Abstract
Purpose
Overall Total hip arthroplasty (THA) is a very successful procedure. However, in case of complication dedicated management is required. Two major complications of THA failures are aseptic loosening (AL) and periprosthetic joint infection (PJI). The primary hypothesis of this study was that joint aspirations in patients with signs of loosening after THA are capable to detect PJI in suspected AL with negative serologic testing.
Methods
In this study a total of 108 symptomatic patients with radiographic signs of prosthetic loosening and hip pain in THA were included. Based on a standardized algorithm all patients underwent serological testing followed by joint aspiration preoperatively. Intraoperatively harvested samples were subjected to microbiological testing and served as the gold standard in differential diagnosis. Demographics, as well as the results of serologic and microbiological testing were collected from the medical records.
Results
Of the included patients 85 were finally diagnosed with an AL and 23 with PJI. Within the patients with PJI 13 (56%) patients demonstrated elevated CRP and WBC counts, as well as positive synovial cultures after joint aspiration. In ten patients (44%) diagnosed with PJI neither CRP nor WBC were abnormal.
Conclusion
The diagnosis of PJI can be difficult in THA with radiographic signs of loosening. Clinical features including pain, fever, and local sings of infection are uncommon especially a long period after index operation. First-line screening testing relies on serological evaluation of CRP and WBC. However, normal CRP and WBC values cannot rule out a PJI. These cases can be detected by joint aspiration and synovial cultures reliably.
Keywords: Total hip arthroplasty, Aseptic loosening, Periprosthetic joint infection
1. Introduction
Total hip arthroplasty is a well-accepted treatment for patients with osteoarthritis or osteonecrosis of the femoral head.1 However, THA requires a standardized management in case of complications and failures. Potential modes of failure in total hip arthroplasty (THA) are aseptic loosening (AL) and periprosthetic joint infection (PJI).2 Both usually present with radiographic signs of loosening. A major challenge represents the reliable identification of a periprosthetic joint infection in these cases. However, further management of these complications differs significantly and depends on accurate diagnosis. In the attempt to reliably diagnose PJI a wide spectrum of tests, including radiographic tests3,4 (scintigraphy, MRI, CT), systemic measures of inflammation5,6 (CRP), local measures of synovial fluid white cell count with the differential,7 and bacterial isolation techniques8 have been described. Up to now, no single measure provides reliable preoperative differential diagnosis between PJI and AL.9,10 However, a misdiagnosed PJI treated as AL may lead to persisting infection after revision surgery.11
Common first step diagnostics consists of serologic testing of white blood cell count (sWBC) and CRP. These tests have been shown to be cost-effective, highly sensitive, and bear a low risk for patients.5,12 CRP evaluation in patients with painful THA was graded as a strong recommendation as part of the American Academy of Orthopaedic Surgeons (AAOS) practice guidelines.13 However, Ting et al.13 and Parvizi et al.14 postulated that only patients with abnormal level of CRP are required to have additional investigations.
Aim of this study is to retrospectively assess the diagnostic value of serologic testing for the differential diagnosis of PJI and AL. The primary hypothesis of this study was that joint aspirations in patients with signs of loosening after THA are capable to detect PJI in suspected AL with negative serologic testing.
2. Patients and methods
In this retrospective study a total of 108 patients with a symptomatic THA and radiographic signs of loosening that underwent revision surgery between July 2012 and December 2016 were included. The study was approved by the local institution review board. Inclusion criteria was symptomatic THA with radiologically detected periimplant lucency greater than 2 mm. All patients with clinically apparent sings of infections, such as a sinus tract, were excluded. All 108 patients underwent the same standardized diagnostic protocol with radiographic imaging, serological testing, and a joint aspiration preoperatively.
Preoperatively PJI was assumed when a combination of three of the four signs were present: abnormal CRP (>1 mg/dl), synovial WBC count greater than 3000 cells/μl, synovial neutrophil percentage > 65%, or a bacterial growth in two synovial aspirate cultures. Patients that did not meet these guidelines were assumed to have an aseptic loosening. Joint aspiration was conducted under strictly aseptic conditions in all cases. The joint aspirate was evaluated for WBC and was incubated in aerobic and anaerobic blood culture bottles. If the first joint aspiration was sterile a second was done 31 days later in all cases. The final diagnosis of AL or PJI was based on microbiologic analysis of intraoperatively harvested soft tissue samples. All cases with 2 or more positive samples were considered as PJI.
Demographics (age, gender distribution, BMI), prosthesis age, CRP, sWBC, WBC, and synovial percentage from synovial fluid, as well as the results from synovial fluid culture and results of five periprosthetic soft tissue samples as a retrospective control during the revision surgery for microbiological analysis were retrieved from the medical records in all patients.
In the clinical algorithm applied all patients with preoperatively AL were treated with a single-stage surgery, whereas all patients with suspected PJI were treated with a multi-stage approach. In supsected PJI antibiotics were withheld until the surgical treatment has been performed. Following the first-stage surgery antibiotics have been started.
For statistical analysis between groups one-way ANOVA test followed by the post-hoc Dunn's test using SPSS software pack (version 23, IBM, New York, USA). P value < 0.05 was considered for statistic significance.
3. Results
Of the 108 patients 85 (78.7%) were diagnosed with AL and 23 (21.3%) with PJI. All 23 patients preoperatively assumed as PJI were positive in 2 or more of the five intraoperatively harvested soft tissue samples that were used as a retrospective control. However, there is a low sample size.
In all patients with suspected AL these soft tissue samples were negative. Hence, the preoperatively suspected diagnosis was correct in all cases. There were no significant differences between the groups in age, gender distribution, and BMI (p > 0.05) (Table 1). Two patients required a 2 nd joint aspiration after 31 days.
Table 1.
Demographic data, ± SD.
| N | age | male | female | BMI | |
|---|---|---|---|---|---|
| aseptic group | 85 | 75.3 ± 8.1 | 38 | 47 | 25.9 ± 3.1 |
| normal CRP | 56 | 75.5 ± 8.1 | 25 | 31 | 23.6 ± 3.6 |
| CRP > 1 mg/dl | 29 | 74.7 ± 5.1 | 13 | 16 | 21.8 ± 2.6 |
| PJI group | 23 | 73.4 ± 7.2 | 11 | 12 | 28.5 ± 3.3 |
| normal CRP | 10 | 72 ± 6.8 | 4 | 6 | 26.3 ± 3.3 |
| CRP > 1 mg/dl | 13 | 74.3 ± 7.9 | 7 | 6 | 29.9 ± 2.2 |
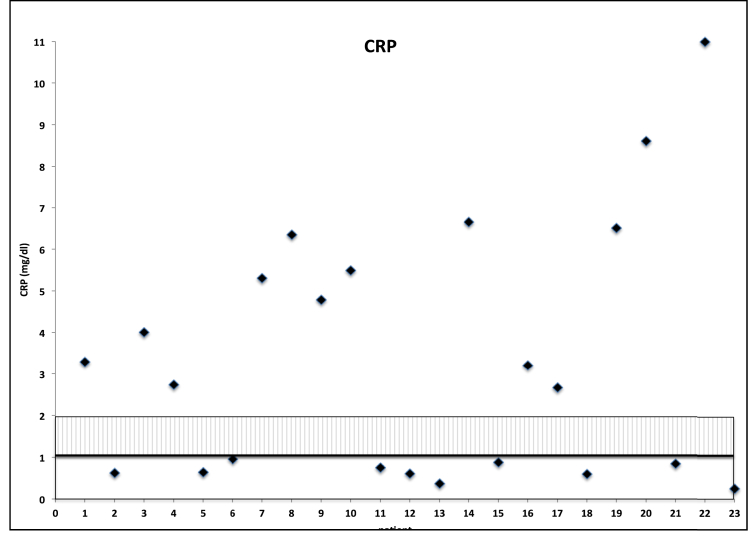
Patients with PJI presented at a significantly shorter time after primary THA (p < 0.05, mean 11.8 years ± 3.6 for AL and mean 5.8 years ± 2.1 for PJI). 10 patients in the PJI group (44%) presented with a CRP value within normal limits at initial consultation for their symptomatic THA. However, these 10 patients showed abnormal synovial WBC count, synovial neutrophil percentage >65%, and a bacterial growth from two synovial aspirate cultures. The distribution of CRP in the PJI group is shown in Fig. 1. Interestingly, there was no patient with CRP value between 1 and 2 mg/dl in the PJI group. Intraoperative component loosening in THA was seen in all cases.
Fig. 1.
CRP values from 23 PJI (norm CRP < 1 mg/dl).
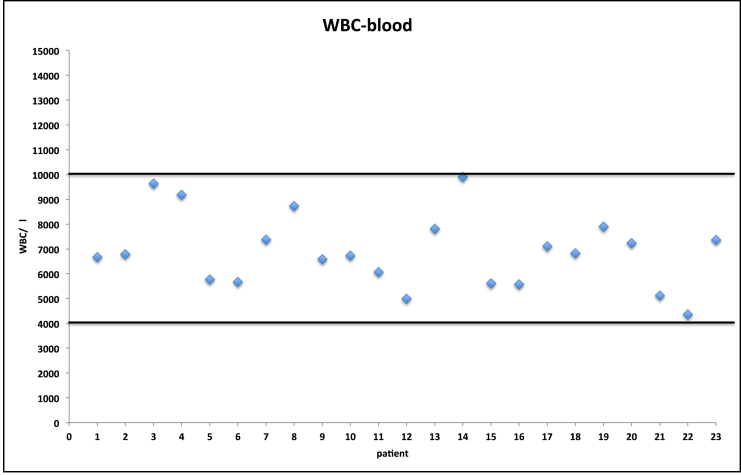
The serum WBC (sWBC) count was normal in all 23 PJI (Fig. 2). In the AL group the CRP values were normal in 56 Patients and increased in 29 patients and serum WBC was normal in 71 patients and increased in 14 patients. One patient with an AL showed abnormal synovial WBC count with normal synovial neutrophil percentage and two negative synovial aspirate cultures.
Fig. 2.
WBC blood values from 23 PJI, (norm: 4000/μl – 10000/μl).
The characteristics of the 10 patients with CRP < 1 mg/dl and PJI are shown in Table 2. The minimum prosthesis age of these 10 patients was 5 years (range 5–8 years). The specificity for CRP to detect a PJI in THA with signs of loosening was 65% with a sensitivity of 56% (cut off >1 mg/dl). At a cut-off level of 10000/μl the leukocyte count demonstrated a sensitivity of 0% and a specificity of 83% to detect a PJI.
Table 2.
Results of test from patients with normal CRP (<1 mg/dl) and PJI.
| Age | Prosthesis- Age | WBC-aspiration (aspirate culture +/−) | PMN (%) | CRP | WBC-blood | tissue culture |
|---|---|---|---|---|---|---|
| 78 | 8 | 4586 (+) | 81 | 0,24 | 7340 | Streptococcus salivarius |
| 75 | 5 | 3153 (+) | 77,1 | 0,59 | 6810 | Staphylococcus epidermidis |
| 84 | 6 | 3841 (+) | 82 | 0,6 | 4970 | Propionibacterium acnes |
| 74 | 7 | 5434 (+) | 94,5 | 0,62 | 6770 | Staphylococcus epidermidis |
| 73 | 5 | 5888 (+) | 80,3 | 0,63 | 5750 | Propionibacterium acnes |
| 75 | 5 | 3799 (+) | 84 | 0,74 | 6050 | Staphylococcus haemolyticus |
| 78 | 8 | 3930 (+) | 83 | 0,84 | 5100 | Propionibacterium acnes |
| 72 | 7 | 18452 (+) | 92,5 | 0,87 | 5600 | Staphylococcus epidermidis |
| 68 | 6 | 19134 (+) | 94,3 | 0,95 | 5650 | Propionibacterium acnes |
| 72 | 7 | 29000 (+) | 89,2 | 0,66 | 7090 | Propionibacterium acnes |
4. Discussion
Loosening and infection after THA remain challenging issues in orthopaedic surgery.15 Correct differential diagnosis between AL and PJI is essential for determining further treatment.16 However, the accurate preoperative identification of PJI may be difficult, as the clinical symptoms often resemble those of AL.17 Serological testing is described as a useful first step in the screening of patients with a symptomatic THA.13 Some authors have suggested the use of CRP and ESR (erythrocyte sedimentation rate) as primary screening tool to rule out PJI.9,13,18 In this study the evaluation of CRP and serum white blood cell count (sWBC) did not provide reliable hints for the differentiation of PJI and AL. However ESR was not evaluated and this study cannot provide information on the value of ESR for the diagnosis of PJI in patients with symptomatic THA and signs of loosening.
Berbari et al.12 reported about sWBC values within normal limitis in low grade PJI after total knee arthroplasty. They concluded that sWBC offers only low diagnostic value for the detection of PJI. This is in accordance to the results of the present study. Other authors19 reported a sensitivity of 55% and a specificity of 66% for sWBC for PJI. Randau et al.17 reported an even higher specificity of 94.5% with a low sensitivity of 21.28% for sWBC in patients with PJI. In the present study all patients diagnosed with a PJI presented with normal WBC values which supports the hypothesis that sWBC do not represent a reliable measure to rule out a PJI in patients with signs of loosening in THA.
In current literature elevated CRP values remain being reported as the most useful laboratory test for the diagnosis of PJI, even though the sensitivity seems to be low.20 Despite its drawbacks, CRP evaluation is recommended in all cases of hip pain after THA.10,14,18 Some authors even report CRP values as the ’’first line decision’’ in the diagnosis of PJI.6,14,21 A CRP value within normal limits has been described providing a good negative predictive value in ruling out PJI.13,22 Patients with a CRP within normal limits should not be subjected to additional evaluations to rule out a periprothetic joint infection.14 However, other authors recommended joint aspiration followed by synovial fluid analyses in cases of abnormally elevated CRP values.23 Comparably, Greidanus et al.22 reported in a study including 207 revisions of total knee arthroplasties that CRP within normal limits does necessitate no further testing to rule out PJI. Spangehl et al.24 analyzed 202 revision THAs and concluded that further investigation is needed if CRP is abnormal. In our study all patients with symptomatic THA presenting with painful hip and radiographic sings of loosening underwent serologic testing and additional joint aspiration. With this approach 10 cases of PJI (44%) that presented with CRP and WBC values within normal limits were detected preoperatively. As all patients with PJI, these patients also underwent a multi-stage surgical revision.
In recent literature a high incidence of revision surgery after revision THA has been observed. In these cases the indication for the initial revision was an AL diagnosed without microbiology testing of a joint aspirate. Here an underdiagnosis of PJI can be suspected and the persisting PJI may have led to further revision efforts.14,25 In contrast, in the present study 85 patients with AL underwent a single-stage surgical revision with removal of all prosthetic components including the cement, followed by a thorough debridement and a re-implantation of new prosthetic components. Furthermore, no patient diagnosed with AL underwent another revision surgery at our department within the observation period of 26 months on average.
Recently published studies report a CRP sensitivity of 59–77% for the detection of PJI.10,17 With a sensitivity of 56% this study show a comparable results.
This study has limitations, such as its retrospective character, and a relatively low sample size. IL-6 and Alpha-defensin detection has also shown promising results to detect a PJI. However, due to the high costs this is no standard diagnostic tool in the algorithm applied.26 As an alternative the cost-effective joint aspiration was used. Bone scans have been shown to have a high sensitivity, but the low specificity for infection limits their use.26 Moreover, using the bone scans increases the overall costs.
5. Conclusion
The diagnosis of PJI can be difficult in THA with radiographic signs of loosening. Clinical features including pain, fever, and local sings of infection are uncommon especially a long period after index operation. We suggest that all patients with radiographic signs of loosening of a THA receive blood testing for CRP and WBC. However, normal CRP and WBC values cannot rule out a PJI. These cases can be detected by joint aspiration and synovial cultures reliably.
Within the limitations, the results of this study suggest joint aspiration with WBC analysis and synovial cultures as a useful tool in all patients with symptomatic THA and radiographic sings of loosening.
Declarations of interest
None.
Founding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgment
This study was not supported.
References
- 1.Caton J., Prudhon J.L. Over 25 years survival after Charnley's total hip arthroplasty. Int Orthop. 2011;35(2):185–188. doi: 10.1007/s00264-010-1197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sadoghi P. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 2013;28(8):1329–1332. doi: 10.1016/j.arth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 3.Hayter C.L., Koff M.F., Potter H.G. Magnetic resonance imaging of the postoperative hip. J Magn Reson Imag. 2012;35(5):1013–1025. doi: 10.1002/jmri.23523. [DOI] [PubMed] [Google Scholar]
- 4.Nagoya S. Diagnosis of peri-prosthetic infection at the hip using triple-phase bone scintigraphy. J Bone Joint Surg Br. 2008;90(2):140–144. doi: 10.1302/0301-620X.90B2.19436. [DOI] [PubMed] [Google Scholar]
- 5.Austin M.S. A simple, cost-effective screening protocol to rule out periprosthetic infection. J Arthroplasty. 2008;23(1):65–68. doi: 10.1016/j.arth.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Ghanem E. The use of receiver operating characteristics analysis in determining erythrocyte sedimentation rate and C-reactive protein levels in diagnosing periprosthetic infection prior to revision total hip arthroplasty. Int J Infect Dis. 2009;13(6):e444–e449. doi: 10.1016/j.ijid.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Chalmers P.N., Sporer S.M., Levine B.R. Correlation of aspiration results with periprosthetic sepsis in revision total hip arthroplasty. J Arthroplasty. 2014;29(2):438–442. doi: 10.1016/j.arth.2013.06.020. [DOI] [PubMed] [Google Scholar]
- 8.Ghanem E. Periprosthetic infection: where do we stand with regard to Gram stain? Acta Orthop. 2009;80(1):37–40. doi: 10.1080/17453670902804943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parvizi J. New definition for periprosthetic joint infection. Am J Orthoped. 2011;40(12):614–615. [PubMed] [Google Scholar]
- 10.Zmistowski B. Diagnosis of periprosthetic joint infection. J Orthop Res. 2014;32(Suppl 1):S98–S107. doi: 10.1002/jor.22553. [DOI] [PubMed] [Google Scholar]
- 11.Fernandez-Sampedro M. 26Postoperative diagnosis and outcome in patients with revision arthroplasty for aseptic loosening. BMC Infect Dis. 2015;15 doi: 10.1186/s12879-015-0976-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berbari E. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2010;92(11):2102–2109. doi: 10.2106/JBJS.I.01199. [DOI] [PubMed] [Google Scholar]
- 13.Ting N.T., Della Valle C.J. Diagnosis of periprosthetic joint infection-an algorithm-based approach. J Arthroplasty. 2017;32(7):2047–2050. doi: 10.1016/j.arth.2017.02.070. [DOI] [PubMed] [Google Scholar]
- 14.Parvizi J. Aseptic loosening of total hip arthroplasty: infection always should be ruled out. Clin Orthop Relat Res. 2011;469(5):1401–1405. doi: 10.1007/s11999-011-1822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ince A. Is "aseptic" loosening of the prosthetic cup after total hip replacement due to nonculturable bacterial pathogens in patients with low-grade infection? Clin Infect Dis. 2004;39(11):1599–1603. doi: 10.1086/425303. [DOI] [PubMed] [Google Scholar]
- 16.Zimmerli W., Trampuz A., Ochsner P.E. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645–1654. doi: 10.1056/NEJMra040181. [DOI] [PubMed] [Google Scholar]
- 17.Randau T.M. Interleukin-6 in serum and in synovial fluid enhances the differentiation between periprosthetic joint infection and aseptic loosening. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parvizi J., Gehrke T. Definition of periprosthetic joint infection. J Arthroplasty. 2014;29(7):1331. doi: 10.1016/j.arth.2014.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Toossi N. Serum white blood cell count and differential do not have a role in the diagnosis of periprosthetic joint infection. J Arthroplasty. 2012;27(8 Suppl):51–54 e1. doi: 10.1016/j.arth.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 20.Garvin K.L., Konigsberg B.S. Infection following total knee arthroplasty: prevention and management. Instr Course Lect. 2012;61:411–419. [PubMed] [Google Scholar]
- 21.Vasso M., Schiavone Panni A. Low-grade periprosthetic knee infection: diagnosis and management. J Orthop Traumatol. 2015;16(1):1–7. doi: 10.1007/s10195-014-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greidanus N.V. Use of erythrocyte sedimentation rate and C-reactive protein level to diagnose infection before revision total knee arthroplasty. A prospective evaluation. J Bone Joint Surg Am. 2007;89(7):1409–1416. doi: 10.2106/JBJS.D.02602. [DOI] [PubMed] [Google Scholar]
- 23.Springer B.D. The diagnosis of periprosthetic joint infection. J Arthroplasty. 2015;30(6):908–911. doi: 10.1016/j.arth.2015.03.042. [DOI] [PubMed] [Google Scholar]
- 24.Spangehl M.J. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am. 1999;81(5):672–683. doi: 10.2106/00004623-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Cui Q. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J Bone Joint Surg Am. 2007;89(4):871–882. doi: 10.2106/JBJS.E.01070. [DOI] [PubMed] [Google Scholar]
- 26.Lopez D. Management of the infected total hip arthroplasty. Indian J Orthop. 2017;51(4):397–404. doi: 10.4103/ortho.IJOrtho_307_16. [DOI] [PMC free article] [PubMed] [Google Scholar]