Abstract
Background:
The Affordable Care Act (ACA) mandates that most women of reproductive age with private health insurance have full contraceptive coverage with no out-of-pocket costs, creating an actionable time for women to evaluate their contraceptive choices without cost considerations. The MyNewOptions study is a three-arm randomized controlled trial testing web-based interventions aimed at assisting privately insured women with making contraceptive choices that are consistent with their reproductive goals.
Methods:
Privately-insured women between the ages of 18 and 40 not intending pregnancy were randomly assigned to one of three groups: 1) a reproductive life planning (RLP) intervention, 2) a reproductive life planning enriched with contraceptive action planning (RLP+) intervention, or 3) an information only control group. Both the RLP and RLP+ guide women to identify their individualized reproductive goals and contraceptive method requirements. The RLP+ additionally includes a contraceptive action planning component, which uses if-then scenarios that allow the user to problem solve situations that make it difficult to be adherent to their contraceptive method. All three groups have access to a reproductive options library, containing information about their contraceptive coverage and the attributes of alternative contraceptive methods. Women completed a baseline survey with follow-up surveys every 6 months over 2 years concurrent with intervention boosters. Study outcomes include contraceptive use and adherence. ClinicalTrials.gov Identifier: NCT02100124
Discussion:
Results from the MyNewOptions study will demonstrate whether web-based reproductive life planning, with or without contraceptive action planning, helps insured women make patient-centered contraceptive choices compared with an information-only control condition.
BACKGROUND
In 2008, over half of all pregnancies in the United States were unintended, representing an increasing incidence over the prior decade (Finer & Zolna, 2014). Prior research has shown that when contraception is provided at no cost and accompanied by contraceptive information or dedicated contraceptive counseling, women are more likely to use prescription contraception and to choose more effective and more expensive methods over less effective, less expensive methods (Gariepy, Simon, Patel, Creinin, & Schwarz, 2011; Pace, Dusetzina, Fendrick, Keating, & Dalton, 2013; Peipert, Madden, Allsworth, & Secura, 2012; Postlethwaite, Trussell, Zoolakis, Shabear, & Petitti, 2007; Secura et al., 2014). The Patient Protection and Affordable Care Act (ACA) requires private insurance plans provide all FDA-approved contraceptive methods (including sterilization) and contraceptive counseling as a covered benefit without copays or deductibles (The Henry J. Kaiser Family Foundation, 2014), thereby removing the cost barrier to contraception for most privately insured women. However, removing the cost barrier to contraception will not necessarily improve contraceptive adherence or reduce unintended pregnancies unless women are also made aware of their covered benefits and given tools to help them optimize their contraceptive decision making.
The MyNewOptions study was designed to test the hypothesis that reproductive life planning and contraceptive action planning are tools that can help insured women to: (a) choose contraception that is compatible with their reproductive goals and, (b) use contraception correctly. The MyNewOptions study is a randomized controlled trial targeting insured women, a group who may benefit from interventions aimed at improving contraceptive adherence and reducing unintended pregnancies in the context of the ACA’s contraceptive mandate.
Theoretical Framework for the MyNewOptions Interventions
The MyNewOptions interventions are based on principles of self-regulation from social cognitive theory (Bandura, 1991; Glanz, Rimer, & Wiswanath, 2008). Social cognitive theory has guided the design of many health behavior change interventions. This approach assumes that behavior is goal-directed and that both self-efficacy (belief in one’s ability to attain a goal) and motivation for behavior change determine behavior. Through self-regulation, individuals can perform short-term behaviors in order to achieve a positive long-term goal. Self-regulation involves controlling one’s behaviors through self-monitoring, goal setting, feedback, self-reward, self-instruction, and enlistment of social support (Glanz et al., 2008).
In the present context, when a woman chooses a contraceptive method, she is deciding what short-term behaviors she is willing to accept (i.e., taking a pill daily, getting an IUD, negotiating with her partner to use a condom) to achieve the goal of avoiding unintended pregnancy. The proposed interventions will engage women through goal setting (through reproductive life planning), self-instruction (through action planning), and feedback (by providing feedback on one’s contraceptive behavior and adherence).
Intervention Components
Reproductive Life Plan.
A reproductive life plan articulates an individual’s goals for having or not having children, as well as a plan for how to achieve those goals. Reproductive life planning may be a useful tool for several reasons. First, it may help women clarify their intentions and reduce feelings of ambivalence about whether or not to have a child at a given time. This is important because ambivalence toward pregnancy has been shown to be associated with contraceptive nonuse, ineffective use, and risk for unintended pregnancy (Schwarz, Lohr, Gold, & Gerbert, 2007). Second, reproductive life planning encourages women and men to think about when the ideal time is to have a baby, factoring in other important considerations including health, job/career, school, finances, pregnancy spacing, partner preferences, and age. Third, it encourages women to think about what contraception method(s) will best help attain their reproductive goals at the same time as meeting their personal requirements for a contraceptive method. In 2009, the Centers for Disease Control and Prevention (CDC)’s Recommendations to Improve Preconception Health and Health Care recommended that each woman, man, and couple be encouraged to have a reproductive life plan (Johnson et al., 2006). Since then, several other organizations have made similar recommendations, including the Title X Family Planning Programs (U.S. Department of Health & Human Services Office of Population Affairs, 2014), and various reproductive life plan tools are now available online. However, whether reproductive life planning decreases ambivalence about future pregnancy, improves contraceptive decision-making, or reduces the risk of unintended pregnancy has not been formally evaluated.
Action Planning.
Contraceptive discontinuation and ineffective use occur commonly—a decision analysis estimated that 20% of the 3.5 million unintended pregnancies that occur each year in the U.S. are attributable to poor adherence or discontinuation of oral contraceptives (Rosenberg, Waugh, & Long, 1995). Poor adherence occurs when women use contraceptives that are not suited to their lifestyle (e.g., because the contraceptive requires frequent ongoing action) or when they have poor self-regulation skills needed to achieve better adherence. Action planning interventions (also known as “if-then planning,” “implementation intentions,” or “contingency planning”) are based on self-regulation and seek to help individuals overcome obstacles to poor adherence.
Action planning interventions present participants with common situations that make it difficult to perform a desired behavior. Next, they ask participants to make a specific plan for what they will do when faced with the specific situational barrier (i.e., “if situation X is encountered, then I will initiate goal-directed behavior Y.”) By specifying when, where, and how one will act, action planning passes control of behavior to future environmental cues, reducing the need for cognitive control and effort (Achtziger, Gollwitzer, & Sheeran, 2008; Gollwitzer & Sheeran, 2006). These interventions have been shown to be highly effective at improving many behaviors, including weight loss (Armitage, 2014; Luszczynska, Sobczyk, & Abraham, 2007; Zandstra, den Hoed, van der Meer, & van der Maas, 2010), smoking (Armitage, 2007, 2008; Armitage & Arden, 2008), alcohol intake (Arden & Armitage, 2012; Armitage & Arden, 2012; Armitage, Harris, & Arden, 2011), physical activity (Armitage & Arden, 2010; Armitage & Sprigg, 2010), and fruit and vegetable consumption (Armitage, 2014; Chapman & Armitage, 2010; Stadler, Oettingen, & Gollwitzer, 2010). Action planning interventions are ideally suited for contraceptive adherence, because effective contraceptive use often requires a series of behaviors to occur that are repeatedly met with certain barriers—e.g., obtaining a prescription, buying condoms, filling/refilling the prescription from a pharmacy, taking a pill every day, using a condom at each instance of intercourse. In a U.K. study by Martin and colleagues, contraceptive action planning for oral contraceptive and condom users was shown to improve contraceptive adherence and reduce unintended pregnancy among a sample of teenage girls presenting to family planning clinics (Martin, Sheeran, Slade, Wright, & Dibble, 2009, 2011).
STUDY DESIGN
Study Objectives
MyNewOptions is a two-year, randomized controlled trial with a three-arm parallel group design, conducted completely online. The primary objective of the MyNewOptions study is to compare contraceptive use and adherence in women who are randomized to reproductive life planning alone, reproductive life planning plus contraceptive action planning, and a control group. Secondary objectives include comparing effectiveness of contraceptive methods chosen, method satisfaction, and contraceptive self-efficacy. This study has been approved by the Institutional Review Board of the XXXXXX.
Patient Engagement
Listening sessions.
A priority of the MyNewOptions study is to include patients in all phases of the study design and execution. During proposal development, 12 insured women of reproductive age participated in 2 listening sessions, which were group sessions for the research team to obtain input from women on how to adapt the CDC’s reproductive life plan tool (Centers for Disease Control and Prevention) into a patient-centered, interactive web-based format. Women discussed what kind of reproductive planning was realistic for them (e.g., unrealistic to make a life plan, but realistic to make a 5-year plan). Women in the listening sessions also shared their personal challenges with contraceptive adherence, which were then used to identify the barriers included in the contraceptive action planning intervention. The women also suggested strategies for reporting information summaries back to the website user after one completes their reproductive life planning and contraceptive action planning exercises.
Patient Advisory Group.
The MyNewOptions Patient Advisory Group (PAG) was subsequently formed to provide patient stakeholder input during all stages of study execution. Eleven reproductive age women who are privately insured form the PAG, with one woman serving as the PAG coordinator. The PAG coordinator is a member of the MyNewOptions research team and attends the monthly investigator meetings. The PAG provided substantive input to the research team on intervention refinement. For example, the MyNewOptions PAG carefully reviewed and pilot tested prototype action plans for birth control pills, condoms, and natural family planning to ensure they were realistic, woman-centered, and viewed as helpful. The action plans were revised to include additional challenging scenarios that could occur with specific method use as well as additional solutions. The PAG also guided website design, recruitment and retention strategies, and design of recruitment materials.
Participants
Inclusion and Exclusion Criteria.
Study participants are 18–40 years of age; privately insured with Highmark Health (a large private health insurer based in Pennsylvania); have Internet access; are sexually active (within the past 6 months or expected in the next 6 months); and wish to avoid pregnancy for at least the next 12 months. Exclusion criteria are having had a tubal ligation, hysterectomy, or a current partner with a vasectomy; and not able to read and write English.
Recruitment.
Highmark identified members with prescription medication coverage who met the following criteria: women who were 18–40 years of age, resided in Pennsylvania, were not covered by an employer group with a religious exception to contraceptive coverage, and had not had a previous Highmark claim for a tubal ligation, hysterectomy, or infertility-related service. Inclusion was not limited to women who were newly insured, but rather included women regardless of how long they had been Highmark members. Because Highmark required an “opt in” approach to participant recruitment, Highmark staff identified a random sample of 15,000 members who met these criteria and mailed them the following recruitment materials: 1) a pre-invitation postcard introducing the MyNewOptions study, 2) a study invitation (one week following the postcard), and 3) a reminder (two weeks following the study invitation). The study invitation and reminder were mailed in sealed envelopes with Highmark’s return address visible on the outside. The mailings invited women to visit the MyNewOptions website to learn more about the study, or to call study staff at the [institution name blinded by WHI editors for peer review] if they had questions. Trained research staff monitored phone, email and website generated questions and responded to each inquiry within one business day. Women enrolled in the study online.
The homepage of the My New Options study website included a written and video description of the study. Women were prompted to enter their unique invitation code, which was printed on the study invitation and reminder, if they were interested in proceeding. The code was required to gain entry past the homepage of the study website; this authentication process was designed to ensure that only women invited to be in the study were able to enroll and participate. Potential participants could then view the study details, eligibility criteria, and the consent documents. If women indicated interest in proceeding, they were directed to REDCap (Research Electronic Data Capture), a secure, web-based application designed exclusively to support surveys for research studies (Harris et al., 2009).
Consent.
Participants were required to check a box during the eligibility process assenting to the Summary Explanation of Research document, which described the study in detail, the rights of the research participant, the potential risks associated with study participation, and a Certificate of Confidentiality from the federal government (a document protecting the research team from being forced to share court ordered information about participants). Participants also agreed to allow Highmark to provide MyNewOptions study investigators with participant contraceptive health claims data for claims occurring 6 months prior to study enrollment until the end of the 2-year study period, including pharmacy claims data to estimate contraceptive adherence with methods that require regular pharmacy dispensed prescriptions.
Baseline Survey and Randomization
Once consented, women received an email containing a web link to the baseline survey in REDCap. The baseline survey was designed to take approximately 20 minutes to complete and collected information about sexual and contraceptive history, pregnancy history, pregnancy intentions, current contraceptive use and adherence, and sociodemographics.
After completing the baseline survey, women were redirected to the MyNewOptions study website where they created a unique username and password and then were immediately randomized to one of the three study conditions. Randomization was accomplished by means of a permuted-block algorithm to achieve 1:1:1 allocation into one of the following groups: 1) RLP, 2) RLP+, or 3) information only (control). Participants then viewed website content specific to their group allocation. Regardless of group allocation, all MyNewOptions participants began their website visit by viewing information about the ACA mandate requiring health plans to cover all FDA-approved contraceptive methods without cost-sharing. All website materials were written at a 6th-7th grade reading level.
Study Conditions
RLP Condition.
Women assigned to the RLP group completed the RLP intervention after the baseline survey. The RLP intervention was designed by the research team and PAG, as described above, to help women: 1) create a reproductive plan, and 2) choose a contraceptive method that is best suited for their personal reproductive goals and personal requirements for a contraceptive method.
Similar to the CDC’s reproductive life plan (Centers for Disease Control and Prevention), the RLP guides women to determine whether or not they intend pregnancy in the next 5 years based on their current goals for school, marriage/partnership, job/career, finances, and other important life circumstances. When applicable, information is provided that may help their personal decision-making, such as risks associated with older age (e.g., decreased fertility, increasing risk of chromosomal abnormalities) and benefits of pregnancy spacing. Using the RLP, women specify if they plan to have children in the next 5 years, how many children they plan to have, and when they plan on having them. The RLP emphasizes that the plan is not set in stone, but can be fluid over time as life circumstances change. Thus, women are encouraged to revisit the website to edit their reproductive plan as needed.
The second objective of the RLP intervention is to assist women in making contraceptive choices that are best suited for the reproductive plan they just created and their personal requirements for a contraceptive method—i.e., reversibility, effectiveness, frequency of use, side effects that are or are not personally acceptable, medical conditions or health risks that may contraindicate a particular method, whether protection from sexually transmitted infections (STIs) is needed, and whether non-contraceptive benefits of certain methods are important. For example, a woman currently using oral contraceptives who occasionally misses pills is asked to consider whether the 9% typical-use failure rate is acceptable, and she is given the option to consider more effective methods (Hatcher et al., 2011). Another woman may indicate that she is not willing to manage her contraception on a regular basis, and would rather “get it and forget it.”
The RLP intervention then summarizes information about the contraceptive method(s) that meets all or most of the woman’s requirements, some of her requirements, or none of her requirements, so she can choose the method that best suits her individual contraceptive needs (or confirm that her current method is the best choice). After completing the RLP, the participant can print, save, or email herself her personal reproductive life plan, specifying her goals for future pregnancy, when she wants to be pregnant, how far apart she wants her children, and how she plans to prevent pregnancy until she is ready to be pregnant. If a woman decides to change her method as a result of the RLP intervention, she is directed to contact her health care provider if the change requires a prescription or procedure. If she does not have a current health care provider, the RLP intervention directs her to the Highmark member services site that will help her find a provider in her area. We expected the RLP intervention would take approximately 30 minutes to complete.
Women in the RLP group subsequently get an RLP booster after completing the 6-month, 12-month, and 18-month surveys (there is no booster at 24-months). The RLP booster instructs the participant to view and confirm her previous reproductive life plan, or she can develop a new plan.
RLP+ Condition.
The Reproductive Life Planning Plus (RLP+) intervention is the RLP intervention described above plus an additional contraceptive action planning step aimed at improving contraceptive adherence. Each woman is shown a list of situations that may challenge her ability to use her birth control method perfectly; she then selects which situations she believes could happen to her. For each situation, she is shown a list of possible strategies for managing the scenario and asked to pick one of the strategies or to come up with her own plan. Participants can complete action plans for more than one contraceptive method, if desired. We expected the RLP+ intervention would take approximately 45 minutes to complete.
Women assigned to the RLP+ group subsequently complete an RLP+ booster after the 6-month, 12-month, and 18-month surveys (there is no booster at 24-months). In the RLP+ booster the participant views and confirm her previous reproductive life plan, or she can develop a new plan. She also completes the contraception action plan again. While most action planning intervention studies only use a single intervention “dose,” Chapman and colleagues observed that a “booster” dose significantly increased the impact of action planning interventions (Chapman & Armitage, 2008, 2010). Women still using the same birth control method will be asked to complete an action plan for that same method, while women using a different birth control method will complete an action plan for the new method.
Information Only Control Condition.
The information only control condition is also delivered on the study website. Like the intervention groups, women in the control group view information about the contraceptive coverage mandate as required by ACA and have access to information about all FDA-approved contraceptive methods, using patient education materials from the American College of Obstetricians and Gynecologists (ACOG)(The American Congress of Obstetricians and Gynecologists, 2015), the National Campaign to Prevent Teen and Unplanned Pregnancy (The National Campaign to Prevent Teen and Unplanned Pregnancy, 2015), and the Association of Reproductive Health Professionals (Association of Reproductive Health Professionals, 2015).
Follow-up surveys and intervention boosters
Participants receive an email 6 months after completing their baseline survey inviting them to take their next survey in REDCap. The same process is repeated at 12, 18 and 24 months post baseline. Surveys measure any interval pregnancies, current pregnancy intentions, current contraceptive use, and current contraceptive adherence. Surveys are conducted at 6-month intervals (as opposed to longer intervals) to improve recall of contraceptive history and to capture life changes (e.g., partner changes, job changes) that could affect pregnancy intentions. Non-responders receive email and phone reminders up to 3 weeks after the initial reminder for completing the survey.
Following the completion of each follow-up survey, all participants are again reminded that their health plan is required to cover all FDA-approved contraceptive methods without co-pays. They are then directed to complete boosters of their respective conditions, according to their randomization allocation.
Participant retention
Participants receive a $25 incentive for completing the baseline survey and each of the 4 follow-up surveys, for a total of $125 for perfect retention throughout the 2-year study. Incentives are in the form of gift cards from companies recommended by the PAG. Participants also are emailed electronic newsletters bi-annually to keep them informed about the study and to alert them of upcoming surveys. Emailing newsletters also alerts us in advance of any disabled email addresses allowing us to contact participants by phone to obtain updated contact information.
Sample size
The pre-specified sample size for the study was 972 randomized participants (324 for each of the three study groups). Sample size was calculated for detecting a 10% difference in contraceptive use (25% vs. 35% in nonuse) with 90% statistical power using a two-sided, 0.025 significance level test (Bonferroni correction) comparing RLP to control, RLP+ to control, and RLP to RLP+, with an expected attrition of 10% lost to follow-up per year and another 10% lost per year for those women who become pregnant (intentionally or unintentionally).
Planned analyses
The primary outcome variable is contraceptive use when not intending pregnancy, which will be defined in 2 ways: 1) whether the participant is using any contraceptive method to prevent pregnancy (e.g., hormonal methods, barrier methods, withdrawal, natural family planning, etc), and 2) whether the participant is using any contraceptive method that requires a health care provider visit, procedure, or prescription. These contraceptive use variables will be defined as binary variables (yes/no) at each 6-month interval post-baseline (6, 12, 18, and 24 months). We will construct a proportion for each participant as the number of time periods in which the participant is using contraception, divided by the number of time periods in which the participant is not intending pregnancy. We will apply a binomial regression analysis to these proportions, using intervention group assignment (intention-to-treat analysis) as the sole regressor in the primary analysis, but we will investigate in secondary analyses the effects of selected covariates on the proportional response (demographics; pregnancy history; sexual and contraceptive history; perceived control/fatalism toward contraception; relationships; compliance with completing intervention and boosters). In terms of the three randomized groups, we will construct two-sided test statistics for comparing: 1) RLP to control, 2) RLP+ to control, and 3) RLP to RLP+. Therefore, we will impose a Bonferroni correction factor to the significance level (alpha = 0.0167). We will apply additional secondary analyses that are longitudinal, in which we invoke a logistic regression model with random participant effects to investigate if there are time period effects and/or time period by intervention interactions for the binary outcomes. Finally, we will invoke a shared parameter model (Vonesh, Greene, & Schluchter, 2006) to account for the informative censoring that could occur due to participant withdrawal in a longitudinal study. In our analysis, the shared parameter model includes a Weibull time-to-event regression model for the time to participant withdrawal in conjunction with a logistic regression model with random participant effects for the binary outcome.
Secondary outcome measures include contraceptive adherence, effectiveness of contraceptive methods chosen, method satisfaction, and contraceptive self-efficacy. Contraceptive adherence will be classified as high, medium, and low using self-report and pharmacy claims data (using medication possession ratios, when applicable) (Borrero et al., 2013; Burger & Inderbitzen, 1985; Hall, White, Reame, & Westhoff, 2010; Jaccard, Dittus, & Gordon, 1996). For women using LARCs, adherence will be categorized as high. Contraceptives will be classified into tiers based on published effectiveness rates (no method, less effective, more effective, and most effective methods) (Centers for Disease Control and Prevention, 2015). A validated 5-item contraceptive satisfaction measure will be used that measures satisfaction with ease of use, effectiveness, side effects, cost, and overall satisfaction (Rosenberg, Waugh, & Burnhill, 1998). For the purposes of the MyNewOptions study, we developed and pilot tested a 9-item contraceptive self-efficacy scale for adult women. Pilot testing indicated good internal reliability with a Cronbach’s alpha of 0.78.
MyNewOptions enrolled sample
Participant recruitment for the MyNewOptions study occurred between April and August 2014. A total of 994 women were enrolled in the study and randomized (see Figure 1), of whom 7 were later found to be ineligible due because they indicated on the baseline survey that they were intending pregnancy in the next year (n=5) or were not part of the original sampling frame (n=2), resulting in a study sample size of 987. Table 1 shows the characteristics of the enrolled study sample in comparison to the 13,623 women in the sampling frame who were not enrolled in the study. Women in the MyNewOptions study are slightly younger (mean age 27.1 vs. 28.0, p<0.0001) compared with women in the sampling frame, but are representative of the sampling frame in terms of Pennsylvania region and rural/urban residence. U.S. Census definitions for rural/urban residence was used based on Rural Urban Commuting Area (RUCA) codes.
Figure.
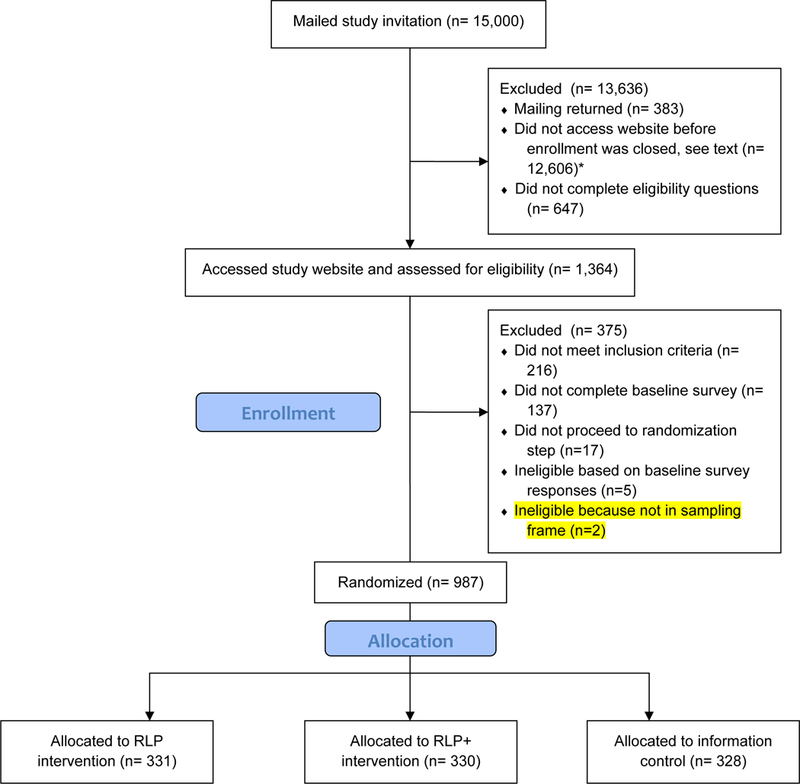
MyNewOptions Enrollment and Randomization * Target sample was attained in 4 months
Table.
Comparison of MyNewOptions study sample (N=987) with the sampling frame (N=13,623)
| Women in sampling frame not enrolled in the MyNewOptions study (n=13,623) |
MyNewOptions study sample (n=987) |
p-value* | |
|---|---|---|---|
| Age group (years) 18–25 26–33 34–40 |
5953 (43.7) 4127 (30.3) 3543 (26.0) |
449 (45.5) 365 (37.0) 173 (17.5) |
<0.001 |
| Pennsylvania region Northeast Southeast Northcentral Southcentral Northwest Southwest |
979 (7.2) 189 (1.4) 361 (2.7) 3121 (22.9) 2152 (15.8) 6815 (50.1) |
59 (6.0) 11 (1.1) 20 (2.0) 235 (23.8) 160 (16.2) 501 (50.8) |
0.508 |
| Rural/Urban residence Urban Rural |
10256 (75.7) 3298 (24.3) |
746 (76.0) 236 (24.0) |
0.832 |
Chi-square test
DISCUSSION
By eliminating the out-of-pocket costs for contraception, the ACA mandate was instituted with the expectation of increasing the use of effective contraception, reducing unintended pregnancies, and improving birth spacing. While we expect that removing the cost barrier will enable women to choose more effective (and more expensive) contraceptive methods, this depends on women’s awareness of their contraceptive coverage benefits and of the attributes of alternative methods so that they can select a method that best meets their reproductive, personal, and health-related needs. We hypothesize that this process will be accelerated if tools such as reproductive life planning and contraceptive action planning are made available to women with contraceptive coverage (Weisman and Chuang 2014).
The primary strength of the MyNewOptions study is that it allows for testing of reproductive life planning and contraceptive action planning interventions in a randomized controlled trial design. Reproductive life planning has been recommended by the CDC, federally-funded family planning clinics, and many reproductive health experts, but it has not yet been rigorously tested to determine if it is an effective intervention for reducing ambivalence about future pregnancy intent, improving contraceptive use, reducing unintended pregnancies, or helping women meet their individual reproductive goals. In addition, MyNewOptions uses a web-based format, which would increase the ability to disseminate widely and reach more women if the interventions were found to be effective.
The main weakness of the MyNewOptions study design is the potential for selection bias. Although a random sample of female Highmark members in the target age group was invited to participate, the women who chose to enroll in the study could differ from the women who did not choose to enroll. Although the enrollees were only slightly younger from non-enrollees and did not differ in terms of geographic residence, it is unknown how they may differ by race/ethnicity, income, current contraceptive attitudes and behavior, or other characteristic that may be relevant to contraceptive decision-making. In addition, because the study is conducted in one state, results may not be generalizable to insured women in other geographic areas.
IMPLICATIONS FOR PRACTICE AND POLICY.
In the context of first-dollar insurance coverage for contraception, reproductive life planning and contraceptive action planning interventions may assist women to choose contraceptive methods better suited for their individual needs, to be more adherent to those methods, and to reduce unintended pregnancy and improve birth spacing. The MyNewOptions study uses a web-based version of reproductive life planning and contraceptive action planning interventions intended for privately insured women. If effective, these interventions could be easily adapted to be used by employers, payors, or providers to reach a broad population of insured women.
Acknowledgements:
The authors would like to thank Suzanne Stoner and Vanessa Adjei for their assistance with participant recruitment; John Webster and Robert Stouffer of The John Webster Company for web design; and the members of the MyNewOptions Patient Advisory Group (Kathy Robbins, Brooke Hess, Melissa Halvin, Adrienne Billmyer, Shellie Reigel, Roberta Stacer, Kristin Samson, Lauren Miller, Stephanie Sanders, and Allyson Billmyer) and listening session participants for their contributions to study design. We would like to thank Highmark Health for their assistance with participant recruitment; the findings and conclusions presented are solely those of the authors and do not represent the views of Highmark Health.
Funding statement: This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Program Award (CD-1304–6117). All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee.
Study data were collected and managed using REDCap electronic data capture tools hosted at the Penn State Milton S. Hershey Medical Center and College of Medicine. REDCap is supported by the Penn State Clinical & Translational Science Institute, Pennsylvania State University CTSI, NIH/NCATS Grant Number UL1 TR000127. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH/NCATS.
References
- Achtziger A, Gollwitzer PM, & Sheeran P (2008). Implementation intentions and shielding goal striving from unwanted thoughts and feelings. Pers Soc Psychol Bull, 34(3), 381–393. doi: 10.1177/0146167207311201 [DOI] [PubMed] [Google Scholar]
- Arden MA, & Armitage CJ (2012). A volitional help sheet to reduce binge drinking in students: a randomized exploratory trial. Alcohol Alcohol, 47(2), 156–159. doi: 10.1093/alcalc/agr164 [DOI] [PubMed] [Google Scholar]
- Armitage CJ (2007). Efficacy of a brief worksite intervention to reduce smoking: the roles of behavioral and implementation intentions. J Occup Health Psychol, 12(4), 376–390. doi: 10.1037/1076-8998.12.4.376 [DOI] [PubMed] [Google Scholar]
- Armitage CJ (2008). A volitional help sheet to encourage smoking cessation: a randomized exploratory trial. Health Psychol, 27(5), 557–566. doi: 10.1037/0278-6133.27.5.557 [DOI] [PubMed] [Google Scholar]
- Armitage CJ (2014). Evidence that self-incentives increase fruit consumption: a randomized exploratory trial among high-risk romanian adolescents. Prev Sci, 15(2), 186–193. doi: 10.1007/s11121-012-0346-6 [DOI] [PubMed] [Google Scholar]
- Armitage CJ, & Arden MA (2008). How useful are the stages of change for targeting interventions? Randomized test of a brief intervention to reduce smoking. Health Psychol, 27(6), 789–798. doi: 10.1037/0278-6133.27.6.789 [DOI] [PubMed] [Google Scholar]
- Armitage CJ, & Arden MA (2010). A volitional help sheet to increase physical activity in people with low socioeconomic status: A randomised exploratory trial. Psychol Health, 25(10), 1129–1145. doi: 10.1080/08870440903121638 [DOI] [PubMed] [Google Scholar]
- Armitage CJ, & Arden MA (2012). A volitional help sheet to reduce alcohol consumption in the general population: a field experiment. Prev Sci, 13(6), 635–643. doi: 10.1007/s11121-012-0291-4 [DOI] [PubMed] [Google Scholar]
- Armitage CJ, Harris PR, & Arden MA (2011). Evidence that self-affirmation reduces alcohol consumption: randomized exploratory trial with a new, brief means of self-affirming. Health Psychol, 30(5), 633–641. doi: 10.1037/a0023738 [DOI] [PubMed] [Google Scholar]
- Armitage CJ, & Sprigg CA (2010). The roles of behavioral and implementation intentions in changing physical activity in young children with low socioeconomic status. J Sport Exerc Psychol, 32(3), 359–376. [DOI] [PubMed] [Google Scholar]
- Association of Reproductive Health Professionals. (2015). Contraception Patient Resources Retrieved January 22, 2015, from http://www.arhp.org/topics/contraception/patient-resources
- Bandura A (1991). Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes, 50(2), 248–287. [Google Scholar]
- Borrero S, Zhao X, Mor MK, Schwarz EB, Good CB, & Gellad WF (2013). Adherence to hormonal contraception among women veterans: differences by race/ethnicity and contraceptive supply. [Research Support, U.S. Gov’t, Non-P.H.S.]. Am J Obstet Gynecol, 209(2), 103 e101–111. doi: 10.1016/j.ajog.2013.03.024 [DOI] [PubMed] [Google Scholar]
- Burger JM, & Inderbitzen HM (1985). Predicting contraceptive behavior among college students: the role of communication, knowledge, sexual anxiety, and self-esteem. Arch Sex Behav, 14(4), 343–350. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention.). Preconception Health and Health Care: My Reproductive Life Plan Retrieved January 15, 2015, from http://www.cdc.gov/preconception/reproductiveplan.html
- Centers for Disease Control and Prevention. (2015). Contraception: How effective are birth control methods?, from http://www.cdc.gov/reproductivehealth/UnintendedPregnancy/Contraception.htm
- Chapman J, & Armitage CJ (2008). Increasing fruit and vegetable intake over a six-month period: An investigation of ‘booster’ implementation intentions. Psychology & Health, 23, 79–79. [Google Scholar]
- Chapman J, & Armitage CJ (2010). Evidence that boosters augment the long-term impact of implementation intentions on fruit and vegetable intake. Psychol Health, 25(3), 365–381. doi: 10.1080/08870440802642148 [DOI] [PubMed] [Google Scholar]
- Finer LB, & Zolna MR (2014). Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health, 104 Suppl 1, S43–48. doi: 10.2105/AJPH.2013.301416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gariepy AM, Simon EJ, Patel DA, Creinin MD, & Schwarz EB (2011). The impact of out-of-pocket expense on IUD utilization among women with private insurance. Contraception, 84(6), e39–42. doi: 10.1016/j.contraception.2011.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Rimer B, & Wiswanath K (Eds.). (2008). Health behavior and health education: theory, research, and practice (4th ed.): Jossey-Bass. [Google Scholar]
- Gollwitzer PM, & Sheeran P (2006). Implementation intentions and goal achievement: A meta‐analysis of effects and processes. Advances in experimental social psychology, 38, 69–119. [Google Scholar]
- Hall KS, White KO, Reame N, & Westhoff C (2010). Studying the Use of Oral Contraception: A Review of Measurement Approaches. Journal of Womens Health, 19(12), 2203–2210. doi: DOI 10.1089/jwh.2010.1963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher, R. A., Trussell, J., Nelson, A. L., Cates, W., Kowal, D., & Poicar, M. S. (Eds.). (2011). Contraceptive Technology (20 ed.).
- Jaccard J, Dittus PJ, & Gordon VV (1996). Maternal correlates of adolescent sexual and contraceptive behavior. Fam Plann Perspect, 28(4), 159–165, 185. [PubMed] [Google Scholar]
- Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, Parker CS, . . . Select Panel on Preconception, C. (2006). Recommendations to improve preconception health and health care--United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep, 55(RR-6), 1–23. [PubMed] [Google Scholar]
- Luszczynska A, Sobczyk A, & Abraham C (2007). Planning to lose weight: randomized controlled trial of an implementation intention prompt to enhance weight reduction among overweight and obese women. Health Psychol, 26(4), 507–512. doi: 10.1037/0278-6133.26.4.507 [DOI] [PubMed] [Google Scholar]
- Martin J, Sheeran P, Slade P, Wright A, & Dibble T (2009). Implementation intention formation reduces consultations for emergency contraception and pregnancy testing among teenage women. Health Psychol, 28(6), 762–769. doi: 10.1037/a0016200 [DOI] [PubMed] [Google Scholar]
- Martin J, Sheeran P, Slade P, Wright A, & Dibble T (2011). Durable effects of implementation intentions: reduced rates of confirmed pregnancy at 2 years. Health Psychol, 30(3), 368–373. doi: 10.1037/a0022739 [DOI] [PubMed] [Google Scholar]
- Pace LE, Dusetzina SB, Fendrick AM, Keating NL, & Dalton VK (2013). The impact of out-of-pocket costs on the use of intrauterine contraception among women with employer-sponsored insurance. Med Care, 51(11), 959–963. doi: 10.1097/MLR.0b013e3182a97b5d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peipert JF, Madden T, Allsworth JE, & Secura GM (2012). Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol, 120(6), 1291–1297. doi: http://10.1097/AOG.0b013e318273eb56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postlethwaite D, Trussell J, Zoolakis A, Shabear R, & Petitti D (2007). A comparison of contraceptive procurement pre- and post-benefit change. Contraception, 76(5), 360–365. doi: 10.1016/j.contraception.2007.07.006 [DOI] [PubMed] [Google Scholar]
- Rosenberg MJ, Waugh MS, & Burnhill MS (1998). Compliance, counseling and satisfaction with oral contraceptives: a prospective evaluation. [Research Support, Non-U.S. Gov’t]. Fam Plann Perspect, 30(2), 89–92, 104. [PubMed] [Google Scholar]
- Rosenberg MJ, Waugh MS, & Long S (1995). Unintended pregnancies and use, misuse and discontinuation of oral contraceptives. J Reprod Med, 40(5), 355–360. [PubMed] [Google Scholar]
- Schwarz EB, Lohr PA, Gold MA, & Gerbert B (2007). Prevalence and correlates of ambivalence towards pregnancy among nonpregnant women. Contraception, 75(4), 305–310. doi: DOI 10.1016/j.contraception.2006.12.002 [DOI] [PubMed] [Google Scholar]
- Secura GM, Madden T, McNicholas C, Mullersman J, Buckel CM, Zhao Q, & Peipert JF (2014). Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med, 371(14), 1316–1323. doi: 10.1056/NEJMoa1400506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadler G, Oettingen G, & Gollwitzer PM (2010). Intervention effects of information and self-regulation on eating fruits and vegetables over two years. Health Psychol, 29(3), 274–283. doi: 10.1037/a0018644 [DOI] [PubMed] [Google Scholar]
- The American Congress of Obstetricians and Gynecologists. (2015). For Patients Retrieved January 22, 2015, from http://www.acog.org/patients/
- The Henry J. Kaiser Family Foundation. (2014). Preventive Services Covered by Private Health Plans under the Affordable Care Act Retrieved December 10, 2014, from http://files.kff.org/attachment/preventive-services-covered-by-private-health-plans-under-the-affordable-care-act-fact-sheet
- The National Campaign to Prevent Teen and Unplanned Pregnancy. (2015). Bedsider Retrieved January 22, 2015, from www.bedsider.org
- U.S. Department of Health & Human Services Office of Population Affairs. (2014). Title X Family Planning Program Priorities Retrieved January 15, 2015, from http://www.hhs.gov/opa/title-x-family-planning/title-x-policies/program-priorities/
- Vonesh EF, Greene T, & Schluchter MD (2006). Shared parameter models for the joint analysis of longitudinal data and event times. Stat Med, 25(1), 143–163. doi: 10.1002/sim.2249 [DOI] [PubMed] [Google Scholar]
- Zandstra EH, den Hoed W, van der Meer N, & van der Maas A (2010). Improving compliance to meal-replacement food regimens. Forming implementation intentions (conscious IF-THEN plans) increases compliance. Appetite, 55(3), 666–670. doi: 10.1016/j.appet.2010.09.021 [DOI] [PubMed] [Google Scholar]


