Abstract
Narcolepsy is the most common neurological cause of chronic sleepiness. The discovery about 20 years ago that narcolepsy is caused by selective loss of the neurons producing orexins (also known as hypocretins) sparked great advances in the field. Here, we review the current understanding of how orexin neurons regulate sleep–wake behaviour and the consequences of the loss of orexin neurons. We also summarize the developing evidence that narcolepsy is an autoimmune disorder that may be caused by a T cell-mediated attack on the orexin neurons and explain how these new perspectives can inform better therapeutic approaches.
Introduction
Narcolepsy affects about 1 in 2,000 people in the United States and Europe1–3. Every individual with narcolepsy shows some degree of excessive daytime sleepiness, with a tendency to doze off when sedentary in school, at work or even when driving. Most people with narcolepsy feel rested when they wake in the morning or after a nap, but within a few hours, they feel as sleepy as a healthy person would feel if awake for the entire night.
In addition to excessive daytime sleepiness, most people with narcolepsy also have symptoms indicative of abnormal rapid eye movement (REM) sleep. REM sleep is normally characterized by dreaming and muscle paralysis that prevents an individual from acting out their dreams. In narcolepsy, REM sleep can occur at any time of day, and elements of REM sleep can mix into wake, manifesting as hypnopompic and hypnagogic hallucinations or sleep paralysis. A very distinctive symptom of narcolepsy is cataplexy: sudden muscle paralysis triggered by strong, generally positive emotions, such as when laughing or unexpectedly meeting a friend. The muscle weakness of cataplexy usually begins in the face and neck and then sometimes spreads to the trunk and limbs; in severe episodes, an individual may slump to the ground, conscious yet unable to speak or move for a minute or two. Strangely, more than half of people with the classical form of narcolepsy also have the opposite problem: an intermittent failure of REM sleep paralysis, which results in the enactment of dreams (known as REM sleep behaviour disorder)4.
Narcolepsy has been studied by clinicians and researchers for almost 150 years, but only in the past 20 years has the underlying cause become clear. In 1998, two research groups independently discovered orexin A and orexin B (also known as hypocretin 1 and hypocretin 2, respectively), small neuropeptides produced solely by neurons in the lateral hypothalamus5,6. Derived from a precursor protein (prepro-orexin), orexin A and orexin B have excitatory effects on postsynaptic neurons via the orexin 1 receptor (OX1R) and OX2R6. Soon after, researchers found that narcolepsy is caused by a highly selective and severe loss of the orexin neurons that results in low levels of orexins in the brain and cerebrospinal fluid (CSF)7–10. This discovery spurred the recognition of two types of narcolepsy: narcolepsy type 1 (NT1) and narcolepsy type 2 (NT2)11. The classic phenotype, NT1, is characterized by chronic sleepiness plus cataplexy, and CSF orexin levels in this disorder are very low or undetectable, owing to severe loss of the orexin neurons. NT2 has generally less severe symptoms, and 90% of patients have normal CSF orexin levels. NT2 affects up to half of all narcolepsy patients1–3 and may be caused by a partial loss of the orexin neurons, but little is known about its underlying neuropathology12,13. In rare cases, narcolepsy results from brain injuries that damage the orexin neurons or their projections, and narcolepsy-like symptoms occur in some families, although the underlying genetics remain unknown14,15. In NT1, the rate of orexin neuron loss is unknown, but the loss may be rapid in some patients who develop severe narcolepsy symptoms over just a few days and slower in others who develop cataplexy many years after the onset of sleepiness16,17; some small studies have also shown a decrease in CSF orexin levels over several months from the onset of sleepiness18,19 (BOX 1).
Box 1 | Natural history of narcolepsy.
Narcolepsy typically begins in the early teen years1183. Over the course of a few days or weeks, sleepiness becomes quite problematic, with children falling asleep at school and when doing homework. In addition, many patients develop hypersomnia. For example, a 12-year-old who previously slept about 9 hours each night might now sleep 9–10 hours at night plus another 1–2 hours of napping in the day184. Over a few years, this hypersomnia resolves, but nocturnal sleep is often fragmented, with numerous spontaneous awakenings and vivid dreams. In children, abrupt weight gain is common, with about half of children gaining 5–15 kg in just a few months, possibly owing to a reduction in basal metabolism. About 1 in 6 children with narcolepsy can develop precocious puberty99.
Cataplexy often starts to occur in the first months after the initial increase in sleepiness but sometimes lags behind the sleepiness by years. Cataplexy in children can be quite severe and prolonged, sometimes manifesting as status cataplecticus2185. Some researchers suggest that moderate loss (~50%) of the orexin neurons causes sleepiness, whereas cataplexy and rapid transitions into rapid eye movement (REM) sleep during the day probably involve severe loss (>80%) of orexin neurons12,67,176. Although much remains to be learned about the natural history of narcolepsy, this evolution of symptoms suggests that the orexin neurons may die over a period of weeks to months, and if the cause of orexin neuron loss can be identified, it may be possible to halt this progression.
This clear connection of NT1 to selective loss of the orexin neurons sparked tremendous advances in our understanding of narcolepsy, yet major questions and controversies remain. This article reviews the normal functions of the orexin system and how loss of the orexin neurons results in the symptoms of narcolepsy. We examine the emerging evidence suggesting that an autoimmune process may kill the orexin neurons, and present crucial outstanding questions.
Orexin neurons: anatomy and functions
Anatomy.
The orexin peptides are produced only by a cluster of neurons in the lateral hypothalamus but are released by projections of these neurons to much of the CNS, from the cortex to the spinal cord. The orexin neurons heavily innervate several regions that promote arousal and suppress REM sleep, including the basal forebrain, tuberomammillary nucleus (TMN), periaqueductal grey (PAG), dorsal raphe (DR) and locus coeruleus (LC)20 (FIG. 1). They also innervate regions that regulate reward processing, such as the ventral tegmental area (VTA) and nucleus accumbens, as well as many brain areas implicated in feeding and metabolism (for example, the arcuate nucleus and lateral hypothalamus), and autonomic tone (for example, the paraventricular nucleus, parabrachial nucleus, nucleus of the solitary tract, rostral ventrolateral medulla, rostral ventromedial medulla and intermediolateral cell column of the spinal cord)20. In turn, the orexin neurons receive inputs from brain regions that regulate sleep–wake states (including the DR, LC and basal forebrain), circadian rhythms, reward processing (for example, the VTA), autonomic tone (such as the paraventricular nucleus), fear and anxiety, and regions associated with visceral sensations (including the nucleus of the solitary tract and parabrachial nucleus)21–24 (FIG. 2). This broad pattern of connections has spurred many researchers to hypothesize that the orexin neurons act as integrators of neuronal signals related to sleep–wake state, motivation and visceral needs such as hunger, to help enhance arousal and autonomic tone, especially when seeking food or other rewards, or responding to threats.
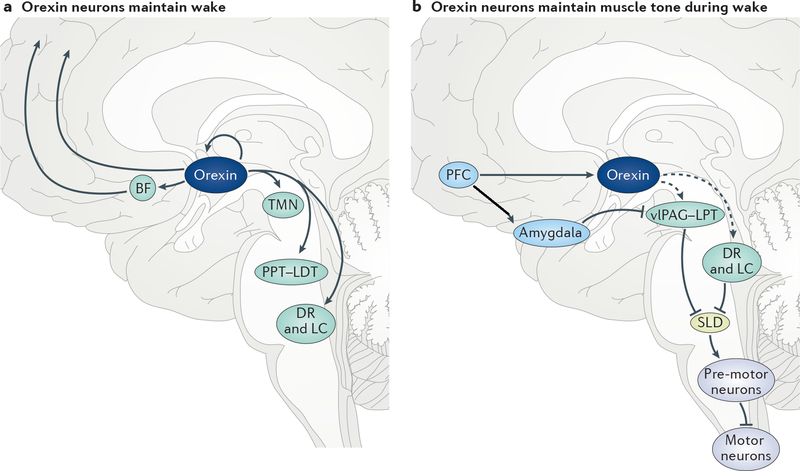
Fig. 1 |. Wake-promoting and cataplexy-suppressing orexin pathways.
a | Orexin neurons (dark blue) maintain wake by exciting various wake-promoting neurons (green), including those in the cortex, basal forebrain (BF), tuberomammillary nucleus (TMN), pedunculopontine and laterodorsal tegmental nuclei (PPT–LDT), dorsal raphe (DR) and locus coeruleus (LC). Orexin neurons may also undergo auto-excitation, helping drive sustained activity in the orexin neurons and their targets. b | Normally, orexin neurons (dark blue) block the occurrence of muscle paralysis during wake by activating rapid eye movement (REM) sleep-suppressing regions (green), such as neurons in the ventral lateral periaqueductal grey and lateral pontine tegmentum (vlPAG–LPT), DR and LC. All these nuclei inhibit the sublaterodorsal nucleus (SLD), a region which, during REM sleep, drives muscle paralysis by activating GABAergic premotor neurons that inhibit motor neurons (purple). With strong emotional stimuli, signals from the medial prefrontal cortex (mPFC) probably activate orexin neurons and neurons in the central nucleus of the amygdala, which have opposing effects on the vlPAG–LPT, DR and LC. However, in narcolepsy, the excitatory drive from the orexin neurons is absent, and signals from the amygdala can inhibit these REM sleep-suppressing regions, enabling activity in the SLD and resulting in cataplexy.
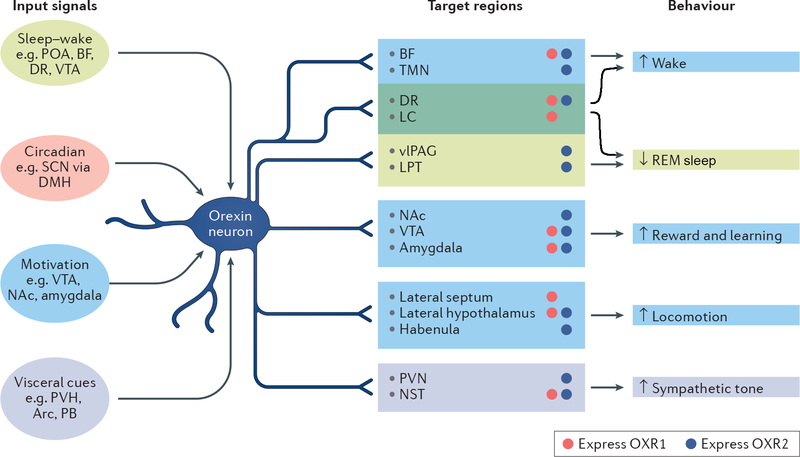
Fig. 2 |. Inputs and outputs of the orexin neurons.
The orexin neurons are influenced by signals related to sleep–wake states, circadian phase, motivational cues and visceral cues such as hunger or thirst, and they innervate many brain regions. Their activity ultimately results in long periods of wakefulness, suppression and regulation of rapid eye movement (REM) sleep, enhanced responses to rewards, increased locomotion and increased autonomic tone. In addition to the orexin neuropeptides, which bind to orexin 1 receptors (OX1Rs; red circles) and OX2Rs (dark blue circles), orexin neurons also release the fast-acting neurotransmitter glutamate and possibly dynorphin. This pattern of connections highlights how the orexin neurons are uniquely positioned to integrate a wide variety of signals to acutely and persistently promote many aspects of arousal. Arc, arcuate nucleus; BF, basal forebrain; DMH, dorsomedial nucleus of the hypothalamus; DR, dorsal raphe; LC, locus coeruleus; LPT, lateral pontine tegmentum; NAc, nucleus accumbens; NST, nucleus of the solitary tract; PB, parabrachial nucleus; POA, preoptic area; PVH, paraventricular nucleus of the hypothalamus; SCN, suprachiasmatic nucleus; TMN, tuberomammillary nucleus; vlPAG, ventrolateral periaqueductal grey; VTA, ventral tegmental area.
Activity and signalling.
Orexin neurons regulate many functions, and chief among these are stabilizing wakefulness and orchestrating REM sleep physiology25,26. In rodents and dogs, orexin neurons are active during wake, especially during increased locomotor activity or motivated behaviour such as foraging; by contrast, these neurons fire less during quiet wake and very little during non-REM (NREM) or REM sleep27–30. Photostimulation of the orexin neurons rouses mice from sleep, whereas their photoinhibition or chemoinhibition promotes sleep31–34. In addition, intracerebroventricular injection of orexin A or an orexin agonist in rodents can promote wakefulness and strongly suppress REM sleep for hours35,36, most probably by exciting neurons in the basal forebrain, PAG and monoaminergic nuclei that promote wake and suppress REM sleep. With the transition to sleep, GABAergic neurons in the ventrolateral preoptic and median preoptic areas likely inhibit the orexin neurons as well as many other wake-promoting neurons, allowing the animal to maintain sleep37–39.
How orexins produce such long periods of wake is unclear. Little is known about orexin kinetics in vivo, but orexin A may persist in the extracellular space for long periods, whereas orexin B is likely to have a shorter half-life6. Orexin peptides may auto-excite orexin neurons via OX2R (FIG. 1) and, as such, once these cells start firing, they may remain active for long periods, helping sustain wake over long periods40,41. However, this idea of auto-excitation is controversial, as some have reported that orexin neurons do not express orexin receptors42. Quite little is known about the firing patterns of orexin neurons, and more in vivo, long-term recordings are needed27,28.
Importantly, the conditions that trigger release of orexins are unknown, although high-frequency firing in the orexin neurons probably triggers their release from dense core vesicles31,43. In addition, as with other neuropeptides that are spontaneously released, some basal level of orexin tone may persist at all times; in support of this idea, orexin receptor antagonists promote sleep in humans even during the night, when orexin neurons might be expected to be inactive44,45.
The orexin neurons produce other neurotransmitters in addition to the orexin peptides. However, whether the loss of these co-transmitters contributes to the symptoms of narcolepsy is not clear. Glutamate is released by the orexin neurons, and its effects may synergize with the excitatory effects of orexins43,46,47. Orexin neurons probably also secrete neuronal activity-regulated pentraxin (NARP), a protein that promotes clustering of AMPA receptors at excitatory synapses48–50. The role of NARP in the orexin system is still undetermined, but it might enhance postsynaptic responses to glutamate. Surprisingly, the orexin neurons may also co-release dynorphin, which inhibits neurons via the κ-opioid receptor51,52. In mice, κ-opioid receptors are found in most of the same brain regions as the orexin receptors, and how the excitatory effects of orexins are integrated with the inhibitory effects of dynorphin is an active area of research52,53. Orexin and dynorphin have synergistic effects on some neurons; for example, orexin neurons themselves can be excited by orexin B, and perhaps by orexin A, and local GABAergic inputs to the orexin neurons are inhibited by dynorphin, thus disinhibiting the orexin neurons40,41,54. The net effect of these co-transmitters on other neurons may depend on the resting membrane potential of the cell or the specifics of its connectivity53,55. Nevertheless, these co-transmitters are probably important, as mice lacking the orexin neurons exhibit a phenotype that is closer to human NT1 than that of mice simply lacking the orexin peptides (BOX 2). Fully understanding the consequences of orexin neuron loss in NT1 will require more work into the contributions of these co-transmitters.
Box 2 | Comparison of human type 1 narcolepsy and murine and canine models.
Mouse and canine models of narcolepsy capture many of the key features of the disease and enable researchers to study the underlying molecular and circuit-level neurobiology. Poor maintenance of wakefulness (short bouts of wake during the active period) is common in most mouse models26,69,71,77,186. Mice lacking the orexin neurons, such as mice with acute expression of diphtheria toxin in the orexin neurons (orexin-tTa;TetO-DTA mice) or mice with gradual loss of the orexin neurons owing to specific expression of a toxic variant of the ataxin 3 protein (orexin–ataxin 3 mice), generally exhibit more severe symptoms than do mice with constitutive loss of orexins or orexin receptors13,26,70,187. Mice lacking both orexin receptors have sleepiness similar to mice lacking the orexin peptides77,188. However, mice lacking only orexin 2 receptor (OX2R) exhibit only mild sleepiness, and mice lacking OX1R are surprisingly normal, suggesting that there are important synergies between OX1R and OX2R signalling25,72,186,188. Cataplexy in mice requires loss of orexins or loss of both orexin receptors71,77,189. Obesity is more striking in mice with loss of the orexin neurons than in orexin-null mice, possibly owing to concomitant loss of co-expressed signalling molecules, such as glutamate, dynorphin and neuronal activity-regulated pentraxin (NARP)70,190. The severity of narcolepsy symptoms, including obesity, can also vary with genetic background of the mouse strain70,190,191.
Dogs with narcolepsy were the first animal models of narcolepsy and provided key insights into the cause of the disorder. Dogs with narcolepsy exhibit severe sleepiness, fragmented sleep, poor rapid eye movement (REM) sleep regulation and cataplexy192–195. Some of the first links of narcolepsy to orexin signalling came with the observations that inherited canine narcolepsy is caused by loss-of-function mutations in the canine OX2R gene196 and that sporadic canine narcolepsy results from the loss of production of the orexin peptides197.
| Disease or model | General description | Duration of wake bouts | Cataplexy | Short latency to REM sleep | Body weight | Refs |
|---|---|---|---|---|---|---|
| Human NT1 | Loss of orexin neurons | ↓↓ | ↑↑ | Yes | ↑ | 198,199 |
| Orex- in-tTA;TetO-DTA mice | Rapid death of orexin neurons with acute expression of DTA upon withdrawal of doxycycline | ↓↓ | ↑↑↑ | n/a | ↑↑ | 13,73 |
| Orexin–ataxin 3 mice | Progressive neurotoxic death of orexin neurons starting at birth | ↓ | ↑ | Yes | ↑ | 26,70,190 |
| Ox−/− mice | No orexin A or orexin B | ↓↓ | ↑↑ | Yes | Small ↑ | 26,69 |
| Ox1r−/−;Ox2r−/− mice | No functional orexin receptors | ↓↓ | ↑ | Yes | n/a | 25,77,200,201 |
| Ox1r−/− mice | No functional OX1R | Small ↓ | None | n/a | No change | 25,202 |
| Ox2r−/− mice | No functional OX2R | ↓ | Rare | n/a | n/a | 72,186 |
| Sporadic canine narcolepsy | Loss of orexin A (and probably of orexin neurons) | ↓ | ↑↑ | Yes | n/a | 197,203 |
| OX2R−/− dogs | Loss of functional OX2R | ↓ | ↑↑ | Yes | n/a | 196,197 |
DTA, diphtheria toxin A; n/a, no published data found; NT1, narcolepsy type 1; OX, prepro-orexin; TetO, tetracycline operator; tTA, tetracycline-controlled transactivator.
Orexin neurons have several other functions in addition to controlling sleep–wake behaviour. For example, through their projections to mesolimbic pathways, orexins promote reward-seeking. Mice that lack orexin neurons or that have been treated with an OX1R antagonist show much weaker conditioned preference for places associated with rewards such as morphine or cocaine56–59. Orexins also increase home-cage locomotor activity, heart rate, brown fat thermogenesis and metabolic rate in rodents47,60–66. Overall, orexins may help to generate a high arousal state in which an animal is motivated, attentive and autonomically primed for action.
Effects of orexin neuron loss
Poor maintenance of wakefulness.
Almost all individuals with narcolepsy feel sleepy during the day and easily transition into NREM sleep67. Most feel rested on waking in the morning or after a nap, indicating that sleep is restorative, but sleepiness returns in just an hour or two, suggesting dysfunction in the systems that maintain wake. When sedentary or encouraged to sleep, people with narcolepsy can fall asleep very rapidly. On the Multiple Sleep Latency Test (MSLT), patients are instructed to try to sleep every 2 hours across the day. On average, across these five 20-minute nap opportunities, people with narcolepsy fall asleep in less than 8 minutes, and often in just 1–2 minutes, whereas people without narcolepsy usually fall asleep in 10–20 minutes68. Similarly, in orexin-null mice, bouts of wakefulness are only half as long as in control mice, owing to frequent and rapid transitions into NREM sleep69–75.
Recent research in animal models indicates that orexins drive long periods of wake via their projections to important wake-promoting brain regions, such as the TMN, LC and basal forebrain76 (FIG. 1). Re-expression of OX2Rs, specifically in the TMN region of mice globally lacking these receptors, completely rescued their ability to produce long wake bouts72. Similarly, re-expression of OX1R in the LC markedly improved the maintenance of wake in mice lacking orexin receptors77, whereas in TH::IRES-Cre mice, photoinhibition of the LC reduced the awakening effect of orexin neuron photostimulation78. Together, these results suggest that orexin signalling through the TMN and LC regions is sufficient to promote sustained periods of wake. However, more work is needed to determine precisely which orexin projections are necessary for normal arousal.
Poor regulation of REM sleep.
Orexin neurons suppress REM sleep, and individuals with narcolepsy exhibit dysregulation of REM sleep that manifests as poor circadian timing of REM sleep, rapid transitions into REM sleep and disruption of REM sleep physiology (for example, REM sleep behaviour disorder or sleep paralysis). Normally, REM sleep occurs only during the typical sleep period, but with loss of orexin signalling, REM sleep can occur at any time of day26,79. In fact, this pattern is central for diagnosing narcolepsy; on the MSLT, people with narcolepsy typically enter REM sleep in two or more of the five daytime naps, whereas healthy individuals rarely enter REM sleep during the day68. Indeed, during the night, REM sleep is usually preceded by at least 60 minutes of NREM sleep, but in NT1, REM sleep often occurs within a few minutes of sleep onset80,81.
Mechanistically, the propensity of individuals with narcolepsy to enter REM sleep during the day may arise from poor circadian control or disinhibition of REM sleep26,82,83. REM sleep exhibits a strong circadian rhythm and is normally suppressed during the active period via circadian signals relayed from the suprachiasmatic nucleus to the dorsomedial nucleus of the hypothalamus (DMH)84. DMH neurons signal to the orexin neurons, and lack of the orexin neurons in mice reduces the amplitude of the circadian REM sleep rhythm by about half26,79. These results suggest that the orexin neurons, along with additional projections from the DMH, help to suppress REM sleep during the active period85.
In addition to alterations of the timing of REM sleep in narcolepsy, the coherence of REM sleep physiology is also disrupted in narcolepsy, with dream-like hallucinations and episodes of muscle paralysis mixing into wakefulness. Just as in people with narcolepsy, orexin-null mice may suddenly transition from active wake into cataplexy for up to a minute. In individuals with narcolepsy, cataplexy is often triggered by laughter and joking, and in mice lacking orexins, such episodes are much more common with exposure to rewarding stimuli such as chocolate and running wheels86,87.
This paralysis most probably arises from a dysfunction of brainstem pathways that produce the typical paralysis of REM sleep (FIG. 1). The sub-laterodorsal nucleus (SLD) is a key region for triggering muscle atonia during REM sleep, and the SLD is normally inhibited during wake by GABAergic neurons of the ventrolateral PAG and adjacent lateral pontine tegmentum (vlPAG–LPT)88–92. The heavy innervation of the vlPAG–LPT by orexin neurons may typically ensure strong suppression of REM sleep during the active period20,93. The vlPAG–LPT also receives inputs from GABAergic neurons of the central nucleus of the amygdala (CeA)93. Signals related to positive emotions normally engage the medial prefrontal cortex, which excites orexin neurons and the CeA; under normal conditions, the inhibitory effects of the CeA on the vlPAG–LPT are offset by excitatory signals from the orexin neurons. However, in narcolepsy, this orexin tone is absent, and the CeA can inhibit the vlPAG–LPT, thus disinhibiting the SLD and other atonia-promoting brain regions, resulting in cataplexy. In support of this model, chemoactivation of GABAergic neurons in the CeA of orexin-null mice increases cataplexy, whereas chemoinhibition or lesioning of the CeA reduces cataplexy93–95. Chemogenetic inhibition of the medial prefrontal cortex in orexin-null mice also reduces cataplexy that would normally be triggered by chocolate86. Orexins may also suppress cataplexy via projections to the DR neurons, which in turn are well positioned to suppress REM sleep via their projections to the amygdala and other brain regions77,96.
Overall, many researchers view the abnormal sleep architecture in narcolepsy as ‘behavioural state instability’, with low thresholds for transition between states and poor coherence within states that allows for frequent transitions between states and strange, intermediate states, such as cataplexy and hypnagogic hallucinations71,75,97,98.
Effects on metabolism and feeding.
In addition to sleepiness and altered REM sleep, people with narcolepsy are prone to gain weight, possibly owing to a lower metabolic rate. Soon after NT1 onset, children can rapidly gain 5–15 kg, and adults with NT1 are often overweight or obese, despite roughly normal caloric intake and activity levels99–104. Feeding diaries do not indicate increased caloric consumption, but in the laboratory, individuals with NT1 tend to snack more even when satiated and report more binge eating105,106. Mice lacking orexin neurons have obesity and a reduced metabolic rate, especially during their inactive phase13,107; however, research on metabolic rate in people with narcolepsy remains inconclusive104,108. Moreover, there is no consistent evidence for glucose intolerance or insulin resistance in individuals with narcolepsy108–113. More detailed metabolic studies and studies of eating and exercise habits in people with NT1, especially around NT1 onset, when weight gain is most pronounced, are required to help define the best recommendations for managing the weight of this population.
Effects on reward behaviours.
In mice and rats, considerable research indicates that loss of orexin signalling reduces drug-seeking behaviour for cocaine, amphetamine, nicotine, opiates and ethanol114–120 (but see REFS121–123). However, whether the same is true in individuals with NT1 is less clear. People with narcolepsy perform normally on a gambling task and use recreational drugs at typical rates106,124,125. Any underactivity of reward pathways in NT1 could potentially manifest as depression, and indeed several studies indicate that depression is twice as prevalent among individuals with NT1 (REFS126–129). Whether this increased rate of depression is a direct consequence of the loss of orexin neurons, or reflective of the many everyday challenges associated with narcolepsy, is unknown (BOX 3).
Box 3 | Is narcolepsy simply due to loss of the orexin neurons?
The loss of orexin signalling seems sufficient to explain the major features of narcolepsy, but some symptoms such as fragmented night-time sleep, rapid eye movement (REM) sleep behaviour disorder and resolution of hypersomnia over time cannot be easily explained by current models.
The loss of the orexin neurons might trigger compensatory responses that are helpful in some ways but harmful in others. For example, two groups have shown substantially increased numbers of histaminergic neurons in the tuberomammillary nucleus of people with narcolepsy type 1 (NT1)204,205. Histamine is a key wake-promoting transmitter, and in contrast to the other monoamine-producing neurons, histamine neurons remain active during cataplexy206. Thus, increased histamine signalling might help to counter a tendency towards hypersomnia and help to maintain consciousness during cataplexy by preventing full transitions into REM sleep. However, the persistence of histamine signalling at night could also contribute to fragmented sleep. Currently, whether histamine signalling is increased in NT1 is controversial; however, if it is, it may be a useful therapeutic target.
In addition, the neuropathology of NT1 might involve more than just the hypothalamus. Volumetric and white-matter neuroimaging techniques have suggested that grey-matter volume in regions such as in the hypothalamus and inferior temporal and right prefrontal regions may be decreased in individuals with narcolepsy207,208. Other studies have described reduced grey-matter concentration in the cortex and thalamus in NT1 (REF.209). However, imaging results are inconsistent, possibly owing to differences in technique and patient characteristics210. Still, a broader search into additional brain changes would be helpful, as nearly all neuropathology research in the narcolepsy field has focused simply on the orexin neurons and a few other cell types in the hypothalamus.
Evidence for an autoimmune mechanism
Narcolepsy is caused by the selective destruction of the orexin-producing neurons. What kills the orexin-producing neurons remains a major mystery, but several lines of evidence suggest that NT1 is an autoimmune disease mediated by T cells.
T cells can be divided into two categories: CD4+ helper T cells secrete cytokines to regulate or assist in the active immune response, and CD8+ killer T cells use cytotoxic granules to lyse their target cells. The responses of both types of T cell are triggered through T cell receptors (TCRs) that recognize small, processed peptides presented to them by major histocompatibility complex (MHC) molecules on antigen-presenting cells; peptide fragments bound to MHC molecules are known as MHC–peptide complexes. CD4+ T cells recognize antigens bound to MHC class II molecules present on the surface of antigen-presenting cells, including astrocytes and other glial cells130,131, and CD8+ T cells respond to antigens presented by MHC class I molecules, which are expressed on all nucleated cells but very rarely by neurons132–134. A T cell is initially considered ‘naive’ before it encounters the antigen that binds its specific TCR. Once a T cell encounters its antigen alongside the appropriate co-stimulatory signals, it clonally expands to control the pathogen. Once the pathogen is cleared, the T cell numbers contract, and the remaining pathogen-specific memory T cells can respond more quickly and strongly to the same pathogen in the future.
Narcolepsy after vaccination with Pandemrix.
The most direct evidence that NT1 can be caused by an autoimmune process occurred with the H1N1 influenza pandemic in the winter of 2009–2010. Clinicians noticed a surge in individuals developing NT1 after vaccination with Pandemrix, a brand of flu vaccine mainly used in northern Europe. Pandemrix inoculation was associated with an 8–12-fold increase in new cases of NT1 in children and adolescents and a 3–5-fold increase in adults135,136. Importantly, all these affected individuals carried the class II human leukocyte antigen (HLA) allele DQB1*06:02 and developed NT1 a few weeks to months after vaccination. Why NT1 was triggered by Pandemrix but not by other flu vaccines remains unclear, but altered viral nuclear proteins in Pandemrix may have contributed137. This tragic event suggests that NT1 can arise from an inflammatory trigger in a genetically susceptible population, especially during childhood and adolescence. One group reported a threefold increase in new cases of NT1 in the months after the H1N1 pandemic in China138; in this population, NT1 may have been triggered by H1N1 flu infection itself, as flu vaccination rates were very low in China.
Some researchers now hypothesize that NT1 arises from a process of molecular mimicry (FIG. 3). In addition to the increase in NT1 diagnoses after inoculation with Pandemrix, many spontaneous cases of NT1 are preceded by infection with streptococcus or influenza138,139, and NT1 commonly first develops in the late spring and early summer138, suggesting that it may follow immune responses triggered by winter infections. CD4+ T cells responding to streptococcus or influenza may cross-react with orexin peptides presented by MHC class II molecules140.
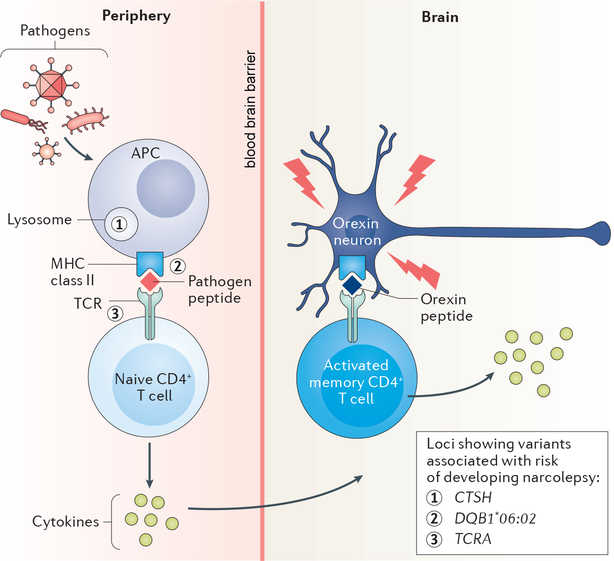
Fig. 3 |. A model for T cell-mediated killing of the orexin neurons in narcolepsy.
In a possible model of T cell-mediated killing of orexin neurons, an antigen-presenting cell (APC) first takes up a pathogen and presents fragments of pathogen proteins to a naive CD4+ T cell using a major histocompatibility complex (MHC) class II molecule, perhaps DQB1*0602. The naive CD4+ T cell may secrete cytokines (circles) to help clear the infection. Memory CD4+ T cells are formed from the initial infection. Fever may promote the migration of pathogen-specific CD4+ T cells across the blood–brain barrier (BBB). The activated memory CD4+ T cell cross-recognizes fragments of prepro-orexin with a similar epitope as the pathogen peptide and secretes cytokines that promote destruction of the orexin neurons. Genes for which certain alleles are known to increase the risk of developing narcolepsy related to this model of T cell-mediated killing of orexin neurons are illustrated at their respective sites of action. TCR, T cell receptor.
MHC class II alleles and narcolepsy susceptibility.
HLA alleles strongly influence the development of narcolepsy. More than 90% of individuals with NT1 bear the HLA class II allele DQB1*06:02 (REFS141–143), and crystalline structure modelling indicated that a fragment of the prepro-orexin protein fits well in the binding groove of DQB1*06:02 (REF.144). The DQB1*06:02 allele increases the risk of developing NT1 200-fold143 — the strongest known association of an HLA with any disease — and NT1 rarely develops in people lacking this allele. People who are homozygous for this allele have twice the risk of developing NT1 as those who are heterozygous145,146. The HLA allele DQA1*01:02 is in strong linkage disequilibrium with DQB1*06:02 and carries similar risk143,147. DPB1*05:01 also increases the risk of NT1, although the effect is smaller148. By contrast, some other class II alleles, including DPB1*04:02, DQB1*06:03 and DQB1*06:09, are protective, as indicated by genome-wide association studies149–151. Although class II alleles most strongly influence the risk of narcolepsy, two studies have shown small, independent effects of class I alleles149,150.
Additional genetic factors.
Genome-wide association studies have also suggested that NT1 is associated with polymorphisms in additional genes that influence the response of CD4+ T cells to antigens. Several studies have identified a single nucleotide polymorphism in the gene encoding the TCR α-chain that roughly doubles the risk of NT1 (REFS152–154), suggesting that NT1 might arise from an interaction of DQB1*06:02 and specific TCRs. Further, according to preliminary work, specific, rare single nucleotide polymorphisms within the TCR genes may greatly increase the reactivity of T cells to fragments of the orexin neuropeptides155. NT1 risk is also associated with variants of the gene coding for cathepsin H, an enzyme involved in digesting proteins into smaller peptides that can be presented by MHC class II molecules154. Variants of OX40L, which is involved in T cell differentiation, have also been implicated in NT1 risk154,156; how polymorphisms in OX40L may contribute to NT1 is unknown, but imbalances in T helper cell subsets are commonly observed in autoimmune disorders157.
Targets of the autoimmune response.
The actual target of this autoimmune process is not clear, but the orexin peptides seem to be a likely target. The orexin-producing neurons are the only cells known to be missing in NT1, and they do not produce any other unique proteins, as demonstrated by histology and gene expression arrays158–162. Orexins are produced only in the hypothalamus6, although unidentified peptides antigenically similar to orexins can be found in the myenteric plexus163. In theory, an autoimmune process might kill cells outside the brain, but there is no clinical evidence yet for cell loss in the gut or elsewhere in individuals with narcolepsy. Most importantly, the loss of the orexin neurons in the hypothalamus alone is an adequate explanation for the phenotype of the disorder, as selective killing of these cells in mice recapitulates the major features of NT1 (REFS13,70).
Other proposed autoimmune targets include the OX2R and the intracellular protein Tribbles homologue 2 (TRIB2)42,162–164, but OX2R and TRIB2 are expressed widely in the brain, and there is no evidence for loss of cells other than those that make orexins in NT1. Furthermore, whether orexin neurons even express OX2R is a matter of debate40–42.
Orexin neurons may be killed by T cells.
In addition to the genetic evidence above implicating the MHC class II DQB1*06:02 allele141–143 and a specific polymorphism in the locus encoding the TCR α-chain, several other lines of evidence suggest that a T cell-mediated immune mechanism destroys the orexin neurons in NT1 and that CD4+ cells are crucial. Notably, CD4+ cells probably do not directly destroy the orexin neurons, but they could release cytokines that could spur an attack on the orexin neurons by CD8+ T cells, macrophages and natural killer cells. Using a transgenic mouse model in which orexin neurons expressed haemagglutinin and T cells possessed a TCR specific for haemagglutinin, one group showed that CD8+ T cells are capable of destroying orexin neurons165. However, a primary CD8+ cell attack on the orexin neurons is not likely to occur in NT1, as MHC class I molecules, which are involved in the activation of CD8+ T cells, are rarely expressed by neurons in humans, except very early in development and after exposure to interferon-γ132–134.
The genetic data implicate CD4+ T cells in the pathology of narcolepsy, yet direct evidence is just emerging. One recent study used a sensitive method to detect rare T cell populations166. The researchers polyclonally expanded rare, reactive T cell populations and detected CD4+ T cells reacting to epitopes along the entire prepro-orexin peptide. T cell populations reactive to TRIB2 were present in just as many controls as individuals with NT1, but those from NT1 subjects proliferated more. In some people with NT1, CD8+ T cells reacting to prepro-orexin were also detected, suggesting that NT1 may arise from an interaction of CD4+ and CD8+ T cells. This new, sensitive method is considered an important advance, as previous studies had been unable to identify autoreactive T cells, or found them in only a fraction of NT1 subjects166–168. However, it still remains unclear whether these CD4+ T cells reactive to prepro-orexin are the primary cause of NT1, or whether they contribute once another process starts to damage the orexin neurons.
Most research on T cells in NT1 has focused on CD4+ or CD8+ T cells, but most autoimmune disorders are characterized by deficiencies in immune system regulation by CD4+ regulatory T cells (Treg cells)157. One report suggested that Treg cells circulating in peripheral blood were more numerous and highly activated in individuals with NT1 than in control individuals169. However, the activation of Treg cells correlated with systemic activation of all T cells, suggesting that this activation was nonspecific. Furthermore, the antigen specificity of Treg cells was not examined169; thus, whether these cells could control orexin-specific autoimmune CD4+ T cells and CD8+ T cells remains to be determined.
Might antibodies contribute to the death of the orexin neurons?
A T cell response seems to be the primary mechanism in NT1, but this may also generate a humoral response, the possible effects of which remain highly debated. In contrast to other autoimmune disorders such as multiple sclerosis, the CSF of patients with NT1 does not show oligoclonal bands or an increase in total proteins compared with healthy controls, and researchers have found no consistent pattern of antibodies targeting the orexin peptides. In a study of 20 DQB1*06:02-positive individuals with narcolepsy who had been inoculated with the Pandemrix vaccine, 17 had antibodies that bound OX2R164. This report contradicted an earlier study in which only 5% of patients with NT1 had OX2R-targeting antibodies, as compared with 3% of healthy individuals170. The inconsistency of these results may be attributable to the differences in time from narcolepsy onset when the sera were collected, as OX2R antibodies were more common 500 days after disease onset than at a much later date170. Further complicating matters, another group found no increase in OX2R-targeting antibodies in Pandemrix-inoculated individuals with NT1, leaving the existence of these antibodies contentious42,171. Nevertheless, a separate study noted that whereas overall serum levels of immunoglobulin G (IgG) did not differ from controls, individuals with NT1 had higher levels of IgG complexed with orexin A172, raising the possibility of a specific antibody response to orexin A in NT1 as opposed to a nonspecific increase in systemic IgG. The inconsistencies of these clinical studies highlight the need for careful tracking of time from NT1 onset as well as consideration of HLA genotype when measuring the antibody response.
In addition, individuals with NT1 have also been reported to possess higher levels of antibodies to TRIB2, a protein expressed in orexin neurons and many other cell types162. Perhaps predictably, these autoantibodies were observed at their highest levels within the first 3 years after NT1 onset and remained slightly elevated compared with controls even 30 years after diagnosis of NT1 (REF.162). One group reported that TRIB2-targeting antibodies from patients with NT1 caused orexin neuron loss in mice, but these mice displayed nonspecific immobility in their rest period rather than true cataplexy, and the orexin neuron loss was not replicated in a later study173,174. Another study found that antisera from some NT1 individuals bound to non-orexin neurons in the hypothalamus, cortex or striatum, but there was no binding to orexin neurons, suggesting that these antibodies may arise only after orexin neurons are injured by another mechanism175. Currently, whether antibodies contribute to the death of the orexin neurons, or are simply a non-pathogenic consequence of the cell loss, is unknown.
Future directions
In the past several years, much has been learned about the neuropathology, neural circuitry and neuroimmunology of narcolepsy; however, much remains unknown.
One of the largest mysteries is the nature of NT2. Besides a lack of cataplexy, the symptoms of NT2 are similar to those of NT1, yet almost nothing is known about its neuropathology. In NT2, CSF orexin levels are usually normal176; thus, it may be caused by a modest loss of orexin neurons or a completely different process177,178.
For patients with NT1, identifying the autoreactive T cells and the antigens that activate them will be required for the development of treatments. The selection of immunomodulatory therapies will also hinge on determining whether NT1 is a monophasic, self-limited disease or a chronic disorder that progresses over months to years. Narcolepsy is usually diagnosed years after disease onset, and for those patients, it may be too late to rescue the orexin neurons. Thus, it will be crucial to develop well-targeted therapies that can normalize activity in the key neural pathways underlying sleepiness, fragmented sleep and cataplexy. Researchers recently mapped the crystal structure of the orexin receptors179, which facilitates the design of small-molecule agonists. Early preclinical research is quite encouraging, with intraperitoneal administration of one OX2R agonist increasing wake, reducing cataplexy and reducing weight in orexin-null mice36. Furthermore, clinical trials are now underway with orexin agonists and unique medications that enhance signalling by histamine and other monoamine systems180–182. Addressing the questions above and designing better treatments will be a challenge, but these goals are now achievable and should deliver great scientific and clinical benefits.
Acknowledgements
The authors acknowledge support from the US National Institutes of Health grants P01 HL095491, R21 NS099787 and R01 NS106032.
Glossary
- Hypnopompic and hypnagogic hallucinations
Vivid, sometimes frightening, dream-like hallucinations that occur when falling asleep (hypnopompic) or immediately after waking (hypnagogic)
- Sleep paralysis
An inability to move when falling asleep or immediately after waking
- Cataplexy
Muscle weakness or full paralysis triggered by strong, generally positive, emotions
- REM sleep behaviour disorder
A disorder characterized by impaired motor inhibition during rapid eye movement sleep, resulting in enactment of dreams
- Major histocompatibility complex
(MHC). A set of immune molecules that bind antigens derived from pathogens and display them on the surface of antigen-presenting cells to promote acquired immune responses
- Human leukocyte antigen (HLA) allele
An allele encoding a human major histocompatibility complex molecule
- Molecular mimicry
A mechanism of autoimmunity in which a foreign antigen is structurally similar to ‘self’-peptides, such that immune cells targeting a pathogen accidentally target healthy tissue
- Linkage disequilibrium
When the observed frequency of two alleles at two loci occurring together is more frequent than would occur by chance
- Myenteric plexus
The network of sensory and motor neurons that control gut secretions and motility
- Regulatory T cells
(Treg cells). T cells that maintain tolerance to self-antigens by downregulating the activity of effector T cells using anti-inflammatory cytokines and cell-to-cell inhibition
- Hypersomnia
An abnormally high total amount of sleep over 24 hours
- Status cataplecticus
A prolonged period of moderate to severe weakness with low muscle tone, usually without emotional triggers
Footnotes
Competing interests
The authors declare no competing interests.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Silber MH, Krahn LE, Olson EJ & Pankratz VS The epidemiology of narcolepsy in Olmsted County, Minnesota: a population-based study. Sleep 25, 197–202 (2002). [DOI] [PubMed] [Google Scholar]
- 2.Shin YK et al. Prevalence of narcolepsy-cataplexy in Korean adolescents. Acta Neurol. Scand 117, 273–278 (2008). [DOI] [PubMed] [Google Scholar]
- 3.Longstreth WT Jr. et al. Prevalence of narcolepsy in King County, WA, USA. Sleep Med. 10, 422–426 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knudsen S, Gammeltoft S & Jennum PJ Rapid eye movement sleep behaviour disorder in patients with narcolepsy is associated with hypocretin-1 deficiency. Brain 133, 568–579 (2010). [DOI] [PubMed] [Google Scholar]
- 5.de Lecea L et al. The hypocretins: hypothalamus-specific peptides with neuroexcitatory activity. Proc. Natl Acad. Sci. USA 95, 322–327 (1998).This paper is one of the first descriptions of the orexin neuropeptides (naming them hypocretins).
- 6.Sakurai T et al. Orexins and orexin receptors: a family of hypothalamic neuropeptides and G protein-coupled receptors that regulate feeding behavior. Cell 92, 573–585 (1998).This article is one of the first to describe the orexin neuropeptides.
- 7.Nishino S, Ripley B, Overeem S, Lammers GJ & Mignot E Hypocretin (orexin) deficiency in human narcolepsy. Lancet 355, 39–40 (2000). [DOI] [PubMed] [Google Scholar]
- 8.Peyron C et al. A mutation in a case of early onset narcolepsy and a generalized absence of hypocretin peptides in human narcoleptic brains. Nat. Med 6, 991–997 (2000).This paper highlights the discovery of a lack of orexin in the brains of people with narcolepsy.
- 9.Thannickal TC et al. Reduced number of hypocretin neurons in human narcolepsy. Neuron 27, 469–474 (2000).This study also shows a lack of orexin in the brains of people with narcolepsy.
- 10.Crocker A et al. Concomitant loss of dynorphin, NARP, and orexin in narcolepsy. Neurology 65, 1184–1188 (2005).This paper demonstrates that orexin neurons co-express dynorphin and NARP and that narcolepsy is due to a loss of the orexin neurons, not just a reduction in orexin expression.
- 11.American Academy of Sleep Medicine. International Classification of Sleep Disorders 3rd edn (AASM, 2014). [Google Scholar]
- 12.Thannickal TC, Nienhuis R & Siegel JM Localized loss of hypocretin (orexin) cells in narcolepsy without cataplexy. Sleep 32, 993–998 (2009).This paper shows that NT2 may be caused by partial loss of the orexin neurons.
- 13.Tabuchi S et al. Conditional ablation of orexin/hypocretin neurons: a new mouse model for the study of narcolepsy and orexin system function. J. Neurosci. 34, 6495–6509 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kanbayashi T et al. The pathophysiologic basis of secondary narcolepsy and hypersomnia. Curr. Neurol. Neurosci. Rep 11, 235–241 (2011). [DOI] [PubMed] [Google Scholar]
- 15.Hor H et al. A missense mutation in myelin oligodendrocyte glycoprotein as a cause of familial narcolepsy with cataplexy. Am. J. Hum. Genet 89, 474–479 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andlauer O et al. Predictors of hypocretin (orexin) deficiency in narcolepsy without cataplexy. Sleep 35, 1247–1255 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luca G et al. Clinical, polysomnographic and genome-wide association analyses of narcolepsy with cataplexy: a European Narcolepsy Network study. J. Sleep Res 22, 482–495 (2013). [DOI] [PubMed] [Google Scholar]
- 18.Lopez R et al. Temporal changes in the cerebrospinal fluid level of hypocretin-1 and histamine in narcolepsy. Sleep 40, zsw010 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pizza F et al. Primary progressive narcolepsy type 1: the other side of the coin. Neurology 83, 2189–2190 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peyron C et al. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J. Neurosci 18, 9996–10015 (1998).This study thoroughly describes the projections of the orexin neurons.
- 21.Yoshida K, McCormack S, Espana RA, Crocker A & Scammell TE Afferents to the orexin neurons of the rat brain. J. Comp. Neurol 494, 845–861 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gonzalez JA, Iordanidou P, Strom M, Adamantidis A & Burdakov D Awake dynamics and brain-wide direct inputs of hypothalamic MCH and orexin networks. Nat. Commun. 7, 11395 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van den Pol AN Hypothalamic hypocretin (orexin): robust innervation of the spinal cord. J. Neurosci 19, 3171–3182 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sakurai T et al. Input of orexin/hypocretin neurons revealed by a genetically encoded tracer in mice. Neuron 46, 297–308 (2005). [DOI] [PubMed] [Google Scholar]
- 25.Mieda M et al. Differential roles of orexin receptor-1 and −2 in the regulation of non-REM and REM sleep. J. Neurosci 31, 6518–6526 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kantor S et al. Orexin neurons are necessary for the circadian control of REM sleep. Sleep 32, 1127–1134 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee MG, Hassani OK & Jones BE Discharge of identified orexin/hypocretin neurons across the sleep-waking cycle. J. Neurosci 25, 6716–6720 (2005).This paper describes the firing pattern of orexin neurons across different sleep–wake states.
- 28.Mileykovskiy BY, Kiyashchenko LI & Siegel JM Behavioral correlates of activity in identified hypocretin/orexin neurons. Neuron 46, 787–798 (2005).This study highlights increased activity in the orexin neurons during exploratory behaviour and wake.
- 29.Estabrooke IV et al. Fos expression in orexin neurons varies with behavioral state. J. Neurosci 21, 1656–1662 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.España RA, Valentino RJ & Berridge CW Fos immunoreactivity in hypocretin-synthesizing and hypocretin-1 receptor-expressing neurons: effects of diurnal and nocturnal spontaneous waking, stress and hypocretin-1 administration. Neuroscience 121, 201–217 (2003). [DOI] [PubMed] [Google Scholar]
- 31.Adamantidis AR, Zhang F, Aravanis AM, Deisseroth K & de Lecea L Neural substrates of awakening probed with optogenetic control of hypocretin neurons. Nature 450, 420–424 (2007).This study is the first demonstration that photostimulation of the orexin neurons promotes waking from sleep.
- 32.Carter ME et al. Tuning arousal with optogenetic modulation of locus coeruleus neurons. Nat. Neurosci 13, 1526–1533 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsunematsu T et al. Long-lasting silencing of orexin/hypocretin neurons using archaerhodopsin induces slow-wave sleep in mice. Behav. Brain Res 255, 64–74 (2013). [DOI] [PubMed] [Google Scholar]
- 34.Sasaki K et al. Pharmacogenetic modulation of orexin neurons alters sleep/wakefulness states in mice. PLOS ONE 6, e20360 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mieda M et al. Orexin peptides prevent cataplexy and improve wakefulness in an orexin neuron-ablated model of narcolepsy in mice. Proc. Natl Acad. Sci. USA 101, 4649–4654 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Irukayama-Tomobe Y et al. Nonpeptide orexin type-2 receptor agonist ameliorates narcolepsy-cataplexy symptoms in mouse models. Proc. Natl Acad. Sci. USA 114, 5731–5736 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suntsova N et al. The median preoptic nucleus reciprocally modulates activity of arousal-related and sleep-related neurons in the perifornical lateral hypothalamus. J. Neurosci 27, 1616–1630 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saper CB, Scammell TE & Lu J Hypothalamic regulation of sleep and circadian rhythms. Nature 437, 1257–1263 (2005). [DOI] [PubMed] [Google Scholar]
- 39.Uschakov A, Gong H, McGinty D & Szymusiak R Efferent projections from the median preoptic nucleus to sleep- and arousal-regulatory nuclei in the rat brain. Neuroscience 150, 104–120 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li Y, Gao XB, Sakurai T & van den Pol AN Hypocretin/orexin excites hypocretin neurons via a local glutamate neuron — a potential mechanism for orchestrating the hypothalamic arousal system. Neuron 36, 1169–1181 (2002). [DOI] [PubMed] [Google Scholar]
- 41.Yamanaka A, Tabuchi S, Tsunematsu T, Fukazawa Y & Tominaga M Orexin directly excites orexin neurons through orexin 2 receptor. J. Neurosci 30, 12642–12652 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vassalli A, Li S & Tafti M Comment on “Antibodies to influenza nucleoprotein cross-react with human hypocretin receptor 2”. Sci. Transl Med 7, 314le2 (2015). [DOI] [PubMed] [Google Scholar]
- 43.Schone C, Apergis-Schoute J, Sakurai T, Adamantidis A & Burdakov D Coreleased orexin and glutamate evoke nonredundant spike outputs and computations in histamine neurons. Cell Rep 7, 697–704 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Herring WJ et al. Orexin receptor antagonism for treatment of insomnia: a randomized clinical trial of suvorexant. Neurology 79, 2265–2274 (2012). [DOI] [PubMed] [Google Scholar]
- 45.Svetnik V et al. Insight into reduction of wakefulness by suvorexant in patients with insomnia: analysis of wake bouts. Sleep 41, zsx178 (2018). [DOI] [PubMed] [Google Scholar]
- 46.Schone C & Burdakov D Glutamate and GABA as rapid effectors of hypothalamic “peptidergic” neurons. Front. Behav. Neurosci 6, 81 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kosse C, Schone C, Bracey E & Burdakov D Orexin-driven GAD65 network of the lateral hypothalamus sets physical activity in mice. Proc. Natl Acad. Sci. USA 114, 4525–4530 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chang MC et al. Narp regulates homeostatic scaling of excitatory synapses on parvalbumin-expressing interneurons. Nat. Neurosci 13, 1090–1097 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reti IM, Reddy R, Worley PF & Baraban JM Selective expression of Narp, a secreted neuronal pentraxin, in orexin neurons. J. Neurochem 82, 1561–1565 (2002). [DOI] [PubMed] [Google Scholar]
- 50.Blouin AM et al. Narp immunostaining of human hypocretin (orexin) neurons: loss in narcolepsy. Neurology 65, 1189–1192 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chou TC et al. Orexin (hypocretin) neurons contain dynorphin. J. Neurosci 21, RC168 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Muschamp JW et al. Hypocretin (orexin) facilitates reward by attenuating the antireward effects of its cotransmitter dynorphin in ventral tegmental area. Proc. Natl Acad. Sci. USA 111, E1648–E1655 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ferrari LL et al. Dynorphin inhibits basal forebrain cholinergic neurons by pre- and postsynaptic mechanisms. J. Physiol 594, 1069–1085 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ferrari LL et al. Regulation of lateral hypothalamic orexin activity by local GABAergic neurons. J. Neurosci 38, 1588–1599 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baimel C, Lau BK, Qiao M & Borgland SL Projection-target-defined effects of orexin and dynorphin on VTA dopamine neurons. Cell Rep. 18, 1346–1355 (2017).This paper shows that the effects of orexin and dynorphin vary across VTA neurons that innervate different targets.
- 56.Narita M et al. Direct involvement of orexinergic systems in the activation of the mesolimbic dopamine pathway and related behaviors induced by morphine. J. Neurosci 26, 398–405 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aston-Jones G, Smith RJ, Moorman DE & Richardson KA Role of lateral hypothalamic orexin neurons in reward processing and addiction. Neuropharmacology 56 (Suppl. 1), 112–121 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harris GC & Aston-Jones G Arousal and reward: a dichotomy in orexin function. Trends Neurosci. 29, 571–577 (2006). [DOI] [PubMed] [Google Scholar]
- 59.Smith RJ, Tahsili-Fahadan P & Aston-Jones G Orexin/hypocretin is necessary for context-driven cocaine-seeking. Neuropharmacology 58, 179–184 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beig MI, Dampney BW & Carrive P Both Ox1r and Ox2r orexin receptors contribute to the cardiovascular and locomotor components of the novelty stress response in the rat. Neuropharmacology 89, 146–156 (2015). [DOI] [PubMed] [Google Scholar]
- 61.Ciriello J & de Oliveira CV Cardiac effects of hypocretin-1 in nucleus ambiguus. Am. J. Physiol. Regul. Integr. Comp. Physiol 284, R1611–R1620 (2003). [DOI] [PubMed] [Google Scholar]
- 62.Ciriello J, Li Z & de Oliveira CV Cardioacceleratory responses to hypocretin-1 injections into rostral ventromedial medulla. Brain Res. 991, 84–95 (2003). [DOI] [PubMed] [Google Scholar]
- 63.Shirasaka T, Nakazato M, Matsukura S, Takasaki M & Kannan H Sympathetic and cardiovascular actions of orexins in conscious rats. Am. J. Physiol 277, R1780–R1785 (1999). [DOI] [PubMed] [Google Scholar]
- 64.Li A, Hindmarch CC, Nattie EE & Paton JF Antagonism of orexin receptors significantly lowers blood pressure in spontaneously hypertensive rats. J. Physiol 591, 4237–4248 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mohammed M, Ootsuka Y, Yanagisawa M & Blessing W Reduced brown adipose tissue thermogenesis during environmental interactions in transgenic rats with ataxin-3-mediated ablation of hypothalamic orexin neurons. Am. J. Physiol. Regul. Integr. Comp. Physiol 307, R978–R989 (2014). [DOI] [PubMed] [Google Scholar]
- 66.Lubkin M & Stricker-Krongrad A Independent feeding and metabolic actions of orexins in mice. Biochem. Biophys. Res. Commun 253, 241–245 (1998). [DOI] [PubMed] [Google Scholar]
- 67.Hansen MH, Kornum BR & Jennum P Sleep-wake stability in narcolepsy patients with normal, low and unmeasurable hypocretin levels. Sleep Med. 34, 1–6 (2017). [DOI] [PubMed] [Google Scholar]
- 68.Littner MR et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 28, 113–121 (2005). [DOI] [PubMed] [Google Scholar]
- 69.Chemelli RM et al. Narcolepsy in orexin knockout mice: molecular genetics of sleep regulation. Cell 98, 437–451 (1999).This paper provides the first evidence that loss of orexin signalling in mice produces sleepiness and cataplexy.
- 70.Hara J et al. Genetic ablation of orexin neurons in mice results in narcolepsy, hypophagia, and obesity. Neuron 30, 345–354 (2001). [DOI] [PubMed] [Google Scholar]
- 71.Mochizuki T et al. Behavioral state instability in orexin knock-out mice. J. Neurosci 24, 6291–6300 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mochizuki T et al. Orexin receptor 2 expression in the posterior hypothalamus rescues sleepiness in narcoleptic mice. Proc. Natl Acad. Sci. USA 108, 4471–4476 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Branch AF et al. Progressive loss of the orexin neurons reveals dual effects on wakefulness. Sleep 39, 369–377 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vassalli A & Franken P Hypocretin (orexin) is critical in sustaining theta/gamma-rich waking behaviors that drive sleep need. Proc. Natl Acad. Sci. USA 114, E5464–E5473 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Diniz Behn CG, Klerman EB, Mochizuki T, Lin SC & Scammell TE Abnormal sleep/wake dynamics in orexin knockout mice. Sleep 33, 297–306 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.España RA, Baldo BA, Kelley AE & Berridge CW Wake-promoting and sleep-suppressing actions of hypocretin (orexin): basal forebrain sites of action. Neuroscience 106, 699–715 (2001). [DOI] [PubMed] [Google Scholar]
- 77.Hasegawa E, Yanagisawa M, Sakurai T & Mieda M Orexin neurons suppress narcolepsy via 2 distinct efferent pathways. J. Clin. Invest 124, 604–616 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Carter ME et al. Mechanism for hypocretin-mediated sleep-to-wake transitions. Proc. Natl Acad. Sci. USA 109, E2635–E2644 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Roman A, Meftah S, Arthaud S, Luppi PH & Peyron C The inappropriate occurrence of rapid eye movement sleep in narcolepsy is not due to a defect in homeostatic regulation of rapid eye movement sleep. Sleep 41, zsy046 (2018). [DOI] [PubMed] [Google Scholar]
- 80.Andlauer O et al. Nocturnal rapid eye movement sleep latency for identifying patients with narcolepsy/hypocretin deficiency. JAMA Neurol. 70, 891–902 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Reiter J, Katz E, Scammell TE & Maski K Usefulness of a nocturnal SOREMP for diagnosing narcolepsy with cataplexy in a pediatric population. Sleep 38, 859–865 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tafti M, Villemin E, Carlander B, Besset A & Billiard M Sleep onset rapid-eye-movement episodes in narcolepsy: REM sleep pressure or nonREM–REM sleep dysregulation? J. Sleep Res. 1, 245–250 (1992). [DOI] [PubMed] [Google Scholar]
- 83.Dantz B, Edgar DM & Dement WC Circadian rhythms in narcolepsy: studies on a 90 minute day. Electroencephalogr. Clin. Neurophysiol. 90, 24–35 (1994). [DOI] [PubMed] [Google Scholar]
- 84.Chou TC et al. Critical role of dorsomedial hypothalamic nucleus in a wide range of behavioral circadian rhythms. J. Neurosci 23, 10691–10702 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen KS et al. A hypothalamic switch for REM and non-REM sleep. Neuron 97, 1168–1176 (2018). [DOI] [PubMed] [Google Scholar]
- 86.Oishi Y et al. Role of the medial prefrontal cortex in cataplexy. J. Neurosci 33, 9743–9751 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.España RA, McCormack SL, Mochizuki T & Scammell TE Running promotes wakefulness and increases cataplexy in orexin knockout mice. Sleep 30, 1417–1425 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lu J, Sherman D, Devor M & Saper CB A putative flip-flop switch for control of REM sleep. Nature 441, 589–594 (2006). [DOI] [PubMed] [Google Scholar]
- 89.Kaur S et al. Hypocretin-2 saporin lesions of the ventrolateral periaquaductal gray (vlPAG) increase REM sleep in hypocretin knockout mice. PLOS ONE 4, e6346 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Luppi PH et al. Paradoxical (REM) sleep genesis: the switch from an aminergic-cholinergic to a GABAergic-glutamatergic hypothesis. J. Physiol. Paris 100, 271–283 (2006). [DOI] [PubMed] [Google Scholar]
- 91.Sapin E et al. Localization of the brainstem GABAergic neurons controlling paradoxical (REM) sleep. PLOS ONE 4, e4272 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Luppi PH et al. Brainstem mechanisms of paradoxical (REM) sleep generation. Pflugers Arch. 463, 43–52 (2012). [DOI] [PubMed] [Google Scholar]
- 93.Burgess CR, Oishi Y, Mochizuki T, Peever JH & Scammell TE Amygdala lesions reduce cataplexy in orexin knock-out mice. J. Neurosci 33, 9734–9742 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mahoney CE, Agostinelli LJ, Brooks JN, Lowell BB & Scammell TE GABAergic neurons of the central amygdala promote cataplexy. J. Neurosci 37, 3995–4006 (2017).This paper demonstrates that the central amygdala is necessary for emotion-triggered cataplexy.
- 95.Snow MB et al. GABA cells in the central nucleus of the amygdala promote cataplexy. J. Neurosci 37, 4007–4022 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hasegawa E et al. Serotonin neurons in the dorsal raphe mediate the anticataplectic action of orexin neurons by reducing amygdala activity. Proc. Natl Acad. Sci. USA 114, E3526–E3535 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Broughton R et al. Excessive daytime sleepiness and the pathophysiology of narcolepsy-cataplexy: a laboratory perspective. Sleep 9, 205–215 (1986). [DOI] [PubMed] [Google Scholar]
- 98.Schoch SF et al. Dysregulation of sleep behavioral states in narcolepsy. Sleep 40, zsx170 (2017). [DOI] [PubMed] [Google Scholar]
- 99.Ponziani V et al. Growing up with type 1 narcolepsy: its anthropometric and endocrine features. J. Clin. Sleep Med 12, 1649–1657 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lammers GJ et al. Spontaneous food choice in narcolepsy. Sleep 19, 75–76 (1996). [DOI] [PubMed] [Google Scholar]
- 101.Schuld A, Hebebrand J, Geller F & Pollmacher T Increased body-mass index in patients with narcolepsy. Lancet 355, 1274–1275 (2000). [DOI] [PubMed] [Google Scholar]
- 102.Nishino S et al. Low cerebrospinal fluid hypocretin (orexin) and altered energy homeostasis in human narcolepsy. Ann. Neurol 50, 381–388 (2001). [DOI] [PubMed] [Google Scholar]
- 103.Poli F et al. High prevalence of precocious puberty and obesity in childhood narcolepsy with cataplexy. Sleep 36, 175–181 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang Z et al. Body weight and basal metabolic rate in childhood narcolepsy: a longitudinal study. Sleep Med. 25, 139–144 (2016). [DOI] [PubMed] [Google Scholar]
- 105.van Holst RJ et al. Aberrant food choices after satiation in human orexin-deficient narcolepsy type 1. Sleep 39, 1951–1959 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dimitrova A et al. Reward-seeking behavior in human narcolepsy. J. Clin. Sleep Med 7, 293–300 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang S, Zeitzer JM, Sakurai T, Nishino S & Mignot E Sleep/wake fragmentation disrupts metabolism in a mouse model of narcolepsy. J. Physiol 581, 649–663 (2007).This paper demonstrates that resting metabolic rate is reduced in mice lacking orexin neurons.
- 108.Fronczek R et al. Increased heart rate variability but normal resting metabolic rate in hypocretin/orexin-deficient human narcolepsy. J. Clin. Sleep Med 4, 248–254 (2008). [PMC free article] [PubMed] [Google Scholar]
- 109.Dahmen N, Tonn P, Messroghli L, Ghezel-Ahmadi D & Engel A Basal metabolic rate in narcoleptic patients. Sleep 32, 962–964 (2009). [PMC free article] [PubMed] [Google Scholar]
- 110.Chabas D et al. Eating disorder and metabolism in narcoleptic patients. Sleep 30, 1267–1273 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Donjacour CE et al. Glucose and fat metabolism in narcolepsy and the effect of sodium oxybate: a hyperinsulinemic-euglycemic clamp study. Sleep 37, 795–801 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Maurovich-Horvat E et al. Hypothalamo-pituitary-adrenal axis, glucose metabolism and TNF-α in narcolepsy. J. Sleep Res. 23, 425–431 (2014). [DOI] [PubMed] [Google Scholar]
- 113.Poli F et al. Body mass index-independent metabolic alterations in narcolepsy with cataplexy. Sleep 32, 1491–1497 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hutcheson DM et al. Orexin-1 receptor antagonist SB-334867 reduces the acquisition and expression of cocaine-conditioned reinforcement and the expression of amphetamine-conditioned reward. Behav. Pharmacol 22, 173–181 (2011). [DOI] [PubMed] [Google Scholar]
- 115.Sartor GC & Aston-Jones GS A septal-hypothalamic pathway drives orexin neurons, which is necessary for conditioned cocaine preference. J. Neurosci 32, 4623–4631 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Plaza-Zabala A, Flores A, Maldonado R & Berrendero F Hypocretin/orexin signaling in the hypothalamic paraventricular nucleus is essential for the expression of nicotine withdrawal. Biol. Psychiatry 71, 214–223 (2012). [DOI] [PubMed] [Google Scholar]
- 117.Plaza-Zabala A, Martin-Garcia E, de Lecea L, Maldonado R & Berrendero F Hypocretins regulate the anxiogenic-like effects of nicotine and induce reinstatement of nicotine-seeking behavior. J. Neurosci 30, 2300–2310 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Georgescu D et al. Involvement of the lateral hypothalamic peptide orexin in morphine dependence and withdrawal. J. Neurosci 23, 3106–3111 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sharf R, Sarhan M & Dileone RJ Orexin mediates the expression of precipitated morphine withdrawal and concurrent activation of the nucleus accumbens shell. Biol. Psychiatry 64, 175–183 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shoblock JR et al. Selective blockade of the orexin-2 receptor attenuates ethanol self-administration, place preference, and reinstatement. Psychopharmacology 215, 191–203 (2011). [DOI] [PubMed] [Google Scholar]
- 121.Sharf R, Guarnieri DJ, Taylor JR & DiLeone RJ Orexin mediates morphine place preference, but not morphine-induced hyperactivity or sensitization. Brain Res. 1317, 24–32 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Riday TT et al. Orexin-1 receptor antagonism does not reduce the rewarding potency of cocaine in Swiss-Webster mice. Brain Res. 1431, 53–61 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Voorhees CM & Cunningham CL Involvement of the orexin/hypocretin system in ethanol conditioned place preference. Psychopharmacology 214, 805–818 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bayard S, Langenier MC & Dauvilliers Y Decision-making, reward-seeking behaviors and dopamine agonist therapy in restless legs syndrome. Sleep 36, 1501–1507 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Barateau L et al. Smoking, alcohol, drug use, abuse and dependence in narcolepsy and idiopathic hypersomnia: a case-control study. Sleep 39, 573–580 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cohen A, Mandrekar J, St Louis EK, Silber MH & Kotagal S Comorbidities in a community sample of narcolepsy. Sleep Med. 43, 14–18 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lee MJ et al. Comorbidity of narcolepsy and depressive disorders: a nationwide population-based study in Taiwan. Sleep Med. 39, 95–100 (2017). [DOI] [PubMed] [Google Scholar]
- 128.Inocente CO et al. Depressive feelings in children with narcolepsy. Sleep Med. 15, 309–314 (2014). [DOI] [PubMed] [Google Scholar]
- 129.Lopez R, Barateau L, Evangelista E & Dauvilliers Y Depression and hypersomnia: a complex association. Sleep Med. Clin 12, 395–405 (2017). [DOI] [PubMed] [Google Scholar]
- 130.Chastain EM, Duncan DS, Rodgers JM & Miller SD The role of antigen presenting cells in multiple sclerosis. Biochim. Biophys. Acta 1812, 265–274 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yong VW & Antel JP Major histocompatibility complex molecules on glial cells. Semin. Neurosci. 4, 231–240 (1992). [Google Scholar]
- 132.Wuthrich C, Batson S & Koralnik IJ Lack of major histocompatibility complex class I upregulation and restrictive infection by JC virus hamper detection of neurons by T lymphocytes in the central nervous system. J. Neuropathol. Exp. Neurol 74, 791–803 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Clarkson BDS, Patel MS, LaFrance-Corey RG & Howe CL Retrograde interferon-gamma signaling induces major histocompatibility class I expression in human-induced pluripotent stem cell-derived neurons. Ann. Clin. Transl Neurol 5, 172–185 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhang A et al. Developmental expression and localization of MHC class I molecules in the human central nervous system. Exp. Brain Res 233, 2733–2743 (2015). [DOI] [PubMed] [Google Scholar]
- 135.Partinen M et al. Increased incidence and clinical picture of childhood narcolepsy following the 2009 H1N1 pandemic vaccination campaign in Finland. PLOS ONE 7, e33723 (2012).This paper describes the increased incidence of narcolepsy in children and adolescents after vaccination with Pandemrix.
- 136.Sarkanen TO, Alakuijala APE, Dauvilliers YA & Partinen MM Incidence of narcolepsy after H1N1 influenza and vaccinations: systematic review and meta-analysis. Sleep Med. Rev 38, 177–186 (2018). [DOI] [PubMed] [Google Scholar]
- 137.Vaarala O et al. Antigenic differences between AS03 adjuvanted influenza A (H1N1) pandemic vaccines: implications for Pandemrix-associated narcolepsy risk. PLOS ONE 9, e114361 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Han F et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Ann. Neurol 70, 410–417 (2011). [DOI] [PubMed] [Google Scholar]
- 139.Aran A et al. Elevated anti-streptococcal antibodies in patients with recent narcolepsy onset. Sleep 32, 979–983 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Mahlios J, De la Herran-Arita AK & Mignot E The autoimmune basis of narcolepsy. Curr. Opin. Neurobiol 23, 767–773 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Honda Y et al. HLA-DR2 and Dw2 in narcolepsy and in other disorders of excessive somnolence without cataplexy. Sleep 9, 133–142 (1986). [DOI] [PubMed] [Google Scholar]
- 142.Mignot E, Hayduk R, Black J, Grumet FC & Guilleminault C HLA DQB1*0602 is associated with cataplexy in 509 narcoleptic patients. Sleep 20, 1012–1020 (1997). [PubMed] [Google Scholar]
- 143.Tafti M et al. DQB1 locus alone explains most of the risk and protection in narcolepsy with cataplexy in Europe. Sleep 37, 19–25 (2014).This study, drawing upon a large number of subjects, confirms that presence of the DQB1*06:02 allele increases the risk of narcolepsy about 200-fold.
- 144.Siebold C et al. Crystal structure of HLA-DQ0602 that protects against type 1 diabetes and confers strong susceptibility to narcolepsy. Proc. Natl Acad. Sci. USA 101, 1999–2004 (2004).This study shows that fragments of the orexin peptides fit well within the binding pocket of DQB1*06:02.
- 145.Pelin Z, Guilleminault C, Risch N, Grumet FC & Mignot E HLA-DQB1*0602 homozygosity increases relative risk for narcolepsy but not disease severity in two ethnic groups. US Modafinil in Narcolepsy Multicenter Study Group. Tissue Antigens 51, 96–100 (1998). [DOI] [PubMed] [Google Scholar]
- 146.van der Heide A, Hegeman-Kleinn IM, Peeters E, Lammers GJ & Fronczek R Immunohistochemical screening for antibodies in recent onset type 1 narcolepsy and after H1N1 vaccination. J. Neuroimmunol 283, 58–62 (2015). [DOI] [PubMed] [Google Scholar]
- 147.Mignot E et al. Complex HLA-DR and -DQ interactions confer risk of narcolepsy-cataplexy in three ethnic groups. Am. J. Hum. Genet 68, 686–699 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Miyagawa T et al. New susceptibility variants to narcolepsy identified in HLA class II region. Hum. Mol. Genet 24, 891–898 (2015). [DOI] [PubMed] [Google Scholar]
- 149.Ollila HM et al. HLA-DPB1 and HLA class I confer risk of and protection from narcolepsy. Am. J. Hum. Genet 96, 136–146 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Tafti M et al. Narcolepsy-associated HLA class I alleles implicate cell-mediated cytotoxicity. Sleep 39, 581–587 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Hor H et al. Genome-wide association study identifies new HLA class II haplotypes strongly protective against narcolepsy. Nat. Genet 42, 786–789 (2010). [DOI] [PubMed] [Google Scholar]
- 152.Hallmayer J et al. Narcolepsy is strongly associated with the T cell receptor alpha locus. Nat. Genet 41, 708–711 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Han F et al. Genome wide analysis of narcolepsy in China implicates novel immune loci and reveals changes in association prior to versus after the 2009 H1N1 influenza pandemic. PLOS Genet. 9, e1003880 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Faraco J et al. ImmunoChip study implicates antigen presentation to T cells in narcolepsy. PLOS Genet. 9, e1003270 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Luo G et al. Autoimmunity to hypocretin and molecular mimicry to flu antigens in Type 1 narcolepsy. Preprint at https://www.biorxiv.org/content/early/2018/08/24/378109 (2018). [DOI] [PMC free article] [PubMed]
- 156.Croft M, So T, Duan W & Soroosh P The significance of OX40 and OX40L to T cell biology and immune disease. Immunol. Rev 229, 173–191 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Buckner JH Mechanisms of impaired regulation by CD4+CD25+FOXP3+ regulatory T cells in human autoimmune diseases. Nat. Rev. Immunol 10, 849–859 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Dalal J et al. Translational profiling of hypocretin neurons identifies candidate molecules for sleep regulation. Genes Dev. 27, 565–578 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mickelsen LE et al. Neurochemical heterogeneity among lateral hypothalamic hypocretin/orexin and melanin-concentrating hormone neurons identified through single-cell gene expression analysis. eNeuro 4, ENEURO.0013–17.2017 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Azzam S et al. Proteomic profiling of the hypothalamus in two mouse models of narcolepsy. Proteomics 17, 1600478 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yelin-Bekerman L et al. Hypocretin neuron-specific transcriptome profiling identifies the sleep modulator Kcnh4a. eLife 4, e08638 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Cvetkovic-Lopes V et al. Elevated Tribbles homolog 2-specific antibody levels in narcolepsy patients. J. Clin. Invest 120, 713–719 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Baumann CR, Clark EL, Pedersen NP, Hecht JL & Scammell TE Do enteric neurons make hypocretin? Regul. Pept 147, 1–3 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ahmed SS et al. Antibodies to influenza nucleoprotein cross-react with human hypocretin receptor 2. Sci. Transl Med 7, 294ra105 (2015). [DOI] [PubMed] [Google Scholar]
- 165.Bernard-Valnet R et al. CD8 T cell-mediated killing of orexinergic neurons induces a narcolepsy-like phenotype in mice. Proc. Natl Acad. Sci. USA 113, 10956–10961 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Latorre D et al. T cells in patients with narcolepsy target self-antigens of hypocretin neurons. Nature 562, 63–68 (2018).This paper identifies a rare T cell population that targets fragments of prepro-orexin.
- 167.Kornum BR et al. Absence of autoreactive CD4+ T cells targeting HLA-DQA1*01:02/DQB1*06:02 restricted hypocretin/orexin epitopes in narcolepsy type 1 when detected by EliSpot. J. Neuroimmunol 309, 7–11 (2017). [DOI] [PubMed] [Google Scholar]
- 168.Ramberger M et al. CD4+ T-cell reactivity to orexin/hypocretin in patients with narcolepsy type 1. Sleep 40, zsw070 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lecendreux M et al. Narcolepsy type 1 is associated with a systemic increase and activation of regulatory T cells and with a systemic activation of global T cells. PLOS ONE 12, e0169836 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Tanaka T, Honda Y, Inoue Y & Honda M Detection of autoantibodies against hypocretin, hcrtr1, and hcrtr2 in narcolepsy: anti-hcrt system antibody in narcolepsy. Sleep 29, 633–638 (2006). [DOI] [PubMed] [Google Scholar]
- 171.Luo G et al. Absence of anti-hypocretin receptor 2 autoantibodies in post Pandemrix narcolepsy cases. PLOS ONE 12, e0187305 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Deloumeau A et al. Increased immune complexes of hypocretin autoantibodies in narcolepsy. PLOS ONE 5, e13320 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Katzav A et al. Passive transfer of narcolepsy: anti-TRIB2 autoantibody positive patient IgG causes hypothalamic orexin neuron loss and sleep attacks in mice. J. Autoimmun 45, 24–30 (2013). [DOI] [PubMed] [Google Scholar]
- 174.Tanaka S et al. Anti-Tribbles pseudokinase 2 (TRIB2)-immunization modulates hypocretin/orexin neuronal functions. Sleep 40, zsw036 (2017). [DOI] [PubMed] [Google Scholar]
- 175.Bergman P et al. Narcolepsy patients have antibodies that stain distinct cell populations in rat brain and influence sleep patterns. Proc. Natl Acad. Sci. USA 111, E3735–E3744 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Mignot E et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch. Neurol 59, 1553–1562 (2002). [DOI] [PubMed] [Google Scholar]
- 177.Sasai T, Inoue Y, Komada Y, Sugiura T & Matsushima E Comparison of clinical characteristics among narcolepsy with and without cataplexy and idiopathic hypersomnia without long sleep time, focusing on HLA-DRB1*1501/DQB1*0602 finding. Sleep Med. 10, 961–966 (2009). [DOI] [PubMed] [Google Scholar]
- 178.Nakamura M, Kanbayashi T, Sugiura T & Inoue Y Relationship between clinical characteristics of narcolepsy and CSF orexin-A levels. J. Sleep Res. 20, 45–49 (2011). [DOI] [PubMed] [Google Scholar]
- 179.Yin J et al. Structure and ligand-binding mechanism of the human OX1 and OX2 orexin receptors. Nat. Struct. Mol. Biol 23, 293–299 (2016). [DOI] [PubMed] [Google Scholar]
- 180.US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/show/NCT01789398 (2015). [DOI] [PubMed]
- 181.US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/show/NCT03332784 (2018). [DOI] [PubMed]
- 182.US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/show/NCT02348593 (2018). [DOI] [PubMed]
- 183.Okun ML, Lin L, Pelin Z, Hong S & Mignot E Clinical aspects of narcolepsy–cataplexy across ethnic groups. Sleep 25, 27–35 (2002). [DOI] [PubMed] [Google Scholar]
- 184.Pizza F et al. Clinical and polysomnographic course of childhood narcolepsy with cataplexy. Brain 136, 3787–3795 (2013).This paper provides a detailed description of status cataplecticus and obesity in children with narcolepsy.
- 185.Plazzi G et al. Complex movement disorders at disease onset in childhood narcolepsy with cataplexy. Brain 134, 3480–3492 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Willie JT et al. Distinct narcolepsy syndromes in orexin receptor-2 and orexin null mice: molecular genetic dissection of non-REM and REM sleep regulatory processes. Neuron 38, 715–730 (2003). [DOI] [PubMed] [Google Scholar]
- 187.Bastianini S, Silvani A, Berteotti C, Lo Martire V & Zoccoli G High-amplitude theta wave bursts during REM sleep and cataplexy in hypocretin-deficient narcoleptic mice. J. Sleep Res 21, 185–188 (2012). [DOI] [PubMed] [Google Scholar]
- 188.Hondo M et al. Histamine-1 receptor is not required as a downstream effector of orexin-2 receptor in maintenance of basal sleep/wake states. Acta Physiol. 198, 287–294 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Chemelli R, Sinton C & Yanagisawa M Polysomnographic characterization of orexin-2 receptor knockout mice. Sleep 23, A296–A297 (2000). [Google Scholar]
- 190.Hara J, Yanagisawa M & Sakurai T Difference in obesity phenotype between orexin-knockout mice and orexin neuron-deficient mice with same genetic background and environmental conditions. Neurosci. Lett. 380, 239–242 (2005). [DOI] [PubMed] [Google Scholar]
- 191.Lo Martire V, Silvani A, Bastianini S, Berteotti C & Zoccoli G Effects of ambient temperature on sleep and cardiovascular regulation in mice: the role of hypocretin/orexin neurons. PLOS ONE 7, e47032 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kaitin KI, Kilduff TS & Dement WC Sleep fragmentation in canine narcolepsy. Sleep 9, 116–119 (1986). [DOI] [PubMed] [Google Scholar]
- 193.Kaitin KI, Kilduff TS & Dement WC Evidence for excessive sleepiness in canine narcoleptics. Electroencephalogr. Clin. Neurophysiol 64, 447–454 (1986). [DOI] [PubMed] [Google Scholar]
- 194.Mitler MM & Dement WC Sleep studies on canine narcolepsy: pattern and cycle comparisons between affected and normal dogs. Electroencephalogr. Clin. Neurophysiol 43, 691–699 (1977). [DOI] [PubMed] [Google Scholar]
- 195.Lucas EA, Foutz AS, Dement WC & Mitler MM Sleep cycle organization in narcoleptic and normal dogs. Physiol. Behav 23, 737–743 (1979). [DOI] [PubMed] [Google Scholar]
- 196.Lin L et al. The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene. Cell 98, 365–376 (1999). [DOI] [PubMed] [Google Scholar]
- 197.Ripley B, Fujiki N, Okura M, Mignot E & Nishino S Hypocretin levels in sporadic and familial cases of canine narcolepsy. Neurobiol. Dis 8, 525–534 (2001). [DOI] [PubMed] [Google Scholar]
- 198.Scammell TE Narcolepsy. N. Engl. J. Med 373, 2654–2662 (2015). [DOI] [PubMed] [Google Scholar]
- 199.Dauvilliers Y & Barateau L Narcolepsy and other central hypersomnias. Continuum 23, 989–1004 (2017). [DOI] [PubMed] [Google Scholar]
- 200.Kalogiannis M et al. Cholinergic modulation of narcoleptic attacks in double orexin receptor knockout mice. PLOS ONE 6, e18697 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Kisanuki Y et al. Behavioral and polysomnographic characterization of orexin-1 receptor and orexin-2 receptor double knockout mice. Sleep 24, A22 (2001). [Google Scholar]
- 202.Abbas MG et al. Comprehensive behavioral analysis of male Ox1r–/–mice showed implication of orexin receptor-1 in mood, anxiety, and social behavior. Front. Behav. Neurosci 9, 324 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Hungs M et al. Identification and functional analysis of mutations in the hypocretin (orexin) genes of narcoleptic canines. Genome Res. 11, 531–539 (2001).This paper describes a large increase in histaminergic neurons in the brains of people and mice with narcolepsy.
- 204.Valko PO et al. Increase of histaminergic tuberomammillary neurons in narcolepsy. Ann. Neurol 74, 794–804 (2013).This study demonstrates an increase in histaminergic neurons in narcolepsy.
- 205.John J et al. Greatly increased numbers of histamine cells in human narcolepsy with cataplexy. Ann. Neurol 74, 786–793 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.John J, Wu MF, Boehmer LN & Siegel JM Cataplexy-active neurons in the hypothalamus: implications for the role of histamine in sleep and waking behavior. Neuron 42, 619–634 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Buskova J, Vaneckova M, Sonka K, Seidl Z & Nevsimalova S Reduced hypothalamic gray matter in narcolepsy with cataplexy. Neuro Endocrinol. Lett 27, 769–772 (2006). [PubMed] [Google Scholar]
- 208.Kaufmann C, Schuld A, Pollmacher T & Auer DP Reduced cortical gray matter in narcolepsy: preliminary findings with voxel-based morphometry. Neurology 58, 1852–1855 (2002). [DOI] [PubMed] [Google Scholar]
- 209.Joo EY, Tae WS, Kim ST & Hong SB Gray matter concentration abnormality in brains of narcolepsy patients. Kor. J. Radiol 10, 552–558 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Hong SB Neuroimaging of narcolepsy and Kleine–Levin syndrome. Sleep Med. Clin 12, 359–368 (2017). [DOI] [PubMed] [Google Scholar]