Abstract
Fractures of the proximal humerus are a very common presentation in modern Trauma and Orthopaedic practice. In an ever-aging population, the incidence has dramatically increased resulting in a large socioeconomical burden.
The surgical management of these injuries has evolved over the years. Patient outcomes are variable and there is no consensus on treatment approach. This review article focuses on the outcomes following fracture fixation using common surgical techniques.
1. Introduction
Fractures of the proximal humerus are very common and account for 6–10% of all fractures.1,2 Their incidence is rapidly increasing with age and they are the third most common fractures in those over 65 years of age.3 Women are three times more likely to sustain a proximal humeral fracture compared to men.1,2 In 90% of cases, fractures result from a low energy trauma such as falling from standing height.3 Other causes include direct blow to the shoulder, fracture dislocation secondary to epileptic fit or electrical shock.3
The burden created by these fractures is quite significant, especially in the elderly. The vast majority of these patients are still active and, subsequently to the injury, lose their independence in terms of activities of daily living.3 This undoubtedly affects their quality of life and renders them reliant on others for assistance.3 The estimated cost to the French Health System, which is similar to the UK with a comparable population, for dealing with consequences and rehabilitation is over €86 million a year.4
1.1. Literature review
Management remains controversial. Conservative treatment is generally accepted for minimally displaced fractures which account for 80% of all fractures with good reported functional outcomes.3 Surgery is considered for displaced and unstable fractures. The aim of surgical fixation is to achieve a stable anatomical construct that allows pain free early mobilisation, bony union and early return to activities.5 Fixation can be achieved through plate fixation, intramedullary device or percutaneously using k-wires. For displaced and severely comminuted fractures, joint replacement could also be offered in the form of hemiarthroplasty or reverse shoulder replacement.6
Good outcomes are reported with the majority of studies looking at operative interventions.6 However, most studies have no control groups and often only look at simple fracture patterns. A recent Cochrane review looking at 23 randomised-controlled trials (RCTs) concluded that not enough evidence is available to provide recommendation for conservative or any different surgical intervention.7 However, a large number of included articles come from the early days of surgical fixation with implants that are mostly no longer in use and have been superseded by more advanced implants.
A more recent RCT looking at the effectiveness of surgery versus non-surgical management of displaced fractures in adults concluded that there was no difference in clinical outcomes at two years.6 Nevertheless, a retrospective cohort study looking at functional outcomes for operative versus non-operative patients taking into account age and fracture type concluded that surgery has a better functional outcome than conservative management at all ages, especially young patients.8 This does not include plate fixation where no difference between surgery and conservative management was found.8
This review will focus on the outcomes of fracture fixation using plates, nails or pinning techniques.
1.2. Fracture classification
Proximal humeral fractures are generally described by the number of parts generated, level of displacement and angulation to each other.9 The most quoted system used is the Neer classification from the 1970s which relies on Codman's description (almost a century earlier) on how fractures follow lines of epiphyseal fusion.3,9
The humeral head is a distinct part where articular cartilage covers a dense subchondral bone. The articular cartilage margin is attached to the joint capsule and this area is thin, rendering it vulnerable to fractures. This is described as the anatomical neck. The fracture lines can propagate here into the head leading to articular damage.
The most common fractures occur at the surgical neck area.1,7 The humeral shaft is a thick mechanically strong cortical bone and as it proximally expands to form the metaphysis, its mechanical properties weaken rendering it liable to fractures. Moreover, the metaphysis expands further proximally in between the rotator cuff attachments at the tuberosities. Fracture displacement occurs due to the mechanical pull of the rotator cuff tendons attachments to the greater and lesser tuberosities as the fracture lines propagate between them.10 Hence, these tuberosities form two further parts that either separate from the anatomical head or surgical neck.
Neer's classification has a complex but clear criteria about part displacement (>1 cm gap) or angulation/rotation between the parts (>45°).9 Therefore, fractures could range from a one part minimally displaced fracture to two, three and four parts fracture. Two more categories were later added - head dislocation and head splitting.9,10
However, Hertel et al.10 simplified this by describing the parts as different blocks of Lego that could separate in different combinations with distinct treatment options that have different prognostic features. Furthermore, Hertel et al. described the loss of the medial hinge in posteriomedial metaphyseal fracture extension as the most important predictor of ischaemia and resistance to varus collapse leading to failure of fixation (see later).10
1.3. Outcomes of surgical fixation
Different surgical fixation methods have been used in the management of proximal humeral fractures. Surgical outcomes rely on patient and surgical factors7,8 (Table 1).
Table 1.
Patient and surgical factors affection proximal humeral management.
| Patient factors | Surgical factors |
|---|---|
| Age | Implant choice |
| Bone quality | Surgical planning |
| Fracture configuration | Surgical technique |
| Health status | Expertise |
| Rehabilitation | |
| Compliance |
Surgical techniques can be categorised into three different groups: percutaneous Kirschner wires, proximal humeral nails, and fixation using locking plates. In otherwise fit and healthy patients, age, fracture type and bone quality play a vital part in the success of surgery.7
2. Percutaneous Kirschner wire (K-wire)
This is one of the first techniques used in the surgical management of proximal humeral fractures.11 It is suitable for two-part displaced fractures which make up 20–30% of all proximal humeral fractures.8,11
Under X-ray guidance, closed reduction is first achieved with traction and manipulation of the fracture. This can also be supported by temporary non-threaded k-wires to joystick and manipulate the fracture into position. Two threaded K-wires are inserted above the deltoid insertion and directed proximally into the head. This can be further reinforced by two more threaded k-wires starting from the tuberosities directed distally into the humeral shaft.
It is a technically demanding procedure, but good results are reported in the literature. A recent cohort study investigating all three surgical options mentioned above as well as hemiarthroplasty for displaced 2 and 3 parts fractures against conservative management found K-wire fixation has a superior Constant Score of 68.7 when compared to conservative management.8 Furthermore, a case series that looked at 27 patients undergoing K-wire fixation in 2- and 3-part fractures and fixed with percutaneous screws showed excellent results with a mean Constant score of 89.9 at 1–3 year follow up.12
Another emergent technique is the use of metal humeral block screwed into the lateral humeral cortex to secure wires threaded into the head at 35°to the shaft and 25°to each other. Screws can be added to secure other fragments if necessary. Early results show a good mean Constant score of 80–90 compared to the contralateral arm.13,14
K-wire fixation is generally safe with minimal blood loss, less soft tissue disruption, shorter operative time and low cost.13,14 However, it is associated with complications such as pin site infection, fracture collapse, neurovascular injury, fracture malunion and pin migration.15 If a humeral metal block is used removal in a second operation is common due to the bulkiness of the block.14 In patients with significantly osteoporotic bone, they should be warned regarding the risk of construct failure or collapse. Nevertheless, in patients with multiple co-morbidities where open surgery is contraindicated this technique is considered safe and valuable.16
3. Open reduction and internal fixation using locking plates (LP)
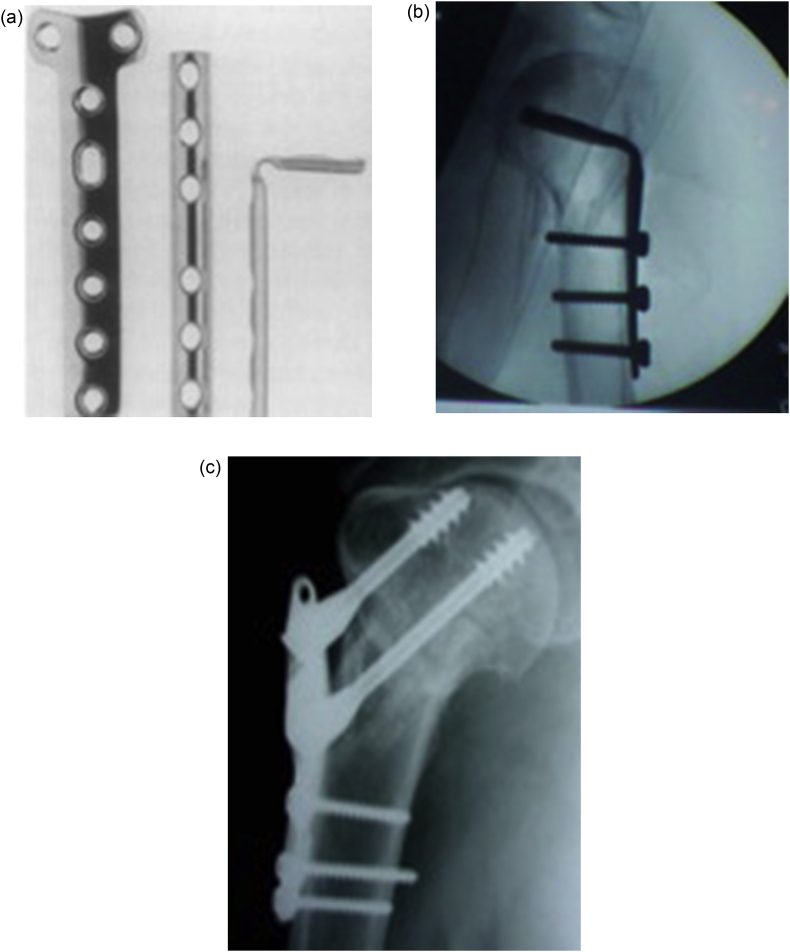
LP technology has evolved over the past 80 years. In 1949, the first 120° blade plate was introduced.17 T-shape and bent tubular plates were later introduced to prevent angular and rotational failure of fixation. A more advanced blade plate was introduced by the AO group and later the Plant-Tan plate which had more angular stability (Fig. 1a–c).18, 19, 20 However, failure rate in osteoporotic bone was relatively high.21 The introduction of LP technology provided a low profile stable angular device that has succeeded in osteoporotic bone by providing greater stiffness and torsional resistance.22,23 The divergence of locking screws provides polyaxial locking support which is vital in osteoporotic bone.
Fig. 1.
a) AO T-plate and semitubular plate (pre- and post bending), b) AO Blade plate c) Plant-Tan plate.
LP is commonly used for 2-part surgical neck fractures.22, 23, 24 In 3-part fractures, biomechanical studies have shown that LP has lower failure rates compared to other methods of fixation.24 However, there is a high complication rate reported in the literature such as avascular necrosis, plate impingement, and screw cut out.25 Medial comminution compromises stability leading to varus collapse and risks avascular necrosis as described by Hertel et al.10 Without medial support, the construct entirely relies on the implant rather than anatomical support. However, this can be avoided using medial support screws that run distal to proximal above the calcar to prevent varus collapse.26,27 A recent prospective RCT showed maintenance of reduction and higher functional outcomes at 31 months in 3 and 4-parts fractures when medial support screws were used.28
In a recent cohort study, Constant and Disability of the Arm, Shoulder and Hand (DASH) scores in 44 patients with 2,3 and 4-part fractures fixed with LP did not prove to be advantageous when compared to conservative management.8
Nonetheless, new techniques are being employed in displaced 3 and 4-part fractures yielding promising results. The use of fibular strut allograft, cancellous bone graft and synthetic bone graft in deficient medial calcar have shown promising results on cadaveric models.29
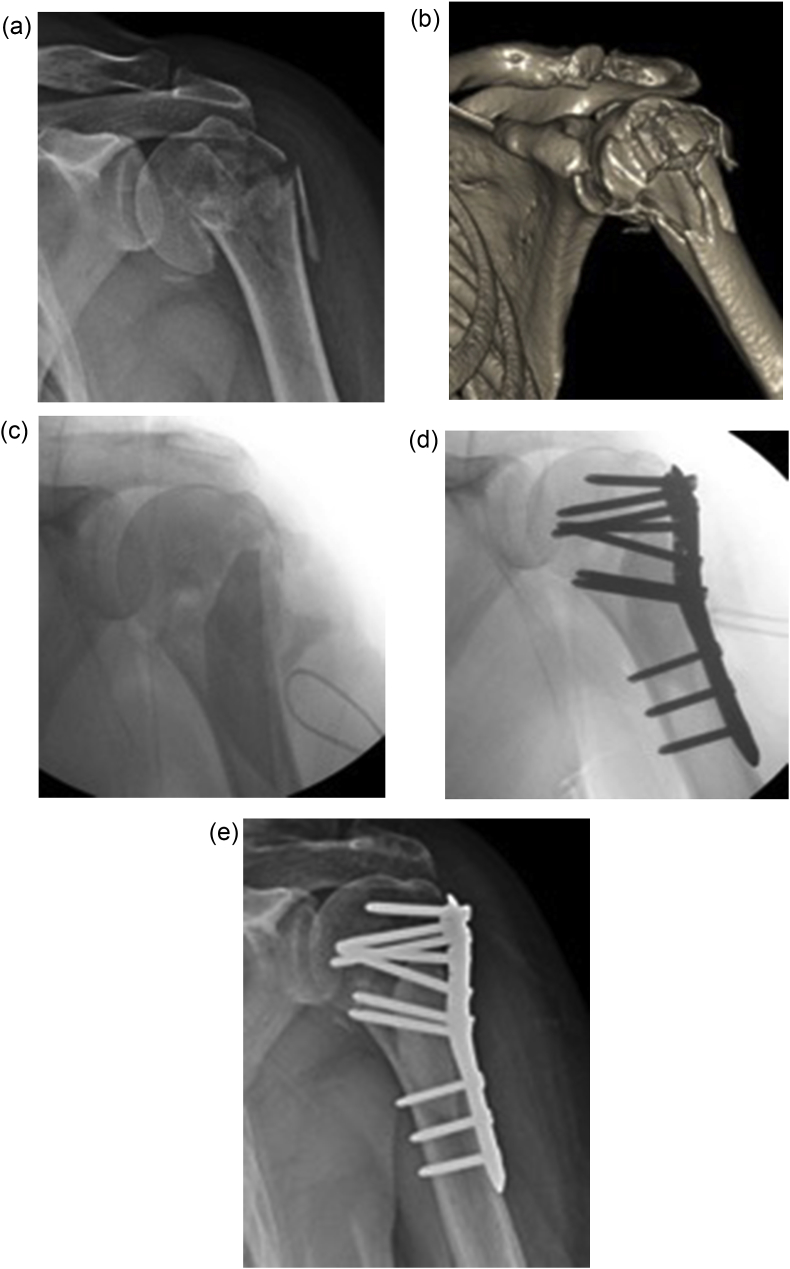
A case series looking at LP fixation of 71 adults with 2-, 3- and 4-part fractures with fibular strut graft with more than one year follow up showed a mean Constant score of 82.7.30 Furthermore, a systematic review looking at the use of fibular strut graft concluded that the complication rates, especially varus collapse, are much lower than in traditional LP fixation.31 Fig. 2a–e demonstrate LP fixation of communited proximal humerus augmented with fibular strut graft.
Fig. 2.
(a and b): Radiograph and 3D CT of comminuted proximal humeral fracture with deficient medial calcar. (c and d): Fracture fixed with locking plate augmented with cortical strut graft technique. (e): Radiograph of shoulder at final follow-up.
Calcium sulphate augmentation with LP fixation have also shown promising results. A retrospective case series of 21 patients found very good outcomes with modified Constant and Murley score of 64.04 with two-year follow-up.32 Finally, another group have used an endosteal implant with LP plating in 34 patients and reported low avascular necrosis rates though acknowledging the technical difficulty during fixation.33
Functional outcomes following LP fixation are difficult to interpret. Complication rates of over 20% are reported in most series despite achieving bony union in over 75% of cases.34,35 Medial comminution and varus collapse are the most consistent predictors of poor outcome.34,35 Increasing age, bone stock availability and female-sex have also been found to predict poor outcomes.34,36,37 A recent Cochrane review concluded that evidence is lacking to support LP fixation over conservative management; although acknowledging that LP technology has evolved, and surgical expertise may play a bigger part in achieving a good outcome.7
Therefore, a steep learning curve of surgical techniques, predicting factors outside the surgeon's control (age, female-sex and poor bone stock) and lack of robust evidence in the literature dictates a cautious approach to LP fixation especially in elderly patients.
4. Proximal humeral nail (HN)
HN is a rigid angular stable device that gives a biomechanical advantage over plates with a shorter leaver arm and higher stiffness in bending and torsional rigidity.24,38 Fracture reduction is achieved closed and this allows minimal soft tissue disruption and a shorter operating time.39
As for LP, HN is commonly used for 2-part, and to lesser extent, 3-part fractures.40, 41, 42 Good results have been reported in the literature. A case series of 29 patients treated with HN fixation showed a mean Constant score of 65.7 with minimum one year follow up. Another case series of 18 patients treated with HN fixation with an average age of 71 years showed a mean Constant and American Shoulder & Elbow Surgeons scores of 61 and 67, respectively, after 42-month average follow-up.41 Both studies recommend the use of HN as a safe and reliable way to fix displaced 2- and 3-parts fractures.
The literature also reports on a few complications associated with HN.40, 41, 42 Impingement, non-union, avascular necrosis, implant backing out, joint stiffness, rotator cuff dysfunction are commonly observed issues. A case series of 18 patients with 2- and 3-part fracture fixed with HN with average follow-up of 42 months, showed increased unsatisfactory results due to rotator cuff dysfunction where a curvilinear HN was used.42
However, starting medial to the greater tuberosity and through the muscular part of supraspinatus avoids rotator cuff dysfunction, post-operative pain and joint stiffness.43 A RCT of 54 patients in 2014 concluded that straight HN has reduced symptomatic rotator cuff pain when compared to curvilinear HN with an average follow-up of 14 months.44 Lower reoperation rate and better functional outcomes have also been reported with straight nails.44
As per LP, it is vital to restore and maintain medial buttress and anatomical neck/shaft angle for successful outcomes.26,34 This can be achieved through screws or curved blades locked to the nail with or without bone graft.26,34 This will prevent varus collapse and reduction of the lever arm of the rotator cuffs.26,34 In 4-part fractures, loss of soft tissue attachment to the head and tuberosities compromises success of fixation.39
In a recent retrospective cohort study, mean Constant and DASH scores of 19 patients with 2-, 3- and 4-part fractures showed a distinct outcome compared with conservative management when age was taking into consideration.8 Patients younger than 65 years recorded better outcome scores than those above that age.8 This may be explained by the increased rotator cuff disruption and damage to subacromial space in already compromised rotator cuff tendons in this age group which is poorly tolerated.45 Furthermore, and as per LP, poor bone stock compromises mechanical stability leading to construct failure.46
HN is gaining popularity among surgeons as it offers a high degree of stability and better biomechanics with a short level arm even in poor bone quality. However, the lack of strong evidence to support their use in those over the age of 65 years restricts their wider use in fracture fixation.
5. Discussion
Proximal humeral fractures are very common injuries in an ever-ageing population with increased burden to the health system and wider social effects on patients. No consensus has been established with regards to management, with the literature leaning toward conservative management in the majority of cases.
Many surgical techniques and implants have evolved in the past 80 years. The complexity of the fracture may dictate the type of fixation suitable although surgical expertise and patient factors (age, sex and bone stock availability) directly affect surgical outcomes.
In 2011, Smejkal et al. compared percutaneous K-wiring with LP fixation in 61 patients.47 There was no difference in the mean Constant score between the two groups relative to the healthy limb. There was also a higher complication rate in LP and longer hospital stay. In the same year, a prospective randomised-controlled trial compared LP with HN fixation in 57 patients with 2-part fractures. LP fixation recorded slightly better mean Constant and ASES scores at 1- and 3-year follow-up but higher complication rates were recorded.39 Clinically, however, there was no statistical difference in the range of movement recorded at 1 or 3-year follow-up.
In 2015, the Proximal Fracture of the Humerus Evaluation by Randamisation (PROFHER) national UK multicentre randomised clinical trial published on clinical effectiveness of surgical versus non-surgical treatment of proximal humeral fractures in one of the highest impact journals.6 Two hundred and thirty-one patients were included between 2008 and 2011 with a follow up of two years. Fixation or replacement was performed by experienced surgeons and conservative management consisted of sling immobilisation - both groups received similar community rehabilitation. The results showed no difference in reported outcomes in terms of function and quality of life at two years between the two groups. The trial concluded that little evidence is available to support the increased trend of surgical fixation in displaced proximal humeral fractures.
However, at closer inspection the conclusion may not be that simple. The PROFHER trial only included 11 4-part fractures (4.4%) which is much lower than the expected 20–30% seen in the population.48 Furthermore, over 66 surgeons took part with an average of less than one patient per surgeon per year operated on. More significantly, a large number of patients meeting the inclusion criteria were excluded due to associated dislocation (100 patients) or if the surgeon felt surgery is indicated (87 patients). This alarmingly questions the trial findings and tips the balance towards surgical management once more.
Another recent meta-analysis on specific fracture configuration has concluded that differences in the type of fracture and surgical treatment results in outcomes that are distinct from those generated from analysis of all types of fracture and surgical treatments grouped together.49 The trial concluded that future work should focus on specific fracture configuration and surgical techniques to determine the indication for surgical fixation.
With advanced surgical implant designs and techniques, the jury is out in recommending either approaches.
6. Conclusion
Proximal humeral fracture management remains a controversial topic. Conservative management is showing a good clinical outcome in the treatment of 2 -, 3- and 4-part fractures in a recent level I evidence trial. However, flaws in their data collection and interpretation coupled with advanced surgical techniques and improved implant choice continues to tip the balance towards surgical management for displaced fractures.
Recent study looked at the difficulties in decision making in the treatment of 476 patients with displaced proximal humeral fractures and its subsequent effect on surgical outcomes.50 It showed the experienced fellowship-trained surgeons of the study could only agree on 63.5% in regard to treatment choice offered to the patients (p < 0.001). They concluded that outcomes in the surgical group are not predictable due to the discrepancy in decision making.
Therefore, as per current evidence, we conclude that the management of proximal humeral fracture should be considered on a case-by-case bases taking into consideration the merits and potential complications of each treatment modality. Until more robust evidence emerges, both conservative and surgical options are justifiable in the treatment of proximal humeral fractures.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.01.029.
Contributor Information
Tony Antonios, Email: tantonios@doctors.org.uk.
Nik Bakti, Email: nik.bakti@gmail.com.
Obinna Nzeako, Email: OJ-nzeako@doctors.org.uk.
Paras Mohanlal, Email: parasmohanlal@gmail.com.
Bijayendra Singh, Email: bijayendra.singh@nhs.net.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Bell J.E., Leung B.C., Spratt K.F. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93(2):121e131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palvanen M., Kannus P., Niemi S. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442(442):87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 3.Court-Brown C.M., Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 4.Maravic M., Briot K., Roux C. Burden of proximal humerus fractures in the French national hospital database. Orthop Traumatol Surg. 2014 Dec;100(8):931–934. doi: 10.1016/j.otsr.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 5.Hawkins R.J., Angelo R.L. Displaced proximal humerus fractures-selecting treatment, avoiding pitfalls. Orthop Clin N Am. 1987;18:421e31. [PubMed] [Google Scholar]
- 6.Rangan A., Handoll H., Brealey S. Surgical vs nonsurgical treatment of adults with displaced fractures of the proximal humerus: the PROFHER randomized clinical trial. JAMA. 2015;313:1037–1047. doi: 10.1001/jama.2015.1629. [DOI] [PubMed] [Google Scholar]
- 7.Handoll H.H.G., Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015;11 doi: 10.1002/14651858.CD000434.pub4. [DOI] [PubMed] [Google Scholar]
- 8.Tamimi I., Montesa G., Collado F. Displaced proximal humeral fractures: when is surgery necessary? Injury. 2015 Oct;46(10):1921–1929. doi: 10.1016/j.injury.2015.05.049. [DOI] [PubMed] [Google Scholar]
- 9.Neer C.S. Four-segment classification of proximal humerus fractures. Instr Course Lect. 1975;24:160e8. [Google Scholar]
- 10.Hertel R., Hempfing M., Stiehler M. Predictors of humeral head ischaemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004;13:427e33. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 11.Bergdahl C., Ekholm C., Wennergren D. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish Fracture Register. BMC Muscoskelet Disord. 2016;17:159. doi: 10.1186/s12891-016-1009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eid A., Osman M., Fekry H.-E. Percutaneous fixation with Schanz screws for displaced two- and three- part fractures of the proximal humerus in patients above fifty years of age. Int J Shoulder Surg. 2011;5(2):38–43. doi: 10.4103/0973-6042.83195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vundelinckx B.J., Dierickx C.A., Bruckers L. Functional and radiographic medium-term outcome evaluation of the humerus block, a minimally invasive operative technique for proximal humeral fractures. J Shoulder Elbow Surg. 2012;21(9):1197–1206. doi: 10.1016/j.jse.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 14.Bogner R., Hubner C., Matis N. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br. 2008;90(12):1602–1607. doi: 10.1302/0301-620X.90B12.20269. [DOI] [PubMed] [Google Scholar]
- 15.Magovern B., Ramsey M.L. Percutaneous fixation of proximal humerus fractures. Orthop Clin N Am. 2008;39:405–416. v. doi: 10.1016/j.ocl.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Innocenti M., Carulli C., Civinini R. Displaced fragility fractures of proximal humerus in elderly patients affected by severe comorbidities: percutaneous fixation and conservative treatment. Aging Clin Exp Res. 2013;25:447–452. doi: 10.1007/s40520-013-0063-4. [DOI] [PubMed] [Google Scholar]
- 17.Bosworth D.M. Blade plate fixation; technique suitable for fractures of the surgical neck of the humerus and similar lesions. J Am Med Assoc. 1949;141:1111e3. doi: 10.1001/jama.1949.02910160001001. [DOI] [PubMed] [Google Scholar]
- 18.Sehr J.R., Szabo R.M. Semitubular blade plate for fixation in the proximal humerus. J Orthop Trauma. 1988;2:327e32. doi: 10.1097/00005131-198802040-00010. [DOI] [PubMed] [Google Scholar]
- 19.Instrum K., Fennell C., Shrive N. Semitubular blade plate fixation in proximal humeral fractures: a biomechanical study in a cadaveric model. J Shoulder Elbow Surg. 1998;7:462e6. doi: 10.1016/s1058-2746(98)90195-1. [DOI] [PubMed] [Google Scholar]
- 20.Ring D., Jupiter J.B. Wave plate osteosynthesis in the upper extremity. Tech Hand Up Extrem Surg. 1997;1:168e74. doi: 10.1097/00130911-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Machani B., Sinopidis C., Brownson P. Mid term results of PlantTan plate in the treatment of proximal humerus fractures. Injury. 2006;37:269e76. doi: 10.1016/j.injury.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Weinstein D.M., Bratton D.R., Ciccone W.J., 2nd Locking plates improve torsional resistance in the stabilization of three- part proximal humeral fractures. J Shoulder Elbow Surg. 2006;15:239e43. doi: 10.1016/j.jse.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Siffri P.C., Peindl R.D., Coley E.R. Biomechanical analysis of blade plate versus locking plate fixation for a proximal humerus fracture: comparison using cadaveric and synthetic humeri. J Orthop Trauma. 2006;20:547e54. doi: 10.1097/01.bot.0000244997.52751.58. [DOI] [PubMed] [Google Scholar]
- 24.Kitson J., Booth G., Day R. A biomechanical comparison of locking plate and locking nail implants used for fractures of the proximal humerus. J Shoulder Elbow Surg. 2007;16(3):362–366. doi: 10.1016/j.jse.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 25.Schulte L.M., Matteini L.E., Neviaser R.J. Proximal periarticular locking plates in proximal humeral fractures: functional outcomes. J Shoulder Elbow Surg. 2011;20:1234–1240. doi: 10.1016/j.jse.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Gardner M.J., Weil Y., Barker J.U. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21(3):185e191. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 27.Newman J.M., Kahn M., Gruson K.I. Reducing postoperative fracture displacement after locked plating of proximal humerus fractures: current concepts. Am J Orthop (Belle Mead NJ) 2015;44(7):312–320. [PubMed] [Google Scholar]
- 28.Zhang L., Zheng J., Wang W. The clinical benefit of medial support screws in locking plating of proximal humerus fractures: a prospecive randomized study. Int Orthop. 2011;35:1655e61. doi: 10.1007/s00264-011-1227-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bae J.H., Oh J.K., Chon C.S. The biomechanical performance of locking plate fixation with intramedullary fibular strut graft augmentation in the treatment of unstable fractures of the proximal humerus. J Bone Joint Surg Br. 2011;93:937e41. doi: 10.1302/0301-620X.93B7.26125. [DOI] [PubMed] [Google Scholar]
- 30.Hinds R.M., Garner M.R., Tran W.H. Geriatric proximal humeral fracture patients show similar clinical outcomes to non-geriatric patients after osteo- synthesis with endosteal fibular strut allograft augmentation. J Shoulder Elbow Surg. 2015;24(6):889–896. doi: 10.1016/j.jse.2014.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Saltzman B.M., Erickson B.J., Harris J.D. Fibular strut graft augmentation for open reduction and internal fixation of proximal humerus fractures: a systematic review and the authors' preferred surgical technique. Orthop J Sports Med. 2016 Jul;4(7) doi: 10.1177/2325967116656829. PMC4962341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Somasundaram K., Huber C.P., Babu V. Proximal humeral fractures: the role of calcium sulphate augmentation and extended deltoid splitting approach in internal fixation using locking plates. Injury. 2013 Apr;44(4):481–487. doi: 10.1016/j.injury.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 33.Neviaser A.S., Hettrich C.M., Dines J.S. Rate of avascular necrosis following proximal humerus fractures treated with a lateral locking plate and endosteal implant. Arch Orthop Trauma Surg. 2011;131:1617e22. doi: 10.1007/s00402-011-1366-6. [DOI] [PubMed] [Google Scholar]
- 34.Krappinger D., Bizzotto N., Riedmann S. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283e8. doi: 10.1016/j.injury.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 35.Sudkamp N., Bayer J., Hepp P. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320e8. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 36.Sudkamp N.P., Audige L., Lambert S. Path analysis of factors for functional outcome at one year in 463 proximal humeral fractures. J Shoulder Elbow Surg. 2011;20:1207e16. doi: 10.1016/j.jse.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 37.Sproul R.C., Iyengar J.J., Devcic Z. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011;42:408e13. doi: 10.1016/j.injury.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 38.Fuchtmeier B., May R., Hente R. Proximal humerus fractures: a comparative biomechanical analysis of intra and extramedullary implants. Arch Orthop Trauma Surg. 2007;127:441e7. doi: 10.1007/s00402-007-0319-6. [DOI] [PubMed] [Google Scholar]
- 39.Zhu Y., Lu Y., Shen J. Locking intramedullary nailsand locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am. 2011 Jan 19;93:159e68. doi: 10.2106/JBJS.J.00155. [DOI] [PubMed] [Google Scholar]
- 40.Hatzidakis A., Shevlin M., Fenton D. Angular-stable locked intramedullary nailing of two-part surgical neck fractures of the proximal part of the humerus. A multicenter retrospective observational study. J Bone Joint Surg Am. 2011;93:2172e9. doi: 10.2106/JBJS.J.00754. [DOI] [PubMed] [Google Scholar]
- 41.Nolan B.M., Kippe M.A., Wiater J.M. Surgical treatment of displaced proximal humerus fractures with a short intramedullary nail. J Shoulder Elbow Surg. 2011;20:1241e7. doi: 10.1016/j.jse.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 42.Witney-Lagen C., Datir S. Treatment of proximal humerus fractures with the Stryker T2 proximal humeral nail: a study of 61 cases. Shoulder Elbow. 2012:1758e5740. [Google Scholar]
- 43.Park J.Y., Pandher D.S., Chun J.Y. Antegrade humeral nailing through the rotator cuff interval: a new entry portal. J Orthop Trauma. 2008 Jul;22:419e25. doi: 10.1097/BOT.0b013e318173f751. [DOI] [PubMed] [Google Scholar]
- 44.Lopiz Y., Garcia-Coiradas J., Garcia-Fernandez C. Proximal humerus nailing: a randomized clinical trial between curvilinear and straight nails. J Shoulder Elbow Surg. 2014;23(3):369–376. doi: 10.1016/j.jse.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 45.Sher J.S., Uribe J.W., Posada A. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 46.Faraj D., Kooistra B.W., Vd Stappen W.A. Results of 131 consecutive operated patients with a displaced proximal humerus fracture: an analysis with more than two years follow-up. Eur J Orthop Surg Traumatol: Orthop Traumatol. 2011;21:7–12. doi: 10.1007/s00590-010-0655-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smejkal K., Lochman P., Dedek T. Surgical treatment for proximal humerus fracture [Czech] [Operacni lecba zlomenin proximalniho humeru] Acta Chir Orthop Traumatol Cech. 2011;78(4):321–327. [PubMed] [Google Scholar]
- 48.Dean B.J.F., Jones L.D., Palmer A.J.R. A review of current surgical practice in the operative treatment of proximal humeral fractures: does the PROFHER trial demonstrate a need for change? Bone Joint Res. 2016;5:178–184. doi: 10.1302/2046-3758.55.2000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sabharwal S., Patel N.K., Griffiths D. Trials based on specific fracture configuration and surgical procedures likely to be more relevant for decision-making in the management of proximal humerus fractures: findings of a meta-analysis. Bone Joint Res. 2016;5:470–480. doi: 10.1302/2046-3758.510.2000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.LaMartina J., Christmas K.N., Simon P. Difficulty in decision making in the treatment of displaced proximal humerus fractures: the effect of uncertainty on surgical outcomes. J Shoulder Elbow Surg. 2018;27:470–477. doi: 10.1016/j.jse.2017.09.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.