Abstract
Objectives:
Although it has long been known that communication with medical professionals presents a strong relationship with patient satisfaction, research on this topic has been hindered by conceptual and methodological issues (e.g. single-item measures, inclusion of idiosyncratic patient characteristics, etc.). Using a more comprehensive and integrated approach, this study had two objectives: to document the multidimensional structure of the Picker Patient Experience–15, and to test a patient communication/satisfaction model that organizes its dimensions in a conceptually logical array of relationships. First, the factorial structure of the Picker Patient Experience–15 was hypothesized to comprise five dimensions: communication with patient, with family, addressing fears/concerns, preparation for discharge, and patient satisfaction. Second, the hypothesized model included positive relationships between all four communications dimensions, on the one hand, and patient satisfaction, on the other. Within communication dimensions, communication with patient was hypothesized to be the incipient factor for other dimensions, and thus to be positively associated with the other three forms of communication.
Methods:
This research is based on a single time point design, which relied on administrative and questionnaire data. The study was conducted at a large University Hospital in Switzerland. The sample included 54,686 patients who received inpatient treatment, excluding those who were cared for in the intensive and intermediate care units. Patients filled out, over a 5-year period, the Picker Patient Experience questionnaire (PPE-15) after discharge (overall response rate of 41%).
Results:
The proposed five-factor structure of the Picker Patient Experience–15 was successfully supported by the results of a confirmatory factor analysis. Moreover, the hypothesized network of associations between communication and satisfaction latent constructs was substantiated using structural equation modeling. With the exception of the association between preparation for discharge and patient satisfaction, the hypothesized model was fully corroborated.
Conclusion:
A more in-depth understanding of patient satisfaction can be achieved when it is studied as a multifaceted phenomenon.
Keywords: Patient satisfaction, PPE-15, communication with medical professionals, confirmatory factor analysis, structural equation modeling
Since the beginning of the major public finances crisis, which started in the mid-70s, hospital administrators are faced with dire financial constraints such as anti-deficit legislation, budget and service cuts, the gradual introduction of case-related reimbursement, and pressures linked to greater financial autonomy. These have become the driving force behind various cost-reduction initiatives such as results-based management, balanced scorecards, and, more recently, lean management. Needless to say, balancing patient needs and satisfaction with cost effectiveness is a challenging task. Many hospitals have cut to the chase by adopting an input–output approach based on quantitative targets and volume of activity rather than patient-centered outcomes. However, a recent surge of interest for patients’ perceptions of their experience while in hospital has been brought about by the generalized implementation in 2008 in the United States of what is referred to as the Consumer Assessment of Healthcare Providers and Systems (CAHPS) patient satisfaction survey.1,2
This continuous data collection system is aimed at producing comparable information regarding the quality of care received in American hospitals. Patients, governmental agencies, and insurance company representatives, all have access to the results of the survey, which creates incentives to satisfy patients in order to have better ratings. Another major patient satisfaction survey is also used in this context: the Press Ganey survey,3,4 which includes all the CAHPS items along with a larger array of variables. This attention to patients’ perceptions has expanded outside of the United States, most notably in England and Switzerland, which have been monitoring patient satisfaction respectively since 2002 and 2009.5 In the European context, structured efforts aimed at measuring satisfaction are based on various instruments, which are similar to the CAHPS but are not used as systematically. Among those, the Picker Patient Experience (PPE) questionnaire appears to be the most widely used.6–8 To that effect, the french Institut de la Santé et de la Recherche Médicale (Institute of Health and Medical Research) has published a brief review of international perspectives on the measurement of patient satisfaction.6
It must be noted that the two major funding sources for American hospitals (Medicare and Medicaid) use this type of data to apply financial penalties to low-performing hospitals.9 Thus, patient satisfaction is now directly related to financial gains, at least in the United States, because it partially determines reimbursement rates.1 However, interest in patient satisfaction is also supported by a number of studies that have demonstrated the positive impact of satisfaction assessment on hospital performance,10 as well as on patients’ willingness to comply with their treatment plan.11 This has become particularly relevant in the context of efforts aimed at establishing a more balanced partnership between health care professionals and patients.12
But what is patient satisfaction? How is it best measured? At the onset, the concept of satisfaction is poorly defined,13,14 especially considering the fact that the medical community seems to hold a dim view of patients evaluating the quality of their work. Currently, satisfaction is thus measured in various ways and with different foci depending on the opinions sought from and expressed by patients.10 For instance, the CAHPS survey relies on a two-item measure of satisfaction based first on an overall quality score, and second on the probability of returning to or recommending the hospital to friends and family. This very general approach to satisfaction bears striking similarities with marketing and consumer research aimed at product merchandising, where a direct relationship is purported between satisfaction measured with a single item, and client brand loyalty.15 This rather crude operationalization of satisfaction is nonetheless useful; its parsimony and simplicity outweighing its methodological and conceptual flaws, especially because of the often lower threshold of validity required for data used in results-based management or for educational purposes.16 Furthermore, the availability of a simple satisfaction variable enables researchers to conceive a vast array of comparative or correlational studies limited only by the scope of individual, demographic, medical condition, or treatment-related independent variables.
To that effect, some of the main patient-level variables, which have been linked to satisfaction, are the patient’s health status,17 ethnicity,18 resource utilization,19 pain management,20 age,21 emergency or elective admission,22 along with a host of illnesses and medical conditions.2 An important difficulty relates to the lack of consensus on the factors that have the greatest impact on satisfaction,13 in part because of the heterogeneity of patients’ experiences from one hospital department or service to the other. However, neither the technical quality of care23 nor the outcome of medical procedures24 appears to be linked to patient satisfaction.
Nevertheless, several studies have found that communication between the health care professionals and the patient and his family seems to play a key role in the patient’s assessment of his experience of hospitalization,12,25–32 which begs an important question: is there an optimal type, content, channel, or competency with regard to patient/health professional communication? To that effect, the relationship between patient communication ratings and overall patient satisfaction may be influenced by staff and/or patient-level factors, but controlling for these factors still generates a significant association between physicians’ communication behaviors and overall patient satisfaction.33,34
General communication skills have been found to be the main factor explaining a positive assessment of hospitals,35 but individual differences among physicians and nursing staff in terms of communication competency have not been studied extensively, since most studies rely on aggregate institutional scores. Moreover, within staff, comparisons are usually performed through pre-experimental designs in which a group exposed to a communication enhancement intervention is compared to a control group. Still, physicians’ specific communication styles have also been studied in terms of dominance, affectivity, and cognitive orientation. Physicians perceived as highly affective or highly cognitive generated the highest satisfaction scores.36 Another aspect of the relationship between satisfaction and communication is based on staff stability: communication and satisfaction scores are negatively affected when there is more than one attending physician of record.37,38
Many attempts have been made to foster better communication between patients and medical staff in hopes of generating higher levels of satisfaction, but with mixed results.26,39–43 Inconclusive outcomes are usually explained by speculations regarding the need for a better match between communication practices and skills, on the one hand, and patient characteristics and individual differences, on the other.44–48 Still, it has been reported that the explanatory value of patient socio-demographic and health characteristics of the variance in satisfaction scores was low.49
To summarize, albeit neither the quality of care nor the outcome of medical procedures has been consistently linked to patient satisfaction,23,24 and although the results that relate patient experience variables to this outcome are inconclusive,16 communication between health care professionals and patients is an antecedent of satisfaction that has yielded promising results that warrant closer conceptual scrutiny and further empirical investigation.
Toward a patient satisfaction model based on communication
Most high-profile quality of care and patient experience instruments, such as the CAHPS50 and the Press Ganey,51 include items assessing communication between patients and health professionals. Indeed, all of the 11 instruments designed to evaluate patient experience of health care that were systematically and critically reviewed by Beattie and her colleagues16 comprise elements that target communication. However, these items are either included within general communication subscales or interspersed with heterogeneous content under multifarious headings. That is, the dimensions of patient/hospital personnel communication remain to be identified, and their associations with patient satisfaction clarified. The content of the PPE-15,7 meshed with information extracted from the literature, provided the foundation for the conceptual framework that was elaborated herein to achieve these aims.
The themes that act as item headings in the full version of the PPE were initially identified from data acquired through focus groups and nationwide surveys of patients that were categorized by experts according to their face validity.7,14,25 The resulting aggregates, described as key aspects of patient experience that served to formulate national guidelines regarding patient-centered care,52 include information and education, coordination of care, physical comfort, emotional support, respect for patient preferences, involvement of family and friends, continuity and transition, and overall impression. While this information is undoubtedly valuable and useful in its own right, its structure has never, to our knowledge, been examined nor validated by means of factor or component analyses. The role played by communication variables in defining patient experience, within this wealth of diversified and loosely structured information, cannot therefore be easily derived.
Fortunately, a more concise version of the PPE provides a potentially fruitful content pool that is directly germane to this purpose. Using data collected from large samples recruited in five different countries, the PPE-15 was designed to retain items that were most representative of the integral 40-item PPE questionnaire, as evaluated, among other criteria, by the amount of explained variance, thereby providing a meaningful yet more focused picture of patient experience.7,8 The structure of the items of the PPE-15 has not been statistically evaluated. However, it is proposed here that a theoretical evaluation of the content of those items reveals that they can be conceptually grouped into four communication dimensions: communication with patient, addressing fears/concerns, preparation for discharge, and communication with family, as well as a single satisfaction construct (see Table 1). The relevance and importance of these five dimensions of patient experience is underscored and supported by the following considerations.
Table 1.
Dimensions of patient experience.
| Communication with patient |
| COMM1-When you had important questions to ask a nurse, did you
get answers you could understand? COMM2-When you had important questions to ask a doctor, did you get answers you could understand? |
| Addressing fears/concerns |
| FEARS1-If you had any anxieties or fears about your condition or
treatment, did a doctor discuss them with you? FEARS2-If you had any anxieties or fears regarding your condition or treatment, did a nurse discuss them with you? FEARS3-Was it easy for you to find someone on the hospital staff to talk to regarding your concerns? |
| Preparation for discharge |
| DISCH1-Did someone on the hospital staff explain the purpose of
the medicine you were to take at home in a way you could
understand? DISCH2-Did someone tell you about the medication side effects to watch out for after you went home? DISCH3-Were you informed about possible danger signals for your illness, or from operation, which you should watch out for at home? |
| Communication with family |
| FAM1-Did your family, or someone close to you, have enough
opportunity to talk to your doctor? FAM2-Did the doctors and nurses give your family, or someone close to you, all the information they needed to help you recover? |
| Patient satisfaction |
| SAT1-Did you have enough to say about your
treatment? SAT2-Did you feel like you were treated with respect and dignity while you were in the hospital? SAT3-Do you think that the hospital staff did everything they could to help control pain? SAT4-How do you rate the quality of treatment you were given in general? SAT5-Would you come to our hospital again to treat the same disease/give birth? |
First, communication is a foremost aspect of human interactions in all contexts. In hospitals, its central function is obviously the transmission of information between medical personnel and patients. Sick or injured patients are in a vulnerable position. They rely on the expertise of health professionals to understand their symptoms, condition, prognosis, and treatment.53 They are thus likely to be keenly interested in this information, grateful to those who provide it, and dissatisfied if it is lacking.
Second, medical content aside, communication between health professionals and patients also serves psychological needs, such as addressing fears and concerns. Experiencing apprehension, and expecting support and reassurance, is natural when one’s physical integrity is compromised.54–57 Being ignored or rebuffed is typically unpleasant and dispiriting, and encountering indifference or hostility from those that are tasked with one’s care is worse and has been described as dehumanizing. The extent to which fears and concerns are alleviated is therefore liable to be a significant aspect of patient experience that impacts their satisfaction positively.
Beyond interactions that target patient issues and care, imparting information that helps patients prepare for discharge constitutes a third possible focus of communication. Managing one’s condition once outside the controlled environment provided by the hospital can raise a variety of questions or insecurities. Specific knowledge regarding aftercare and the symptoms to be on the lookout for is required.58,59 Preparation for discharge thus complements inpatient care and facilitates the transition back to the home environment. To that effect, patient experience has been conceptualized60 as sequential stages of the hospital journey, wherein discharge is viewed as the endpoint and is theorized to positively influence satisfaction when it is cogently anticipated.
Fourth, from a systemic standpoint, most patients do not enter health care institutions alone, and communication with concerned family and friends must also be considered. Significant others often request information directly from nurses or doctors, to complement the information provided by the patient.61,62 Also, significant others that are well briefed are better equipped to offer support during hospital stay and following discharge. Alternatively, caring family members and friends may be needlessly worried if medical professionals are unavailable or uncommunicative. Friends and family can thus take an important part in patient experience, and fruitful communication between significant others and medical professionals has the potential to be positively associated with self-reported patient satisfaction.
Finally, having examined communication dimensions, it is now pertinent to touch briefly on the concept of patient satisfaction. In accordance with other prominent measures, the satisfaction construct first included two general indicators of overall satisfaction. The three remaining items, issued from the PPE-15, were drawn from the 40-item version of the PPE on the basis of their explanatory potential (i.e. from a technical standpoint, because they accounted for a high degree of variance).7 The content of these items relates to patient participation in treatment-related decision making, pain control efficiency, as well as respectful and dignified care.
It is thus proposed here that the structure of patient experience is defined by four communication dimensions (communication with patient, addressing fears/concerns, preparation for discharge, and communication with family) and by a patient satisfaction factor. This theoretical assertion raises a further question. How do these hypothetical dimensions relate to one another?
As detailed above, all four communication dimensions could logically be expected to influence patient satisfaction. It would also make sense for communication constructs to be associated with one another, considering that they are all relational in nature, and that they complement one another. Moreover, because it is more general, and more likely to act as a starting point, communication with patient is theorized to act as a foundation for the three other forms of communication. Positive relationships are thus expected between communication with patient, on the one hand, and the three other forms of communication (addressing fears/concerns, preparation for discharge, and communication with family), on the other. Finally, because leaving the care received in a health institution could entail apprehensive feelings, addressing fears/concerns is expected to be positively related with preparation for discharge.
Summary of goals and hypotheses
The aim of this article is twofold: to test the factorial structure of communication and satisfaction dimensions as measured by the PPE-15, and to assess the network of relationships between these factors using structural equation modeling (SEM). Two hypotheses were tested:
The items of the PPE-15 will form a factorial structure comprising five dimensions: communication with patient, addressing fears/concerns, preparation for discharge, communication with family, and patient satisfaction.
The five dimensions of the PPE-15 will adopt the configuration of a model composed of the following network of relationships. First, communication with patient and family, addressing fears/concerns, and preparation for discharge, will be positively associated with patient satisfaction. Second, communication with patient will be positively associated with communication with family, with addressing fears/concerns, and with preparation for discharge. Finally, addressing fears/concerns will be positively associated with preparation for discharge.
Methods
Participants
All patients treated at a University Hospital located in Switzerland, from July 2010 to December 2014, were invited after discharge to fill out a satisfaction questionnaire. Patients treated in the more highly staffed intensive care and intermediate care units were excluded. The sample included 54,686 patients (out of 134,593) who filled out the PPE questionnaire. Power calculations were performed using equations and tables designed for SEM.63 Results indicated that when type I error is set at 5%, model fit is good, and degrees of freedom exceed 60, statistical power then reaches 80% for a sample size of 200 participants. Beyond power considerations, the stability of fit indices is optimal for sample sizes equal to or greater than 5000.63–65 Therefore, the size of this sample (N > 54 K) was more than sufficient to ensure that all data requirements were met for the confirmatory factor analysis (CFA) and the SEM analyses. The overall response rate was 41%, with variations from year to year, ranging from a low of 36% to a high of 48%, which are good return rates for a mail-in survey, the average rate being around 33%.66 No participants versus nonparticipants differences were found between patients’ profiles; thus, the possibility of a self-selection bias can be excluded. Average age of patients was 59 years (SD = 18.89) with equivalent gender representation (51% males; 49% females).
Instrument
The PPE questionnaire focuses on the interaction between patients and health care professionals. It includes questions dealing with quality, focus and content of communications, overall satisfaction, experience during treatment, and preparation for discharge. The most widely used version of the PPE is the 15-item short form, to which two generic satisfaction items (perception of care quality, intention to return) are added as supplemental variables. Most items are rated with a three-point Likert-type frequency scale ranging from no, to sometimes, to always. Psychometric qualities of the PPE in terms of content validity, criterion validity, test–retest stability, and internal consistency are well documented in various countries and settings.6,7,16,67–70 In order to reach the largest number of potential participants, translated versions in German, English, Italian, Spanish, French, and Turkish languages were prepared using parallel back-translation protocols. The medical and administrative records of the hospital provided background and demographic data that were merged with questionnaire responses prior to the complete anonymization of the dataset, as approved by the data security officer of the Kanton Basel-Stadt, Switzerland. In the Swiss context, this type of approval is mandatory to ensure that ethical guidelines concerning patient anonymity are respected.
Procedure
Participants received the PPE questionnaire by mail along with a self-return envelope and were invited to assess their health care experience at the hospital. The questionnaire was filled out by hand and returned, generally within 1 week.
Data treatment
Missing values were managed by generating a correlation matrix with pairwise deletion of missing data and by subsequently converting it to a covariance matrix that served as the database for the CFA, as well as for the structural equation model. Provided that sample size is large, which was the case here, using correlation matrices as data allows for appropriate multivariate solutions.71
Results
Descriptive statistics
Descriptive statistics indicated that satisfaction levels were high across genders with differences ranging between .02 and .06 decimal points for all items; older patients (>60) reported slightly lower scores except for the two overall satisfaction items (quality of care and intention of returning). Finally, patients with private insurance generally rated their satisfaction as being slightly higher. In order to test for differential response patterns according to demographics, comparative correlations were computed for each item according to gender, age groups, and insurance status. Correlations between items had almost identical magnitudes and levels of significance across the three demographic variables. Thus, the model was tested using the entire sample.
Factor structure
The factorial structure of the Picker Patient Experience questionnaire (PPE-15) was tested by means of a CFA, using the Bentler–Weeks algorithm.72 Technical specifications included the estimation of all parameters typically included in a CFA model: target factor loadings, measurement error for each item, as well as factor variances and covariances.
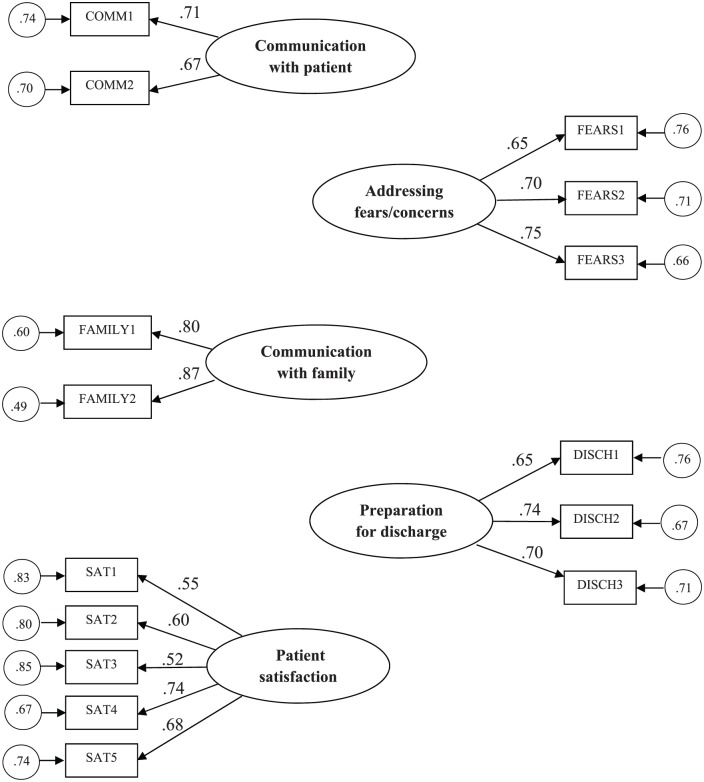
Initial results revealed that loadings were unsatisfactory for items 3 and 5 (i.e. standardized values were below .35). These items were thus withdrawn, and the CFA performed anew. No other post hoc modifications were implemented. The deletion of items 3 and 5 had no impact on overall model fit, which was satisfactory. Items included in the final CFA solution are displayed in Table 1. Values for the comparative fit index (CFI)73 and incremental fit index (IFI)74 were both .95; the range that is conventionally considered acceptable for these indices is from .90 to 1.00. Also, the goodness of fit index (GFI)75 was .97, which indicated that the estimated model explained 97% of the variance in the data. On the other hand, the standardized root mean square residual (SRMR)75 was .04, and the root mean square error of approximation (RMSEA)76 was .06 (90% confidence interval = .05–.06). For residual-based fit indices such as the SRMR and the RMSEA, values below .08 are considered indicative of a reasonable fit.77 All estimated parameters were statistically significant (p < .001) and of acceptable magnitude (see Figure 1).
Figure 1.
Confirmatory factor analysis.
Predicting patient satisfaction
A full structural equation model was performed, using the Bentler–Weeks algorithm,72 to examine the relationships between the quality of communication between medical professionals and patients, the extent to which patient’s fears or concerns were addressed, the information provided to family members, preparation for discharge, and patient satisfaction.
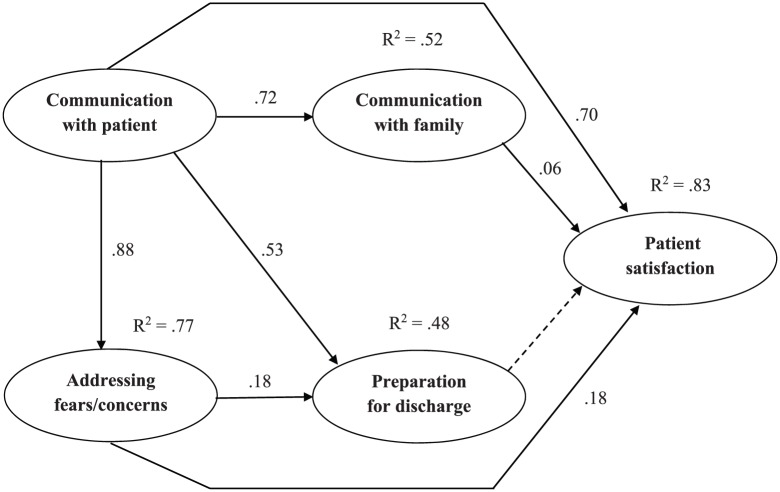
Results, presented in Figure 2, largely corroborated hypotheses. Model fit was satisfactory (CFI = .94; IFI = .94; GFI = .96; SRMR = .04; RMSEA = .06). With one minor exception, all expected associations were statistically significant. First, communication between medical professionals and patients was positively related to addressing patients’ fears or concerns. This association explained 77% of the variance of patients’ fears/concerns. Second, communication with patient was also positively related to information provided to family members. This association explained 52% of the variance of the extent to which information was communicated to family members. Third, communication with patient was further related, in conjunction with the extent to which patients’ fears/concerns were eased, to heightened preparation for discharge. Together, communication and addressing fears/concerns explained 48% of the variance of preparation for discharge. Fourth, communication with patient, addressing fears/concerns, and informing family members were all related to patient satisfaction. Jointly, these three variables explained 83% of patients’ satisfaction. Finally, contrary to expectations, preparation for discharge did not offer any unique contribution to patients’ satisfaction when assessed concurrently, as predictors of this outcome, with communication with patient, alleviating fears/concerns and informing family.
Figure 2.
Patient communication-satisfaction model. Standardized regression coefficients are reported on individual arrows; the proportion of explained variance (R2) is presented above each latent endogenous factor.
Discussion
This research had two main objectives: the first one was to validate the factor structure of the PPE-15 and the second one was to test a model of patient satisfaction through SEM. CFA results successfully documented the presence of the five expected factors: communication with patient, addressing fears and concerns, communication with family, preparation for discharge, and patient satisfaction.
The communication with patient factor included two items centered on the quality and intelligibility of the information transmitted both by nurses and by doctors, while the addressing fears/concerns factor included three items dealing with the availability and willingness of hospital staff to address the patient’s worries and apprehensions. With respect to these two factors, no differences were observed whether the information came from a doctor or a nurse. The communication with family factor included two items focused on the availability and clarity of information provided to patients’ kin or close ones. The preparation for discharge factor was comprised of three items targeting the transmission of information pertaining to patients’ needs and required home care post hospitalization (e.g. medication and symptoms).
Finally, the satisfaction factor is an aggregate of five items representing various dimensions of the patients’ experience: the impression of having been consulted about the treatment, of having been treated with respect and dignity, that the staff did what they could to help control pain, along with two general items: an overall assessment of the quality of treatment and the intention of returning to the same hospital, if required.
Results of the SEM analysis corroborated hypotheses. As expected, communication with patient predicted the extent to which their fears and concerns were addressed, the degree of preparation for discharge, and the quality of information given to the family. Alleviating fears and concerns also predicted preparation for discharge. Finally, satisfaction was jointly predicted by communication with patient (β = .70) and addressing fears and concerns (β = .06), although this association was clearly higher for the former than the latter.
Overall, the pattern of associations obtained herein calls for two noteworthy observations: (1) the factors that compose the model were complementary and worked together to predict patients’ satisfaction; (2) communication with patient played a key role in this model. As the single exogenous independent variable, it acted as the cornerstone of the model. Moreover, it was the only factor that was associated with all others, and it was the factor that was most highly related to others, by a substantial order of magnitude. Thus, while the other factors contributed unique variance that is important to the global picture in their own right, a large portion of the variance of these factors was also derived from the quality of communication with patient, which displayed the highest level of distinct variance with satisfaction. Quality of communication can therefore be seen as the basis from which other contributing factors to patients’ satisfaction unfold, as well as the unifying factor that organizes the antecedents of patients’ satisfaction into a coherent whole. To summarize, results suggest that the quality of communication acts both as the foundation and as the backbone of the patient satisfaction model.
This network of associations appears to be conceptually and statistically sound, with proximal factors closely linked to the patient’s experience being uniquely related to satisfaction, and more distal factors, such as communication with family and preparation for discharge, being more in the backdrop. This echoes preliminary results indicating that satisfaction is associated with patient-prompted information giving.78
The homogeneous and straightforward nature of items included in four of the factors contrasts with items regrouped in the satisfaction factor, which deals with pain, respect, consultation, and overall impressions through five different items. With a different research design and without item aggregation procedures, satisfaction could have been measured with a single “overall quality” item and possibly be predicted by any of the four remaining items of the satisfaction factor identified here. However, results presented here underscore the complexity of satisfaction as a construct.
A large number of related studies use ad hoc definitions with very low levels of conceptualization: satisfaction is generally measured on a Likert-type scale with high and low satisfaction scores, the respondent being solely in charge of defining the criteria used to attribute lower or higher marks. Obviously, satisfaction must be related to expectations, and the former vary according to financial constraints—privately insured patients having more expectations. Another way of measuring satisfaction is assessing the intention of the discharged patient of returning to the same hospital for future health problems. This approach does have its drawbacks: there could be a certain amount of confusion between the intention to return and the wish of not having to return; furthermore, there may be numerous reasons for not wanting to return to the same hospital which are not related to satisfaction, such as costs, distance, family pressures, specialized services, and so forth.
Patient satisfaction is the product of a specific set of variables and such is the nature of exploratory factor analyses (EFAs) and CFAs: aggregates are affected by the number, scope, and coherence of the variables that are available in the data set. Still, one of the interesting observations stemming from this research is that, according to the respondents, engaging patients while respecting them and treating them with dignity is tantamount to being satisfied overall and being open to the possibility of returning to the same hospital.
Still, more research needs to be conducted regarding the nature and scope of patient satisfaction as a measurable construct. Obviously, this can only be accomplished through complexity reduction and parsimony. The rather basic operationalization of satisfaction which is now in use is based on two questionable assumptions: (1) patients, medical and nursing staff, and hospital administrators share a common definition of what satisfaction is; (2) the intention to return to the same hospital is a clear indicator of patient satisfaction. It has been reported that patient satisfaction is not a good predictor of the intention to return to the same hospital.79,80 Our data indicated the presence of a moderate correlation between these same variables (r = .57; p < .01), which were nonetheless closely linked through the satisfaction factor. It would be interesting to compare how overall satisfaction expressed through low-specificity items (such as rate your degree of satisfaction on a scale from 1–10) relates similarly or not to intentions of returning to the same hospital as opposed to recommending this hospital to friends and family. The main difficulty here resides in the simplicity and usefulness of an imperfect measure of satisfaction which nonetheless generates scores, rankings, and information for results-based management. Historically, one is reminded how a much more complex construct, intelligence, is still equated with IQ scores, despite criticisms, largely because of its practicality.
On what objective basis does the patient assess his personal satisfaction, or is this the right question? By removing the “objective” nature of this assessment, one must conclude that patient satisfaction rests on a highly individualized mosaic of environmental and individual differences, which unfortunately must be expressed through a very crude quantitative indicator. If communication is a key component of patient satisfaction, how does the impact of communication practices stack up to the quality of the strictly medical procedures, especially since it has been reported that there is no correlation between patient satisfaction scores and hospital performance for trauma centers, leading certain authors to question the appropriateness of hospital reimbursement decisions based on CAHPS patient satisfaction scores.81 Alternatively, can medical procedures be considered as a distinct area of practice for which quality indicators can only be assessed by experts, leaving communication and patient satisfaction in the black box of qualitative concepts?
The search for higher patient satisfaction scores is now a major concern, and some of the literature reviewed here indicates clearly that there is a huge disproportion between efforts aimed at providing a quality experience for patients through exemplary practices and attempts made to micro-manage satisfaction scores by identifying what will trigger the patient’s willingness to give high scores. For instance, data-driven approaches could help generate algorithms enabling to put emphasis on specific satisfaction triggers for specific patients.45 Cultural proximity and relatedness should also be promoted, since satisfaction scores are significantly lower when foreign medical staff are attending the patient,82 with possible negative effects linked to racial profiling. Other possible strategies include multilevel patient-centered communication improvement strategies46 along with communication practices related to disease classification.83 Finally, “focusing (communication) efforts based on gender may allow for better patient satisfaction, optimized reimbursements, and improved hospital ratings.”84 All these suggestions rest on differences in terms of satisfaction scores measured in mostly uncontrolled settings through pre-experimental designs, which limits their scientific impact. Many patient-centered variables generate significant yet moderate differences; still, when these individual characteristics are controlled for, the largest proportion of variance for satisfaction is linked to communication.33 On this basis, designing highly specific communication strategies which factor in all possible patient-centered variables could prove to be a costly endeavor, with no guarantee that all these efforts will indeed generate higher satisfaction scores.
Limits of this research are mostly linked to methodological issues. Self-reports are notoriously vulnerable to single subject-method variance problems, which could not be controlled for here. Furthermore, all the data were collected in a single Swiss institution, which must be considered when trying to draw inferences applicable to other settings.
Future research should focus on the triangulation of satisfaction with other sources, on the extraction of the specific contribution of communication to patient satisfaction while controlling for individual differences and, finally, on the ecological, humanistic, and strictly medical dimensions of satisfaction, in order to ascertain whether they can be isolated or whether satisfaction must remain a diffuse, impressionist, and crude concept. Efforts aimed at identifying factors which can be acted upon in order to foster or increase satisfaction should be identified, as well as those which must solely be taken into account, being impervious or resistant to change, such as individual differences between patients and diagnosis. Perhaps research efforts could also draw upon satisfaction models used in other disciplines. For example, Herzberg’s85 model of job satisfaction includes two independent dimensions: dissatisfaction and satisfaction, which are not placed on a continuum as polar opposites. Dissatisfaction is linked to “hygiene” factors such as health issues and security, while satisfaction is linked to higher order factors such as communication. Exploring satisfaction with this two-tier conceptual framework could prove useful here by weighing differently “experiential” satisfaction and dissatisfaction factors as they relate to the quality of medical procedures and care.
Conclusion
The aim of this research was to study communication and satisfaction items included in the PPE questionnaire (PPE-15) in order to better understand the nature of and the relationships between these two constructs. Results indicated the presence of a five-item satisfaction factor combining overall satisfaction, the intention to return, the perception of having been treated with respect and dignity, being consulted, and pain management. CFA analyses also revealed that communication factors were structured according to the target of communication (patient or family) and to the contents of communication (addressing fears and concerns or preparation for discharge). Moreover, communication and satisfaction dimensions were logically associated with one another. These results underscore the contribution of a multidimensional approach to our understanding of patient experience.
Acknowledgments
The authors wish to thank all the participants in this study.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Kanton Basel Administrative Office and Basel University Hospital. No file number or certificate was issued.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: One week after discharge, all inpatients who were treated at the hospital received an invitation to take part in the study by regular mail, along with the questionnaire and a self-return envelope. All the necessary information was given to ensure an informed consent, including the usual ethical requirements for participants (anonymity, confidentiality, use of the data, absolute control over consent). Therefore, consent to participate was implicit: by filling out the questionnaire and returning it by mail, participants were giving their consent. Permission to publish was secured through a written consent form signed by all authors.
ORCID iDs: Daniel Pelletier  https://orcid.org/0000-0002-6635-9839
https://orcid.org/0000-0002-6635-9839
Pierre Collerette  https://orcid.org/0000-0002-8430-2617
https://orcid.org/0000-0002-8430-2617
References
- 1. Elliott MN, Beckett MK, Lehrman WG, et al. Understanding the role played by Medicare’s patient experience points system in hospital reimbursement. Health Aff 2016; 35(9): 1673–1680. [DOI] [PubMed] [Google Scholar]
- 2. Mazurenko O, Collum T, Ferdinand A, et al. Predictors of hospital patient satisfaction as measured by HCAHPS: a systematic review. J Healthc Manag 2017; 62(4): 272–283. [DOI] [PubMed] [Google Scholar]
- 3. Griffiths B. Enhanced communication performance improvement and patient satisfaction in an endoscopy/ambulatory surgery unit. Gastroenterol Nurs 2015; 38(3): 194–200. [DOI] [PubMed] [Google Scholar]
- 4. Press-Ganey. What is Press Ganey? http://www.pressganey.com/about (accessed September 2017).
- 5. Heberer MB, Bourke L, Widhaber F, et al. Partnership between patients and health care professionals is an important determinant of patient satisfaction. Int J Healthcare 2016; 2(1): 90–101. [Google Scholar]
- 6. INSERM. Measuring the patient experience: analysis of international initiatives (Mesure de l’expérience du patient: analyse des initiatives internationals). Paris: Institut National de la Santé et de la Recherche Médicale, 2011. [Google Scholar]
- 7. Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care 2002; 14(5): 353–358. [DOI] [PubMed] [Google Scholar]
- 8. Jenkinson C, Coulter A, Bruster S, et al. Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care 2002; 11(4): 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bentley-Kumar K, Jackson T, Holland D, et al. Trauma patients: I can’t get no (patient) satisfaction? Am J Surg 2016; 212(6): 1256–1260. [DOI] [PubMed] [Google Scholar]
- 10. Hekkert KD, Cihangir S, Kleefstra SM, et al. Patient satisfaction revisited: a multilevel approach. Soc Sci Med 2009; 69(1): 68–75. [DOI] [PubMed] [Google Scholar]
- 11. Pascoe GC. Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plan 1983; 6(3–4): 185–210. [DOI] [PubMed] [Google Scholar]
- 12. Adams DR, Flores A, Coltri A, et al. A missed opportunity to improve patient satisfaction? Patient perceptions of inpatient communication with their primary care physician. Am J Med Qual 2016; 31(6): 568–576. [DOI] [PubMed] [Google Scholar]
- 13. Avis M, Bond M, Arthur A. Questioning patient satisfaction: an empirical investigation in two outpatient clinics. Soc Sci Med 1997; 44(1): 85–92. [Google Scholar]
- 14. Drain MC, Clark PA. Measuring experience from the patient’s perspective: implications for national initiatives. J Healthc Qual 2004; 26: W4–W16. [Google Scholar]
- 15. Reynolds FD, Wells WD. Consumer behavior. New York: McGraw-Hill, 1977. [Google Scholar]
- 16. Beattie M, Murphy DJ, Atherton I, et al. Instruments to measure patient experience of healthcare quality in hospitals: a systematic review. Syst Rev 2015; 4: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wanzer MB, Booth-Butterfield M, Gruber K. Perceptions of health care providers’ communication: relationships between patient-centered communication and satisfaction. Health Commun 2004; 16(3): 363–383. [DOI] [PubMed] [Google Scholar]
- 18. Züllich D, Zimmering M, Keil T, et al. Migration background and patient satisfaction in a pediatric nephrology outpatient clinic. Pediatr Nephrol 2012; 27(8): 1309–1316. [DOI] [PubMed] [Google Scholar]
- 19. Morgan MW, Salzman JG, LeFevere RC, et al. Demographic, operational, and healthcare utilization factors associated with emergency department patient satisfaction. West J Emerg Med 2015; 16(4): 516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Alaloul F, Williams K, Myers J, et al. Impact of a script-based communication intervention on patient satisfaction with pain management. Pain Manag Nurs 2015; 16(3): 321–327. [DOI] [PubMed] [Google Scholar]
- 21. Chiu C, Feuz MA, McMahan RD, et al. “Doctor, make my decisions”: decision control preferences, advance care planning, and satisfaction with communication among diverse older adults. J Pain Symptom Manage 2016; 51(1): 33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fenton JJ, Jerant AF, Franks P. Influence of elective versus emergent hospital admission on patient satisfaction. J Am Board Fam Med 2014; 27(2): 249–257. [DOI] [PubMed] [Google Scholar]
- 23. Chang JT, Hays RD, Shekelle PG, et al. Improving patient care. Patients’ global ratings of their health care are not associated with the technical quality of their care. Ann Intern Med 2006; 144(9): 665–672. [DOI] [PubMed] [Google Scholar]
- 24. Chughtai M, Gwam CU, Khlopas A, et al. No correlation between Press Ganey survey responses and outcomes in post-total hip arthroplasty patients. J Arthroplasty 2018; 33(3): 783–785. [DOI] [PubMed] [Google Scholar]
- 25. Azizam NA, Shamsuddin K. Healthcare provider-patient communication: a satisfaction study in the outpatient clinic at hospital Kuala Lumpur. Malays J Med Sci 2015; 22(3): 56–64. [PMC free article] [PubMed] [Google Scholar]
- 26. Burgener AM. Enhancing communication to improve patient safety and to increase patient satisfaction. Health Care Manag 2017; 36(3): 238–243. [DOI] [PubMed] [Google Scholar]
- 27. Eichhorn L, Murday AK, Kohnen B, et al. Patient satisfaction as a measure of quality of patient care—comparison between a university hospital and a general hospital. Gesundheitswesen 2017; 79(8–9): 627–632. [DOI] [PubMed] [Google Scholar]
- 28. Patel NK, Kim E, Khlopas A, et al. What influences how patients rate their hospital stay after total hip arthroplasty? Surg Technol Int 2017; 30: 405–410. [PubMed] [Google Scholar]
- 29. Pieper C, Haag S, Gesenhues S, et al. Guideline adherence and patient satisfaction in the treatment of inflammatory bowel disorders-an evaluation study. BMC Health Serv Res 2009; 9: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schmocker RK, Holden SE, Vang X, et al. The number of inpatient consultations is negatively correlated with patient satisfaction in patients with prolonged hospital stays. Am J Surg 2016; 212(2): 282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shiozaki L, Burgomaster K, Lemonde M. Improving patient engagement and satisfaction: lessons from a patient-driven care initiative in a community-based hospital. Healthc Q 2017; 20(1): 62–66. [DOI] [PubMed] [Google Scholar]
- 32. Wong ELY, Coulter A, Hewitson P, et al. Patient experience and satisfaction with inpatient service: development of short form survey instrument measuring the core aspect of inpatient experience. PLoS ONE 2015; 10(4): e0122299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Clever SL, Jin L, Levinson W, et al. Does doctor-patient communication affect patient satisfaction with hospital care? Results of an analysis with a novel instrumental variable. Health Serv Res 2008; 43(5 Pt 1): 1505–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mann RK, Siddiqui Z, Kurbanova N, et al. Effect of HCAHPS reporting on patient satisfaction with physician communication. J Hosp Med 2016; 11(2): 105–110. [DOI] [PubMed] [Google Scholar]
- 35. Vural F, Ciftci S, Cakiroglu Y, et al. Patient satisfaction with outpatient health care services: evaluation of the components of this service using regression analysis. North Clin Istanb 2014; 1(2): 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kim SS, Park BK. Patient-perceived communication styles of physicians in rehabilitation: the effect on patient satisfaction and compliance in Korea. Am J Phys Med Rehabil 2008; 87(12): 998–1005. [DOI] [PubMed] [Google Scholar]
- 37. Turner J, Hansen L, Hinami K, et al. The impact of hospitalist discontinuity on hospital cost, readmissions, and patient satisfaction. J Gen Intern Med 2014; 29(7): 1004–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Velez VJ, Kaw R, Hu B, et al. Do HCAHPS doctor communication scores reflect the communication skills of the attending on record? A cautionary tale from a tertiary-care medical service. J Hosp Med 2017; 12(6): 421–427. [DOI] [PubMed] [Google Scholar]
- 39. Boissy A, Windover A, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med 2016; 31(7): 755–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fadhilah M, Oda Y, Emura S, et al. Patient satisfaction questionnaire for medical students’ performance in a hospital outpatient clinic: a cross-sectional study. Tohoku J Exp Med 2011; 225(4): 249–254. [DOI] [PubMed] [Google Scholar]
- 41. Oda Y, Onishi H, Sakemi T, et al. Improvement in medical students’ communication and interpersonal skills as evaluated by patient satisfaction questionnaire after curriculum reform. J Clin Biochem Nutr 2014; 55(1): 72–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. O’Leary KJ, Darling TA, Rauworth J, et al. Impact of hospitalist communication-skills training on patient-satisfaction scores. J Hosp Med 2013; 8(6): 315–320. [DOI] [PubMed] [Google Scholar]
- 43. O’Leary KJ, Killarney A, Hansen LO, et al. Effect of patient-centred bedside rounds on hospitalised patients’ decision control, activation and satisfaction with care. BMJ Qual Saf 2016; 25(12): 921–928. [DOI] [PubMed] [Google Scholar]
- 44. Davidson KW, Shaffer J, Ye S, et al. Interventions to improve hospital patient satisfaction with healthcare providers and systems: a systematic review. BMJ Qual Saf 2017; 26(7): 596–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Li L, Lee NJ, Glicksberg BS, et al. Data-driven identification of risk factors of patient satisfaction at a large urban academic medical center. PLoS ONE 2016; 11(5): e0156076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. McFarland DC, Johnson Shen M, Holcombe RF. Predictors of satisfaction with doctor and nurse communication: a national study. Health Commun 2017; 32(10): 1217–1224. [DOI] [PubMed] [Google Scholar]
- 47. Radtke K. Improving patient satisfaction with nursing communication using bedside shift report. Clin Nurse Spec 2013; 27(1): 19–25. [DOI] [PubMed] [Google Scholar]
- 48. Simmons SA, Sharp B, Fowler J, et al. Implementation of a novel communication tool and its effect on patient comprehension of care and satisfaction. Emerg Med J 2013; 30(5): 363–370. [DOI] [PubMed] [Google Scholar]
- 49. Wolf A, Olsson L-E, Taft C, et al. Impacts of patient characteristics on hospital care experience in 34,000 Swedish patients. BMC Nurs 2012; 11: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hays RD, Berman LJ, Kanter MH, et al. Evaluating the psychometric properties of the CAHPS patient-centered medical home survey. Clin Ther 2014; 36(5): 689.e1–696.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Presson AP, Chong Z, Abtahi AM, et al. Psychometric properties of the Press Ganey® outpatient medical practice survey. Health Qual Life Outcomes 2017; 15: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. NCGC. Patient experience of care for people using adult NHS services: patient experience in generic terms. London: Royal College of Physicians, 2012. [PubMed] [Google Scholar]
- 53. Finefrock D, Patel S, Zodda D, et al. Patient-centered communication behaviors that correlate with higher patient satisfaction scores. J Patient Exp 2018; 5(3): 231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gerteis M, Edgman-Levitan S, Walker JD, et al. What patients really want. Health Manage Q 1993; 15(3): 2–6. [PubMed] [Google Scholar]
- 55. Houwen J, Moorthaemer BJE, Lucassen PLBJ, et al. The association between patients’ expectations and experiences of task-, affect- and therapy-oriented communication and their anxiety in medically unexplained symptoms consultations. Health Expect. Epub ahead of print 30 December 2018. DOI: 10.1111/hex.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Stortenbeker IA, Houwen J, Lucassen PLBJ, et al. Quantifying positive communication: doctor’s language and patient anxiety in primary care consultations. Patient Educ Couns 2018; 101(9): 1577–1584. [DOI] [PubMed] [Google Scholar]
- 57. Zwingmann J, Baile WF, Schmier JW, et al. Effects of patient-centered communication on anxiety, negative affect, and trust in the physician in delivering a cancer diagnosis: a randomized, experimental study. Cancer 2017; 123(16): 3167–3175. [DOI] [PubMed] [Google Scholar]
- 58. Droz M, Senn N, Cohidon C. Communication, continuity and coordination of care are the most important patients’ values for family medicine in a fee-for-services health system. BMC Fam Pract 2019; 20(1): 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Newnham H, Barker A, Ritchie E, et al. Discharge communication practices and healthcare provider and patient preferences, satisfaction and comprehension: a systematic review. Int J Qual Health Care 2017; 29(6): 752–768. [DOI] [PubMed] [Google Scholar]
- 60. Boyd J. The 2006 inpatients importance study. Oxford: Picker Institute Europe, 2006. [Google Scholar]
- 61. Branson CF, Houseworth J, Chipman JG. Communication deficits among surgical residents during difficult patient family conversations. J Surg Educ 2019; 76(1): 158–164. [DOI] [PubMed] [Google Scholar]
- 62. Croke L. Enhancing intraoperative communication with patients’ families. AORN J 2018; 108(5): P7–P9. [DOI] [PubMed] [Google Scholar]
- 63. Lee T, Cai L, MacCallum RC. Power analysis for tests of structural equation models: handbook of structural equation modeling. New York: The Guilford Press, 2012, pp. 181–194. [Google Scholar]
- 64. Hoyle R, Gottfredson NC. Sample size considerations in prevention research applications of multilevel modeling and structural equation modeling. Prev Sci 2015; 16(7): 987–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: the effect of sample size. Psychol Bull 1988; 103(3): 391–410. [Google Scholar]
- 66. SurveyAnyplace. What’s the average survey response rate? [2018 benchmark], https://surveyanyplace.com/average-survey-response-rate/ (accessed February 2018).
- 67. Barrio-Cantalejo IM, Simón-Lorda P, Sánchez Rodriguez C, et al. Cross-cultural adaptation and validation of the Picker Patient Experience Questionnaire-15 for use in the Spanish population. Rev Calid Asist 2009; 24(5): 192–206. [DOI] [PubMed] [Google Scholar]
- 68. Bertran MJ, Viñarás M, Salamero M, et al. Spanish and Catalan translation, cultural adaptation and validation of the Picker Patient Experience Questionnaire-15. J Healthc Qual Res 2018; 33(1): 10–17. [DOI] [PubMed] [Google Scholar]
- 69. Jenkinson C, Coulter A, Reeves R, et al. Properties of the Picker Patient Experience Questionnaire in a randomized controlled trial of long versus short form survey instruments. J Public Health Med 2003; 25(3): 197–201. [DOI] [PubMed] [Google Scholar]
- 70. Leonardsen ACL, Grondahl VA, Ghanima W, et al. Evaluating patient experiences in decentralised acute care using the Picker Patient Experience Questionnaire; methodological and clinical findings. BMC Health Serv Res 2017; 17(1): 685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed. Boston, MA: Pearson Education, 2013. [Google Scholar]
- 72. Bentler PM. EQS6 structural equation program manual. Encino, CA: Multivariate Software Inc, 2006. [Google Scholar]
- 73. Bentler PM. Comparative fit indices in structural models. Psychol Bull 1990; 107(2): 238–246. [DOI] [PubMed] [Google Scholar]
- 74. Bollen KA. Structural equations with latent variables. New York: Wiley, 1989. [Google Scholar]
- 75. Jöreskog KG, Sörbom D. LISREL 7: user’s reference guide. Chicago, IL: Scientific Software International, 1989. [Google Scholar]
- 76. Steiger JH. Structural model evaluation and modification: an interval estimation approach. Multivariate Behav Res 1990; 25(2): 173–180. [DOI] [PubMed] [Google Scholar]
- 77. Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS. (eds) Testing structural equation models. Newbury Park, CA: SAGE Publications, 1993, pp. 136–162. [Google Scholar]
- 78. Ishikawa H, Son D, Eto M, et al. The information-giving skills of resident physicians: relationships with confidence and simulated patient satisfaction. BMC Med Educ 2017; 17(1): 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kessler DP, Mylod D. Does patient satisfaction affect patient loyalty? Int J Health Care Qual Assur 2011; 24(4): 266–273. [DOI] [PubMed] [Google Scholar]
- 80. Schoenfelder T, Schaal T, Klewer J, et al. Patient satisfaction and willingness to return to the provider among women undergoing gynecological surgery. Arch Gynecol Obstet 2014; 290(4): 683–690. [DOI] [PubMed] [Google Scholar]
- 81. Joseph B, Azim A, O’Keeffe T, et al. American College of Surgeons Level I trauma centers outcomes do not correlate with patients’ perception of hospital experience. J Trauma Acute Care Surg 2017; 82(4): 722–727. [DOI] [PubMed] [Google Scholar]
- 82. Mazurenko O, Menachemi N. Use of foreign-educated nurses and patient satisfaction in U.S. hospitals. Health Care Manage Rev 2016; 41(4): 306–315. [DOI] [PubMed] [Google Scholar]
- 83. Meredith P. Patient satisfaction with communication in general surgery: problems of measurement and improvement. Soc Sci Med 1993; 37(5): 591–602. [DOI] [PubMed] [Google Scholar]
- 84. Delanois RE, Gwam CU, Mistry JB, et al. Does gender influence how patients rate their patient experience after total hip arthroplasty? HIP Int 2018; 28(1): 40–43. [DOI] [PubMed] [Google Scholar]
- 85. Herzberg F. One more time: how do you motivate employees? Harv Bus Rev 2003; 81(1): 87–96. [PubMed] [Google Scholar]