Abstract
New indications for meniscal allograft transplantation (MAT) are being added, but the general expert opinion is that it is still a procedure reserved for symptomatic meniscal loss.
Lateral MAT has better clinical outcomes and less failure risk compared to medial MAT.
Ideal conditions (low-grade chondral lesions) make MAT a more survivable and successful procedure.
Meniscal extrusion after MAT is common and does not seem to alter results.
Midterm survivorship of a MAT is reported to be 85–90%, while long-term survivorship decreases to 50–70% depending on chondral status and concomitant procedures.
Even if the procedure is a success, there are high possibilities of not being able to resume sports activities.
Cite this article: EFORT Open Rev 2019;4:115-120. DOI: 10.1302/2058-5241.4.180052
Keywords: allograft, MAT, meniscal, menisectomy, post-menisectomy syndrome, transplantation
Introduction
In recent years, meniscal allograft transplantation (MAT) has become the state-of-the-art treatment for the orthopaedic surgeon presented with symptomatic subtotal or total menisectomy patients, especially in the young population.1 Given the long-term degenerative consequences of subtotal and total meniscectomy,2 MAT was developed as an intuitive method to restore the normal contact pressures of the knee joint that were lost with the ultimate goal of delaying the progression of degenerative arthritis.
Indications
Classical indications for MAT are patients with a symptomatic meniscal deficiency, without the presence of advanced degenerative changes. Any concurrent pathology such as localized osteochondral defects, instability or malalignment should be amenable to surgical correction. On the other hand, classical contraindications are: advanced osteoarthritis, obesity, skeletal immaturity, inflammatory arthritis, previous septic arthritis, and synovial disease.1 However, in recent years, different studies have disputed these indications. Stone et al3 reported 49 MATs in patients with grade III or IV Outerbridge chondral defects that were followed up for a mean 8.6 ± 4.2 years. In their study, a 73.5% of the patients were able to resume sporting activities but a 22.4% failure rate for the MATs was noted. Lee et al4 grouped MAT patients into low-grade chondral lesions (ICRS (International Cartilage Repair Society) grade 2) on both the femoral and tibial sides (ideal indication), high-grade lesions (ICRS grade 3 or 4) on either the femoral or tibial side (relative indication), and high-grade lesions on both sides (salvage indication) to predict survivorship of the MAT according to the cartilage status of the patient. Their results reported that after undergoing a MAT the postoperative scores were not significantly different between the three groups, but the estimated cumulative graft survival rate at five years in the salvage indication group was 62.2%, significantly lower than that in the other two groups (ideal indication: 93.8%, relative indication: 90.9%).
In an effort to know the prophylactic effect of MAT, Jiang et al5 conducted a four to six year follow-up study in which they compared eight patients undergoing an immediate MAT after menisectomy, with 10 patients who underwent delayed MAT (at a mean 35 months). The immediate MAT group showed significantly less increase of cartilage degeneration changes on radiographs and magnetic resonance imaging (MRI). On the other hand, no significant difference was found in terms of the Lysholm score, Tegner score, joint narrowing, or meniscus extrusion.
In 2015, the International Meniscus Reconstruction Experts Forum (IMREF) published a consensus6 regarding different aspects of MAT. In their survey about indications for MAT, 42% of the surgeons stated that they would generally not perform MAT in an asymptomatic patient. Contrarily, 18% answered that they would, but only for the lateral meniscus.
Taking into account the latest publications, we advocate deciding whether to perform a MAT on a case-by-case basis, especially in young patients, but with emphasis on informing the patient of the increased risk of failure when a MAT is carried out in conditions that are not ideal. Therefore, in the young patient we prefer to perform a MAT even in the case of high-grade chondral lesions. It is important to mention that any malalignment or instability should be corrected before or during the same procedure.
Sizing the graft
The size of the MAT must be matched to within 10% of the native meniscus. An oversized graft may result in increased loads seen by the joint. Contrarily, an undersized graft may potentially experience significant shear forces leading to tears of the MAT.1
The gold standard method of measurement is the Pollard method, published in 1995.7 (Fig. 1 and Fig. 2) This method relies on antero-posterior and lateral X-rays (XR) of the knee to estimate the size of the native meniscus with a reported mean error of less than 8.4%.
Fig. 1.

Antero-posterior X-ray showing the Pollard method to size the graft (line parallel to the joint line).
Fig. 2.

Lateral X-ray showing the Pollard method to size the graft (line parallel to the joint line).
Three-dimensional computed tomography (CT) and MRI have been proposed as methods to estimate the size of the MAT graft with mixed results. McConkey et al8 reported that CT fell within 5 mm of anatomic measurements 100% of the time versus 76.5% for XR, and within 2 mm 71.9% of the time versus 34.4% for XR. On the other hand, MRI has shown controversial results, and reports have suggested that it may underestimate the real size by as much as 44%.9
As a group, based in the latest research, we use 3D CT as our preferred method to measure the size of the MAT graft before surgery. But we acknowledge that the Pollard method is still a valid method, and any new measurement tool should be compared with it as it is the gold standard.
Graft processing
Currently there are two main options to process the graft obtained before a MAT: fresh frozen and cryopreservation. Freeze-drying or cryopreservation has been abandoned because the extreme temperatures used for this method can cause deleterious effects on the mechanical properties of the allograft and it can result in high rates of failure.1
There is limited clinical information to decide between using fresh frozen or cryopreserved allografts, with each of them having some drawbacks. Fresh frozen allografts have been shown to have an abnormal collagen network when examined ultrastructurally.10 Cryopreserved allografts have shown no alteration of the mechanical ultrastructure of the allograft, theoretically providing biomechanical properties more similar to the native meniscus.11 But, on the other hand, cryopreservation was found to induce significant apoptotic cell death in meniscal tissue, with reported cell survival ranging from 4% to 54%.12 In terms of experts’ opinions, the IMREF survey found that 68% of their surgeons prefer the use of a fresh frozen meniscus for MAT.6
Regarding radiation, non-irradiated grafts are more frequently used than the irradiated, since a dose of 2.5 Mrad gamma radiation, which is used for inactivation of human immunodeficiency virus, can cause significant changes in the biomechanical properties of the grafts.13
As there is no absolute superiority of one method over the other, we use cryopreservation as it is cheaper in our local reality.
MAT fixation
The three main fixation methods that can be used to fix a MAT are: suture-only fixation (Fig. 3 and Fig. 4), double plug fixation and the keyhole technique (Fig. 5 and Fig. 6).1 The first one consists of fixing a completely soft tissue graft only using sutures through the body and meniscal horns, while the meniscal roots are fixed using a transtibial suture technique, similar to root lesion repairs. The double plug and keyhole techniques are different types of bone fixation. In the double plug technique, the graft is prepared with a 7 mm bone plug (to ensure easy reduction into the 8-mm tibial sockets) attached to each root, securing a bone-to-bone fixation in the meniscal roots, the rest of the meniscus being fixed with sutures. In the keyhole technique a 10 mm wide and high bone bridge is prepared from the anterior to posterior root of the meniscus. Both osseous techniques require the preparation of osseous beds in the receptor knee, so the plugs or bridge can fit in it.
Fig. 3.
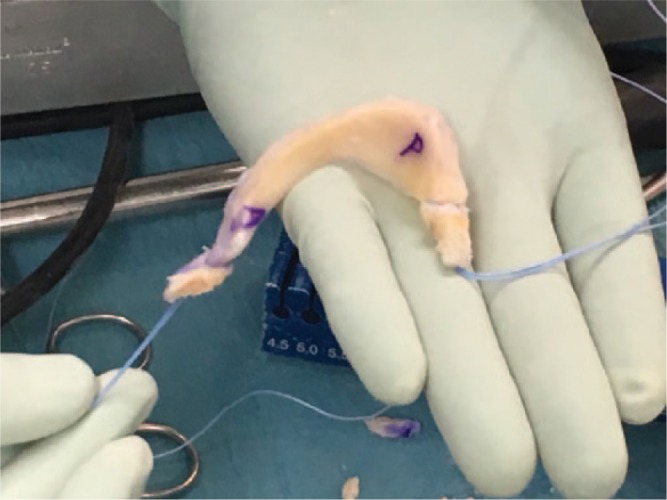
Suture only fixation.
Fig. 4.
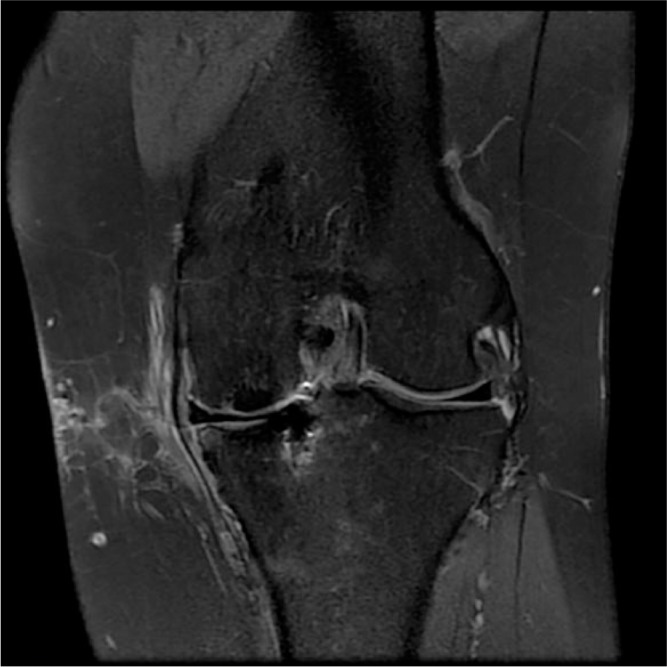
Coronal MRI showing a medial MAT fixed with transtibial sutures.
Fig. 5.

Keyhole technique.
Fig. 6.
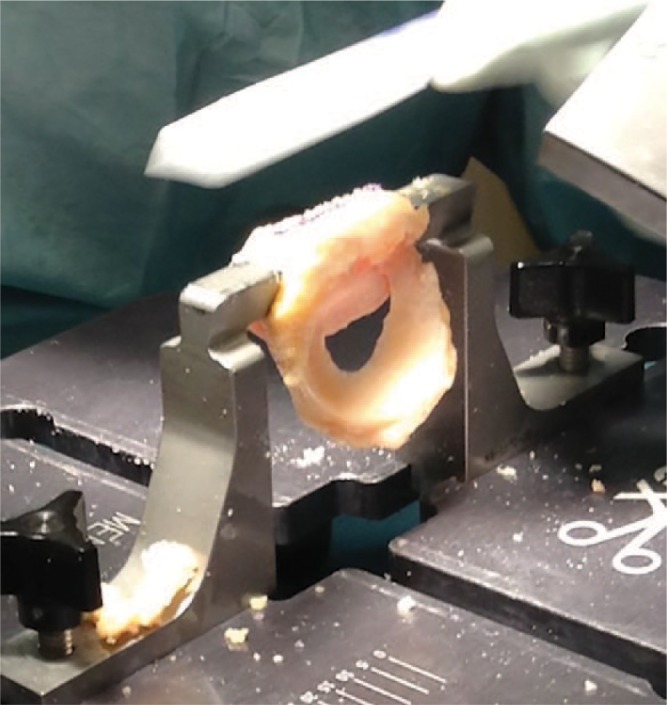
Keyhole technique preparation.
Several studies have been conducted to assess the different fixation methods. Alhalki et al14 compared bone plug fixation with suture-only fixation in a cadaveric study of medial MATs. They reported that the contact mechanics of the meniscus reinserted with bone plug fixation were closest to normal, while fixation with sutures only did not restore normal contact mechanics. Wang et al15 supported that assertation in a study that demonstrated that under dynamic loading, trans-osseous fixation at the meniscal horns provided superior load distribution at the involved knee compartment after meniscal transplantation compared with suture-only fixation. Contrarily, González-Lucena et al,16 reported a high survival rate (87.8%) in a long-term follow-up study of MATs with suture-only fixation.
Following the same trend, a recent meta-analysis published by Jauregui et al17 found no significant differences between the suture-only fixation (485 MATs) and bone fixation (489 MATs) groups in terms of: MAT tear rates (13.4% vs 14.9%), failure rates (17.6% vs 18.8%), Lysholm scores (from 52.3 to 82.4, and from 60.7 to 82.9 respectively), Visual Analogue Scale (VAS) scores (from 65 points to 18 points, and from 63 points to 13 points respectively), and meniscal extrusion, with a weighted mean percentage of extrusion of 40.2% in the suture-only fixation group and 43.1% in the bone fixation group.
We believe that as both fixation methods have similar outcomes, despite the biomechanical differences, the selection of which method to use should be made on a case-by-case basis. We prefer bone fixation for lateral MATs (specifically keyhole fixation as the anterior and posterior horns of the lateral meniscus are anatomically situated close to each other, so the use of bone plugs carries the risk of tunnel communication and breakage) because of the need for the best achievable biomechanical outcome, but on the medial side we think that soft tissue fixation is a valid option and can be used depending on the familiarity of the surgeon with the procedure, as it makes the procedure easier.
Rehabilitation
In order to rehabilitate patients for achievable goals, Spalding et al (in a chapter of a book published by members of the IMREF)18 categorized MAT patients into two main groups with different objectives for them. The first group of patients was called the ‘ideal’ patients with no or minor chondral damage. The second group was named the ‘salvage’ patients with advanced chondral damage. The objective of the first group of was a complete return to sports, while in the second group their objective was only improving their pain during activities of daily living.
Their full rehabilitation protocol consisted of three phases (for isolated and uncomplicated MAT). First an early restorative phase (0–2 months) that consisted of non-weight-bearing, range-of-motion (ROM) exercises from 0–90 degrees and static strengthening. It was followed by a strength and conditioning phase (2–6 months) in which full weight-bearing and full ROM were started with the precaution of limiting squats and strengthening exercises to 70–80 degrees of flexion. The third and final phase was a functional rehabilitation phase (6–9 months) consisting of running and sports-specific training if adequate musculature and balance had been obtained.
Outcomes
A considerable amount of recent literature regarding outcomes of MATs has been published. Bin et al19 in a meta-analysis comparing medial and lateral MATs found that both groups had substantial proportions of knees exhibiting midterm survivorship (85.8% for medial MAT and 89.2% for lateral MAT) but much lower proportions of knees exhibiting long-term survivorship (52.6% for medial MAT and 56.6% for lateral MAT). In contrast, overall pain scores (medial, 65.6 points; lateral, 71.3 points) and Lysholm scores (medial, 67.5 points; lateral, 72.0 points) were significantly higher for lateral MAT compared with medial MAT.
In another meta-analysis regarding the importance of concomitant procedures in MAT surgery, Lee et al20 published that no significant differences in Lysholm scores, Tegner activity scores, International Knee Documentation Committee subjective scores and VAS were observed between isolated MAT and combined MAT, with four studies reporting that additional procedures did not affect MAT failure or survivorship, three studies reporting that ligament surgery, realignment osteotomy, and osteochondral autograft transfer were risk factors for failure, and one study reporting that the medial MAT group in which high tibial osteotomy was performed showed a higher survival rate than the isolated medial MAT group.
Parkison et al21 followed 125 MATs to report the factors predicting failure. Their five-year graft survival was 97% for patients with intact or partial-thickness chondral loss, 82% when full-thickness chondral loss in one condyle was noted, and 62% in patients with full-thickness chondral loss of both condyles. Their reported probability of failure with lateral allografts was 76% lower than medial allografts at any time.
Regarding the progression of knee osteoarthritis after a MAT, Van Der Straeten et al22 followed a group of MATs for a mean 6.8 years (0.2–24.3 years). In their results, they reported that 186 MATs were in situ (56.5%) while 90 (27.4%) had been removed, including 63 being converted to a knee arthroplasty (19.2%). The cumulative allograft survivorship for the whole group was 15.1% at 24.0 years. In patients younger than 35 years at surgery, survival was significantly better (24.1%) compared to patients older than 35 years (8.0%). In knees with no to mild cartilage damage, more allografts survived (43.0%) compared to moderate to severe damage (6.6%). Using consecutive radiographs, they demonstrated a significant OA progression of the cohort at a mean of 3.8 years.
Noyes et al23 carried out a long-term follow-up of 72 MATs. Their group reported that the estimated probability of survival was 85% at two years, 77% at five years, 69% at seven years, 45% at 10 years, and 19% at 15 years.
In terms of the possibility of returning to sport, Waterman et al24 followed 230 MATs that were carried out on military personnel. After a MAT, 50 (22%) patients underwent knee-related military discharge at a mean of 2.49 years postoperatively.
Looking to elucidate the supposedly chondroprotective effect of MATs, Smith et al25 carried out a systematic review in which they reported that meniscal extrusion (minor extrusion (less than 3 mm) and major extrusion (more than 3 mm), in relation to the margin of the tibial plateau) was present in nearly all cases, but was not associated with clinical or other radiological outcomes. They concluded that there is some evidence to support the hypothesis that meniscal allograft transplantation reduces the progression of osteoarthritis, although it is unlikely to be as effective as the native meniscus.
Conclusion
A lot of new data on MAT surgery have been published during recent years. New indications are being added, but the general expert opinion is still that it is a procedure that should be reserved for symptomatic meniscal loss. There are three main fixation methods that can be used to fix a MAT: suture-only fixation, double plug fixation and the keyhole technique. All fixation methods have similar outcomes, meaning that despite the biomechanical differences, the selection of which method to use should be made on a case-by-case basis.
Lateral MAT has better clinical outcomes and less failure risk compared to medial MAT, but this does not preclude the usage of medial MAT, as the benefits are still high. Ideal conditions (low-grade chondral lesions) make MAT a more survivable and successful procedure. Meniscal extrusion after MAT is common and does not seem to alter results. Even if the procedure is a success, there remains a high possibility of not being able to resume sports activities.
Footnotes
ICMJE Conflict of interest statement: DF has a paid consultancy with Stryker and receives payment for lectures including service on speakers bureaus, and payment for development of educational presentations from Stryker and Smith and Nephew.
RC has a paid consultancy with Stryker and receives payment for development of educational presentations from Smith and Nephew.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Trentacosta N, Graham WC, Gersoff WK. Meniscal allograft transplantation: state of the art. Sports Med Arthrosc Rev 2016;24:e23–e33. [DOI] [PubMed] [Google Scholar]
- 2. Englund M. The role of the meniscus in osteoarthritis genesis. Rheum Dis Clin North Am 2008;34:573–579. [DOI] [PubMed] [Google Scholar]
- 3. Stone KR, Pelsis JR, Surrette ST, Walgenbach AW, Turek TJ. Meniscus transplantation in an active population with moderate to severe cartilage damage. Knee Surg Sports Traumatol Arthrosc 2015;23:251–257. [DOI] [PubMed] [Google Scholar]
- 4. Lee BS, Bin SI, Kim JM, Kim WK, Choi JW. Survivorship after meniscal allograft transplantation according to articular cartilage status. Am J Sports Med 2017;45:1095–1101. [DOI] [PubMed] [Google Scholar]
- 5. Jiang D, Ao YF, Gong X, Wang YJ, Zheng ZZ, Yu JK. Comparative study on immediate versus delayed meniscus allograft transplantation: 4- to 6-year follow-up. Am J Sports Med 2014;42:2329–2337. [DOI] [PubMed] [Google Scholar]
- 6. Getgood A, LaPrade RF, Verdonk P, et al. International Meniscus Reconstruction Experts Forum (IMREF) 2015 consensus statement on the practice of meniscal allograft transplantation. Am J Sports Med 2017;45:1195–1205. [DOI] [PubMed] [Google Scholar]
- 7. Pollard ME, Kang Q, Berg EE. Radiographic sizing for meniscal transplantation. Arthroscopy 1995;11:684–687. [DOI] [PubMed] [Google Scholar]
- 8. McConkey M, Lyon C, Bennett DL, et al. Radiographic sizing for meniscal transplantation using 3-D CT reconstruction. J Knee Surg 2012;25:221–225. [DOI] [PubMed] [Google Scholar]
- 9. Donahue TL, Hull ML, Howell SM. New algorithm for selecting meniscal allografts that best match the size and shape of the damaged meniscus. J Orthop Res 2006;24:1535–1543. [DOI] [PubMed] [Google Scholar]
- 10. Gelber PE, Gonzalez G, Lloreta JL, Reina F, Caceres E, Monllau JC. Freezing causes changes in the meniscus collagen net: a new ultrastructural meniscus disarray scale. Knee Surg Sports Traumatol Arthrosc 2008;16:353–359. [DOI] [PubMed] [Google Scholar]
- 11. Gelber PE, Gonzalez G, Torres R, Garcia Giralt N, Caceres E, Monllau JC. Cryopreservation does not alter the ultrastructure of the meniscus. Knee Surg Sports Traumatol Arthrosc 2009;17:639–644. [DOI] [PubMed] [Google Scholar]
- 12. Villalba R, Peña J, Navarro P, et al. Cryopreservation increases apoptosis in human menisci. Knee Surg Sports Traumatol Arthrosc 2012;20:298–303. [DOI] [PubMed] [Google Scholar]
- 13. Lee SR, Kim JG, Nam SW. The tips and pitfalls of meniscus allograft transplantation. Knee Surg Relat Res 2012;24:137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med 1999;27:320–328. [DOI] [PubMed] [Google Scholar]
- 15. Wang H, Gee AO, Hutchinson ID, et al. Bone plug versus suture-only fixation of meniscal grafts: effect on joint contact mechanics during simulated gait. Am J Sports Med 2014;42:1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. González-Lucena G, Gelber PE, Pelfort X, Tey M, Monllau JC. Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthroscopy 2010;26:1633–1640. [DOI] [PubMed] [Google Scholar]
- 17. Jauregui JJ, Wu ZD, Meredith S, Griffith C, Packer JD, Henn RF., III How should we secure our transplanted meniscus? A meta-analysis. Am J Sports Med 2018;46:2285–2290. [DOI] [PubMed] [Google Scholar]
- 18. Getgood A, Spalding T, Cole B, Gersoff W, Verdonk P. Meniscal allograft transplantation: a comprehensive review. London: DJO Publications, 2015. [Google Scholar]
- 19. Bin SI, Nha KW, Cheong JY, Shin YS. Midterm and long-term results of medial versus lateral meniscal allograft transplantation: a meta-analysis. Am J Sports Med 2018;46:1243–1250. [DOI] [PubMed] [Google Scholar]
- 20. Lee BS, Kim HJ, Lee CR, et al. Clinical outcomes of meniscal allograft transplantation with or without other procedures: a systematic review and meta-analysis. Am J Sports Med 2018;46:3047–3056. [DOI] [PubMed] [Google Scholar]
- 21. Parkinson B, Smith N, Asplin L, Thompson P, Spalding T. Factors predicting meniscal allograft transplantation failure. Orthop J Sports Med 2016;4:2325967116663185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Van Der Straeten C, Byttebier P, Eeckhoudt A, Victor J. Meniscal allograft transplantation does not prevent or delay progression of knee osteoarthritis. PLoS One 2016;11:e0156183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Noyes FR, Barber-Westin SD. Long-term survivorship and function of meniscus transplantation. Am J Sports Med 2016;44:2330–2338. [DOI] [PubMed] [Google Scholar]
- 24. Waterman BR, Rensing N, Cameron KL, Owens BD, Pallis M. Survivorship of meniscal allograft transplantation in an athletic patient population. Am J Sports Med 2016;44:1237–1242. [DOI] [PubMed] [Google Scholar]
- 25. Smith NA, Parkinson B, Hutchinson CE, Costa ML, Spalding T. Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports Traumatol Arthrosc 2016;24:2923–2935. [DOI] [PubMed] [Google Scholar]


