in treating progressive interstitial lung disease (ILD) in patients with systemic sclerosis (SSC). American College of Rheumatology/Association of Rheumatology Health Professionals Annual Scientific Meeting; 2015 November 6‐11; San Francisco. 2015; Vol. 67.
- Furst D, Khanna D, Tseng CH, Mayes M, Roth M, Seibold J, et al. Patients with systemic sclerosis (SSC) enrolled in the scleroderma lung study (SLS) have a high mortality within 5 years of stopping Cyclophosphamide (CYC). Clinical and Experimental Rheumatology 2010;28(2 suppl 58):S94. [Google Scholar]
- Goldin J, Elashoff R, Kim HJ, Yan X, Lynch D, Strollo D, et al. Treatment of scleroderma‐interstitial lung disease with cyclophosphamide is associated with less progressive fibrosis on serial thoracic high‐resolution CT scan than placebo: findings from the scleroderma lung study. Chest 2009;136(5):1333‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna D, Furst DE, Clements PJ, Elashoff R, Hong CH, Roth M, et al. Adverse events during the Scleroderma Lung Study. American Journal of Medicine 2011;124(5):459‐67. [DOI] [PubMed] [Google Scholar]
- Khanna D, Tseng CH, Farmani N, Steen V, Furst DE, Clements PJ, et al. Clinical course of lung physiology in patients with scleroderma and interstitial lung disease: analysis of the Scleroderma Lung Study Placebo Group. Arthritis and Rheumatism 2011;63(10):3078‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Tashkin DP, Gjertson DW, Brown MS, Kleerup E, Chong S, et al. Transitions to different patterns of interstitial lung disease in scleroderma with and without treatment. Annals of the Rheumatic Diseases 2016;75(7):1367‐71. [DOI] [PubMed] [Google Scholar]
- Kim HJG, Brown MS, Goldin J, Abtin FG, Lynch DA, Strollo D, et al. Cyclophosphamide treatment versus placebo in scleroderma lung study using total quantitative score of fibrosis, ground glass opacity, and honeycomb. American Thoracic Society International Conference; 2010 May 14‐19; New Orleans. 2010.
- Tashkin DP, Clements P, Roth M, Furst D, Strange C, Silver R, et al. Oral cyclophosphamide (CYC) vs placebo for treatment of scleroderma related interstitial lung disease (SSc ILD) main findings from the scleroderma lung study [Abstract]. American Thoracic Society International Conference; 2006 May 19‐21; San Diego. 2006:A242 [Poster 818].
- Tashkin DP, Clements PJ, Roth MD, Furst DE, Li N, Chung J, et al. Two‐year outcomes of one‐year treatment with oral cyclophosphamide vs placebo for scleroderma‐interstitial lung disease (SSc‐ILD) [Abstract]. American Thoracic Society International Conference; 2007 May 18‐23; San Francisco. 2007:[B91].
- Tashkin DP, Elashoff R, Clements PJ, Goldin J, Roth MD, Furst DE, et al. Cyclophosphamide versus placebo in scleroderma lung disease. New England Journal of Medicine 2006;354:2655‐66. [DOI] [PubMed] [Google Scholar]
- Tashkin DP, Elashoff R, Clements PJ, Roth MD, Furst DE, Silver RM, et al. Effects of 1‐year treatment with cyclophosphamide on outcomes at 2 years in scleroderma lung disease. American Journal of Respiratory and Critical Care Medicine 2007;176(10):1026‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodore AC, Tseng CH, Li N, Elashoff RM, Tashkin DP. Correlation of cough with disease activity and treatment with cyclophosphamide in scleroderma interstitial lung disease: findings from the Scleroderma Lung Study. Chest 2012;142(3):614‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodore AC, Tseng CH, Tashkin D, Scleroderma Research Group. Correlation of cough with disease activity and treatment with cyclosphosphamide in scleroderma interstitial lung disease [Abstract]. American Journal of Respiratory and Critical Care Medicine. Conference: American Thoracic Society International Conference, ATS 2010 New Orleans, LA United States.. American Thoracic Society, 2010; Vol. 181:A2362.
Tashkin 2016 {published data only}
- Khanna D, Roth M, Furst D, Clements P, Goldin J, Arriola E, et al. Double‐blind comparison of mycophenolate mofetil and oral cyclophosphamide for treatment of scleroderma‐related interstitial lung disease (scleroderma lung study [SLS] II): rationale, design, methods, baseline characteristics and patient disposition. Annals of the Rheumatic Diseases. 2013; Vol. 72, issue Suppl 3.
- Scleroderma Lung Study Research Group. Mycophenolate vs oral cyclophosphamide in scleroderma interstitial lung disease (Scleroderma Lung Study II) [Protocol]. www.sclerodermalungstudy.org/ (accessed before 27 March 2017). [Google Scholar]
- Tashkin D, Roth M, Clements P, Furst D, Khanna D, Goldin J, et al. Efficacy and safety of mycophenolate (MMF) vs oral cyclophosphamide (CYC) for treatment of Scleroderma‐Interstitial Lung Disease (SscILD): results of Scleroderma Lung Study II. Chest. 2015; Vol. 148, issue 4 MEETING ABSTRACT.
- Tashkin DP, Roth MD, Clements PJ, Furst DE, Khanna D, Kleerup EC, et al. Double‐blind comparison of mycophenolate mofetil and oral cyclophosphamide for treatment of scleroderma‐related interstitial lung disease (Scleroderma Lung Study [SLS] II): rationale, design, methods, baseline characteristics/intercorrelations and patients. American Thoracic Society International Conference; 2013 May 17‐22; Philadelphia. 2013; Vol. 187:A2921.
- Tashkin DP, Roth MD, Clements PJ, Furst DE, Khanna D, Kleerup EC, et al. Mycophenolate mofetil versus oral cyclophosphamide in scleroderma‐related interstitial lung disease (SLS II): a randomised controlled, double‐blind, parallel group trial. Lancet Respiratory Medicine 2016;4(9):708–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkmann E, Tashkin D, Clements P, Roth M, Furst D, Khanna D, et al. Cyclophosphamide versus mycophenolate for systemic sclerosis‐related interstitial lung disease. Annals of the Rheumatic Diseases 2015;74:821. [Google Scholar]
- Volkmann ER, Roth M, Elashoff R, Clements PJ, Furst DE, Khanna D, et al. Safety and tolerability of cyclophosphamide versus mycophenolate for systemic sclerosis‐related interstitial lung disease [abstract]. Arthritis and Rheumatology 2015;67:suppl 10. [Google Scholar]
Zhang 2015 {published data only}
- Zhang G, Xu T, Zhang H, Ye S, Wang Q, Zhang L, et al. [Randomized control multi‐center clinical study of mycophenolate mofetil and cyclophosphamide in the treatment of connective tissue disease related interstitial lung disease]. Zhonghua Yi Xue Za Zhi 2015;95(45):3641‐5. [PubMed] [Google Scholar]
References to studies excluded from this review
Au 2010 {published data only}
- Au K, Mayes MD, Maranian P, Clements PJ, Khanna D, Steen VD, et al. Course of dermal ulcers and musculoskeletal involvement in systemic sclerosis patients in the scleroderma lung study. Arthritis Care and Research 2010;62(12):1772‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choudhury 2013 {published data only}
- Choudhury SD, Kundu S, Ghosh S, Agarwal R, Paul S, Hariprasath K. Evaluation of pulse IV cyclophosphamide on scleroderma related interstitial lung disease: An Indian experience. 46th Annual Conference of the Indian Pharmacological Society IPSCON 2013 16‐20 Dec; Bangalore. 2013, issue var.pagings:S107.
Goldin 2008 {published data only}
- Goldin JG, Lynch DA, Strollo DC, Suh RD, Schraufnagel DE, Clements PJ, et al. High‐resolution CT scan findings in patients with symptomatic scleroderma‐related interstitial lung disease. Chest 2008;134(2):358‐67. [DOI] [PubMed] [Google Scholar]
Highland 2005 {published data only}
- Highland KB, Silver RM. Clinical aspects of lung involvement: lessons from idiopathic pulmonary fibrosis and the scleroderma lung study. Current Rheumatology Reports 2005;7(2):135‐41. [DOI] [PubMed] [Google Scholar]
Khanna 2005 {published data only}
- Khanna D, Clements PJ, Furst DE, Chon Y, Elashoff R, Roth MD, et al. Correlation of the degree of dyspnea with health‐related quality of life, functional abilities, and diffusing capacity for carbon monoxide in patients with systemic sclerosis and active alveolitis: results from the Scleroderma Lung Study. Arthritis and Rheumatism 2005;52(2):592‐600. [DOI] [PubMed] [Google Scholar]
Khanna 2009 {published data only}
- Khanna D, Tseng CH, Furst DE, Clements PJ, Elashoff R, Roth M, et al. Minimally important differences in the Mahler's Transition Dyspnoea Index in a large randomized controlled trial ‐ Results from the scleroderma lung study. Rheumatology 2009;48(12):1537‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2008 {published data only}
- Kim H, Goldin J, Lynch D, Strollo SD, Ochs R, Vasu F, et al. Cyclophosphamide versus placebo in Scleroderma Lung Study using quantitative lung fibrosis score [Abstract]. American Thoracic Society International Conference; 2008 May 16‐21; Toronto. 2008:A768.
Kim 2011 {published data only}
- Kim HJ, Brown MS, Elashoff R, Li G, Gjertson DW, Lynch DA, et al. Quantitative texture‐based assessment of one‐year changes in fibrotic reticular patterns on HRCT in scleroderma lung disease treated with oral cyclophosphamide. European Radiology 2011;21(12):2455‐65. [DOI] [PubMed] [Google Scholar]
Roth 2011 {published data only}
- Roth MD, Tseng CH, Clements PJ, Furst DE, Tashkin DP, Goldin JG, et al. Predicting treatment outcomes and responder subsets in scleroderma‐related interstitial lung disease. American Thoracic Society International Conference; 2011 May 13‐18; Denver. 2011. [DOI] [PMC free article] [PubMed]
Strange 2008 {published data only}
- Strange C, Bolster MB, Roth MD, Silver RM, Theodore A, Goldin J, et al. Bronchoalveolar lavage and response to cyclophosphamide in scleroderma interstitial lung disease. American Journal of Respiratory and Critical Care Medicine 2008;177(1):91‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tashkin 2009 {published data only}
- Tashkin DP, Elashoff D, Roth MD, Furst DE, Khanna D. Predictors of change in % predicted FVC over time in scleroderma (SSc) interstitial lung disease (ILD: findings from the Scleroderma Lung Study (SLS) [Abstract]. American Thoracic Society International Conference; 2009 May 15‐20 San Diego. 2009:A3940.
References to ongoing studies
Maher 2015 {published data only}
- Maher T. Rituximab Versus Cyclophosphamide in Connective Tissue Disease‐ILD (RECITAL). NCT01862926.
Mouthon 2016 {unpublished data only}
- Mouthon L. Cyclophosphamide Systemic Sclerosis Associated Interstitial Lung Disease (SCLEROCYC). NCT01570764 2016.
Additional references
Assassi 2010
- Assassi S, Sharif R, Lasky RE, McNearney TA, Estrada Y, Martin RM, et al. Predictors of interstitial lung disease in early systemic sclerosis: a prospective longitudinal study of the GENISOS cohort. Arthritis Research and Therapy 2010;12:R166. [DOI] [PMC free article] [PubMed] [Google Scholar]
ATS/ERS Consensus Statement
- American Thoracic Society (ATS), and the European Respiratory Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS Board of Directors, June 2001, and by the ERS Executive Committee, June 2001. American Journal of Respiratory and Critical Care Medicine 2002;165:277‐304. [DOI] [PubMed] [Google Scholar]
Baron 2008
- Baron M, Sutton E, Hudson M, Thombs B, Markland J, Pope J, et al. The relationship of dyspnoea to function and quality of life in systemic sclerosis. Annals of the Rheumatic Diseases 2008;67:644‐50. [DOI] [PubMed] [Google Scholar]
Bongartz 2010
- Bongartz T, Nannini C, Medina‐Velasquez YF, Achenbach SJ, Crowson CS, Ryu JH, et al. Incidence and mortality of interstitial lung disease in rheumatoid arthritis: a population‐based study. Arthritis Rheumatology 2010;62(6):583‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boumpas 1992
- Boumpas DT, Austin HA 3rd, Vaughn EM, Klippel JH, Steinberg AD, Yarboro CH, et al. Controlled trial of pulse methylprednisolone versus two regimens of pulse cyclophosphamide in severe lupus nephritis. Lancet 1992;340:741‐5. [DOI] [PubMed] [Google Scholar]
Bouros 2002
- Bouros D, Wells AU, Nicholson AG, Colby TV, Polychronopoulos V, Pantelidis P, et al. Histopathologic subsets of fibrosing alveolitis in patients with systemic sclerosis and their relationship to outcome. American Journal of Respiratory and Critical Care Medicine 2002;165:1581‐6. [DOI] [PubMed] [Google Scholar]
Corte 2012
- Corte TJ, Copley SJ, Desai SR, Zappala CJ, Hansell DM, Nicholson AG, et al. Significance of connective tissue disease features in idiopathic interstitial pneumonia. European Respiratory Journal 2012;39:661‐8. [DOI] [PubMed] [Google Scholar]
Daoussis 2012
- Daoussis D, Liossis SN, Tsamandas AC, Kalogeropoulou C, Paliogianni F, Sirinian C, et al. Effect of long‐term treatment with rituximab on pulmonary function and skin fibrosis in patients with diffuse systemic sclerosis. Clinical and Experimental Rheumatology 2012;30:S17‐22. [PubMed] [Google Scholar]
Ferri 2002
- Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, Montagna G, et al. Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine 2002;81:139‐53. [DOI] [PubMed] [Google Scholar]
Fischer 2008
- Fischer A, Swigris JJ, Groshong SD, Cool CD, Sahin H, Lynch DA, et al. Clinically significant interstitial lung disease in limited scleroderma: histopathology, clinical features, and survival. Chest 2008;134:601‐5. [DOI] [PubMed] [Google Scholar]
Fischer 2013
- Fischer A, Brown KK, Du Bois RM, Frankel SK, Cosgrove GP, Fernandez‐Perez ER, et al. Mycophenolate mofetil improves lung function in connective tissue disease‐associated interstitial lung disease. Journal of Rheumatology 2013;40:640‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Furst 2010
- Furst D, Khanna D, Tseng CH, Mayes M, Roth M, Seibold J, et al. Patients with systemic sclerosis (SSC) enrolled in the Scleroderma Lung Study (SLS) have a high mortality within 5 years of stopping Cyclophosphamide (CYC). Clinical and Experimental Rheumatology 2010;28(2 suppl 58):S94. [Google Scholar]
Goh 2008
- Goh NS, Desai SR, Veeraraghavan S, Hansell DM, Copley SJ, Maher TM, et al. Interstitial lung disease in systemic sclerosis: a simple staging system. American Journal of Respiratory and Critical Care Medicine 2008;177:1248‐54. [DOI] [PubMed] [Google Scholar]
Goh 2017
- Goh NS, Hoyles RK, Denton CP, Hansell DM, Renzoni EA, Maher TM, et al. Short‐term pulmonary function trends are predictive of mortality in interstitial lung disease associated with systemic sclerosis. Arthritis & Rheumatology 2017;69:1670–8. [DOI] [PubMed] [Google Scholar]
Gourley 1996
- Gourley MF, Austin HA 3rd, Scott D, Yarboro CH, Vaughan EM, Muir J, et al. Methylprednisolone and cyclophosphamide, alone or in combination, in patients with lupus nephritis. A randomized, controlled trial. Annals of Internal Medicine 1996;125:549‐57. [DOI] [PubMed] [Google Scholar]
GradePro GDT 2015 [Computer program]
- GRADE Working Group, McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed before 28 March 2017. Hamilton (ON): GRADE Working Group, McMaster University (developed by Evidence Prime), 2015. Available from gradepro.org.
Hall 1992
- Hall AG, Tilby MJ. Mechanisms of action of, and modes of resistance to, alkylating agents used in the treatment of haematological malignancies. Blood Reviews 1992;6:163‐73. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hoffman 1992
- Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, et al. Wegener granulomatosis: an analysis of 158 patients. Annals of Internal Medicine 1992;116:488‐98. [DOI] [PubMed] [Google Scholar]
Hwang 2009
- Hwang JH, Misumi S, Sahin H, Brown KK, Newell JD, Lynch DA. Computed tomographic features of idiopathic fibrosing interstitial pneumonia: comparison with pulmonary fibrosis related to collagen vascular disease. Journal of Computer Assisted Tomography 2009;33:410‐5. [DOI] [PubMed] [Google Scholar]
Jordan 2015
- Jordan S, Distler JHW, Maurer B, Huscher D, Laar JM, Allanore Y, et al. Effects and safety of rituximab in systemic sclerosis: an analysis from the European Scleroderma Trial and Research (EUSTAR) group. Annals of the Rheumatic Diseases 2015;74(6):1188‐94. [DOI] [PubMed] [Google Scholar]
Khanna 2006
- Khanna D, Furst DE, Hays RD, Park Gs, Wong WK, Seibold SR, et al. Minimally important difference in diffuse systemic sclerosis: results from the d‐penicillamine study. Annals of the Rheumatic Diseases 2006;65(10):1325‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khanna 2011
- Khanna D, Tseng CH, Farmani N, Steen V, Furst DE, Clements PJ, et al. Clinical course of lung physiology in patients with scleroderma and interstitial lung disease: analysis of the Scleroderma Lung Study Placebo Group. Arthritis and Rheumatism 2011;63(10):3078‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khanna 2015
- Khanna D, Denton CP, Jahreis A, Laar JM, Cheng S, Spotswood H, et al. Safety and efficacy of subcutaneous tocilizumab in adults with systemic sclerosis: week 48 data from the faSScinate trial. Annals of the Rheumatic Diseases. 2015; Vol. 74(suppl 2):87‐8.
Kim 2010
- Kim EJ, Elicker BM, Maldonado F, Webb WR, Ryu JH, Uden JH, et al. Usual interstitial pneumonia in rheumatoid arthritis‐associated interstitial lung disease. European Respiratory Journal 2010;35:1322‐8. [DOI] [PubMed] [Google Scholar]
Kim 2016
- Kim HJ, Tashkin DP, Gjertson DW, Brown MS, Kleerup E, Chong S, et al. Transitions to different patterns of interstitial lung disease in scleroderma with and without treatment [2016]. Annals of the Rheumatic Diseases 75(7):1367‐71. [DOI] [PubMed] [Google Scholar]
Labirua‐Iturburu 2013
- Labirua‐Iturburu A, Selva‐O'Callaghan A, Martinez‐Gomez X, Trallero‐Araguas E, Labrador‐Horrillo M, Vilardell‐Tarres M. Calcineurin inhibitors in a cohort of patients with antisynthetase associated interstitial lung disease. Clinical Experimental Rheumatology 2013;31:436‐9. [PubMed] [Google Scholar]
Mathai 2010
- Mathai SK, Gulati M, Peng X, Russell TR, Shaw AC, Rubinowitz AN, et al. Circulating monocytes from systemic sclerosis patients with interstitial lung disease show an enhanced profibrotic phenotype. Laboratory Investigation 2010;90:812‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathai 2016
- Mathai SC, Danoff SK. Management of interstitial lung disease associated with connective tissue disease. BMJ 2016;352:6819. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mira‐Avendano 2013
- Mira‐Avendano IC, Parambil JG, Yadav R, Arrossi V, Meng X, Chapman JT, et al. A retrospective review of clinical features and treatment outcomes in steroid resistant interstitial lung disease from polymyositis/dermatomyositis. Respiratory Medicine 2013;107(6):890‐6. [DOI] [PubMed] [Google Scholar]
Mittoo 2009
- Mittoo S, Gelber AC, Christopher‐Stine L, Horton MR, Lechtzin N, Danoff SK. Ascertainment of collagen vascular disease in patients presenting with interstitial lung disease. Respiratory Medicine 2009;103:1152‐8. [DOI] [PubMed] [Google Scholar]
Murray 2011
- Murray LA, Chen Q, Kramer MS, Hesson DP, Argentieri RL, Peng X, et al. TGF‐beta driven lung fibrosis is macrophage dependent and blocked by serum amyloid P. International Journal of Biochemistry and Cell Biology 2011;43:154‐62. [DOI] [PubMed] [Google Scholar]
Nathan 2016
- Nathan SD, Albera C, Bradford WZ, Costabel U, du Bois RM, Fagan EA, et al. Effect of continued treatment with pirfenidone following clinically meaningful declines in forced vital capacity: analysis of data from three phase 3 trials in patients with idiopathic pulmonary fibrosis. Thorax 2016;71(5):429‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02597933
- NCT02597933. A trial to compare nintedanib with placebo for patients with scleroderma related lung fibrosis. clinicaltrials.gov/ct2/show/NCT02597933 (first received 8 October 2015).
NCT02745145
- NCT02745145. Abituzumab in SSc‐ILD. ClinicalTrials.gov Last updated: July 27, 2017.
NCT02808871
- NCT02808871. Phase ll study of pirfenidone in patients with RAILD. clinicaltrials.gov/ct2/show/NCT02808871 (first received 20 March 2016).
Park 2007
- Park JH, Kim DS, Park IN, Jang SJ, Kitaichi M, Nicholson AG, et al. Prognosis of fibrotic interstitial pneumonia: idiopathic versus collagen vascular disease‐related subtypes. American Journal of Respiratory and Critical Care Medicine 2007;175:705‐11. [DOI] [PubMed] [Google Scholar]
Peng 2011
- Peng X, Mathai SK, Murray LA, Russell T, Reilkoff R, Chen Q, et al. Local apoptosis promotes collagen production by monocyte‐derived cells in transforming growth factor beta1‐induced lung fibrosis. Fibrogenesis and Tissue Repair 2011;4:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Raghu 2012
- Raghu G, Anstrom KJ, King TE Jr, Lasky JA, Martinez FJ. Prednisone, azathioprine, and N‐acetylcysteine for pulmonary fibrosis. New England Journal of Medicine 2012;366:1968‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 5 [Computer program]
- Copenhagen, The Nordic Cochrane Centre: The Cochrane Collaboration. Review Manager (RevMan) Version 5.3. Copenhagen, The Nordic Cochrane Centre: The Cochrane Collaboration, 2014.
Song 2009
- Song JW, Do KH, Kim MY, Jang SJ, Colby TV, Kim DS. Pathologic and radiologic differences between idiopathic and collagen vascular disease‐related usual interstitial pneumonia. Chest 2009;136:23‐30. [DOI] [PubMed] [Google Scholar]
Stock 2013
- Stock CJ, Sato H, Fonseca C, Banya WA, Molyneaux PL, Adamali H, et al. Mucin 5B promoter polymorphism is associated with idiopathic pulmonary fibrosis but not with development of lung fibrosis in systemic sclerosis or sarcoidosis. Thorax 2013;68:436‐41. [DOI] [PubMed] [Google Scholar]
Tashkin 2007
- Tashkin DP, Elashoff R, Clements PJ, Roth MD, Furst DE, Silver RM, et al. Effects of 1‐year treatment with cyclophosphamide on outcomes at 2 years in scleroderma lung disease. American Journal of Respiratory and Critical Care Medicine 2007;176(10):1026‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tashkin 2017
- Tashkin DP, Volkmann ER, Tseng CH, Roth MD, Khanna D, Furst DE, et al. Improved cough and cough‐specific quality of life in patients treated for scleroderma‐related interstitial lung disease: results of Scleroderma Lung Study II. Chest 2017;151(4):813‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tugwell 2007
- Tugwell P, Boers M, Brooks P, Lee S, Strand V, Idzerda L. OMERACT: an international initiative to improve outcome measurement in rheumatology. Trials 2007;8:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Laar 2014
- Laar JM, Farge D, Sont JK, Naraghi K, Marjanovic Z, Larghero J, et al. EBMT/EULAR Scleroderma Study Group. Autologous hematopoietic stem cell transplantation vs intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: a randomized clinical trial. JAMA 2014;311:2490‐8. [DOI] [PubMed] [Google Scholar]
Wells 1994
- Wells AU, Cullinan P, Hansell DM, Rubens MB, Black CM, Newman‐Taylor AJ, et al. Fibrosing alveolitis associated with systemic sclerosis has a better prognosis than lone cryptogenic fibrosing alveolitis. American Journal of Respiratory and Critical Care Medicine 1994;149:1583‐90. [DOI] [PubMed] [Google Scholar]
Wells 2008
- Wells AU, Hirani N, on behalf of the British Thoracic Society Interstitial Lung Disease Guideline Group. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax 2008;63:1‐58. [DOI] [PubMed] [Google Scholar]
Wells 2014
- Wells AU, Denton CP. Interstitial lung disease in connective tissue disease ‐ mechanisms and management. Nature Reviews. Rheumatology 2014;10:728–39. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Glaspole 2014
- Glaspole IN, Westall GP, Goh NSL, Holland AE. Cyclophosphamide for connective tissue disease–associated interstitial lung disease. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD010908] [DOI] [PMC free article] [PubMed] [Google Scholar]


