Abstract
Background
Many systematic reviews exist on interventions to improve safe and effective medicines use by consumers, but research is distributed across diseases, populations and settings. The scope and focus of such reviews also vary widely, creating challenges for decision‐makers seeking to inform decisions by using the evidence on consumers’ medicines use.
This is an update of a 2011 overview of systematic reviews, which synthesises the evidence, irrespective of disease, medicine type, population or setting, on the effectiveness of interventions to improve consumers' medicines use.
Objectives
To assess the effects of interventions which target healthcare consumers to promote safe and effective medicines use, by synthesising review‐level evidence.
Methods
Search methods: We included systematic reviews published on the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects. We identified relevant reviews by handsearching databases from their start dates to March 2012.
Selection criteria: We screened and ranked reviews based on relevance to consumers’ medicines use, using criteria developed for this overview.
Data collection and analysis: We used standardised forms to extract data, and assessed reviews for methodological quality using the AMSTAR tool. We used standardised language to summarise results within and across reviews; and gave bottom‐line statements about intervention effectiveness. Two review authors screened and selected reviews, and extracted and analysed data. We used a taxonomy of interventions to categorise reviews and guide syntheses.
Main results
We included 75 systematic reviews of varied methodological quality. Reviews assessed interventions with diverse aims including support for behaviour change, risk minimisation and skills acquisition. No reviews aimed to promote systems‐level consumer participation in medicines‐related activities. Medicines adherence was the most frequently‐reported outcome, but others such as knowledge, clinical and service‐use outcomes were also reported. Adverse events were less commonly identified, while those associated with the interventions themselves, or costs, were rarely reported.
Looking across reviews, for most outcomes, medicines self‐monitoring and self‐management programmes appear generally effective to improve medicines use, adherence, adverse events and clinical outcomes; and to reduce mortality in people self‐managing antithrombotic therapy. However, some participants were unable to complete these interventions, suggesting they may not be suitable for everyone.
Other promising interventions to improve adherence and other key medicines‐use outcomes, which require further investigation to be more certain of their effects, include:
· simplified dosing regimens: with positive effects on adherence;
· interventions involving pharmacists in medicines management, such as medicines reviews (with positive effects on adherence and use, medicines problems and clinical outcomes) and pharmaceutical care services (consultation between pharmacist and patient to resolve medicines problems, develop a care plan and provide follow‐up; with positive effects on adherence and knowledge).
Several other strategies showed some positive effects, particularly relating to adherence, and other outcomes, but their effects were less consistent overall and so need further study. These included:
· delayed antibiotic prescriptions: effective to decrease antibiotic use but with mixed effects on clinical outcomes, adverse effects and satisfaction;
· practical strategies like reminders, cues and/or organisers, reminder packaging and material incentives: with positive, although somewhat mixed effects on adherence;
· education delivered with self‐management skills training, counselling, support, training or enhanced follow‐up; information and counselling delivered together; or education/information as part of pharmacist‐delivered packages of care: with positive effects on adherence, medicines use, clinical outcomes and knowledge, but with mixed effects in some studies;
· financial incentives: with positive, but mixed, effects on adherence.
Several strategies also showed promise in promoting immunisation uptake, but require further study to be more certain of their effects. These included organisational interventions; reminders and recall; financial incentives; home visits; free vaccination; lay health worker interventions; and facilitators working with physicians to promote immunisation uptake. Education and/or information strategies also showed some positive but even less consistent effects on immunisation uptake, and need further assessment of effectiveness and investigation of heterogeneity.
There are many different potential pathways through which consumers' use of medicines could be targeted to improve outcomes, and simple interventions may be as effective as complex strategies. However, no single intervention assessed was effective to improve all medicines‐use outcomes across all diseases, medicines, populations or settings.
Even where interventions showed promise, the assembled evidence often only provided part of the picture: for example, simplified dosing regimens seem effective for improving adherence, but there is not yet sufficient information to identify an optimal regimen.
In some instances interventions appear ineffective: for example, the evidence suggests that directly observed therapy may be generally ineffective for improving treatment completion, adherence or clinical outcomes.
In other cases, interventions may have variable effects across outcomes. As an example, strategies providing information or education as single interventions appear ineffective to improve medicines adherence or clinical outcomes, but may be effective to improve knowledge; an important outcome for promoting consumers' informed medicines choices.
Despite a doubling in the number of reviews included in this updated overview, uncertainty still exists about the effectiveness of many interventions, and the evidence on what works remains sparse for several populations, including children and young people, carers, and people with multimorbidity.
Authors' conclusions
This overview presents evidence from 75 reviews that have synthesised trials and other studies evaluating the effects of interventions to improve consumers' medicines use.
Systematically assembling the evidence across reviews allows identification of effective or promising interventions to improve consumers’ medicines use, as well as those for which the evidence indicates ineffectiveness or uncertainty.
Decision makers faced with implementing interventions to improve consumers' medicines use can use this overview to inform decisions about which interventions may be most promising to improve particular outcomes. The intervention taxonomy may also assist people to consider the strategies available in relation to specific purposes, for example, gaining skills or being involved in decision making. Researchers and funders can use this overview to identify where more research is needed and assess its priority. The limitations of the available literature due to the lack of evidence for important outcomes and important populations, such as people with multimorbidity, should also be considered in practice and policy decisions.
Plain language summary
Strategies to improve safe and effective medicines use by consumers: an overview of systematic reviews
Review question: This is an update of an overview first published in 2011. Researchers in the Cochrane Collaboration reviewed the evidence from systematic reviews about the effects of interventions to improve safe and effective medicines use by consumers, irrespective of disease, medicine type, population or setting.
Background: Medicines are a cornerstone of treatment for many health problems. Many strategies exist to help people to use medicines safely and effectively, but research in the area is poorly organised across diseases, populations and settings. This can make it difficult for policy makers, health professionals and others to find and use the evidence about what works and what does not.
Study characteristics: This overview summarised the evidence from 75 systematic reviews on consumers' medicine use published to March 2012. Reviews covered acute and chronic diseases in diverse populations and settings; and evaluated a wide range of strategies to improve medicines use, including support for behaviour change, risk minimisation and skills acquisition. Medicines adherence was the most commonly‐reported outcome, with others such as knowledge and clinical outcomes also reported. Adverse events were identified less often.
Key results: Collectively, the results suggest that there are many different potential pathways through which consumers' use of medicines could be targeted to improve outcomes. However, no single strategy improved all medicines‐use outcomes across all diseases, populations or settings.
Strategies that appear to improve medicines use include medicines self‐monitoring and self‐management programmes, while simplified dosing regimens and directly involving pharmacists in medicines management (eg medicines reviews) appear promising. Other strategies, such as delayed antibiotic prescriptions; practical management tools (eg reminders, packaging); education or information combined with other strategies (eg self‐management skills training, counselling); and financial incentives, may also have some positive effects, but their effects are less consistent.
Some strategies, such as directly observed therapy, may be ineffective. Other strategies such as providing information or education alone may have variable effects, being ineffective to change some outcomes (eg medicines adherence) but improving others such as knowledge, which is key for informed medicines choices. Despite a doubling of the number of included reviews in this update, uncertainty remains about the effects of many interventions, and the evidence on what works was particularly sparse for several populations, including children and young people, carers, and people with multimorbidity.
Quality of the evidence: Included reviews often had methodological limitations ‐ at study level, review level, or both ‐ meaning results should be interpreted with caution.
Background
Numerous systematic reviews have examined interventions to improve medicines use. Some reviews include various interventions related to medicines for a specific disease, such as for diabetes or schizophrenia (Vermeire 2005; Zygmunt 2002), while others focus on one type of intervention (eg written information) across different diseases (Mahtani 2011; Nicolson 2009). Still others focus on one primary goal, for example, improving medicines adherence (Haynes 2008; Viswanathan 2012) or immunisation rates (Jacobson 2005; Stone 2002). These differences in the foci of systematic reviews can make it difficult for decision makers to access the review‐level evidence to determine whether potential interventions are effective or not, and for researchers to know where gaps in the evidence exist, or for example, which interventions warrant further investigation to be more certain of their effects.
This is an update of an overview of systematic reviews first published in 2011, which synthesises evidence from systematic reviews of consumers' use of medicines. These comprise interventions targeting consumers to promote evidence‐based prescribing for, and medicines use, by them. It considers such interventions irrespective of disease, setting and/or population.
A consumer perspective on evidence‐based prescribing and medicines use
In this overview, we define consumers to include patients, their family members or carers. We define consumer‐oriented interventions as those principally directed to consumers, in recognition of their central role in decision making and management of medicines, alone or in partnership with healthcare professionals. Since it is ultimately the consumer who decides whether and how to take medicines, the purpose of such interventions might include promoting consumers' knowledge and ability to make informed decisions about medicines, and providing them with sufficient skills and support to take medicines safely and effectively. This overview adopts this inclusive perspective on consumers’ medicines use. Practically, this means considering a wide range of specific interventions targeting consumers, such as purposeful communication, information provision, education, skills training, strategies promoting participation, and support for medicines use.
Organisations working worldwide to regulate and optimise medicines use and availability for individuals and populations have defined evidence‐based prescribing and medicines use in different ways, but definitions rest broadly on the principles of rational use of medicines and evidence‐based health care. These principles specify that medicines are considered as only one among many options for treatment; that the medicine chosen is the safest and most effective option available; and that the medicine is the most appropriate option based on the individual's need. Such principles aim to enable healthcare consumers, professionals and systems to make the best possible use of available medicines and to minimise harms. Internationally, many policies and strategies based on these broad principles have been used to inform, educate, support and communicate with consumers to help them understand and use their medicines in ways that are consistent with healthcare evidence (Chetley 2007; Holloway 2011; NICE 2009).
Quality and safety in the use of medicines: issues of adherence
Internationally, the pursuit of safe, high‐quality health care is a goal, yet major problems in achieving this have been documented across countries (Coulter 2006; Schoen 2005). Amongst other areas of concern, attention has focussed on medicines use, and particularly on high rates of errors by prescribers and patients, on preventable adverse effects (Coulter 2006; Feldstein 2006; Schoen 2005), on inconsistent medicines review, and on difficulties in communication and transitional care (Coleman 2006). Even when medicines are used appropriately, adverse events may occur. The chance of medicines problems occurring is increased by errors such as administration of the wrong drug or dose, failure to adequately take account of allergies or interactions, inadequate monitoring, and insufficient communication of key information to consumers.
Medicines management is only one aspect of managing health, yet it is an important area for decision making by consumers. The developing area of patient‐centred care has promoted greater awareness of the role of consumers as self‐managers and as shared managers of health and illness with healthcare providers, and of the principles and practices of shared and informed decision making (Coulter 2006; Dickinson 2003; Little 2001). Despite these conceptual shifts, much research on consumers' medicines use has focussed primarily or exclusively on adherence, and so involved consumers in largely passive roles.
Medicines adherence has major implications for the effective treatment of many diseases (Haynes 2008; Holloway 2011; Munro 2007; Van Dulmen 2007). If medicines are required, and are selected from available treatment options, they must be taken appropriately to be effective and safe. This might involve ensuring the correct medicine is used, avoiding interactions and identifying contraindications, and taking the medicine according to the appropriate dose, schedule and duration. These activities form a complex set of processes which can be disrupted at any point and so contribute to poor adherence (Coulter 2006).
Poor medicines adherence is of major concern with good cause: studies consistently show that up to half of patients do not take their medicines as prescribed (Haynes 2008; Holloway 2011; Viswanathan 2012), and more than 85% of patients are occasionally non‐adherent (O'Connor 2006). Research suggests that taking less of a medicine than prescribed, rather than more, is most common, although both occur (Britten 2004), and many health problems stem from failing to take medicines properly. Taking too little can dilute any possible therapeutic benefit, but taking medicines in the wrong dose or frequency can also cause problems if, for example, a person tries to compensate for a missed dose by taking more of the medicine when they remember, or takes doses too close together. Poor or inconsistent adherence can therefore cause a range of problems, including increased adverse events, overdose, unnecessary hospitalisations and prescriptions, antimicrobial resistance, rising costs, progression of disease and treatment failure or death (Haynes 2008; Holloway 2011; Tarn 2006a; Viswanathan 2012).
Adherence, however, is complex. A recent systematic review concluded that high levels of adherence to medicines (variously defined but including continued medicine use, or use above a threshold such as 80% of pills taken) was associated in many cases with positive health outcomes, such as decreased mortality (Simpson 2006). However, the review also suggested that good adherence to potentially harmful treatments can lead to adverse outcomes. Other authors have also stressed that increased adherence may have various effects, some of them harmful. These include harmful, or adverse, effects of the medicine itself, as well as harms associated with a loss of patient autonomy and choice (Haynes 2008; Pound 2005).
Many factors affect adherence to medicines (Topinkova 2012). Previous research has concentrated largely on factors affecting consumers' behaviour. These include consumers' ability to remember to take medicines appropriately, the quality of instructions about the medicine, and the demands of complex treatment regimens (Dickinson 2003; Haynes 2008; Mahtani 2011; Mishra 2011; NICE 2009; Van Dulmen 2007). Such factors largely reflect unintentional non‐adherence, which has typically been described as passive non‐adherence occurring as a result of forgetfulness or other factors such as carelessness (Gadkari 2012). Recent research suggests that unintentional non‐adherence may instead be associated with beliefs about medicines (eg perceived need for medicines, perceived affordability; Gadkari 2012). There is also now growing recognition that intentional non‐adherence may also play a role. Factors affecting intentional non‐adherence are complex, and include those associated with cost, adverse effects, patient preferences, disagreement with the need for treatment, or communication breakdown between patient and provider (Britten 2004; Brown 2012; Coleman 2006; Munro 2007; Pound 2005; Ratanawongsa 2013; Soumerai 2006; Tarn 2006a).
Recent qualitative research gives further insight into the many complex factors that interact to affect how and why people take medicines. For example, a so‐called 'aversion' to medicines use has been documented (Britten 2004; Pound 2005; Townsend 2003). Consumers may use medicines only when symptoms demand it, or in ways that least disrupt their daily routines, rather than as prescribed. Sometimes people adjust or halt the regimen to minimise adverse effects or financial costs, or simply because they do not like taking medicines regularly or continuously (Gadkari 2012; Mishra 2011; Pound 2005). These choices reflect the realities of daily medicines use, and the influence of perceptions of health and illness, such as self‐identity and the stigma of having an illness dependent on medicines (Britten 2004; Pound 2005; Townsend 2003). Consumers' concerns about the medicines themselves, including adverse effects, tolerance and dependence, can also affect adherence (Pound 2005).
There is also growing awareness that factors beyond consumers' control can affect adherence (Brown 2012; Coulter 2006; Munro 2007; O'Connor 2006; Ratanawongsa 2013; Soumerai 2006). Research suggests, for example, that healthcare providers' communication and behaviour can affect patients' medicines use, with documented examples of communication breakdown including failure to:
adequately explain how to take a medicine or provide information about new prescription medicines (Tarn 2006a; Tarn 2006b);
review medicines, even where needs are complex (Schoen 2005);
raise and discuss with consumers any reluctance to take medicines (Britten 2004; Pound 2005; Ratanawongsa 2013); and
discuss with consumers their knowledge and beliefs about health and treatment (Munro 2007; Ratanawongsa 2013).
Other factors that can affect medicine use but which may be largely beyond consumers' control include:
financial costs or burden (Gadkari 2012; Munro 2007; Pound 2005; Tarn 2006b);
the co‐existence of problems (co‐morbidity or multimorbidity) (Mishra 2011; Soumerai 2006; Tarn 2006a);
features of health service organisation, such as access to and availability of services, and requirements of the treatment itself; and
the social and cultural context in which treatment occurs, including the influence of community, family members and peers (Garner 2007; Munro 2007).
Given these compounding factors, communication in its entirety is critical, and there is increasingly a view that interventions to improve adherence should focus not just on consumers but on the wider patient context and healthcare system. An emerging theme among recent research is an emphasis on adopting patient‐centred care and shared decision‐making principles in order to achieve better adherence, together with attention to barriers that may be targets for interventions (Garner 2007; Munro 2007).
Why it is important to do this overview
An overview of systematic reviews examined the evidence on interventions to improve adherence to medicines (Van Dulmen 2007). This work identified many simple and complex interventions aiming to improve adherence, typically with mixed effects. Measuring adherence and seeking to understand it as a key aspect of medicines use is important, but taken in isolation fails to consider the wider management, communication and decision‐making roles that exist for consumers when considering or undertaking treatment with medicines.
In this overview we seek to extend previous research in the area beyond adherence, and to systematically identify and organise this literature. There is a need to deliberately consider interventions on consumers' medicines use which have purposes other than, or in addition to, adherence. This includes strategies with broader aims related to medicines, such as promotion of informed decision making or information to improve medicines awareness and literacy, better communication about medicines, improved support for medicines use and increased recognition of and minimisation of medicines‐related adverse events. Our approach also includes collecting information on a comprehensive range of outcomes in addition to adherence, such as consumers' knowledge, skills, capacity and their ability to minimise harms, as well as outcomes for healthcare professionals and systems which are fundamental to understanding and supporting consumers' medicines use. We believe that this broad approach is worthwhile, as improving adherence is not the only important outcome for consumers, health professionals, systems or decision makers.
Taking this wider view of consumers’ medicines use is essential if we are to better understand why ‐ or why not ‐ interventions aiming to improve adherence and medicines use are effective. Partnerships in which consumers are involved actively as managers of medicines and decision makers with health professionals are important. Involving consumers in their choices about medicines could also be central to the sustainability of evidence‐informed treatments. However, since interventions span diseases, populations and treatment settings, it may be difficult for decision makers, healthcare professionals and researchers to find and use the evidence on what works. We therefore originally undertook this overview to systematically gather, evaluate and organise the review‐level evidence on consumer‐oriented medicines interventions, to improve access to the evidence in order to inform decision making. This update was undertaken to ensure currency of the review‐level evidence.
Objectives
To update our synthesis of the evidence from systematic reviews examining the effects of interventions which target healthcare consumers to promote safe and effective medicines use by consumers. This overview also aimed to provide an overall structure and synthesis of the evidence on the range of interventions with which it is possible to target consumers' medicines use.
Methods
Criteria for considering reviews for inclusion
Types of reviews
We included all reviews published in English that met our selection criteria and which were published in the:
Cochrane Database of Systematic Reviews (CDSR); and
Database of Abstracts of Reviews of Effects (DARE).
Reviews eligible for inclusion were those of randomised controlled trials (RCTs), quasi‐randomised controlled trials (CCTs), controlled before‐and‐after studies (CBAs), interrupted time series (ITS) or before‐and‐after (BA) studies. Reviews of other study designs or of qualitative studies were excluded, although issues raised by reviews of qualitative studies were considered in the Background.
Types of participants
We included consumers, defined as any person using medicine(s), either a patient, carer or both, and targeted as individuals or as groups. We also included healthcare professionals who prescribed or monitored medicines. To be included, interventions must have explicitly targeted consumers as primary recipients. We excluded reviews which focussed solely or primarily on interventions for healthcare professionals, services or systems, as these are the focus of work undertaken by the Cochrane Effective Practice and Organisation of Care (EPOC) Review Group (Weir 2009).
There were no restrictions based on the medicines being used or prescribed (type of medicine, indication, number of concurrent medicines), the number or type of health problems, or other participant features.
'Medicines' were defined as any prescribed or over the counter medicine, taken acutely, chronically or intermittently. We also included vaccines but considered them separately to other medicines.
Types of interventions
There are many interventions to influence the use of medicines by consumers. To help to organise and provide a framework for selecting and evaluating interventions we developed a taxonomy based on the purpose of interventions (for details of the intervention taxonomy see Additional Table 1; Lowe 2010). We included interventions which fell into one of the eight categories below:
1. Taxonomy of interventions and reviews mapped to intervention categories.
| Providing information or education (20 original reviews (4 of which are updated) plus 23 new reviews) total = 43 reviews |
|
Definition: Strategies to enable consumers to know about their treatment and their health. Interventions include those to educate, provide information or to promote health or treatment. Interventions can be provided to individuals or groups, in print or verbally, or face to face or remotely. Interventions may be simple, such as those seeking solely to educate or provide information; or complex, such as those to promote or manage health or treatment as part of a multifaceted strategy. |
Examples of interventions:
|
|
Reviews mapped to this category: Al‐aqeel 2011; Amico 2006; Bain‐Brickley 2011; Bennett 2009; Buckley 2010; Chivu 2008; De Bleser 2009; Gleeson 2009; Gray 2009; Halpern 2011; Haynes 2008; Haywood 2009; Holland 2008; Koshman 2008; Lewin 2010; Liu 2008; Machado 2007a; Machado 2007b; Machado 2008; Maglione 2002; Mbuba 2008; Morrison 2001; Nicolson 2009; Nkansah 2010; Odegard 2007; Olthoff 2005; Oyo‐Ita 2008; Parr 2009; Ranji 2008; Rueda 2006; Russell 2006; Schedlbauer 2010; Schroeder 2004; Smith 2009; Stevenson 2004; Stone 2002; Thomas 2010; Wright 2006; Van Wijk 2005; Vergouwen 2003; Vermeire 2005; Yankova 2008; Zygmunt 2002 |
|
Bottom‐line statements of effectiveness: Overall interventions that provide information or education as a single component may be ineffective to improve adherence or clinical outcomes. There is insufficient evidence to determine whether these interventions, when delivered alone, reduce adverse effects, but there is some evidence that they may improve knowledge. There is also some evidence that patient education and/or information as a single component or as part of a more complex intervention may be effective in improving immunisation rates. When used in combination with other interventions, such as self‐management skills training, counselling, or as part of pharmacist‐delivered packages of care, there is some evidence that education or information may improve adherence and other outcomes such as clinical outcomes and knowledge, but results are mixed. |
| Facilitating communication and/or decision making (8 original reviews (1 of which is updated) plus 2 new reviews) total = 10 reviews |
|
Definition: Strategies to involve consumers in decision making about medicines. Interventions include those that aim to help consumers make decisions about medicines use; to encourage consumers to express their beliefs, values and preferences about treatments and care; and/or to optimise communication with consumers about medicines use and related issues. |
Examples of interventions:
|
|
Reviews mapped to this category: Bhogal 2006; Halpern 2011; Haynes 2008; McIntosh 2006; Ranji 2008; Roughead 2005; Spurling 2007; Stevenson 2004; Thomas 2010; Zygmunt 2002 |
|
Bottom‐line statements of effectiveness: There is insufficient evidence from one key review to determine whether interventions focussed on promoting communication about medicines between patients and professionals are effective. There are other interventions which aim to optimise communication but which don't focus specifically on promoting communication per se. Overall, there is some evidence to support the use of these broader interventions which do not have a specific focus on facilitating decision making and/or communication, but effects are mixed. Delayed prescribing is effective to decrease antibiotic use, but has mixed effects on clinical outcomes, adverse events and satisfaction. In general, there is some evidence of effect from education and enhanced follow‐up, facilitators working with physicians to encourage preventive services, and pharmaceutical care services for improving adherence and knowledge. There is insufficient evidence to support the use of psychosocial interventions, which are generally ineffective. There is insufficient evidence to determine the effectiveness of structured counselling or compliance therapy, or of group or home‐based visits to promote vaccination. |
| Acquiring skills and competencies (9 original reviews (1 of which is updated) plus 4 new reviews) total = 13 reviews |
|
Definition: Strategies focussing on the acquisition of skills relevant to medicines use. These interventions aim to assist consumers to develop a broad set of competencies around medicines use and health, such as medicines management or monitoring; or training consumers in the correct use of devices to deliver treatment, or the correct use of treatments. |
Examples of interventions:
|
|
Reviews mapped to this category: Argarwal 2011; Amico 2006; Bainbridge 2006; Bhogal 2006; Garcia‐Alamino 2010; Haynes 2008; Morrison 2001; Rueda 2006; Roughead 2005; Russell 2006; Vermeire 2005; Wright 2006; Yankova 2008 |
|
Bottom‐line statements of effectiveness: There is some evidence that strategies which focus on the acquisition of skills and competencies may improve adherence and clinical outcomes, but results are mixed. Regarding specific types of interventions, there is sufficient evidence that people self‐managing antithrombotics (self‐testing and self‐adjusting therapy based on a predetermined dose schedule) is generally effective to decrease thromboembolic events and mortality; and some evidence that self‐management improves clinical outcomes, with mixed results. There is also insufficient evidence that self‐management improves major haemorrhages, but because these events are rare this result most likely arises due to insufficient power to detect a clinical difference. There is sufficient evidence that self‐monitoring (self‐testing and calling clinic for the appropriate dose adjustment) of antithrombotics is generally effective to decrease major haemorrhages, and some evidence it improves clinical outcomes ‐ results are mixed. However, there is insufficient evidence that self‐monitoring improves thromboembolic events or mortality but again, because these are rare events, these results may arise because of a lack of power to detect a clinical difference. In hypertension, there is sufficient evidence that home blood pressure monitoring is generally effective to improve clinical markers for hypertension, medicines overuse, and therapeutic inertia. There is insufficient evidence to support the provision of training by pharmacists to improve adherence, but some evidence that it improves knowledge and medicines use. There is insufficient evidence to support the use of self‐administration programmes to improve medicines adherence, knowledge, errors or satisfaction ‐ they are generally ineffective. There is some evidence to support the provision of counselling of patients and/or physicians by pharmacists to improve adherence, but insufficient evidence to support more intensive patient care by pharmacists. There is some evidence that patient‐controlled analgesia (PCA) increases analgesic consumption and it may decrease pain scores, although with mixed results. There is some evidence that structured PCA education is generally effective to improve knowledge, but insufficient evidence that it improves postoperative pain control. |
| Supporting behaviour change (26 original reviews (6 of which are updated) plus 27 new reviews) total = 53 reviews) |
|
Definition: Strategies focussing on the adoption or promotion of health behaviours and treatment behaviours, such as adherence to medicines. Included are interventions at an individual level that address behaviour change for the under‐use, overuse or misuse of medicines, and may include practical strategies to assist consumers in taking their medicines correctly such as reminder devices, pre‐packaging of multiple medicines, or different or simplified medicines formulations. |
Examples of interventions:
|
|
Reviews mapped to this category: Al‐aqeel 2011; Amico 2006; Bain‐Brickley 2011;Bennett 2009; Buckley 2010; Bhogal 2006; Chivu 2008; De Bleser 2009; Ford 2009; Garcia‐Alamino 2010; Gleeson 2009; Gray 2009; Halpern 2011; Haynes 2008; Haywood 2009; Holland 2008; Jacobson 2005; Koshman 2008; Lewin 2010; Liu 2008; Lutge 2012; Machado 2007a; Machado 2007b; Machado 2008; Maglione 2002; Mahtani 2011; McIntosh 2006; Molife 2009; Mollon 2009; Morrison 2001; Nicolson 2009; Nishtala 2008; Nkansah 2010; Odegard 2007; Olthoff 2005; Orton 2005; Oyo‐Ita 2008; Parr 2009; Polis 2007; Rueda 2006; Russell 2006; Saini 2009; Schedlbauer 2010; Schroeder 2004; Smith 2009; Stone 2002; Thomas 2010; van Eijken 2003; Vergouwen 2003; Vermeire 2005; Volmink 2007; Wright 2006; Zygmunt 2002 |
|
Bottom‐line statements of effectiveness: Overall, there were mixed effects of interventions to support behaviour change in relation to medicines use. There is some evidence of the effectiveness of simple interventions for short‐term treatments, and complex interventions for long‐term treatments to improve adherence and clinical outcomes. More specifically, there is sufficient evidence that self‐monitoring or self‐management programmes improve medicines use, adherence and clinical outcomes. There is some evidence that immunisation rates are improved by each of the following: reminders, lay health worker interventions, home visits plus vaccination, free vaccination, facilitators working with physicians and financial incentives to physicians. There is some evidence that simplified dosing regimens are generally effective in improving medicines adherence, although the optimal dosing regimen is not known. There is also some evidence that reminders, cues and/or organisers, reminder packaging and material incentives are effective to improve medicines adherence, but with mixed results. There is some evidence that support and education, support and motivation, education and training, or information and counselling interventions, are effective to improve adherence and medicines use outcomes, although results are again mixed. There is also some evidence that quality improvement strategies with an educational component targeting patients are effective to decrease proportions of patients receiving antibiotics, with mixed results. There is also some evidence that pharmacist‐led medicines review is generally effective to reduce medicines problems and unnecessary medicines. There is some evidence that other interventions involving pharmacists directly (such as expanded roles encompassing disease education and medicines management) are effective to improve adherence, numbers of prescribed medicines and clinical outcomes, although results are mixed. Finally there is some evidence that computerised prescribing support can be effectively implemented and change provider behaviour but appears ineffective to change patient outcomes. |
| Support (12 original reviews (1 of which is updated) plus 5 new reviews) total = 17 reviews |
|
Definition: Strategies to provide assistance and encouragement to help consumers to cope with and manage their health and related medicines use. Interventions can target patients or carers, as individuals or in groups, and may be delivered face to face or remotely. |
Examples of interventions:
|
|
Reviews mapped to this category: Amico 2006; Bain‐Brickley 2011; Gleeson 2009; Halpern 2011; Haynes 2008; Holland 2008; Lummis 2006; McIntosh 2006; Odegard 2007; Rueda 2006; Russell 2006; Schroeder 2004; Stevenson 2004; Van Wijk 2005; Vergouwen 2003; Wright 2006; Zygmunt 2002 |
|
Bottom‐line statements of effectiveness: Due to the mixed results from studies found in most reviews, we can state that there is some evidence that interventions that provide support alone or in combination with other strategies may be effective to improve adherence. There is insufficient evidence to determine for which conditions support may be effective, or who should provide the support for greatest effect. |
| Minimising risks or harms (15 original reviews (2 of which are updated) plus 18 new reviews) total = 33 reviews |
|
Definition: Strategies with a specific focus on preventing or managing adverse events of treatment and complications of disease. Interventions can be for ongoing treatment or related to emergency or crisis events. Strategies can be to minimise risks or harms at an individual level or a population level (eg reducing antibiotic use; or augmenting immunisation uptake). |
Examples of interventions:
|
|
Reviews mapped to this category: Amico 2006; Argarwal 2011; Bainbridge 2006; Bayoumi 2009; Bhogal 2006; Castelino 2009; Ford 2009; Garcia‐Alamino 2010; Golicki 2008; Haynes 2008; Holland 2008; Jacobson 2005; Jegu 2011; Koshman 2008; Lewin 2010; Liu 2008; Lutge 2012; Lummis 2006; Maglione 2002; Misso 2010; Mollon 2009; Nishtala 2008; Oyo‐Ita 2008; Pankowska 2009; Ranji 2008; Roughead 2005; Royal 2006; Spurling 2007; Stevenson 2004; Stone 2002; Thomas 2010; Volmink 2007; Wright 2006 |
|
Bottom‐line statements of effectiveness: There is sufficient evidence that self‐management and self‐monitoring interventions are both effective at decreasing adverse events of anticoagulant therapy, but self‐management also appears effective to decrease mortality. For hypertension, there is also sufficient evidence that home blood pressure self‐monitoring is effective, and some evidence that PCA is effective, to improve medicines use and clinical outcomes. For diabetes there is some evidence that continuous insulin infusion in adults and children may improve medicines use and some measures of diabetes control, but it appears ineffective to reduce adverse events. There is also some evidence that strategies to improve interactions between healthcare professionals and patients may decrease adverse events and improve other outcomes such as specific medicines problems, but results are mixed. In particular, there is insufficient evidence to determine whether the use of patients’ own medicines (POMs) in hospital is effective; while self‐administration programmes for hospital inpatients appear ineffective to improve medicines adherence, knowledge or errors. There is some evidence that educational strategies to minimise risks and harms may be effective, and that telling patients about adverse effects of medicines does not negatively influence adherence. There is also some evidence that computerised prescribing support interventions can be effectively implemented and change provider behaviour, but they may be ineffective to improve patient outcomes. For immunisation uptake, there is sufficient‐to‐some evidence that (alone or in different combinations), organisational change, reminders and recall, particularly tailored reminders, financial incentives, home visits, free vaccination, education, lay health worker interventions and facilitators working with physicians are each generally effective. The effects of mass mailings are mixed. Reminders with outreach and physician reminders alone both appear ineffective. There is some evidence that directly observed therapy for tuberculosis (TB) or HIV treatment is generally ineffective to improve treatment completion, adherence or clinical outcomes. There is some evidence that material incentives and lay health worker interventions improve adherence to TB treatment, with mixed results, and insufficient evidence to decide on the effects of late patient tracers. There is sufficient‐to‐some evidence that delayed antibiotic prescription may decrease prescribing rates and antibiotic use without increasing complications, but it may increase supplementary medicines use and results are mixed for clinical outcomes, adverse effects and insufficient to determine effects on antimicrobial resistance. While there is insufficient evidence to determine the effects of broader quality improvement strategy on antimicrobial resistance, adverse events, and health service use; they are generally effective at improving prescribing rates or proportions of patients using antibiotics. |
| Improving quality (17 original reviews (2 of which are updated) plus 13 new reviews) total = 30 reviews |
|
Definition: Strategies to improve the total package, coordination or integration of care delivered. Interventions can involve substitution or expansion of one type of care, such as interventions that aim to overcome system barriers to medicines use, including access and financial barriers. |
Examples of interventions:
|
|
Reviews mapped to this category: Aaserud 2006; Austvoll‐Dahlgren 2008; Bayoumi 2009; Bower 2006; Buckley 2010; Castelino 2009; De Bleser 2009; Giuffrida 1997; Haynes 2008; Haywood 2009; Holland 2008; Koshman 2008; Lewin 2010; Lummis 2006; Maio 2005; Mbuba 2008; Nishtala 2008; Nkansah 2010; Odegard 2007; Oyo‐Ita 2008; Polis 2007; Ranji 2008; Roughead 2005; Royal 2006; Schroeder 2004; Stevenson 2004; Stone 2002; Thomas 2010; van Eijken 2003; Vergouwen 2003 |
|
Bottom‐line statements of effectiveness: As this overview did not specifically identify reviews which targeted organisational or structural interventions to change consumers' medicines use, only provisional conclusions about the effectiveness of those interventions are provided here. There is some evidence that changing the coordination of care (eg changing roles of healthcare professionals to interact with patients or to provide additional services to patients) may improve adherence and other outcomes related to medicines use, such as total numbers prescribed, medicines appropriateness or unnecessary medicines. However, the results from most reviews, taken together, are mixed. Overall, effects on adverse events and clinical outcomes were also typically mixed with these interventions. For depression, there appears to be some evidence that interventions aiming to improve quality are generally effective to improve adherence and symptoms; whereas for heart disease and hypertension effects on adherence and clinical outcomes are typically mixed. In older people, there appears to be some evidence that pharmacist‐delivered interventions to optimise medicines use are generally effective to improve medicines outcomes (such as appropriateness and unnecessary medicines) but mixed evidence for effects on adherence and insufficient evidence for other outcomes including adverse events. When considered broadly, there is some evidence that financial interventions are effective, with mixed results; and that pharmaceutical pricing policies aimed at indirectly influencing consumers’ use of medicines are effective to improve medicines use and costs, but results are mixed for effects on health status and health service use. There is some evidence that organisational interventions are effective at improving immunisation uptake. However, there is insufficient evidence to decide whether free provision of medicines improves treatment adherence; and insufficient evidence to determine the effects of supporting patient’s use of their own medicines in hospital. |
| Consumer system participation (0 reviews) |
|
Definition: Strategies to involve consumers in decision making processes on medicines prescribing and use at a system level, such as in research planning, formulary and policy decisions. Interventions can involve consumers in different roles, such as planning, research, audit and review and governance. |
Examples of interventions:
|
|
Reviews mapped to this category: None. |
|
Bottom‐line statements of effectiveness: There is insufficient evidence to determine the effects of consumer system participation in medicines‐related activities because no reviews were identified. |
Providing information or education
Facilitating communication and/or decision making
Acquiring skills and competencies
Supporting behaviour change
Support
Minimising risks or harms
Improving quality
Consumer system participation.
Many systematic reviews may be relevant to understanding the effects of interventions relevant to the use of medicines by consumers. We developed selection criteria to help us to identify the most highly‐relevant reviews. These selection criteria were used to rank reviews as high, moderate or low/very low relevance. In this overview, we included only those reviews ranked as high relevance to consumers' medicines use, based on them meeting the following criteria:
The main objective of review focussed exclusively on evidence‐based medicines use by and prescribing for consumers (ie safe and effective medicines use by consumers); and
The interventions in the review were directed to consumers and exclusively focussed on evidence‐based medicines use by and prescribing for consumers; and
The outcomes of studies in the review were related to medicines use by and prescribing for consumers (searched for and/or found and/or reported).
We included reviews evaluating both 'direct to consumer' interventions and ‘indirect to consumer’ interventions, or a combination. Direct to consumer interventions were defined as those with a direct interface or line of communication with consumers, for example, through education or counselling. In comparison, indirect to consumer interventions were not immediate to the consumer, but still aimed to influence their medicines use, for example, through structural, organisational, financing or system of care delivery strategies.
There were no restrictions according to the: medical condition(s); type(s) of medicine prescribed, taken or targeted; intervention setting; or duration of treatment.
Reviews were also unrestricted based on comparisons examined, therefore all of the following were eligible for inclusion:
Intervention versus any control (no intervention, usual care, placebo or other control)
One intervention versus another.
Types of outcome measures
We sought data for outcomes in the following categories:
Consumer‐oriented outcomes, such as knowledge and understanding, skills acquisition, and health status and wellbeing;
Provider‐oriented outcomes, including knowledge and understanding and evaluation of care; and
Health service‐oriented outcomes, including service use outcomes and costs.
For a full list of outcomes sought, see Additional Table 2.
2. Taxonomy of medicines outcomes and examples of outcomes reported by reviews.
| Major outcome category | Examples of outcomes from taxonomy category | Examples of outcomes from included reviews |
| Consumer outcomes | ||
| Consultation and communication by consumer | Communication aides (eg summaries, recordings, internet), communication enhancement (eg improved communication with provider) |
|
| Knowledge and understanding | Information access and use, knowledge acquisition (level, change in levels, family members’/carers’ knowledge, knowledge about expected and undesired effects of treatment, knowledge of risk/accurate knowledge of risk, changes to beliefs about disease/treatment), knowledge retention |
|
| Consumer involvement in care process | Decision making (decision making process, decision support provided, decisional conflict, decisions made, patient and carer preferences, agreement between personal values and choices/outcomes), availability of patient‐held information |
|
| Consumer evaluation of care | Consumer‐professional interactions (experience of), perceptions and ratings of care/interventions/treatment, satisfaction (with information provided, with decision made, with care, carer satisfaction, sense of control) |
|
| Support and consumer skills acquisition | Practical support (eg technical aids), psychosocial support (eg self‐help groups, peer or family support), self care skills, communication skills, activities of daily living skills |
|
| Health status and wellbeing | Clinical and physiological outcomes, ie physical health (patient or carer), psychological health (patient or carer), psychosocial outcomes (quality of life, personal cost of illness, personal cost of medicines) |
|
| Health behaviour | Related to attitudes towards the condition/treatment |
|
| Adverse events | Complications, morbidity/mortality, relapse, side effects of medicines |
|
| System benefits | Hospital and specific service use, adverse events (system – complaints and litigation, reporting of adverse events), costs |
|
| Provider outcomes | ||
| Consultation and communication by provider | Practice style – level of patient‐centred care |
|
| Knowledge and understanding | Knowledge, attitudes towards treatments |
|
| Evaluation of care | Satisfaction, anxiety of professional |
|
Search methods for identification of reviews
Handsearching for reviews
Reviews of consumer‐oriented medicines interventions cannot be reliably identified by key word or subject heading searching as they typically encompass a diverse range of interventions. Additionally, relevant interventions may be disease‐specific but also have applicability across diseases, and so are not reliably captured using systematic database searches (Ryan 2011a).
Relevant reviews were therefore identified in two steps:
Step 1: Identification of all reviews on consumer‐oriented interventions.
One investigator handsearched CDSR and DARE databases, screening by review title and abstract to identify all reviews published in English and relevant to communicating with consumers and improving their participation in health care (irrespective of relevance to medicines). This involved identifying all reviews of interventions to communicate with, inform or educate, support or seek the participation of consumers.
Step 2: Selection of reviews relevant to medicines use.
Two investigators independently screened the set of reviews identified in step 1, by title and abstract to identify all reviews of any relevance (high, moderate, low/very low) to consumers' medicines use. All reviews identified as relevant in this step were obtained in full text for further assessment.
For the original overview (Ryan 2011b), we searched from database inception up to and including Issue 3 2008 of The Cochrane Library. In this update we searched forward, from Issue 4 2008 up to March 2012 (inclusive) of The Cochrane Library.
Data collection and analysis
Selection of reviews identified by handsearching
We categorised reviews of any relevance to consumers' medicines use by assessing the full‐text review. Two investigators working independently applied the criteria for ranking reviews (outlined in Criteria for considering reviews for inclusion ‐ Types of interventions) to identify those of high relevance. Differences were resolved by discussion or by consultation with a third party to reach consensus. We excluded from this overview those reviews ranked as moderate relevance or lower; see Characteristics of excluded reviews table for list of excluded reviews and reasons for exclusion (available at https://doi.org/10.26181/19320386.v1).
To minimise duplication amongst reviews, we developed a second set of selection criteria which were applied in two steps (see below) to high relevance non‐Cochrane systematic reviews identified in DARE. This was in order to remove reviews that were considered to duplicate Cochrane reviews, while retaining reviews whose scope was not covered by Cochrane reviews.The rationale for this decision was twofold: first, Cochrane reviews are, in the main, of higher quality than systematic reviews from other sources (Moher 2007); and second, Cochrane reviews are regularly updated to reflect the state of the evidence, whereas reviews from other sources typically are not.
High relevance non‐Cochrane reviews were therefore screened in two further selection steps and were excluded from this overview if:
Step 1:The review was of low quality. The non‐Cochrane review was excluded if it was rated as low quality or had serious methodological flaws according to the Centre for Reviews and Dissemination assessment of the review published as part of the DARE abstract; and as assessed by the authors using the AMSTAR assessment tool (Shea 2007; rating of less than 4 of a possible 11 points; see Data collection and analysis ‐ Quality assessment of included reviews, for details of the AMSTAR tool and assessment).
Step 2: The review had substantial overlap with Cochrane reviews. For each non‐Cochrane review, we identified all Cochrane reviews with a similar scope and the degree of overlap with these Cochrane review(s) assessed to determine how many unique studies would be contributed by inclusion of the non‐Cochrane review. Non‐Cochrane reviews with approximately 50% or more of their studies already captured by Cochrane reviews were generally excluded. Where we identified two non‐Cochrane reviews with similar scope (duplicative reviews) the higher‐quality review was included in this overview. Two investigators working independently assessed these reviews, with differences resolved by discussion or by consultation with a third party to reach consensus. We provide details of high relevance, non‐Cochrane reviews excluded at the full‐text stage based on these two further screening steps in the Characteristics of excluded reviews table, see https://doi.org/10.26181/19320386.v1; also refer to Figure 1.
1.
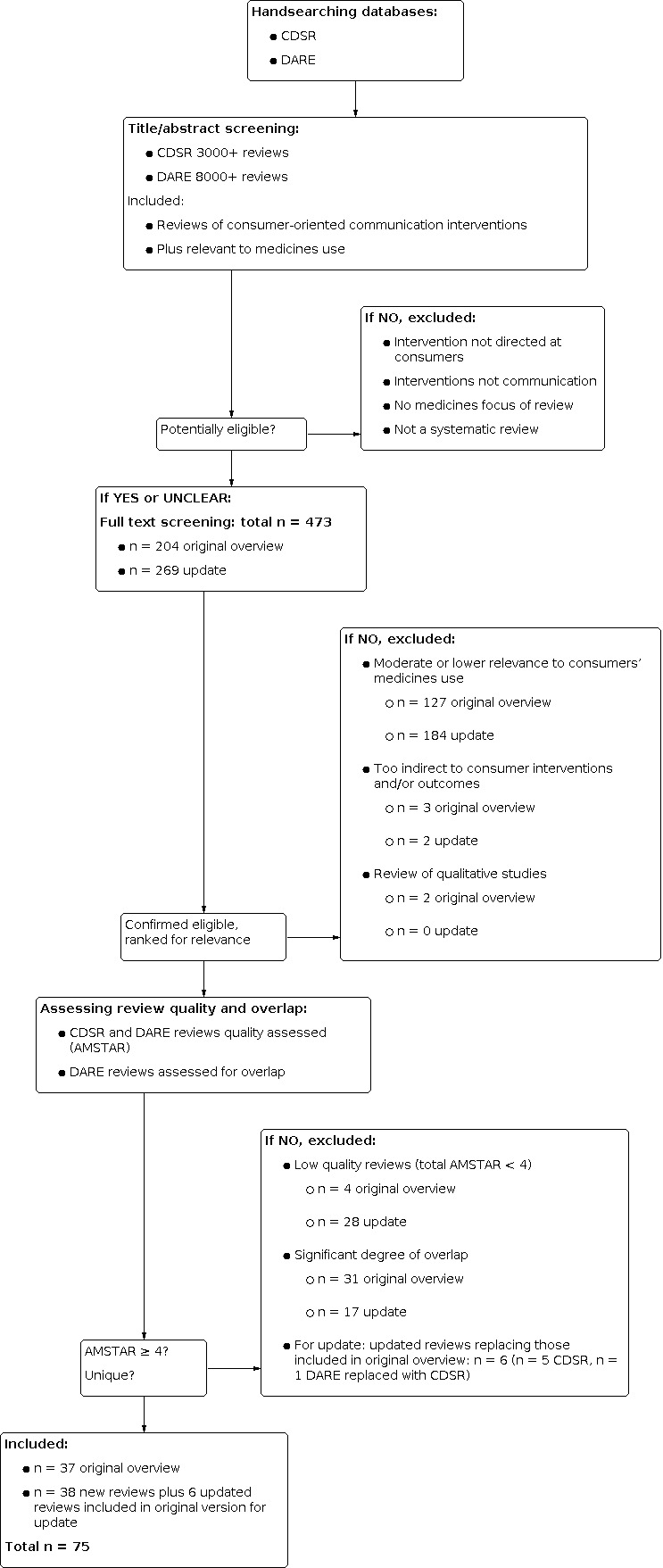
Review screening, selection and assessment steps, and numbers at each stage
Data extraction
We developed and piloted a data extraction form to summarise the key characteristics of reviews, including information about the objectives, participants, intervention features, outcomes assessed and comparisons performed; as well as the quality of included studies, quality of the review and the review's results. One investigator extracted data and a second investigator verified the extracted data. Differences were resolved by discussion to reach consensus.
Quality assessment of included reviews
We assessed the quality of included systematic reviews using the AMSTAR instrument (Shea 2007). AMSTAR assesses the degree to which review methods avoided bias by evaluating the methods against 11 distinct criteria, including:
use of an 'a priori’ design;
duplicate study selection and data extraction;
comprehensive searching of the literature;
use of publication status as an exclusion criterion;
provision of (included and excluded) studies;
provision of characteristics of included studies;
assessment of methodological quality of included studies;
appropriate use of quality of included studies in formulating conclusions;
appropriate methods for combining results of studies;
assessment of publication bias; and
conflict of interest (both review and included studies) stated.
Each AMSTAR item was rated as yes (clearly done), no (clearly not done), can't answer, or not applicable, based on the published review report. A review that adequately met all of the 11 criteria was considered to be a review of the highest quality. Quality rating was as follows:
| AMSTAR score (out of 11 criteria) | Rating |
| 8 to 11 | high quality |
| 4 to 7 | moderate quality |
| 3 or lower | low quality |
One investigator assessed review quality and a second investigator verified this assessment. Differences were resolved by discussion to reach consensus.
Quality assessment of included studies within reviews
We did not reassess the quality of included studies within reviews but instead reported study quality according to the review authors' assessment. We collected this information during the data extraction process. We used ratings of study quality in the synthesis and interpretation of results; for example, to downplay the certainty of conclusions and ratings of effectiveness where studies were all of poor methodological quality or had serious methodological shortcomings that may have predisposed the review's results to bias. For example, finding intervention 'x' effective but with serious methodological limitations, conclusions of 'sufficient evidence' would be downgraded to 'some evidence' to reflect a lower degree of confidence in the findings from the review overall.
Extracting data and identifying relevant outcomes
We identified outcomes for data extraction by screening against the medicines outcome taxonomy developed for this overview (Additional Table 2), agreed upon by two investigators reaching consensus.
We developed the medicines outcome taxonomy by assessing the range and types of interventions on consumers' medicines use (and used to develop the intervention taxonomy; see Lowe 2010; Ryan 2010; Ryan 2011a) and by those outcomes relevant to these medicines interventions. The identified medicines‐related outcomes were then mapped back onto Cochrane Consumers and Communication Review Group (CC&CRG) outcome taxonomy categories, which comprehensively articulates and organises outcomes on communication with and participation by consumers. It maps outcomes at different levels within the health system: consumers, providers and systems (available at: http://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/uploads/Outcomes.pdf).
These steps were undertaken by two investigators working together (NS, RR), in consultation with a third investigator with expertise in research on consumer communication and participation (SH). These steps were used to identify iteratively broad and specific medicines outcomes and to organise them into a meaningful taxonomy.
In the original version of this overview, one author entered all data from data extraction forms into RevMan and this was checked for accuracy by a second author working independently. In the update of this overview, one author entered data from extraction forms into RevMan and a random selection of reviews was checked for accuracy by a second author (MP) working independently.
Statistical presentation of results from reviews
For each included review, we extracted all results for medicines‐related outcomes.
Within individual reviews, we extracted and reported, where available, pooled effect sizes for outcomes meta‐analysed in reviews; or a range of effect sizes from their included studies. We preferred absolute rather than relative effect sizes, and calculated these wherever possible (Akl 2011). In all cases, one investigator extracted results and performed conversions to absolute effect sizes, and this was verified by a second investigator, with disagreements resolved by discussion to reach consensus.
If the above information was not available, we used vote counting by direction of effect or by statistical significance, in order to allow us to report results consistently across included reviews. Vote counting sums and compares the numbers of studies reporting particular outcomes, for example: the numbers of studies reporting positive results compared with the number reporting negative results for a particular outcome; or the number of studies reporting statistically significant results compared with the number reporting no statistically significant results for a certain outcome. Where none of these forms of reporting were possible, for example, where outcomes were reported descriptively by single studies, we reported these results using standardised language indicating direction of effect and statistical significance. It should also be noted that vote counting as a synthesis method is by no means universally accepted, and often researchers are advised to adopt other ways of summarising results (Higgins 2011). We acknowledge that vote counting has limitations, but we adopted it for this overview as there were few other robust alternative methods by which to summarise such diverse results across reviews.
Summaries of main results
As well as numerical data, we extracted and descriptively summarised each study's results using standardised language, in order to allow consistent reporting of results across reviews. Two investigators analysed and summarised results of the included reviews, and reported them narratively to enable identification of broad conclusions within and across reviews.
Synthesis of results and rating the evidence of effectiveness
We formulated standardised ‘effectiveness statements’ to rate the evidence arising from reviews, using a further synthesis step that went beyond a simple summary of the main results of each review. These statements were based on the rating scheme developed by the CC&CRG to help synthesise and rate the evidence across systematic reviews where interventions are complex and diverse (Ryan 2005; Ryan 2009a; Ryan 2011a). See the table below for a full explanation of the terms used and how these definitions were applied to developing effectiveness statements.
| Summary statement | Translation |
| Sufficient evidence | Evidence to make a decision about the effect of the intervention(s) in relation to a specific outcome(s). This includes evidence of an effect in terms of (i) benefit or (ii) harm. Statistically significant results are considered to represent sufficient evidence on which to base decisions, but a judgement of sufficient evidence is also made based on the number of studies/participants included in the analysis for a particular outcome. A rating of sufficient evidence is often based on meta‐analysis producing a statistically significant pooled result that is based on a large number of included studies/participants. This judgement may also be made based on the number of studies and/or study participants showing a statistically significant result ‐ for example (in a narrative synthesis) a result where 12 studies of a total of 14 for a specific outcome showed a statistically significant effect of an intervention would be considered to represent sufficient evidence. |
| Some evidence | Less conclusive evidence to make a decision about the effects of a particular intervention(s) in relation to a specific outcome(s).This may be based on narrative syntheses of review results. In this case, the result is qualified according to the findings of the review ‐ for example, 'some evidence (5 studies of 9) reported a positive effect of .....' (This would be based on a more equivocal set of results than those obtained for 'sufficient evidence' above. For example, while 12/14 statistically significant studies would be classed as 'sufficient evidence', 5/9 statistically significant studies is more equivocal and would be classed as 'some evidence.') This may also be based on a statistically significant result obtained in a small number of studies; a statistically significant result obtained from studies with a small number of participants; or a statistically significant result obtained from studies of low quality. |
| Insufficient evidence | Not enough evidence to support decisions about the effects of the intervention(s) on the basis of the included studies. This should be interpreted as 'no evidence of effect', rather than 'evidence of no effect'. Statistically non‐significant results are considered to represent insufficient evidence. Where the number of studies is small, and/or the number of participants included in the studies is small, insufficient evidence might reflect underpowering of the included studies to be able to detect an effect of the intervention. Where the number of studies is large, and/or the number of participants included in these studies is large, 'insufficient evidence' may reflect underlying ineffectiveness of the intervention to affect the outcomes being examined. In such cases the intervention may additionally be described as 'generally ineffective' in order to separate such results from those cases where insufficient evidence is used to describe results but this is based on a small number of studies and/or participants (where non‐significant results may reflect underpowering of studies rather then ineffectiveness). |
| Insufficient evidence to determine | Not enough evidence to be able to determine whether an intervention is effective or not on the basis of the included studies. This statement is about reporting gaps in the evidence (ie where there are too few studies to be able to determine effects), rather than the situation of the summary statement above, which is about ineffectiveness (eg several studies reporting a statistically non‐significant result). It is likely to arise when the numbers of included studies is very small. |
The effectiveness statements give bottom‐line statements about the main effects of interventions assessed within each intervention category, using standardised language and based on a set of decision rules that take into account the results, statistical significance and the quality and number of studies on which the result is based. For example, the result from a review reported as 'education significantly improved adherence in 1 study' would be given as the bottom‐line statement 'there is insufficient evidence to determine the effects of education on adherence'.
One investigator systematically rated the review's results and a second investigator verified the rating, with disagreements resolved by discussion to reach consensus.
Mapping of reviews to the intervention taxonomy and summarising results across reviews
First, we organised the evidence using the taxonomy of interventions developed in parallel with this overview (Lowe 2010); see Criteria for considering reviews for inclusion ‐ Types of interventions and Additional Table 1.
As part of the data extraction process one investigator assigned reviews to one or more categories of the taxonomy, based on the review's aims. A second investigator verified this mapping, with differences resolved by discussion to reach consensus. As a result of differences in the scope (range) of included interventions within reviews, and the aims of those interventions, intervention categories were not treated as mutually exclusive: some reviews were mapped to multiple categories, while others appear in only one, but this was performed in a deliberate attempt to disaggregate the evidence contributing towards different medicines use objectives. This step was designed to deal with differences across reviews in the way that interventions were split or lumped together. For example some reviews, such as Haynes 2008 (including all interventions to promote medicines adherence) were mapped to almost all intervention categories, based on the diverse range of included interventions. Many other reviews that lumped interventions contained a slightly narrower range of interventions (eg Gleeson 2009 and Gray 2009 both included a range of interventions such as patient education and simplified dosing regimens; Russell 2006 included dose simplification as well as counselling and education; Ranji 2008 included delayed prescribing and educational interventions, amongst others); while others were quite narrow in scope (eg Volmink 2007 and Ford 2009 assessed directly observed therapy; Giuffrida 1997 and Lutge 2012 examined financial and material incentives respectively; Mahtani 2011 assessed the effects of reminder packaging). Such reviews were mapped to fewer intervention categories, based on an assessment of the identifiable aims of the interventions determined by the scope of the review. Since included reviews dealt with the range of potential medicines interventions available so differently, they needed to be unpacked into constituent interventions, based on their purposes, to allow meaningful grouping of like interventions and interpretation of the extracted data and results.
One investigator systematically synthesised each review's extracted data, mapped to an intervention category, to produce an overall summary of the evidence for that intervention category. We developed overall summaries of the standardised statements of effectiveness for each intervention category by systematically summarising the assembled statements for all reviews mapped to that category.
Summaries were written by one investigator and checked by a second investigator, with differences resolved by discussion to reach consensus.
Consumer participation
A consumer representative reviewed the protocol and a consumer peer‐reviewed this overview to ensure that consumers' views are adequately and accurately represented.
Results
Description of included reviews
Figure 1 gives a flow diagram outlining the selection process and review numbers at each stage, for both the original overview and this update.
Stage 1 ‐ original overview
For the original version of this overview (Ryan 2011b), we handsearched the CDSR and DARE databases from inception up to and including Issue 3 (July) 2008, handsearching over 3000 Cochrane systematic reviews of interventions for health care and 8000 reviews in the DARE database, to identify reviews relevant to prescribing for, and medicines use by, consumers.
After screening titles and/or abstracts, we retrieved 204 reviews in full text for further assessment.
After further selection, quality assessment, and categorisation as 'high' or 'other' relevance to consumers' medicines use, we excluded 167 reviews for the following reasons:
Moderate or lower relevance to consumers' medicines use (n = 127).
Significant degree of overlap with other reviews (n = 31).
Low quality review (total AMSTAR score < 4) (n = 4).
Too indirect to consumer (interventions and/or outcomes) (n = 3)
Review of qualitative studies (n = 2).
After all selection and categorisation steps, 37 reviews were identified for inclusion.
Stage 2 ‐ update
For this update we searched forward, from Issue 4 (April) 2008 to March 2012 (inclusive) of the CDSR and DARE databases, retrieving a total of 269 reviews in full text for assessment via handsearching. Of these, we excluded 231 reviews for the following reasons:
Moderate or lower relevance to consumers' medicines use (n = 184)
Significant degree of overlap with other reviews (n = 17)
Low quality review (total AMSTAR score < 4) (n = 28)
Too indirect to consumer (interventions and/or outcomes) (n = 2)
After all selection and categorisation steps, we identified a further 38 new reviews for inclusion in this update. We also checked all CDSR reviews for updates published since the original searches were conducted, identifying 6 updates of reviews included in the original version of the overview (Garcia‐Alamino 2010 (updating Heneghan 2006b); Halpern 2011 (updating Halpern 2006); Lewin 2010 (updating Lewin 2005); Mahtani 2011 (updating Heneghan 2006a); Nkansah 2010 (updating Beney 2000);and Schedlbauer 2010 (updating Schedlbauer 2004)). All six reviews were updates of Cochrane reviews with the exception of Garcia‐Alamino 2010, which was a new Cochrane review updating the previously published DARE review by Heneghan and colleagues (Heneghan 2006b) on the same topic.
In total, 75 unique Cochrane and DARE systematic reviews are included in this updated overview.
Characteristics of the included reviews are presented in tables on the Review Group's website at https://doi.org/10.26181/19320386.v1 together with Characteristics of excluded studies tables containing a full list of reviews with their reasons for exclusion.
Objectives and scope of the reviews
The objectives and scope of included reviews varied, although almost half (35/75, 47%) primarily aimed to improve adherence to medicines or uptake of immunisations (Al‐aqeel 2011; Bain‐Brickley 2011; Amico 2006; Chivu 2008; De Bleser 2009; Ford 2009; Gleeson 2009; Gray 2009; Halpern 2011; Haynes 2008; Haywood 2009; Jacobson 2005; Lewin 2010; Liu 2008; Lutge 2012; Mahtani 2011;Mbuba 2008; McIntosh 2006; Odegard 2007; Olthoff 2005; Orton 2005; Oyo‐Ita 2008; Rueda 2006; Russell 2006; Saini 2009; Schedlbauer 2010; Schroeder 2004; Stone 2002; Thomas 2010; van Eijken 2003; Van Wijk 2005; Vergouwen 2003; Vermeire 2005; Volmink 2007; Zygmunt 2002). These reviews included a wide range of specific strategies, and although reviews most consistently reported on the interventions' effects on adherence, additional effects (outcomes) were also reported, such as clinical outcomes, adverse events, satisfaction, attitudes to medicines, quality of life, and costs.
Almost as many reviews (34/75, 45%) took a slightly wider focus, for example considering medicines use within a clinical or self‐management context, while still targeting consumers directly (Argarwal 2011; Bainbridge 2006; Bayoumi 2009; Bennett 2009; Bhogal 2006; Bower 2006; Buckley 2010; Castelino 2009; Garcia‐Alamino 2010; Golicki 2008; Holland 2008; Jegu 2011; Koshman 2008; Lummis 2006; Machado 2007a; Machado 2007b; Machado 2008; Misso 2010; Molife 2009; Morrison 2001; Nicolson 2009; Nishtala 2008; Nkansah 2010; Pankowska 2009; Parr 2009; Polis 2007; Ranji 2008; Roughead 2005; Royal 2006; Smith 2009; Spurling 2007; Stevenson 2004; Wright 2006; Yankova 2008). These reviews also reported the effects of interventions on adherence, but more consistently reported a range of additional outcomes, such as knowledge, understanding and recall, adverse events, medicines errors, health service use and professionals' workload, dropouts and withdrawals, costs, clinical outcomes and quality of life.
Several reviews evaluated interventions which targeted consumers both directly and indirectly (Bayoumi 2009; Buckley 2010; Haywood 2009; Mbuba 2008; Ranji 2008; Smith 2009; Stone 2002; Vergouwen 2003). For example, Vergouwen 2003 reviewed interventions to improve adherence to antidepressants in which education (direct to consumers) and collaborative care (indirect to consumers through changes to the organisation of care) were evaluated. Bayoumi 2009 evaluated medicines reconciliation interventions designed to identify and reduce discrepancies between what people should be taking and what they actually take, including discharge letters and/or counselling and access to a medicines helpline (direct to consumer interventions) as well as interventions based on academic detailing using weekly audit and feedback (indirect to consumers). Similarly, Ranji 2008 assessed the effects of a range of strategies to reduce antibiotic overuse, including those targetting consumers directly (such as education, financial incentives and disincentives, delayed prescriptions), and those interventions targetting consumers indirectly, such as provider education, audit and feedback, decision support materials and reminders. Stone 2002 reviewed interventions which targeted different levels of the health system to improve adult immunisation, including direct‐to‐consumer interventions such as patient reminders or financial incentives, as well as indirect to consumer interventions such as organisational change, provider financial incentives and provider education. In such reviews, the combined data, plus any separate data from the direct and indirect interventions, were collected and reported wherever possible.
Six reviews (8%) evaluated interventions which were aimed at consumers indirectly (Aaserud 2006; Austvoll‐Dahlgren 2008; Giuffrida 1997; Maio 2005; Maglione 2002; Mollon 2009). All assessed the effects of financial interventions to indirectly influence consumers' use of medicines, except Maglione 2002 which assessed the effects of mass mailing strategies on immunisation uptake and Mollon 2009 which evaluated the effects of prescribing computerised decision support systems (CDSS), including medicine alerts, reminders, medicines reviews and feedback, on providers' prescribing patterns and patient outcomes. These indirect‐to‐consumer reviews reported a range of consumer outcomes relevant to prescribing and medicines use, and this distinguishes the reviews included in this overview from those failing to report consumer outcomes, and which were therefore excluded on the basis of being rated as 'too indirect' to consumer.
Study characteristics and populations
Almost half of the included reviews (32/75 reviews, 43%) included only randomised controlled trials (RCTs) (Argarwal 2011; Bainbridge 2006; Bower 2006; Buckley 2010; Castelino 2009; Ford 2009; Garcia‐Alamino 2010; Giuffrida 1997; Golicki 2008; Halpern 2011; Haynes 2008; Holland 2008; Koshman 2008; Lewin 2010; Lutge 2012; Mahtani 2011; McIntosh 2006; Misso 2010; Mollon 2009; Nicolson 2009; Oyo‐Ita 2008; Pankowska 2009; Parr 2009; Roughead 2005; Rueda 2006; Russell 2006; Schedlbauer 2010; Schroeder 2004; Spurling 2007; Thomas 2010; van Eijken 2003; Vergouwen 2003). This reflects in part the wide recognition that RCTs represent the 'gold standard' study design for evaluating intervention effectiveness. Study designs other than RCTs may be more prone to bias. Nonetheless, selected studies other than RCTs may be appropriate for assessing the effects of complex interventions (EPOC 2013; Higgins 2011; Ryan 2009b).
We explicitly attempted to avoid duplication by excluding non‐Cochrane reviews that had substantial overlap with Cochrane reviews, seeing little advantage in including multiple reviews assessing the same set of trials split and organised in different ways. On the other hand, we also wished to maximise the spread of the interventions under evaluation, and so our assessment of overlap between reviews was formalised and systematic. The result of this trade‐off between duplication and coverage is that there is still some overlap between included reviews. To some extent, overlap is unavoidable where large, general reviews looking across diseases (eg Haynes 2008) are assembled together with more focussed reviews (eg in terms of disease, population, setting or intervention), but with different selection criteria (eg study design, methodological quality, setting and/or participants eligible).
We therefore report the range of studies in each review as opposed to a total number of included studies, as we cannot be certain that there are not duplicated studies across included reviews. There were between 1 (McIntosh 2006) and 78 (Haynes 2008) intervention studies included in each review in this overview. The most recent search date in the reviews was June 2011 (Lutge 2012) and the oldest April 1997 (Giuffrida 1997), but most reviews (60/75, 80%) had conducted their searches before the end of 2008.
Most studies involved adult participants. Seven reviews (Castelino 2009; Holland 2008; Maio 2005; Nishtala 2008; Russell 2006; Thomas 2010; van Eijken 2003) focussed on older adults (60 years or older), while another nine reviews incorporated a wide range of ages that explicitly included older with younger adults (Aaserud 2006; Haynes 2008; Jacobson 2005; Koshman 2008; Lutge 2012; Nicolson 2009; Odegard 2007; Pankowska 2009; Yankova 2008).
Twenty‐one reviews included children together with older participants (Al‐aqeel 2011; Bain‐Brickley 2011; Bhogal 2006; De Bleser 2009; Giuffrida 1997; Haywood 2009; Jacobson 2005; Lewin 2010; Liu 2008; Mbuba 2008; Misso 2010; Molife 2009; Mollon 2009; Nkansah 2010; Oyo‐Ita 2008; Pankowska 2009; Ranji 2008; Roughead 2005; Rueda 2006; Smith 2009; Spurling 2007), and one review included children alone (Golicki 2008).
While most studies focussed on people with a condition and/or taking medicines, as opposed to carers, 19 reviews included studies with carers (Al‐aqeel 2011; Amico 2006; Bain‐Brickley 2011; Bennett 2009; Bhogal 2006; De Bleser 2009; Giuffrida 1997; Haynes 2008; Haywood 2009; Jacobson 2005; Lewin 2010; Liu 2008; Mahtani 2011; Orton 2005; Oyo‐Ita 2008; Ranji 2008; Smith 2009; Spurling 2007; Zygmunt 2002), the majority of whom were family members, for example, parents of children taking medicines or requiring immunisation (eg Lewin 2010; Liu 2008; Oyo‐Ita 2008; Smith 2009).
In 22 reviews, healthcare professionals were included as recipients of the intervention alongside consumers (Buckley 2010; Castelino 2009; Chivu 2008; Gleeson 2009; Haywood 2009; Jacobson 2005; Lummis 2006; Mbuba 2008; Mollon 2009; Morrison 2001; Nishtala 2008; Nkansah 2010; Oyo‐Ita 2008; Ranji 2008; Royal 2006; Smith 2009; Stevenson 2004; Stone 2002; Thomas 2010; Van Wijk 2005; Vergouwen 2003; Wright 2006). In the majority of cases at least some of the professional population were pharmacists, but others including physicians, general practitioners, nurses, psychologists and psychiatrists were also included in a small number of reviews, as were community health workers and informal healthcare providers (eg Lewin 2010; Smith 2009).
In total, 46 reviews evaluated interventions for medicines use in relation to a particular medical condition, including:
asthma (Bhogal 2006
glaucoma or ocular hypertension (Olthoff 2005; Gray 2009)
cardiovascular health: hypertension (Machado 2007b; Schroeder 2004), heart failure (Koshman 2008), hyperlipidaemia (Machado 2008; Schedlbauer 2010) or anticoagulant therapy (Garcia‐Alamino 2010), ischaemic heart disease (Buckley 2010)
mental health: depression (Bower 2006; Vergouwen 2003), schizophrenia (McIntosh 2006; Zygmunt 2002) and psychotropic drug use (Nishtala 2008)
infectious diseases: malaria (Orton 2005; Smith 2009), HIV/AIDS (Amico 2006; Bain‐Brickley 2011; Ford 2009; Rueda 2006), tuberculosis (TB) (Liu 2008; Lutge 2012; Volmink 2007)
diabetes (Golicki 2008; Machado 2007a; Misso 2010; Molife 2009; Odegard 2007; Pankowska 2009; Vermeire 2005)
pregnancy (contraceptive use) (Halpern 2011), advance provision of emergency contraception (Polis 2007) or use of folic acid in pregnancy (Chivu 2008)
epilepsy (Al‐aqeel 2011; Mbuba 2008)
pain relief post cardiac surgery (Bainbridge 2006), postoperatively (Yankova 2008), or for cancer pain (Bennett 2009)
solid organ transplantation (De Bleser 2009)
osteoporosis (Gleeson 2009)
sickle cell disease (Haywood 2009)
opioid dependence (Jegu 2011) and chronic benzodiazepine use (Parr 2009); and
respiratory (Spurling 2007) and other infections (Ranji 2008) in relation to changing antibiotic prescribing and use.
Seven reviews focussed on assessing the effects of interventions for immunisation uptake (Giuffrida 1997; Jacobson 2005; Lewin 2010; Maglione 2002; Oyo‐Ita 2008; Stone 2002; Thomas 2010), although Giuffrida 1997 also included people with a range of chronic and other health problems and treatment aims; as did the review by Lewin 2010 which also aimed to improve adherence to treatments for HIV and TB.
The remaining reviews evaluated interventions for medicines use more generally across populations (and diseases), for example including consumers taking medicines without specifying a particular reason or condition (Aaserud 2006; Austvoll‐Dahlgren 2008; Castelino 2009; Haynes 2008; Holland 2008; Mahtani 2011; Maio 2005; Mollon 2009; Morrison 2001; Nicolson 2009; Royal 2006; Russell 2006; Saini 2009; Stevenson 2004; Van Wijk 2005); although some of these reviews were setting‐specific, for example, considering only hospital inpatients (Lummis 2006; Wright 2006), community‐dwelling older adults (van Eijken 2003), or people in ambulatory and primary care (Bayoumi 2009).
Two other reviews (Nkansah 2010; Roughead 2005) included adults and children with a range of chronic conditions, as well as specifically identifying those at high risk of medicines misadventure, for example, those requiring multiple medicines (polypharmacy).
Most other reviews did not comprehensively consider people requiring polypharmacy, and/or those with co‐morbid conditions (multimorbidity), even though these circumstances may particularly predispose people to medicines‐related problems (such as more adverse events, poor adherence, prescription or dispensing of contraindicated medicines, lack of adequate medicines review, and other problems) which require special attention. This was true even in some reviews where the populations chosen for study are well known to be at risk for sub‐optimal medicines use (eg older community‐dwelling adults).
Of included reviews, 22 did report inclusion criteria and/or included studies in which people with more than one concurrent health problem or taking multiple medicines were represented, but how this was dealt with by studies and/or the reviews themselves was highly varied across included reviews.
In several cases, reviews did explicitly seek and report information on co‐morbid health problems and/or polypharmacy (Gray 2009; Machado 2007a; Machado 2007b; Machado 2008; Misso 2010; Nkansah 2010; Roughead 2005; Russell 2006), although in all of these reviews these issues were only actually addressed in a minority of the included studies within each review.
In several other cases, reviews did not explicitly consider multimorbidity or polypharmac,y but did consider eligible those studies which included people taking multiple medicines and/or with multiple concurrent health problems (ie they did not exclude studies because they considered multiple health conditions and/or medicines) (Austvoll‐Dahlgren 2008; Bayoumi 2009; Haynes 2008; Mahtani 2011; Nicolson 2009; Odegard 2007; Royal 2006; Saini 2009). Again, however, these issues were only considered in the minority of included studies in most of these reviews.
Finally, a number of reviews considered multimorbidity and/or polypharmacy incidentally through their inclusion criteria but not further in the review (Castelino 2009; Holland 2008; Liu 2008; Lutge 2012; Nishtala 2008; Volmink 2007). For example, Castelino 2009 excluded studies that selected people with only a specific condition (where the population eligible for inclusion was older people aged 65 years or more); while three reviews concentrating on medicines for TB did not exclude studies where participants were also HIV‐positive (Liu 2008; Lutge 2012; Volmink 2007).
Interventions
Strategies directly targeting consumers ranged from the very simple (such as reducing the frequency of dosing, changing the medicine formulation, sending a postcard reminder) to the very complex (different combinations of education, medicines reconciliation and/or review, counselling and self‐monitoring, or self‐management programmes). To organise the evidence, we categorised included reviews according to the intervention taxonomy and mapped reviews to intervention categories based on the underlying aim(s) of the included interventions. More detailed descriptions of the interventions included in reviews are presented in the 'Interventions' field of the Characteristics of the included reviews tables, available on the Review Group's website at https://doi.org/10.26181/19320386.v1.
Reviews dealt with interventions in very different ways, reflecting underlying differences in the lumping or splitting of interventions. Some reviews were very focussed, assessing the effects of a single type of intervention with a single identifiable aim ‐ such as reminder packaging (Mahtani 2011), unit‐dose packaging (Orton 2005); or various simplified dose regimens (Saini 2009). These interventions focussed on aiming to improve medicines adherence were mapped to the category 'supporting behaviour change.'
Other reviews were similarly focussed on a single type of intervention, but the intervention itself had multiple purposes. For example, a review on delayed antibiotic prescriptions as a strategy (Spurling 2007) had dual aims, and was mapped to provide evidence for interventions to facilitate communication and decision making (ie enabling decision making about whether to take antibiotics or not) as well as to minimise the risks or harms of medicines use (ie to decrease antibiotic overuse/emergence of antibiotic resistance in the community).
In other cases, reviews incorporated interventions with a broader set of aims, and hence were mapped to a number of intervention categories. For instance, the review by Haynes 2008 assessed all interventions to improve medicines adherence, including practical medicines management interventions such as reminders, packaging or dose simplification (mapped to the supporting behaviour change category); but also included a large range of other interventions with different aims which were mapped to different categories, such as counselling (support), self‐monitoring (acquiring skills and competencies), instruction (providing information or education), and comprehensive pharmaceutical care services (improving quality).
Of note, we identified no reviews on 'consumer system participation' related to medicines, a relatively new area of consumer involvement in health care, in either the original version of this overview (Ryan 2011b) or the current update (see Additional Table 1). Similarly, relatively few reviews addressed the acquisition of skills and competencies (13 reviews with this update), or aimed to facilitate communication and decision making (10 reviews), also relatively new areas in relation to consumers' use of medicines. In contrast, other categories were well populated with evidence from included reviews; in particular, both the 'supporting behaviour change' (53 reviews) and 'providing information or education' (43 reviews) intervention categories.
Outcomes
Most reviews, taken individually and collectively, reported on a relatively narrow range of outcomes, despite the fact that the included interventions and scope of reviews were diverse.
Additional Table 2 shows examples of the range of outcomes reported by included reviews and how these relate to categories of the medicines outcome taxonomy. There was a large range of outcomes reported across the included reviews, taken collectively. However, many individual reviews focussed on adherence, often reporting a very small set of outcomes. Many reviews also did not report outcomes which are necessary for understanding the interventions under consideration, for example, reviews of educational interventions did not routinely report outcomes such as knowledge.
Methodological quality of included reviews
Quality of included reviews
Overall, this overview included 28 Cochrane reviews and 47 DARE reviews. Of the Cochrane reviews, almost all (27/28, 96%) were rated as high quality, with the majority (16/28, 57%) scoring 10 or more points out of a possible 11 on AMSTAR, indicating that these reviews were of high quality and likely to have minimal bias in their design and conduct. Common reasons for a review to lose points on AMSTAR were: not reporting conflicts of interest for both the review authors and in the review's included studies; and the review not assessing publication bias (ie the possibility that results from the review are biased because of the propensity for positive trials to be published and for negative trials not to be).
Of the 47 included DARE reviews, few (6/47, 15%) were rated as high quality (all scored 8 or 9 on AMSTAR). The remaining reviews were rated as moderate quality (scoring between 4 and 7 points); over half of these (25/47, 53%) received a rating of 5 or lower, suggesting that these reviews may be at risk of bias that might influence the results.
Quality of included studies
As reported by review authors, reviews included studies that ranged from high (well designed and conducted studies) to low quality (studies with serious methodological limitations).
A small number of reviews were highly selective about the quality of the studies they included, for example, Haynes 2008 specified that only RCTs with at least 80% follow‐up and unconfounded comparisons would be eligible for inclusion, while Mahtani 2011 included only RCTs with at least 80% follow‐up. Even these measures, however, did not ensure that included studies were of high quality: in both reviews only a minority of studies adequately concealed allocation, for example; while in Mahtani 2011 the majority of included studies were rated as being at high risk of bias, with problems such as unclear randomisation methods identified as methodological limitations.
Almost half of reviews (32/75, 43%) included only RCTs. A small number of these reviews reported that included studies were of generally high quality (eg Buckley 2010; Mollon 2009; Spurling 2007). More commonly, reviews reported that included studies were of generally moderate quality, with some predisposition to bias (eg Argarwal 2011; Ford 2009; Garcia‐Alamino 2010; Holland 2008; Thomas 2010; van Eijken 2003; Vergouwen 2003). In other cases, reviews reported that while included studies were at moderate risk of bias the results were often based on single, or small numbers of, studies (eg Halpern 2011; McIntosh 2006; Nkansah 2010; Oyo‐Ita 2008). Other reviews highlighted particular limitations of the included studies and the likelihood that this would introduce bias, such as studies failing to adequately conceal allocation (Giuffrida 1997; Koshman 2008) or achieve adequate blinding (Koshman 2008; Parr 2009), or with key characteristics being unevenly distributed (Bainbridge 2006).
In other cases, reviews reported that included studies were of variable quality, for example, ranging from moderate to high risk of bias (eg Lewin 2010; Schedlbauer 2010), and several that included studies were of generally low quality and/or had serious methodological limitations (Lutge 2012; Nicolson 2009; Roughead 2005; Rueda 2006; Schroeder 2004), despite study inclusion being restricted to RCTs alone. Methodological quality (risk of bias) was largely unclear or not formally assessed in others (Bower 2006; Castelino 2009; Misso 2010; Russell 2006).
A similar picture of the quality of included studies emerged in those reviews including studies other than RCTs, most often quasi‐randomised controlled trials (although other study designs were also included in many of these reviews). Included studies had methodological limitations, such as failing to meet specific quality criteria (Bennett 2009; Gray 2009; Jacobson 2005; Maglione 2002; Maio 2005; Morrison 2001; Odegard 2007; Royal 2006; Van Wijk 2005; Volmink 2007; Yankova 2008). Other studies had serious methodological limitations, usually highlighted by the review authors (Aaserud 2006; Austvoll‐Dahlgren 2008; Bain‐Brickley 2011; Bayoumi 2009; Chivu 2008; Lummis 2006; Orton 2005; Wright 2006), such as inclusion of studies of poor design for assessing intervention effectiveness (eg studies without a suitable control group; eg Bayoumi 2009;Chivu 2008; De Bleser 2009; Haywood 2009; Jegu 2011; Mbuba 2008; Smith 2009).
Other reviews included studies of moderate methodological quality overall (Bhogal 2006; Gleeson 2009; Machado 2007a; Machado 2007b; Machado 2008; Polis 2007; Ranji 2008; Olthoff 2005; Stevenson 2004; Vermeire 2005), while quality was unclear or not reported in others (Al‐aqeel 2011; Amico 2006; Molife 2009; Nishtala 2008; Saini 2009; Stone 2002; Zygmunt 2002).
In both RCT‐only reviews, and reviews of RCTs plus other designs, it was relatively common that results were based on only a small number of studies (Bain‐Brickley 2011; Castelino 2009; Giuffrida 1997; Gleeson 2009; Golicki 2008; Gray 2009; Haywood 2009; Liu 2008; Nicolson 2009; Nkansah 2010; Odegard 2007; Oyo‐Ita 2008; Smith 2009), and/or samples sizes were too small to detect differences between groups (eg Bainbridge 2006; Giuffrida 1997; Halpern 2011; Haywood 2009), limiting the conclusions that could be drawn from studies and reviews. Overall, included studies were of varied methodological quality and this may in some cases predispose the results to bias. Where reviews had obvious methodological shortcomings, we attempted to adjust for this by downgrading the effectiveness statements (see Appendix 1 for evidence rating scheme).
Effect of interventions
In the following section we present the bottom‐line statements of intervention effectiveness, determined using the evidence rating scheme (see table under 'Synthesis of results and rating the evidence of effectiveness') for each review and summarised within each intervention category.
For a full list of reviews contributing to each intervention category, with definitions of the scope of interventions included within each category, see Additional Table 1.
For detailed information on intervention effects refer to Appendix 1, where the effects of interventions are presented as summaries of results from the assembled reviews in full, for transparency.
Results, reported individually for each included review (as quantitative results; a narrative summary of the results; and effectiveness statements) can be found on the Review Group's website, at https://doi.org/10.26181/19320386.v1.
Providing information or education
Providing information or education are defined as strategies to enable consumers to know about their treatment and their health. Interventions include those to educate, provide information or to promote health or treatment. Interventions can be provided to individuals or groups, in print or verbally, face to face or remotely. Interventions may be simple, such as those seeking solely to educate or provide information; or complex, such as those to promote or manage health or treatment as part of a multifaceted strategy.
Statements are based on our synthesis of results from 43 reviews (20 in original overview (4 updates) plus 23 new reviews).
Overall, interventions that provide information or education as a single component may be ineffective to improve adherence or clinical outcomes. There is insufficient evidence to determine whether these interventions, when delivered alone, reduce adverse effects, but some evidence that they may improve knowledge.
There is also some evidence that patient education and/or information as a single component or as part of a more complex intervention may be effective in improving immunisation rates.
When used in combination with other interventions, such as self‐management skills training, counselling, or as part of pharmacist‐delivered packages of care, there is some evidence that education or information may improve adherence and other outcomes such as clinical outcomes and knowledge, but results are mixed.
Facilitating communication and/or decision making
Facilitating communication and/or decision making involves strategies to involve consumers in decision making about medicines. Interventions include those that aim to help consumers make decisions about medicines use; to encourage consumers to express their beliefs, values and preferences about treatments and care; and/or to optimise communication with consumers about medicines use and related issues.
Statements are based on synthesis of results from 10 reviews (8 in original overview (1 update) plus 2 new reviews).
There is insufficient evidence from one key review to determine whether interventions focussed on promoting communication about medicines between patients and professionals are effective.
There are other interventions which aim to optimise communication but which did not focus specifically on promoting communication as such. Overall, there is some evidence to support the use of these broader interventions which do not have a specific focus on facilitating decision making and/or communication, but effects are mixed.
Delayed prescribing is effective to decrease antibiotic use, but has mixed effects on clinical outcomes, adverse events and satisfaction. In general, there is some evidence of effect from education and enhanced follow‐up, facilitators working with physicians to encourage preventive services, and pharmaceutical care services (consultation to resolve medicines problems, develop a care plan and provide follow‐up) for improving adherence and knowledge. There is insufficient evidence to support the use of psychosocial interventions, which are generally ineffective. There is insufficient evidence to determine the effectiveness of structured counselling or compliance therapy, or of group or home‐based visits to promote vaccination.
Acquiring skills and competencies
The strategies in this category focus on the acquisition of skills relevant to medicines use. These interventions aim to assist consumers to develop a broad set of competencies around medicines use and health, such as medicines management or monitoring; or training consumers in the correct use of devices to deliver treatment, or the correct use of treatments.
Statements are based on synthesis of results from 13 reviews (9 in original overview (1 update) plus 4 new reviews).
There is some evidence that strategies which focus on the acquisition of skills and competencies may improve adherence and clinical outcomes, but results are mixed.
Regarding specific types of interventions, there is sufficient evidence that people self‐managing antithrombotics (self‐testing and self‐adjusting therapy based on a predetermined dose schedule) is generally effective to decrease thromboembolic events and mortality; and some evidence that self‐management improves clinical outcomes, with mixed results. There is also insufficient evidence that self‐management decreases major haemorrhages, but because these events are rare this result most likely arises due to insufficient power to detect a clinical difference. There is sufficient evidence that self‐monitoring (self‐testing and calling clinic for the appropriate dose adjustment) of antithrombotics is generally effective to decrease major haemorrhages, and some evidence it improves clinical outcomes ‐ results are mixed. However, there is insufficient evidence that self‐monitoring decreases thromboembolic events or mortality, but again because these are rare events these results may arise because of a lack of power to detect a clinical difference. In hypertension, there is sufficient evidence that home blood pressure monitoring is generally effective to improve clinical markers for hypertension, medicines overuse and therapeutic inertia.
There is some evidence to support the provision of counselling of patients and/or physicians by pharmacists to improve adherence, but insufficient evidence to support more intensive patient care by pharmacists. There is insufficient evidence to support the provision of training by pharmacists to improve adherence, but some evidence that it improves knowledge and medicines use.
There is insufficient evidence to support the use of self‐administration programmes to improve medicines adherence, knowledge, errors or satisfaction — they are generally ineffective.
There is some evidence that patient‐controlled analgesia (PCA) increases analgesic consumption and it may decrease pain scores, although with mixed results. There is some evidence that structured PCA education is generally effective to improve knowledge, but insufficient evidence that it improves postoperative pain control.
Supporting behaviour change
This category is defined to include strategies focussing on the adoption or promotion of health behaviours and treatment behaviours, such as adherence to medicines. Included are interventions at an individual level that address behaviour change for the under‐use, overuse or misuse of medicines, and may include practical strategies to assist consumers in taking their medicines correctly such as reminder devices, pre‐packaging of multiple medicines, or different or simplified medicines formulations.
Statements are based on our synthesis of results from 53 reviews (26 in original overview (6 updates) plus 27 new reviews).
Overall, there were mixed effects of interventions to support behaviour change in relation to medicines use. There is some evidence of the effectiveness of simple interventions for short‐term treatments, and complex interventions for long‐term treatments to improve adherence and clinical outcomes.
More specifically, there is sufficient evidence that self‐monitoring or self‐management programmes improve medicines use, adherence and clinical outcomes. There is some evidence that immunisation rates are improved by each of the following: reminders, lay health worker interventions, home visits plus vaccination, free vaccination, facilitators working with physicians and financial incentives to physicians.
There is some evidence that simplified dosing regimens are generally effective in improving medicines adherence, although the optimal dosing regimen is not known. There is also some evidence that reminders, cues and/or organisers, reminder packaging and material incentives are effective to improve medicines adherence, but with mixed results.
There is some evidence that support and education, support and motivation, education and training, or information and counselling interventions, are effective to improve adherence and medicines use outcomes, although results are again mixed. There is also some evidence that quality improvement strategies with an educational component targetting patients are effective to decrease proportions of patients receiving antibiotics, with mixed results.
There is also some evidence that pharmacist‐led medicines review is generally effective to reduce medicines problems and unnecessary medicines. There is some evidence that other interventions involving pharmacists directly (such as expanded roles encompassing disease education and medicines management) are effective to improve adherence, numbers of prescribed medicines and clinical outcomes, although results are mixed.
Finally there is some evidence that computerised prescribing support can be effectively implemented and change provider behaviour, but that it appears ineffective to change patient outcomes.
Support
This category includes strategies to provide assistance and encouragement to help consumers to cope with and manage their health and related medicines use. Interventions can target patients or carers, as individuals or in groups, and may be delivered face to face or remotely.
Statements are based on our synthesis of results from 17 reviews (12 in original overview (1 update) plus 5 new reviews).
Due to the mixed results from studies found in most reviews, we can state that there is some evidence that interventions that provide support alone or in combination with other strategies may be effective to improve adherence. There is insufficient evidence to determine for which conditions support may be effective, or who should provide the support for greatest effect.
Minimising risks or harms
Strategies for minimising risks or harms have a specific focus on preventing or managing adverse events of treatment and complications of disease. Interventions can be for ongoing treatment or related to emergency or crisis events. Strategies can be to minimise risks or harms at an individual level or a population level (eg reducing antibiotic use; or augmenting immunisation uptake).
Statements are based on synthesis of results from 33 reviews (15 in original overview (2 updates) plus 18 new reviews).
There is sufficient evidence that both self‐management and self‐monitoring interventions are effective at decreasing adverse events of anticoagulant therapy, but self‐management also appears effective to decrease mortality. For hypertension, there is also sufficient evidence that home blood pressure self‐monitoring is effective, and some evidence that PCA is effective, to improve medicines use and clinical outcomes.
For diabetes there is some evidence that continuous insulin infusion in adults and children may improve medicines use and some measures of diabetes control, but it appears ineffective to reduce adverse events.
There is also some evidence that strategies to improve interactions between healthcare professionals and patients may decrease adverse events and improve other outcomes such as specific medicines problems, but results are mixed.
In particular, there is insufficient evidence to determine whether the use of patients’ own medicines (POMs) in hospital is effective; while self‐administration programmes for hospital inpatients appear ineffective to improve medicines adherence, knowledge or errors.
There is some evidence that educational strategies to minimise risks and harms may be effective, and that telling patients about adverse effects of medicines does not negatively influence adherence. There is also some evidence that computerised prescribing support interventions can be effectively implemented and change provider behaviour, but they may be ineffective to improve patient outcomes.
For immunisation uptake, there is sufficient‐to‐some evidence that (alone or in different combinations), organisational change, reminders and recall (particularly tailored reminders), financial incentives, home visits, free vaccination, education, lay health worker interventions and facilitators working with physicians are each generally effective. The effects of mass mailings are mixed. Reminders with outreach, and physician reminders alone both appear ineffective.
There is some evidence that directly observed therapy for tuberculosis (TB) or HIV is generally ineffective to improve treatment completion, adherence or clinical outcomes. There is some evidence that material incentives and lay health worker interventions improve adherence to TB treatment, with mixed results, and insufficient evidence to decide on the effects of late patient tracers. There is sufficient‐to‐some evidence that delayed antibiotic prescriptions may decrease prescribing rates and antibiotic use without increasing complications, but it may increase supplementary medicines use and results are mixed for clinical outcomes, adverse effects. Evidence is insufficient to determine the effects of delayed prescribing on antimicrobial resistance. While there is insufficient evidence to determine the effects of broader quality improvement strategies on antimicrobial resistance, adverse events, and health service use; they are generally effective at improving prescribing rates or proportions of patients using antibiotics.
Improving quality
Improving quality is a category of interventions that are defined as strategies to improve the total package, coordination or integration of care delivered. Interventions can involve substitution or expansion of one type of care, such as interventions that aim to overcome system barriers to medicines use, including access and financial barriers.
Statements are based on synthesis of results from 30 reviews (17 in original overview (2 updates) plus 13 new reviews).
As this overview did not specifically identify reviews which targeted organisational or structural interventions to change consumers' medicines use, only provisional conclusions about the effectiveness of those interventions are provided here.
There is some evidence that changing the coordination of care (eg changing roles of healthcare professionals to interact with patients or to provide additional services to patients) may improve adherence and other outcomes related to medicines use, such as total numbers prescribed, medicines appropriateness or unnecessary medicines. However, the results from most reviews, taken together, are mixed. Overall, effects on adverse events and clinical outcomes were also typically mixed with these interventions.
For depression, there appears to be some evidence that interventions aiming to improve quality are generally effective to improve adherence and symptoms; whereas for heart disease and hypertension the effects on adherence and clinical outcomes are mixed.
In older people, there appears to be some evidence that pharmacist‐delivered interventions to optimise medicines use are generally effective to improve medicines outcomes (such as appropriateness and unnecessary medicines) but there is mixed evidence for effects on adherence and insufficient evidence for other outcomes including adverse events.
When considered broadly, there is some evidence that financial interventions are effective, with mixed results; and that pharmaceutical pricing policies aimed at indirectly influencing consumers’ use of medicines are effective to improve medicines use and costs, but results are mixed for effects on health status and health service use.
There is some evidence that organisational interventions are effective at improving immunisation uptake.
There is insufficient evidence to decide whether free provision of medicines improves treatment adherence; and insufficient evidence to determine the effects of supporting patients' use of their own medicines in hospital.
Consumer system participation
There is insufficient evidence to determine the effects of consumer system participation in medicines‐related activities, because no relevant reviews were identified.
Discussion
Summary of main results
This updated overview includes 75 unique systematic reviews, an increase from 37 reviews included in the original version (Ryan 2011b). These reviews assess the effects of a range of interventions with diverse aims in relation to consumers' use of medicines, including: the promotion of informed decision making and communication related to medicines; risk minimisation; skills acquisition; education or information provision; and support for behaviour change, including support for adherence to medicines. We identified no reviews aiming to promote consumer participation in medicines‐related activities at the systems level.
Some effective interventions were simple, while others were complex.
Looking collectively across reviews, for most outcomes, medicines self‐monitoring and self‐management programmes appear generally effective to improve medicines use, adherence, adverse events and clinical outcomes; and to reduce mortality in people self‐managing antithrombotic therapy. However, a proportion of participants were unable to complete these interventions, suggesting that they may not be suitable for everyone.
Other interventions that appear promising to improve adherence and other key medicines use outcomes such as medicines problems or knowledge, but require further investigation to be more certain of their effects, include:
simplified dosing regimens: with positive effects on adherence; and
interventions directly involving pharmacists in medicines management, such as medicines reviews (with positive effects on medicines adherence and use, medicines problems and clinical outcomes) and pharmaceutical care services (consultation between pharmacist and patient to resolve medicines problems, develop a care plan and provide follow‐up; with positive effects on adherence and knowledge).
Several other strategies showed some positive effects, in particular in relation to adherence, as well as other outcomes. However, the effects of these interventions were less consistent overall, and so need further study to more clearly assess their effects and to investigate heterogeneity in effects. These included:
delayed antibiotic prescriptions: effective to decrease antibiotic use but with mixed effects on clinical outcomes, adverse effects and satisfaction.
practical strategies like reminders, cues and/or organisers, reminder packaging and material incentives: with positive, although somewhat mixed effects on adherence across studies.
education delivered together with self‐management skills training, counselling, support, training or enhanced follow‐up; information and counselling delivered together; or education/information as part of pharmacist‐delivered packages of care: with positive effects on adherence, medicines use, clinical outcomes and knowledge, although again with mixed effects in some studies; and
financial incentives: with positive, but mixed, effects on adherence.
Several strategies also showed promise in relation to the promotion of immunisation uptake, but require further study to be more certain of their effects. These included organisational interventions; reminders and recall (particularly tailored reminders); financial incentives; home visits; free vaccination; lay health worker interventions; and facilitators working with physicians to promote immunisation uptake. Education and/or information strategies also showed some positive effects on immunisation uptake, but the effects of these interventions were less consistent still and so need further assessment of effectiveness and investigation of heterogeneity.
Collectively these results indicate that there are many different potential pathways through which consumers' use of medicines could be targeted to improve outcomes like adherence. That said, no single intervention assessed by this overview was effective to improve all medicines use outcomes across all diseases, populations or settings. Even where interventions showed promise, the evidence assembled to date still often only provided part of the picture on effectiveness. For example, while simplified dosing regimens seem generally effective to improve adherence, there is not yet sufficient information available from the assembled reviews to identify an optimal dosing regimen.
In some instances, the accumulated evidence suggests that certain interventions are ineffective. For example, from the evidence assembled to date in this overview, directly observed therapy seems generally ineffective to improve treatment completion, adherence or clinical outcomes, at least for tuberculosis and HIV.
In other cases, the collected evidence suggests that interventions may have highly variable effects, for example, that they may be ineffective to improve some outcomes, but not others. An example of this is strategies that provide information or education as single interventions, which appear to be ineffective to improve adherence or clinical outcomes, and effects on adverse events and other relevant outcomes are unknown. However, these interventions may be effective to improve knowledge, which is an important outcome for consumers in relation to informed medicines use and choices.
For many other interventions there is still insufficient evidence to determine how effective or ineffective they might be to change medicines use outcomes with any degree of certainty.
Overall completeness and applicability of evidence
Assembling and assessing the review‐level evidence on consumer's medicines use across diseases and settings has identified major intervention, outcome and population gaps in the research that should be addressed as priorities.
Interventions and outcomes
Although this updated overview includes 75 reviews of interventions, there were relatively few strategies for which there was sufficient evidence to make conclusive statements about effects on medicines use. Even for categories with proportionately more reviews, there was often not necessarily sufficient evidence to draw strong conclusions. It is clear, however, that strategies to improve medicines use has focussed on educating consumers and supporting and changing those behaviours of consumers most practically related to taking their medicines, for example, providing reminders to patients or information pamphlets about how to take medicines. There were proportionately fewer reviews on facilitating communication and decision making, acquiring skills, and minimising risks or harms, and, notably, no reviews addressing the effectiveness of strategies to increase consumer participation at a system level for better medicines use. The focus of existing research on education and changing practical behaviours is in contrast to emerging research suggesting that there are numerous other factors that determine how and why people take medicines, including consumer‐oriented aspects of medicines use such as promotion of informed decision‐making, support and self‐management (Britten 2004; Brown 2012; Coulter 2006; Munro 2007; Pound 2005; Ratanawongsa 2013; Soumerai 2006; Townsend 2003) or consideration of the alignment between consumer priorities and the aims of interventions (Candy 2011; Candy 2013).
Adherence
The other major focus of the included reviews was on adherence. There was often insufficient evidence to draw any conclusions about the effects of interventions on consumer wellbeing and health status, or effects on a system level. The relatively narrow range of outcomes reported reflects the included reviews' primary focus on medicines adherence, and even where reviews did not focus solely on promoting adherence there was often only a limited range of outcomes reported. It is not clear whether reviews and their included studies are selectively reporting adherence as a primary outcome. There may be a few reasons for this lack of reporting: a general lack of awareness of review authors or study authors of the complexity of factors likely to affect adherence and medicines use (relating to reporting of relevant outcomes by included studies and/or reviews); or a lack of awareness of the many factors that can affect consumers' healthcare behaviours more generally.
Other outcomes including adverse events
It appears that many reviews, and probably the research on medicines use on which reviews are based, are still centred around adherence, which is undoubtedly an essential component of prescribing and medicine taking. However, other outcomes such as safe use or risk minimisation, informed decision making or overall satisfaction with medicines use and effects, are arguably as important as adherence but seem to be regarded as less so, or may be used as surrogates for adherence. Few reviews reported on possible adverse events related to the use of interventions specifically, or related to better adherence or to changes in medicines use. This may be due to the lack of adverse event reporting in primary research, which was highlighted as an issue by some reviews; nonetheless before implementing strategies to improve adherence or to modify medicines use the potential harms of those strategies should be adequately evaluated in both trials and in systematic reviews of trials, as recently suggested by another review of reviews (Zorzela 2014). Monitoring for harms associated with interventions should also be performed once interventions are implemented, to provide a more complete picture of the effects of interventions. Information on costs associated with interventions was poorly reported, and full cost effectiveness analyses were largely missing from the included reviews. This too represents a major gap in reporting which needs to be addressed by future trials and reviews.
Many reviews did not report outcomes which seem intuitive and important for understanding consumers' medicines use. For example, reviews of educational and informational interventions did not always report outcomes such as knowledge, understanding or recall of information; while reviews of more behaviourally‐based interventions, such as reminder packaging aids, did not always assess participants' skill level to use packaging, or to correctly fill aids, also as documented by other authors (Topinkova 2012). The few cases where such factors were considered indicate that considering such factors is important: for example, Garcia‐Alamino 2010 showed that although self‐monitoring and self‐management of anticoagulant therapy had positive effects on adverse events and clinical outcomes, fully 25% of people assigned to these interventions dropped out, and trial participation was very low (68% overall refusing participation) in the first place. Such results suggest that key 'medicines' outcomes cannot and should not be considered in isolation from other factors that may critically determine the overall success or failure of the intervention strategy.
In this overview, however, most reviews tended to focus on endpoint outcomes such as behaviour change (often adherence) or treatment (clinical) outcomes, which limits inferences about how and why interventions aimed at consumers may or may not be effective. Concentrating on a narrow range of outcomes may even lead to incomplete or misleading conclusions about the effects of particular interventions. For example strategies providing information or education as single interventions appear ineffective to change adherence, but do seem to improve knowledge. In the interests of informed decision making about medicines these strategies therefore clearly have merit ‐ directly related to the aims of the intervention ‐ but are also not suited to addressing all of the challenges of poor medicines adherence in isolation. Identifying which outcomes are relevant and then setting out to assess a broad range of relevant outcomes should therefore be a priority for future research in this area, and should be guided by the direct and indirect aims of interventions under assessment.
Interventions
Included interventions ranged from the very simple (such as a medicines chart or postcard or telephone reminder) to the very complex (eg self‐monitoring or self‐management, with and without medicines adjustment; complex interventions incorporating medicines review to reduce adverse events; problem solving or self‐administration skills training; alone or in combination with other interventions). To help deal with the varying complexity of included interventions, we categorised included reviews according to the intervention taxonomy and mapped reviews to intervention categories based on the underlying aim(s) of the interventions the review included.
The intervention taxonomy developed alongside this overview represents a conceptual framework for organising the evidence (Lowe 2010; Ryan 2010). It provides a broad definition of consumers' medicines use that extends beyond adherence to envisage a more complex and interactive role for consumers in relation to decision making and management of medicines. We hope that this overview, and the taxonomic structures developed alongside it, may encourage other researchers to consider and report a wider range of outcomes than those typically captured in existing research on consumers' medicines use to date.
Other research has highlighted areas in which research findings are inconsistent. Mixed findings may arise where interventions differ in their design, or where participants are drawn from different populations. A recent analysis of systematic review evidence on adherence to medicines has suggested that effective interventions were more likely to include components aligning with issues identified as important to patients than those interventions that did not significantly improve adherence (Candy 2011). More recently these authors reported that, again relating to interventions to improve medicines adherence, there is generally poor agreement between patients' ideas about what is important and what is actually incorporated into such interventions. The authors of this study suggested that mixed findings from different studies may be explained by individual patients responding more or less well to different strategies for promoting adherence (Candy 2013). Consideration of consumers' views and priorities therefore seems integral to understanding how such complex interventions related to medicines use may work, and can usefully inform the future development of interventions for evaluation.
One limitation of this current overview is that it did not have a primary focus on assessing the evidence on strategies provided at a system level, such as changing the role of pharmacists or financial structures, that may indirectly influence consumers' medicines use. This overview did include some evidence about such 'indirect' to consumer interventions, and some conclusions about their effects have been drawn because many reviews which took a broad approach to medicines use in a particular clinical area often included such interventions at a system level. However, we cannot draw strong conclusions about these interventions.
Populations
Although this update more than doubled the number of reviews included in this overview, we identified several significant gaps in the populations assessed. Many reviews included cross‐disease populations, and there was a large spread of acute and chronic conditions represented, as well as interventions specifically addressing immunisation uptake, contraceptive use, post‐surgical pain relief and medicines for infectious diseases.
However, there are also gaps in the evidence for a several key populations. In the original version of this overview (Ryan 2011b) we highlighted the small number of reviews considering children and adolescents, as well as parents and other carers. This update added more than twice the number of reviews included in the original overview, yet the proportion of those considering medicines use in children and/or adolescents increased only slightly (from 38% to 41%), while the proportion of reviews involving parents and/or other carers actually fell slightly (from 27% to 25%). There has been more recognition in the consumer health literature of carers' issues, which may eventually lead to more reviews in this area. There remains, for now, insufficient evidence to draw conclusions about the effects of interventions targetting carers with respect to medicines use.
Another major gap in the review literature relates to polypharmacy; in particular, what are the effects of interventions for people taking medicines for more than one concurrent health problem (multimorbidity)? This gap is likely to arise for several reasons, including that people with more than one co‐existing condition are often directly excluded from trials; and even where they are not directly excluded, information about comorbid conditions often fails to be adequately reported or implications considered (Boyd 2005; Trumble 2006). While a review published after our search date in 2012 (Smith 2012) goes some way towards addressing this gap, its focus was broader than consumers' medicines use interventions and would not have been eligible for inclusion in this review on this basis.
As we found in the original version of this overview, most reviews did not provide information directly relevant to people requiring polypharmacy, and/or those with comorbid conditions, even though these people are particularly prone to poor outcomes, including those associated specifically with medicines use (eg higher rates of adverse events, poor adherence, prescription or dispensing of contraindicated medicines, lack of adequate medicines review). Some of the included reviews did report selected details relating to polypharmacy and/or multimorbidity, but this was highly varied. For example, a small number of reviews (11%) did explicitly seek and report information on comorbid health problems and/or polypharmacy, although only a minority of studies within each of these reviews actually addressed these issues, so limiting the information available or conclusions that could be drawn. In several other cases, reviews did consider multimorbidity or polypharmacy on some level but this was often as incidentally as simply not explicitly excluding this population, with little or no further consideration given in the review; or explicitly allowing multimorbid or polypharmacy populations to be included, but exploring this to very different degrees by the reviews themselves. Most often, there was little or no exploration of the issues in reviews apart from those affecting very old and/or frail populations identified as high‐risk populations (eg polypharmacy in elderly patients).
Rising chronic disease rates internationally means that multimorbidity rates are also rising, particularly among younger populations (Fortin 2005; Fortin 2007; Smith 2012; Starfield 2003). Multimorbidity is associated with substantially poorer outcomes than those of others in the community, including higher rates of medicines use and adverse events (Boyd 2005; Fortin 2005; Mishra 2011; Smith 2012). Research is needed as a priority to develop an evidence base applicable to people with more than one concurrent condition, and specifically on medicines use in these populations, in order to improve health and other outcomes (Ryan 2011c; Ryan 2013). For example, recent studies have reported that people with multimorbidity may be taking multiple medicines, from multiple prescribers, without sharing of this information between either prescribers or the patient (Mishra 2011; Ryan 2013). Systematic reviews could usefully contribute to this area by reporting data on co‐occurring conditions wherever they are available from primary research and reporting the absence of data as a gap where they are not (May 2009; Ryan 2009c).
Quality of the evidence
The quality of the reviews and of included studies within this overview varied. We excluded reviews rated as low quality using the AMSTAR tool (Shea 2007). While almost all (96%) Cochrane reviews were rated as high quality, only 15% of DARE reviews received a similar rating. Only 3 reviews (all of them Cochrane reviews) met all 11 AMSTAR criteria adequately (Bhogal 2006; Garcia‐Alamino 2010; Lutge 2012). This suggests that the majority of the reviews included in this overview have limitations in design, conduct and/or reporting that may influence the results when considered both individually and collectively.
Similarly, at the study level, methodological quality ranged from studies that were well designed and conducted to those with serious methodological limitations. Around half (43%) of included reviews included only RCTs. While this ensured rigorous design for assessing intervention effectiveness, it did not guarantee that the included studies were of high quality. In fact almost all reviews of RCTs reported methodological limitations in included trials, even in the small number of reviews that were highly restrictive about study inclusion based on rigorous methodological design and quality (eg Haynes 2008; Mahtani 2011).
The other half of reviews in this overview included studies of other designs, most commonly quasi‐randomised trials, but sometimes also designs such as controlled before‐and‐after studies. These reviews, too, noted that included studies generally had methodological limitations.
We have reflected limitations in the quality of the evidence by interpreting the results and formulating the statements of intervention effectiveness in light of the quality of included studies. However, methodological limitations at both the included study and review levels mean that the results of this overview should be interpreted with caution, as there is the possibility of bias arising from different sources within and across reviews.
Potential biases in the overview process
This overview developed and adopted rigorous methods with the aim of reducing the impact of bias contributed by the overview process itself.
A major strength of this overview, compared with previous overviews by others in the area, is the comprehensiveness of our searches. We used handsearching, performed by two researchers working independently, to identify all reviews potentially relevant to consumers' use of medicines. Since the research evidence on interventions directed to consumers is typically not well indexed, database searches do not reliably identify all relevant reviews. We believe that handsearching is therefore essential to ensure identification of a comprehensive set of reviews in this area.
We selected reviews for inclusion in this overview based on relevance. The dataset we have presented is, therefore, only a selection of the total available data. However, we developed and piloted criteria to enable us to select reviews for inclusion in a consistent manner, based on their focus and content; we systematically assessed the quality of reviews using an established and validated tool (Shea 2007); and all review selection and ranking steps were performed by two researchers to maximise consistency of judgement.
A strength of this overview is that we developed an evidence rating scheme to enable consistent judgements to be made and statements formulated about the effects of interventions, across diseases, populations and settings.
We also sought to reduce double counting of the evidence, by excluding from this overview non‐Cochrane reviews which overlapped in focus with included Cochrane reviews. However, some individual studies have contributed evidence to multiple included reviews, and this remains a limitation.
Agreements and disagreements with other studies or reviews
This overview was, to our knowledge, the first synthesis of reviews to take a broad perspective on evidence‐based prescribing and medicines use; broader than adherence, but focussed on consumers' medicines use. In the period since the overview was first published (Ryan 2011b) we are not aware of any other emerging pieces of research with a comparable scope or aim. To our knowledge the overview by Van Dulmen 2007, which focussed on adherence to medical treatments, including appointment keeping, and dietary and exercise recommendations, remains the most comparable piece of research on review‐level evidence in this area. In contrast to Van Dulmen, our overview and its update excluded duplicative reviews and took a more inclusive approach to medicines use interventions. Despite the differences in inclusion and exclusion criteria, both overviews found some evidence for the effectiveness of interventions to improve adherence primarily for supporting behaviour change, such as simplified dosing regimens and reminders. However, the effects of such interventions on other outcomes were not addressed in Van Dulmen's overview. Our overview is also more current: even in the original version of this overview we identified and included several additional Cochrane and DARE reviews focusing on adherence that would likely have fitted the scope of the Van Dulmen review. With this update that number is much increased.
The World Health Organization (WHO) (Chetley 2007) has produced the manual How to improve the use of medicines by consumers which emphasises planning a strategy after determining the reasons for irrational medicines use, using social marketing. In this overview, there were no reviews assessing this process for improving medicines use ‐ which in itself is a strategy. The key messages, however, are similar to this overview. The focus is on empowerment at both an individual and system level, and includes issues such as self‐medication and self‐management, safe use and misuse. The other focus of the WHO review is on communication as a principal tool by which other strategies are implemented at an individual or system level. Strategies that are used in combination with other strategies, such as by providing information and supporting behaviour change, are promoted as being more effective than single strategies.
The more recent WHO document The World Medicines Situation 2011 (Holloway 2011), on improving rational use of medicines internationally, focusses on improving adherence to treatments prescribed and dispensed. This report includes consideration of interventions targeted at providers to promote better adherence to guidelines, which is beyond the scope of this overview. It also acknowledges the difficulty of improving consumers' adherence to medicines and highlights some promising interventions to improve the use of medicines, such as multifaceted interventions, those including provider and consumer education together with supervision, and strategies such as self‐monitoring. These results, while not directly comparable with those of this overview, are consistent with the findings were have presented.
The UK's National Institute for Health and Clinical Excellence (NICE) also has relevant and up‐to‐date guidance for medicines adherence (NICE 2009). The overarching principles for adherence to medicines in its guidance are patient involvement in decision making, and supporting adherence. Considered further, this includes an emphasis on improving provider‐consumer communication about medicines; involving patients actively in decisions; understanding consumers' knowledge, beliefs and concerns about medicines; providing information; supporting adherence; reviewing medicines; and ensuring good communication between healthcare professionals involved in the consumer's care and prescribing. Interventions targeted at both professionals and patients were included in the NICE review, in contrast to our overview which has focussed on consumer interventions. In addition, reviews and trials not specific to medicines use were also included in the NICE review. For this reason, it is difficult to compare findings. However, the evidence and the recommendations are similar to the underlying concept in this overview, in that the goal of an intervention for consumers is not simply adherence to any medicines prescribed by a physician.
Authors' conclusions
Implications for practice.
This overview presents current evidence from 75 unique reviews that have synthesised trials and other studies evaluating the effects of interventions to improve consumers' medicines use. Information on a wide range of outcomes was sought. The most commonly measured and reported outcome was adherence, but many other outcomes have been reported and help to inform choices.
Decision makers who are faced with implementing interventions to improve consumers' use of medicines can use the results of this overview to inform decisions about which interventions may be most promising to improve particular outcomes. Additionally, the intervention taxonomy may assist people to identify the full range of strategies available in relation to specific purposes, for example, gaining skills or being involved in decision making about medicines.
Implications for research.
Despite the large and growing body of evidence assembled in this updated overview, many areas of uncertainty remain, and many interventions on consumers' medicines use still need rigorous assessment. Gaps in the medicines intervention and outcome taxonomies, and the evidence accumulated within both, indicate a clear need for further high‐quality research. Researchers and funders can use this overview to identify where more research is needed and assess its priority. The limitations of the available literature due to the lack of evidence for important outcomes related to medicines use and for important populations, such as people with multimorbidity, should also be considered in policy and practice decisions.
In general terms, outcomes could be better reported in future research on consumers' medicines use and should be guided by the direct and indirect aims of the interventions under investigation, as well as by the medicines outcome taxonomy. Several populations deserve particular attention in research, including children and young people, carers and those with multiple co‐existent conditions. Further research is also needed on a range of additional interventions to improve safe and effective medicines use by and for consumers. These might include studies of training interventions to improve the recognition of harms or adverse events; those to enhance problem solving or medicines management; interventions to address individual barriers to adherence, such an targeted counselling; those to promote better communication about medicines and involvement in decisions by consumers; or others from among the range of interventions described by the taxonomy. The intervention taxonomy focusses on the aim of the intervention (eg supporting behaviour change) rather than the type of intervention (eg reminders). This change in perspective could also be used to focus systematic reviews and objectives of individual studies in the future.
What's new
| Date | Event | Description |
|---|---|---|
| 6 May 2022 | Amended | Updated weblinks to additional tables |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 5, 2011
| Date | Event | Description |
|---|---|---|
| 8 February 2018 | Amended | Updated web link to additional data tables. |
| 25 March 2014 | New citation required but conclusions have not changed | We updated the overview last published on issue 5 2011 of The Cochrane Library. Authorship has been amended. Title has been changed to better reflect the subject of the overview. Large tables (Characteristics of included studies; Characteristics of excluded studies; and Table of results) have been removed from RevMan due to problems with display and are now located on the Cochrane Consumers and Communication Review Group's website at http://cccrg.cochrane.org/consumers‐clinicians‐and‐policymakers. |
| 15 July 2013 | New search has been performed | Searches, methods, results and conclusions updated to incorporate eligible reviews (n = 38 new reviews plus n = 6 updated reviews) published up to March 2012 (inclusive). |
| 13 December 2011 | Amended | Due to continuing problems with display of this overview in PDF format, we have now split the Characteristics of Included Studies, and Results by Individual Review, into 5 tables each (Parts A to E). |
| 21 September 2011 | Amended | We split each of the large tables on Characteristics of included studies, and Results by individual review, into three parts, to improve their presentation. |
Notes
The protocol for this overview was originally published in the standard format of a Cochrane review protocol, as Ryan 2008. On issue 2 2009 of The Cochrane Library the Cochrane Consumers and Communication Review Group withdrew the above protocol and republished it in 'overview' format with the citation Ryan 2009. The contents of the protocol were unchanged.
Acknowledgements
The Canadian Agency for Drugs and Technologies in Health (CADTH) contracted the Cochrane Effective Practice and Organisation of Care (EPOC) Group and the Cochrane Consumers and Communication Review Group to summarise the evidence on interventions for healthcare professionals and healthcare consumers in relation to evidence‐based prescribing. This overview presents results from part of the project that focusses on interventions targeted to consumers.
We thank the Cochrane Consumers and Communication Review Group Managing Editor Dr. Megan Prictor, and Editor Prof. Sandy Oliver for their assistance with this review.
Appendices
Appendix 1. Results of reviews ‐ Summary of effects of interventions
The effects of interventions are presented below by intervention category, based on the aims of the interventions and our taxonomy's organisation. Many reviews evaluated interventions which fall into multiple categories and so contributed evidence to determining the effects of different interventions.
Additional tables of results are located at http://cccrg.cochrane.org/our-reviews: these present the results of each review individually as: quantitative results; a narrative summary of the results; and effectiveness statements.
Providing information or education
Several reviews evaluated interventions to enable people to know about their treatments and/or health, by providing information or by educating consumers about medicines: 23 new reviews (Al‐aqeel 2011; Bain‐Brickley 2011; Bennett 2009; Buckley 2010; Chivu 2008; De Bleser 2009; Gleeson 2009; Gray 2009; Haywood 2009; Holland 2008; Liu 2008; Machado 2007a; Machado 2007b; Machado 2008; Mbuba 2008; Odegard 2007; Oyo‐Ita 2008; Parr 2009; Ranji 2008; Smith 2009; Thomas 2010; Wright 2006; Yankova 2008) and 4 updated reviews (Halpern 2011; Lewin 2010; Nkansah 2010; Schedlbauer 2010) have been added in this update, bringing the total to 43 reviews in this category.
Relatively few of these reviews separated out patient information or education interventions, as many interventions were multi‐faceted and included an information or education component. Most reviews also did not pool results over studies but instead vote‐counted positive and negative results across studies.
Information or education as single interventions
Most reviews examining education or information alone showed little or no difference in adherence or in clinical outcomes: 1 of 2 studies improved adherence in the review by Schedlbauer 2010; 1 of 6 studies in Schroeder 2004; 1 of 4 studies in Vergouwen 2003; 3 of 8 studies in Vermeire 2005; and 0 of 1 studies in Gleeson 2009 for both adherence and persistence. In single studies, patient education improved knowledge but did not improve adherence, however adherence was improved by parent education (Al‐aqeel 2011). In the review by Mbuba 2008, patient education, alone or including information pamphlets, improved patient default rates, knowledge, and side effects (1 study); but not seizure frequency (1 study) or adherence (2 studies). A review on written medicines information (Nicolson 2009) also found adherence to medicines instructions improved in only a minority of studies (2 of 6 studies), although half of studies showed improvements in knowledge (6 of 12 studies) and recall of side effects (3 of 6 interventions).
Another review on patient‐based cancer pain management education (Bennett 2009) reported improvements in key outcomes in the minority of studies: adherence (1 of 3 studies), knowledge and attitudes to cancer pain and analgesia (7 of 17 studies), but several clinical measures of pain intensity were significantly lowered. Another review (Yankova 2008) reported improved knowledge (4 studies) with structured patient‐controlled analgesia education, but pain control was significantly improved in only a minority of studies (1 of 5 studies).
A review of 39 studies (Zygmunt 2002) found that psycho‐education interventions (including dissemination of knowledge about disease, treatment and medicines) delivered in different ways were ineffective when compared with usual care. However, a review (Vermeire 2005) of education interventions for people with type II diabetes did show an improvement in glycosylated haemoglobin levels (an indicator of long‐term glucose control), although the review authors questioned the clinical importance of this improvement because it was small in size. Patient education and information also resulted in increased immunisation rates, in 3 of 5 studies of mass mailings (Maglione 2002), and an odds ratio (OR) of 1.29 (95% confidence Interval (CI) 1.14 to 1.45) from 22 studies (Stone 2002). Few reviews reported other outcomes.
Information or education as components of more complex interventions
In reviews which included interventions with an information and education component, results were mixed. In a large review of many interventions across health conditions, fewer than half of the studies (41 of 93 interventions) improved adherence, or clinical outcomes (29 of 93 interventions) (Haynes 2008). In a review of complex interventions in older adults, about half of the studies (20 of 41) improved adherence (Russell 2006). A minority of studies in some reviews improved adherence: 8 of 18 studies for hypertension (Schroeder 2004); 1 of 6 studies with a focus on counselling and education for contraceptive use (Halpern 2011); and none of 2 studies of self‐management education in sickle cell disease (Haywood 2009). This is in contrast to a review in which education combined with self‐management skills training for antiretroviral therapy improved adherence in the majority (6 of 8) of studies (Rueda 2006), and a meta‐analysis of 26 interventions including an education component that showed a small improvement in adherence to antiretroviral therapy (standardised mean increase (standardised MI) = 0.35 (95% CI 0.20 to 0.51)) (Amico 2006).
Lewin 2010 also showed improved immunisation rates in four studies with lay health workers providing interventions which included education (absolute risk increase, ARI, of meta‐analysis of 4 studies, 11 more people out of 100 (95% CI 4 to 18 more). Similarly in Oyo‐Ita 2008, single studies of each of information campaigns or different forms of education (facility‐based or evidence‐based discussion with community groups) improved immunisation uptake. The review by Thomas 2010, looking at influenza vaccination in elderly people, also reported improved immunisation demand with education plus an offer of vaccination (absolute risk increase (ARI) of meta‐analysis of 2 studies, 16 more immunisations out of 100 (95% CI 7 to 27 more)), and in single studies, with education by nurses plus vaccinated patients, and with reminder telephone calls delivered with an educational brochure.
A single study in Olthoff 2005 reported improved adherence with education and training for glaucoma; while in Gray 2009 education with personalised care planning for ocular hypertension and glaucoma improved adherence problems (1 study) and adherence in only half (1 of 2) of studies.
Education and psychosocial therapy for epilepsy improved adherence, but not seizure frequency in a single study in Al‐aqeel 2011. Similarly, in the review by Gleeson 2009, patient education and medicines barriers counselling improved adherence (2 studies) but not persistence (1 study), while patient plus provider education, and feedback on response to therapy plus patient education and/or medicines barriers counselling interventions each, in single studies, found no effects on adherence and persistence. Home based‐education plus support had mixed effects on adherence, and none on clinical outcomes, in a single study (Bain‐Brickley 2011); while in single studies in the review by Liu 2008, health education combined with home visit (late patient tracer) interventions improved tuberculosis (TB) treatment non‐completion and interruption, and clinical outcomes but not death. The review by Lewin 2010 also assessed TB treatment adherence and outcomes, reporting increased cure rates for new and re‐treated smear‐positive patients with lay health worker interventions (meta‐analysis of 4 studies, ARI 13 more people out of 100 (95% CI 4 to 18 more), while other treatment outcomes (smear‐positive cure rates, combined cure and completion, completion of preventive therapy) improved in only a minority of studies or not at all.
In a review including before‐and‐after assessments (Smith 2009), education improved patient knowledge of appropriate antimalarial (AM) use (2 studies), and in single studies, appropriate treatment but not appropriate dose. Education/training plus pre‐packaged AM significantly increased appropriate AM treatment (1 study) and adherence in half (1 of 2) of studies. Training/education for informal providers significantly increased appropriate AM and dose prescribed (2 studies). In a single study, training plus community education significantly increased appropriate AM treatment, adherence and knowledge of correct dose.
In addition, in a review by Stevenson 2004 single studies of interventions combining education and communication training, counselling or tailoring of medicines found improved knowledge and adherence, but not clinical outcomes. In contrast, a minority of studies in a review of self‐administration medicines programmes incorporating information and education with reminders and other interventions such as counselling (Wright 2006), showed improved knowledge (6 of 16 studies) and adherence (4 of 12 studies) in a minority of studies, with mixed effects on medicines errors. A review of studies including before‐and‐after assessments of interventions with information provision via different formats and in combination with other interventions such as counselling, provision of folic acid and reminders, showed improved knowledge, awareness and consumption of folic acid in the majority of studies (Chivu 2008). In Parr 2009, brief interventions recommending benzodiazepine dose reduction, with or without self‐help information, improved cessation of benzodiazepine use in the majority of studies (4 of 5 studies).
Education or information interventions (combined with behavioural or affective components) to promote adherence to medicines post organ transplantation (De Bleser 2009) improved knowledge in single studies, but adherence inconsistently; whereas combined patient informational and behavioural interventions improved adherence and target immunosuppressant blood levels (2 studies).
Education and/or counselling delivered by pharmacists, often as part of a more comprehensive package of care, similarly showed mixed results for adherence and clinical outcomes. Adherence to chronic medicines for different diseases improved in a minority of studies (6 of 17) with community pharmacists (Van Wijk 2005), but effects were mixed in populations with heart failure alone (Koshman 2008), and tailored education with or without pharmacist medicines review did not significantly change adherence or barriers to adherence in diabetes (1 study) (Odegard 2007). Three further reviews (Machado 2007a; Machado 2007b; Machado 2008) involving pharmacists in hospital and community settings providing disease education and medicines management interventions (for hypertension, diabetes and hyperlipidaemia) reported mixed effects: all three reported improved adherence in only the minority of studies or not at all, and had variable effects on clinical outcomes and on knowledge of medicines and health. In contrast, adherence improved in a majority of studies (4 of 6) involving both community and hospital pharmacists to convey information, educate or provide specific advice for any people requiring pharmacist assistance (Morrison 2001).
In Nkansah 2010, looking at the effects of outpatient pharmacists, studies including a primarily educational intervention for patients showed improvement in clinical outcomes (6 of 8 studies) such as blood glucose levels and quality of life (1 study). The remainder of studies, assessing the effects of complex outpatient pharmacist interventions with a patient education component, showed changes in medicines use, such as significantly reduced total numbers of medicines prescribed (3 studies), while adverse medicines reactions were non‐significantly changed (1 study), and other effects on medicines use were mixed and dependent on medicines class. Complex intervention with an educational component generally improved clinical outcomes, such as lower glycated haemoglobin (HbA1c) ( 3 of 5 studies) and systolic (4 of 7 studies) and diastolic (6 of 7 studies) blood pressure, improved mortality in half of studies (1 of 2 studies) and quality of life in a minority of studies (3 of 9 studies).
In comparison, in Holland 2008, which assessed the effects of pharmacists in hospital, clinic and community settings, those studies with a major educational component found a decrease in numbers of medicines (1 study) but no effects on mortality (3 studies) and mixed effects on hospitalisation.
Service organisation interventions including doctor, nurse or pharmacist delivery of complex packages of secondary prevention for heart disease, incorporating patient education, had mixed effects on clinical outcomes such as blood pressure and no effects on medicines prescribing (Buckley 2010).
In a review of interventions to reduce unnecessary antibiotic prescribing (Ranji 2008), patient education, with or without clinician education; alone or as part of community‐based and non‐community based interventions, reduced prescriptions and/or proportion of patients receiving antibiotics, to varying degrees, but did not change service use.
Facilitating communication and/or decision making
Relatively few reviews considered interventions to facilitate communication or decision making for medicines use. Two new reviews (Ranji 2008; Thomas 2010) and one update (Halpern 2011) were added in this update, bringing the total to 10 reviews in this category.
Among the reviews in this category, few focussed specifically on improving communication skills and/or decision making about medicines. Therefore this section reports the results from one key review, however noting that this review included several before‐and‐after studies.
Stevenson 2004 assessed interventions promoting communication between patients and healthcare professionals. The review divided studies into three groups according to whether the intervention was designed to improve communication between patients and doctors, patients and pharmacists, or patients and nurses or medical assistants.
Doctor‐patient communication (5 studies): There were four studies in communication skills training. One study targeted patients and compared it to medicines education and found it improved medicines knowledge, question asking, and question asking skill but not clinical outcomes. Three studies targeted doctors in which physician communication outcomes, such as addressing patient fears (1 study of 1) and asking patients to repeat instructions (2 of 3 studies) significantly increased, and patient medical recall was increased (1 study of 1). In another study, fact sheets with counselling by doctors increased patient medicines knowledge compared to fact sheets alone.
Pharmacist‐patient communication (6 studies): One study evaluated communication skills training targeted to pharmacists and found patients were more satisfied with pharmacist time and answering their questions. One study evaluated a mass media campaign targeting patients in which the number of questions asked did not increase, but information was more tailored by pharmacists. Written prompts used by patients in one study did not increase questions asked. Prompts to patients to write questions for pharmacists did increase questions asked, but not adherence or patient recall. Three studies changed pharmacist visits (clinic or home) which improved satisfaction and, in single studies, decreased medicines problems and costs, but effects were mixed for adherence and clinical outcomes.
Nurses or medical assistants‐patient communication (5 studies): Three studies assessed provision of face‐to‐face patient education/counselling, with single studies reporting significantly increased adherence and increased discussions with doctors about medicines, but no change to barriers to adherence. Two studies evaluated telephone contact to discuss medical problems: one study found no difference in reporting of adverse effects or in adherence; the other study found patients discussed more issues on the call and found the calls useful.
There were also other reviews which included numerous strategies that may have promoted communication and decision making about medicines. An overview of results from these reviews is as follows.
Cross‐disease reviews of interventions without a specific focus on communication and/or facilitating decision making reported mixed effects for various outcomes. Similar to Stevenson 2004, Roughead 2005 evaluated studies which changed the interactions between pharmacists and patients, and most studies improved knowledge (4 of 6 studies) and medicines use (6 of 9 studies), but only a minority of studies improved adherence (2 of 8 studies). In addition, a large review of 93 interventions aiming specifically to improve adherence (Haynes 2008) reported mixed effects on both adherence and clinical outcomes.
Disease‐specific reviews, where interventions included a communication or decision‐making support component, were largely inconclusive. Reviews on compliance therapy in schizophrenia (McIntosh 2006) and written action plans for asthma in children (Bhogal 2006) showed no significant or consistent effects on adherence or clinical outcomes. In other reviews, adherence was improved in only a minority of studies using structured counselling for contraceptive use (Halpern 2011), or in single or multimodal psychosocial interventions in schizophrenia (Zygmunt 2002).
Delaying antibiotic prescriptions (leaving the decision to initiate therapy up to patients) reduced antibiotic use, but also significantly reduced patient satisfaction. Delaying prescriptions also resulted in unchanged or significantly worse clinical outcomes, and mixed adverse effects (Spurling 2007). A second review of quality improvement interventions to reduce unnecessary antibiotic prescribing (Ranji 2008) included several studies of delayed prescriptions and reported similar results: fewer patients filling antibiotic prescriptions (6 studies) and lower mean number of antibiotic prescriptions (1 study), again with mixed adverse effects (1 study). However, this review found satisfaction was lower with delayed antibiotics only in the minority (1 of 4 studies).
A range of interventions to promote influenza vaccine uptake in older adults was assessed (Thomas 2010), some of which included a communication and/or decision‐making component. Group (1 study) or home (2 studies) visits plus the offer to vaccinate, and home visits with vaccination encouragement and development of a care plan (1 study) all significantly increased immunisation rates. Facilitators working with physicians to encourage the use of preventive measures like influenza vaccination also significantly increased immunisation rates in most studies (2 of 3 studies).
Acquiring skills and competencies
A number of reviews focussed on interventions to train or assist consumers to develop skills around medicines monitoring, management and/or use: 4 new reviews (Argarwal 2011; Bainbridge 2006; Wright 2006; Yankova 2008) and 1 updated review (Garcia‐Alamino 2010) have been added in this update, bringing the total to 13 in this category. Most of the reviews in this category showed mixed results for adherence and clinical outcomes, but there was also a number of promising results.
A review of highly active antiretroviral therapy showed improved adherence, improvement in most studies (6 studies of 8) on medicines management skills, and mixed effects on clinical outcomes (Rueda 2006). Another review of antiretroviral therapy (Amico 2006) found a small effect from a meta‐analysis of 26 interventions to improve adherence (SMD 0.35 (95% CI 0.20 to 0.51)). In this review, high intensity interventions (eg self‐management skills training) were no more effective than low intensity interventions (eg education). In older adults (Russell 2006), self‐management of medicines also improved adherence (2 studies of 2). In a review comparing home and clinic monitoring of blood pressure, clinical outcomes (blood pressure, 22 studies), therapeutic inertia (defined as no change in medicines use, 15 studies) and medicines overuse (9 studies) were improved with home monitoring (Argarwal 2011). In contrast, in a review of 22 studies where pharmacists provided care in medicines use and management, few studies (2 studies of 8) improved adherence and there were mixed results for clinical outcomes in 16 studies (Roughead 2005). Similarly, Wright 2006 found that for hospital inpatients, medicines self‐administration programmes improved adherence in only a minority of studies (4 of 12 studies). Morrison 2001 found interventions provided by pharmacists improved adherence in most studies (5 studies of 7), but improved clinical outcomes in only a minority (1 study of 5). However, counselling of patients and physicians together improved both adherence and clinical outcomes in half of studies (2 studies of 4). There were also mixed improvements in clinical outcomes in a diabetes education programme, with non‐significant decreases in glycosylated haemoglobin (4 studies of 4), and mixed results for other clinical outcomes (Vermeire 2005).
A review of self‐management and self‐monitoring for oral anticoagulation therapy (Garcia‐Alamino 2010) found generally positive effects on clinical outcomes and adverse effects. With self‐management interventions (self‐testing and self‐adjusting therapy based on a predetermined dose schedule) mortality and risk of adverse events such as thromboembolic events significantly decreased (absolute risk reduction (ARR) of 2 fewer people out of 100 from meta‐analysis of 12 studies (95% CI 3 to 1 fewer), but major hemorrhages were not improved and clinical outcomes (International normalized ratio (INR) within range) improved in half (5 of 10) of studies. Conversely, with self‐monitoring interventions (self‐testing and calling clinic for the appropriate dose adjustment) mortality and risk of thromboembolic events decreased, although not significantly, but major haemorrhages significantly decreased (ARR of 3 fewer people out of 100 in meta‐analysis of 7 studies (95% CI 5 to 1 fewer)) and clinical outcomes improved (INR within range) in most studies (3 of 4 studies). Since several outcomes (eg thromboembolic events, mortality) reflect relatively rare events it is possible that studies were underpowered to detect clinical differences for some of these outcomes.
Several reviews also reported other outcomes related to medicines use. Roughead 2005 found that a majority of studies showed significant improvements in knowledge (4 of 6 studies) and medicines use (6 of 9 studies). These included improvements following education on techniques for using medicines (eg inhaler use) (2 of 2) and improved risk management (2 of 2). However, there were no differences in quality of life (11 of 16 studies) or adverse effects (3 of 4 studies). Morrison 2001 on pharmacist counselling and education reported individual studies with significantly improved medicines error identification, possible improvements in knowledge, and correct use of inhaler, and decreased adverse experiences. Wright found that self‐administration programmes for hospital inpatients improved knowledge in a minority of studies (6 of 16 studies), with no clear effects on medicines errors or satisfaction. Garcia‐Alamino 2010 reported that a significant proportion of people undertaking self‐monitoring or self‐management for oral anticoagulation therapy (mean 25%) were unable to complete treatment and dropped out, with reasons including device problems, physical limitations preventing self‐testing, inability to attend training or failing the assessment. Trial participation was also low with 68% overall refusing participation.
Bhogal 2006's review compared asthma management in children who used written action plans based on symptoms, or based on clinical measures. Improvements in clinical outcomes and other outcomes were inconsistent between the two types of action plans, but significantly more children (but not parents) intended to use the symptom‐based written action plans.
Two reviews looked at the effects of post‐surgical patient‐controlled analgesia (PCA), with mixed results. The review by Bainbridge 2006 comparing patient‐administered with nurse‐administered analgesia, reported increased analgesic consumption (7 studies) and decreased pain (8 studies) with PCA, although there were no differences in severe pain, mortality or adverse events. Another review (Yankova 2008) assessing structured PCA education found improved knowledge over standard PCA education (4 studies) but significantly better pain relief in only the minority (1 of 5) of studies.
Supporting behaviour change
Several reviews assessed strategies to promote or support medicine‐related behaviour change, including changes to address under‐use, overuse or misuse of medicines. This included 27 new reviews (Al‐aqeel 2011; Bain‐Brickley 2011; Bennett 2009; Buckley 2010; Chivu 2008; De Bleser 2009; Ford 2009; Gleeson 2009; Gray 2009; Haywood 2009; Holland 2008; Liu 2008; Lutge 2012; Machado 2007a; Machado 2007b; Machado 2008; Molife 2009; Mollon 2009; Odegard 2007; Oyo‐Ita 2008; Parr 2009; Polis 2007; Ranji 2008; Saini 2009; Smith 2009; Thomas 2010; Wright 2006) and 6 updated reviews (Garcia‐Alamino 2010; Halpern 2011; Lewin 2010; Mahtani 2011; Nkansah 2010; Schedlbauer 2010), bringing the total to 53 in this category.
One large review (93 interventions) across diseases reported mixed effects of interventions to support behaviour change for adherence and clinical outcomes (Haynes 2008). Most of the effective interventions for short‐term treatment were simple, while most of the effective interventions for long‐term treatment were complex.
Disease‐related reviews
When considering all reviews across diseases using simple or complex interventions, the results were mixed. Various interventions to support behaviour change showed improvements in medicines use, with few clear overall patterns.
Simplified dosing regimens (eg decreasing frequency of doses from four to twice daily; changing formulation from tablet to transdermal form; or from syrup to tablet form) improved adherence in the majority of studies in several reviews (Schroeder 2004; Vermeire 2005), including adherence to chronic medicines in older adults (Russell 2006); and in single studies in several other reviews (Gleeson 2009; Gray 2009; Schedlbauer 2010; Smith 2009). In one other review in chronic diseases (Saini 2009), simplified dosing changing regimens from more frequently to once daily improved adherence, whereas effects of simplifying doses to other schedules (eg changing to simplified regimens of two or three times daily) were less clear.
Self‐monitoring and self‐management interventions to support behaviour change in people using oral anticoagulation medicines generally had positive effects on clinical outcomes and adverse effects. Self‐management improved mortality and decreased adverse events, with mixed effects on clinical outcomes; while self‐monitoring did not significantly reduce mortality or thromboembolic events but did decrease major hemorrhages and improve clinical outcomes (Garcia‐Alamino 2010)). However, a significant proportion (25%) of people self‐monitoring or self‐managing was unable to complete treatment, and dropped out. Both studies in Russell 2006 on self‐medication management programs for older people improved adherence. Bhogal 2006 found mixed results for clinical outcomes when comparing different written action plans for asthma. The review found that more children intended to use the plan, and had a lower risk of exacerbations, when symptoms rather than clinical measures were used to guide treatment decisions. Molife 2009 compared insulin pen devices with syringe and vial for delivering insulin in diabetes, reporting better ease of use, pain, preference, acceptability and flexibility with pens in the majority of studies.
Support and education, alone or as part of multifaceted interventions, improved adherence in approximately half of studies in two reviews (Rueda 2006 and Schroeder 2004), but effects on clinical outcomes were mixed.
In contrast, many reviews reported non‐significant changes in adherence and other outcomes or improvements in only a minority of studies. These included interventions such as patient motivation and support to promote behavior change in hypertension (Schroeder 2004); counselling to support behaviour change in a range of conditions including epilepsy, glaucoma, schizophrenia, or for oral contraception (Al‐aqeel 2011; Halpern 2011; McIntosh 2006; Olthoff 2005; van Eijken 2003; Zygmunt 2002); peer support groups for children with HIV (Bain‐Brickley 2011); medicines self‐administration programmes for hospital inpatients (Wright 2006); and directly observed therapy for adherence to medicines for TB (Volmink 2007) and HIV (Ford 2009).
Interventions including education or information to support behaviour change
Results were also mixed for reviews of interventions which included an education or information component to support behaviour change. Adherence improved in a minority of those studies in Schedlbauer 2010, Schroeder 2004 and Vergouwen 2003. There were few consistent effects on knowledge, clinical or other outcomes.
In another review, education and facilitation in diabetes significantly improved metabolic control (glycosylated haemoglobin levels), but only a minority of studies improved adherence (Vermeire 2005). Similarly, a review by Bennett 2009 on patient‐based cancer pain management education showed improved pain intensity on several measures, but again improved adherence (1 of 3 studies) and knowledge (7 of 17 studies) in only a minority of studies.
Nicolson 2009 also showed improved adherence with medicines instructions in only a minority of studies (2 of 6 studies) that provided written information. Half of studies (20 of 41 studies) using a combination of education and counselling among older people improved adherence (Russell 2006).
However, a review including before‐and‐after assessments of interventions with information provision via different formats and in combination with other interventions such as counselling, provision of folic acid and reminders showed improved consumption of folic acid during pregnancy in the majority of studies (9 of 14 studies) as well as improved knowledge (7 of 10 studies) (Chivu 2008). In Parr 2009, brief interventions recommending benzodiazepine dose reduction, with or without self‐help information, improved cessation of benzodiazepine use in the majority (4 of 5) of studies.
Education or information interventions (combined with behavioural or affective components) to promote adherence to medicines post organ transplantation (De Bleser 2009) improved knowledge in single studies, but adherence inconsistently; whereas combined patient informational and behavioural interventions improved adherence (2 studies); similarly, combined education and medicines barriers counselling for osteoporosis medicines in Gleeson 2009 improved adherence (2 studies) but not persistence, and single studies of education or counselling alone showed little effect on adherence.
In single studies, education and medicines usage training improved adherence (glaucoma, Olthoff 2005); parent, but not patient education improved adherence, while education and psychosocial therapy improved adherence but not seizure frequency (epilepsy, Al‐aqeel 2011); and home‐based education and support had mixed effects on adherence and no significant effects on viral load (antiretroviral therapy in children, Bain‐Brickley 2011).
In Oyo‐Ita 2008, single studies of information campaigns or different forms of education improved immunisation uptake; while in Thomas 2010 education plus a vaccination offer improved immunisation demand (absolute risk increase (ARI) of meta‐analysis of 2 studies of 16 more immunisations out of 100 (95% CI 7 to 27 more)), as did (in single studies) education by nurses and vaccinated patients, and reminder telephone calls delivered with an education brochure.
Ranji 2008, assessing interventions to reduce unnecessary antibiotic prescribing, found that patient education alone (6 interventions) or patient plus clinician education with (3 interventions) and without (5 interventions) audit and feedback, each reduced the proportion of patients receiving antibiotics to varying degrees, with unclear significance, but did not change health service use. Community‐based interventions (mass media campaign, education, written materials, other combinations) reduced the proportion of patients receiving antibiotics in the majority (3 of 5 interventions) of cases; while non‐community‐based interventions targeting patients alone (such as financial incentives, educational videos and pamphlets) also reduced the proportion of patients receiving antibiotics (2 interventions), without changing health service use (1 intervention). In Smith 2009, education or training plus pre‐packaged antimalarial medicines (AM) improved appropriate AM treatment and adherence in half (1 of 2) of studies. Integrated childhood disease management programmes also improved appropriate AM treatment by providers (2 studies). Training or education for informal healthcare providers improved appropriate AM prescribing, treatment and dose whereas training/education for formal providers did not. In single studies, training plus community education significantly increased appropriate AM treatment, adherence and knowledge of correct dose; and dispensing and communication skills training increased provider appropriate AM treatment and dose, and patient prompt treatment seeking and adherence.
Reminders to support behaviour change
Reviews including studies evaluating the use of reminders to support behaviour change also showed mixed effects.
Adherence improved by a small amount in a review of 24 studies which included practical management tools like reminders (Amico 2006) (mean Increase (MI) 0.35 (95% CI 0.20 to 0.51)), with mixed effects in a review of intensified patient care (reminders; Schedlbauer 2010). Packaging showed mixed results for adherence and ease of use in long‐term medicines in Mahtani 2011, but increased adherence in a majority of studies (3 of 4 studies) for malaria in Orton 2005. In single studies in Odegard 2007 reminders, unit‐dose packaging and reminders plus unit‐dose packaging each improved adherence, whereas cue‐dose training did not.
Among older people adherence improved in a majority of cue interventions for behaviour change, half of the studies of cues plus organisers, and a minority of studies of organisers alone (Russell 2006). In epilepsy (Al‐aqeel 2011) single studies of cue identification improved adherence, whereas patient reminders plus counselling did not.
Alarms (1 study) and compliance devices (2 studies) improved adherence in a review of adherence for ocular hypotensive medicines (Olthoff 2005); in another (Bain‐Brickley 2011), a medicines diary with support for HIV‐positive children (1 study) did not change adherence. In single studies in Liu, late patient tracers for TB treatment adherence in the form of letters, home visits and/or education generally reduced treatment non‐completion. However in another review on older adults, practical reminder devices such as reminder packaging, pillboxes, organisers, charts or schedules, improved adherence in only 3 of 13 assessed interventions (van Eijken 2003).
Reminders were generally successful in improving adherence to immunisation uptake (Jacobson 2005; Stone 2002), however small the effect (Maglione 2002), although tailored reminders appeared to be most effective (Thomas 2010).
Interventions for organisational change
The few reviews which evaluated changing care organisation and delivery to support behaviour change show mixed effects. Most collaborative care studies in primary care, involving multimodal interventions to support behaviour change, improved both adherence (9 of 11 studies) and depressive symptoms (10 of 11 studies; Vergouwen 2003). Lay health workers also improved immunisation uptake (Lewin 2010). However, effects of pharmacy‐based education and facilitation (Vermeire 2005) or services provided by community or hospital pharmacists (Koshman 2008; Morrison 2001) were mixed for adherence and clinical outcomes, but reduced the numbers of medicines prescribed (Nkansah 2010). Three further reviews (Machado 2007a; Machado 2007b; Machado 2008) involving pharmacists in hospital and community settings providing disease education and medicines management interventions (for hypertension, diabetes and hyperlipidaemia) reported improved adherence in only the minority of studies or not at all, and had variable effects on clinical outcomes and on medicines knowledge. Few studies (1 of 3) improved adherence with multifaceted generalised interventions including telephone‐linked computer system and instructions with reminders for older people (van Eijken 2003). Similarly, adherence improved in half (7 of 14) of studies of pharmacist‐led medicines review to avoid hospital admissions in older people, with improvements in a range of medicines problems (Holland 2008). In Parr 2009, gradual dose reduction and/or psychological interventions improved cessation of benzodiazepines.
In Haywood 2009, provider‐targeted interventions for sickle cell disease treatment adherence improved pain management, although mainly measured in single studies, while patient‐targeted interventions to improve self‐management did not improve adherence. Advance provision of emergency contraception (Polis 2007) increased use of emergency contraception but pregnancy rates and standard contraceptive use were unchanged, and incorrect use increased by 17% in a minority (1 of 3) of studies with advance provision, as did multiple use of emergency contraception. Lutge 2012, assessing the effects of material incentives, found mixed effects on TB treatment adherence, with improvements in prophylactic treatment but no change to completion rates.
Service organisation interventions (Buckley 2010), including doctor, nurse or pharmacist delivery of complex packages of secondary prevention for heart disease, had mixed effects on clinical outcomes and no effects on numbers or types of medicines prescribed.
A review of computerised decision support systems (CDSS) to prevent medicines errors and promote evidence‐based prescribing (Mollon 2009) reported that interventions were successfully implemented (36 of 40 studies) and healthcare provider behaviour changed in the majority of studies (25 of 40 studies) but patient‐related outcomes improved in only the minority of studies (5 of 22 studies).
Support
A number of reviews assessed strategies to assist and encourage consumers to manage their health and medicines use: 5 new reviews (Bain‐Brickley 2011; Gleeson 2009; Holland 2008; Odegard 2007; Wright 2006) and 1 updated review (Halpern 2011) have been added in this update, bringing the total to 17 reviews in this category.
No reviews included studies of support provided as a single intervention to improve adherence or medicines use. However, two key reviews focussing on support and psychosocial interventions had conflicting results (Vergouwen 2003; Zygmunt 2002); we highlight them here.
In Vergouwen 2003, 9 of 11 studies evaluating collaborative care involving psychological and psychiatric care for people with depression showed improved adherence, and 10 of 11 studies showed improved depression. In comparison Zygmunt 2002 evaluated single or multimodal psychosocial interventions for people with schizophrenia, and found that only a minority of the interventions improved adherence to antipsychotic medicines. Specifically, adherence improved after: individual interventions (2 of 4 studies), group interventions (2 of 4 studies) and family therapy (3 of 12 studies), community‐based interventions (4 of 10 studies), and mixed interventions and comparisons (5 of 9 studies). However, 5 of the 9 studies which had a specific goal to improve adherence led to improvements.
The limited or lack of change to medicines adherence with interventions focussing on support alone is similar to the results of several reviews in which support was provided in combination with other strategies. A meta‐analysis of 26 interventions, many including support, to promote adherence to antiretroviral therapy found a small positive effect (Amico 2006). One of 8 studies including support in counselling improved adherence to hormonal contraceptives (Halpern 2011).
No studies including motivational interviewing improved adherence to antiretroviral therapy in adults and children (Rueda 2006). Similarly, peer support groups or support delivered with medicines diaries or education had little or no effect on adherence to antiretrovirals or clinical outcomes in HIV‐positive children (Bain‐Brickley 2011). However, home‐based education plus support improved adherence when measured by pharmacy refill (but not self‐report) in a single study.
One study in McIntosh 2006, providing compliance therapy specifically to improve adherence, found no significant difference in adherence or clinical outcomes, attitudes towards medicines, quality of life, or health services use. Also in single studies in Gleeson 2009, simplified dosing plus support improved adherence and persistence, while patient education and medicines barriers counselling improved adherence to osteoporosis medicines, but not persistence; and when combined with feedback on response to therapy neither persistence (2 studies) nor adherence (1 study) improved.
Mixed results for adherence and other outcomes were found in other reviews. A minority of studies (10 of 24 studies) of interventions including social and family support and counselling for people with hypertension, increased adherence (Schroeder 2004). Van Wijk 2005 found mixed effects for adherence with support interventions which included encouragement, counselling, and problem identification. Counselling or weekly follow‐up did not improve adherence to diabetes treatments (3 studies) but did increase blood glucose testing and decrease hospitalisations in single studies in another review (Odegard 2007). Finally, in a review of medicines self‐administration programmes for hospital inpatients, including a range of support such as counselling (Wright 2006), a minority of studies (4 of 12 studies) reported improved adherence and knowledge (6 of 16 studies), with mixed effects on medicines errors and satisfaction.
Russell 2006 found that in half of studies (20 of 41 studies), education and counselling interventions improved adherence. Stevenson 2004, a review that included before‐and‐after studies, also found mixed results for adherence in studies which promoted contact (face‐to‐face or by telephone) between patients and nurses or medical assistants, but found increased discussion of medicine issues with doctors. Stevenson also reported a study involving medicines counselling visits between pharmacist and patients, which found mixed results, including a tendency for improved quality of life and knowledge in the intervention group. Before‐and‐after studies of interactions between pharmacists and patients were also reviewed by Lummis 2006. This review found that overall support and encouragement by pharmacists for the use of patients’ own medicines in hospital improved the identification of medicines errors and reduced costs to hospitals and patients. As part of pharmacist medicines review interventions in the review by Holland 2008, neither the two studies which included counselling and support, nor the four studies including home visits and follow‐up,showed significant effects on numbers of medicines prescribed or on mortality or hospital admissions.
More broadly, a large review of adherence‐promoting interventions by Haynes 2008 found that most of the effective interventions in long‐term treatments were complex. These included interventions such as counselling, reinforcement, family therapy, psychological therapy and crisis intervention. However, both Zygmunt 2002 and Amico 2006 found no relationship between the complexity of an intervention (which included support) and better adherence.
Minimising risks or harms
In a number of reviews, strategies were focussed on preventing or managing adverse events or complications; whether for individuals experiencing an emergency event or needing ongoing treatment, or for reducing population‐level risks. This included 18 new reviews (Argarwal 2011; Bainbridge 2006; Bayoumi 2009; Castelino 2009; Ford 2009; Golicki 2008; Holland 2008; Jegu 2011; Liu 2008; Lutge 2012; Misso 2010; Mollon 2009; Nishtala 2008; Oyo‐Ita 2008; Pankowska 2009; Ranji 2008; Thomas 2010; Wright 2006) and 2 updated reviews (Garcia‐Alamino 2010; Lewin 2010), bringing the total to 33 reviews in this category.
There were few specific strategies to minimise risks and harms of treatment or disease at an individual level. Of note are four reviews of interventions which place responsibility for disease management with the patient. A review of self‐management and self‐monitoring for oral anticoagulation therapy (Garcia‐Alamino 2010) found generally positive effects on clinical outcomes and adverse effects. With self‐management interventions (self‐testing and self‐adjusting therapy based on a predetermined dose schedule), mortality and risk of adverse events such as thromboembolic events significantly decreased (absolute risk reduction (ARR) of 2 fewer people out of 100 from meta‐analysis of 12 studies (95% CI 3 to 1 fewer)), but major hemorrhages were not improved and clinical outcomes (INR within range) improved in half (5 of 10) of studies. Conversely, with self‐monitoring interventions (self‐testing and calling clinic for the appropriate dose adjustment), mortality and risk of thromboembolic events decreased, although not significantly, but major haemorrhages significantly decreased (ARR of 3 fewer people out of 100 in meta‐analysis of 7 studies (95% CI 5 to 1 fewer)) and clinical outcomes improved (INR within range) in most studies (3 of 4 studies). Since several outcomes (eg thromboembolic events, mortality) reflect relatively rare events it is possible that studies were underpowered to detect clinical differences for some of these outcomes.
Another review comparing specific monitoring plans showed that risk of asthma exacerbations requiring acute care was lower for symptom monitoring, compared with peak flow monitoring action plans (Bhogal 2006). Similarly, Argarwal 2011 comparing home and clinic blood pressure monitoring, reported reduced systolic, diastolic and arterial blood pressures and therapeutic inertia (defined as no change in medicines use despite elevated blood pressure), as well as reducing medicines used. In contrast, a minority of studies in a review of self‐administration medicines programmes (Wright 2006), showed improved knowledge (6 of 16 studies) and adherence (4 of 12 studies) in only a minority of studies, with mixed effects on medicines errors.
In diabetes care, three reviews looked at ways of delivering insulin to better control blood glucose and avoid adverse events. The review by Golicki 2008 looked at continuous monitoring (Continuous Glucose Monitoring Service device, CGMS), compared with self‐monitoring, in children with type 1 diabetes, reporting increased insulin dose adjustments in half (1 of 2) of studies, but few differences in adverse events such as major or minor hypoglycaemic episodes or local adverse events, although adverse events were reported in few studies. Also in children with type 1 diabetes, Pankowska 2009 compared subcutaneous insulin infusion (CSII) with multiple daily injections (MI), reporting significantly lower total insulin dose and improved glycemic control (total HbA1c), compared with multiple daily injections (MDI), while severe hypoglycemia rates were unchanged but ketoacidosis rates increased, with the only two cases reported in the CSII group. No CSII participants discontinued treatment at the end of trial; and the majority of participants opted to continue or switch to CSII over MDI (2 studies), with mixed effects on quality of life for children but improvements in a single study for parents.
Misso 2010 looked at this same comparison in adults with type 1 diabetes, reporting significantly reduced HbA1c levels with CSII, but mixed effects on daily insulin requirements. Of the 22 studies reporting mortality, one event was reported in the CSII group; with no clinically meaningful minimal differences in quality of life reported in any study. CSII reduced severe hypoglycaemic events in the majority (9 of 15) of studies, and serious adverse events were measured in 14 studies, with only 1 study observing an adverse event in the CSII group (significance unclear), while mixed effects or no changes were seen in with dropouts due to adverse events, non‐severe and nocturnal hypoglycaemic events, injection or infusion site injury, or ketoacidosis.
In Jegu 2011, assessing the effectiveness of slow‐release oral morphine (SROM) as an option for opioid maintenance therapy, compared with usual care, the majority of studies showed improved quality of life (3 of 5 studies), preference (3 of 3 studies) and fewer adverse events (2 of 3 studies), with mixed effects on treatment adherence. In Bainbridge 2006, comparing patient‐controlled analgesia (PCA) with nurse‐controlled analgesia (NCA), post‐surgical pain was significantly lower at 48 hours, but not earlier; and analgesic consumption was increased, but there were no differences in all‐cause mortality, severe pain, adverse events (nausea and vomiting, severe sedation, respiratory depression), or treatment discontinuation.
A review of 24 studies, including interventions of education or counselling about adverse effects of antiretroviral medicines, found small improvements to medicines adherence (MI 0.35 (95% CI 0.20 to 0.51); Amico 2006). The interventions with education or counselling were considered medium‐level intensity, and level of intensity was not related to effect size, nor was duration of the intervention. In one large, high‐quality review, several studies that examined the effects of telling patients about adverse effects of medicines showed no significant decrease in adherence (Haynes 2008). A review of computerised decision support systems (CDSS) to prevent medicines errors and promote evidence‐based prescribing (Mollon 2009) reported that interventions were successfully implemented (36 of 40 studies) and healthcare provider behaviour changed in the majority of studies (25 of 40) but patient‐related outcomes improved in only the minority (5 of 22) of studies.
Interventions involving healthcare professional and patient interactions were investigated in several reviews, reporting mixed results for various outcomes. Overall, a review of 22 studies of pharmaceutical care interventions for managing health or medicines‐related problems (Roughead 2005) showed that a minority of studies (2 of 8 studies) significantly improved adherence, but a majority showed significant improvements in knowledge (4 of 6 studies), medicines use (6 of 9 studies) and risk management (2 of 2 studies). A minority of included studies showed an improvement in adverse events (1 of 4 studies); and health resource use (2 of 8 studies), but effects on clinical outcomes were mixed. In a review of interventions to improve communication between healthcare professionals and patients (Stevenson 2004), modified pharmacy services and medicines review decreased medicines problems (1 study of 1), but telephone contact by nurse or assistant did not change the number of people reporting adverse events or stopping treatment because of them. Lummis 2006 primarily included before‐and‐after studies to evaluate the use of patients’ own medicines (POMs) in hospital with pharmacist assessment. Results from included studies showed that the identification of patient medicines errors was increased when POMs were used together with pharmacist assessment. There was no difference in medicine administration errors on wards when POMs were used without pharmacist review. Royal 2006 also found mixed results for pharmacist‐led interventions to decrease adverse events and mortality; a minority of studies (4 of 15 studies) reduced hospital admissions, but there were no significant changes to emergency department visits. Similarly, Bayoumi 2009 also reported mixed results for ambulatory care medicines reconciliation interventions aiming to decrease adverse events through interventions such as reviews of medicines lists, updating patient records, and access to a medicines helpline. With ambulatory care medicines reconciliation, there was a lower mean proportion of medicines discrepancies and medicine lists with medicines discrepancies in half (1 of 2) of before‐and‐after studies, but mixed effects on clinically significant and serious discrepancies (1 study). Post‐hospital discharge medicines reconciliation, in a single study, reduced medicines name but not dose discrepancies; and in one further before‐and‐after study the mean proportion of medicines discrepancies was unchanged and there was a small (1.2%) increase in clinically‐important errors detected (significance unknown). Finally, Koshman 2008 assessed the effects of community pharmacist‐led interventions for people with heart failure, and reported mixed results. There were significantly fewer hospitalisations with pharmacist collaborative care interventions (ARR of 12 fewer people out of 100 from meta‐analysis of 4 studies (95% CI 22 to 1 people fewer)), but not with pharmacist‐directed care. Neither intervention type had a significant effect on mortality.
Two further reviews (Castelino 2009; Holland 2008) reviewed interventions involving pharmacists taking on different roles to optimise medicines use in older people. Pharmacist‐led medicines reviews ( Holland 2008) showed a small decrease in numbers of medicines prescribed (15 studies), fewer medicines problems (4 of 4 studies) and, in the majority of studies, decreased storage problems (2 of 3 studies) and unnecessary medicines (5 of 7 studies). Adherence improved in half of these studies and adverse events (1 of 9 studies) in only a minority, while mortality, hospital admissions and quality of life were unchanged. Castelino 2009 reviewed interventions involving pharmacists alone or as members of multidisciplinary teams. Pharmacist‐delivered interventions improved Medication Appropriateness Index (MAI) scores (3 studies) but in single studies had mixed effects on markers of inappropriate prescribing, while other outcomes including adverse events, adherence, number of medicines, and quality of life were unchanged. A multidisciplinary team intervention including a pharmacist improved MAI scores in half (1 of 2) of studies, with mixed effects on a range of medicines and prescribing outcomes, and reduced serious adverse events in a single study.
Also in older people, the review by Nishtala 2008 looked at a range of interventions including pharmacist‐led medicines review and education of health professionals to improve appropriate use of psychotropic medicines. In single studies, medicines review increased the cessation of antipsychotics and non‐recommended hypnotics, but use of other medicines (psycholeptics and benzodiazepines), was unchanged. Heathcare worker education decreased days of psychotropic drug use (2 studies) and psychotropic drug use in half of studies (2 out of 4 studies) and in single studies decreased use of more than one hypnotic drug and increased as‐required use of antipsychotics.
Public health interventions to minimise risks or harms
Reviews showed a range of interventions improved immunisation uptake. A broad overview of interventions including meta‐analyses (Stone 2002) showed that organisational change interventions were most effective (10 studies, OR 16.0 (95% CI 11.2 to 22.8). Also effective were reminders (23 studies, OR 2.52 (95% CI 2.24 to 2.82), patient financial incentives (8 studies, OR 3.42 (95% CI 2.89 to 4.06) and education (22 studies, OR 1.29 (95% CI 1.14 to 1.45). Maglione 2002 reviewed the effect of mass mailings, showing that most of the mass mailing studies found improved immunisation uptake, but effects were small and not clinically significant. More recent reviews showed increased immunisation uptake with lay health worker interventions (Lewin 2010); and with reminder and recall interventions which included person‐to‐person calls, letters, autodialer computer reminders and patient plus provider reminders, which resulted overall in an 11% absolute increase in immunisation rates (Jacobson 2005). Person‐to‐person calls were the most effective single intervention. In particular, however, one study showed no effect of reminders in adolescents, and reminders with outreach did not significantly increase immunisation. The review by Thomas 2010, looking at a broad range of approaches to increase influenza vaccination in the elderly, reported mixed effects on community demand for immunisation of different reminder and recall strategies, with tailored reminders appearing most effective (effective in the majority of studies (9 of 13 studies)). Combinations of patient education, health risk appraisals, group or home visits, offers of vaccination and/or free vaccination improved immunisation demand and/or access, although almost always assessed only in single studies. Physician or other health professional reminders and education with feedback had mixed effects on immunisation rates, often in single studies; while immunisation rates were improved with provider financial incentives and with facilitators working with physicians on prevention measures in the majority of studies (2 of 3 studies). Another review (Oyo‐Ita 2008) found, in single studies, that information campaigns or different forms of education, home visits, provider training or complex combined interventions improved immunisation uptake, whereas financial incentives did not.
Several strategies to aid in the eradication of tuberculosis (TB) were reviewed. Lewin 2010, assessing lay heath worker interventions for improving TB treatment adherence, reported increased cure rates for new and re‐treated smear‐positive patients with lay health worker interventions (absolute risk increase, ARI, of meta‐analysis of 4 studies, of 13 more people out of 100 (95% CI 4 to 18 more), while other treatment outcomes improved in only a minority of studies or not at all. In single studies in Liu 2008, late patient tracers in the form of letters, home visits, and/or education generally reduced treatment non‐completion and clinical outcomes including treatment failure and numbers of smear‐positive patients at end of treatment. Lutge 2012, assessing the effects of material incentives, found mixed effects on TB treatment adherence, with improved uptake and continuation of prophylactic treatment (3 of 3 studies) but no change to completion rates for prevention (3 studies) or treatment (1 study). In single studies, monetary incentives compared to non‐monetary incentives significantly increased adherence (completion) of TB prophylaxis, whereas immediate compared to delayed incentive payments did not.
Volmink 2007 found no significant differences in treatment completion or cure of tuberculosis with directly observed therapy (DOT) overall, although there was a small difference in favour of DOT delivered at home compared with self‐administration. Similarly, in Ford 2009, assessing DOT for adherence to highly active antiretroviral therapy (HAART), no significant differences in adherence, all‐cause mortality, AIDS‐defining events, development of resistance mutations or losses to follow‐up were found when compared to self‐administered therapy.
Spurling 2007 reviewed delayed prescribing as a strategy to reduce widespread antibiotic resistance. Meta‐analysis of 6 studies showed that delayed prescribing reduced antibiotic use (ARR 64 fewer people out of 100 used antibiotics with delayed antibiotic interventions (95% CI 81 to 38 fewer)), but heterogeneity was high; and 1 of 2 studies showed increased supplementary medicines use. Delayed prescribing also had mixed effects on clinical outcomes and adverse effects. A second review of quality improvement interventions to reduce unnecessary antibiotic prescribing (Ranji 2008) included several studies of delayed prescriptions and reported similar results: fewer patients filling antibiotic prescriptions (6 studies) and lower mean number of antibiotic prescriptions in a single study, again with mixed adverse effects (1 study). However, this review found satisfaction was lower with delayed antibiotics only in the minority (1 of 4 studies). This review also reported that patient or clinician education, patient plus clinician education with and without audit and feedback, and other quality improvement strategies (such as decision support, written materials, financial disincentives, alone or in combination) each reduced the proportion of patients receiving antibiotics to varying degrees, with unclear significance, but did not change health service use. Community‐based interventions (mass media campaign, education, written materials, other combinations) and non‐community‐based interventions targeting clinicians and patients (audit and feedback, educational workshops, combinations) or patients alone also reduced the proportion of patients receiving antibiotics, without changing health service use.
Improving quality
Several reviews focussed on strategies to improve care coordination or integration, such as substitution or expansion of care or aiming to address barriers to medicines use. This included 13 new reviews (Bayoumi 2009; Buckley 2010; Castelino 2009; De Bleser 2009; Haywood 2009; Holland 2008; Mbuba 2008; Nishtala 2008; Odegard 2007; Oyo‐Ita 2008; Polis 2007; Ranji 2008; Thomas 2010) and 2 updated reviews (Lewin 2010; Nkansah 2010), bringing the total to 30 reviews in this category. These reviews primarily examined changing healthcare professionals' roles and their interactions with consumers (eg pharmacists and nurses), and, to a lesser extent, financial incentives and medicines pricing policies.
Eight reviews evaluated the roles of healthcare professionals across diseases/conditions.
Roughead 2005 reviewed 22 studies of pharmaceutical care interventions (consultations between pharmacist and patient), and found that a minority of studies (2 of 8 studies) showed significant improvements in adherence; and there were mixed results for clinical outcomes in 16 studies; and mortality and morbidity in 25 studies. However, a majority showed significant improvements in knowledge (4 of 6 studies) and medicines use (6 of 9 studies), better techniques for using medicines (eg inhaler use) (2 of 2 studies), quality of life (11 of 16 studies), and improved risk management (2 of 2 studies).
Nkansah 2010 assessing the effects of additional outpatient pharmacist services for patients, reported similar findings, with mixed effects on clinical outcomes and a number of changes in medicines use including smaller total numbers of medicines prescribed (3 studies), and in single studies, decreased therapeutic duplication, inappropriate prescriptions, and doses per day, although significance was not always clear, and other effects on medicines use were mixed and dependent on medicines class. Adverse effects were unchanged in a single study. In this same review, pharmacist services targeted at professionals increased the number of patients treated according to practice guidelines (1 study) and the number of medicines prescribed per month for women but not men (1 study); but did not change medicines use or number of medicines used or antibiotics prescribed.
Bayoumi 2009 reviewed the effects of ambulatory care medicines reconciliation interventions aiming to decrease adverse events through interventions such as medicines list reviews, updating patient records, and access to a medicines helpline. With ambulatory care medicines reconciliation, there was a lower mean proportion of medicines discrepancies and medicine lists with medicines discrepancies in half (1 of 2) of before‐and‐after studies, but mixed effects on the clinical relevance of discrepancies detected, with minor discrepancies increasing and clinically significant and serious discrepancies decreasing, although significance was unclear (1 study). Post‐hospital discharge medicines reconciliation, in a single study, reduced medicines name discrepancies but not dose discrepancies. In one further before‐and‐after study the mean proportion of medicines discrepancies was unchanged, together with a small (1.2%) increase in clinically‐important errors detected (significance unknown).
Another review by Stevenson 2004, focussing on interventions to improve communication between providers and patients, found mixed results for adherence in studies which promoted contact between patients and nurses or medical assistants either face to face or by telephone. It did find better discussion of medicines issues and a tendency for better quality of life and knowledge. Two studies changed pharmacist visits (clinic or home) which improved satisfaction and decreased medicines problems as well as costs. Effects were mixed for adherence and clinical outcomes. One further review looking across diseases/conditions assessed interventions involving different health professionals that aimed to decrease medicines‐related adverse events (Royal 2006). In this review, pharmacist‐led interventions had mixed effects. Mortality decreased in half of studies (2 of 4 studies), and in a minority of studies there were fewer adverse events (1 of 3 studies) and hospital admissions (4 of 15 studies). There were no changes to emergency department visits, however. Interventions led by primary healthcare professionals or nurses did not consistently change any reported outcomes.
Three further reviews (Castelino 2009; Holland 2008; van Eijken 2003) reviewed interventions involving pharmacists taking on different roles to optimise medicines use in older people. van Eijken 2003 reviewed seven multifaceted interventions which included new services provided by pharmacists and nurses to older adults with various conditions. They found mixed results with 3 of the 7 interventions increasing adherence in older adults. The review by Holland 2008 on pharmacist‐led medicines reviews showed a small decrease in numbers of medicines prescribed (15 studies), fewer medicines problems (4 studies) and, in the majority of studies, decreased storage problems (2 of 3 studies) and unnecessary medicines (5 of 7 studies), as well as improved knowledge (6 of 11 studies). Adverse events (1 of 9 studies) and costs (4 of 14 studies) were lower in only a minority of studies, and adherence (7 of 14 studies) and satisfaction (2 of 4 studies) improved in half, but mortality, hospital admissions and quality of life were unchanged.
Castelino 2009 reviewed interventions involving pharmacists alone or as members of multidisciplinary teams to address overuse, under‐use and misuse of medicines. Pharmacist‐delivered interventions improved MAI scores (3 studies) but in single studies had mixed effects on markers of inappropriate prescribing, while other outcomes including adverse events, adherence, number of medicines, costs, quality of life, satisfaction and knowledge were unchanged. A multidisciplinary team intervention including a pharmacist improved MAI scores in half (1 of 2) of studies, with mixed effects on a range of medicines and prescribing outcomes, however in single studies serious adverse events and proportion of therapeutic duplication were reduced and under‐use of drugs (in‐ and out‐patient) improved.
In a review of interventions to reduce unnecessary antibiotic prescribing (Ranji 2008), patient or clinician education; patient plus clinician education, with and without audit and feedback; and other quality improvement strategies (such as decision support, written materials, financial disincentives, alone or in combination) each reduced the proportion of patients receiving antibiotics to varying degrees, with unclear significance, but did not change health service use. Community‐based interventions (mass media campaign, education, written materials, other combinations) reduced the proportion of patients receiving antibiotics in the majority of cases (3 of 5 interventions) and antimicrobial resistance (1 intervention); whereas community‐based interventions incorporating audit and feedback did not change antibiotic prescriptions (2 interventions) but may reduce cost (1 intervention; significance unclear). Non‐community‐based interventions targeting clinicians and patients (audit and feedback, educational workshops, combinations) or targeting patients alone decreased antibiotic prescriptions or consumption (2 interventions) without changing health service use, while non‐community based interventions targeting clinicians alone (various combinations) reduced antibiotic prescribing in only a minority of studies (3 of 7 interventions; significance unknown); without changing satisfaction or health service use.
Other reviews evaluated the changing of roles in relation to specific diseases/conditions. Two reviews (Bower 2006; Vergouwen 2003) reported positive effects of collaborative care interventions delivered by various healthcare professionals. Vergouwen 2003 found that the majority of studies improved adherence to antidepressant medicines (9 of 11 studies) and depression (10 of 11 studies). Bower 2006 similarly reported significantly improved adherence (OR 1.92 (95% CI 1.54 to 2.39)) and significantly lower depressive symptoms (OR 0.24 (95% CI 0.17 to 0.32). In hypertension (Schroeder 2004), 8 of 18 studies evaluating complex interventions improved adherence (from 5% to 41%); one study of work site care showed better adherence and clinical outcomes; home visits and education improved adherence in 2 studies; a pharmaceutical care model in 2 studies improved adherence with 1 improving hypertension; and rewards in 1 study improved adherence with no effects on clinical outcomes. Tailored education and/or pharmacist medicines review interventions for diabetes (Odegard 2007) did not significantly change adherence or barriers to adherence (2 studies), while counselling or weekly follow‐up interventions increased blood glucose testing (1 study) and decreased hospital admissions (1 study) but did not change adherence (3 studies). In a review including before‐and‐after studies on sickle cell disease treatment adherence, Haywood 2009 reported that provider‐targeted interventions including audit and feedback, day hospital establishment interventions and clinical protocol interventions, with or without sensitivity training, typically improved pain management although these outcomes were mainly measured in single studies each, and significance was not always clear.
Advance provision of emergency contraception (Polis 2007) increased use (7 studies) and multiple uses of emergency contraception (3 studies), decreased time to emergency contraceptive use in the majority of studies (4 of 5 studies), and reduced non‐use of emergency contraception (5 studies, significance unknown), but pregnancy rates and standard contraceptive use were unchanged and incorrect use increased by 17% in a minority (1 of 3) of studies with advance provision.
In heart failure (Koshman 2008), interventions involving pharmacist‐led services had mixed effects overall. Pharmacist‐directed care interventions had mixed effects on adherence and improved health‐related quality of life in the minority of studies (1 of 6 studies) but had no significant effects on mortality or hospital admissions. However pharmacist collaborative care interventions significantly decreased hospital admissions with an absolute risk reduction (ARR), of meta‐analysis of 4 studies, 12 people fewer per 100 (95% CI 22 to 1 fewer) hospitalised.
Mortality was not significantly changed and effects on adherence and health‐related quality of life were mixed in single studies. In contrast, in ischaemic heart disease (Buckley 2010), service organisation interventions including doctor, nurse or pharmacist delivery of complex packages of secondary prevention for heart disease, decision support and clinical guideline promotion and advice, had mixed effects on clinical outcomes such as blood pressure and cholesterol levels and no effects on numbers or types of medicines prescribed.
Two reviews (De Bleser 2009; Mbuba 2008) included evaluation of provision of free medicines. Mbuba 2008 looked at epilepsy treatment in developing countries. In two before‐and‐after studies, providing antiepileptic medicines, alone or with nurse education, may have reduced seizure frequency, and improved adherence, dropout, and response to therapy, as well as awareness; while providing nurse education may have increased medicines supply. In De Bleser 2009, a single study assessing the provision of free immunosuppressants for solid organ transplant recipient did not change adherence but reduced sub‐target immunosuppressant blood levels.
Lay health worker interventions in Lewin 2010 increased cure rates for new and retreated smear‐positive TB patients, and improved smear‐positive cure rates in half (1 of 2) of studies, but combined cure and treatment completion improved in only the minority (1 of 3) studies, while completion of preventive therapy was unchanged (2 studies).
One review (Lummis 2006), which included before‐and‐after studies, evaluated the use of patients’ own medicines in hospital (POMs). Individual studies showed that the identification of patient medicines errors was increased with POMs but there was no difference in medicines administration errors on the wards. Studies also showed costs to hospitals and patients after discharge were reduced with POMs (3 of 3 studies), but workload for pharmacists was increased (1 of 1 study) while dispensary staff workload was decreased (2 of 2 studies).
To improve immunisation uptake, Stone 2002 reviewed and meta‐analysed the results of various interventions in adults: organisational changes improved adherence the most (OR 16.0 (95% CI 11.2 to 22.8) from 10 studies). Lewin 2010 investigated the effect of lay health workers to promote knowledge, attitudes or behaviour changes to increase immunisation uptake. From the 4 studies found, there was a significant increase in immunisation uptake in adults and in children (absolute risk increase (ARI) 11 more people out of 100 (95% CI 4 to 18 more). Oyo‐Ita 2008 reported, in single studies, provider‐oriented training and home visits each improved immunisation uptake. Single studies in Thomas 2010, assessing interventions to promote influenza immunisation uptake in older people, including health risk appraisal or group visits plus an offer of vaccination, and home visits with vaccination encouragement plus a GP care plan, improved immunisation demand or access. Home visits plus immunisation offer (2 studies) and free vaccination (2 studies) also increased immunisation access, as did facilitators working with physicians on prevention measures including influenza vaccination in the majority of studies (2 of 3). Of interventions targeting physicians, financial incentives increased immunisation rate (2 studies), while combinations of education, academic detailing, feedback and/or comparisons with peers did not.
Three reviews investigated financial incentives targeting patients for immunisation uptake (Giuffrida 1997; Oyo‐Ita 2008; Stone 2002). Stone meta‐analysed the effects of patient financial incentives in 8 studies, reporting improved immunisation uptake (OR 3.42 (95% CI 2.89 to 4.06)), but also reporting that this was a relatively less effective intervention to improve immunisation uptake than organisational change interventions. In contrast, Oyo‐Ita reported, in single studies, non‐significant changes to immunisation uptake with financial incentives and with complex health system interventions that included patient financial incentives (such as provision of equipment, medicines and materials plus provider training).
Financial incentives, more generally, were also reviewed by Giuffrida 1997. The authors included one study specifically on incentives for immunisation uptake, reporting significant increases compared with no intervention, or when compared with telephone calls or prompts, but not when compared with other interventions (specific prompts or access). Guiffrida also looked at incentives to improve medicines adherence: studies comparing four financial interventions, such as rewards, compared to no intervention or usual care found increased adherence or uptake (two non‐significant); while studies comparing six financial interventions to another intervention (eg telephone prompts) showed increases in adherence or uptake (all six non‐significant).
Three reviews assessed the effects of different pharmaceutical pricing policies (Aaserud 2006; Austvoll‐Dahlgren 2008; Maio 2005) which indirectly influence consumers’ medicines use through different pricing structures and/or by altering the financial impact of medicines use. Although we included indirect‐to‐consumer interventions in this overview, we did not seek to include all reviews which used financial interventions or other indirect strategies to change consumer medicines use. There are likely to be other reviews of these interventions not included in this overview (eg if they were classified as too 'indirect to consumer') and which might contribute evidence on the effects of these interventions. We therefore provide only an overview of results from these reviews on financial interventions here.
Aaserud 2006 assessed pharmaceutical pricing and purchasing policies, and reported primarily on reference pricing policies (where one reference medicine is chosen from a therapeutically similar group, the price of which is covered; if people opt for a more expensive option they have to pay the price difference). Reference pricing increased the use of specific reference medicines, and decreased the use of cost share medicines, without affecting total reference medicines use, or use of medicines other than those in the reference group. Reference pricing also decreased total medicines expenditure but had mixed effects on healthcare use, including increased emergency visits and hospital admissions through emergency in a minority (1 of 10 interventions) of cases, and significantly increased non‐emergency hospital admissions and physician visits (5 of 10 interventions). Austvoll‐Dahlgren 2008 assessed cap and co‐payment strategies where patients share payment in different ways for their prescription medicines and reported similar effects. Caps, co‐payments, co‐insurance with ceiling strategies and changes in tiered co‐payments, alone or in different combinations, significantly decreased insurance plan overall medicines expenditure and overall prescription medicines use. However, these policies had mixed effects on discretionary and essential medicines use, patterns of healthcare use and patient medicines expenditure. The effects of fixed co‐payments, fixed co‐payments plus co‐insurance with or without ceilings, or of index pricing policies were unable to be determined. Pharmacy Utilisation Management (PUM) strategies (cost‐sharing and administrative restriction processes) were assessed in another review in older adult populations (Maio 2005). Although PUM strategies involving caps or co‐payments reduced prescription medicines use and medicines costs, they also both increased health service use and may reduce health status among older adults. PUM strategies involving formularies may reduce costs without significant effects on health system use or health status.
Consumer system participation
We found no reviews addressing interventions for consumer system participation in medicines‐related activities, such as in research planning, or formulary or policy decisions.
Appendix 2. Abbreviations used
ACE inhibitors = Angiotensin‐Converting Enzyme Inhibitors
AED = Anti‐Epileptic Drug(s)
AGAS = Antiretroviral General Adherence Scale
AIDS = Acquired Immunodeficiency Syndrome
ALT = Alanine Aminotransferase Test (Liver function)
AM = Anti‐malarial medicine
AMI = Absolute Mean Increase
AMR = Absolute Mean Reduction
ARD = Adjusted Risk Difference
ARI = Absolute Risk Increase
ARR = Absolute Risk Reduction
ART = Anti‐Retroviral Therapy
BP = Blood Pressure
BC = Blood Cholesterol
CD4 = Cluster of differentiation 4 (T‐helper lymphocytes with CD4 cell marker)
CDSS = Computer Decision Support Systems
CGMS = Continuous Glucose Monitoring System
CI = Confidence Interval
COPD = Chronic Obstructive Pulmonary Disease
CPOE = Computer Physician Order Entry
CSII = Continuous Subcutaneous Insulin Infusion
DOT = Directly Observed Therapy
FEC = Forced Expiration Capacity
FEV1 = Forced Expiratory Volume (1 second)
GDR = Gradual Dose Reduction
H = Heterogeneity
HbA1c = Glycosylated haemoglobin
HAART = Highly Active Antiretroviral Therapy
HDL(‐C) = High Density Lipoprotein (Cholesterol)
HIV = Human Immunodeficiency Virus
hr = hour
HRT = Hormone Replacement Therapy
INR = International Normalised Ratio
Int(s) = Intervention(s)
ITS = Interrupted Time Series
LDL(‐C) = Low Density Lipoprotein (Cholesterol)
LHW = Lay Health Worker
MAI = Medication Appropriateness Index
MD = Mean Difference
MDI = Multiple Daily Insulin Injections
MEMS = Medication Event Monitoring System
mg/dL = milligrams per decilitre
MI = Mean Increase
mmHg = millimetres of mercury
mmol/l = millimoles per litre
MR = Mean Reduction
MSK = Musculoskeletal
NCA = Nurse‐Controlled Analgesia
NRT = Nicotine Replacement Therapy
NRTI = Nucleoside reverse transcriptase inhibitor
NNRTI = Non‐nucleoside reverse transcriptase inhibitor
NSAIDS = Non‐Steroidal Anti‐inflammatory Drugs
OR = Odds Ratio
PCA = Patient‐Controlled Analgesia
PI = Protease Inhibitor
POM = Patient’s Own Medicine
QoL = Quality of Life
RD = Risk Difference
RM = Repeated Measures
RR = Risk Ratio
SD = Standard Deviation
SMBG = Self Monitoring of Blood Glucose
SMI = Standardised Self‐Management Interview
SROM = Slow Release Oral Morphine
TB = Tuberculosis
TG = Triglycerides
VAS = Visual Analogue Scale
95% CI = 95% Confidence Interval
Differences between protocol and review
In the protocol (Ryan 2009) we planned to include only CDSR reviews; however given the substantial gaps in the evidence based on these reviews alone a decision was made retrospectively to additionally search for and select DARE reviews for inclusion in this overview. These DARE reviews were selected for inclusion in such a way as to give preference to inclusion of CDSR reviews, while maximising the spread of review‐level evidence on consumers' use of medicines as outlined in the methods of the overview.
In this update we have followed the same methods as outlined in the original version of the overview (Other published versions of this review), with two differences:
In the original version of this overview (Ryan 2011b), one author entered data from data extraction forms into RevMan and this was checked for accuracy by a second author working independently. In the update of this overview, one author entered data from spreadsheets or data extraction forms into RevMan and a random selection of reviews was checked for accuracy by a second author working independently.
The title of the overview has been changed with this update.
Large tables (Characteristics of included studies; Characteristics of excluded studies; and Table of results) have been removed from RevMan due to problems with display and are now housed on the CC&CRG website at http://cccrg.cochrane.org/consumers-clinicians-and-policymakers.
Contributions of authors
Rebecca Ryan contributed to: original overview: all stages. This update: review selection; data extraction and quality assessment; synthesis of results and writing the overview.
Nancy Santesso contributed to: original overview: all stages. This update: commenting on drafts.
Dianne Lowe contributed to: original overview: conduct and writing the overview. This update: review selection; data extraction and quality assessment; checking synthesis of results, writing and commenting on drafts.
Sophie Hill contributed to: original overview: all stages. This update: writing and commenting on drafts.
Jeremy Grimshaw contributed to: original overview: all stages. This update: commenting on drafts.
Megan Prictor: original overview: copyediting and organising layout of the overview. This update: data checking, copyediting and commenting on drafts.
Caroline Kaufman contributed to: original overview: writing of the protocol. This update: commenting on drafts.
Genevieve Cowie: this update: review selection; data extraction and quality assessment; commenting on drafts.
Michael Taylor: this update: review selection; data extraction and quality assessment.
Sources of support
Internal sources
No sources of support provided
External sources
-
Canadian Agency for Drugs and Technologies in Health, Canada
Supported the development and updating of the Rx for Change database, the consumer arm of which contributed to this overview. Salary support to RR, DL, GC, MT.
-
National Health and Medical Research Council, Australia
Salary support to RR, SH
-
Department of Health, Victoria, Australia
Salary support to MP, SH
Declarations of interest
RR: This work was completed by RR as part of her role as Research Fellow with the CC&CRG, funded by a Cochrane Infrastructure Grant provided by the National Health and Medical Research Council (NHMRC).
MP: As Managing Editor, MP was responsible for managing the editorial and peer review feedback process on this review. She was not responsible for deciding whether or not to publish the review.
SH: SH is Coordinating Editor of the Cochrane Consumers and Communication Review Group which approved publication of this overview on The Cochrane Library. She referred decisions concerning the publication of this overview to an editor who was not an overview author.
Other authors: None known.
Edited (no change to conclusions)
References
References to included reviews
Aaserud 2006
- Aaserud M, Austvoll-Dahlgren AAA, Kösters JP, Oxman AD, Ramsay C, Sturm H.Pharmaceutical policies: effects of reference pricing, other pricing, and purchasing policies. Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No: CD005979. [DOI: 10.1002/14651858.CD005979] [DOI] [PubMed] [Google Scholar]
Al‐aqeel 2011
- Al-aqeel S, Al-sabhan J.Strategies for improving adherence to antiepileptic drug treatment in patients with epilepsy. Cochrane Database of Systematic Reviews 2011, Issue 1. Art. No: CD008312. [DOI: 10.1002/14651858.CD008312.pub2] [DOI] [PubMed] [Google Scholar]
Amico 2006
- Amico KR, Harman JJ, Johnson BT.Efficacy of antiretroviral therapy adherence interventions: a research synthesis of trials, 1996 to 2004. Journal of Acquired Immune Deficiency Syndromes 2006;41(3):285-97. [DOI] [PubMed] [Google Scholar]
Argarwal 2011
- Argarwal R, Bills JE, Hecht TJW, Light RP.Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control. Hypertension 2011;57(1):29-38. [DOI] [PubMed] [Google Scholar]
Austvoll‐Dahlgren 2008
- Austvoll-Dahlgren AAA, Aaserud M, Vist GE, Ramsay C, Oxman AD, Sturm H, et al.Pharmaceutical policies: effects of cap and co-payment on rational drug use. Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No: CD007017. [DOI: 10.1002/14651858.CD007017] [DOI] [PubMed] [Google Scholar]
Bain‐Brickley 2011
- Bain-Brickley D, Butler LM, Kennedy GE, Rutherford GW.Interventions to improve adherence to antiretroviral therapy in children with HIV infection. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD009513. [DOI: 10.1002/14651858.CD009513] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bainbridge 2006
- Bainbridge D, Martin JE, Cheng DC.Patient-controlled versus nurse-controlled analgesia after cardiac surgery: a meta-analysis. Canadian Journal of Anaesthesia 2006;53(5):492-9. [DOI] [PubMed] [Google Scholar]
Bayoumi 2009
- Bayoumi I, Howard M, Holbrook A, Schabort I.Interventions to improve medication reconciliation in primary care. The Annals of Pharmacotherapy 2009;43(10):1667-75. [DOI] [PubMed] [Google Scholar]
Bennett 2009
- Bennett M, Bagnall A, Jose CS.How effective are patient-based educational interventions in the management of cancer pain? Systematic review and meta-analysis. Pain 2009;143(3):192-9. [DOI] [PubMed] [Google Scholar]
Bhogal 2006
- Bhogal S, Zemek R, Ducharme FM, Bhogal S, Zemek R, Ducharme FM.Written action plans for asthma in children. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No: CD005306. [DOI: 10.1002/14651858.CD005306.pub2] [DOI] [PubMed] [Google Scholar]
Bower 2006
- Bower P, Gilbody S, Richards D, Fletcher J, Sutton A, et al.Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. British Journal of Psychiatry 2006;189:484-93. [DOI] [PubMed] [Google Scholar]
Buckley 2010
- Buckley B, Byrne M, Smith S.Service organisation for the secondary prevention of ischaemic heart disease in primary care. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No: CD006772. [DOI: 10.1002/14651858.CD006772.pub2] [DOI] [PubMed] [Google Scholar]
Castelino 2009
- Castelino R, Bajorek B, Chen T.Targeting suboptimal prescribing in the elderly: a review of the impact of pharmacy services. The Annals of Pharmacotherapy 2009;43(6):1096-106. [DOI] [PubMed] [Google Scholar]
Chivu 2008
- Chivu CM, Tulchinsky TH, Soares-Weiser K, Braunstein R, Brezis M.A systematic review of interventions to increase awareness, knowledge, and folic acid consumption before and during pregnancy. American Journal of Health Promotion 2008;22(4):237-45. [DOI] [PubMed] [Google Scholar]
De Bleser 2009
- De Bleser L, Matteson M, Dobbels F, Russell C, De Geest S.Interventions to improve medication-adherence after transplantation: a systematic review. Transplant International 2009;22(8):780-97. [DOI] [PubMed] [Google Scholar]
Ford 2009
- Ford N, Nachega J, Engel M, Mills E.Directly observed antiretroviral therapy: a systematic review and meta-analysis of randomised clinical trials. Lancet 2009;374(9707):2064-71. [DOI] [PubMed] [Google Scholar]
Garcia‐Alamino 2010
- Garcia-Alamino JM, Ward AM, Alonso-Coello P, Perera R, Bankhead C, Fitzmaurice D, et al.Self-monitoring and self-management of oral anticoagulation. Cochrane Database of Systematic Reviews 2010, Issue 4. Art. No: CD003839. [DOI: 10.1002/14651858.CD003839.pub2] [DOI] [PubMed] [Google Scholar]
Gilbody 2006
- Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ.Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine 2006;166(21):2314-21. [DOI: 10.1001/archinte.166.21.2314] [DOI] [PubMed] [Google Scholar]
Giuffrida 1997
- Giuffrida A, Torgerson DJ.Should we pay the patient? Review of financial incentives to enhance patient compliance. BMJ 1997;315(7110):703-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gleeson 2009
- Gleeson T, Iversen MD, Avorn J, Brookhart AM, Katz JN, Losina E, et al.Interventions to improve adherence and persistence with osteoporosis medications: a systematic literature review. Osteoporosis International 2009;20(12):2127-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Golicki 2008
- Golicki DT, Golicka D, Groele L, Pankowska E.Continuous Glucose Monitoring System in children with type 1 diabetes mellitus: a systematic review and meta-analysis. Diabetologia 2008;51(2):233-40. [DOI] [PubMed] [Google Scholar]
Gray 2009
- Gray TA, Orton LC, Henson D, Harper R, Waterman H.Interventions for improving adherence to ocular hypotensive therapy. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD006132. [DOI: 10.1002/14651858.CD006132.pub2] [DOI] [PubMed] [Google Scholar]
Halpern 2011
- Halpern V, Lopez LM, Grimes DA, Gallo MF.Strategies to improve adherence and acceptability of hormonal methods of contraception. Cochrane Database of Systematic Reviews 2011, Issue 4. Art. No: CD004317. [DOI: 10.1002/14651858.CD004317.pub3] [DOI] [PubMed] [Google Scholar]
Haynes 2008
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X.Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No: CD000011. [DOI: 10.1002/14651858.CD000011.pub3] [DOI] [PubMed] [Google Scholar]
Haywood 2009
- Haywood CJ, Beach M, Lanzkron S, Strouse J, Wilson R, Park H.A systematic review of barriers and interventions to improve appropriate use of therapies for sickle cell disease. Journal of the National Medical Association 2009;101(10):1022-33. [DOI] [PubMed] [Google Scholar]
Holland 2008
- Holland R, Desborough J, Goodyer L, Hall S, Wright D, Loke YK.Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. British Journal of Clinical Pharmacology 2008;65(3):303-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jacobson 2005
- Jacobson VJ, Szilagyi P.Patient reminder and patient recall systems to improve immunization rates. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD003941. [DOI: 10.1002/14651858.CD003941.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jegu 2011
- Jegu J, Gallini A, Soler P, Montastruc JL, Lapeyre-Mestre M.Slow-release oral morphine for opioid maintenance treatment: a systematic review. British Journal of Clinical Pharmacology 2011;71(6):832-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koshman 2008
- Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT.Pharmacist care of patients with heart failure. Archives of Internal Medicine 2008;168(7):687-94. [DOI] [PubMed] [Google Scholar]
Lewin 2010
- Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, Wyk BE, et al.Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No: CD004015. [DOI: 10.1002/14651858.CD004015.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2008
- Liu Q, Abba K, Alejandria MM, Balanag VM, Berba RP, Lansang MA.Reminder systems and late patient tracers in the diagnosis and management of tuberculosis. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No: CD006594. [DOI: 10.1002/14651858.CD006594.pub2] [DOI] [PubMed] [Google Scholar]
Lummis 2006
- Lummis H, Sketris I, Veldhuyzen van Zanten S.Systematic review of the use of patients' own medications in acute care institutions. Journal of Clinical Pharmacy & Therapeutics 2006;31(6):541-63. [DOI] [PubMed] [Google Scholar]
Lutge 2012
- Lutge EE, Wiysonge CS, Knight SE, Volmink J.Material incentives and enablers in the management of tuberculosis. Cochrane Database of Systematic Reviews 2012, Issue 1. Art. No: CD007952. [DOI: 10.1002/14651858.CD007952.pub2] [DOI] [PubMed] [Google Scholar]
Machado 2007a
- Machado M, Bajcar J, Guzzo GC, Einarson TR.Sensitivity of patient outcomes to pharmacist interventions. Part I: systematic review and meta-analysis in diabetes management. Annals of Pharmacotherapy 2007;41(10):1569-82. [DOI] [PubMed] [Google Scholar]
Machado 2007b
- Machado M, Bajcar J, Guzzo GC, Einarson TR.Sensitivity of patient outcomes to pharmacist interventions. Part II: systematic review and meta-analysis in hypertension management. Annals of Pharmacotherapy 2007;41(11):1770-81. [DOI] [PubMed] [Google Scholar]
Machado 2008
- Machado M, Nassor N, Bajcar JM, Guzzo GC, Einarson TR.Sensitivity of patient outcomes to pharmacist interventions. Part III: systematic review and meta-analysis in hyperlipidemia management. Annals of Pharmacotherapy 2008;42(9):1195-207. [DOI] [PubMed] [Google Scholar]
Maglione 2002
- Maglione MA, Stone EG, Shekelle PG.Mass mailings have little effect on utilization of influenza vaccine among Medicare beneficiaries. American Journal of Preventive Medicine 2002;23(1):43-6. [DOI] [PubMed] [Google Scholar]
Mahtani 2011
- Mahtani KR, Heneghan CJ, Glasziou PP, Perera R.Reminder packaging for improving adherence to self-administered long-term medications. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD005025. [DOI: 10.1002/14651858.CD005025.pub3] [DOI] [PubMed] [Google Scholar]
Maio 2005
- Maio V, Pizzi L, Roumm AR, Clarke J, Goldfarb NI, Nash DB, et al.Pharmacy utilization and the Medicare Modernization Act. Milbank Quarterly 2005;83(1):101-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mbuba 2008
- Mbuba CK, Ngugi AK, Newton CR, Carter JA.The epilepsy treatment gap in developing countries: a systematic review of the magnitude, causes, and intervention strategies. Epilepsia 2008;49(9):1491-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
McIntosh 2006
- McIntosh AM, Conlon L, Lawrie SM, Stanfield AC, McIntosh AM, Conlon L, et al.Compliance therapy for schizophrenia. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No: CD003442. [DOI: 10.1002/14651858.CD003442.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Misso 2010
- Misso ML, Egberts K, Page M, O'Connor D, Shaw J.Continuous subcutaneous insulin infusion (CSII) versus multiple insulin injections for type 1 diabetes mellitus. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD005103. [DOI: 10.1002/14651858.CD005103.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Molife 2009
- Molife C, Lee L, Shi L, Sawhney M, Lenox S.Assessment of patient-reported outcomes of insulin pen devices versus conventional vial and syringe. Diabetes Technology & Therapeutics 2009;11(8):529-38. [DOI] [PubMed] [Google Scholar]
Mollon 2009
- Mollon B, Chong J Jr, Holbrook AM, Sung M, Thabane L, Foster G.Features predicting the success of computerized decision support for prescribing: a systematic review of randomized controlled trials. BMC Medical Informatics and Decision Making 2009;9(11):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrison 2001
- Morrison A, Wertheimer AI.Evaluation of studies investigating the effectiveness of pharmacists' clinical services. American Journal of Health-System Pharmacy 2001;58(7):569-77. [DOI] [PubMed] [Google Scholar]
Nicolson 2009
- Nicolson D, Knapp P, Raynor DK, Spoor P.Written information about individual medicines for consumers. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD002104. [DOI: 10.1002/14651858.CD002104.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nishtala 2008
- Nishtala PS, McLachlan A, Bell JS, Chen TF.Psychotropic prescribing in long-term care facilities: impact of medication reviews and educational interventions. American Journal of Geriatric Psychiatry 2008;16(8):621-32. [DOI] [PubMed] [Google Scholar]
Nkansah 2010
- Nkansah N, Mostovetsky O, Yu C, Chheng T, Beney J, Bond CM, et al.Effect of outpatient pharmacists' non-dispensing roles on patient outcomes and prescribing patterns. Cochrane Database of Systematic Reviews 2010, Issue 7. Art. No: CD000336. [DOI: 10.1002/14651858.CD000336.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Odegard 2007
- Odegard PS, Capoccia K.Medication taking and diabetes: a systematic review of the literature. The Diabetes Educator 2007;33(6):1014-29. [DOI] [PubMed] [Google Scholar]
Olthoff 2005
- Olthoff CM, Schouten JS, de Borne BW, Webers CA.Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology 2005;112(6):953-61. [DOI] [PubMed] [Google Scholar]
Orton 2005
- Orton L, Barnish G.Unit-dose packaged drugs for treating malaria. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD004614. [DOI: 10.1002/14651858.CD004614.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oyo‐Ita 2008
- Oyo-Ita A, Nwachukwa CE, Oringanje C, Meremikwu MM.Interventions for improving coverage of child immunization in low- and middle-income countries. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD008145. [DOI: 10.1002/14651858.CD008145.pub2] [DOI] [PubMed] [Google Scholar]
Pankowska 2009
- Pankowska E, Blazik M, Dziechciarz P, Szypowska A, Szajewska H.Continuous subcutaneous insulin infusion vs. multiple daily injections in children with type 1 diabetes: a systematic review and meta-analysis of randomized control trials. Pediatric Diabetes 2009;10(1):52-8. [DOI] [PubMed] [Google Scholar]
Parr 2009
- Parr JM, Kavanagh DJ, Cahill L, Mitchell G, Young RM.Effectiveness of current treatment approaches for benzodiazepine discontinuation: a meta-analysis. Addiction 2009;104(4):13-24. [DOI] [PubMed] [Google Scholar]
Polis 2007
- Polis CB, Schaffer K, Blanchard K, Glasier A, Harper CC, Grimes DA.Advance provision of emergency contraception for pregnancy prevention: a meta-analysis. Obstetrics and Gynecology 2007;110(6):1379-88. [DOI] [PubMed] [Google Scholar]
Ranji 2008
- Ranji SR, Steinman MA, Shojania KG, Gonzales R.Interventions to reduce unnecessary antibiotic prescribing: a systematic review and quantitative analysis. Medical Care 2008;46(8):847-62. [DOI] [PubMed] [Google Scholar]
Roughead 2005
- Roughead EE, Semple SJ, Vitry AI.Pharmaceutical care services: a systematic review of published studies, 1990 to 2003, examining effectiveness in improving patient outcomes. International Journal of Pharmacy Practice 2005;13(1):53-70. [Google Scholar]
Royal 2006
- Royal S, Smeaton L, Avery AJ, Hurwitz B, Sheikh A.Interventions in primary care to reduce medication related adverse events and hospital admissions: systematic review and meta-analysis. Quality and Safety in Health Care 2006;15(1):23-31. [DOI] [PMC free article] [PubMed]
Rueda 2006
- Rueda S, Park-Wyllie LY, Bayoumi AM, Tynan AM, Antoniou TA, Rourke SB, et al.Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No: CD001442. [DOI: 10.1002/14651858.CD001442.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Russell 2006
- Russell CL, Conn VS, Jantarakupt P.Older adult medication compliance: integrated review of randomized controlled trials. American Journal of Health Behavior 2006;30(6):636-50. [DOI] [PubMed] [Google Scholar]
Saini 2009
- Saini S, Schoenfeld P, Kaulback K, Dubinsky M.Effect of medication dosing frequency on adherence in chronic diseases. American Journal of Managed Care 2009;15(6):e22-e33. [PubMed] [Google Scholar]
Schedlbauer 2010
- Schedlbauer A, Davies P, Fahey T.Interventions to improve adherence to lipid lowering medication. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No: CD004371. [DOI: 10.1002/14651858.CD004371.pub3] [DOI] [PubMed] [Google Scholar]
Schroeder 2004
- Schroeder K, Fahey T, Ebrahim S.Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database of Systematic Reviews 2004, Issue 2. Art. No: CD004804. [DOI: 10.1002/14651858.CD004804] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2009
- Smith LA, Jones C, Meek S, Webster J.Review: Provider practice and user behavior interventions to improve prompt and effective treatment of malaria: do we know what works? American Journal of Tropical Medicine and Hygiene 2009;80(3):326-35. [PubMed] [Google Scholar]
Spurling 2007
- Spurling GKP, Del Mar CB, Dooley L, Foxlee R.Delayed antibiotics for respiratory infections. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD004417. [DOI: 10.1002/14651858.CD004417.pub3] [DOI] [PubMed] [Google Scholar]
Stevenson 2004
- Stevenson FA, Cox K, Britten N, Dundar Y.A systematic review of the research on communication between patients and health care professionals about medicines: the consequences for concordance. Health Expectations 2004;7(3):235-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stone 2002
- Stone EG, Morton SC, Hulscher ME, Maglione MA, Roth EA, Grimshaw JM, et al.Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Annals of Internal Medicine 2002;136(9):641-51. [DOI] [PubMed] [Google Scholar]
Thomas 2010
- Thomas RE, Russell M, Lorenzetti D.Interventions to increase influenza vaccination rates of those 60 years and older in the community. Cochrane Database of Systematic Reviews 2010, Issue 9. Art. No: CD005188. [DOI: 10.1002/14651858.CD005188.pub2] [DOI] [PubMed] [Google Scholar]
van Eijken 2003
- Eijken M, Tsang S, Wensing M, Smet PA, Grol RP.Interventions to improve medication compliance in older patients living in the community: a systematic review of the literature. Drugs and Aging 2003;20(3):229-40. [DOI] [PubMed] [Google Scholar]
Van Wijk 2005
- Van Wijk BL, Klungel OH, Heerdink ER, Boer A.Effectiveness of interventions by community pharmacists to improve patient adherence to chronic medication: a systematic review. Annals of Pharmacotherapy 2005;39(2):319-28. [DOI] [PubMed] [Google Scholar]
Vergouwen 2003
- Vergouwen AC, Bakker A, Katon WJ, Verheij TJ, Koerselman F.Improving adherence to antidepressants: a systematic review of interventions. Journal of Clinical Psychiatry 2003;64(12):1415-20. [DOI] [PubMed] [Google Scholar]
Vermeire 2005
- Vermeire E, Wens J, Van Royen P, Biot Y, Hearnshaw H, Lindenmeyer A.Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD003638. [DOI: 10.1002/14651858.CD003638.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Volmink 2007
- Volmink J, Garner P.Directly observed therapy for treating tuberculosis. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD003343. [DOI: 10.1002/14651858.CD003343.pub3] [DOI] [PubMed] [Google Scholar]
Wright 2006
- Wright J, Emerson A, Stephens M, Lennan E.Hospital inpatient self-administration of medicine programmes: a critical literature review. Pharmacy World & Science 2006;28(3):140-51. [DOI] [PubMed] [Google Scholar]
Yankova 2008
- Yankova Z.Patients' knowledge of patient controlled analgesia (PCA) and their experience of postoperative pain relief: a review of the impact of structured preoperative education. Journal of Advanced Perioperative Care 2008;3(3):91-9. [Google Scholar]
Zygmunt 2002
- Zygmunt A, Olfson M, Boyer CA, Mechanic D.Interventions to improve medication adherence in schizophrenia. American Journal of Psychiatry 2002;159(10):1653-64. [DOI] [PubMed] [Google Scholar]
References to excluded reviews
Akl 2011a
- Akl EA, Oxman AD, Herrin J, Vist GE, Terrenato I, Sperati F, et al.Framing of health information messages. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD006777. [DOI: 10.1002/14651858.CD006777.pub2] [DOI] [PubMed] [Google Scholar]
Akl 2011b
- Akl EA, Oxman AD, Herrin J, Vist GE, Terrenato I, Sperati F, et al.Using alternative statistical formats for presenting risks and risk reductions. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No: CD006776. [DOI: 10.1002/14651858.CD006776.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Al‐Ansary 2011
- Al-Ansary L, Farmer A, Hirst J, Roberts N, Glasziou P, Perera R, et al.Point-of-care testing for Hb A1c in the management of diabetes: a systematic review and meta-analysis. Clinical Chemistry 2011;57(4):568-76. [DOI] [PubMed] [Google Scholar]
Allemann 2009
- Allemann S, Houriet C, Diem P, Stettler C.Self-monitoring of blood glucose in non-insulin treated patients with type 2 diabetes: a systematic review and meta-analysis. Current Medical Research Opinion 2009;25(12):2903-13. [DOI] [PubMed] [Google Scholar]
Allen 2009
Alvarez‐Jimenez 2011
- Alvarez-Jiménez M, Parker AG, Hetrick SE, McGorry PD, Gleeson JF.Preventing the second episode: a systematic review and meta-analysis of psychosocial and pharmacological trials in first-episode psychosis. Schizophrenia Bulletin 2011;37(3):619-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ammenwerth 2008
- Ammenwerth E, Schnell-Inderst P, Machan C, Siebert U.The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. Journal of the American Medical Informatics Association 2008;15(5):585-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ara 2004
- Ara S.Literature review of cardiovascular disease management programs in managed care populations. Journal of Managed Care Pharmacy 2004;10(4):326-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Armour 2005
- Armour TA, Norris SL, Jack L Jr, Zhang X, Fisher L.The effectiveness of family interventions in people with diabetes mellitus: a systematic review. Diabetic Medicine 2005 Oct;22(10):1295-305. [DOI] [PubMed] [Google Scholar]
Arnold 2005
- Arnold SR, Straus SE.Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No: CD003539. [DOI: 10.1002/14651858.CD003539.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Arroll 2003
- Arroll B, Kenealy T, Kerse N.Do delayed prescriptions reduce antibiotic use in respiratory tract infections: a systematic review. The British Journal of General Practice 2003;53(496):871-7. [PMC free article] [PubMed] [Google Scholar]
Asfar 2011
- Asfar T, Ebbert JO, Klesges RC, Relyea GE.Do smoking reduction interventions promote cessation in smokers not ready to quit? Addictive Behaviours 2011;36(7):764-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bailey 2009
- Bailey EJ, Cates CJ, Kruske SG, Morris PS, Brown N, Chang AB.Culture-specific programs for children and adults from minority groups who have asthma. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD006580. [DOI: 10.1002/14651858.CD006580.pub4] [DOI] [PubMed] [Google Scholar]
Banham 2010
- Banham L, Gilbody S.Smoking cessation in severe mental illness: what works? Addiction 2010;105(7):1176-89. [DOI] [PubMed] [Google Scholar]
Baradaran 2010
- Baradaran HR, Shams-Hosseini N, Noori-Hekmat S, Tehrani-Banihashemi A, Khamseh ME.Effectiveness of diabetes educational interventions in Iran: a systematic review. Diabetes Technology and Therapeutics 2010;12(4):317-31. [DOI] [PubMed] [Google Scholar]
Barlow 2010
- Barlow C, Cooke D, Mulligan K, Beck E, Newman S.A critical review of self-management and educational interventions in inflammatory bowel disease. Gastroenterology Nursing 2010;33(1):11-8. [DOI] [PubMed] [Google Scholar]
Barnard 2007
- Barnard L, Ferriday D, Guenther N, Strauss B, Balen AH, Dye L.Quality of life and psychological well being in polycystic ovary syndrome. Human Reproduction 2007;22(8):2279-86. [DOI] [PubMed] [Google Scholar]
Barnard 2010
- Barnard K, Thomas S, Royle P, Noyes K, Waugh N.Fear of hypoglycaemia in parents of young children with type 1 diabetes: a systematic review. BMC Pediatrics 2010;10:50-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Batty 2010
- Batty C.Systematic review: interventions intended to reduce admission to hospital of older people. International Journal of Therapy and Rehabilitation 2010;17(6):301-22. [Google Scholar]
Baumeister 2011
- Baumeister H, Hutter N, Bengel J.Psychological and pharmacological interventions for depression in patients with coronary artery disease. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD008012. [DOI: 10.1002/14651858.CD008012.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Belling 2009
- Belling R, McLaren S, Woods L.Specialist nursing interventions for inflammatory bowel disease. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No: CD006597. [DOI: 10.1002/14651858.CD006597.pub2] [DOI] [PubMed] [Google Scholar]
Beney 2000
- Beney J, Bero LA, Bond C.Expanding the roles of outpatient pharmacists: effects on health services utilisation, costs, and patient outcomes. Cochrane Database of Systematic Reviews 2000, Issue 2. Art. No: CD000336. [DOI: 10.1002/14651858.CD000336] [DOI] [PubMed] [Google Scholar]
Berkman 2011
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K.Low health literacy and health outcomes: an updated systematic review. Annals of Internal Medicine 2011;155(2):97-107. [DOI] [PubMed] [Google Scholar]
Blackstock 2006
- Blackstock F, Webster K.Disease-specific health education for COPD: a systematic review of changes in health outcomes. Health Education Research 2007 Oct;22(5):703-17. [DOI] [PubMed] [Google Scholar]
Blaya 2010
- Blaya JA, Fraser HS, Holt B.E-health technologies show promise in developing countries. Health Affairs (Millwood) 2010;29(2):244-51. [DOI: ] [DOI] [PubMed] [Google Scholar]
Bloomfield 2011
- Bloomfield HE, Krause A, Greer N, Taylor BC, MacDonald R, Rutks I, et al.Meta-analysis: effect of patient self-testing and self-management of long-term anticoagulation on major clinical outcomes. Annals of Internal Medicine 2011;154(7):472-82. [DOI] [PubMed] [Google Scholar]
Boonacker 2010
- Boonacker CW, Hoes AW, Dikhoff MJ, Schilder AG, Rovers MM.Interventions in health care professionals to improve treatment in children with upper respiratory tract infections. International Journal of Pediatric Otorhinolaryngology 2010;74(10):1113-21. [DOI: 10.1016/j.ijporl.2010.07.008] [DOI] [PubMed] [Google Scholar]
Bordley 2000
- Bordley WC, Chelminski A, Margolis PA, Kraus R, Szilagyi PG, Vann JJ.The effect of audit and feedback on immunization delivery: a systematic review. American Journal of Preventive Medicine 2000 May;18(4):343-50. [DOI] [PubMed] [Google Scholar]
Boren 2009a
- Boren SA, Wakefield BJ, Gunlock TL, Wakefield DS.Heart failure self-management education: a systematic review of the evidence. International Journal of Evidence-Based Healthcare September 2009;7(3):159-68. [DOI] [PubMed] [Google Scholar]
Boren 2009b
- Boren SA, Puchbauer AM, Williams F.Computerized prompting and feedback of diabetes care: a review of the literature. Journal of Diabetes Science and Technology 2010;3(4):944-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borkhoff 2011
- Borkhoff CM, Wieland ML, Myasoedova E, Ahmad Z, Welch V, Hawker GA, et al.Reaching those most in need: a scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Research 2011;63(1):39-52. [DOI] [PubMed] [Google Scholar]
Bosch‐Capblanch 2007
- Bosch-Capblanch X, Abba K, Prictor M, Garner P.Contracts between patients and healthcare practitioners for improving patients' adherence to treatment, prevention and health promotion activities. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No: CD004808. [DOI: 10.1002/14651858.CD004808.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bosch‐Capblanch 2011
- Bosch-Capblanch X, Liaqat S, Garner P.Managerial supervision to improve primary health care in low- and middle-income countries. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD006413. [DOI: 10.1002/14651858.CD006413.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyd 2009
- Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M.Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD001290. [DOI: 10.1002/14651858.CD001290.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyle 2011
- Boyle R, Solberg L, Fiore M.Use of electronic health records to support smoking cessation. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD008743. [DOI: 10.1002/14651858.CD008743.pub2] [DOI] [PubMed] [Google Scholar]
Bradley 2008
- Bradley PM, Lindsay B.Care delivery and self-management strategies for adults with epilepsy. Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No: CD006244. [DOI: 10.1002/14651858.CD006244.pub2] [DOI] [PubMed] [Google Scholar]
Bravata 2007
- Bravata DM, Sundaram V, Lewis R, Gienger A, Gould MK, McDonald KM, et al.Closing the quality gap: a critical analysis of quality improvement strategies. Volume 5: Asthma care. Agency for Healthcare Research and Quality 2007:199. [PubMed]
Bray 2010
- Bray EP, Holder R, Mant J, McManus RJ.Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Annals of Medicine 2010;42(5):371-86. [DOI] [PubMed] [Google Scholar]
Bridle 2005
- Bridle C, Riemsma RP, Pattenden J, Sowden AJ, Mather L, Watt IS, et al.Systematic review of the effectiveness of health behavior interventions based on the transtheoretical model. Psychology and Health 2005 June;20(3):283-301. [Google Scholar]
Briss 2000
- Briss PA, Rodewald LE, Hinman AR, Shefer AM, Strikas RA, Bernier RR, et al.Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. American Journal of Preventive Medicine 2000;18(1):97-140. [DOI] [PubMed] [Google Scholar]
Brown 2004
- Brown HC, Smith HJ.Giving women their own case notes to carry during pregnancy. Cochrane Database of Systematic Reviews 2004, Issue 2. Art. No: CD002856. [DOI: 10.1002/14651858.CD002856.pub2] [DOI] [PubMed] [Google Scholar]
Brown 2011
- Brown JPR, Clark AM, Dalal H, Welch K, Taylor RS.Patient education in the management of coronary heart disease. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD008895. [DOI: 10.1002/14651858.CD008895.pub2] [DOI] [PubMed] [Google Scholar]
Brownstein 2007
- Brownstein JN, Chowdhury FM, Norris SL, Horsley T, Jack L Jr, Zhang X, et al.Effectiveness of community health workers in the care of people with hypertension. American Journal of Preventive Medicine May 2007;32(5):435-47. [DOI] [PubMed] [Google Scholar]
Bunn 2004
- Bunn F, Byrne G, Kendall S.Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database of Systematic Reviews 4, Issue 3. Art. No: CD004180. [DOI: 10.1002/14651858.CD004180.pub2] [DOI] [PubMed] [Google Scholar]
Burton 2010
- Burton A, Marougka S, Priebe S.Do financial incentives increase treatment adherence in people with severe mental illness? A systematic review. Epidemiologia e Psichiatria Sociale 2010;19(3):233-42. [PubMed] [Google Scholar]
Cabana 2004
- Cabana MD, Jee SH.Does continuity of care improve patient outcomes? Journal of Family Practice 2004;53 (12):974-80. [PubMed] [Google Scholar]
Cabassa 2007
- Cabassa LJ, Hansen MC.A systematic review of depression treatments in primary care for Latino adults. Research on Social Work Practice 2007;17:494. [Google Scholar]
Cameron 2010
- Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG et al.Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD005465. [DOI: 10.1002/14651858.CD005465.pub2] [DOI] [PubMed] [Google Scholar]
Cape 2010
- Cape J, Whittington C, Bower P.What is the role of consultation-liaison psychiatry in the management of depression in primary care? A systematic review and meta-analysis. General Hospital Psychiatry 2010;32(3):246-54. [DOI] [PubMed] [Google Scholar]
Carson 2012
- Carson KV, Brinn MP, Labiszewski NA, Peters M, Chang AB, Veale A, et al.Interventions for tobacco use prevention in Indigenous youth. Cochrane Database of Systematic Reviews 2012, Issue 8. Art. No: CD009325. [DOI: 10.1002/14651858.CD009325.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
Carter 2009
- Carter BL, Rogers M, Daly J, Zheng S, James PA.The potency of team-based care interventions for hypertension. Archives of Internal Medicine 2009;169(19):1748-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan 2011
- Chan RJ, Webster J, Marquart L.Information interventions for orienting patients and their carers to cancer care facilities. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD008273. [DOI: 10.1002/14651858.CD008273.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2007
- Chang AB, Taylor B, Masters IB, Laifoo Y, Brown ADH.Indigenous healthcare worker involvement for Indigenous adults and children with asthma. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD006344. [DOI: 10.1002/14651858.CD006344.pub2] [DOI] [PubMed] [Google Scholar]
Chang 2010
- Chang L, Harris J, Humphreys E.Optimal monitoring strategies for guiding when to switch first-line antiretroviral therapy regimens for treatment failure in adults and adolescents living with HIV in low-resource settings. Cochrane Database of Systematic Reviews 2010, Issue 4. Art. No: CD008494. [DOI: 10.1002/14651858.CD008494] [DOI] [PubMed] [Google Scholar]
Chisholm 2008
- Chisholm SS, Taylor SL, Balkrishnan R, Feldman SR.Written action plans: potential for improving outcomes in children with atopic dermatitis. Journal of the American Academy of Dermatology 2008 October;58(4):677-83. [DOI] [PubMed] [Google Scholar]
Chisholm‐Burns 2010
- Chisholm-Burns MA, Kim Lee J, Spivery CA, Slack M, Herrier RN, Hall-Lipsy E, et al.US pharmacists' effect as team members on patient care: systematic review and meta-analyses. Medical Care 2010;48(10):923-33. [DOI] [PubMed] [Google Scholar]
Christensen 2007
- Christensen T, Johnsen S, Hjortdal V, Hasenkam J.Self-management of oral anticoagulant therapy. International Journal of Cardiology 2007;118(1):54-61. [DOI] [PubMed] [Google Scholar]
Churchill 2009
- Churchill JN, Ruppe RL, Smaldone A.Use of continuous insulin infusion pumps in young children with type 1 diabetes: a systematic review. Journal of Pediatric Health Care 2009;23(3):173-9. [DOI] [PubMed] [Google Scholar]
Clar 2007
- Clar C, Waugh N, Thomas S.Routine hospital admission versus out-patient or home care in children at diagnosis of type 1 diabetes mellitus. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No: CD004099. [DOI: 10.1002/14651858.CD004099.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2007
- Clark RA, Inglis SC, McAlister FA, Cleland JCF, Stewart S.Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ 2007;334:942. [DOI: 10.1136/bmj.39156.536968.55] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clark 2010
- Clark CE, Smith LF, Taylor RS, Campbell JL.Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ 2010;341(c3995). [DOI: 10.1136/bmj.c3995] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clement 2009
- Clement S, Ibrahim S, Crichton N, Wolf M, Rowlands G.Complex interventions to improve the health of people with limited literacy: a systematic review. Patient Education and Counseling 2009;75(3):340-51. [DOI] [PubMed] [Google Scholar]
Coffman 2009
- Coffman JM, Cabana MD, Yelin EH.Do school-based asthma education programs improve self-management and health outcomes? Pediatrics 2009;124(2):729-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cole‐Lewis 2010
- Cole-Lewis H, Kershaw T.Text messaging as a tool for behaviour change in disease prevention and management. Epidemiologic Reviews 2010;32(1):56-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coleman 2010
- Coleman T, Agboola S, Leonardi-Bee J, Taylor M, McEwan A, McNeill A.Relapse prevention in UK Stop Smoking Services: current practice, systematic reviews of effectiveness and cost-effectiveness analysis. Health Technology Assessment 2010;14(49):1-152, iii – iv. [DOI] [PubMed] [Google Scholar]
Concha 2009
- Concha JB, Kravitz HM, Chin MH, Kelley MA, Chavez N, Johnson TP.Review of type 2 diabetes management interventions for addressing emotional well-being in Latinos. Diabetes Educator 2009;35(6):941-58. [DOI] [PubMed] [Google Scholar]
Connock 2007
- Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anticoagulation therapy: a systematic review and economic modelling. Health Technology Assessment October 2007;11(38):iii-iv, ix-66. [DOI] [PubMed]
Connor 2004
- Connor J, Rafter N, Rodgers A.Do fixed-dose combination pills or unit-of-use packaging improve adherence? A systematic review. Bulletin of the World Health Organization 2004;82(12):935-9. [PMC free article] [PubMed] [Google Scholar]
Cooper 2006
- Cooper C, Wheeler DM, Woolfenden SR, Boss T, Piper S.Specialist home-based nursing services for children with acute and chronic illnesses. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD004383. [DOI: 10.1002/14651858.CD004383.pub2] [DOI] [PubMed] [Google Scholar]
Coren 2010
- Coren E, Hutchfield J, Thomae M, Gustafsson C.Parent training support for intellectually disabled parents. Cochrane Database of Systematic Reviews 2010, Issue 6. Art. No: CD007987. [DOI: 10.1002/14651858.CD007987.pub2] [DOI] [PubMed] [Google Scholar]
Costello 2004
- Costello I, Wong IC, Nunn AJ.A literature review to identify interventions to improve the use of medicines in children. Child: Care, Health & Development 2004;30(6):647-65. [DOI] [PubMed] [Google Scholar]
Costello 2008
- Costello E, Edelstein J.Update on falls prevention for community-dwelling older adults: review of single and multifactorial intervention programs. Journal of Rehabilitation Research and Development 2008;45(8):1135-52. [PubMed] [Google Scholar]
Cote 2005
- Cote JK, Godin G.Efficacy of interventions in improving adherence to antiretroviral therapy. International Journal of STD & AIDS 2005;16(5):335-43. [DOI] [PubMed] [Google Scholar]
Cox 2008
- Cox HS, Morrow M, Deutschmann PW.Long term efficacy of DOTS regimens for tuberculosis: systematic review. BMJ 2008;336(7642):484-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Craven 2006
- Craven MA, Bland R.Better practices in collaborative mental health care: an analysis of the evidence base. Canadian Journal of Psychiatry 2006 May;51(6 Suppl 1):7S-72S. [PubMed] [Google Scholar]
Currell 2000
- Currell R, Urquhart C, Wainwright P, Lewis R.Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2000, Issue 2. Art. No: CD002098. [DOI: 10.1002/14651858.CD002098] [DOI] [PubMed] [Google Scholar]
Cushing 2010
- Cushing CC, Steele RG.A meta-analytic review of eHealth interventions for pediatric health promoting and maintaining behaviors. Journal of Pediatric Psychology 2010;35(9):937-49. [DOI] [PubMed] [Google Scholar]
Cutrona 2010
- Cutrona SL, Choudhry NK, Fischer MA, Servi A, Liberman JN, Brennan TA, et al.Modes of delivery for interventions to improve cardiovascular medication adherence. American Journal of Managed Care 2010;16(12):929-42. [PMC free article] [PubMed] [Google Scholar]
Dalal 2010
- Dalal HM, Zawada A, Jolly K, Moxham T, Taylor RS.Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ 2010;340. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dale 2008
- Dale J, Caramlau IO, Lindenmeyer A, Williams SM.Peer support telephone calls for improving health. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No: CD006903. [DOI: 10.1002/14651858.CD006903.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dalton 2008
- Dalton JE.Web-based care for adults with type 2 diabetes. Canadian Journal of Dietetic Practice and Research 2008;69(4):185-91. [DOI] [PubMed] [Google Scholar]
Davey 2005
- Davey P, Brown E, Fenelon L, Finch R, Gould I, Hartman G, et al.Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No: CD003543. [DOI: 10.1002/14651858.CD003543.pub2] [DOI] [PubMed] [Google Scholar]
Deakin 2005
- Deakin T, McShane CE, Cade JE, Williams RD.Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD003417. [DOI: 10.1002/14651858.CD003417.pub2] [DOI] [PubMed] [Google Scholar]
Dean 2010
- Dean AJ, Walters J, Hall A.A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Archives of Disease in Childhood 2010;95(9):717-23. [DOI] [PubMed] [Google Scholar]
de Belvis 2009
- Belvis AG, Pelone, Biasco A, Ricciardi W, Volpe M.Can primary care professionals' adherence to Evidence Based Medicine tools improve quality of care in type 2 diabetes mellitus? A systematic review. Diabetes Research and Clinical Practice 2009;85(2):119-31. [DOI] [PubMed] [Google Scholar]
Deenadayalan 2010
- Deenadayalan Y, Perraton L, Machotka Z, Kumar S.Day therapy programs for adolescents with mental health problems: a systematic review. Internet Journal of Allied Health Sciences and Practice 2010;8(1):1-14. [Google Scholar]
Desplenter 2006
- Desplenter FMA, Simoens S, Laekeman G.The impact of informing psychiatric patients about their medication. Pharmacy World & Science 2006;28(6):329-41. [DOI] [PubMed] [Google Scholar]
Dexheimer 2008
- Dexheimer JW, Talbot TR, Sanders DL, Rosenbloom ST, Aronsky D.Prompting clinicians about preventive care measures: a systematic review of randomized controlled trials. Journal of the American Medical Informatics Association May-June 2008;15(3):311-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dieterich 2010
- Dieterich M, Irving CB, Park B, Marshall M.Intensive case management for severe mental illness. Cochrane Database of Systematic Reviews 2010, Issue 10. Art. No: CD007906. [DOI: 10.1002/14651858.CD007906.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ditewig 2010
- Ditewig JB, Blok H, Havers J, Veenendaal H.Effectiveness of self-management interventions on mortality, hospital readmissions, chronic heart failure hospitalization rate and quality of life in patients with chronic heart failure: a systematic review. Patient Education and Counseling 2010;78(3):297-315. [DOI] [PubMed] [Google Scholar]
Doggett 2005
- Doggett C, Burrett S, Osborn DA.Home visits during pregnancy and after birth for women with an alcohol or drug problem. Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No: CD004456. [DOI: 10.1002/14651858.CD004456.pub2] [DOI] [PubMed] [Google Scholar]
Dolan 2008
- Dolan G, Smith LA, Collins S, Plumb JM.Effect of setting, monitoring intensity and patient experience on anticoagulation control: a systematic review and meta-analysis of the literature. Current Medical Research and Opinion May 2008;24(5):1459-72. [DOI] [PubMed] [Google Scholar]
Dolder 2003
- Dolder CR, Lacro JP, Leckband S, Jeste DV.Interventions to improve antipsychotic medication adherence: review of recent literature. Journal of Clinical Psychopharmacology 2003;23(4):389-99. [DOI] [PubMed] [Google Scholar]
Donald 2005
- Donald M, Dowera J, Kavanagh D.Integrated versus non-integrated management and care for clients with co-occurring mental health and substance use disorders: a qualitative systematic review of randomised controlled trials. Social Science & Medicine 2005;60(6):1371-83. [DOI] [PubMed] [Google Scholar]
Dorresteijn 2011
- Dorresteijn JAN, Kriegsman DMW, Valk GD.Complex interventions for preventing diabetic foot ulceration. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD007610. [DOI: 10.1002/14651858.CD007610.pub2] [DOI] [PubMed] [Google Scholar]
Duke 2009
- Duke SAS, Colagiuri S, Colagiuri R.Individual patient education for people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No: CD005268. [DOI: 10.1002/14651858.CD005268.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duncan 2010
- Duncan E, Best C, Hagen S.Shared decision making interventions for people with mental health conditions. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD007297. [DOI: 10.1002/14651858.CD007297.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Durrani 2009
- Durrani H, Khoja S.A systematic review of the use of telehealth in Asian countries. Journal of Telemedicine and Telecare 2009;15(4):175-81. [DOI] [PubMed] [Google Scholar]
Ebrahim 2006
- Ebrahim S, Beswick A, Burke M, Davey Smith G.Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD001561. [DOI: 10.1002/14651858.CD001561.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Effing 2007
- Effing T, Monninkhof EEM, Valk PP, Zielhuis GGA, Walters EH, Palen JJ, et al.Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD002990. [DOI: 10.1002/14651858.CD002990.pub2] [DOI] [PubMed] [Google Scholar]
Ersser 2007
- Ersser SJ, Latter S, Sibley A, Satherley PA, Welbourne S.Psychological and educational interventions for atopic eczema in children. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD004054. [DOI: 10.1002/14651858.CD004054.pub2] [DOI] [PubMed] [Google Scholar]
Eslami 2009
- Eslami S, Abu-Hanna A, Jonge E, Keizer NF.Tight glycemic control and computerized decision-support systems: a systematic review. Intensive Care Medicine 2009;35(9):1505-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fahey 2005
- Fahey T, Schroeder K, Ebrahim S.Educational and organisational interventions used to improve the management of hypertension in primary care: a systematic review. British Journal of General Practice 2005 Nov;55(520):875-82. [PMC free article] [PubMed] [Google Scholar]
Fahey 2006
- Fahey T, Schroeder K, Ebrahim S.Interventions used to improve control of blood pressure in patients with hypertension . Cochrane Database of Systematic Reviews 2006, Issue 2. Art. No: CD005182. [DOI: 10.1002/14651858.CD005182.pub2] [DOI] [PubMed] [Google Scholar]
Fatourechi 2009
- Fatourechi MM, Kudva YC, Murad MH, Elamin MB, Tabini CC, Montori VM.Hypoglycemia with intensive insulin therapy: a systematic review and meta-analyses of randomized trials of continuous subcutaneous insulin infusion versus multiple daily injections. Journal of Clinical Endocrinology and Metabolism 2009;94(3):729-40. [DOI] [PubMed] [Google Scholar]
Fealy 2009
- Fealy G, McCarron M, O'Neill D, McCallion P, Clarke M, Small V et al.Effectiveness of gerontologically informed nursing assessment and referral interventions for older persons attending the emergency department: systematic review. Journal of Advanced Nursing 2009;65(5):934-45. [DOI] [PubMed] [Google Scholar]
Felder 2011
- Felder TM, Palmer NR, Lal LS, Mullen PD.What is the evidence for pharmaceutical patient assistance programs? A systematic review. Journal of Health Care for the Poor and Underserved 2011;22(1):24-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferreira 2009
- Ferreira AL, Lemos A, Figueiroa JN, Souza AI.Effectiveness of contraceptive counselling of women following an abortion: a systematic review and meta-analysis. European Journal of Contraception and Reproductive Health Care 2009;14(1):1-9. [DOI] [PubMed] [Google Scholar]
Ferron 2009
- Ferron JC, Alterman AI, McHugo GJ, Brunette MF, Drake RE.A review of research on smoking cessation interventions for adults with schizophrenia spectrum disorders. Mental Health and Substance Use 2009;2(1):64-79. [Google Scholar]
Finley 2003
- Finley PR, Crismon ML, Rush AJ.Evaluating the impact of pharmacists in mental health: a systematic review. Pharmacotherapy 2003;23(12):1634-44. [DOI] [PubMed] [Google Scholar]
Fischer 2010
- Fischer SH, Tjia J, Field TS.Impact of health information technology interventions to improve medication laboratory monitoring for ambulatory patients: a systematic review. Journal of the American Medical Informatics Association 2010;17(6):631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fjeldsoe 2009
- Fjeldsoe BS, Marshall AL, Miller YD.Behavior change interventions delivered by mobile telephone short-message service. American Journal of Preventive Medicine 2009;36(2):165-73. [DOI] [PubMed] [Google Scholar]
Fleury 2009
- Fleury J, Keller C, Perez A, Lee SM.The role of lay health advisors in cardiovascular risk reduction: a review. American Journal of Community Psychology 2009;44(1-2):28-42. [DOI] [PubMed] [Google Scholar]
Flodgren 2011
- Flodgren G, Pomey MP, Taber SA, Eccles MP.Effectiveness of external inspection of compliance with standards in improving healthcare organisation behaviour, healthcare professional behaviour or patient outcomes. Cochrane Database of Systematic Reviews 2011, Issue 11. Art. No: CD008992. [DOI: 10.1002/14651858.CD008992.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Forsetlund 2009
- Forsetlund L, Bjørndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf F, et al.Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD003030. [DOI: 10.1002/14651858.CD003030.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Forsetlund 2010
- Forsetlund L, Eike MC, Vist GE.Effect of interventions to improve health care services for ethnic minority populations. Norsk Epidemiologi 2010;20(1):41-52. [Google Scholar]
Forster 2008
- Smith J, Forster A, House A, Knapp P, Wright JJ, Young J.Information provision for stroke patients and their caregivers. Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No: CD001919. [DOI: 10.1002/14651858.CD001919.pub2] [DOI] [PubMed] [Google Scholar]
Foster 2007
- Foster G, Taylor SJC, Eldridge S, Ramsay J, Griffiths CJ.Self-management education programmes by lay leaders for people with chronic conditions. Cochrane Database of Systematic Reviews 2007, Issue 4. Art. No: CD005108. [DOI: 10.1002/14651858.CD005108.pub2] [DOI] [PubMed] [Google Scholar]
Fox 2009
- Fox MP.A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Education and Counseling 2009;77(1):6-13. [DOI] [PubMed] [Google Scholar]
Freund 2009
- Freund M, Campbell E, Paul C, Sakrouge R, McElduff P, Walsh RA, et al.Increasing smoking cessation care provision in hospitals: a meta-analysis of intervention effect. Nicotine and Tobacco Research 2009;11(6):650-62. [DOI] [PubMed] [Google Scholar]
Gagnon 2007
- Gagnon AJ.Individual or group antenatal education for childbirth/parenthood. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD002869. [DOI: 10.1002/14651858.CD002869] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gaston 2005
- Gaston CM, Mitchell G.Information giving and decision-making in patients with advanced cancer: A systematic review. Social Science & Medicine 2005;61(10):2252-64. [DOI] [PubMed] [Google Scholar]
Gensichen 2006
- Gensichen J, Beyer M, Muth C, Gerlach FM, Von Korff M, Ormel J.Case management to improve major depression in primary health care: a systematic review. Psychological Medicine 2006;36(1):7-14. [DOI] [PubMed] [Google Scholar]
George 2008
- George J, Elliott R, Stewart D.A systematic review of interventions to improve medication taking in elderly patients prescribed multiple medications. Drugs & Aging 2008;25(4):307-24. [DOI] [PubMed] [Google Scholar]
Gialamas 2010
- Gialamas A, St John A, Laurence CO, Bubner TK, PoCT Management Committee.Point-of-care testing for patients with diabetes, hyperlipidaemia or coagulation disorders in the general practice setting: a systematic review. Family Practice 2010;27(1):17-24. [DOI] [PubMed] [Google Scholar]
Gibson 2002
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Hensley MJ, Abramson M, et al.Limited (information only) patient education programs for adults with asthma. Cochrane Database of Systematic Reviews 2002, Issue 2. Art. No: CD001005. [DOI: 10.1002/14651858.CD001005] [DOI] [PubMed] [Google Scholar]
Gibson 2003
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, et al.Self-management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews 2003, Issue 1. Art. No: CD001117. [DOI: 10.1002/14651858.CD001117] [DOI] [PubMed] [Google Scholar]
Gilbody 2003
- Gilbody S, House A, Sheldon T.Outcome measures and needs assessment tools for schizophrenia and related disorders. Cochrane Database of Systematic Reviews 2003, Issue 1. Art. No: CD003081. [DOI: 10.1002/14651858.CD003081] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gill 1999
- Gill PS, Makela M, Vermeulen KM, Freemantle N, Ryan G, Bond C, et al.Changing doctor prescribing behaviour. Pharmacy World & Science 1999;21(4):158-67. [DOI] [PubMed] [Google Scholar]
Gillespie 2001
- Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH.Interventions for preventing falls in elderly people. Cochrane Database of Systematic Reviews 2003, Issue 4. Art. No: CD000340. [DOI: 10.1002/14651858.CD000340] [DOI] [PubMed] [Google Scholar]
Gillespie 2009
- Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al.Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD007146. [DOI: 10.1002/14651858.CD007146.pub2] [DOI] [PubMed] [Google Scholar]
Glasdam 2010
- Glasdam S, Timm H, Vittrup R.Support efforts for caregivers of chronically ill persons. Clinical Nursing Research 2010;19(3):233-65. [DOI] [PubMed] [Google Scholar]
Glazier 2006
- Glazier RH, Bajcar J, Kennie NR, Willson K.A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care 2006;29(7):1675-88. [DOI] [PubMed] [Google Scholar]
Glenton 2011
- Glenton C, Scheel IB, Lewin S, Swingler GH.Can lay health workers increase the uptake of childhood immunisation? Systematic review and typology. Tropical Medicine and International Health 2011;16(9):1044-53. [DOI] [PubMed] [Google Scholar]
Glueckauf 2009
- Glueckauf RL, Lustria ML.E-health self-care interventions for persons with chronic illnesses: review and future directions. In: Database of Abstracts of Reviews of Effects. Vol. 2. Springer Publishing Company, 2009:151-242. [http://www.healthsystemsevidence.org/one-page-summary.aspx?A=99&T=Ehealthsel&L=EN] [Google Scholar]
Gogia 2010
- Gogia S, Sachdev HS.Home visits by community health workers to prevent neonatal deaths in developing countries: a systematic review. Bulleting of the World Health Organization 2010;88(9):658-66B. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldman 2007
- Goldman DP, Joyce GF, Zheng Y.Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA 2007;298:61-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goulding 2010
- Goulding L, Furze G, Birks Y.Randomized controlled trials of interventions to change maladaptive illness beliefs in people with coronary heart disease: systematic review. Journal of Advanced Nursing 2010;66(5):946-61. [DOI] [PubMed] [Google Scholar]
Govindan 2010
- Govindan M, Van Citters AD, Nelson EC, Kelly-Cummings J, Suresh G.Automated detection of harm in healthcare with information technology: a systematic review. Quality and Safety in Health Care 2010;19(5):e11. [DOI: 10.1136/qshc.2009.033027] [DOI] [PubMed] [Google Scholar]
Graziano 2009
- Graziano JA, Gross CR.The effects of isolated telephone interventions on glycemic control in type 2 diabetes: a literature review. ANS Advances in Nursing Science 2009;32(3):E28 – E41. [DOI] [PubMed] [Google Scholar]
Grilli 2002
- Grilli R, Ramsay C, Minozzi S.Mass media interventions: effects on health services utilisation. Cochrane Database of Systematic Reviews 2002, Issue 1. Art. No: CD000389. [DOI: 10.1002/14651858.CD000389] [DOI] [PubMed] [Google Scholar]
Guldberg 2009
- Guldberg TL, Lauritzen T, Kristensen JK, Vedsted P.The effect of feedback to general practitioners on quality of care for people with type 2 diabetes: a systematic review of the literature. BMC Family Practice 2009;10(30). [DOI: doi: 10.1186/1471-2296-10-30] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gunn 2006
- Gunn J, Diggens J, Hegarty K, Blashki G.A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Services Research 2006 Jul 16;6:88. [DOI: 10.1186/1472-6963-6-88] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haby 2001
- Haby M, Waters E, Robertson C, Gibson PG, Ducharme FM.Interventions for educating children who have attended the emergency room for asthma. Cochrane Database of Systematic Reviews 2001, Issue 1. Art. No: CD001290. [DOI: 10.1002/14651858.CD001290] [DOI] [PubMed] [Google Scholar]
Hailey 2008
- Hailey D, Roine R, Ohinmaa A.The effectiveness of telemental health applications: a review. Canadian Journal of Psychiatry 2008;53(11):769-78. [DOI] [PubMed] [Google Scholar]
Hajjar 2007
- Hajjar ER, Cafiero AC, Hanlon JT.Polypharmacy in elderly patients. American Journal of Geriatric Pharmacotherapy December 2007;5(4):345-51. [DOI] [PubMed] [Google Scholar]
Halpern 2006
- Halpern V, Grimes DA, Lopez L, Gallo MF.Strategies to improve adherence and acceptability of hormonal methods for contraception. Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No: CD004317. [DOI: 10.1002/14651858.CD004317.pub2] [DOI] [PubMed] [Google Scholar]
Han 2012
- Han S, Crowther CA, Middleton P.Interventions for pregnant women with hyperglycaemia not meeting gestational diabetes and type 2 diabetes diagnostic criteria. Cochrane Database of Systematic Reviews 2012, Issue 1. Art. No: CD009037. [DOI: 10.1002/14651858.CD009037.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Handford 2006
- Handford CD, Tynan AM, Rackal JM, Glazier RH.Setting and organization of care for persons living with HIV/AIDS. Cochrane Database of Systematic Reviews 2006, Issue 19. Art. No: CD004348. [DOI: 10.1002/14651858.CD004348.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harding 2005
- Harding R, Karus D, Easterbrook P, Raveis VH, Higginson IJ, Marconi K.Does palliative care improve outcomes for patients with HIV/AIDS: a systematic review of the evidence. Sexually Transmitted Infections 2005;81(1):5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harris 2005
- Harris M, Smith B, Veale A.Printed patient education interventions to facilitate shared management of chronic disease: a literature review. Journal of Internal Medicine 2005 Dec;35(12):711-6. [DOI] [PubMed] [Google Scholar]
Harris 2006
- Harris R, Ullman R, Griffiths P.Self-assessment of health and social care needs by older people. Reviews in Clinical Gerontology 2006;16:301-12. [Google Scholar]
Hart 2010
- Hart JE, Jeon CY, Ivers LC, Behforouz HL, Caldas A, Drobac PC, et al.Effect of directly observed therapy for highly active antiretroviral therapy on virologic, immunologic, and adherence outcomes: a meta-analysis and systematic review. Journal of Acquired Immune Deficiency Syndromes 2010;54(2):167-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hartmann 2010
- Hartmann M, Bazner E, Wild B, Eisler I, Herzog W.Effects of interventions involving the family in the treatment of adult patients with chronic physical diseases: a meta-analysis. Psychotherapy and Psychosomatics 2010;79(3):136-48. [DOI] [PubMed] [Google Scholar]
Hawkins 2007
- Hawkins LC, Edwards JN, Dargan PI.Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: a review of the literature. Drug Safety 2007;30(6):465-79. [DOI] [PubMed] [Google Scholar]
Hawthorne 2010
- Hawthorne K, Robles Y, Cannings-John R, Edwards AG.Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabetic Medicine 2010;27(6):613-23. [DOI] [PubMed] [Google Scholar]
Haynes 1996
- Haynes RB, McKibbon KA, Kanani R.Systematic review of randomised trials of interventions to assist patients to follow prescriptions for medications. Lancet 1996;348(9024):383-6. [DOI] [PubMed] [Google Scholar]
Heideman 2005
- Heideman J, Rijswijk E, Lin N, Loos S, Laurant M, Wensing M, et al.Interventions to improve management of anxiety disorders in general practice: a systematic review. British Journal of General Practice 2005;55:867-74. [PMC free article] [PubMed] [Google Scholar]
Heinrich 2010
- Heinrich E, Schaper NC, Vries NK.Self-management interventions for type 2 diabetes: a systematic review. European Diabetes Nursing 2010;7(2):71-6. [Google Scholar]
Hemmingsen 2011
- Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal T, Hemmingsen C, et al.Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2011, Issue 6. Art. No: CD008143. [DOI: 10.1002/14651858.CD008143.pub2] [DOI] [PubMed] [Google Scholar]
Henderson 1999
- Henderson C, Laugharne R.Patient held clinical information for people with psychotic illnesses. Cochrane Database of Systematic Reviews 1999, Issue 3. Art. No: CD001711. [DOI: 10.1002/14651858.CD001711] [DOI] [PubMed] [Google Scholar]
Heneghan 2006a
- Heneghan CJ, Glasziou P, Perera R.Reminder packaging for improving adherence to self-administered long-term medications. Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No: CD005025. [DOI: 10.1002/14651858.CD005025.pub2] [DOI] [PubMed] [Google Scholar]
Heneghan 2006b
- Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P.Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet 2006;367(9508):404-11. [DOI] [PubMed] [Google Scholar]
Herman 2009
- Herman AD, Johnson TM, Ritchie CS, Parmelee PA.Pain management interventions in the nursing home: a structured review of the literature. Journal of the American Geriatrics Society 2009;57(7):1258-67. [DOI] [PubMed] [Google Scholar]
Hersh 2006
- Hersh WR, Hickam DH, Severance AM, Dana TL, Krages KP, Hefland M.Telemedicine for the Medicare population: update. Agency for Healthcare Research and Quality 2006;41. [PMC free article] [PubMed]
Heselmans 2009
- Heselmans A, Van de Velde S, Donceel P, Aertgeerts B, Ramaekers D.Effectiveness of electronic guideline-based implementation systems in ambulatory care settings - a systematic review. Implementation Science 2009;4(82). [DOI: 10.1186/1748-5908-4-82] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hey 2005
- Hey K, Perera R.Competitions and incentives for smoking cessation. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD004307. [DOI: 10.1002/14651858.CD004307.pub2] [DOI] [PubMed] [Google Scholar]
Higgins 2004
- Higgins N, Regan C.A systematic review of the effectiveness of interventions to help older people adhere to medication regimes. Age & Ageing 2004;33(3):224-9. [DOI] [PubMed] [Google Scholar]
Hiller 2002
- Hiller JE, Griffith E, Jenner F.Education for contraceptive use by women after childbirth. Cochrane Database of Systematic Reviews 2002, Issue 3. Art. No: CD001863. [DOI: 10.1002/14651858.CD001863] [DOI] [PubMed] [Google Scholar]
Hodge 2010
- Hodge DR, Jackson KF, Vaughn MG.Culturally sensitive interventions and health and behavioral health youth outcomes: a meta-analytic review. Social Work in Health Care 2009;49(5):401-23. [DOI] [PubMed] [Google Scholar]
Hodnett 2000
- Hodnett ED.Continuity of caregivers for care during pregnancy and childbirth. Birth 2000;27(3):217. [DOI] [PubMed] [Google Scholar]
Hoeks 2011
- Hoeks LB, Greven WL, Valk HW.Real-time continuous glucose monitoring system for treatment of diabetes: a systematic review. Diabetic Medicine 2011;28(4):386-94. [DOI] [PubMed] [Google Scholar]
Holland 2005
- Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L.Systematic review of multidisciplinary interventions in heart failure. Heart 2005;91(7):899-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollands 2010
- Hollands GJ, Hankins M, Marteau TM.Visual feedback of individuals' medical imaging results for changing health behaviour. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD007434. [DOI: 10.1002/14651858.CD007434.pub2] [DOI] [PubMed] [Google Scholar]
Hood 2010
- Hood KK, Rohan JM, Peterson CM, Drotar D.Interventions with adherence-promoting components in pediatric type 1 diabetes: meta-analysis of their impact on glycemic control. Diabetes Care 2010;33(7):1658-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoogendoorn 2010
- Hoogendoorn M, Feenstra TL, Hoogenveen RT, Rutten-van Molken MP.Long-term effectiveness and cost-effectiveness of smoking cessation interventions in patients with COPD. Thorax 2010;65(8):711-8. [DOI] [PubMed] [Google Scholar]
Horsley 2010
- Horsley T, O'Neill J, McGowan J, Perrier L, Kane G, Campbell C.Interventions to improve question formulation in professional practice and self-directed learning. Cochrane Database of Systematic Reviews 2010, Issue 5. Art. No: CD007335. [DOI: 10.1002/14651858.CD007335.pub2] [DOI] [PubMed] [Google Scholar]
Huffman 2010
- Huffman LC, Brat GA, Chamberlain LJ, Wise PH.Impact of managed care on publicly insured children with special health care needs. Academic Pediatrics 2010;10(1):48-55. [DOI: 10.1016/j.acap.2009.09.007] [DOI] [PubMed] [Google Scholar]
Hulscher 1999
- Hulscher ME, Wensing M, Grol RP, Weijden T, Weel C.Interventions to improve the delivery of preventive services in primary care. American Journal of Public Health. 1999;89(5):737-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hwang 2005
- Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE.Interventions to improve the health of the homeless: a systematic review. American Journal of Preventive Medicine. 2005;29(4):311-19. [DOI] [PubMed] [Google Scholar]
Ilott 2005
- Ilott R.Does compliance therapy improve use of antipsychotic medication? British Journal of Community Nursing 2005;10(11):514-9. [DOI] [PubMed] [Google Scholar]
Ioannidis 2001
- Ioannidis JP, Lau J.Evidence on interventions to reduce medical errors: an overview and recommendations for future research. Journal of General Internal Medicine 2001;16(5):325-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Irani 2009
- Irani JS, Middleton JL, Marfatia R, Omana ET, D’Amico F.The use of electronic health records in the exam room and patient satisfaction: a systematic review. Journal of the American Board of Family Medicine 2009;22(5):553-62. [DOI] [PubMed] [Google Scholar]
Jaber 2006
- Jaber R, Braksmajer A, Trilling JS.Group visits: a qualitative review of current research. Journal of the American Board of Family Medicine 2006;19(3):276-90. [DOI] [PubMed] [Google Scholar]
Jamtvedt 2006
- Jamtvedt G, Young JM, Kristoffersen DT, O'Brien MA, Oxman AD.Does telling people what they have been doing change what they do: a systematic review of the effects of audit and feedback. Quality and Safety in Health Care 2006;15(6):433-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johansson 2010
- Johansson T, Wild C.Telemedicine in acute stroke management: systematic review. International Journal of Technology Assessment in Health Care 2010;26(2):149-55. [DOI] [PubMed] [Google Scholar]
Johnson 2003
- Johnson A, Sandford J, Tyndall J.Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Cochrane Database of Systematic Reviews 2003, Issue 4. Art. No: CD003716. [DOI: 10.1002/14651858.CD003716] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2002
- Jones A, Fay JK, Ram FSF.Primary care based clinics for asthma. Cochrane Database of Systematic Reviews 2002, Issue 1. Art. No: CD003533. [DOI: 10.1002/14651858.CD003533] [DOI] [PubMed] [Google Scholar]
Jovicic 2006
- Jovicic A, Holroyd-Leduc JM, Straus SE.Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovascular Disorders 2006;6:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaboli 2006
- Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL.Clinical pharmacists and inpatient medical care: a systematic review. Archives of Internal Medicine 2006;166(9):955-64. [DOI] [PubMed] [Google Scholar]
Kangelaris 2009
- Kangelaris KN, Bent S, Nussbaum RL, Garcia DA, Tice JA.Genetic testing before anticoagulation? A systematic review of pharmacogenetic dosing of warfarin. Journal of General Internal Medicine May 2009;24(5):656-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kang‐Yi 2010
- Kang-Yi CD, Gellis ZD.A systematic review of community-based health interventions on depression for older adults with heart disease. Aging and Mental Health 2010;14(1):1-19. [DOI] [PubMed] [Google Scholar]
Kaper 2005
- Kaper J, Wagena EJ, Severens JL, Van Schayck CP.Healthcare financing systems for increasing the use of tobacco dependence treatment. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No: CD004305. [DOI: 10.1002/14651858.CD004305.pub2] [DOI] [PubMed] [Google Scholar]
Karjalainen 1999
- Karjalainen KA, Malmivaara A, Tulder MW, Roine R, Jauhiainen M, Hurri H, et al.Multidisciplinary rehabilitation for fibromyalgia and musculoskeletal pain in working age adults. Cochrane Database of Systematic Reviews 1999, Issue 3. Art. No: CD001984. [DOI: 10.1002/14651858.CD001984] [DOI] [PMC free article] [PubMed] [Google Scholar]
Karjalainen 2003a
- Karjalainen KA, Malmivaara A, Tulder MW, Roine R, Jauhiainen M, Hurri H, et al.Multidisciplinary biopsychosocial rehabilitation for neck and shoulder pain among working age adults. Cochrane Database of Systematic Reviews 2003, Issue 2. Art. No: CD002194. [DOI: 10.1002/14651858.CD002194] [DOI] [PubMed] [Google Scholar]
Karjalainen 2003b
- Karjalainen KA, Malmivaara A, Tulder MW, Roine R, Jauhiainen M, Hurri H, et al.Multidisciplinary biopsychosocial rehabilitation for subacute low-back pain among working age adults. Cochrane Database of Systematic Reviews 2003, Issue 2. Art. No: CD002193. [DOI: 10.1002/14651858.CD002193] [DOI] [PubMed] [Google Scholar]
Kastner 2008
- Kastner M, Straus SE.Clinical decision support tools for osteoporosis disease management: a systematic review of randomized controlled trials. Journal of General Internal Medicine 2008 December;23(12):2095-3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kendrick 2000
- Kendrick D, Hewitt M, Dewey M, Elkan R, Blair M, Robinson J, et al.The effect of home visiting programmes on uptake of childhood immunization: a systematic review and meta-analysis. Journal of Public Health Medicine 2000;22(1):90-8. [DOI] [PubMed] [Google Scholar]
Kendrick 2008
- Kendrick D, Smith S, Sutton A, Watson M, Coupland C, Mulvaney C, et al.Effect of education and safety equipment on poisoning-prevention practices and poisoning: systematic review, meta-analysis and meta-regression. Archive of Diseases of Childhood 2008;93(7):599-608. [DOI] [PubMed] [Google Scholar]
Kirby 2008
- Kirby D.The impact of programs to increase contraceptive use among adult women: a review of experimental and quasi-experimental studies. Perspectives on Sexual and Reproductive Health March 2008;40(1):34-41. [DOI] [PubMed] [Google Scholar]
Kisely 2011
- Kisely SR, Campbell LA, Preston NJ.Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database of Systematic Reviews 2011, Issue 2. Art. No: CD004408. [DOI: 10.1002/14651858.CD004408.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kongnyuy 2009
- Kongnyuy EJ, Uthman OA.Use of criterion-based clinical audit to improve the quality of obstetric care: a systematic review. Acta Obstetricia et Gynecologica Scandinavica 2009;88(8):873-81. [DOI] [PubMed] [Google Scholar]
Kripalani 2007
- Kripalani S, Yao X, Haynes B.Interventions to enhance medication adherence in chronic medical conditions. Archives of Internal Medicine 2007;167(6):540-50. [DOI] [PubMed] [Google Scholar]
Krishna 2009
- Krishna S, Boren SA, Balas EA.Healthcare via cell phones: a systematic review. Telemedicine and E-Health 2009;15(3):231-40. [DOI] [PubMed] [Google Scholar]
Krueger 2003
- Krueger KP, Felkey BG, Berger BA.Improving adherence and persistence: a review and assessment of interventions and description of steps toward a national adherence initiative. Journal of the American Pharmacists Association 2003;43(6):668-78; quiz 678-9. [DOI] [PubMed] [Google Scholar]
Kruk 2006
- Kruk ME, Schwalbe N.The relation between intermittent dosing and adherence: Preliminary insights. Clinical Therapeutics 2006;28(12):1989-95. [DOI] [PubMed] [Google Scholar]
Kwan 2004
- Kwan J, Sandercock PAG.In-hospital care pathways for stroke. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD002924. [DOI: 10.1002/14651858.CD002924.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lagarde 2007
- Lagarde M, Haines A, Palmer N.Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA 2007;298(16):1900-10. [DOI] [PubMed] [Google Scholar]
Lagarde 2009
- Lagarde M, Haines A, Palmer N.The impact of conditional cash transfers on health outcomes and use of health services in low and middle income countries. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No: CD008137. [DOI: 10.1002/14651858.CD008137] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lagarde 2011
- Lagarde M, Palmer N.The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database of Systematic Reviews 2011, Issue 4. Art. No: CD009094. [DOI: 10.1002/14651858.CD009094] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lai 2010
- Lai DTC, Cahill K, Qin Y, Tang JL.Motivational interviewing for smoking cessation. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD006936. [DOI: 10.1002/14651858.CD006936.pub2] [DOI] [PubMed] [Google Scholar]
Lai 2010b
- Lai P, Chua SS, Chan SP.A systematic review of interventions by healthcare professionals on community-dwelling postmenopausal women with osteoporosis. Osteoporosis International 2010;21(10):1637-56. [DOI] [PubMed] [Google Scholar]
Lancaster 2002
- Lancaster T, Stead LF.Self-help interventions for smoking cessation. Cochrane Database of Systematic Reviews 2002, Issue 3. Art. No: CD001118. [DOI: 10.1002/14651858.CD001118] [DOI] [PubMed] [Google Scholar]
Lancaster 2004
- Lancaster T, Stead LF.Physician advice for smoking cessation. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD000165. [DOI: 10.1002/14651858.CD000165.pub2] [DOI] [PubMed] [Google Scholar]
Lancaster 2005
- Lancaster T, Stead LF.elf-help interventions for smoking cessation. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD001118. [DOI: 10.1002/14651858.CD001118.pub2] [DOI] [PubMed] [Google Scholar]
Lassi 2010
- Lassi ZS, Haider BA, Bhutta ZA.Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database of Systematic Reviews 2010, Issue 11. Art. No: CD007754. [DOI: 10.1002/14651858.CD007754.pub2] [DOI] [PubMed] [Google Scholar]
Leach 2006
- Leach LS, Christensen H.A systematic review of telephone-based interventions for mental disorders. Journal of Telemedicine and Telecare 2006;12(3):122-9. [DOI] [PubMed] [Google Scholar]
Légaré 2010
- Légaré F, Ratté S, Stacey D, Kryworuchko J, Gravel K, Graham ID, et al.Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database of Systematic Reviews 2010, Issue 5. Art. No: CD006732. [DOI: 10.1002/14651858.CD006732.pub2] [DOI] [PubMed] [Google Scholar]
Lemmens 2009
- Lemmens KM, Nieboer AP, Huijsman R.A systematic review of integrated use of disease-management interventions in asthma and COPD. Respiratory Medicine 2009;103(5):670-91. [DOI] [PubMed] [Google Scholar]
Lewin 2001
- Lewin S, Skea Z, Entwistle VA, Zwarenstein M, Dick J.Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews 2001, Issue 4. Art. No: CD003267. [DOI: 10.1002/14651858.CD003267] [DOI] [PubMed] [Google Scholar]
Lewin 2005
- Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, Wyk B, et al.Lay health workers in primary and community health care. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No: CD004015. [DOI: 10.1002/14651858.CD004015.pub2] [DOI] [PubMed] [Google Scholar]
Li 2010
- Li X, Mao M, Ping Q.Effect of pharmaceutical care programs on glycemic control in patients with diabetes mellitus: a meta-analysis of randomized controlled trials. Journal of Pharmacy Technology 2010;26(5):255-63. [Google Scholar]
Li 2011
- Li T, Wu HM, Wang F, Huang CQ, Yang M, Dong BR, et al.Education programmes for people with diabetic kidney disease. Cochrane Database of Systematic Reviews 2011, Issue 6. Art. No: CD007374. [DOI: 10.1002/14651858.CD007374.pub2] [DOI] [PubMed] [Google Scholar]
Liang 2011
- Liang X, Wang Q, Yang X, Cao J, Chen J, Mo X, et al.Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabetic Medicine 2011;28(4):455-63. [DOI] [PubMed] [Google Scholar]
Lindsay 2010
- Lindsay B, Bradley PM.Care delivery and self-management strategies for children with epilepsy. Cochrane Database of Systematic Reviews 2010, Issue 12. Art. No: CD006245. [DOI: 10.1002/14651858.CD006245.pub2] [DOI] [PubMed] [Google Scholar]
Liss 2002
- Liss HJ, Glueckauf RL, Ecklund-Johnson EP.Research on telehealth and chronic medical conditions: critical review, key issues, and future directions. Rehabilitation Psychology 2002;47(1):8-30. [Google Scholar]
Lodewijckx 2009
- Lodewijckx C, Sermeus W, Vanhaecht K, Panella M, Deneckere S, Leigheb F, et al.In-hospital management of COPD exacerbations: a systematic review of the literature with regard to adherence to international guidelines. Journal of Evaluation in Clinical Practice 2009;15(6):1101-10. [DOI] [PubMed] [Google Scholar]
Lopez 2009
- Lopez LM, Tolley EE, Grimes DA, Chen-Mok M.Theory-based interventions for contraception. Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No: CD007249. [DOI: 10.1002/14651858.CD007249.pub2] [DOI] [PubMed] [Google Scholar]
Lopez 2010
- Lopez LM, Hiller JE, Grimes DA.Postpartum education for contraception: a systematic review. Obstetric and Gynecological Survey 2010;65(5):325-31. [DOI] [PubMed] [Google Scholar]
Loveman 2003
- Loveman E, Royle P, Waugh N.Specialist nurses in diabetes mellitus. Cochrane Database of Systematic Reviews 2003, Issue 2. Art. No: CD003286. [DOI: 10.1002/14651858.CD003286] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lu 2008
- Lu CY, Ross-Degnan D, Soumerai SB, Pearson SA.Interventions designed to improve the quality and efficiency of medication use in managed care: A critical review of the literature – 2001–2007. BMC Health Services Research 2008 2008;8(75). [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lugtenberg 2009
- Lugtenberg M, Burgers JS, Westert GP.Effects of evidence-based clinical practice guidelines on quality of care: a systematic review. Quality and Safety in Health Care 2009;18(5):385-92. [DOI] [PubMed] [Google Scholar]
Lumley 2009
- Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley L, Watson L.Interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No: CD001055. [DOI: 10.1002/14651858.CD001055.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lussier 2006
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST.A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction 2006;101(2):192-203. [DOI] [PubMed] [Google Scholar]
Maeda 2009
- Maeda K.A systematic review of the effects of improvement of prescription to reduce the number of medications in the elderly with polypharmacy. Journal of the Pharmaceutical Society of Japan 2009;129(5):631-45. [DOI] [PubMed] [Google Scholar]
Malone 2007
- Malone D, Marriott S, Newton-Howes G, Simmonds S, Tyrer P.Community mental health teams (CMHTs) for people with severe mental illnesses and disordered personality. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD000270. [DOI: 10.1002/14651858.CD000270.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maric 2009
- Maric B, Kaan A, Ignaszewski A, Lear SA.A systematic review of telemonitoring technologies in heart failure. European Journal of Heart Failure 2009;11(5):506-17. [DOI] [PubMed] [Google Scholar]
Marshall 1998
- Marshall M, Gray A, Lockwood A, Green R.Case management for people with severe mental disorders. Cochrane Database of Systematic Reviews 1998, Issue 2. Art. No: CD000050. [DOI: 10.1002/14651858.CD000050] [DOI] [PubMed] [Google Scholar]
Martire 2005
- Martire LM.The "relative" efficacy of involving family in psychosocial interventions for chronic illness: are there added benefits to patients and family members? Families, Systems, and Health 2005;23(3):312-28. [Google Scholar]
Martire 2010
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM.Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioural Medicine 2010;40(3):325-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Matteson 2010
- Matteson ML, Russell C.Interventions to improve hemodialysis adherence: a systematic review of randomized-controlled trials. Hemodialysis International 2010;14(4):370-82. [DOI] [PubMed] [Google Scholar]
McClure 2005
- McClure R, Turner C, Peel N, Spinks A, Eakin E, Hughes K.Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No: CD004441. [DOI: 10.1002/14651858.CD004441.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McDonald 2002
- McDonald HP, Garg AX, Haynes RB.Interventions to enhance patient adherence to medication prescriptions. JAMA 2002;288(22):2868-78. [DOI] [PubMed] [Google Scholar]
McGraw 2004
- McGraw C.Multi-compartment medication devices and patient compliance. British Journal of Community Nursing 2004;9(7):285-90. [DOI] [PubMed] [Google Scholar]
McKinstry 2006
- McKinstry B, Ashcroft R, Car J, Freeman GK, Sheikh A.Interventions for improving patients' trust in doctors and groups of doctors. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No: CD004134. [DOI: 10.1002/14651858.CD004134.pub2] [DOI] [PubMed] [Google Scholar]
McLean 2010
- McLean S, Chandler D, Nurmatov U, Liu J, Pagliari C, Car J, et al.Telehealthcare for asthma. Cochrane Database of Systematic Reviews 2010, Issue 10. Art. No: CD007717. [DOI: 10.1002/14651858.CD007717.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
McLean 2011
- McLean S, Nurmatov U, Liu JL, Pagliari C, Car J, Sheikh A.Telehealthcare for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD007718. [DOI: 10.1002/14651858.CD007718.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Meyer‐Massetti 2011
- Meyer-Massetti C, Cheng CM, Schwappach DL, Paulsen L, Ide B, Meier CR, et al.Systematic review of medication safety assessment methods. American Journal of Health Systems Pharmacy 2011;68(3):227-40. [DOI] [PubMed] [Google Scholar]
Michael 2010
- Main C, Moxham T, Wyatt JC, Kay J, Anderson R, Stein K.Computerised decision support systems in order communication for diagnostic, screening or monitoring test ordering: systematic reviews of the effects and cost-effectiveness of systems. Health Technology Assessment 2010;14(48):1-227. [DOI] [PubMed] [Google Scholar]
Michael 2010b
- Michael YL, Lin JS, Whitlock EP, Gold R, Fu R, O’Connor EA et al.Interventions to prevent falls in older adults: an updated systematic review. Evidence Syntheses 2010;80. [Agency for Healthcare Research and Quality. Report No: 11-05150-EF-1] [PubMed]
Michie 2003
- Michie S, Miles J, Weinman J.Patient-centredness in chronic illness: what is it and does it matter? Patient Education and Counseling 2003;51(3):197-206. [DOI] [PubMed] [Google Scholar]
Minet 2010
- Minet L, Moller S, Vach W, Wagner L, Henriksen JE.Mediating the effect of self-care management intervention in type 2 diabetes: a meta-analysis of 47 randomised controlled trials. Patient Education and Counseling 2010;80(1):29-41. [DOI] [PubMed] [Google Scholar]
Mistiaen 2006
- Mistiaen P, Poot E.Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD004510. [DOI: 10.1002/14651858.CD004510.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohanan 2009
- Mohanan P, Kamath A.Family support for reducing morbidity and mortality in people with HIV/AIDS. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No: CD006046. [DOI: 10.1002/14651858.CD006046.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moonesinghe 2011
- Moonesinghe SR, Lowery J, Shahi N, Millen A, Beard JD.Impact of reduction in working hours for doctors in training on postgraduate medical education and patients' outcomes: systematic review. BMJ 2011;342:d1580-93. [DOI: 10.1136/bmj.d1580] [DOI] [PubMed] [Google Scholar]
Motamedi 2011
- Motamedi SM, Posadas-Calleja J, Straus S, Bates DW, Lorenzetti DL, Baylis B, et al.The efficacy of computer-enabled discharge communication interventions: a systematic review. BMJ Quality and Safety 2011;20(5):403-15. [DOI] [PubMed] [Google Scholar]
Murray 2005
- Murray E, Burns J, See Tai S, Lai R, Nazareth I.Interactive Health Communication Applications for people with chronic disease. Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No: CD004274. [DOI: 10.1002/14651858.CD004274.pub4] [DOI] [PubMed] [Google Scholar]
Nabhan 2011
- Nabhan AF, Elsedawy MM.Tight control of mild-moderate pre-existing or non-proteinuric gestational hypertension. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD006907. [DOI: 10.1002/14651858.CD006907.pub2] [DOI] [PubMed] [Google Scholar]
Ndiaye 2005
- Ndiaye SM, Hopkins DP, Shefer AM, Hinman AR, Briss PA, Rodewald L, et al.Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. American Journal of Preventive Medicine 2005;28(5 Suppl):248-79. [DOI] [PubMed] [Google Scholar]
Newell 1999
- Newell SA, Bowman JA, Cockburn JD.A critical review of interventions to increase compliance with medication-taking, obtaining medication refills, and appointment-keeping in the treatment of cardiovascular disease. Preventive Medicine 1999;29(6 Pt 1):535-48. [DOI] [PubMed] [Google Scholar]
Ni 2009
- Ni Y, Chen Y, Huang W.The effect of pharmaceutical care programs on blood pressure control in individuals with hypertension: a meta-analysis. Journal of Pharmacy Technology 2009;25(5):292-6. [Google Scholar]
Niesink 2007
- Niesink A, Trappenburg JC, Weert-van Oene GH, Lammers JW, Verheij TJ, Schrijvers AJ.Systematic review of the effects of chronic disease management on quality-of-life in people with chronic obstructive pulmonary disease. Respiratory Medicine 2007;101(11):2233-9. [DOI] [PubMed] [Google Scholar]
Nilsen 2006
- Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD.Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No: CD004563. [DOI: 10.1002/14651858.CD004563.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norris 2006
- Norris SL, Chowdhury FM, Van Le K, Horsley T, Brownstein JN, Zhang X, et al.Effectiveness of community health workers in the care of persons with diabetes. Diabetic Medicine 2006;23(5):544-56. [DOI] [PubMed] [Google Scholar]
Nose 2003
- Nose M, Barbui C, Gray R, Tansella M.Clinical interventions for treatment non-adherence in psychosis: meta-analysis. British Journal of Psychiatry 2003;183:197-206. [DOI] [PubMed] [Google Scholar]
O'Connor 2009
- O'Connor AM, Stacey D, Entwistle V, Llewellyn-Thomas H, Rovner D, Holmes-Rovner M, et al.Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No: CD001431. [DOI: 10.1002/14651858.CD001431.pub2] [DOI] [Google Scholar]
Odegaard 2004
- Odegaard KJ.Self-management in anticoagulation: a meta-analysis. Tidsskrift for Den Norske Laegeforening 2004;124(22):2900-3. [PubMed] [Google Scholar]
Oeseburg 2009
- Oeseburg B, Wynia K, Middel B, Reijneveld SA.Effects of case management for frail older people or those with chronic illness: a systematic review. Nursing Research 2009;58(3):201-10. [DOI] [PubMed] [Google Scholar]
Okoli 2010
- Okoli CT, Khara M, Procyshyn RM, Johnson JL, Barr AM, Greaves L.Smoking cessation interventions among individuals in methadone maintenance: a brief review. Journal of Substance Abuse Treatment 2010;38(2):191-9. [DOI] [PubMed] [Google Scholar]
Oldenmenger 2009
- Oldenmenger WH, Sillevis Smitt PA, Dooren S, Stoter G, Rijt CC.A systematic review on barriers hindering adequate cancer pain management and interventions to reduce them: a critical appraisal. European Journal of Cancer 2009;45(8):1370-80. [DOI] [PubMed] [Google Scholar]
Ontario HTA Series 2008
- Ontario Health Technology Assessment Series.Prevention of falls and fall-related injuries in community-dwelling seniors: an evidence-based analysis. Ministry of Health and Long-Term Care 2008;8(2):1-78. [PMC free article] [PubMed]
Oringanje 2009
- Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE.Interventions for preventing unintended pregnancies among adolescents. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No: CD005215. [DOI: 10.1002/14651858.CD005215.pub2] [DOI] [PubMed] [Google Scholar]
Page 2005
- Page T, Lockwood C, Conroy-Hiller T.Effectiveness of nurse-led cardiac clinics in adult patients with a diagnosis of coronary heart disease. International Journal of Evidence-Based Healthcare 2005;3:2-26. [DOI] [PubMed] [Google Scholar]
Pampallona 2002
- Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C.Patient adherence in the treatment of depression. British Journal of Psychiatry 2002;180:104-9. [DOI: 10.1192/bjp.180.2.104] [DOI] [PubMed] [Google Scholar]
Papadakis 2010
- Papadakis S, McDonald P, Mullen KA, Reid R, Skulsky K, Pipe A.Strategies to increase the delivery of smoking cessation treatments in primary care settings: a systematic review and meta-analysis. Preventive Medicine 2010;51(3-4):199-213. [DOI] [PubMed] [Google Scholar]
Paré 2007
- Paré G, Jaana M, Sicotte C.Systematic review of home telemonitoring for chronic diseases: the evidence base [2007 May-June]. Journal of the American Medical Informatics Association 14;14(3):269-77. [DOI: 10.1197/jamia.M2270] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parienti 2009
- Parienti JJ, Bangsberg DR, Verdon R, Gardner EM.Better adherence with once-daily antiretroviral regimens: a meta-analysis. Clinical Infectious Diseases 2009;48(4):484-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pearson 2009
- Pearson SA, Moxey A, Robertson J, Hains I, Williamson M, Reeve J, et al.Do computerised clinical decision support systems for prescribing change practice. BMC Health Services Research 2009;9(154). [DOI: 10.1186/1472-6963-9-154] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pegurri 2005
- Pegurri E, Fox-Rushby JA, Damian W.The effects and costs of expanding the coverage of immunisation services in developing countries: a systematic literature review. Vaccine 2005;23(13):1624-35. [DOI] [PubMed] [Google Scholar]
Pekkala 2002
- Pekkala E, Merinder L.Psychoeducation for schizophrenia. Cochrane Database of Systematic Reviews 2002, Issue 2. Art. No: CD002831. [DOI: 10.1002/14651858.CD002831] [DOI] [PubMed] [Google Scholar]
Pelletier 2001
- Pelletier KR.Studies of comprehensive health promotion and disease management programs at the worksite: 1998 -2000 update. American Journal of Health Promotion 2001;16(2):107-16. [DOI] [PubMed] [Google Scholar]
Petersen 2006
- Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S.Does pay-for-performance improve the quality of health care? Annals of Internal Medicine 2006;145(4):265-72. [DOI] [PubMed] [Google Scholar]
Petersen 2009
- Peterson MC.A systematic review of outcomes and quality measures in adult patients cared for by hospitalists vs nonhospitalists. Mayo Clinic Proceedings 2009;84(3):248-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pharoah 2006
- Pharoah F, Mari J, Rathbone J, Wong W.Family intervention for schizophrenia. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD000088. [DOI: 10.1002/14651858.CD000088.pub2] [DOI] [PubMed] [Google Scholar]
Pickup 2011
- Pickup JC, Freeman SC, Sutton AJ.Glycaemic control in type 1 diabetes during real time continuous glucose monitoring compared with self monitoring of blood glucose: meta-analysis of randomised controlled trials using individual patient data. BMJ 2011;343(d3805). [DOI: 10.1136/bmj.d3805] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pignone 2005
- Pignone M, DeWalt DA, Sheridan S, Berkman N, Lohr KN.Interventions to improve health outcomes for patients with low literacy. A systematic review. Journal of General Internal Medicine 2005;20(2):185-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pimouguet 2011
- Pimouguet C, Le Goff M, Thiébaut R, Dartigues JF, Helmer C.Effectiveness of disease-management programs for improving diabetes care: a meta-analysis. Canadian Medical Association Journal 2011;183(2):E115-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ploeg 2005
- Ploeg J, Feightner J, Hutchison B, Patterson C, Sigouin C, Gauld M.Effectiveness of preventive primary care outreach interventions aimed at older people: meta-analysis of randomized controlled trials. Canadian Family Physician 2005;51:1244-5. [PMC free article] [PubMed] [Google Scholar]
Polisena 2009
- Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K.Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obesity and Metabolism 2009;11(10):913-30. [DOI] [PubMed] [Google Scholar]
Polisena 2010
- Polisena J, Tran K, Cimon K, Hutton B, McGill S, Palmer K, et al.Home telemonitoring for congestive heart failure: a systematic review and meta-analysis. Journal of Telemedicine and Telecare 2010;16(2):68-76. [DOI] [PubMed] [Google Scholar]
Ponniah 2007
- Ponniah A, Anderson B, Shakib S, Doecke C J, Angley M.Pharmacists' role in the post-discharge management of patients with heart failure: a literature review. Journal of Clinical Pharmacy and Therapeutics. 2007;;32(4):343-52. [DOI] [PubMed] [Google Scholar]
Poolsup 2008
- Poolsup N, Suksomboon N.Systematic review of the benefits of self-monitoring of blood glucose on glycemic control in type 2 diabetes patients. Diabetes Technology & Therapeutics 2008;10(S1). [DOI: 10.1089/dia.2008.0001] [DOI] [PubMed] [Google Scholar]
Poolsup 2009
- Poolsup N, Suksomboon N, Rattanasookchit S.Meta-analysis of the benefits of self-monitoring of blood glucose on glycemic control in type 2 diabetes patients: an update. Diabetes Technology and Therapeutics 2009;11(12):775-84. [DOI] [PubMed] [Google Scholar]
Post 2009
- Post PN, Wittenberg J, Burgers JS.Do specialized centers and specialists produce better outcomes for patients with chronic diseases than primary care generalists? A systematic review. International Journal for Quality in Health Care 2009;21(6):387-96. [DOI] [PubMed] [Google Scholar]
Postma 2009
- Postma J, Karr C, Kieckhefer G.Community health workers and environmental interventions for children with asthma: a systematic review. Journal of Asthma 2009;46(6):564-76. [DOI] [PubMed] [Google Scholar]
Powell 2003
- Powell H, Gibson PG.Options for self-management education for adults with asthma. Cochrane Database of Systematic Reviews 2003, Issue 1. Art. No: CD004107. [DOI: 10.1002/14651858.CD004107] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rackal 2011
- Rackal JM, Tynan AM, Handford CD, Rzeznikiewz D, Agha A, Glazier R.Provider training and experience for people living with HIV/AIDS. Cochrane Database of Systematic Reviews 2011, Issue 6. Art. No: CD003938. [DOI: 10.1002/14651858.CD003938.pub2] [DOI] [PubMed] [Google Scholar]
Raymond 2007
- Raymond EG, Trussell J, Polis CB.Population effect of increased access to emergency contraceptive pills: a systematic review. Obstetrics and Gynecology 2007;109(1):181-8. [DOI] [PubMed] [Google Scholar]
Raynor 2007
Reda 2001
- Reda S, Makhoul S.Prompts to encourage appointment attendance for people with serious mental illness. Cochrane Database of Systematic Reviews 2001, Issue 2. Art. No: CD002085. [DOI: 10.1002/14651858.CD002085] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reda 2009
- Reda AA, Kaper J, Fikrelter H, Severens JL, Schayck CP.Healthcare financing systems for increasing the use of tobacco dependence treatment. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD004305. [DOI: 10.1002/14651858.CD004305.pub3] [DOI] [PubMed] [Google Scholar]
Reed 2010
- Reed DA, Fletcher KE, Arora VM.Systematic review: association of shift length, protected sleep time, and night float with patient care, residents' health, and education. Annals of Internal Medicine 2010;153(12):829-42. [DOI] [PubMed] [Google Scholar]
Reeves 2010
- Reeves S, Zwarenstein M, Goldman J, Barr H, Freeth D, Koppel I, et al.The effectiveness of interprofessional education: key findings from a new systematic review. Journal of Interprofessional Care 2010;24(3):230-41. [DOI] [PubMed] [Google Scholar]
Renders 2000
- Renders CM, Valk GD, Griffin SJ, Wagner E, Eijk JT, Assendelft WJJ.Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database of Systematic Reviews 2000, Issue 4. Art. No: CD001481. [DOI: 10.1002/14651858.CD001481] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rex 2006
- Rex J, Jensen KH, Lawton SA.A review of 20 years' experience with the NovoPen family of insulin injection devices. Clinical Drug Investigation 2006;26(7):367-401. [DOI] [PubMed] [Google Scholar]
Rice 2004
- Rice VH, Stead LF.Nursing interventions for smoking cessation. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD001188. [DOI: 10.1002/14651858.CD001188.pub2] [DOI] [PubMed] [Google Scholar]
Riemsma 2003
- Riemsma RP, Kirwan JR, Taal E, Rasker HJJ.Patient education for adults with rheumatoid arthritis. Cochrane Database of Systematic Reviews 2003, Issue 2. Art. No: CD003688. [DOI: 10.1002/14651858.CD003688] [DOI] [PubMed] [Google Scholar]
Rigotti 2008
- Rigotti NA, Munafo MR, Stead LF.Smoking cessation interventions for hospitalized smokers: a systematic review. Archives of Internal Medicine 2008;168(18):1950-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2010
- Robertson J, Walkom E, Pearson SA, Hains I, Williamsone M, Newby D.The impact of pharmacy computerised clinical decision support on prescribing, clinical and patient outcomes: a systematic review of the literature. International Journal of Pharmacy Practice 2010;18(2):69-87. [PubMed] [Google Scholar]
Roccaforte 2005
- Roccaforte R, Demers C, Baldassarre F, Teo KK, Yusuf S.Effectiveness of comprehensive disease management programmes in improving clinical outcomes in heart failure patients: a meta-analysis. European Journal of Heart Failure 2005;7(7):1133-44. [DOI] [PubMed] [Google Scholar]
Rollason 2003
- Rollason V, Vogt N.Reduction of polypharmacy in the elderly: a systematic review of the role of the pharmacist. Drugs & Aging 2003;20(11):817-32. [DOI] [PubMed] [Google Scholar]
Russell‐Minda 2009
- Russell-Minda E, Jutai J, Speechley M, Bradley K, Chudyk A, Petrella R.Health technologies for monitoring and managing diabetes: a systematic review. Journal of Diabetes Science and Technology 2009;3(6):1460-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryhanen 2010
- Ryhanen AM, Siekkinen M, Rankinen S Korvenranta H, Leino-Kilpi H.The effects of Internet or interactive computer-based patient education in the field of breast cancer: a systematic literature review. Patient Education and Counseling 2010;79(1):5-13. [DOI] [PubMed] [Google Scholar]
Sajatovic 2004
- Sajatovic M, Davies M, Hrouda DR.Enhancement of treatment adherence among patients with bipolar disorder. Psychiatric Services 2004;55(3):264-9. [DOI] [PubMed] [Google Scholar]
Saksena 2010
- Saksena A.Computer-based education for patients with hypertension: a systematic review. Health Education Journal 2010;69(3):246-45. [Google Scholar]
Samoocha 2010
- Samoocha D, Bruinvels DJ, Elbers NA, Anema JR, Beek AJ.Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. Journal of Medical Internet Research 2010;12(2):e23. [DOI: 10.2196/jmir.1286] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sanders 2006
- Sanders DL, Aronsky D.Biomedical informatics applications for asthma care: a systematic review. Journal of the American Medical Informatics Association 2006;13(4):418-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sangani 2001
- Sangani P, Rutherford G, Kennedy GE.Population-based interventions for reducing sexually transmitted infections, including HIV infection. Cochrane Database of Systematic Reviews 2004, Issue 3. Art. No: CD001220. [DOI: 10.1002/14651858.CD001220.pub2] [DOI] [PubMed] [Google Scholar]
Sanghera 2006
- Sanghera N, Chan PY, Khaki ZF, Planner C, Lee KK, Cranswick NE, et al.Interventions of hospital pharmacists in improving drug therapy in children: a systematic literature review. Drug Safety 2006;29(11):1031-47. [DOI] [PubMed] [Google Scholar]
Santschi 2011
- Santschi V, Chiolero A, Burnand B, Colosimo AL, Paradis G.Impact of pharmacist care in the management of cardiovascular disease risk factors: a systematic review and meta-analysis of randomized trials. Archives of Internal Medicine 2011;171(16):1441-53. [DOI] [PubMed] [Google Scholar]
Saokaew 2010
- Saokaew S, Permsuwan U, Chaiyakunapruk N, Nathisuwan S, Sukonthasarn A.Effectiveness of pharmacist-participated warfarin therapy management: a systematic review and meta-analysis. Journal of Thrombosis and Haemostasis 2010;8(11):2418-27. [DOI] [PubMed] [Google Scholar]
Savage 2011
- Savage E, Beirne PV, Ni Chroinin M, Duff A, Fitzgerald T, Farrell D.Self-management education for cystic fibrosis. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD007641. [DOI: 10.1002/14651858.CD007641.pub2] [DOI] [PubMed] [Google Scholar]
Schedlbauer 2004
- Schedlbauer A, Schroeder K, Peters TJ, Fahey T.Interventions to improve adherence to lipid lowering medication. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD004371. [DOI: 10.1002/14651858.CD004371.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schedlbauer 2007
- Schedlbauer A, Schroeder K, Fahey T.How can adherence to lipid-lowering medication be improved? A systematic review of randomized controlled trials. Family Practice 2007;24(4):380-7. [DOI] [PubMed] [Google Scholar]
Schedlbauer 2009
- Schedlbauer A, Prasad V, Mulvaney C, Phansalkar S, Stanton W, Bates DW, et al.What evidence supports the use of computerized alerts and prompts to improve clinicians' prescribing behavior? Journal of the American Medical Informatics Association 2009;16(4):531-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schiffman 2010
- Schiffman J, Darmstadt GL, Agarwal S, Baqui AH.Community-based intervention packages for improving perinatal health in developing countries: a review of the evidence. Seminars in Perinatology 2010;34(6):462-76. [DOI] [PubMed] [Google Scholar]
Schroeder 2004a
- Schroeder K, Fahey T, Ebrahim S.How can we improve adherence to blood pressure-lowering medication in ambulatory care? Archives of Internal Medicine 2004;164(7):722-32. [DOI] [PubMed] [Google Scholar]
Schuetz 2011
- Schuetz P, Chiappa V, Briel M, Greenwald JL.Procalcitonin algorithms for antibiotic therapy decisions: a systematic review of randomized controlled trials and recommendations for clinical algorithms. Archives of Internal Medicine 2011;171(15):1322-31. [DOI] [PubMed] [Google Scholar]
Scott 2003
- Scott JT, Harmsen M, Prictor MJ, Entwistle VA, Sowden AJ, Watt I.Recordings or summaries of consultations for people with cancer. Cochrane Database of Systematic Reviews 2003, Issue 2. Art. No: CD001539. [DOI: 10.1002/14651858.CD001539] [DOI] [PubMed] [Google Scholar]
Scott 2008
- Scott JT, Harmsen M, Prictor MJ, Sowden AJ, Watt I.Interventions for improving communication with children and adolescents about their cancer. Cochrane Database of Systematic Reviews 2003, Issue 3. Art. No: CD002969. [DOI: 10.1002/14651858.CD002969] [DOI] [PubMed] [Google Scholar]
Scott 2011
- Scott A, Sivey P, Ait Ouakrim D, Willenberg L, Naccarella L, Fuler J, et al.The effect of financial incentives on the quality of health care provided by primary care physicians. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD008451. [DOI: 10.1002/14651858.CD008451.pub2] [DOI] [PubMed] [Google Scholar]
Shahab 2009
- Shahab L, McEwen A.Online support for smoking cessation: a systematic review of the literature. Addiction 2009;104(11):1792-804. [DOI] [PubMed] [Google Scholar]
Shaw 2007
- Shaw EJ, Stokes T, Camosso-Stefinovic J, Baker R, Baker GA, Jacoby A.Self-management education for adults with epilepsy. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No: CD004723. [DOI: 10.1002/14651858.CD004723.pub2] [DOI] [PubMed] [Google Scholar]
Shea 2009
- Shea B, Andersson N, Henry D.Increasing the demand for childhood vaccination in developing countries: a systematic review. BMC International Health and Human Rights 2009;9(Supplement 1):S5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepperd 2004
- Shepperd S, Parkes J, McClaran J, Phillips C.Discharge planning from hospital to home. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD000313. [DOI: 10.1002/14651858.CD000313] [DOI] [PubMed] [Google Scholar]
Shepperd 2010
- Shepperd S, McClaran J, Phillips CO, Lannin NA, Clemson LM, McCluskey A, et al.Discharge planning from hospital to home. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD000313. [DOI: 10.1002/14651858.CD000313.pub3] [DOI] [PubMed] [Google Scholar]
Shojania 2009
- Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J.The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database of Systematic Reviews 2009, Issue 3. Art. No: CD001096. [DOI: 10.1002/14651858.CD001096.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shojania 2010
- Shojania KG, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J.Effect of point-of-care computer reminders on physician behaviour: a systematic review. Canadian Medical Association Journal 2010;182(5):E216-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siebenhofer 2004
- Siebenhofer A, Berghold A, Sawicki PT.Systematic review of studies of self-management of oral anticoagulation. Thrombosis and Haemostasis 2004;91(2):225-32. [DOI] [PubMed] [Google Scholar]
Simoni 2006
- Simoni JM, Pearson CR, Pantalone DW, Marks G, Crepaz N.Efficacy of interventions in improving Highly Active Antiretroviral Therapy adherence and HIV-1 RNA viral load: a meta-analytic review of randomized controlled trials. Journal of Acquired Immune Deficiency Syndrome 2006;43:S23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simpson 2005
- Simpson SH, Marrie TJ, Majumdar SR.Do guidelines guide pneumonia practice: a systematic review of interventions and barriers to best practice in the management of community-acquired pneumonia. Respiratory Care Clinics of North America 2005;11(1):1-13. [DOI] [PubMed] [Google Scholar]
Sinclair 2004
- Sinclair HK, Bond CM, Stead LF.Community pharmacy personnel interventions for smoking cessation. Cochrane Database of Systematic Reviews 2004, Issue 1. Art. No: CD003698. [DOI: 10.1002/14651858.CD003698.pub2] [DOI] [PubMed] [Google Scholar]
Smeets 2007
- Smeets HM, Hoes AW, Wit NJ.Effectiveness and costs of implementation strategies to reduce acid suppressive drug prescriptions: a systematic review. BMC Health Services Research November 2007;5(7):177. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smetana 2007
- Smetana GW, Landon BE, Bindman AB, Burstin H, Davis RB, Tjia J, et al.A comparison of outcomes resulting from generalist vs specialist care for a single discrete medical condition: a systematic review and methodologic critique. Archives of Internal Medicine 2007;167(1):10-20. [DOI] [PubMed] [Google Scholar]
Smith 2001
- Smith B, Appleton S, Adams R, Southcott A, Ruffin D.Home care by outreach nursing for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2001, Issue 3. Art. No: CD000994. [DOI: 10.1002/14651858.CD000994] [DOI] [PubMed] [Google Scholar]
Smith 2005
- Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BD, et al.A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma. Health Technology Assessment 2005;9(23):1-182. [DOI] [PubMed] [Google Scholar]
Smith 2007a
- Smith JR, Mugford M, Holland R, Noble MJ, Harrison BD.Psycho-educational interventions for adults with severe or difficult asthma: a systematic review. Journal of Asthma 2007;44(3):219-41. [DOI] [PubMed] [Google Scholar]
Smith 2007b
- Smith SM, Allwright S, O'Dowd T.Effectiveness of shared care across the interface between primary and specialty care in chronic disease management. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD004910. [DOI: 10.1002/14651858.CD004910.pub2] [DOI] [PubMed] [Google Scholar]
Smith 2007c
- Smith MY, DePue JD, Rini C.Computerized decision-support systems for chronic pain management in primary care. Pain Medicine 2007;8(s3):S155-s166. [Google Scholar]
Smith 2008
- Smith SM, Allwright S, O'Dowd T.Does sharing care across the primary-specialty interface improve outcomes in chronic disease? A systematic review. American Journal of Managed Care April 2008;14(4):213-24. [PubMed] [Google Scholar]
Smith 2010
- Smith CA.A systematic review of healthcare professional-led education for patients with osteoporosis or those at high risk for the disease. Orthopaedic Nursing 2010;29(2):119-32. [DOI] [PubMed] [Google Scholar]
Sorsdahl 2009
- Sorsdahl K, Ipser JC, Stein DJ.Interventions for educating traditional healers about STD and HIV medicine. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No: CD007190. [DOI: 10.1002/14651858.CD007190.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stacey 2011
- Stacey D, Bennett CL, Barry MJ, Col NF, Eden KB, Holmes-Rovner M, et al.Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD001431. [DOI: 10.1002/14651858.CD001431.pub3] [DOI] [PubMed] [Google Scholar]
Steffen 2009
- Steffen S, Kösters M, Becker T, Puschner B.Discharge planning in mental health care: a systematic review of the recent literature. Acta Psychiatrica Scandinavica 2009;120(1):1-9. [DOI] [PubMed] [Google Scholar]
Stemer 2010
- Stemer G, Lemmens-Gruber R.Clinical pharmacy services and solid organ transplantation: a literature review. Pharmacy World and Science 2010;32(1):7-18. [DOI] [PubMed] [Google Scholar]
Stinson 2009
- Stinson J, Wilson R, Gill N, Yamada J, Holt J.A systematic review of internet-based self-management interventions for youth with health conditions. Journal of Pediatric Psychology 2009;34(5):495-510. [DOI] [PubMed] [Google Scholar]
St John 2009
- St John A, Davis WA, Price CP, Davis TM.The value of self-monitoring of blood glucose: a review of recent evidence. Journal of Diabetes Complications 2010;24(2):129-41. [DOI] [PubMed] [Google Scholar]
Stokes 2007
- Stokes T, Shaw EJ, Camosso-Stefinovic J, Baker R, Baker GA, Jacoby A.Self-management education for children with epilepsy. Cochrane Database of Systematic Reviews 2007, Issue 2. Art. No: CD004724. [DOI: 10.1002/14651858.CD004724.pub2] [DOI] [PubMed] [Google Scholar]
Stolic 2010
- Stolic S, Mitchell M, Wollin J.Nurse-led telephone interventions for people with cardiac disease: a review of the research literature. European Journal of Cardiovascular Nursing 2010;9(4):203-17. [DOI] [PubMed] [Google Scholar]
Sutcliffe 2011
- Sutcliffe P, Martin S, Sturt J, Powell J, Griffiths F, Adams A, et al.Systematic review of communication technologies to promote access and engagement of young people with diabetes into healthcare. BMC Endocrine Disorders 2011;11(1). [DOI: 10.1186/1472-6823-11-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Szilagyi 2000
- Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, et al.Effect of patient reminder/recall interventions on immunization rates: a review. JAMA 2000;284(14):1820-7. [DOI] [PubMed] [Google Scholar]
Tapp 2007
- Tapp S, Lasserson TJ, Rowe B.Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No: CD003000. [DOI: 10.1002/14651858.CD003000.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2005
- Taylor SJC, Bestall JC, Cotter S, Falshaw M, Hood SG, Parsons S, et al.Clinical service organisation for heart failure. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD002752. [DOI: 10.1002/14651858.CD002752.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2010b
- Thomas RE, Russell ML, Lorenzetti DL.Systematic review of interventions to increase influenza vaccination rates of those 60 years and older. Vaccine 2010;28(7):1684-701. [DOI] [PubMed] [Google Scholar]
Tieu 2010
- Tieu J, Middleton P, Crowther CA.Preconception care for diabetic women for improving maternal and infant health. Cochrane Database of Systematic Reviews 2010, Issue 12. Art. No: CD007776. [DOI: 10.1002/14651858.CD007776.pub2] [DOI] [PubMed] [Google Scholar]
Toelle 2004
- Toelle BG, Ram FS.Written individualised management plans for asthma in children and adults. Cochrane Database of Systematic Reviews 2004, Issue 2. Art. No: CD002171. [DOI: 10.1002/14651858.CD002171.pub2] [DOI] [PubMed] [Google Scholar]
Towfigh 2008
- Towfigh A, Romanova M, Weinreb JE, Munjas B, Suttorp MJ, Zhou A, et al.Self-monitoring of blood glucose levels in patients with type 2 diabetes mellitus not taking insulin: a meta-analysis. American Journal of Managed Care July 2008;14(7):468-75. [PubMed] [Google Scholar]
Tremblay 2008
- Tremblay A, Sheeran L, Aranda SK.Psychoeducational interventions to alleviate hot flashes: a systematic review. Menopause 2008 Jan-Feb;15(1):193-202. [DOI] [PubMed] [Google Scholar]
Tsai 2005
- Tsai AC, Morton SC, Mangione CM, Keeler EB.A meta-analysis of interventions to improve care for chronic illnesses. American Journal of Managed Care 2005;11(8):478-88. [PMC free article] [PubMed] [Google Scholar]
Tully 2000
- Tully MP, Seston EM.Impact of pharmacists providing a prescription review and monitoring service in ambulatory care or community practice. Annals of Pharmacotherapy 2000;34(11):1320-31. [DOI] [PubMed] [Google Scholar]
Turnock 2005
- Turnock AC, Walters EH, Walters JA, Wood-Baker R.Action plans for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2005, Issue 4. Art. No: CD005074. [DOI: 10.1002/14651858.CD005074] [DOI] [PubMed] [Google Scholar]
Urquhart 2005
- Urquhart C, Currell R.Reviewing the evidence on nursing record systems. Health Informatics Journal 2005;11(1):33-44. [Google Scholar]
Vaapio 2009
- Vaapio SS, Salminen MJ, Ojanlatva A, Kivelä SL.Quality of life as an outcome of fall prevention interventions among the aged: a systematic review. European Journal of Public Health 2009;19(1):7-15. [DOI: 10.1093/eurpub/ckn099.] [DOI] [PubMed] [Google Scholar]
Valk 2005
- Valk GD, Kriegsman DMW, Assendelft WJJ.Patient education for preventing diabetic foot ulceration. Cochrane Database of Systematic Reviews 2001, Issue 4. Art. No: CD001488. [DOI: 10.1002/14651858.CD001488.pub2] [DOI] [PubMed] [Google Scholar]
Van der Wal 2005
- Van der Wal MH, Jaarsma T, Veldhuisen DJ.Non-compliance in patients with heart failure: how can we manage it? European Journal of Heart Failure 2005;7(1):5-17. [DOI] [PubMed] [Google Scholar]
van Rosse 2009
- Rosse F, Maat B, Rademaker CM, Vught AJ, Egberts AC, Bollen CW.The effect of computerized physician order entry on medication prescription errors and clinical outcome in pediatric and intensive care: a systematic review. Pediatrics 2009;123(4):1184-90. [DOI: 10.1542/peds.2008-1494] [DOI] [PubMed] [Google Scholar]
Viswanathan 2009
- Viswanathan M, Kraschnewski J, Nishikawa B, Morgan LC, Thieda P, Honeycutt A, et al.Outcomes of community health worker interventions . Evidence Report / Technology Assessment June 2009;181:1-144. [PMC free article] [PubMed] [Google Scholar]
Volmink 1997
- Volmink J, Garner P.Systematic review of randomised controlled trials of strategies to promote adherence to tuberculosis treatment. BMJ 1997;315:1403-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Von Gunten 2007
- Von Gunten V, Reymond JP, Beney J.Clinical and economic outcomes of pharmaceutical services related to antibiotic use: a literature review. Pharmacy World Science 2007;29(3):146-63. [DOI] [PubMed] [Google Scholar]
Walburn 2001
- Walburn J, Gray R, Gournay K, Quraishi S, David AS.Systematic review of patient and nurse attitudes to depot antipsychotic medication. British Journal of Psychiatry 2001;179(4):300-7. [DOI] [PubMed] [Google Scholar]
Walker 2010
- Walker BF, French SD, Grant W, Green S.Combined chiropractic interventions for low-back pain. Cochrane Database of Systematic Reviews 2010, Issue 4. Art. No: CD005427. [DOI: 10.1002/14651858.CD005427.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walton 2008
- Walton T, Harvey E, Dovey S, Freemantle N.Computerised advice on drug dosage to improve prescribing practice. Cochrane Database of Systematic Reviews 2008, Issue 3. Art. No: CD002894. [DOI: 10.1002/14651858.CD002894] [DOI] [PubMed] [Google Scholar]
Watson 2009
- Watson PW, McKinstry B.A systematic review of interventions to improve recall of medical advice in healthcare consultations. Journal of the Royal Society of Medicine 2009;102(6):235-43. [DOI: doi: 10.1258/jrsm.2009.090013.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Webel 2010
- Webel AR, Okonsky J, Trompeta J, Holzemer WL.A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. American Journal of Public Health 2010;100(2):247-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wei 2011
- Wei I, Pappas Y, Car J, Sheikh A, Majeed A.Computer-assisted versus oral-and-written dietary history taking for diabetes mellitus. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD008488. [DOI: 10.1002/14651858.CD008488.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Welschen 2005
- Welschen LMC, Bloemendal E, Nijpels G, Dekker JM, Heine RJ, Stalman WAB, et al.Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No: CD005060. [DOI: 10.1002/14651858.CD005060.pub2] [DOI] [PubMed] [Google Scholar]
Welsh 2011
- Welsh EJ, Hasan M, Li P.Home-based educational interventions for children with asthma. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD008469. [DOI: 10.1002/14651858.CD008469.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wendt 1998
- Wendt DA.Evaluation of medication management interventions for the elderly. Home Healthcare Nurse 1998;16(9):612-7. [DOI] [PubMed] [Google Scholar]
Wens 2008
- Wens J, Vermeire E, Hearnshaw H, Lindenmeyer A, Biot Y, Van Royen P.Educational interventions aiming at improving adherence to treatment recommendations in type 2 diabetes: a sub-analysis of a systematic review of randomised controlled trials. Diabetes Research and Clinical Practice 2008;79(3):377-88. [DOI] [PubMed] [Google Scholar]
Werawatganon 2005
- Werawatganon T, Charuluxananan S.Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No: CD004088. [DOI: 10.1002/14651858.CD004088.pub2] [DOI] [PubMed] [Google Scholar]
White 2010
- White HJ, Bettiol SS, Perera R, Roberts NW, Javaid MK, Farmer AJ.A systematic review assessing the effectiveness of interventions to improve persistence with anti-resorptive therapy in women at high risk of clinical fracture. Family Practice 2010;27(6):593-603. [DOI] [PubMed] [Google Scholar]
Whittaker 2002
- Whittaker K.Lay workers for improving the uptake of childhood immunization. British Journal of Community Nursing 2002;7(9):474-9. [DOI] [PubMed] [Google Scholar]
Winkley 2006
- Winkley K, Ismail K, Landau S, Eisler I.Psychological interventions to improve glycaemic control in patients with type 1 diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ 2006;333:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winterbottom 2008
- Winterbottom JB, Smyth RMD, Jacoby A, Baker GA.Preconception counselling for women with epilepsy to reduce adverse pregnancy outcome. Cochrane Database of Systematic Reviews 2008, Issue 3. Art. No: CD006645. [DOI: 10.1002/14651858.CD006645.pub2] [DOI] [PubMed] [Google Scholar]
Wise 2007
- Wise PH, Huffman LC, Brat G.A critical analysis of care coordination strategies for children with special health care needs. Agency for Healthcare Research and Quality 2007;36. [PubMed]
Wise 2008
- Wise J, Operario D.Use of electronic reminder devices to improve adherence to antiretroviral therapy: a systematic review. AIDS Patient Care and STDs June 2008;22(6):495-504. [DOI] [PubMed] [Google Scholar]
Witter 2012
- Witter S, Fretheim A, Kessy FL, Lindahl AK.Paying for performance to improve the delivery of health interventions in low- and middle-income countries. Cochrane Database of Systematic Reviews 2012, Issue 2. Art. No: CD007899. [DOI: 10.1002/14651858.CD007899.pub2] [DOI] [PubMed] [Google Scholar]
Wofford 2005
- Wofford JL, Smith ED, Miller DP.The multimedia computer for office-based patient education: a systematic review. Patient Education and Counseling 2005;59(2):148-57. [DOI] [PubMed] [Google Scholar]
Wolf 2003
- Wolf F, Guevara JP, Grum CM, Clark NM, Cates CJ.Educational interventions for asthma in children. Cochrane Database of Systematic Reviews 2002, Issue 4. Art. No: CD000326. [DOI: 10.1002/14651858.CD000326] [DOI] [PubMed] [Google Scholar]
Wolfstadt 2008
- Wolfstadt JI, Gurwitz JH, Field TS, Lee M, Kalkar S, Wu W et al.The effect of computerized physician order entry with clinical decision support on the rates of adverse drug events: a systematic review. Journal of General Internal Medicine 2008;23(4):451-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wong 2010
- Wong K, Yu SK, Holbrook A.A systematic review of medication safety outcomes related to drug interaction software. Journal of Population Therapeutics and Clinical Pharmacology 2010 Summer;17(2):e243-55. [PubMed] [Google Scholar]
Woolacott 2006
- Woolacott N, Orton L, Beynon S, Myers L, Forbes C.Systematic review of the clinical effectiveness of self care support networks in health and social care. University of York, Centre for Reviews and Dissemination 2006;291.
Wu 2010
- Wu L, Forbes A, Griffiths P, Milligan P, While A.Telephone follow-up to improve glycaemic control in patients with type 2 diabetes: systematic review and meta-analysis of controlled trials. Diabetic Medicine 2010;27(11):1217-25. [DOI] [PubMed] [Google Scholar]
Young 2010
- Young T, Busgeeth K.Home-based care for reducing morbidity and mortality in people infected with HIV/AIDS. Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No: CD005417. [DOI: 10.1002/14651858.CD005417.pub2] [DOI] [PubMed] [Google Scholar]
Yourman 2008
- Yourman L, Concato J, Agostini JV.Use of computer decision support interventions to improve medication prescribing in older adults: a systematic review. American Journal of Geriatric Pharmacotherapy 2008 June;6(2):119-29. [DOI] [PubMed] [Google Scholar]
Yu 2006
- Yu DS, Thompson DR, Lee DT.Disease management programmes for older people with heart failure: crucial characteristics which improve post-discharge outcomes. European Heart Journal 2006;27(5):596-612. [DOI] [PubMed] [Google Scholar]
Yuen 2010
- Yuen A, Sugeng Y, Weiland TJ, Jelinek GA.Lifestyle and medication interventions for the prevention or delay of type 2 diabetes mellitus in prediabetes: a systematic review of randomised controlled trials. Australian and New Zealand Journal of Public Health 2010;34(2):172-8. [DOI] [PubMed] [Google Scholar]
Zaki 2009
- Zaki A, Abrishami A, Wong J, Chung FF.Interventions in the preoperative clinic for long term smoking cessation: a quantitative systematic review. Canadian Journal of Anaesthesia 2009;55(1):11-21. [DOI: 10.1007/BF03017592] [DOI] [PubMed] [Google Scholar]
Zedler 2011
- Zedler BK, Kakad P, Colilla S, Murrelle L, Shah NR.Does packaging with a calendar feature improve adherence to self-administered medication for long-term use? A systematic review. Clinical Therapeutics 2011;33(1):62-73. [DOI] [PubMed] [Google Scholar]
Zhang 2007
- Zhang X, Norris SL, Chowdhury FM, Gregg EW, Zhang P.The effects of interventions on health-related quality of life among persons with diabetes: a systematic review. Medical Care 2007;45(9):820-34. [DOI] [PubMed] [Google Scholar]
Additional references
Akl 2011
- Akl EA, Oxman AD, Herrin J, Vist GE, Terrenato I, Sperati F, et al.Using alternative statistical formats for presenting risks and risk reductions. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No: CD006776. [DOI: 10.1002/14651858.CD006776.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyd 2005
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW.Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 2005;294(6):716-24. [DOI] [PubMed] [Google Scholar]
Britten 2004
- Britten N, Stevenson F, Gafaranga J, Barry C, Bradley C.The expression of aversion to medicines in general practice consultations. Social Science and Medicine 2004;59:1495-503. [DOI] [PubMed] [Google Scholar]
Brown 2012
- Brown TM, Siu K, Walker D, Pladevall-Vila M, Sander S, Mordin M.Development of a conceptual model of adherence to oral anticoagulants to reduce risk of stroke in patients with atrial fibrillation. Journal of Managed Care Pharmacy June 2012;18(5):351-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Candy 2011
- Candy B, King M, Jones L, Oliver S.Using qualitative evidence on patients’ views to help understand variation in effectiveness of complex interventions: a qualitative comparative analysis. BMC Medical Research Methodology 2011;11:124. [http://www.biomedcentral.com/1471-2288/11/124] [Google Scholar]
Candy 2013
- Candy B, King M, Jones L, Oliver S.Using qualitative evidence on patients’ views to help understand variation in effectiveness of complex interventions: a qualitative comparative analysis. Trials 2013;14:179. [http://www.trialsjournal.com/content/14/1/179] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chetley 2007
- Chetley A, Hardon A, Hodgkin C, Haaland A, Fresle DA.How to improve the use of medicines by consumers. apps.who.int/medicinedocs/documents/s14229e/s14229e.pdf (accessed 13 April 2010).
Coleman 2006
- Coleman EA, Parry C, Chalmers S, Min SJ.The care transitions: results of a randomised controlled trial. Archives of Internal Medicine 2006;166:1822-8. [DOI] [PubMed] [Google Scholar]
Coulter 2006
- Coulter A, Ellins J.Patient-focused Interventions. A review of the evidence. www.pickereurope.org/Filestore/Publications/QEI_Review_AB.pdf August 2006.
Dickinson 2003
- Dickinson D, Raynor DKT, Kennedy LG, Bonaccorso S, Sturchio JL.What information do patients need about medicines? BMJ 2003;327:861-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
EPOC 2013
- Effective Practice and Organisation of Care Group.Study Designs for EPOC Reviews. http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/EPOC%20Study%20Designs%20About.pdf [accessed 18 June 2013].
Feldstein 2006
- Feldstein AC, Smith DH, Perrin N, Yang X, Rix M, Raebel MA, et al.Improved therapeutic monitoring with several interventions: a randomised trial. Archives of Internal Medicine 2006;166:1848-54. [DOI] [PubMed] [Google Scholar]
Fortin 2005
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L.Prevalence of multimorbidity among adults seen in family practice. Annals of Family Medicine 2005;3:223-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fortin 2007
- Fortin M, Soubhi H, Hudon C, Bayliss EA, den Akker M.Multimorbidity's many challenges. BMJ 2007;334:1016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gadkari 2012
- Gadkari AS, McHorney CA.Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Services Research 2012;12:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garner 2007
- Garner P, Smith H, Munro S, Volminck J.Promoting adherence to tuberculosis treatment. Bulletin of the World Health Organization 2007;85(5):404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors).Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration. Available from www.cochrane-handbook.org. 2011 [updated March 2011];Version 5.1.0.
Holloway 2011
- Holloway K, Dijk L.The World Medicines Situation 2011, 3rd edition. http://apps.who.int/medicinedocs/documents/s18064en/s18064en.pdf. Accessed July 15 2013. 2011.
Little 2001
- Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, et al.Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ 2001;322(7284):468-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowe 2010
- Lowe D, Ryan R, Santesso N, Hill S.Development of a taxonomy of interventions to organise the evidence on consumers' medicines use. Patient Education and Counseling 2010. [DOI: 10.1016/j.pec.2010.09.024] [DOI] [PubMed] [Google Scholar]
May 2009
- May C, Montori VM, Mair FS.We need minimally disruptive medicine. BMJ 2009;339:b2803. [DOI] [PubMed] [Google Scholar]
Mishra 2011
- Mishra SI, Gioia D, Childress S, Barnet B, Webster RL.Adherence to medication regimens among low-income patients with multiple comorbid chronic conditions. Health Social Work November 2011;36(4):249-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2007
- Moher D, Tetzlaff J, Tricco, AC, Sampson M, Altman DG.Epidemiology and reporting characteristics of systematic reviews. PLoS Medicine 2007;4(3):e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Munro 2007
- Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J.Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Medicine 2007;4(7):e238. [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2009
- National Institute for Health and Clinical Excellence.Medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. http://guidance.nice.org.uk/CG76 (accessed 15 July 2013).
O'Connor 2006
- O'Connor PJ.Improving medication adherence: challenges for physicians, payers and policy makers. Archives of Internal Medicine 2006;166:1802-4. [DOI] [PubMed] [Google Scholar]
Pound 2005
- Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al.Resisting medicines: a synthesis of qualitative studies of medicine taking. Social Science and Medicine 2005;61:133-55. [DOI] [PubMed] [Google Scholar]
Ratanawongsa 2013
- Ratanawongsa N, Karter A, Parker MM, Lyles CR, Heisler M, Moffet HH, et al.Communication and medication adherence: the diabetes study of Northern California. JAMA Internal Medicine 2013;173(3):210-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2005
- Ryan RE, Hill S.Developing an overview of Cochrane systematic reviews: a framework for synthesising the evidence on interventions to improve people's involvement in healthcare. (Poster) XIII Cochrane Colloquium, Melbourne October 2005.
Ryan 2009a
- Ryan RE, Kaufman CA, Hill SJ.Building blocks for meta-synthesis: data integration tables for summarising, mapping, and synthesising evidence on interventions for communicating with health consumers. BMC Medical Research Methodology 2009 Mar 4;9(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2009b
- Ryan R, Hill S, Broclain D, Horey D, Oliver S, Prictor M.Cochrane Consumers and Communication Review Group. Study Design Guide. http://cccrg.cochrane.org/author-resources July 2009 (accessed 19 January 2010).
Ryan 2009c
- Ryan R, Hill S.Multimorbidity decision burden for medicines not recognised. BMJ (letter) 19 August 2009. [Google Scholar]
Ryan 2010
- Ryan R, Lowe D, Santesso N, Hill S.Development of a taxonomy of interventions directed at consumers to promote evidence-based prescribing and medicines use: a tool for evidence-based decision-making. In: National Medicines Symposium 26-28 May 2010, Melbourne. Vol. Abstract number 273. 2010:191.
Ryan 2011a
- Ryan RE, Weir M, Leslie B, Worswick J, Lowe DB, Hill SJ.Evidence on optimal prescribing and medicines use for decision makers: scope and application of the Rx for Change Database. Journal of Pharmacy Practice and Research 2011;41(4):295-9. [Google Scholar]
Ryan 2011c
- Ryan R, Hill S.Managing multiple health problems: is there evidence to support consumer-focused communication and participation. In: Hill S, editors(s). The Knowledgeable Patient. Chichester: Wiley Blackwell, 2011:161-72. [Google Scholar]
Ryan 2013
- Ryan R, Hill S.Improving the experiences and health of people with multimorbidity: exploratory research with policymakers and information providers on comorbid arthritis. Australian Journal of Primary Health 20 March 2013:(online early). [DOI: 10.1071/PY12083] [DOI] [PubMed] [Google Scholar]
Schoen 2005
- Schoen C, Osborn R, Huynh PT, Doty M, Zapert M, Peugh J, et al.Taking the pulse of health care systems: experiences of patients with health problems in six countries. Health Affairs 3 November 2005;web exclusive:W5-509 - W5-525. [DOI] [PubMed] [Google Scholar]
Shea 2007
- Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al.Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology 2007;15(7):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simpson 2006
- Simpson SH, Eurich DT, Majumdar SR, Padwall RS, Tsuyuki RT, Varney J, et al.A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006;333(7557):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2012
- Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T.Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database of Systematic Reviews 2012, Issue 4. Art. No: CD006560. [DOI: 10.1002/14651858.CD006560.pub2] [DOI] [PubMed] [Google Scholar]
Soumerai 2006
- Soumerai SB, Pierre-Jacquaes M, Zhang F, Ross-Degnan AS, Adams AS, Gurwitz J, et al.Cost-related medication nonadherence among elderly and disabled Medicare beneficiaries: a national survey 1 year before the Medicare drug benefit. Archive of Internal Medicine 2006;166:1829-35. [DOI] [PubMed] [Google Scholar]
Starfield 2003
- Starfield B.Threads and yarns: weaving the tapestry of comorbidity. Annals of Family Medicine 2003;4:101-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tarn 2006a
- Tarn DM, Heritage J, Paterniti DA, Hays RD, Kravitz RL, Wenger NS.Physician communication when prescribing new medications. Archive of Internal Medicine 2006;166:1855-62. [DOI] [PubMed] [Google Scholar]
Tarn 2006b
- Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS.Physician communication about the cost and acquisition of newly prescribed medications. American Journal of Managed Care 2006;12(11):657-64. [PubMed] [Google Scholar]
Topinkova 2012
- Topinkova E, Baeyens JP, Michel JP, Lang PO.Evidence-based strategies for the optimization of pharmacotherapy in older people. Drugs & Aging 2012;29(6):477-94. [DOI] [PubMed] [Google Scholar]
Townsend 2003
- Townsend A, Hunt K, Wyke S.Managing multiple morbidity in mid-life: a qualitative study of attitudes to drug use. BMJ 2003;327(7419):837. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trumble 2006
- Trumble S, O'Brien M, O'Brien M, Hartwig B.Communication skills training for doctors increases patient satisfaction. Clinical Governance: An International Journal 2006;11:299-307. [Google Scholar]
Van Dulmen 2007
- Van Dulmen S, Sluijs E, Dijk L, Ridder D, Heerdink R, Bensing J.Patient adherence to medical treatment: a review of reviews. BMC Health Services Research 2007;7(55). [DOI: 10.1186/1472-6963-7-55] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viswanathan 2012
- Viswanathan M, Golin CE, Jones CD, Askok M, Blalock SJ, Wines RCM, et al.Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Annals of Internal Medicine 2012;157:785-95. [DOI] [PubMed] [Google Scholar]
Weir 2009
- Weir M, Mayhew A, Worswick JFD, Grimshaw J.The Epidemiology and Quality of Systematic Reviews of Health Professional Behaviour Change Interventions. In: 17th Cochrane Colloquium: 11-14 October 2009. www.imbi.unifreiburg.de/OJS/cca/index.php/cca/article/view/8042.
Zorzela 2014
- Zorzela L, Golder S, Liu Y, Pilkington K, Hartling L, Joffe A, et al.Quality of reporting in systematic reviews of adverse events: systematic review. BMJ 2014;348. [DOI: 10.1136/bmj.f7668] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Ryan 2008
- Ryan R, Santesso N, Hill S, Kaufman C, Grimshaw J.Consumer-oriented interventions for evidence-based prescribing and medicine use: an overview of Cochrane reviews. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No: CD007508. [DOI: 10.1002/14651858.CD007508] [DOI] [PubMed] [Google Scholar]
Ryan 2009
- Ryan R, Santesso N, Hill S, Kaufman C, Grimshaw J.Consumer-oriented interventions for evidence-based prescribing and medicine use: an overview of Cochrane reviews. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD007768. [DOI: 10.1002/14651858.CD007768] [DOI] [PubMed] [Google Scholar]
Ryan 2011b
- Ryan R, Santesso N, Hill S, Lowe D, Kaufman C, Grimshaw J.Consumer-oriented interventions for evidence-based prescribing and medicines use: an overview of systematic reviews. Cochrane Database of Systematic Reviews 2011, Issue 5. Art. No: CD007768. [DOI: 10.1002/14651858.CD007768.pub2] [DOI] [PubMed] [Google Scholar]


