Abstract
Introduction:
The postpartum period represents the time of risk for the emergence of maternal postpartum depression. There are no systematic reviews of the overall maternal outcomes of maternal postpartum depression. The aim of this study was to evaluate both the infant and the maternal consequences of untreated maternal postpartum depression.
Methods:
We searched for studies published between 1 January 2005 and 17 August 2016, using the following databases: MEDLINE via Ovid, PsycINFO, and the Cochrane Pregnancy and Childbirth Group trials registry.
Results:
A total of 122 studies (out of 3712 references retrieved from bibliographic databases) were included in this systematic review. The results of the studies were synthetized into three categories: (a) the maternal consequences of postpartum depression, including physical health, psychological health, relationship, and risky behaviors; (b) the infant consequences of postpartum depression, including anthropometry, physical health, sleep, and motor, cognitive, language, emotional, social, and behavioral development; and (c) mother–child interactions, including bonding, breastfeeding, and the maternal role.
Discussion:
The results suggest that postpartum depression creates an environment that is not conducive to the personal development of mothers or the optimal development of a child. It therefore seems important to detect and treat depression during the postnatal period as early as possible to avoid harmful consequences.
Keywords: infant outcomes, maternal outcomes, maternal postpartum depression, mother–infant interactions, systematic review
Introduction
Pregnancy and childbirth are two major events in a woman’s life. The birth of a baby induces sudden and intense changes in a woman’s roles and responsibilities. Thus, the postpartum period represents the time of risk for the emergence of maternal postpartum depression (PPD).1 PPD is a serious mental health problem. The Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV) defines PPD as a specifier for major depressive disorder (MDD).2 PPD is also defined symptomatically as exceeding a given threshold on a screening measure, such as the Edinburgh Postnatal Depression Scale (EPDS).3,4 In general, PPD occurs within 4 to 6 weeks after childbirth, and symptoms similar to MDD that may be present include depressed mood, loss of interest or pleasure in activities, sleep disturbance, appetite disturbance, loss of energy, feelings of worthlessness or guilt, diminished concentration, irritability, anxiety, and thoughts of suicide.5
The prevalence of PPD varies substantially depending on the definition of the disorder, country, diagnostic tools used, threshold of discrimination chosen for the screening measure, and period over which the prevalence is determined.3,6 For example, Halbreich and Karkun7 performed a review of the literature and found a PPD prevalence that varied between 0.5% and 60% among countries, as estimated by the self-reported 10-item EPDS questionnaire. The prevalence of PPD varies from 1.9% to 82.1% in developed countries, with the lowest prevalence reported in Germany and the highest prevalence in the United States.7,8 In developing countries, the prevalence varies from 5.2% to 74.0%, with the lowest prevalence reported in Pakistan and the highest prevalence in Turkey.8 This tremendous variation in the prevalence of PPD could be explained by heterogeneous study designs or the use of different diagnostic tools (e.g. the EPDS, Center for Epidemiologic Studies Depression Scale (CES-D), or Beck Depression Inventory (BDI)).9
Untreated PPD seems to have negative consequences for both infants and mothers. Nonsystematic reviews have indicated that the risks to children of untreated depressed mothers (compared to mothers without PPD) include problems such as poor cognitive functioning, behavioral inhibition, emotional maladjustment, violent behavior, externalizing disorders, and psychiatric and medical disorders in adolescence.5,10–17 These nonsystematic reviews reported the outcomes of these children from birth to adolescence. Other nonsystematic and systematic reviews have also explored specific maternal risks when mothers’ PPD is untreated, including more weight problems,18,19 alcohol and illicit drug use,20 social relationship problems,21 breastfeeding problems,22 or persistent depression23 compared with women who have received treatment. Nevertheless, there are no well-established systematic reviews of the overall maternal and/or infant outcomes of maternal PPD. Thus, the aim of this study was to evaluate all the maternal consequences of untreated PPD and its effects on children between 0 and 3 years of age.
Methods
To the extent possible, this research adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.24
Search strategy
We searched for all studies published between 1 January 2005 and 17 August 2016, using the following databases: MEDLINE via Ovid, PsycINFO, and the Cochrane Pregnancy and Childbirth Group trials registry. The following keywords were applied in the databases during the literature search: “postpartum depression” OR “postnatal depression” OR “puerperal depression.” The research was limited to human studies published in the English language. The search strategy and search terms used for this research are detailed in Appendix 1. Additional studies were identified through a manual search of the bibliographic references of the relevant articles and existing reviews.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (a) cohort and cross-sectional epidemiological and qualitative individual studies; (b) studies that included mothers of all ages who suffered from PPD (all combinations of comparison groups were possible: PPD vs no PPD, severe PPD vs mild PPD, etc.); and (c) studies that included health (physical or psychological) or social outcomes of PPD in the results.
The exclusion criteria were as follows: (a) meta-analyses, systematic and nonsystematic reviews, randomized controlled trials, and case studies; and (b) studies that included mothers who received treatment for PPD. Meta-analyses and systematic and nonsystematic reviews were only accessed to review their bibliographic references.
It is also important to note that there are many factors (e.g. comorbid conditions (anxiety, posttraumatic stress disorder, or substance abuse), socioeconomic status, education level, co- or single-parenting, and number of previous pregnancies) that could play an important role in the experience of PPD. Nevertheless, in the present systematic review, these factors were not considered as exclusion criteria; instead, they were treated as potential confounding factors. Moreover, because these confounding factors are difficult to account for in a systematic review, the adjusted results were used and discussed in this article when available.
After duplicates were removed, studies identified by the search strategy were exported to an Excel spreadsheet for study selection.
Study selection
In the first step, two investigators performed the study selection and assessed the titles and abstracts of the studies to exclude articles that were immaterial to the systematic review based on the inclusion criteria. In the second step, the same two investigators selected, read and evaluated the full-text studies that met the inclusion criteria. Given the large number of abstracts and full-text articles that needed to be read, the two investigators selected the studies independently.
Data extraction
The studies were divided between the two investigators for data extraction. However, if there was doubt regarding an article, the article was discussed by the two investigators, and a consensus was reached. The two investigators extracted the data from the selected studies according to a standardized data extraction form. The following data were isolated for each study: authors; journal name; year of publication; country of origin; objective of the study; study population data (type of population, mean age, sex ratio of the children, and age, if provided); sample size; design (length of intervention, number of groups, and description of groups); tools used to assess maternal PPD; reported prevalence of maternal PPD; types of infant and/or maternal outcomes and main (adjusted) results; and conclusion. To ensure that as many studies as possible were included in our systematic review, we systematically contacted the authors or co-authors when the full-text paper was not available.
Analysis and synthesis of the results
To facilitate data extraction, the included studies were initially grouped according to three types of outcomes: physical (e.g. weight, length, anthropometric indices, motor development, and physical health); psychological (e.g. mental health, cognitive development, language development, and bonding); or “other” (e.g. social relationships, quality of life, breastfeeding, and risky behaviors). Each outcome group was then thematically analyzed, coded by topic, and divided into more appropriate subgroups. The outcome subgroups were based on information obtained from the studies included in this review. In terms of the studies’ outcomes, key words were labeled and classified into groups with similar consequences. For example, the subcategories “weight,” “length,” and “anthropometric indices” were combined into the more general category of “anthropometry.”
This systematic review of the literature used a narrative synthesis methodology. Each included study was described in a commentary that reported the findings. Similarities and differences among the studies were also synthesized to draw conclusions within the subgroups.
Results
Included studies
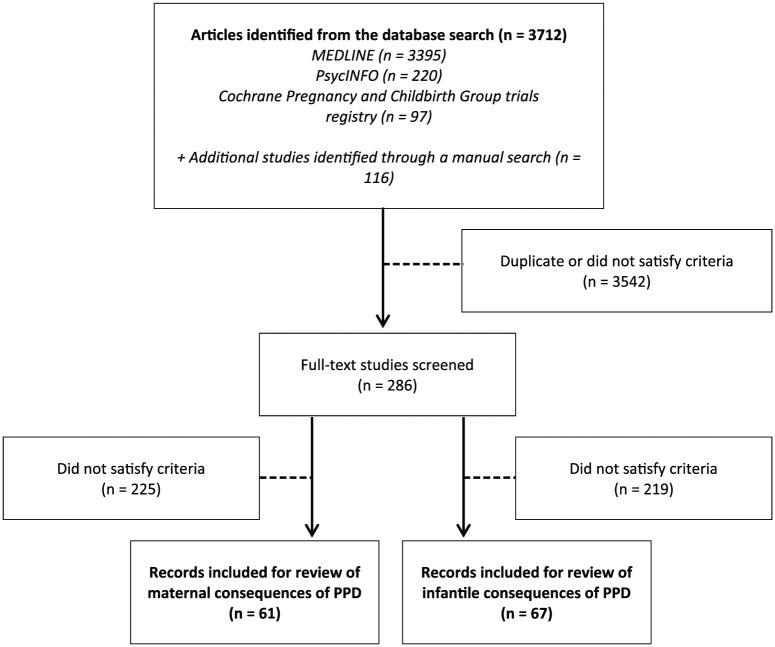
Of the 3712 references retrieved from the bibliographic databases (Figure 1), we identified 122 eligible studies that evaluated the consequences of PPD: 68 that evaluated the maternal consequences and 73 that evaluated the infant consequences. Among the included studies, 19 examined both the infant and the maternal consequences of PPD.
Figure 1.
Flowchart of the selection of relevant literature.
The group of studies that evaluated the maternal consequences of PPD included 46 cohort studies25–72 and 21 cross sectional studies73–92 (including 1 qualitative study).93 The majority of the studies were performed in the United States (28 of 68) and Europe (22 of 68), 10 studies were performed in Asia, and 8 studies were performed in Australia and New Zealand. All studies included women aged between 13 and 45 years. The number of participants ranged from 1593 to 22,118,28 and the duration of follow-up varied from 2 weeks32 to 6 years33 for the cohort studies.
PPD was mainly diagnosed according to the 10-item EPDS (46 studies); however, there were studies that used the BDI (6 studies), the World Health Organization Composite International Diagnostic Interview—Short Form (CIDI-SF; 3 studies), the Mini International Neuropsychiatric Interview (MINI; 3 studies), the Postpartum Depression Screening Scale (PDSS; 4 studies), and the CES-D (2 studies). To assess PPD, other studies used other questionnaires (e.g. the Patient Health Questionnaire depression module (PHQ-942 or PHQ-874), the Brief Symptom Inventory (BSI),31 or the Hamilton Depression Rating Scale (HDRS)30). The prevalence of PPD varied from 4.5% in a population of Canadian mothers at 6 weeks postpartum89 to 68.8% in a population of Australian mothers at 4 months postpartum.64
The group of studies that evaluated the infant consequences of PPD included 61 cohort studies31,34,37,45,48,49,52,53,56,64–66,69–72,94–138 and 12 cross-sectional studies.90–92,139–147 Most of the studies were performed in the United States (27 of 73) and Europe (20 of 73), 12 studies were performed in Asia, 10 studies were performed in Africa, and 4 studies were performed in Australia and New Zealand. All studies included women aged between 14 and 49 years and a percentage of baby girls that varied between 37.7%49 and 57.5%.147 The number of participants ranged from 28123 to 24,263,98 and the duration of follow-up varied from 2 months31,118,123 to 5 years96 for the cohort studies.
PPD was mainly diagnosed according to the 10-item EPDS (37 studies); however, there were studies that used the CES-D (9 studies), the BDI (7 studies), and the depression section of the Structured Clinical Interview for DSM-IV (SCID; 4 studies). To assess PPD, other studies used various types of questionnaires (e.g. the PHQ-9135,136 or the BSI100). Only one study did not specify the questionnaire that was used to detect PPD.98 The prevalence of PPD varied from 2.7% in a population of Pakistani mothers at 18 months postpartum94 to 68.8% in a population of Australian mothers at 4 months postpartum.64
The outcomes were separated into three sections: “maternal consequences of PPD,” “infant consequences of PPD,” and “mother–child interactions.” The first section, “maternal consequences of PPD,” reported results for 5 different types of outcomes: physical health (3 studies),35,67,88 including health care practices and utilization measures (2 studies);63,78 psychological health, including anxiety and depression (6 studies);36,37,42,44,66,88 quality of life (8 studies);27,37,39,48,66,85,86,88 relationships, including social relationships and relationships with the partner and sexuality (7 studies);37,38,44,66,73,74,85 and risky behaviors, including addictive behavior (smoking behavior and alcohol consumption: 4 studies)55,68,84,87 and suicidal ideation (7 studies).28,30,33,76,81,85,93 The second section, “infant consequences of PPD,” reported results for 9 different types of outcomes: anthropometry, including weight, length, and anthropometric indices (13 studies);97,100,104,109,110,112,113,119,125,126,131,140,142 infant health (10 studies);48,104,119,122–124,135,136,138,142 infant sleep (3 studies);104,108,130 motor development (7 studies);66,94,95,97,103,107,141 cognitive development (11 studies);94,95,99,101–103,107,134,139,141,147 language development (13 studies);66,94,95,102,103,105,116,117,129,131,132,139,141 emotional development (5 studies);94–96,115,121 social development (4 studies);66,115,141,143 and behavioral development (12 studies).49,52,96,110,111,114,115,120,121,131,133,141 Finally, the third section, “mother–child interactions,” reported results for 3 different types of outcomes: bonding and attachment, including mother-to-infant and infant-to-mother bonding (15 studies);29,31,34,37,43,44,47,52,54,56,61,64,82,106,127 breastfeeding (22 studies);25,26,32,41,45,59,60,62,65,69–72,77,89–92,118,119,130,137 and maternal role, including maternal behaviors (9 studies),26,40,49,52,53,62,79,83,85 maternal competence (2 studies),51,75 maternal care for the infant (6 studies),37,53,130,137,145,146 infant health care practices or utilization measures (8 studies),26,37,57,63,98,128,130,142 maternal perception of the infant’s patterns (5 studies),40,46,50,58,80 and the risk of maltreatment (2 studies).130,144
Maternal consequences of PPD
Physical health
Only three studies evaluated the physical health of depressed mothers (Table 1). One study found that compared to the general population of women, depressed mothers scored significantly lower on the 36-Item Short Form Health Survey (SF-36) physical component summary score (assessed based on physical functioning, role limitations due to physical health, bodily pain, and general health perceptions).88 However, this study indicated that the severity of the depressed mood was not associated with a worse physical health status, whereas a worse aerobic capacity emerged as a significant independent contributor to physical health status. The two last studies evaluated postpartum weight retention (PPWR) and found that significantly more women with PPWR had higher scores on the PPD scale.35,67
Table 1.
Characteristics of the studies included in the evaluation of maternal physical health.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Physical health | |||||||
| Biesmans35 | Belgium Mean age: 30.1 ± 4.3 years Gender of newborns: not given |
75 | Cohort study 14 months Two groups: - PPWR - No PPWR |
EPDS (Depressed = EPDS ⩾ 10) |
PPWR: 30.8% No PPWR: 8.3% |
PPWR | 52% of the women did not reach their pre-pregnancy weight 1 year after childbirth. Women with PPWR weighed approximately 2 (M = 2.3; SD = 2.8) kg above their weight from before the last pregnancy. There were significantly more women with higher scores on the PPD scale in the group with PPWR (p = 0.015). |
| Da Costa88 | Canada Mean age: 33.2 ± 4.6 years Gender of newborns: not given |
78 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
63% | Physical health status; mental health status; health-related quality of life | Compared to Canadian normative data, women experiencing postpartum depressed mood scored significantly lower on all SF-36 domains and on the SF-36 physical and mental component summary scores. Severity of depressed mood was not associated with worse physical health status, while poorer aerobic capacity emerged as a significant independent contributor of physical health status. |
| Herring67 | USA Mean age: 33.0 ± 4.7 years Gender of newborns: not given |
850 | Cohort study 18 months Four groups: - None - Pregnancy only - Postpartum only - Pregnancy and postpartum |
EPDS (Depressed = EPDS > 12) |
4% | Risk of substantial weight retention | In multivariate logistic regression analyses, after adjustment for weight-related covariates, maternal sociodemographics, and parity, new-onset PPD was associated with more than double the risk of retaining at least 5 (OR = 2.54, 95% CI = 1.06, 6.09) kg. |
| Health care practices and utilization measures | |||||||
| Eilat-Tsanani63 | Israel Age: 18 years and above Gender of newborns: not given |
527 | Cohort study 2 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) (+survey) |
9.9% | Women’s’ consultations with physicians (family physicians, gynecologists, and/or pediatricians) | Women with PPD differed from those without PPD in terms of the frequency of and reasons for consultations. The rate of PPD was significantly higher in women who consulted for medical reasons than those who came for routine care (13% vs 4%, p = 0.001). Women with multiple visits (four or more) to all doctors had higher rates of PPD than the others (16.7% vs 7%, p = 0.002). Women with PPD consulted more with family physicians (20.6% vs 7.8%, p = 0.01) and pediatricians (18.3% vs 7.1%, p = 0.001). No significant difference in PPD rates was found in relation to the number of visits to gynecologists. |
| McCallum78 | Australia Mean age: 33.0 ± 4.5 years Gender of newborns: not given |
875 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 9) |
16.7% | Health service use | Poorer maternal mental health was also implicated with a one-point increase in the EPDS associated with a 4% (0.4%–8%) increase in the likelihood of using more than three services (adjusted for socioeconomic position, partner status, language, gestational age, and unsettled infant behavior). Women with worse depressive symptoms were more likely to consult a general practitioner or mental health professional, but not other services. |
PPD: postpartum depression; PPWR: postpartum weight retention; EPDS: Edinburgh Postnatal Depression Scale; SD: standard deviation; SF-36: 36-Item Short Form Health Survey; OR: odds ratio; CI: confidence interval.
Health care practices and utilization measures
Two studies63,78 demonstrated an effect of maternal PPD on health care practices and utilization measures (Table 1). One of these studies demonstrated that women with worse depressive symptoms were more likely to consult a general practitioner or mental health professional than women with milder depressive symptoms.78 The other study showed that women with PPD consulted with family physicians more often than nondepressed mothers did.63
Psychological health
Six studies (Table 2) evaluated the association between PPD and psychological health; five studies focused on overall psychological health,37,42,44,66,88 two studies focused on anxiety,36,37 and three studies focused on depression.36,37,66
Table 2.
Characteristics of the studies included in the evaluation of the maternal psychological health.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Da Costa88 | Canada Mean age: 33.2 ± 4.6 years Gender of newborns: not given |
78 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
63% (EPDS ⩾ 12) | Physical health status; mental health status; health-related quality of life | Depressed mood was a significant predictor (β = −0.44, p < 0.0001) of mental health status, explaining 18% of the variance. After controlling for depressed mood, the occurrence of pregnancy complications (p = 0.001), cesarean delivery (p = 0.005), poorer sleep quality (p = 0.009), lower perceived social support (p = 0.045), and greater life stress (p = 0.003) were significant independent determinants of worse mental health status. Together, the variables in the second step explained an additional 30% of the variance. |
| Gollan42 | USA Mean age (years): Depressed: 27.5 ± 6.8 Nondepressed: 30 ± 4.9 Gender of newborns: not given |
80 | Cohort study 15 weeks Two groups: - PPD - No PPD |
DSM-IV PHQ-9 QIDS-SR |
33.8% | Affective reactivity (affective information processing) | Results of the GLM analyses of variance for postpartum ratings of valence and arousal revealed a significant main effect for group (p < 0.05) in which postpartum women with major depression demonstrated significantly lower arousal ratings for negative stimuli compared with healthy women (p < 0.001). In addition, postpartum women with major depression had significantly lower valence ratings for negative stimuli (p = 0.03) compared with healthy women. |
| Lilja44 | Sweden Mean age: 27.8 years Gender of newborns: not given |
419 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
22.2% | Women’s mood over the first year postpartum; women’s relationship with their infant; women’s relationship with their partner | Mothers who scored high on the EPDS on day 10 rated their mood lower, for example, they reported being less happy and more dysphoric and sad than mothers who scored low on the EPDS. Significant positive correlations were found between the EPDS and the mood scale at day 3 (r = 0.355, p < 0.001), day 10 (r = 0.615, p < 0.001), 6 months (r = 0.349, p < 0.001), and 12 months (r = 0.370, p < 0.001). Thus, a moderately increased score on the EPDS on day 10 postpartum predicted a low mood over the first year postpartum. |
| Prenoveau36 | UK Age (years): GAD and MDD: 32.5 ± 5.3 GAD only: 31.8 ± 5.1 MDD only: 32.3 ± 5.6 No diagnosis: 32.6 ± 4.8 Female babies (%): GAD and MDD: 41.5 GAD only: 50 MDD only: 52.5 No diagnosis: 51.9 |
296 | Cohort study 21 months Four groups: - GAD and MDD - GAD only - MDD only - No diagnosis |
EPDS (cut-off value not given) |
GAD and MDD: 13.9% GAD only: 27.0% MDD only: 13.5% |
GAD MDD |
Women diagnosed with MDD at 3 months postpartum were significantly more likely to meet diagnostic criteria for MDD at least once during the follow-up period than those who were not diagnosed with MDD at 3 months (MDD only → MDD only (coefficient): 3 months → 6 months: 23.7; 6 months → 10 months: 28.6; 10 months → 14 months: 37.3; 14 months → 24 months: 135.0, p < 0.001). Women with MDD at 3 months were also significantly more likely to present with GAD at 6 months (3 months → 6 months: 10.9, p < 0.05), but not after. |
| Wang66 | Taiwan Age (years): Depressed: 28.34 ± 5.52 Nondepressed: 29.45 ± 4.13 Female babies: 55.0% |
60 | Cohort study 1 year Two groups: - PPD - No PPD |
BDI-II | 48.3% | Psychosocial health | At 1 year after childbirth, women in the depressed group still suffered mild depression and reported greater perceived stress and lower perceived social support and self-esteem than women in the nondepressed group. Women at 6 weeks after childbirth suffered mainly from moderate-to-severe depression (23.76 ± 6.25 on the BDI), and symptoms improved to mild-to-moderate depression at 1 year (14.66 ± 7.22 on the BDI). |
| Vliegen37 | Belgium Mean age (years): T1: 29.39 ± 4.40 T2: 32.95 ± 4.51 Gender of newborns: not given |
41 | Cohort study 3.5 years Two groups: - PPD - No PPD |
BDI-II (Depressed = BDI ⩾ 13) |
39% | Maternal depression; treatment after hospitalization; life events; relationship | Mothers who were depressed at follow-up had not only
significantly elevated scores for severity of depression
but also significantly elevated levels of state and
trait anxiety, state and trait anger, and negative
affect compared to nondepressed mothers. Depressed
mothers also had significantly higher levels of anger,
lower scores on anger control, and lower levels of
positive affect. Regarding emotional availability, they
showed a significantly lower level of mutual attunement,
but no differences were found on the other indices of
emotional availability. The number of depressive
episodes between Time 1 and Time 2 did not differ
between mothers with and mothers without current
depression at follow-up. However, currently depressed
mothers had significantly longer depressive episodes
(M = 90 weeks, SD = 80) compared to the mothers without
current depression (M = 42 weeks, SD = 45, p < 0.05).
Regarding treatment after hospitalization, the proportion of mothers who were hospitalized during the follow-up period was approximately 20% and did not differ between samples. |
GAD: generalized anxiety disorder; MDD: major depressive disorder; PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.); PHQ-9: Patient Health Questionnaire depression module; QIDS-SR: Quick Inventory of Depressive Symptomatology (Self-Report); BDI-II: Beck Depression Inventory-II; GLM: general linear models; SD: standard deviation.
Overall psychological health
Several studies showed that depressed mothers presented lower mood scores in the long term (1 year after childbirth) than mothers without depression. One study highlighted that compared to the general population of women, depressed mothers scored significantly lower on the SF-36 mental component summary score (based on vitality, social functioning, role limitations due to emotional problems, and mental health).88 This study also showed that depressed mood was a significant predictor of mental health status in the future (explaining 18% of its variance).88 Another study showed that women with PPD had lower self-esteem than mothers without depression.66 Depressed mothers also reported being less happy, more dysphoric, and sadder than mothers without depression.44 In addition, women with high depression scores had significantly higher levels of anger, lower scores for anger control, and lower levels of positive affect than mothers with low depression scores.37 Finally, mothers with PPD were generally less responsive to negative stimuli, with lower ratings for intensity and reactions to negative pictorial stimuli, than mothers without PPD.42
Anxiety
One study showed that depressed mothers had significantly elevated levels of state and trait anxiety at 1 year and 3.5 years after childbirth compared with nondepressed mothers.37 Another study highlighted that depressed mothers at 3 months postpartum were more likely to exhibit an anxiety disorder than nondepressed mothers at 6 months postpartum, but not after this time point.36
Depression
Compared to nondepressed women, women who were diagnosed with depression in the first weeks after childbirth continued to suffer from depression at 1 year after childbirth.36,37,66 However, one study underlined that although mothers continued to suffer from depression, the symptoms appeared to improve, progressing from moderate-to-severe depression at 6 weeks to mild-to-moderate depression at 1 year.66 Therefore, there appeared to be a slight improvement in the severity of depression over time with or without treatment.66 Another study used a life history calendar method and found that compared to currently nondepressed mothers, mothers who were depressed at follow-up (3.5 years) did not have more depressive episodes; however, they had longer depressive episodes, received more psychotherapy after hospitalization, and experienced more negative life events during the follow-up period.37
Quality of life
Eight studies27,37,39,48,66,85,86,88 examined the overall quality of life of depressed mothers compared with nondepressed mothers (Table 3). Three studies48,86,88 demonstrated a significantly negative association between maternal depressive symptoms and quality of life. Women with PPD had lower scores on all dimensions of quality of life (e.g. SF-36 or a generic Health-Related Quality of Life (HRQoL) questionnaire) than women without PPD. However, one of the three studies showed that after controlling for mental health-related quality of life earlier in the postpartum period, there was no difference in the subsequent mental health-related quality of life according to the presence of significant depressive symptoms later in the postpartum period.48
Table 3.
Characteristics of the studies included in the evaluation of the maternal quality of life.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Curtis27 | USA Mean age: 25.0 ± 6.0 years Female babies: 48% |
2974 | Cohort study 3 years Two groups: - PPD - No PPD |
CIDI-SF | 12.6% | Homelessness or risk of homeless (lack of fixed, regular, and adequate night-time residence or residence in a temporary accommodation or space not intended for residence) | Mothers who experienced depression were significantly more likely than those who did not to become homeless (6% vs 2%) and to be at risk of homelessness (conditional on not having become homeless; 14% vs 9%). Depression during the postpartum year was associated with more than twice the odds of homelessness (OR = 2.29, 95% CI = 1.08, 4.85) and almost 1.5 times the odds of being at risk of homelessness (OR = 1.40, 95% CI = 1.12, 1.75) at 3 years. |
| Da Costa88 | Canada Mean age: 33.2 ± 4.6 years Gender of newborns: not given |
78 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
63% (EPDS ⩾ 12) | Physical health status; mental health status; health-related quality of life | Women who were depressed during postpartum scored significantly lower on all eight SF-36 dimensions and on both summary component scores compared to age-appropriate normative means. |
| Darcy48 | USA Mean age: 30.3 years Gender of newborns: not given |
217 | Cohort study 1 year Two groups: - PPD - No PPD |
CES-D | 32.7% | Maternal health-related quality of life (mental component and physical component) | Mothers with significant depressive symptoms had significantly worse physical (p = 0.02) and mental (< 0.0001) health-related quality of life. After controlling for mental health-related quality of life earlier in the postpartum period, there was no difference in subsequent mental health-related quality of life based on the presence of significant depressive symptoms later in the postpartum period. |
| De Tychey86 | France Age: not given Female babies: 48.1% |
181 | Cross-sectional study Three groups: - No depression - Mild depression - Severe depression |
EPDS (Mild, ⩾8 and <12; Severe, ⩾12) |
Mild depression: 22.1% Severe depression: 9.4% |
Postnatal quality of life | Postnatal depression strongly and negatively influenced all dimensions of life quality explored through the SF-36, e.g., physical functioning (PF), physical role (RP), bodily pain (BP), mental health (MH), emotional role (RE), social functioning (SF), vitality (VT), general health (GH), standardized physical component (PCS), and standardized mental component (MCS). |
| Posmontier85 | USA Mean age (years): No PPD: 31.0 ± 4.5 PPD: 30.0 ± 5.5 Female babies (%): No PPD: 78.3 PPD: 30.4 |
46 | Cross-sectional study Two groups: - PPD - No PPD |
MINI | Not applicable (number of PPD and no PPD women were
fixed at the beginning of the study)
Nondepressed: n = 23 Depressed: n = 23 |
Functional status (physical infant care, personal care, household care, social activities, and occupational activities) | Specifically, lower levels of household, social, and personal functioning were correlated with PPD. In multiple regression analyses, PPD predicted lower overall functional status (p < 0.001), household function (p < 0.05), social function (p < 0.001), and personal function (p < 0.001). |
| Wang66 | Taiwan Age (years): Depressed: 28.34 ± 5.52 Nondepressed: 29.45 ± 4.13 Female babies: 55.0% |
60 | Cohort study 1 year Two groups: - PPD - No PPD |
BDI-II | 48.3% | Psychosocial health | Significant differences were found between the depressed and the nondepressed groups for depression, perceived stress, social support, and self-esteem. At 1 year after childbirth, women in the depressed group still suffered from mild depression and showed greater perceived stress and lower perceived social support and self-esteem than women in the nondepressed group. |
| Taylor39 | Australia Mean age: 30.3 ± 5.0 years Gender of newborns: not given |
615 | Cohort study 24 weeks Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
T1: 9.2% T2: 9.4% T3: 8.4% T4: 7.0% |
Fatigue | One week after birth, state anxiety (0.47) and more depressive symptoms (0.28) were significantly (< 0.05 to < 0.01) correlated with fatigue. At 6 weeks, 3 months, and 6 months, depression was no longer associated with fatigue, but maternal state anxiety was a major predictor of fatigue (ranging from β = 0.38 to 0.51). |
| Vliegen37 | Belgium Mean age (years): T1: 29.39 ± 4.40 T2: 32.95 ± 4.51 Gender of newborns: not given |
41 | Cohort study 3.5 years Two groups: - PPD - No PPD |
BDI-II (Depressed = BDI ⩾ 13) |
39% | Maternal depression; treatment after hospitalization; life events; relationship | Currently depressed mothers reported significantly more negative life events, indicating greater distress and discontinuity. More specifically, currently depressed mothers reported more financial problems (69% vs 31%, p < 0.05) and more illness among close relatives (100% vs 46%, p < 0.05). |
PPD: postpartum depression; CIDI-SF: Composite International Diagnostic Interview—Short Form; EPDS: Edinburgh Postnatal Depression Scale; CES-D: Center for Epidemiologic Studies Depression Scale; MINI: Mini International Neuropsychiatric Interview; BDI-II: Beck Depression Inventory-II; OR: odds ratio; CI: confidence interval.
Studies also showed that PPD was associated with greater perceived stress,66 more negative life events (indicating greater distress and discontinuity), more financial problems, and more illness among close relatives.37 Depressive symptoms were also associated with fatigue during the first week but not at 6 weeks, 3 months, and 6 months after childbirth.39
Regarding the life environment, one study showed that PPD predicted lower levels of household functioning (household care).85 Another study demonstrated that mothers who experienced depression were twice as likely to become homeless and approximately 1.5 times more likely to be at risk for homelessness than nondepressed mothers.27
Relationships
Seven studies evaluated social and couple relationships in relation to maternal depressive symptoms (Table 4); four studies were related to social relationships,37,66,73,85 and four studies were related to relationships with partners and sexuality.37,38,44,74
Table 4.
Characteristics of the studies included in the evaluation of the maternal social and couple relationship.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Dagher73 | USA Mean age: 29.3 ± 5.6 years Gender of newborns: not given |
882 | Cross-sectional study Two groups: - PPD - No PPD |
PDSS-SF | 62.0% | Return to work and intention to return to work | Tending to the baby and being depressed suppressed the return to paid work. Nondepressed mothers with unintended pregnancies returned to work the soonest. Compared with mothers who were not depressed and had an unintended pregnancy, the RR of returning to paid work (0.70) was significantly lower for mothers who were depressed and had an intended pregnancy. Mothers who were not depressed and had an intended pregnancy also had a significantly lower RR (0.60) of returning to paid work than those who were not depressed and had an unintended pregnancy. |
| Faisal-Cury38 | Brazil Mean age: 25 years Gender of newborns: not given |
644 | Cohort study Approximately 2 years Four groups: - None - Pregnancy only - Postpartum only - Pregnancy and postpartum |
SRQ-20 | Pregnancy only: 15.2% Postpartum only: 12.1% Pregnancy and postpartum: 15.7% |
Sexual life | The mean time to the resumption of sexual activity during the postpartum period was 2.1 (range = 1–12) months. In the multivariable analysis after adjustment for wealth score, episiotomy, forceps delivery, previous pregnancies and marriage status, depression during pregnancy and postpartum (RR = 3.17, 95% CI = 2.18, 4.59), depression during only the postpartum period (RR = 3.45, 95% CI = 2.39, 4.98), a previous miscarriage, and patient age were significantly associated with sexual decline. |
| Khajehei74 | Australia Mean age: 29.8 years Female babies (%): FSD: 49.3 No FSD: 51.7 |
325 | Cross-sectional study Two groups: - FSD - No FSD |
PHQ-8 | FSD: 14.8% No FSD: 9.5% |
Sexual dysfunction during the first year after childbirth | Depression (OR = 2.876; 95% CI = 1.318, 6.276; p = 0.008) was a significant risk factor for sexual dysfunction during the first year after childbirth. |
| Lilja44 | Sweden Mean age: 27.8 years Gender of newborns: not given |
419 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
22.2% | Women’s mood over the first year postpartum; women’s relationship with their infant; women’s relationship with their partner | Mothers who scored high on the EPDS at 10 days postpartum tended to rate their relationship with their partner lower at all observations during the first year than mothers who had low EPDS scores on day 10. The same applied to the relationship between EPDS at day 3 and the relationship scales. Thus, mothers with a high score on the EPDS early in the postpartum period rated their relationship with their partner as more distant, cold and difficult, and felt less confident than mothers with low EPDS scores over the first year. |
| Posmontier85 | USA Mean age (years): No PPD: 31.0 ± 4.5 PPD: 30.0 ± 5.5 Female babies (%): No PPD: 78.3 PPD: 30.4 |
46 | Cross-sectional study Two groups: - PPD - No PPD |
MINI | Not applicable (number of PPD and no PPD women were
fixed at the beginning of the study)
Nondepressed: n = 23 Depressed: n = 23 |
Functional status (physical infant care, personal care, household care, social activities, and occupational activities) | Specifically, lower household, social, and personal functioning were correlated with PPD. In multiple regression analyses, PPD predicted lower overall functional status (p < 0.001), household function (p < 0.05), social function (p < 0.001), and personal function (p < 0.001). |
| Wang66 | Taiwan Age (years): Depressed: 28.34 ± 5.52 Nondepressed: 29.45 ± 4.13 Female babies: 55.0% |
60 | Cohort study 1 year Two groups: - PPD - No PPD |
BDI-II | 48.3% | Psychosocial health | Significant differences were found between the depressed and the nondepressed groups in depression, perceived stress, social support, and self-esteem. At 1 year after childbirth, women in the depressed group still suffered mild depression and reported greater perceived stress and lower perceived social support and self-esteem than women in the nondepressed group. |
| Vliegen37 | Belgium Mean age (years): T1: 29.39 ± 4.40 T2: 32.95 ± 4.51 Gender of newborns: not given |
41 | Cohort study 3.5 years Two groups: - PPD - No PPD |
BDI-II (Depressed = BDI ⩾ 13) |
39% | Maternal depression; treatment after hospitalization; life events; relationship | Currently depressed mothers reported having to move more often (92% vs 73%, ns) and having more relationship difficulties, including romantic break-ups (46% vs 35%, ns). |
FSD: female sexual dysfunction; PPD: postpartum depression; PDSS-SF: Postpartum Depression Screening Scale—Short Form; SRQ-20: Self-Reporting Questionnaire-20; PHQ-8: Patient Health Questionnaire depression module; EPDS: Edinburgh Postnatal Depression Scale; MINI: Mini International Neuropsychiatric Interview; BDI-II: Beck Depression Inventory-II; RR: risk ratio; CI: confidence interval; OR: odds ratio.
Social relationships
PPD was associated with more relationship difficulties37 and therefore with lower social function.85 Depressed mothers also presented lower (perceived) social support scores than nondepressed mothers.66 Regarding the probability of returning to paid work, one study showed that there was no difference between depressed and nondepressed mothers.73 The authors of this study specified that most mothers experienced depressive symptoms during the first year after childbirth; thus, depression was not an independent predictor of how quickly mothers would return to work.
Partner relationships and sexuality
Depressed mothers rated their relationship with their partner as more distant, cold and difficult, and felt less confident than nondepressed mothers over the first year after childbirth.44 Depressed mothers also reported having more relationship difficulties, including romantic break-ups, than nondepressed mothers; however, this difference was not significant.37 Regarding sexual life during the first year after childbirth, mothers who had resumed sexual activity had lower depression scores than mothers who did not resume sexual activity during the postpartum period.38 In addition, depression appeared to cause nearly three times more sexual dysfunction during the first year after childbirth.74
Risky behaviors
Addictive behavior
Three studies55,84,87 evaluated the influence of PPD on smoking behavior (Table 5). One study showed that smoking and depression often co-occurred among mothers during the postpartum period.87 The prevalence of PPD was higher among smokers than nonsmokers; conversely, smoking was also more common among mothers with a major depressive episode. The two other studies demonstrated that women who quit smoking during pregnancy might be more likely to relapse if they experience negative emotions or depressive symptoms.55,84 In addition, one study evaluated the influence of PPD on postpartum “risky” drinking at 3 months among women who were frequent drinkers before pregnancy.68 This study emphasized that there was no significant association between maternal PPD and risky drinking.
Table 5.
Characteristics of the studies included in the evaluation of the maternal risky behavior.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Addictive behavior | |||||||
| Allen84 | USA Age (years): <20: 15.3% 20–24: 37.8% 25–29: 27.0% >29: 19.9% Gender of newborns: not given |
2566 | Cross-sectional study Two groups: - PPD - No PPD |
Specific to the survey | 18.8% | Relapse of smoking during postpartum | Compared to women who did not experience postpartum depressive symptoms, women who did were 1.86 (95% CI = 1.31, 2.65) times as likely to relapse during the postpartum period. After adjusting for demographic characteristics, intensity of smoking, and time since delivery, the association decreased slightly (adjusted OR = 1.77, 95% CI = 1.21, 2.59). |
| Jagodzinski68 | USA Age (years): 18–25: 42.3% 26–35: 44.6% ⩾36: 12.3% Missing: 0.8% Gender of newborns: not given |
381 | Cross-sectional study (recruitment phase of a
randomized clinical trial) Two groups: - Low risk of drinking - At risk of drinking |
EPDS (Depressed = EPDS > 12) |
16.0% | Postpartum risky drinking | At 3 months postpartum, the risk of drinking was not significantly different between women who had an EPDS score >12 and women who had an EPDS score ⩽12 (adjusted OR (95% CI) = 1.1 (0.5, 2.5)). |
| Park55 | USA Mean age: 28.8 ± 6.1 years Gender of newborns: not given |
65 | Cohort study 22 weeks Two groups: - Smokers - Nonsmokers |
BDI | Not given Mean BDI: 5.8 ± 4.7 |
Postpartum relapse of smoking | In a regression model, the slope of BDI scores from baseline to the 12-week follow-up differed between nonsmokers and smokers (−0.12 vs +0.11 units/week, p = 0.03). The mean slope of BDI scores between baseline and 24 weeks postpartum decreased (−0.07 units/week) among nonsmokers and rose (+0.05 units/week) among those who smoked (p = 0.01). |
| Whitaker87 | USA Age (years): <20: 17.9% 20–29: 59.2% ⩾30: 22.9% Gender of newborns: not given |
4353 | Cross-sectional study Two groups: - PPD - No PPD |
CIDI-SF | 13.6% | Smoking behavior | After adjusting for sociodemographic characteristics, the prevalence (95% CI) of a major depressive episode was higher among smokers than nonsmokers: 17.7% (15.7, 19.8) vs 12.1% (10.9, 13.3). Smoking was also more common among mothers who had had a major depressive episode than among those who had not: 34.0% (30.6, 37.4%) vs 25.5% (24.1, 26.8%). |
| Suicidal ideation | |||||||
| Barr93 | Australia Age: between 20 and 34 years Gender of newborns: not given |
15 | Cross-sectional study (qualitative study)
One group: - PPD |
Not given | 100% | Thoughts of infanticide that did not lead to the act | Women who experienced nonpsychotic depression preferred not to disclose their thoughts of infanticide to health professionals, including trusted general practitioners or psychiatrists. These women were more likely to mention their suicidal thoughts than their infanticidal thoughts to obtain health care. |
| Do33 | USA Mean age: not given Gender of newborns: not given |
178,714 | Cohort study 6 years Four groups: Active component service women: - PPD - No PPD Dependent spouses: - PPD - No PPD |
ICD-9-CM | Active component service women: 9.9%
Dependent spouses: 8.2% |
Suicide attempt | Service women with PPD had higher odds of suicidality compared to service women without PPD (OR = 42.2, 95% CI = 28.8, 61.9). Dependent spouses with PPD also had higher odds of suicidality compared to dependent spouses without PPD (OR = 14.5, 95% CI = 10.8, 19.4). |
| Kim28 | USA Mean age (years): Suicidal ideation: 32.2 ± 6.3 No suicidal ideation: 32.2 ± 5.6 Gender of newborn: not given |
22,118 | Cohort study 23 weeks Two groups: - Suicidal ideation - No suicidal Ideation |
EPDS (Depressed = EPDS ⩾ 12) |
Not given | Suicidal ideation | Among 22,118 EPDS questionnaires studied, suicidal ideation was reported on 842 (3.8%, 95% CI = 3.5, 4.1) and was positively associated with pre-existing psychiatric diagnosis during the postpartum (12.0% compared with 5.8%, p = 0.001). Among perinatal women screened for depression, 3.8% reported suicidal ideation; 1.1% of this subgroup was at high risk of suicide. Multivariable postpartum models did not retain the PPD. |
| Paris81 | USA Mean age: 32.5 ± 5.6 years Gender of newborns: not given |
32 | Cross-sectional study Two groups: - Low suicidality - High suicidality |
PDSS | 100% | Suicidality (suicidal ideation) | Overall, women in this clinical sample had wide ranging levels of suicidal thinking. When divided into low and high suicidality groups, the mothers with high suicidality experienced greater mood disturbances and cognitive distortions, and more severe postpartum symptomatology. |
| Pope30 | UK Mean age: 29.0 ± 5.5 years Gender of newborns: not given |
147 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (use of item 10 on the EPDS referring to “thoughts of self-harm”) HDRS |
Not applicable (only women with MDD (64%) or bipolar disorder (36%) were included in the study) |
Thoughts of self-harm; suicidal ideation | Women with suicidal ideation were more likely to have higher levels of depression than women without suicidal ideation (EPDS: 21.5 vs 9.9, p = 0.03; HDRS: 18.6 vs 7.73, p = 0.04). Women with thoughts of self-harm were more likely to have higher levels of depression than women without thoughts of self-harm (EPDS: 16.4 vs 9.5, p = 0.04; HDRS: 13.0 vs 7.5, p = 0.05). Women with hypomanic symptoms during the postpartum period were also more likely to have thoughts of self-harm or suicidal ideation. |
| Posmontier85 | USA Mean age (years): No PPD: 31.0 ± 4.5 PPD: 30.0 ± 5.5 Female babies (%): No PPD: 78.3 PPD: 30.4 |
46 | Cross-sectional study Two groups: - PPD - No PPD |
MINI | Not applicable (number of PPD and no PPD women were
fixed at the beginning of the study)
Nondepressed: n = 23 Depressed: n = 23 |
Functional status (physical infant care, personal care, household care, social activities, and occupational activities) | Depressed mothers presented more suicidal thoughts (6.52, SD = 3.64) than nondepressed mothers (4.25, SD = 0.25, p < 0.01). |
| Tavares76 | Brazil Age (years): 13–19: 20.0% 20–34: 69.9% 35–45: 10.1% Gender of newborns: not given |
919 | Cross-sectional study Two groups: - PPD - No PPD |
MINI | 8.5% | Suicide risk | Lower education levels and psychiatric disorders were associated with suicide risk. The mothers who experienced depressive episodes had a 12.6 (95% CI = 7.0, 22.6) times greater risk of presenting with suicidal signs. Women who had hypomanic episodes were 7.01 (95% CI = 3.54, 13.9) times more likely to show signs of suicide risk compared to those without hypomanic episodes. Bipolar disorder was the psychiatric disorder with the highest impact on suicide risk. |
PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; CIDI-SF: Composite International Diagnostic Interview—Short Form; ICD-9-CM: International Classification of Diseases, Ninth Revision, Clinical Modification; PDSS: Postpartum Depression Screening Scale; HDRS: Hamilton Depression Rating Scale; MINI: Mini International Neuropsychiatric Interview; MDD: maternal major depressive disorder; OR: odds ratio; CI: confidence interval; SD: standard deviation.
Suicidal ideation
Five studies showed that higher levels of depressive symptoms were associated with an increased prevalence of suicidal ideation30,33,76,81,85 (Table 5). Mothers with high suicidality risks experienced greater mood disturbances and more severe postpartum symptomatology than mothers with low suicidality risks.81 One of the five studies also demonstrated that women who reported higher levels of depression were also significantly more likely to report thoughts of self-harm than women with low levels of depression.30 The sixth study28 showed a significant association between PPD and suicidal ideation in an unadjusted analysis, but not in adjusted analysis. An additional study demonstrated that mothers who experienced PPD could imagine acts of infanticide.93 The authors of this study explained that many mothers preferred to describe their suicidal thoughts rather than their infanticidal thoughts when seeking health care.
Infant consequences of PPD
Anthropometry
The characteristics and main results of the studies included in the evaluation of anthropometric parameters are presented in Table 6.
Table 6.
Characteristics of the studies included in the evaluation of infant anthropometric outcomes.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Adewuya119 | Nigeria Mean age: not given Gender of newborns: not given |
242 | Cohort study 8 months Two groups: - PPD - No PPD |
SCID-NP | 49.6% | Infants’ physical growth (weight and length); cases of diarrhea and other childhood illnesses in infants; breastfeeding | The differences in weight and length gradually increased starting at the 6th week, peaked at the 6th month, and declined afterwards. |
| Avan110 | South Africa Age (years): <35: 91.5% ⩾35: 8.5% Female babies: 49.9% |
1035 | Cohort study 18 months Two groups: - PPD - No PPD |
Pitt Inventory | 24.0% | Child growth; child behavioral problems (Richman Child Behavior Scale) | Two-year-old children with depressed mothers had an increased risk of stunted growth compared to those with nondepressed mothers. |
| Bakare140 | Nigeria Mean age: 28.2 ± 5.1 years Female babies: 47.8% |
408 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 9) |
24.8% | Weight; length; head circumference | Maternal PPD was significantly associated with infants’ weight and length, but not their head circumference. |
| Ertel109 | USA Mean age: 33.0 ± 4.5 years Female babies: 52.3% |
872 | Cohort study 3 years Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
7.3% | Height and linear growth | Exposure to PPD was associated with a greater height-for-age z-score and longer leg length starting at 6 months and continuing to age 3 years. |
| Ertel112 | USA Mean age: 33.0 ± 4.46 years Female babies: 52.2% |
838 | Cohort study 3.5 years Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
7.04% | BMI z-score; WHZ; sum of SS and TR skinfold thickness for overall adiposity; sum of SS and TR skinfold thickness ratio for central adiposity | In multivariable models, PPD was only associated with a higher sum of SS and TR skinfold thickness (SS + TR) for overall adiposity (adjusted OR (95% CI) = 1.14 (0.11, 2.18)), but this association was not significant. The results for other outcomes showed very small effect estimates. For example, regarding the association between PPD and child WHZ, the estimated associations were similar for each age from 6 months to 3 years: 0.08 (95% CI = −0.14, 0.30) when controlling for child sex and age at assessment, maternal age, race/ethnicity, household income, pre-pregnancy BMI, pregnancy weight gain, gestational diabetes or impaired glucose intolerance, gestational age at delivery, and birthweight-for-gestational age. |
| Ertel100 | The Netherlands Mean age: 30.3 ± 5.24 years Female babies: 49.5% |
6782 | Cohort study 41 months Two groups: - PPD - No PPD |
BSI | 8.25% at 2 months 8.85% at 6 months |
Child overweight | There was no association between perinatal depression and child BMI at any time point. |
| Gress-Smith104 | USA Mean age: 26.5 ± 5.59 years Gender of newborns: not given NB: very low-income population |
132 | Cohort study 9 months Three groups: - No PPD - Significant levels of depressive symptoms (CES-D ⩾ 16) - Severe depressive symptoms (CES-D ⩾ 24) |
CES-D | 5 months: 33% of depressive symptoms; 12% of severe
depressive symptoms 9 months: 38% of depressive symptoms; 18% of severe depressive symptoms |
Infant weight; infant health; infant sleep | Higher depressive symptoms at 5 months postpartum were associated with less infant weight gain from 5 to 9 months. |
| Grote113 | Belgium, Germany, Italy, Poland, Spain Age (years): <28: 27.3% 28 ⩽ 33: 39.1% 33–44: 33.6% Female babies: 51.7% |
929 | Cohort study 2 years Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
11.0% | Weight; length; TR skinfold thickness; SS skinfold thickness; weight for length | Infant weight, length, and BMI at 24 months of age did not differ between high and normal EPDS groups. TR skinfold thickness and SS skinfold thickness did not differ between the two groups. |
| Kalita131 | India Age (years): Depression: 28.2 ± 0.93 Anxiety: 29.8 ± 1.68 Not diagnosed: 28.3 ± 1.28 Female babies: 52.0% |
100 | Cohort study 6 months Three groups: - PPD - Anxiety - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
18.0% | Weight; communication; symbolic behaviors | Infants with mothers suffering from PPD had significantly lower weights at 6 months of age compared to infants born to mothers who did not suffer from PPD. |
| Nasreen97 | Bangladesh Mean age: 24.2 ± 6.7 years Female babies: 50.7% |
652 | Cohort study 1 year Four groups: - No depression - PPD during pregnancy only - PPD during pregnancy and postpartum - PPD during postpartum only |
EPDS (Depressed = EPDS ⩾ 10) |
14.1% at 2–3 months 31.7% at 6–8 months |
Infant’s growth (underweight at 6–8 months, stunting at 6–8 months); infant’s motor development | Maternal depressive symptoms at 2–3 months postpartum were associated with infant underweight at age 6–8 months. No significant association was found between maternal postpartum depressive symptoms at 2–3 months and infant stunting at 6–8 months. |
| Ndokera142 | Zambia Age (years): ⩽18: 9% 19–24: 35.6% 25–30: 33.1% ⩾31: 22.3% Female babies: 45.3% |
278 | Cross-sectional study Two groups: - PPD - No PPD |
SRQ-20 | 9.7% | Weight; length; diarrheal episodes; incomplete vaccination | Infants of depressed mothers were lighter and shorter than infants of nondepressed mothers after adjustment for age, gender, and maternal weight. |
| Tomlinson126 | South Africa Age (years): <20: 15.3% 20–24: 26.5% 25–29: 32.7% 30–39: 25.5% Female babies: 44.9% |
147 | Cohort study 18 months Two groups: - PPD - No PPD |
SCID | 34.7% at 2 months 12% at 18 months |
Infant weight; infant length | There were no significant relationships at 2 and 18 months between maternal depression and mean standardized infant weight or length. |
| Wright125 | UK Mean age: not given Gender of newborns: not given |
915 (923 infants) |
Cohort study 13 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
12.0% | Overall infant weight gain; weight faltering | Infants of depressed mothers showed slower overall weight gain and an increased rate of weight faltering from birth to 4 months. However, over the 12-month period, there was no difference in weight gain between the infants of depressed and nondepressed mothers. |
PPD: postpartum depression; CES-D: Center for Epidemiologic Studies Depression Scale; SCID-NP: Structured Clinical Interview for DSM-IV, Non-Patient edition; EPDS: Edinburgh Postnatal Depression Scale; BSI: Brief Symptom Inventory; SRQ-20: Self-Reporting Questionnaire-20; BMI: body mass index; WHZ: weight-for-height z-score; SS: subscapular; TR: triceps; OR: odds ratio; CI: confidence interval.
Weight
A total of 11 studies reported weight as an outcome. Among them, five studies97,104,131,140,142 demonstrated a significant effect of maternal PPD on the child’s weight; infants of depressed mothers gained less weight than infants of nondepressed mothers. Four studies were conducted in low-resource countries (India,131 Nigeria,140 Zambia,142 and Bangladesh97), and one study was conducted in the United States with a very low-income population.104 Two other studies (one in the United Kingdom125 and one in Nigeria119) showed that while there were differences in infant weight in the first months of life, they did not persist. Finally, four studies demonstrated that maternal PPD had no effect100,113,126 or a very small effect112 on the child’s weight. Two studies were conducted in high-income countries (a multicountry study that included Belgium, Germany, Italy, Poland, and Spain113 and one study conducted in the Netherlands100). The third study126 was conducted in South Africa; however, the authors stated that they were unable to test their hypothesis due to a lack of statistical power.
Length
Eight studies identified in this systematic review reported infant length as an outcome. Three of the studies110,140,142 showed a significant effect of maternal PPD on stunting. The three studies were conducted in low-resource countries (Nigeria,140 Zambia,142 and South Africa110). One other study119 showed differences in length in the first months of life; however, it was determined that these differences did not persist over time (Nigeria). Three other studies97,113,126 demonstrated that maternal PPD had no effect on stunting. One multicountry study113 evaluated high-income countries (Belgium, Germany, Italy, Poland, and Spain), and two studies were conducted in low-income countries, including Bangladesh97 and South Africa.126 The authors of the South African study stated that they were unable to test their hypothesis due to a lack of statistical power. Another study109 conducted in a high-income country (the United States) showed the opposite effect: exposure to PPD was associated with a greater height-for-age z-score and a longer leg length.
Anthropometric indices
Four studies evaluated anthropometric indices, and two of them showed no effect of maternal PPD. One study140 found that maternal PPD was not associated with head circumference (Nigeria). Two studies demonstrated that the triceps and subscapular skinfold thicknesses did not differ between infants of depressed and nondepressed mothers (one study was conducted in Belgium, Germany, Italy, Poland, and Spain;113 the other was from the United States112). In contrast, one study from the United States109 showed that PPD was associated with higher subscapular and triceps skinfold thickness scores, which indicated overall adiposity.
Infant health
Of the 10 cohort studies, 9 indicated a significant association between maternal PPD and health concerns in infants (Table 7). Maternal depressive symptoms at 5 months seemed to predict more overall physical health concerns for infants at 9 months104 and a greater proportion of childhood illnesses.119 Three studies showed that infants of depressed mothers had significantly more diarrheal episodes per year than those of nondepressed mothers,119,122,138 and one study reported that infants of depressed mothers had more days of illness with diarrhea.138 Harriet et al. specified that these associations with diarrheal episodes were accurate only within the first 3 months. One study also associated maternal depressive symptoms with infant colic.124 Two studies reported greater overall pain in the infants of depressed mothers48 and a stronger infant pain response during routine vaccinations.123 One study demonstrated that maternal PPD at 4 months predicted worse health-related quality of life for the infant in the following months.48 One study indicated a robust and predictive association between maternal PPD and febrile disease in children.135 Another study136 showed that probable postnatal depression was associated with an approximately three-fold increased risk of mortality in infants up to 6 months of age, with an approximately two-fold increased risk of mortality up to 12 months of age. This study also showed that probable postnatal depression was associated with an increased risk of infant morbidity. Only one cross-sectional study reported a nonsignificant association between a high risk of maternal depression and serious illness or diarrheal episodes after adjusting for infant age and other possible confounders.142 Nevertheless, the occurrence of these two outcomes was proportionally higher among infants of depressed mothers.
Table 7.
Characteristics of the studies included in the evaluation of infant health.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Adewuya119 | Nigeria Mean age: not given Gender of newborns: not given |
242 | Cohort study 8 months Two groups: - PPD - No PPD |
SCID-NP | 49.6% | Infant physical growth (weight and length); cases of diarrhea and other childhood illnesses in the infants; breastfeeding | By the 9th month, the average number of cases of diarrhea and other childhood illnesses in the infants of depressed mothers was 5.23 (SD = 2.37), while the average number of those illnesses in infants of nondepressed mothers was 3.70 (SD = 4.14). The difference was statistically significant (p = 0.001). |
| Akman124 | Turkey Age (years): Infant colic+: 31.1 ± 6.0 Infant colic−: 29.6 ± 4.8 Female babies: 50.0% |
78 | Cohort study 6 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
12.9% | Infant colic | Infant colic was present in 17 infants (21.7%), and 12.9% of the mothers had an EPDS score >13. The mean EPDS score of mothers whose infants had infant colic (10.2 ± 6.0) was significantly higher than that of mothers of infants without colic (6.3 ± 4.0). |
| Darcy48 | USA Mean age: 30.3 years Gender of newborns: not given |
217 | Cohort study 1 year Two groups: - PPD - No PPD |
CES-D | 32.7% | Infant health-related quality of life (pain/discomfort and health-related concerns) | Mothers with significant depressive symptoms reported greater pain in their infant and had more health-related concerns about their child. Maternal depressive symptoms at 4 months predicted poorer health-related quality of life for the infant at 8, 12, and 16 months. |
| Gress-Smith104 | USA Mean age: 26.5 ± 5.59 years Gender of newborns: not given NB: very low-income population |
132 | Cohort study 9 months Three groups: - No PPD - Significant levels of depressive symptoms (CES-D ⩾ 16) - Severe depressive symptoms (CES-D ⩾ 24) |
CES-D | 5 months: 33% of depressive symptoms; 12% of severe
depressive symptoms. 9 months: 38% of depressive symptoms; 18% of severe depressive symptoms. |
Infant weight; infant health; infant sleep | Maternal depressive symptoms at 5 months predicted more physical health concerns in the infants at 9 months (B = 0.05, SE = 0.03, p < 0.05). |
| Guo135 | Côte d’Ivoire, Ghana Mean age: 29.1 ± 5.4 years Female babies: 48.9% |
654 | Cohort study 2 years Two groups: - PPD - No PPD |
PHQ-9 | 3 months: 11.8% in Côte d’Ivoire; 8.9% in Ghana.
12 months: 16.1% in Côte d’Ivoire; 7.2% in Ghana. |
Febrile illness | The hazard of febrile disease in children of depressed mothers was 57% higher than the hazard in children of nondepressed mothers. Country and SES were identified as confounders. After adjusting for both, the hazard of developing a febrile illness was 32% higher in children whose mothers had depression than in children whose mothers did not have depression. The authors constructed a cumulative depression exposure by categorizing the mothers as “never depressed” or “depressed one time” and “depressed 2 or 3 times.” The crude and adjusted hazard ratios for children of recurrently depressed mothers compared to those for children of mothers with fewer episodes of depression were 2.20 (95% CI = 1.51, 3.19) and 1.90 (95% CI = 1.32, 2.75), respectively. |
| Harriet138 | Ghana Mean age: 28.5 ± 0.3 years Gender of newborns: not given NB: HIV-infected mothers |
552 | Cohort study 12 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
10.0% | Diarrhea | In the first 3 months of life, infants of mothers who reported PND symptoms had almost twice the number of diarrheal episodes (p = 0.0005) and more than twice as many days ill with diarrhea (p = 0.0002) compared to infants whose mothers reported no PND symptoms. No significant association was observed after 3 months. |
| Moscardino123 | Italy Mean age: 33.3 ± 5.1 years Female babies: 50.0% |
28 | Cohort study 2.5 months Two groups: - PPD - No PPD |
EPDS (cut-off value not given) |
Not given (mean EPDS score = 7.5) | Infant response to vaccination | Higher levels of depressed maternal mood were predictive of a stronger infant pain response to routine vaccination. Infants exhibiting a stronger pain response during the inoculation procedure at 4.5 months were more likely to have mothers who reported higher levels of depressed mood at 2 months (p = 0.032) and at 4.5 months (p = 0.016). The mothers’ PND at 2 months was only marginally related to the infant pain response (p = 0.086). |
| Ndokera142 | Zambia Age (years): ⩽18: 9% 19–24: 35.6% 25–30: 33.1% ⩾31: 22.3% Female babies: 45.3% |
278 | Cross-sectional study Two groups: - PPD - No PPD |
SRQ-20 | 9.7% | Weight; length; diarrheal episodes; incomplete vaccination | All outcomes were proportionally higher among the infants of “depressed” mothers, although none of these differences were statistically significant. Logistic regression analysis to adjust for infant age and other possible confounders showed no significant association between a high risk of maternal depression and serious illness or diarrheal episodes. |
| Rahman122 | Pakistan Mean age: 26.0 years Female babies: 49.8% |
265 | Cohort study 1 year Two groups: - PPD - No PPD |
Schedules for Clinical Assessment in Neuropsychiatry developed by the WHO | 49.1% | Diarrheal illness | Infants of depressed mothers had significantly more diarrheal episodes per year than those in the control group. The RR of having >5 diarrheal episodes per year in infants of depressed mothers was 2.3 (95% CI = 1.6, 3.1). The association remained significant after other risk factors were adjusted by a multivariate analysis (RR = 3.1; 95% CI = 1.8, 5.6; p < 0.01). |
| Weobong136 | Ghana Mean age: not given Gender of newborns: not given |
16,560 | Cohort study 6 months Two groups: - PPD - No PPD |
PHQ-9 | 3.5% | Infant mortality; infant morbidity | All-cause infant mortality from the time of the PND assessment up to 6 months of age (adjusted RR = 2.86, 95% CI = 1.58, 5.19) was almost three times higher for infants of depressed mothers compared to those whose mothers were not depressed, and there was almost a two-fold increase in all-cause infant mortality up to 12 months of age (adjusted RR = 1.88, 95% CI = 1.09, 3.24). Among the potential confounders included in the model, only time of delivery (preterm) was also associated with an almost five-fold increased risk of infant deaths up to 6 months of age (adjusted RR = 4.61, 95% CI = 2.02, 10.51). An increased risk of infant morbidity indicators was associated with probable PND. |
PPD: postpartum depression; CES-D: Center for Epidemiologic Studies Depression Scale; SCID-NP: Structured Clinical Interview for DSM-IV, Non-Patient edition; EPDS: Edinburgh Postnatal Depression Scale; PHQ-9: Patient Health Questionnaire depression module; SRQ-20: Self-Reporting Questionnaire-20; WHO: World Health Organization; SD: standard deviation; CI: confidence interval; SES: socioeconomic status; PND: postnatal depression; RR: risk ratio.
Infant sleep
Three studies evaluated the association between maternal depressive symptoms and infant sleep patterns (Table 8). Two studies showed that higher depressive symptoms were associated with an increased incidence of infant night-time awakenings and predicted more problematic infant sleep patterns.104,108 One of the two studies demonstrated that children whose mothers had severe and/or chronic depressive symptoms had a higher risk of sleep disorders than those with mothers who had mild depressive symptoms.108 The third study reported that significantly fewer children of mothers with depressive symptoms were placed in the recommended back-to-sleep position compared with children of women who had not experienced depression.130
Table 8.
Characteristics of the studies included in the evaluation of infant sleep.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Gress-Smith104 | USA Mean age: 26.5 ± 5.59 years Gender of newborns: not given NB: very low-income population |
132 | Cohort study 9 months Three groups: - No PPD - Significant levels of depressive symptoms (CES-D ⩾ 16) - Severe depressive symptoms (CES-D ⩾ 24) |
CES-D | 5 months: 33% of depressive symptoms; 12% of severe
depressive symptoms 9 months: 38% of depressive symptoms; 18% of severe depressive symptoms |
Infant weight; infant health; infant sleep | Higher depressive symptoms at 5 months were associated with increased infant night-time awakenings at 9 months (p = 0.001). A multinomial logistic regression analysis was performed to investigate the relationship between maternal depressive symptoms at 5 months and infant sleep at 9 months while controlling for infant sleep at 5 months. Maternal depressive symptoms at 5 months significantly predicted more problematic infant sleep at 9 months (B = 0.03, p = 0.01). |
| Tavares Pinheiro108 | Brazil Mean age: 26.2 ± 6.6 years Gender of newborns: not given |
366 | Cohort study 10 months Two groups: - PPD - No PPD |
EPDS (mild = 10–12; severe ⩾ 13) |
22.7% in direct PP 24.6% at 12 months |
Infant sleep disorders | The risk of sleep problems for children whose mothers presented with a new onset and severe depression at 12 months was higher than the risks observed among children born to mildly depressed mothers. When chronicity was considered, an additional risk of 2.20 (95% CI = 0.62, 7.86) was observed for mild and chronically depressed mothers, which was even higher (2.58; 95% CI = 1.15, 5.63) for chronic and severe cases. Moreover, a linear trend toward a higher risk of sleep problems as the severity and chronicity of the mother’s depressive symptoms increased could be observed (p = 0.05). |
| Zajicek-Farber130 | USA Age (years): Depressed: 22.3 ± 4.3 Nondepressed: 22.6 ± 3.9 Female babies: 54.0% |
134 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 11) PHQ |
55.2% | Infant health practices | Significantly fewer children of depressed women were placed in the recommended back-to-sleep position compared to children of women who had never experienced depression (68.9% vs 85.0%). The RR of sleeping in a “wrong” position was two times greater for children of depressed women than those of women who were never depressed. |
PPD: postpartum depression; CES-D: Center for Epidemiologic Studies Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; PHQ: Patient Health Questionnaire; CI: confidence interval; RR: risk ratio.
Motor development
Three of seven studies showed a significant effect of maternal PPD on the motor development of infants (Table 9). The first study,97 conducted in Bangladesh, showed that symptoms of maternal PPD that were present at 2–3 months predicted impaired motor development in infants at 6–8 months. The second study95 included Greek mothers in Crete and demonstrated that symptoms of maternal PPD were associated with lower fine motor scores in infants at 18 months of age (a 5-unit decrease on the scale of fine motor development). The third study94 showed a nonsignificant impact of maternal depression on the fine and gross motor development of children at 2 and 6 months that became significant at 12 months for gross motor development and at 18 months for fine motor development (Pakistan). The fourth study141 underlined the indirect effect of maternal PPD on motor development as a consequence of the effects of maternal depressive symptoms on the quality of the home environment. This mechanism had a direct effect on early child development. Three studies66,103,107 demonstrated that maternal PPD had no effect on motor development (Table 9). Two studies66,107 explained the nonsignificant results by stating that most of the mothers in the depressed group had moderate-to-severe depression symptoms that were similar to a general description of psychological difficulty during the postnatal period and were less severe than a psychiatric diagnosis of a depressive illness (France and Taiwan). The third study103 emphasized that the home environment remained a significant predictor of infant development in Australia.
Table 9.
Characteristics of the studies included in the evaluation for motor development in children.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Ali94 | Pakistan Mean age: 26.3 years Female babies: 48.8% |
420 | Cohort study 30 months Two groups: - PPD - No PPD |
AKUADS | 1 month: 4.8% 2 months: 4.7% 6 months: 5.7% 12 months: 9.2% 18 months: 2.7% 24 months: 6.1% |
Delayed gross motor, fine motor, emotional, cognitive, and language development | At the 2- and 6-month follow-ups, there was no significant impact of maternal depression on children’s gross motor development. However, there was an approximately three-fold higher impact at the 12-month follow-up (adjusted OR = 2.8, 95% CI = 1.2, 6.6). At the 2-, 6-, and 12-month follow-ups, there was no significant impact of maternal depression on children’s fine motor development. At the 18-month follow-up, there was a significant impact; children of depressed mothers had a four times higher risk (adjusted OR = 4.0, 95% CI = 1.4, 11.3). |
| Chen141 | Taiwan Mean age: 26.6 ± 4.2 years Female babies: 42.6% NB: immigrant mothers |
60 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
31.1% | Child development (global score for cognitive, language, motor, self-regulation, and social development); quality of the home environment | Maternal depressive symptoms had a direct and negative effect on the quality of the home environment (−0.32, p < 0.05). Maternal depressive symptoms did not have a direct effect on child development (0.05, p > 0.05). The quality of the home environment had a significant and positive effect on child development (0.55, p < 0.001). |
| Koutra95 | Crete Mean age: 30.09 ± 4.53 years Female babies: 45.5% |
470 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
Not given | Fine motor, gross motor, cognitive, and social-emotional development; receptive and expressive communication | High levels of maternal PPD (EPDS score ⩾ 13) were associated with 5-unit decrease in the fine motor development scale score at 18 months of age. |
| Nasreen97 | Bangladesh Mean age: 24.2 ± 6.7 years Female babies: 50.7% |
652 | Cohort study 1 year Four groups: - No depression - Pregnancy only - Pregnancy and postpartum - Postpartum only |
EPDS (Depressed = EPDS ⩾ 10) |
14.1% at 2–3 months 31.7% at 6–8 months |
Infant growth (underweight at 6–8 months, stunting at 6–8 months); infant motor development | Maternal depressive symptoms at 2–3 months postpartum predicted impaired infant motor development at 6–8 months. |
| Piteo103 | Australia Age: not given Female babies: 53% |
360 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
19% | Motor, cognitive, and language development | In the first 6 months postpartum, there were no significant associations between maternal depression and motor development after controlling for infant prematurity, breastfeeding status, and socioeconomic level. There were no significant differences between maternal depression groups for motor development at 18 months based on unadjusted analyses. However, the home environment was a significant predictor of language development. |
| Sutter-Dallay107 | France Mean age: 29.6 ± 4.2 years Female babies: 47.8% |
515 | Cohort study 2 years Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
6 weeks: 4.7% 3 months: 4.5% 6 months: 4.3% 12 months: 3.7% 18 months: 5.8% 24 months: 4.3% |
Psychomotor Developmental Index; Mental Developmental Index | No association was found between PND 6 weeks after delivery and the child’s motor performance over the follow-up period. No association was found between EPDS scores and motor scores (B = 0.60, p = 0.24). |
| Wang66 | Taiwan Age (years): Depressed: 28.34 ± 5.52 Nondepressed: 29.45 ± 4.13 Female babies: 55.0% |
60 | Cohort study 1 year Two groups: - PPD - No PPD |
BDI-II | 48.3% | Gross motor, fine motor, expressive language, comprehension-conceptual, situational help, self-help, personal-social, and general development | No significant difference was found between the infant development variables in the two groups (gross motor development: p = 0.514; fine motor development: p = 0.514). |
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; BDI-II: Beck Depression Inventory-II; CI: confidence interval; OR: odds ratio; PND: postnatal depression.
Cognitive development
Of the 11 studies, 794,95,99,101,102,107,147 indicated a significant and negative association between maternal postpartum depressive symptoms and cognitive development in children (Table 10). One of the studies147 specifically emphasized the important role of maternal insensitivity in delays in children’s cognitive development. The eighth study141 underlined the indirect effect of maternal PPD on cognitive development, which occurred as a result of maternal depressive symptoms that impacted the quality of the home environment and had a direct effect on early child development. Three studies103,134,139 showed that maternal PPD was not significantly correlated with children’s cognitive development. One of the studies found a nonsignificant effect of maternal PPD and indicated that the home environment was a more important predictor of infant cognitive development in Australia.103
Table 10.
Characteristics of the studies included in the evaluation of child cognitive development.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborn |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Ali94 | Pakistan Mean age: 26.3 years Female babies: 48.8% |
420 | Cohort study 30 months Two groups: - PPD - No PPD |
AKUADS | 1 month: 4.8% 2 months: 4.7% 6 months: 5.7% 12 months: 9.2% 18 months: 2.7% 24 months: 6.1% |
Delayed gross motor, fine motor, emotional, cognitive, and language development | At the 2-month follow-up, maternal depression showed no significant impact on children’s cognitive development. However, the impact of maternal depression on delayed cognitive development of the child was approximately three-fold at the 6-month follow-up (adjusted OR = 3.3, 95% CI = 1.1, 9.9) and approximately seven-fold at the 12-month follow-up (adjusted OR = 6.8, 95% CI = 3.0, 15.7). |
| Azak99 | Norway Mean age: 64.3 years Female babies: 50% |
50 | Cohort study 1 year Two groups: - PPD - No PPD |
CES-D | Not applicable (number of PPD and no PPD women were
fixed at the beginning of the study)
Nondepressed: n = 24 Depressed: n = 26 |
Trajectories of cognitive development | Maternal depression was significantly related to the MSEL composite score. Infants of depressed mothers had a stable lower cognitive score over a 12-month period (6–18 months of age) compared to infants of nondepressed mothers. Over the same time period, girls tended to show a greater increase in cognitive scores compared to boys. |
| Chen141 | Taiwan Mean age: 26.6 ± 4.2 years Female babies: 42.6% NB: immigrant mothers |
60 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
31.1% | Child development (global score for cognitive, language, motor, self-regulation, and social development); quality of the home environment | Maternal depressive symptoms had a direct and negative effect on the quality of the home environment (−0.32, p < 0.05). Maternal depressive symptoms did not have a direct effect on child development (0.05, p > 0.05). The quality of the home environment had a significant and positive effect on child development (0.55, p < 0.001). |
| Evans134 | UK Age (years): Depressed: 28.0 ± 5.3 Nondepressed: 28.6 ± 4.7 Female babies: 48.4% |
6735 | Cohort study 33 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
13.1% | Cognitive development | After multiple imputations for missing data, there was no effect of PND on child IQ independent of depression that may have occurred at other times. |
| Kaplan102 | USA Mean age: 29.9 ± 5.1 years Female babies: 45.7% |
97 | Cohort study 8 months Two groups: - PPD - No PPD |
BDI-II DSM-IV |
4 months: 42.3% (BDI-II) 12.4% (DSM-IV) 12 months: 17.5% (BDI-II) 2.1% (DSM-IV) |
Cognitive development; ability to associate a face with a segment of an unfamiliar nondepressed mother’s infant-directed speech | At 4 months, all infants learned the voice–face association. At 12 months, even though none of the mothers were still clinically depressed, the average infant of mothers with chronically elevated self-reported depressive symptoms or elevated self-reported depressive symptoms at 4 months, but not 12 months, did not learn the association. For infants of mothers diagnosed with depression who were in remission, learning at 12 months was negatively correlated with the postpartum duration of the mother’s depressive episode. |
| Kaplan139 | USA Mean age: 29.9 ± 5.2 years Female babies: 56.0% |
91 | Cross-sectional study Two groups: - PPD - No PPD |
BDI-II | 33.0% | Cognitive development; language development (receptive and expressive communication) | BDI-II scores did not significantly correlate with cognitive scale percentiles (p > 0.10). |
| Kaplan147 | USA Mean age: 30.9 years Female babies: 57.6% |
136 (165 infants) |
Cross-sectional study Two groups: - PPD - No PPD |
BDI-II | 14.7% | Infant learning | Current depression diagnosis accounted for a significant proportion of the variance in infant learning. After the effects of maternal depression were accounted for, there was a significant effect of maternal hostility (p = 0.01). Finally, there was a further significant effect of maternal sensitivity (p = 0.02); after this effect was accounted for, the effects of maternal hostility were no longer significant (p = 0.16), but the effect of maternal depression remained significant (p < 0.05). Both maternal depression and maternal insensitivity negatively and additively predicted poor learning. |
| Koutra95 | Crete Mean age: 30.09 ± 4.53 years Female babies: 45.5% |
470 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
Not given | Fine motor, gross motor, cognitive, and social-emotional development; receptive and expressive communication | High levels of maternal PPD (defined as an EPDS score ⩾13) were associated with 5.6-unit decrease in the cognitive development scale (B = −5.64, 95% CI = −9.56, –1.72). |
| USA Mean age at birth: 32.6 ± 5.8 Female babies: 50.4% NB: mothers of preterm infants (<35 weeks) |
137 | Cohort study 12 months Two groups: - PPD - No PPD |
CES-D (Depressed = CES-D ⩾ 16) |
20.4% | Infant cognitive function | PND at 4 months was associated with lower cognitive function in children at 16 months after controlling for a host of socioeconomic characteristics (mean difference = −5.22, 95% CI = −10.19, −0.25). Being female and in a household with a family income greater than $60,000 was associated with higher cognitive function. There appeared to be a maternal support gradient in infant cognitive function for mothers with fewer depressive symptoms. That is, among mothers with fewer depressive symptoms, more maternal support was associated with higher cognitive function. Among mothers with elevated depressive symptoms, the maternal support slope was relatively flat. | |
| Piteo103 | Australia Age: not given Female babies: 53% |
360 | Cohort study 17 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
19% | Motor, cognitive, and language development | There were no significant associations between maternal depression in the first 6 months postpartum and cognitive development after controlling for infant prematurity, breastfeeding status, and socioeconomic level. However, home environment was a significant predictor of language development. |
| Sutter-Dallay107 | France Mean age: 29.6 ± 4.2 years Female babies: 47.8% |
515 | Cohort study 2 years Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
6 weeks: 4.7% 3 months: 4.5% 6 months: 4.3% 12 months: 3.7% 18 months: 5.8% 24 months: 4.3% |
Psychomotor Developmental Index; Mental Developmental Index | Children of mothers with a 6-week PND were significantly more likely than children of nonsymptomatic mothers to have a poor cognitive outcome. |
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; CES-D: Center for Epidemiologic Studies Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; BDI-II: Beck Depression Inventory-II; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.);
OR: odds ratio; CI: confidence interval; MSEL: Mullen Scales of Early Learning; PND: postnatal depression.
Language development
A series of different variables may be used to assess language development. Across all studies included in the review (Table 11), language development was evaluated using the following measures: overall language development,94,103,105,117 expressive and receptive communication,66,95,102,139 parent-to-child reading,116 composite speech,131 and literacy and enrichment literacy activities combined with an understanding of vocabulary and production.132
Table 11.
Characteristics of the studies included in the evaluation of child language development.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborn |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Ali94 | Pakistan Mean age: 26.3 years Female babies: 48.8% |
420 | Cohort study 30 months Two groups: - PPD - No PPD |
AKUADS | 1 month: 4.8% 2 months: 4.7% 6 months: 5.7% 12 months: 9.2% 18 months: 2.7% 24 month: 6.1% |
Delayed gross motor, fine motor, emotional, cognitive, and language development | There was a significant interaction between a mother’s depression and her husband’s income. Among women whose husband’s income was ⩾3500 rupees/month, there was no significant impact of maternal depression on children’s language development. Children of depressed mothers whose husband’s income was <3500 rupees/month had more than a five-fold risk of delayed language development relative to children whose mothers were not depressed and whose father’s income was ⩾3500 rupees/month (adjusted OR = 5.4, 95% CI = 2.3, 12.4). |
| Chen141 | Taiwan Mean age: 26.6 ± 4.2 years Female babies: 42.6% NB: immigrant mothers |
60 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
31.1% | Child development (global score for cognitive, language, motor, self-regulation, and social development); quality of the home environment | Maternal depressive symptoms had a direct and negative effect on the quality of the home environment (−0.32, p < 0.05). Maternal depressive symptoms did not have a direct effect on child development (0.05, p > 0.05). The quality of the home environment had a significant and positive effect on child development (0.55, p < 0.001). |
| Friedman129 | USA Mean age: 28.8 ± 6.58 years Female babies: 42.6% |
122 | Cohort study 4 months Two groups: - PPD - No PPD |
CES-D | 26.2% | Infant vocal affect qualities | Maternal depression was a predictor of less silence and accounted for 3.5% of the variability in silence (B = −0.186). Depression was a predictor of infant neutral/positive/high positive vocalizations and accounted for 3.5% of the variability in neutral/positive/high positive vocalizations (B = 0.186). Infants were most likely to maintain their vocal state in the following order: silence, cry, fuss/whimper, high positive, angry protest, and neutral/positive. Infants of depressed mothers were more likely to maintain fuss v2 (p < 0.001). Infants of nondepressed mothers were more likely to maintain silence v2 (p < 0.01). Infants of depressed mothers were more likely to maintain positive v2 (p < 0.01). Infants of depressed mothers were more likely to maintain high positive vocalizations (rare behavior, p < 0.001) than infants of nondepressed mothers. Finally, the ratio of maintaining vocal affect states to transitioning vocal affect states was 5.36:1 for infants of depressed mothers vs 5.69:1 for infants of nondepressed mothers. |
| Kalita131 | India Age (years): Depression: 28.2 ± 0.93 Anxiety: 29.8 ± 1.68 Not diagnosed: 28.3 ± 1.28 Female babies: 52.0% |
100 | Cohort study 6 months Three groups: - PPD - Anxiety - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
18.0% | Weight; communication; symbolic behavior | PPD in the mothers had a negative effect on infant development. Composite speech scores (on the CSBS-DP) were lower in the depressed group (3.0 ± 0.33 vs 5.9 ± 0.28, p < 0.001). |
| Kaplan102 | USA Mean age: 29.9 ± 5.1 years Female babies: 45.7% |
97 | Cohort study 8 months Two groups: - PPD - No PPD |
BDI-II DSM-IV |
4 months: 42.3% (BDI-II) 12.4% (DSM-IV) 12 months: 17.5% (BDI-II) 2.1% (DSM-IV) |
Cognitive development; ability to associate a face with a segment of an unfamiliar nondepressed mother’s infant-directed speech | At 4 months, all infants learned the voice–face association. At 12 months, even though none of the mothers were still clinically depressed, the infants of mothers with chronically elevated self-reported depressive symptoms and those with elevated self-reported depressive symptoms at 4 months, but not 12 months, did not learn the association on average. For infants whose mothers were diagnosed with depression but were in remission, learning at 12 months was negatively correlated with the postpartum duration of the mother’s depressive episode. |
| Kaplan139 | USA Mean age: 29.9 ± 5.2 years Female babies: 56.0% |
91 | Cross-sectional study Two groups: - PPD - No PPD |
BDI-II | 33.0% | Cognitive development; language development (receptive and expressive communication) | BDI-II scores were significantly and negatively correlated with the Bayley expressive communication scale percentiles (p = 0.01) but did not correlate significantly with receptive communication scale percentiles (p > 0.1). |
| Koutra95 | Crete Mean age: 30.09 ± 4.53 years Female babies: 45.5% |
470 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
Not given | Fine motor, gross motor, cognitive, and social-emotional development; receptive and expressive communication | There was no significant association between PPD and receptive communication (B = –2.37, p > 0.05) or between PPD and expressive communication (B = −0.71, p > 0.05). |
| Paulson116 | USA Age (years): <20: 1.8% 20–34: 69.9% 35+: 28.3% Female babies: 47.8% |
4109 | Cohort study 16 months Two groups: - PPD - No PPD |
CES-D | 14.0% | Child language development (expressive language) | Depression at 9 months was negatively associated with contemporaneous parent-to-child reading. Depression was a significant problem that impacted reading to the child and, subsequently, the child’s language development. |
| Piteo103 | Australia Age: not given Female babies: 53% |
360 | Cohort study 17 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
19% | Motor, cognitive, and language development | There were no significant differences in child language development at 18 months between maternal depression groups based on unadjusted analyses. However, the home environment was a significant predictor of language development. |
| Quevedo105 | Brazil Age (years): >19: 18.9% 20–34: 65.3% ⩾35: 15.8% Female babies: 47.4% |
296 | Cohort study 11 months Four groups: - No PPD - Postpartum - Current - Postpartum and present |
MINI | 25.5% | Language development | Maternal depression at both time points (postpartum and at 12 months) was significantly associated with the language development of infants at 12 months of age. Children whose mothers were depressed at both assessments had worse language development than the children of mothers who were depressed at only one time point or not at all (–2.87, 95% CI = −5.01, −0.64). |
| Stein117 | UK Age: minimum 16 years Gender of newborns: not given |
1036 | Cohort study 33 months Two groups: - PPD - No PPD |
EPDS (cut-off value not given) |
Not given | Language development | Maternal depressive symptomatology in the first postnatal year (but not at 36 months) was associated with worse child language skills at 36 months; maternal caregiving was positively associated with language. Depression was associated with worse caregiving but was not independently associated with language. When the sample was split by socioeconomic factors, the effects of depression on caregiving were stronger in the less-advantaged group. |
| Wang66 | Taiwan Age (years): Depressed: 28.34 ± 5.52 Nondepressed: 29.45 ± 4.13 Female babies: 55.0% |
60 | Cohort study 1 year Two groups: - PPD - No PPD |
BDI-II | 48.3% | Gross motor, fine motor, expressive language, compressive-conceptual, situational help, self-help, personal-social, and general development | No significant difference was found in expressive language development between the two groups (p = 0.638). |
| Zajicek-Farber132 | USA Mean age: 24.6 ± 5.5 years Female babies: 52.0% |
198 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 11) |
55.0% | Emergent language; children’s exposure to literacy-oriented stimulation activities | Depressed mothers were significantly less likely to involve their child in direct literacy-oriented stimulation (p = 0.001) or enrichment literacy activities (p = 0.001). On average, children with depressed mothers had significantly lower language competence in the areas of understanding (p = 0.003) and producing (p = 0.013) the amount of age-expected vocabulary compared with children whose mothers were without symptoms. |
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; EPDS: Edinburgh Postnatal Depression Scale; CES-D: Center for Epidemiologic Studies Depression Scale; BDI-II: Beck Depression Inventory-II; DSM-IV: Diagnostic and Statistical Manual of Mental Disorders (4th ed.); MINI: Mini International Neuropsychiatric Interview; OR: odds ratio; CI: confidence interval; CSBS-DP: Communication and Symbolic Behavior Scales Developmental Profile.
Of 13 studies, 6102,105,116,131,132,139 demonstrated a significant effect of maternal PPD on the language development of infants. Four studies demonstrated an indirect effect on language development; in particular, one study117 showed that maternal depressive symptomatology in the postnatal year was indirectly associated with worse child language skills at 36 months. Moreover, depression was associated with worse caregiving, and maternal caregiving was positively associated with language. In addition, the effects of depression on caregiving were stronger in less-advantaged socioeconomic groups. Another study141 underlined the indirect effect of maternal PPD on language development via maternal depressive symptoms that impacted the quality of the home environment and had a direct effect on early child development. The third study,94 conducted in Pakistan, showed that a child’s language development was affected by maternal PPD only when the father’s income was high. The fourth study129 reported that maternal PPD was a predictor of less silence and of neutral, positive, and high positive infant vocalizations. This study also found that infants of depressed mothers were more likely to maintain high positive vocalizations than infants of nondepressed mothers, which is a rare vocal quality affective behavior.
The last three studies66,95,103 showed that maternal PPD had no effect on the language development of infants. One study66 justified the nonsignificant results because the majority of the mothers in the depressed group suffered from moderate-to-severe depressive symptoms that were less severe than a psychiatric diagnosis of a depressive illness (Taiwan). The third study103 highlighted that the home environment remained the significant predictor of infant development in Australia.
Emotional development
Four of five studies94,96,115,121 demonstrated a significant effect of maternal PPD on the emotional development of infants (Table 12). Infants of depressed mothers also had a significantly higher fear score115,121 and higher degrees of emotional disorders that included anxiety96 than infants of nondepressed mothers. In addition, one study showed that mothers with a low depression score after birth and a high depression score after several months postpartum had children with significantly higher fear scores than women with decreasing or stable depressive symptomatology.121 One study indicated a nonsignificant effect of maternal PPD on the social-emotional development of children at 18 months of age.95 The last study showed that maternal PPD was not associated with separation anxiety.96
Table 12.
Characteristics of the studies included in the evaluation of child emotional development.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborn |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Ali94 | Pakistan Mean age: 26.3 years Female babies: 48.8% |
420 | Cohort study 30 months Two groups: - PPD - No PPD |
AKUADS | 1 month: 4.8% 2 months: 4.7% 6 months: 5.7% 12 months: 9.2% 18 months: 2.7% 24 months: 6.1% |
Delayed gross motor, fine motor, emotional, cognitive, and language development | When other variables were adjusted in the model, maternal depression placed children at an approximately six-fold risk of delayed emotional development (adjusted OR = 5.9, 95% CI = 3.0, 11.9). |
| Feldman115 | Israel Mean age: 30.7 ± 3.4 years Female babies: 47.0% |
100 | Cohort study 9 months Two groups: - PPD - No PPD |
BDI-II | 22.0% | Child social engagement; fear regulation; cortisol reactivity; behavior | The infants of depressed mothers scored the worst on all outcomes at 9 months. More negative emotionality and the highest cortisol reactivity were noted in anxious dyads, which received lower scores for maternal sensitivity and infant social engagement than the controls. |
| Koutra95 | Crete Mean age: 30.09 ± 4.53 years Female babies: 45.5% |
470 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
Not given | Fine motor, gross motor, cognitive, and social-emotional development; receptive and expressive communication | Postpartum depressive symptoms were not associated with children’s social-emotional development at age 18 months. |
| Moehler121 | Germany Age: 33.3 years Female babies: 44.6% |
101 | Cohort study 14 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 9) |
Not given | Infant’s fear score; behavioral inhibition | Postpartum depression at 4 months, as measured by the EPDS, was strongly associated with the fear score and behavioral inhibition of toddlers at 14 months. Mothers with low depression and anxiety at 6 weeks and high depression at 4 months postpartum had children with significantly higher fear scores than women with decreasing or stable depressive symptomatology between the 6-week and 4-month period. |
| Walker96 | Canada Age (years): 25–34: 68.4% 15–24: 18.8% ⩾35: 12.8% Female babies: 49.2% |
1452 | Cohort study 5 years Two groups: - PPD - No PPD |
Specific to the survey | 8.4% in the year following birth of the child; 8.3% when the child was 2–3 years of age. | Hyperactivity inattention; emotional disorder-anxiety; physical aggression-opposition; separation anxiety | PPD was not significantly associated with most child behavioral or emotional outcomes. However, children of mothers who had PPD were 2.61 times more likely to display high degrees of emotional disorder in the form of anxiety (OR = 2.61, 95% CI = 1.40, 4.86). PPD was not associated with separation anxiety (OR = 1.34, 95% CI = 0.75, 2.40). |
PPD: postpartum depression; AKUADS: Aga Khan University Anxiety and Depression Scale; BDI-II: Beck Depression Inventory-II; EPDS: Edinburgh Postnatal Depression Scale; OR: odds ratio; CI: confidence interval.
Social development
The results of the four studies included in the evaluation of social development are presented in Table 13. One study indicated that the infants of depressed mothers had lower social engagement scores at 9 months than infants of nondepressed mothers.115 In this study, the effect of MDD on social engagement was moderated by maternal sensitivity. Another study showed the indirect effect of maternal PPD on social development via the impact of maternal depressive symptoms on the quality of the home environment, which directly affected early child development.141
Table 13.
Characteristics of the studies included in the evaluation of child social development.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Chen141 | Taiwan Mean age: 26.6 ± 4.2 years Female babies: 42.6% NB: immigrant mothers |
60 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
31.1% | Child development (global score for cognitive, language, motor, self-regulation, and social development); quality of the home environment | Maternal depressive symptoms had a direct and negative effect on the quality of the home environment (−0.32, p < 0.05). Maternal depressive symptoms did not have a direct effect on child development (0.05, p > 0.05). The quality of the home environment had a significant and positive effect on child development (0.55, p < 0.001). |
| Feldman115 | Israel Mean age: 30.7 ± 3.4 years Female babies: 47.0% |
100 | Cohort study 9 months Two groups: - PPD - No PPD |
BDI-II | 22.0% | Child social engagement; fear regulation; cortisol reactivity; behavior | The infants of depressed mothers scored the poorest on all three outcomes at 9 months: lowest social engagement, less mature regulatory behaviors, and more negative emotionality. The effect of MDD on social engagement was moderated by maternal sensitivity. |
| Hartley143 | South Africa Age (years): 15–19: 4.8% 20–29: 57.8% 30–39: 33.7% ⩾40: 3.6% Female babies: 56.6% NB: HIV-infected mothers |
83 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
42.2% | Social withdrawal | One-third of infants (31%) were socially withdrawn. Maternal depression did not predict infant social withdrawal, as measured by the m-ADBB. Infant social withdrawal was also not significantly associated with gender or failure to thrive. |
| Wang66 | Taiwan Age (years): Depressed: 28.34 ± 5.52 Nondepressed: 29.45 ± 4.13 Female babies: 55.0% |
60 | Cohort study 1 year Two groups: - PPD - No PPD |
BDI-II | 48.3% | Gross motor, fine motor, expressive language, compressive-conceptual, situational help, self-help, personal-social, and general development | No significant difference was found in personal-social development between the two groups (p = 0.204). |
PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; BDI-II: Beck Depression Inventory-II; m-ADBB: Modified Alarm Distress Baby Scale.
One study did not find differences between infants of depressed or nondepressed mothers in the area of social development,66 and another study showed that maternal PPD did not predict infant social withdrawal (in infants of HIV-infected mothers).143
Behavioral development
Of 12 studies, 10 demonstrated a significant effect of maternal postpartum depressive symptoms on negative behavior in infants (Table 14). Studies described multiple behavioral traits in children with depressed mothers, including an increase in child behavioral problems at age 2 years,110 more mood disorders and a more difficult temperament,114 more internalizing of problems,111,120 lower scores on the Communication and Symbolic Behavior Scales Developmental Profile,131 less mature regulatory behaviors,115 and higher fear scores that increased behavioral inhibition.121 One study examined the bidirectional effect of depressed maternal mood on mother–infant engagement using a picture book activity and found that infants of mothers with a depressed mood tended to push away and close books more often.49 Another study showed a detrimental effect of maternal PPD on dysregulated behavior in infants only when PPD was associated with a comorbid personality disorder.133 Another study demonstrated that depression explained a significant portion of children’s warmth-seeking behavior toward their mothers (for all mothers) and infant attention and arousal (only for adolescent mothers).52
Table 14.
Characteristics of the studies included in the evaluation of child behavioral development.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborns |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Main results |
|---|---|---|---|---|---|---|---|
| Avan110 | South Africa Age (years): <35: 91.5% ⩾35: 8.5% Female babies: 49.9% |
1035 | Cohort study 18 months Two groups: - PPD - No PPD |
Pitt Inventory | 24.0% | Child growth; child behavioral problems (Richman Child Behavior Scale) | Maternal postnatal depression was significantly associated with child behavioral problems at age 2 years, independent of socioeconomic status (B = 0.353, p = 0.015). |
| Bagner111 | USA Mean age: 27.5 ± 2.77 years Female babies: 52.0% |
167 | Cohort study 1 year |
K-SADS | 20.4% | Child behavior problems (Children’s Internalizing, Externalizing, and Total Behavioral Problem scores) | MMD during the sensitive period was a significant predictor of internalizing and total problem scores on the CBCL when several demographic variables were controlled (e.g. child and mother age, and child gender). Maternal depression prior to the pregnancy and during the prenatal period did not significantly predict later behavioral problems in the child, which suggested that the effect was not driven by the presence of previous MMD and was specific to the first year of life. |
| Chen141 | Taiwan Mean age: 26.6 ± 4.2 years Female babies: 42.6% NB: immigrant mothers |
60 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
31.1% | Child development (global score for cognitive, language, motor, self-regulation, and social development); quality of the home environment | Maternal depressive symptoms had a direct and negative effect on the quality of the home environment (−0.32, p < 0.05). Maternal depressive symptoms did not have a direct effect on child development (0.05, p > 0.05). The quality of the home environment had a significant and positive effect on child development (0.55, p < 0.001). |
| Conroy133 | USA Mean age: 30.7 ± 6.58 years Female babies: 52.5% |
200 | Cohort study 18 months Two groups: - PPD - No PPD |
SCID | 53% | Infant behavior | At 18 months, the children of women with depression at Time 1 and those born to women with PD had significantly higher mean scores for dysregulated, externalizing, and internalizing behaviors. There was a significant interaction between Time 1 depression and PD in the model (p = 0.005). This interaction showed that the detrimental effect of maternal depression on infant dysregulated behavior was evident only among mothers with comorbid PD (p = 0.001) and that maternal depression had no effect on the dysregulation in the absence of PD (p = 0.6). Children of mothers with a depressive episode at Time 1 had significantly lower Bayley MDI scores compared to the children of women with no depressive episodes (p = 0.02). |
| Feldman115 | Israel Mean age: 30.7 ± 3.4 years Female babies: 47.0% |
100 | Cohort study 9 months Two groups: - PPD - No PPD |
BDI-II | 22.0% | Child social engagement; fear regulation; cortisol reactivity; behavior | The infants of depressed mothers scored the poorest on all three outcomes at 9 months: lowest social engagement, less mature regulatory behaviors, and more negative emotionality. The effect of MDD on social engagement was moderated by maternal sensitivity. |
| Gao120 | New Zealand Age (years): <20: 7.6% 20–29: 50.9% 30–39: 38.1% ⩾40: 3.3% Female babies: 47.4% |
1021 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12/ 13) |
16.1% | Child behavioral problems | Prevalence rates for internalized problems were significantly higher in the children of mothers who had self-reported symptoms of psychological disorder (11.9% for those with no symptoms, 27.8% for those with early symptoms of postnatal depression, 21.1% for those with late symptoms of psychological disorder, and 42.9% for those with persistent or recurrent symptoms). The adjusted OR of a child having internalized problems was 1.38 (95% CI = 0.79, 2.43) among those whose mothers reported early symptoms of postnatal depression. |
| Hanington114 | UK Mean age: not given Gender of newborns: not given |
10,325 | Cohort study 19 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
8.8% (Time 1) 9.9% (Time 2) |
Child temperament | Maternal depression at Time 1 predicted a child’s mood disorder at Time 2 (p < 0.001). Maternal depression at Time 1 significantly predicted higher child intensity scores (higher scores indicate more difficult temperament, p < 0.001). Maternal depression at Time 1 significantly predicted child temperament at Time 2 for both genders. |
| Kalita131 | India Age (years): Depressed: 28.2 ± 0.93 Anxious: 29.8 ± 1.68 Not diagnosed: 28.3 ± 1.28 Female babies: 52.0% |
100 | Cohort study 6 months Three groups: - PPD - Anxiety - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
18.0% | Weight; communication; symbolic behavior | The infants were rated using the CSBS-DP. The mean values on the three components of the scale were significantly lower in the infants born to depressed or anxious mothers compared to those born to mothers without depression. These scores did not differ significantly between the infants born to mothers with depressive and anxiety disorders. |
| Lanzi52 | USA Mean age: 19.8 years Female babies: 53.5% |
660 | Cohort study 11 months Four groups: - No depression - Mild-to-moderate depression - Moderate-to-severe depression - Severe depression |
BDI | 23.7% of mild-to-moderate depression; 7.5% of moderate-to-severe depression; 2.7% of severe depression | Babies’ warmth-seeking (toward their mothers); babies’ attention and arousal | For each grouping of mothers, data suggested that as depression increased, both the mothers and babies scored less favorably on each significant domain. For the total sample of mothers, analyses indicated that depression explained a significant portion of the unique variance in the warmth-seeking behaviors of children (B = −13, p < 0.01). For adolescent mothers, depression explained a significant portion of the unique variance in the babies’ attention and arousal (B = −15, p < 0.05). |
| Moehler121 | Germany Age: 33.3 years Female babies: 44.6% |
101 | Cohort study 14 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 9) |
Not given | Infant fear score; behavioral inhibition | PPD at 4 months, as measured by the EPDS, was strongly associated with toddlers’ fear scores and increased behavioral inhibition at 14 months. |
| Reissland49 | UK Mean age: not given Female babies: 37.7% |
61 | Cohort study 3 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 9) |
44.3% (visit 1) 27.9% (visit 2) |
Infant nonverbal behaviors | There was a significant effect of depressed mood on negative behaviors; infants of mothers with a depressed mood tended to push away and close books more often. |
| Walker96 | Canada Age (years): 25–34: 68.4% 15–24: 18.8% ⩾35: 12.8% Female babies: 49.2% |
1452 | Cohort study 5 years Two groups: - PPD - No PPD |
Specific to the study | 8.4% in the year following birth of the child; 8.3% when the child was 2–3 years of age. | Hyperactivity inattention; emotional disorder-anxiety; physical aggression-opposition; separation anxiety | PPD was not significantly associated with hyperactivity with inattention (OR (95% CI) = 1.65 (0.89, 3.04)) or physical aggression in the form of opposition (1.94 (0.98, 3.81)). |
PPD: postpartum depression; K-SADS: Kiddie Schedule for Affective Disorders and Schizophrenia; EPDS: Edinburgh Postnatal Depression Scale; SCID: Structured Clinical Interview for DSM-IV; BDI-II: Beck Depression Inventory-II; MMD: maternal mood disorder; CBCL: Child Behavior Checklist; PD: personality disorders; MDD: major depressive disorder; MDI: Major Depression Inventory; OR: odds ratio; CI: confidence interval; CSBS-DP: Communication and Symbolic Behavior Scales Developmental Profile.
One study141 reported the indirect effect of maternal PPD on self-regulatory behaviors via maternal depressive symptoms, which had an impact on the quality of the home environment and directly affected early child development.
Only one study explored hyperactivity with inattention and physical aggression in the form of opposition; it did not identify an association between maternal PPD and children’s behavioral outcomes.96
Mother–child interactions
Bonding and attachment
Mother-to-infant bonding
A total of 11 studies29,31,34,37,43,44,47,52,56,61,82 demonstrated a negative effect of maternal depression on mother-to-infant bonding (Table 15). These studies showed that maternal depression might be a risk factor in the development of the mother–infant relationship. For example, O’Higgins et al.34 demonstrated that women who scored ⩾13 on the EPDS at week 4 were five times more likely to be experiencing poor bonding at the same time as women who scored <13 on the EPDS. Despite these results, Muzik et al.43 concluded that all women, regardless of whether they are depressed, showed increased bonding with their infant over the first 6 months postpartum. Unfortunately, depressed women showed consistently greater impairment in bonding scores at all time points than nondepressed mothers. However, one study showed that mother–infant bonding appeared to be negatively affected by maternal PPD only in the first months;61 these studies did not identify an effect of PPD on maternal bonding at 14 months, despite finding negative effects at 2 weeks, 6 weeks, and 4 months postnatally.
Table 15.
Characteristics of the studies included in the evaluation of bonding/attachment between mother and infant.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborn |
Sample size | Design: 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Type of consequences |
|---|---|---|---|---|---|---|---|
| Mother-to-infant bonding | |||||||
| Dubber29 | Germany Mean age: 32.8 ± 4.4 years Female babies: 51.9% |
80 | Cohort study 21 weeks Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
Not given Mean EPDS: 4.36 ± 3.86 |
Postpartum bonding | Maternal education, MFAS, PRAQ-R, EPDS, and STAI-T were significantly correlated with the PBQ-16. The final regression mode revealed that maternal–fetal bonding (B = −0.076, SE = 0.026, p < 0.01) and postpartum depressive symptoms (B = 0.529, SE = 0.183, p = 0.01) remained significant for explaining postpartum bonding. The results support the hypothesized negative relationship between maternal–fetal bonding and postpartum maternal bonding impairment as well as the role of postpartum depressive symptoms. |
| Edhborg47 | Bangladesh Mean age: 24.6 ± 6.1 years Female babies: 50.8% |
671 | Cohort study 3 months Four groups: - Depressive symptoms - Anxiety symptoms - Both depressive and anxiety symptoms - Neither depressive nor anxiety symptoms |
EPDS (Depressed = EPDS ⩾ 10) |
Depressive symptoms: 11%; anxiety symptoms: 35%; both depressive and anxiety symptoms: 3.4%; neither depressive nor anxiety symptoms: 51% | Maternal emotional bonding to the infant | In the adjusted model, maternal depressive symptoms showed a direct association with the mother’s emotional bonding to the infant, indicating a negative impact on maternal bonding to the infant if the mother shows depressive symptoms 2–3 months postpartum. |
| Figueiredo82 | Portugal Mean age: 26.6 years Female babies: 47.6% |
315 | Cross-sectional study Three groups: - Positive bonding - Negative bonding - Unclear bonding |
EPDS (Depressed = EPDS ⩾ 13) |
EPDS > 9: 15.7% EPDS > 13: 5.9% |
Emotional involvement; bonding | Lower emotional involvement with the newborn was observed when the mother was unemployed, unmarried, had less than a grade-9 education, had previous obstetrical/psychological problems, or was depressed, and when the infant was female, had neonatal problems, or was admitted to the intensive care unit. Lower total bonding results were significantly predicted when the mother was depressed and had a lower educational level; being depressed, unemployed, and single predicted more negative emotions toward the infant as well. |
| Korja56 | Finland Mean age: 28.8 ± 5.05 years Female babies: 43.0% NB: mothers of preterm infants |
30 | Cohort study 6 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
12.6% | Mother–infant interaction | PCERA scores on the maternal positive affective involvement scale (p = 0.03) and maternal positive communication scale (p = 0.009) were lower in mothers with depressive symptoms compared to mothers who did not have symptoms of depression. The number of depressive features did not affect any of the infant scales. In dyadic variables, mothers with depressive symptoms had slightly, but not statistically significantly, lower scores on dyadic mutuality scales (p = 0.09) and dyadic flatness scales (p = 0.06). |
| Korja54 | Finland Mean age (years): Preterm infants: 28.3 ± 5.1 Full-term infants: 28.2 ± 4.8 Female babies (%): Preterm infants: 45 Full-term infants: 49 NB: mothers of preterm and full-term infants |
83 | Cohort study 1 year Two groups: - Preterm infants - Full-term infants |
EPDS (cut-off value not given) |
Not given | Maternal attachment representations (balanced, disengaged, and distorted) | The relationship between the EPDS score and the main three representation categories (balanced, disengaged, and distorted) showed that the mean score on the EPDS was higher for the mothers in the distorted category (M = 8.69, SD = 6.42) than for the mothers in the disengaged (M = 5.50, SD = 3.00) and balanced (M = 5.27, SD = 3.9) categories (χ2 = 6.62, p = 0.037). |
| Lanzi52 | USA Mean age: 19.8 years Female babies: 53.5% |
660 | Cohort study 11 months Four groups: - No depression - Mild-to-moderate depression - Moderate-to-severe depression - Severe depression |
BDI | 23.7% of mild-to-moderate depression; 7.5% of moderate-to-severe depression; 2.7% of severe depression | Contingent responsiveness and general verbalness; maternal warmth and sensitivity | For each grouping of mothers, the data suggested that as depression increased, both the mothers and the babies scored less favorably on warmth and sensitivity. |
| Lilja44 | Sweden Mean age: 27.8 years Gender of newborn: not given |
419 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
22.2% | Women’s mood over the first year postpartum; women’s relationship with their infant; women’s relationship with their partner | The mothers who scored high on the EPDS 10 days postpartum rated their relationship less positive on the infant relationship scale throughout the entire first year (at 6 months and 1 year) compared with the mothers who scored low on the EPDS 10 days postpartum. Mothers who scored high on the EPDS on day 3 scored significantly lower on the infant relationship scale on day 3 (t = −4.269, p < 0.001) and day 10 than mothers with low EPDS scores on day 3 postpartum (t = −4.074, p < 0.001). This relationship was not found at 6 and 12 months postpartum. In addition, women with depressive symptoms showed less closeness and warmth and experienced more difficulties in their relationship with their child during the first year. |
| McMahon64 | Australia Mean age: 31.4 ± 4.2 years Female babies: 47.0% |
111 | Cohort study 11 months Three groups: - Never depressed - Brief depression - Chronic depression |
CIDI | 68.8%: 33.9% of brief depressed and 34.8% of chronic depressed | Insecure state of mind regarding attachment | Mothers diagnosed as depressed were more likely to have an insecure state of mind regarding attachment. Logistic regression analyses (secure vs insecure) revealed a significant main effect for depression group (Wald χ2(2) = 6.47, p < 0.05). Chronically depressed mothers were significantly more likely than never depressed mothers to be classified as having an insecure state of mind regarding attachment (Wald χ2(1) =5.44, p < 0.025, OR = 4.03), with a similar but nonsignificant trend (after Bonferroni correction) emerging when briefly depressed mothers were compared with never depressed mothers (Wald χ2(1) = 4.01, p < 0.05, OR = 3.01). |
| Moehler61 | Germany Mean age: 33.3 years Female babies: 45.0% |
101 | Cohort study 14 months Two groups: - PPD - No PPD |
EPDS; SCL-90-R |
Not given | Maternal bonding to the infant and child | Maternal depressive symptoms at 2 weeks, 6 weeks, and 4 months postnatally, but not at 14 months, were found to be strongly associated with lower quality of maternal bonding to the infant and child from 2 weeks to 14 months postnatal age. EPDS scores at 4 months were correlated with bonding at 2 weeks (r = 0.28), 6 weeks (r = 0.39), 4 months (r = 0.35), and 14 months (r = 0.28). Mothers with postnatal depressive symptoms at 4 months postnatal age had more negative bonding patterns starting before 2 weeks postnatally and lasting at least until 14 months postnatally. Even mild and unrecognized maternal depressive symptoms had a significant impact on maternal bonding if they occurred during the first four months of life. |
| Muzik43 | USA Mean age (years): Event+: 29.26 ± 5.93 Event–: 28.3 ± 5.15 Gender of newborn: not given |
150 | Cohort study 5 months Two groups: - PPD - No PPD |
PDSS | Not given | Mother–infant bonding | All women, independent of risk status, showed increased bonding with their infant over the first 6 months postpartum; however, women with postpartum psychopathology (depression and PTSD) showed consistently greater bonding impairment scores at all time points. |
| O’Higgins34 | UK Mean age: 33.5 years Female babies: 45.5% |
79 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
63.3% | Mother-to-infant bonding | A comparison of the bonding scores for the depressed and the nondepressed groups (defined by the EPDS score at 4 weeks) showed differences between them in the early weeks (1–4 weeks: p < 0.001), at 9 weeks (p = 0.001), at 16 weeks (p < 0.5), and at 1 year postnatal (p < 0.05). Women who scored ⩾13 on the EPDS at week 4 were 5.13 times more likely to experience poor bonding (MIBQ ⩾ 2) at the same time (p < 0.01). Both EPDS at 4 weeks and bonding in the early weeks were associated with bonding at 1 year. However, when both factors were entered simultaneously into a logistic regression, only the early bonding scores predicted bonding at 1 year (p < 0.01). |
| Orün31 | Turkey Mean age: 25.1 ± 5.2 years Female babies: 54% |
189 | Cohort study 2 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) BSI |
16.9% | Mother-to-infant bonding | The PBQ score was significantly correlated with depression (r = 0.225, p = 0.002). Significant correlations were found between the MIBS and EPDS scores (r = 0.377, p < 0.001) and between the PBQ and EPDS scores (r = 0.449, p < 0.001). The MIBS score was correlated with the depression subscales of the BSI (r = 0.150, p = 0.041). Mother–infant bonding and later interaction were associated with maternal psychopathologies, especially PPD. |
| Vliegen37 | Belgium Mean age (years): T1: 29.39 ± 4.40 T2: 32.95 ± 4.51 Gender of newborn: not given |
41 | Cohort study 3.5 years Two groups: - PPD - No PPD |
BDI-II (Depressed = BDI ⩾ 13) |
39% | Maternal depression; treatment after hospitalization; life events; relationships | Regarding emotional availability, a significantly lower level of mutual attunement was observed, but no differences were found in the other indices of emotional availability. |
| Infant-to-mother bonding | |||||||
| Korja56 | Finland Mean age: 28.8 ± 5.05 years Female babies: 43.0% NB: mothers of preterm infants |
30 | Cohort study 6 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
12.6% | Mother–infant interaction at 6 and 12 months corrected age | PCERA scores on the maternal positive affective involvement scale (p = 0.03) and the maternal positive communication scale (p = 0.009) were lower in mothers with depressive symptoms. The number of depressive features did not affect any of the infant scales (evaluated as expressed positive and negative affect and characteristic mood, behavior/adaptive abilities, activity level, and communication skills). In dyadic variables, mothers with depressive symptoms had slightly but not statistically significantly lower scores on the dyadic mutuality scales (p = 0.09) and the dyadic flatness scales (p = 0.06). |
| Lanzi52 | USA Mean age: 19.8 years Female babies: 53.5% |
660 | Cohort study 11 months Four groups: - No depression - Mild-to-moderate depression - Moderate-to-severe depression - Severe depression |
BDI | 23.7% of mild-to-moderate depression; 7.5% of moderate-to-severe depression; 2.7% of severe depression | Babies’ warmth-seeking (toward their mothers); babies’ attention and arousal | For each grouping of mothers, data suggested that as depression increased, both the mothers and the babies scored less favorably on each significant domain. For the total sample of mothers, analyses indicated that depression explained a significant portion of the unique variance in the children’s warmth-seeking (B = −13, p < 0.01). |
| McMahon64 | Australia Mean age: 31.4 ± 4.2 years Female babies: 47.0% |
112 | Cohort study 11 months Three groups: - Never depressed - Brief depression - Chronic depression |
CIDI | 68.8%: 33.9% of brief depressed and 34.8% of chronic depressed | Insecure child attachment; disorganized child attachment | Infants of chronically depressed mothers were significantly more likely than infants of mothers who had never experienced depression to be classified as insecure (p < 0.025, OR = 3.31), while infants of briefly depressed mothers did not differ from infants of mothers who had never been depressed. 17% of the infants of never-depressed mothers were classified as disorganized or unstable-resistant, compared to 18% of the infants of briefly depressed mothers and 40% of the infants of mothers in the chronically depressed group. Neither the logistic regression analysis nor the planned comparisons results were significant. |
| O’Higgins34 | UK Mean age: 33.5 years Female babies: 45.5% |
79 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
63.3% | Mother–infant bonding | A comparison of the bonding scores between the depressed and the nondepressed groups showed a difference in the early weeks (1–4 weeks, p < 0.001), at 9 weeks (p = 0.001), at 16 weeks (p < 0.5), and 1 year postnatal (p < 0.05). Women who scored ⩾13 on the EPDS at week 4 were 5.13 times more likely to experience poor bonding (MIBQ ⩾ 2) at the same time (p < 0.01). |
| Orün31 | Turkey Mean age: 25.1 ± 5.2 years Female babies: 54% |
189 | Cohort study 2 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) BSI |
16.9% | Mother-to-infant bonding | The PBQ score was significantly correlated to depression (r = 0.225, p = 0.002). The MIBS score was correlated with the depression subscales of the BSI (r = 0.150, p = 0.041). Significant correlations were also found between the MIBS and EPDS scores (r = 0.377, p < 0.001) and between the PBQ and EPDS scores (r = 0.449, p < 0.001). |
| Tharner106 | The Netherlands Age: ±32 years Female babies: 49.9% |
627 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
8.5% | Infant attachment (attachment insecurity and disorganization) | Postnatal depressive symptoms were not related to attachment insecurity or disorganization at 14 months. |
| Tomlinson127 | South Africa Age (years): <20: 15.3% 20–24: 26.5% 25–29: 32.7% 30–39: 25.5% Female babies: 44.9% |
147 | Cohort study 16 months Two groups: - PPD - No PPD |
SCID | 34.7% at 2 months 12.4% at 18 months | Infant attachment | Postpartum depression at 2 months and indices of poor parenting at both 2 and 18 months were associated with insecure infant attachment. The critical 2-month predictor variables for insecure infant attachment were maternal intrusiveness and remoteness, and early maternal depression. When concurrent maternal sensitivity was considered, the quality of the early mother–infant relationship remained important, but maternal depression was no longer predictive. |
PPD: postpartum depression; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; CIDI: Composite International Diagnostic Interview; SCL-90-R: Symptom Checklist-90—Revised; PDSS: Postpartum Depression Screening Scale; BSI: Brief Symptom Inventory; SCID: Structured Clinical Interview for DSM-IV; MFAS: Maternal–Fetal Attachment Scale; PRAQ-R: Pregnancy Related Anxiety Questionnaire—Revised; STAI-T: State-Trait Anxiety Inventory—Trait version; PBQ-16: Postpartum Bonding Questionnaire-16; PCERA: Parent–Child Early Relational Assessment; OR: odds ratio; SD: standard deviation; PTSD: posttraumatic stress disorder; MIBQ: Mother–Infant Bonding Questionnaire; MIBS: Mother-to-Infant Bonding Scale.
In addition, women with depressive symptoms showed less closeness,44 warmth,44,52 and sensitivity44,52 and a significantly lower level of mutual attunement (with regard to emotional availability)37 and experienced more difficulties in their relationships with their child44 during the first year than women without depressive symptoms. Lower emotional involvement with the newborn was observed among mothers who suffered from PPD.82
Finally, mothers who were diagnosed as depressed were more likely to have an insecure state of mind regarding attachment; they had more negative perceptions of their relationship with their infant than nondepressed mothers.54,64 McMahon et al.64 highlighted that chronically depressed mothers were more likely to be classified as feeling insecure about their attachment, whereas briefly depressed mothers did not differ from mothers who had never been depressed.
Infant-to-mother bonding
Four studies31,34,52,64 demonstrated a significantly negative effect of maternal PPD on infant–mother bonding (Table 15). One study showed that infants of chronically depressed mothers were more likely to be insecurely attached, while infants of briefly depressed mothers did not differ from infants of mothers who had never been depressed.64 Another study reported that as maternal depression increased, babies scored less favorably with respect to seeking warmth from their mothers.52
One study showed that scores on both the maternal positive affective involvement scale and the positive communication scale were lower in mothers with depressive symptoms than in mothers who did not have symptoms of depression.56 Nevertheless, this study showed that the number of depressive features did not affect infant scale scores (for preterm babies). Another study found that maternal PPD at 2 months was associated with insecure infant attachment at 2 and 18 months.127 However, this study noted that when concurrent maternal sensitivity was considered, the quality of the early mother–infant relationship remained important, although maternal depression was no longer predictive. Two studies showed that postnatal depressive symptoms were not related to attachment insecurity106 or disorganization64,106 at 14 months.
Breastfeeding
A total of 22 studies evaluated the association between maternal PPD and breastfeeding,25,26,32,41,45,59,60,62,65,69–72,77,89–92,118,119,130,137 (Table 16). Of which, 16 studies found a significant negative effect of maternal depressive symptoms on breastfeeding and/or its parameters. Mothers with depressive symptoms were significantly more likely to discontinue breastfeeding (early interruption of exclusive breastfeeding in the first months),41,59,69,71,90,91,118,119,137 engage in less-healthy feeding practices with their infant25,62,130 (e.g. significantly more depressed women fed their children prematurely and inappropriately compared with nondepressed women),130 be unsatisfied with their infant feeding method,59 experience significant breastfeeding problems,59 report lower levels of breastfeeding self-efficacy,59,92 and exhibit a lack of breastfeeding confidence91 and bottle feed45,62,65 than mothers without depressive symptoms. Higher depression scores were also associated with early weaning.89
Table 16.
Characteristics of the studies included in the evaluation of breastfeeding.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborn |
Sample size | Design 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Outcomes | Type of consequences |
|---|---|---|---|---|---|---|---|
| Adewuya119 | Nigeria Mean age: not given Gender of newborns: not given |
242 | Cohort study 8 months Two groups: - PPD - No PPD |
SCID-NP | 49.6% | Infant physical growth (weight and length); cases of diarrhea and other childhood illnesses in the infants; breastfeeding | At the 6 weeks and 3, 6, and 9 months postpartum, only 75 (62.5%), 58 (48.3%), 37 (30.8%), and 26 (21.7%) of the depressed mothers, respectively, were still breastfeeding, compared to 100 (82.0%), 87 (71.3%), 63 (51.6%), and 52 (42.6%) of the nondepressed mothers, respectively. |
| Annagür70 | Turkey Mean age: 28.6 ± 5.0 years Gender of newborns: not given |
197 | Cohort study 6 weeks Two groups: - Exclusive breastfeeding - Mixed feeding (bottle feeding and/or partial breastfeeding |
EPDS (Depressed = EPDS > 12) |
14.2% at 48 h; 11.2% at 6 weeks | Exclusive breastfeeding | At 6 weeks postpartum, the majority of women (65.5%, n = 129) were exclusively breastfeeding, with 18.8% (n = 37) partially breastfeeding (both breast milk and formula) and 15.7% (n = 31) bottle feeding. There were no significant differences between the depressed and nondepressed mothers (evaluation at 48 h: p = 0.67; evaluation at 6 weeks: p = 0.34). |
| Balbierz26 | USA Mean age: 30.3 ± 6.1 years Gender of newborn: not given |
945 | Cohort study 3 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 10) |
8.25% | Parenting practices (safety practices, feeding practices, and health care practices) | Depressed mothers were more likely to introduce water, juice, or cereal to their infants’ diets (36% vs 25%, p = 0.04) earlier than nondepressed mothers. Feeding practices at 3 months did not differ between mothers with depressive symptoms and those without depressive symptoms in multivariable models. |
| Dennis59 | Canada Mean age: 28.5 ± 5.0 years Gender of newborn: not given |
498 | Cohort study 8 weeks Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
1 week: 14.6% 4 weeks: 9.2% 8 weeks: 7.6% |
Infant feeding outcomes | Mothers with an EPDS score >12 at 1 week postpartum were significantly more likely at 4 and/or 8 weeks to discontinue breastfeeding, be unsatisfied with their infant feeding method, experience significant breastfeeding problems, and report lower levels of breastfeeding self-efficacy. |
| Dunn89 | Canada Age (years): <24: 10.7% 25–34: 61.8% ⩾35: 26.0% Gender of newborns: not given |
526 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
4.5% | Weaning | Higher scores on the EPDS were associated with early weaning. Depression was related to early weaning after adjusting for both age (p = 0.01) and education (p = 0.01), with stronger associations among women aged 25 years or older and those who had completed high school. Women who scored 12 or higher on the EPDS were more likely to wean (OR = 0.28, 95% CI = 0.11, 0.71, p = 0.007) than women who scored less than 12. |
| Feldens69 | Brazil Age (years): <18: 81.9% >18: 18.1% Female babies: 42.5% |
360 | Cohort study 12 months Two groups: - Discontinued breastfeeding before 12 months - Continued breastfeeding before 12 months |
BDI (minimal: <2; low: 12–19; moderate to severe: >19) |
Minimal: 62.1%; low: 19.6%; moderate to severe: 18.3% | Discontinued breastfeeding before 12 months | A multivariate Cox regression model revealed that symptoms of maternal depression (low levels: RR = 1.59, 95% CI = 1.02, 2.47; moderate to severe: RR = 2.03, 95% CI = 1.35, 3.01) were independently associated with the outcomes after adjusting for confounders. |
| Figueiredo72 | Portugal Age (years): ⩽19: 5% 20–29: 47% 30–39: 47% ⩾40: 1% Female babies: 40% |
145 | Cohort study 1 year Three groups: - Exclusive breastfeeding, no initiation - Exclusive breastfeeding, early cessation (0–3 months) - Exclusive breastfeeding for ⩾3 months |
EPDS (cut-off value not given) |
Not given | Exclusive breastfeeding duration | Depression scores at 3 months postpartum were not found to predict exclusive breastfeeding duration (B = 0.04, OR = 1.04, CI 95% = 0.91, 1.18). |
| Flores-Quijano91 | Mexico Mean age: 27.3 ± 8.1 years Gender of newborns: not given |
163 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
24.5% | Breastfeeding confidence; breastfeeding practice | A total of 40 women (24.5%) had an EPDS score compatible
with the risk of a depressive episode, and 63 (41%) did
not feel confident about breastfeeding. These two
variables were significantly correlated to each other
(14.6% of breastfeeding confidence in depressed women vs
85.4% in nondepressed women; p < 0.001).
There was a significant correlation between PPD and confidence (r = 0.28, p < 0.01), and significantly fewer depressed women believed their milk was sufficient for their babies (p = 0.001). In addition, PPD was individually correlated with exclusive breastfeeding (67.5% of depressed women did not exclusively breastfeed, compared to 42.3% of nondepressed women; p = 0.006). |
| Gagliardi45 | Italy Mean age: 32.3 years Gender of newborns: not given |
592 | Cohort study 14 weeks Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
EPDS > 9: 15.7%; EPDS > 12: 6.8% | Breastfeeding; breastfeeding problems | Mothers with higher EPDS scores were more likely to bottle feed at 3 months; the odds of bottle feeding increased with increasing EPDS results, even at low scores (OR = 1.06, 95% CI = 1.01, 1.11). In a multinomial logistic regression, the OR of bottle feeding associated with a one-point increase in the EPDS score was 1.06 (95% CI = 1.01, 1.11, p = 0.02), and it remained the same after adjusting for the mother’s parity, mode of delivery, age and nationality (Italian/foreigner) and sex of the infant. This study showed that even low levels of depressive symptoms detected by the EPDS were negatively associated with breastfeeding. |
| Hasselmann118 | Brazil Age (years): <18: 12.1% ⩾18: 87.9% Female babies: 49.0% |
429 | Cohort study 2 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
22.5% | Early interruption of exclusive breastfeeding | Children of mothers with postpartum depressive symptoms were at a higher risk of early interruption of exclusive breastfeeding in the first and second months of follow-up (RR = 1.46, 95% CI = 0.98, 2.17; RR = 1.21, 95% CI = 1.02, 1.45, respectively). Among mothers that were exclusively breastfeeding during the first month, PPD was not associated with the interruption of exclusive breastfeeding in the second month (RR = 1.44, 95% CI: 0.68, 3.06). |
| Hatton65 | USA Age (years): Lactating: 23.5 ± 5.0 No lactating: 20.0 ± 3.5 Gender of newborns: not given |
377 | Cohort study 12 weeks Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 14) |
Not given Mean EPDS score: lactating: 7.8 ± 1.5; no lactating: 9.8 ± 1.6 |
Breastfeeding | There was an inverse relationship between depressive symptoms and breastfeeding at 6 weeks postpartum (p < 0.001), but not at 12 weeks. Women who were breastfeeding had significantly fewer depressive symptoms (p < 0.05), even after controlling for age, income, education, and race as predictors of breastfeeding at 6 weeks (but not at 12 weeks) postpartum. The women with the greatest probability of having an early MDD (EPDS ⩾ 14) were nonbreastfeeders. There was a significant drop-off in depressive symptoms between 6 and 12 weeks postpartum (p < 0.001) for all women studied at both time points. Unexpectedly, those who stopped breastfeeding after 6 weeks postpartum (n = 38) showed significantly greater improvement in depressive symptoms relative to those who continued to breastfeed (Δ 2.76 ± 4.6 vs 0.89 ± 3.0) (p < 0.005). |
| Kawano32 | Japan Mean age: 32.7 ± 4.5 years Gender of newborns: not given |
81 | Cohort study 2 weeks Two groups: - PPD - No PPD |
POMS + GHQ | Not given Mean POMS: 5.5 ± 6.7 |
Breast milk secretory immunoglobulin A level | Weak negative correlations were observed between breast milk SigA levels and all negative POMS states (tension-anxiety, depression-dejection, anger-hostility, fatigue, and confusion). However, no correlation was observed between breast milk SigA level and the positive POMS state (vigor). These results indicate that the maternal psychological state may affect the immune properties of breast milk. |
| Kondo77 | Japan Mean age: 30.7 ± 5.1 years Gender of newborns: not given |
129 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 9) |
11.0% | Concentrations of transforming growth factor-beta in breast milk | Mothers with depression or poor self-rated health had higher TGF-β2 concentrations than mothers without depression (OR for a higher TGF-β2 quartile: 3.11, 95% CI = 1.03, 9.37) and those reporting better health (OR: 2.34, 95% CI = 1.21, 4.55). |
| Mallan25 | Australia Mean age: 30.0 ± 5.0 years Female babies: 52% |
211 | Cohort study 2 years Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) |
Not given | Mother-reported child-feeding practices | Higher EPDS scores were associated with less responsive feeding practices when the child was 2 years old. After adjustments for key maternal and child covariates, a higher EPDS score was significantly associated with more pressure to eat (B = 0.18, p = 0.01), restriction (B = 0.14, p = 0.05), instrumental feeding (B = 0.14, p = 0.04) and emotional feeding (B = 0.15, p = 0.03) practices. |
| McCarter-Spaulding60 | USA Mean age: 30.5 years Gender of newborns: not given |
122 | Cohort study 14 months One group: - PPD |
EPDS (Mild, EPDS: 10–12; moderate, EPDS: 13–15; severe, EPDS > 16) BDI-II |
100% Mild (EPDS: 10–12): 58.2%; moderate (EPDS: 13–15): 20.9%; severe (EPDS: >16): 20% |
Breastfeeding | Maternal education was a significant predictor of either exclusive breastfeeding or combination feeding compared to bottle feeding, but it was not a significant predictor of exclusive versus combination feeding. These results suggest that women with PPD symptoms who breastfed, either exclusively or in combination with formula feeding, may be more similar to each other than to mothers who chose to formula feed only. Severity of depression symptoms was not a significant predictor of feeding pattern at 4–8, 10–14, or 14–18 weeks postpartum. NB: compared to a random sample, the level of exclusive breastfeeding was significantly lower in this sample than the level of combination feeding. |
| McLearn137 | USA Age (years): <20: 13.3% 20–29: 50.6% ⩾30: 36.2% Gender of newborns: not given |
4874 | Cohort study 3 months Two groups: - PPD - No PPD |
CES-D | 17.8% | Practices to promote child development; breastfeeding | Mothers with depressive symptoms had reduced odds of continued breastfeeding (Adjusted OR = 0.73, 95% CI = 0.61, 0.88). |
| Nishioka71 | Japan Mean age: 31.3 ± 4.7 years Gender of newborns: not given |
405 | Cohort study 5 months Two groups: - Breastfeeding-based group - Formula milk-based group |
EPDS (Depressed = EPDS ⩾ 9) |
19.5% at 1 month; 13.0% at 5 months | Breastfeeding | A high proportion of breastfeeding mothers at 1 month postpartum had EPDS scores ⩾9 at 5 months postpartum (p = 0.01). These mothers were more likely to switch to formula milk-based feeding at 5-month postpartum than the mothers in the breastfeeding-based group at both 1- and 5-month postpartum. The appearance of depressive symptoms seems to promote the discontinuation of breastfeeding at 5-month postpartum. |
| Paulson62 | USA Age (years): <20: 3.9% 20–34: 74.7% ⩾35: 21.3% Gender of newborns: not given NB: two-parent families |
5089 | Cohort study 9 months Two groups: - PPD - No PPD |
CES-D | 14.0% | Maternal health behaviors (putting the child to sleep on its back, putting the child to bed without a bottle, putting the child to sleep awake, and breastfeeding); Mother–child interaction behaviors | Mothers who were depressed were 1.5 times more likely to engage in less healthy feeding practices with their infant. Depressed mothers were less likely to have ever breastfed their infants (OR: 1.48, p < 0.01), and more likely to put their infants to bed with a bottle (OR: 1.53, p < 0.01). |
| Stuebe41 | North Carolina Mean age: 31.6 ± 4.8 years Gender of newborns: not given |
47 | Cohort study 8 weeks Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 10) |
2 weeks postpartum: 17.0%; 8 weeks postpartum: 8.5% | Breastfeeding duration; neuroendocrine response to infant feeding | At 2 weeks, baseline oxytocin was inversely correlated with EPDS score (Spearman’s R = −0.33, p = 0.03). We found no correlations between maternal EPDS score and baseline cortisol, CRF, estradiol, progesterone, prolactin, FT4, or total T4. Mothers with higher depressive symptoms reported feeling more depressed, overwhelmed, and stressed during feeding than mothers with lower symptoms (p < 0.05). At the 8 weeks, we found statistically significant associations between maternal mood and oxytocin, total T4, and affect during feeding. EPDS scores were inversely correlated with oxytocin measures during and after feeding and with oxytocin area under the curve (Spearman’s R for EPDS: −0.48, −0.53, and −0.44, respectively, all p < 0.01). Total T4 was inversely correlated with EPDS (Spearman’s R = −0.41, p = 0.01 before and R = −0.36, p = 0.03 after). We found no significant correlations between maternal mood measures and baseline cortisol, CRF, estradiol, progesterone, prolactin, or free T4 (p > 0.05). |
| Thome90 | Iceland Mean age: 28.3 years Female babies: 51.5% |
Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
14.0% | Exclusive breastfeeding | Mothers who were exclusively breastfeeding had a lower mean EPDS scores than mothers who were not exclusively breastfeeding (5.9 (SD = 4.6) and 7.1 (SD = 4.9), p < 0.001). EPDS score remained a significant predictor in the conditional regression model: a low EPDS score increased the likelihood of exclusive breastfeeding. An increase of 5 points on the EPDS scale resulted in an almost 20% reduction in the likelihood of exclusive breastfeeding. High maternal education level, low EPDS score and singleton birth increased the likelihood of exclusive breastfeeding. In addition, single mothers were less likely to breastfeed exclusively (OR = 0.58) than those who were married or lived with a partner. Being a mother of twins decreased the likelihood of exclusive breastfeeding to a great extent when other factors were held equal (p < 0.001, OR = 0.12). | |
| Zajicek-Farber130 | USA Age (years): Depressed: 22.3 ± 4.3 Nondepressed: 22.6 ± 3.9 Female babies: 54.0% |
134 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 11) PHQ |
55.2% | Infant health practices | Significantly more depressed women fed children prematurely and inappropriately compared to women who were never depressed (54.1% vs 23.3%). The RR for inappropriate feeding was 2.3 times greater for depressed women than those who were never depressed. |
| Zubaran92 | Brazil Mean age: 25.4 ± 7.0 years Gender of newborns: not given |
89 | Cross-sectional study Two groups: - Exclusive breastfeeding - Partial breastfeeding |
EPDS (Depressed = EPDS ⩾ 13) PDSS (Depressed = EPDS ⩾ 81) |
EPDS: 22.5% PDSS: 34.8% |
Breastfeeding self-efficacy | Mothers who combined breastfeeding and bottle feeding presented higher PDSS (73.2 ± 26.4 vs 70.3 ± 25.2; p = 0.66) and EPDS scores (9.1 ± 5.5 v. 8.0 ± 5.6; p = 0.42). However, these differences were not significant. The BSES-SF scores were higher in mothers who exclusively breastfed (65.6 ± 4.0 in women who exclusively breastfed vs 56.6 ± 7.0 in women who partially breastfed; p < 0.001) and were negatively associated with both EPDS (64.8 ± 5.3 in nondepressed women vs 59.0 ± 7.4 in depressed women; p = 0.003) and PDSS scores (65.3 ± 4.6 vs 60.2 ± 7.6; p = 0.002). |
PPD: postpartum depression; SCID-NP: Structured Clinical Interview for DSM-IV, Non-Patient edition; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; POMS: Profile of Mood States; GHQ: General Health Questionnaire; CES-D: Center for Epidemiologic Studies Depression Scale; PHQ: Patient Health Questionnaire; PDSS: Postpartum Depression Screening Scale; OR: odds ratio; CI: confidence interval; RR: risk ratio; MDD: major depressive disorder; TGF: transforming growth factor; CRF: corticotropin-releasing factor; FT4: plasma free thyroxine; SD: standard deviation; BSES-SF: Breastfeeding Self-Efficacy Scale—Short Form.
Hatton et al.65 showed conflicting results; they reported a significant inverse relationship between depressive symptoms and breastfeeding at 6 weeks postpartum, but not at 12 weeks.
The four remaining studies did not find a difference between depressed mothers and nondepressed mothers with respect to feeding practices;26,60,70,72 one study showed that a delayed onset of lactation within the first 48 h, methodological breastfeeding problems, and nipple pain were significantly predictive of breastfeeding cessation.70
Breast milk concentration and endocrine response to breastfeeding
Three studies evaluated the association between PPD and breast milk concentration and/or the endocrine response to breastfeeding. Maternal depressive symptoms appeared to be correlated with lower oxytocin,41 total T441 concentrations, and higher TGF-β2 concentrations.77 Kawano and Emori32 identified weak negative correlations between breast milk secretory immunoglobulin A levels (breast milk SigA level) and all negative profile of mood states (POMS: tension–anxiety, depression–dejection, anger–hostility, fatigue, and confusion); however, there was no correlation between breast milk SigA level and positive POMS state.
Maternal role
Studies that evaluated the association between PPD and the maternal role are presented in Table 17. Nine studies focused on maternal behaviors and PPD,26,40,49,52,53,62,79,83,85 two studies focused on PPD and maternal competence,51,75 six studies focused on PPD and maternal care for infants,37,53,130,137,145,146 eight studies focused on PPD and infant health care practices or utilization measures,26,37,57,63,98,128,130,142 five studies focused on maternal perceptions of the infant’s patterns and depression,40,46,50,58,80 and two studies focused on PPD and the risk of maltreatment.130,144
Table 17.
Characteristics of the studies included in the evaluation of the maternal role.
| First author’s name | Sociodemographic data: 1. Country 2. Maternal mean age 3. Gender of newborn |
Sample size | Design 1. Study design 2. Time of follow-up 3. Number of groups 4. Description of groups |
Tool used to assess PPD | Prevalence of PPD | Type of consequences | |
|---|---|---|---|---|---|---|---|
| Maternal behaviors | |||||||
| Balbierz26 | USA Mean age: 30.3 ± 6.1 years Gender of newborns: not given |
945 | Cohort study 3 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 10) |
8.25% | Parenting practices (safety practices, feeding practices, and health care practices) | In the multivariable model, depressed mothers remained less likely to put their infant to sleep on their backs (OR = 0.37, 95% CI = 0.22, 0.61), to use a car seat (OR = 0.44, 95% CI = 0.25, 0.79) and to have a working smoke alarm in the home (OR = 0.26, 95% CI = 0.12, 0.56). |
| Cowley-Malcolm53 | New Zealand Age (years): <20: 3.81% 20–29: 50.7% 30–39: 40.6% ⩾40: 4.72% Gender of newborns: not given |
1207 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
17.5% | Discipline; nurturing practices (behavior that promotes a child’s psychological growth) | Low nurturance was significantly associated with postnatal depression, alcohol consumption and gambling. High discipline scores were significantly associated with gambling, postnatal depression and lack of alignment to either Pacific or to European traditions. |
| De l’Etoile79 | USA Mean age: 30.0 years Female babies: 46.6% |
73 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 9 or any response indicating suicidal ideation) |
20.5% | Acoustic parameters of infant-directed singing | Extraction and analyses of vocal data revealed a main effect of tempo, meaning that as mothers reported more depressive symptoms, they tended to sing faster to their infants. In addition, an interaction effect indicated that mothers with depressive symptoms were more likely to sing with tonal key clarity to their male infants. |
| Kerstis40 | Sweden Mean age: 30.0 ± 5.0 years Female babies: 49% |
401 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 9) |
18% | Mother’s SOC (comprehensibility, manageability and meaningfulness); parents’ perception of infant’s temperament | A higher proportion of the mothers with self-scored depressive symptoms had poor SOC compared with those without depressive symptoms (p < 0.001). |
| Lanzi52 | USA Mean age: 19.8 years Female babies: 53.5% |
660 | Cohort study 11 months Four groups: - No depression - Mild-to-moderate depression - Moderate-to-severe depression - Severe depression |
BDI | 23.7% of mild-moderate depression; 7.5% of moderate-to-severe depression; 2.7% of severe depression | Contingent responsiveness and general verbalness; maternal warmth and sensitivity | Regression analyses were conducted separately for maternal parenting behaviors such as positive affect, warmth and sensitivity, contingent responsiveness, physical intrusiveness, punitive tone, verbal content, and general verbalness. For each grouping of mothers, the data suggested that as depression increased, both mothers and babies scored less favorably on each significant domain. |
| Paulson62 | USA Age (years): <20: 3.9% 20–34: 74.7% ⩾35: 21.3% Gender of newborns: not given NB: two-parent families |
5089 | Cohort study 9 months Two groups: - PPD - No PPD |
CES-D | 14.0% | Maternal health behaviors (putting the child to sleep on its back, putting the child to bed without a bottle, putting the child to sleep awake, and breastfeeding) | Depressed mothers were less likely to put their infants to sleep on their backs (OR = 1.40, p < 0.01), less likely to have ever breastfed their infants (OR = 1.48, p < 0.01), and more likely to put their infants to bed with a bottle (OR = 1.53, p < 0.01). Depressed mothers were less likely to tell their child stories every day (OR = 1.42, p < 0.05) and played peekaboo less often (OR = 1.57, p < 0.05). |
| Posmontier85 | USA Mean age (years): No PPD: 31.0 ± 4.5 PPD: 30.0 ± 5.5 Female babies (%): No PPD: 78.3 PPD: 30.4 |
46 | Cross-sectional study Two groups: - PPD - No PPD |
MINI | Not applicable (number of PPD and no PPD women were
fixed at the beginning of the study)
Nondepressed: n = 23 Depressed: n = 23 |
Functional status (physical infant care, personal care, household care, social activities, and occupational activities) | Functional status was negatively correlated with PPD with the exception of infant care activities. Specifically, lower household, social, and personal functioning were correlated with PPD. In multiple regression analyses, PPD predicted lower overall functional status (p < 0.001), household function (p < 0.05), social function (p < 0.001), and personal function (p < 0.001). NB: functional status was evaluated using the IFSAC, a 52-item self-rated scale that measures physical infant care, personal care, household care, social activities, and occupational activities. |
| Reissland83 | UK Mean age: 31.8 years Female babies: 44.3% |
79 | Cross-sectional study Four groups: - Stress and depression - Only depression - Only stress - Neither stress nor depression |
EPDS (Depressed = EPDS ⩾ 9) |
Stress and depression: 16.4%; depression: 7.59%; stress: 39.2% | Cradling side of mothers (left or right) | The results indicated that 86% of mothers who were neither stressed nor depressed cradled to the left, and 14% cradled to the right. When the cradling side of stressed mothers was compared with that of the mothers who were neither stressed nor depressed, more in the former group showed right-sided cradling. In contrast, mothers who were just depressed preferred to cradle to the left. The lack of a left-sided cradling bias might be due to stress rather than depression experienced by mothers. Furthermore, this study provides evidence that the state of a mother’s mental health might be indicated by the side on which she prefers to cradle her child. |
| Reissland49 | UK Mean age: not given Female babies: 37.7% |
61 | Cohort study 3 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 9) |
44.3% (visit 1) 27.9% (visit 2) |
Mother–infant engagement with a picture book (mother gazes at book, at infant; mother restrains infant; mother keeps/pulls book away; infant gazes at book, at mother; infant pushes book away; and infant tries to close book) | The complexity of the effects of depressed mood on mothers and infants is highlighted by the fact that no significant differences were found when simply comparing maternal behavior of depressed and nondepressed groups. In contrast, infants in these two groups of mothers showed significant differences in their nonverbal behaviors. Specifically, during the first visit, infants of depressed mothers showed significantly more negative touch behaviors compared with infants of nondepressed mothers. |
| Maternal competence | |||||||
| Kohlhoff75 | Australia Mean age: 32.2 ± 5.1 years Female babies: 47.6% |
83 | Cross-sectional study Two groups: - PPD - No PPD |
MINI; EPDS (cut-off value not given) | 32.5% | Parenting self-efficacy (perceived parenting efficacy in parents) | Significant predictors of parenting self-efficacy were recollections of parental abuse, attachment avoidance, infant gender and depressive symptom severity (B = −0.42, p = 0.004). This suggests that women with higher parenting self-efficacy were less likely to report depressive symptoms. |
| Ngai51 | China Mean age: 31.3 ± 3.8 years Gender of newborns: not given |
184 | Cohort study Approximately 10 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS 9/10) |
Not given Mean EPDS: 7.7 ± 4.7 |
Perceived maternal role competence; perceived maternal role satisfaction | Postnatal variables, including learned resourcefulness (B = 0.18, p < 0.05) and depressive symptoms (B = −0.56, p < 0.01), explained 33.6% of the variance of the final model predicting maternal role competence and satisfaction at 6 weeks postpartum. Postpartum depression was the strongest correlate of maternal role competence and satisfaction at 6 weeks postpartum, accounting for 32.3% of the total variance. |
| Maternal care for infant | |||||||
| Bank146 | USA Mean age: not given Gender of newborns: not given |
84 | Cross-sectional study Two groups: - PPD - No PPD |
CES-D | Not given | Quantity and content of infant media use; depressed mothers who sat and talked to their children during television use or consulted outside sources for information about media | Having a depressed mother predicted a significant proportion of the variance in weekday hours spent watching television (p < 0.001), while ethnicity, socioeconomic status, maternal education, and childcare hours did not. The same pattern existed for weekend television exposure (p < 0.001). There was a significant difference between the average number of both weekday (p < 0.01) and weekend hours (p < 0.01) for the depressed (weekday, M = 4.81 h, SD = 4.04, weekend, M = 5.61 h, SD = 4.16) and nondepressed mothers (weekday, M = 2.26 h, SD = 1.60, weekend, M = 2.70, SD = 1.98). The infants of depressed mothers were exposed to significantly more children’s programming (M = 1 h 36 min, SD = 3 h 36 min) than the infants of nondepressed mothers (M = 18 min, SD = 40 min). |
| Cowley-Malcolm53 | New Zealand Age (years): <20: 3.81% 20–29: 50.7% 30–39: 40.6% ⩾40: 4.72% Gender of newborns: not given |
1207 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 12) |
17.5% | Discipline (yelling at child, threatening to punish child, telling child that he or she is bad, smacking child, and hitting child with an object); nurturing practices (taking child to the park or playground, playing with child, child spends time with a partner or relatives, etc.) | High nurturance was significantly associated with Samoan ethnicity and postschool qualifications, and low nurturance was significantly associated with postnatal depression, alcohol consumption and gambling. At the univariate level, high discipline scores were significantly associated with gambling, postnatal depression and a lack of alignment to either Pacific or to European traditions. |
| Hibino145 | Japan Mean age: 29.7 ± 4.7 years Gender of newborns: not given |
155 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 9) |
11.6% | Trouble with infant care | EPDS scores were significantly correlated with increased “trouble with infant care” (B = 0.47, p < 0.001). |
| McLearn137 | USA Age (years): <20: 13.3% 20–29: 50.6% ⩾30: 36.2% Gender of newborns: not given |
4874 | Cohort study 3 months Two groups: - PPD - No PPD |
CES-D | 17.8% | Practices to promote child development; breastfeeding | Mothers with depressive symptoms had a reduced probability of sharing books (adjusted OR = 0.81; 95% CI = 0.68, 0.97), playing with the infant (adjusted OR = 0.70; 95% CI = 0.54, 0.90), talking to the infant (adjusted OR = 0.74; 95% CI = 0.63, 0.86), or following routines (adjusted OR = 0.61; 95% CI = 0.52, 0.72). |
| Vliegen37 | Belgium Mean age (years): T1: 29.39 ± 4.40 T2: 32.95 ± 4.51 Gender of newborns: not given |
41 | Cohort study 3.5 years Two groups: - PPD - No PPD |
BDI-II (Depressed = BDI ⩾ 13) |
39% | Maternal/parental care; child treatment | A very important clinical finding was that almost all children (92%) of mothers without current depression received continuous parental care, while proportionally more children (31%) of mothers who were depressed at follow-up experienced interruptions and breaks in parental care, with care taken over by family members or children who were placed in institutions or foster care. Almost all mothers with elevated levels of depression at T2 sought some form of professional help for their child. However, this was the only study that included half of the nondepressed mothers. |
| Zajicek-Farber130 | USA Age (years): Depressed: 22.3 ± 4.3 Nondepressed: 22.6 ± 3.9 Female babies: 54.0% |
134 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 11) PHQ |
55.2% | Infant health practices | Significantly more depressed women had poor parenting practices compared to women who were never depressed (63.5% vs 26.7%). The difference was statistically significant (p < 0.001). The RR for having poor parenting practices was 2.4 times greater for depressed women than those who were never depressed. |
| Infant health care practices and utilization measures | |||||||
| Balbierz26 | USA Mean age: 30.3 ± 6.1 years Gender of newborns: not given |
945 | Cohort study 3 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS > 10) |
8.25% | Parenting practices (safety practices, feeding practices, and health care practices) | Depressed mothers were more likely to bring their babies for emergency room visits (26 vs 16%, p = 0.03) than nondepressed mothers were. There was no significant difference in routine childcare visits. Health care utilization did not differ for mothers with depressive symptoms versus those mothers without depressive symptoms in multivariable models (controlled for age, race, marital status, education, parity, intervention status, employment status and language). |
| Chee57 | Singapore Mean age: 31 ± 4.7 years Female babies: 50.1% |
471 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 8) |
15.3% | Nonroutine visits to the infant’s doctor | After adjusting for confounders, women who had brought their infants for three or more nonroutine visits to the infant’s doctor had a significantly higher prevalence of depression (32.6%) than those with fewer visits (13.6%) (OR = 2.87; 95% CI = 1.41,5.85; p = 0.004). |
| Eilat-Tsanani63 | Israel Age: 18 years and above Gender of newborns: not given |
527 | Cohort study 2 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 13) (+survey) |
9.9% | Women’s consultations with physicians (family physicians, gynecologists, and/or pediatricians) | Women with PPD differed from those without PPD in terms of the frequency of and reasons for consultations. The rate of PPD was significantly higher among women who sought medical consultations than those who came for routine care (13 vs 4%, p = 0.001). Women with multiple visits (four or more) to all doctors had higher rates of PPD than the others (16.7 vs 7%, p = 0.002). Women with PPD consulted more with family physicians (20.6 vs 7.8%, p = 0.01) and pediatricians (18.3% vs 7.1%, p = 0.001). No significant difference in PPD rates was found in relation to the number of visits to gynecologists. |
| Farr98 | USA Age (years): <25: 27.7% 25–29: 32% 30–34: 26.6% ⩾35: 13.7% Gender of newborns: not given |
24,263 | Cohort study ±1 year Four groups: - No depression - Pregnancy only - Pregnancy and postpartum - Postpartum only |
Not given | 13.4% | Infant health care utilization | Infants of mothers with PPD had only a marginally increased risk of hospitalization (RR = 1.2; 95% CI = 1.0, 1.4). Of the 128 hospitalizations among infants of mothers diagnosed with PPD, 70.3% occurred before the mother’s diagnosis. Compared to infants of mothers without depression, infants of mothers with depression diagnosed during the postpartum period only (RR = 1.2; 95% CI = 1.1, 1.2) were more likely to have ⩾6 sick or emergency visits. |
| Minkovitz128 | USA Age (years): <20: 13.3% 20–29: 50.5% ⩾30: 36.2% Female babies: 50.1% |
4896 | Cohort study 33 months Two groups: - PPD - No PPD |
CES-D | 17.8% at 2–4 months; 15.5% at 30–33 months | Child’s receipt of acute and preventive health care services | Children whose mothers had depressive symptoms at 2 to 4 months had 0.74 to 0.81 reduced odds of receiving age-appropriate well-child visits. This result was significant for visits between 6 and 24 months. The association with maternal depressive symptoms and vaccinations was also significant for children who were up to date on their vaccinations at 24 months and had received an age-appropriate dose of MMR. The influence of maternal depressive symptoms on the reception of acute care persisted for ED visits in the previous year and tended to continue during hospitalizations, as reported at 30 to 33 months. Mothers who had depressive symptoms had increased odds of reporting that their children sustained injuries in the preceding year but also had decreased odds of their children using the ED specifically for an injury in the year preceding the 30- to 33-month interview. Children whose mothers had depressive symptoms at 2 to 4 months had fewer sick visits through the first 32 months of life (p = 0.04) than children whose mothers did not have symptoms. However, in adjusted analyses, there was no significant association between depressive symptoms at 2 to 4 months and the number of sick visits. Children whose mothers had depressive symptoms at 2 to 4 months had an increased likelihood of having an ED visit between 1.5 and 2.5 years of age (OR = 1.38; CI = 1.12, 1.71). |
| Ndokera142 | Zambia Age (years): ⩽18: 9% 19–24: 35.6% 25–30: 33.1% ⩾31: 22.3% Female babies: 45.3% |
278 | Cross-sectional study Two groups: - PPD - No PPD |
SRQ-20 | 9.7% | Weight; length diarrheal episodes; incomplete vaccination |
After adjustment for infant age and other possible confounders, a logistic regression analysis showed no significant association between a high risk of maternal depression and incomplete immunization. Clinic location and older infant age were significantly associated with incomplete vaccination. |
| Vliegen37 | Belgium Mean age (years): T1: 29.39 ± 4.40 T2: 32.95 ± 4.51 Gender of newborns: not given |
41 | Cohort study 3.5 years Two groups: - PPD - No PPD |
BDI-II (Depressed = BDI ⩾ 13) |
39% | Maternal/parental care; child treatment | Almost all mothers with elevated levels of depression at T2 sought some form of professional help for their child. However, this was the only study that included an equal number of nondepressed mothers. |
| Zajicek-Farber130 | USA Age (years): Depressed: 22.3 ± 4.3 Nondepressed: 22.6 ± 3.9 Female babies: 54.0% |
134 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 11) PHQ |
55.2% | Infant health practices | On average, the mothers with a history of depression completed 5.91 (SD = 1.03) well-child health visits, whereas the women who were never depressed completed 6.42 (SD = 0.77) visits (p < 0.002). Significantly fewer children of women who were never depressed than children of depressed women (16.7% vs 33.8%) had inadequate (five or fewer) well-child visits. Significantly fewer children of women who were never depressed had an incomplete immunization series compared to depressed women (11.7% vs 39.2%). On average, children of depressed mothers had 1.32 (SD = 1.4) acute care visits, whereas children of mothers who had never been depressed made no such visits to the emergency department (p < 0.001). Significantly more depressed women spanked their infant within the week preceding the interview compared to women who were never depressed (35.1% vs 8.3%). |
| Maternal perception of infants’ patterns | |||||||
| Arteche46 | UK Mean age: 33.2 ± 5.2 years Female babies (%): Control: 61.8 MDD: 61.9 GAD: 47.1 |
89 | Cohort study 15 months Three groups: - Control - MDD - GAD |
EPDS (Depressed = EPDS > 12) GAD-Q |
MDD: 23.6% GAD: 38.2% |
Infant facial expression identification by the mother | Planned contrasts revealed that participants with
depression were significantly less accurate at
identifying happy faces than controls (p = 0.005).
Participants with GAD identified happy faces at a significantly lower intensity than control participants (p = 0.005), and participants with depression, compared to control participants, showed a nonsignificant trend in the same direction, (p = 0.05). Moreover, similar to the findings on all trials, analyses of sad faces revealed no significant differences between controls and either participants with depression (p > 0.01), or participants with GAD (p > 0.01). |
| Gil80 | France Mean age: not given |
79 | Cross-sectional study Two groups: - PPD - No PPD |
EPDS (Cut-off value not given) |
30.4% | Evaluation of emotional facial expressions | The only difference between mothers with and without postpartum depressive mood lays in their assessment of the babies’ faces, neutral baby faces being judged to be less neutral, thus demonstrating the specificity of postpartum affective disorders. |
| Kerstis40 | Sweden Mean age: 30.0 ± 5.0 years Female babies: 49% |
401 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 9) |
18% | Mother’s SOC (comprehensibility, manageability and meaningfulness); parents’ perception of infant’s temperament | A higher ICQ score indicated a perception of a “more difficult” child temperament. Mothers with depressive symptoms had a higher ICQ score then mothers without depressive symptoms (p = 0.028) at 3 months postpartum, but not at 18 months (p = 0.145). |
| Orhon58 | Turkey Age (years): EPDS < 12: 29.7 ± 4.8 EPDS ⩾ 12: 28.9 ± 3.2 Gender of newborns: not given |
103 | Cohort study 1 year Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 12) |
34.0% | Maternal perceptions of infant patterns (infant feeding patterns, sleeping patterns, infant cry-fuss problems, and infant temperament) | Mothers with elevated depressive symptoms were more inclined to report infant cry-fuss, sleeping and temperamental problems through the follow-up. Postpartum depressive symptoms may lead to negative maternal perceptions of infant patterns. |
| Stein50 | UK Mean age (years): Control: 32.7 ± 5.0 Anxiety: 33.3 ± 5.0 Depression: 33.6 ± 5.3 Gender of newborns: not given |
45 | Cohort study 3 months Three groups: - Controls - Depressed mothers - Anxious mothers |
EPDS (Depressed = EPDS > 12) GAD-Q |
Not applicable (number of women were fixed at the beginning of the study) |
Mothers’ perceptions of infant facial expressions | Mothers with postnatal depression were more likely to rate negative infant faces shown for a longer period more negatively than controls. The differences were specific to depression rather than an effect of general postnatal psychopathology as no differences were observed between anxious mothers and controls. There were no other significant differences in maternal ratings of infant faces shown for short periods or for positive or neutral valence faces shown for either length of time. |
| Risk of maltreatment | |||||||
| Choi144 | Japan Mean age: 30.4 ± 4.5 years Female babies: 47.2% |
413 | Cross-sectional study Two groups: - PPD - No PPD |
ZSDS | 41.4% of mild depression; 14.5% of major depression | Violence; neglect; emotional explosion | Depression was strongly influenced by “worries about parenting” in all variances but was not associated with “abusive behavior.” “Worries about parenting” also had a strong influence on the “fear of being abusive,” but did not affect “abusive behavior.” Low “maternal care” had the greatest influence on difficulty of bonding,” which affected “abusive behavior” only. |
| Zajicek-Farber130 | USA Age (years): Depressed: 22.3 ± 4.3 Nondepressed: 22.6 ± 3.9 Female babies: 54.0% |
134 | Cohort study 18 months Two groups: - PPD - No PPD |
EPDS (Depressed = EPDS ⩾ 11) PHQ |
55.2% | Infant health practices | The RR for spanking a child was 4.2 times greater for depressed women than those who were never depressed. |
PPD: postpartum depression; MDD: major depressive disorder; GAD: generalized anxiety disorder; EPDS: Edinburgh Postnatal Depression Scale; BDI: Beck Depression Inventory; CES-D: Center for Epidemiologic Studies Depression Scale; MINI: Mini International Neuropsychiatric Interview; PHQ: Patient Health Questionnaire; SRQ-20: Self-Reporting Questionnaire-20; GAD-Q: Generalized Anxiety Disorder Questionnaire; ZSDS: Zung Self-Rating Depression Scale; SOC: sense of coherence; IFSAC: Inventory of Functional Status after Childbirth; OR: odds ratio; CI: confidence interval; SD: standard deviation; RR: risk ratio; ED: emergency department; ICQ: Infant Care Questionnaire.
Maternal behaviors
Depressed mothers appeared to be more likely to engage in less-healthy practices with their infant compared to nondepressed mothers (Table 17). They were less likely to place their infant in the back-to-sleep position,26,62 to use a car seat,26 and to have a working smoke alarm in the home.26 A higher proportion of the mothers with self-scored depressive symptoms had a poor sense of coherence (comprehensibility, manageability, and meaningfulness) compared with mothers without depressive symptoms.40 Depressive symptoms were also negatively associated with participation in positive enrichment activities with the child.52,53,62 Mothers with PPD were less likely to tell their child stories every day62 and played games less often62 than nondepressed mothers. One study found no significant differences in mother–infant engagement with a picture book between depressed and nondepressed mothers.49 However, this study noted that the infants of these two groups of mothers showed significant differences in their nonverbal behaviors. Depressed mothers also tended to sing faster to their infants than nondepressed mothers.79 Reissland et al.83 demonstrated that depressed mothers preferred to cradle their infant to the left, similar to stressed mothers; nondepressed mothers showed right-sided cradling, similar to nonstressed mothers. Nevertheless, the authors added that the left-sided cradling bias might be due to stress rather than depression experienced by mothers. In addition, as depression increased, mothers scored less favorably on positive affect, contingent responsiveness, physical intrusiveness, punitive tone, verbal content, and general verbalness.52 Low nurturance (defined as behaviors that promotes a child’s psychological growth) and high discipline scores were significantly associated with postnatal depression.53 Finally, one study showed that functional status, an evaluation of overall functional status, household function, social function, personal function, and infant care activities, was negatively correlated with PPD, with the exception of infant care activities.85
Maternal competence
Two studies showed that depressed mothers had a lower perception of their competence than nondepressed mothers (Table 17). The first study highlighted that women with lower parenting self-efficacy were more likely to report depressive symptoms than women with higher parenting self-efficacy.75 The second study concluded that maternal depression was an important factor (32.3% of the total variance) that affected perceived maternal role competence and satisfaction at 6 weeks postpartum.51
Maternal care for infant
All six studies indicated a significant association between maternal PPD and the care that mothers provided to their child (Table 17). Studies showed that EPDS scores were significantly correlated with increased difficulty with infant care145 and that significantly more depressed women had poor parenting practices than women who had not experienced PPD.130 One study highlighted that children of depressed mothers experienced more interruptions and breaks in parental care.37 Another study indicated that mothers with depressive symptoms showed books, played with or talked to the infant and followed routines significantly less often than nondepressed mothers.137 A further study demonstrated that low nurturance and high discipline scores were significantly associated with PPD (higher scores were indicative of greater nurturance and a greater use of discipline behaviors).53 Another study146 reported that children with a depressed mother had a greater mean number of hours of household television exposure during both weekdays and weekends. Bank et al.146 also showed that infants of depressed mothers were exposed to significantly more children’s programming than infants of nondepressed mothers.
Infant health care practices and utilization measures
Six out of eight studies demonstrated an effect of maternal PPD on infant health care practices and utilization (Table 17). The first study128 showed that children whose mothers had depressive symptoms at 2 to 4 months had a reduced probability of receiving age-appropriate vaccinations or age-appropriate well-child visits between 6 and 24 months. This study also showed that these children had an increased likelihood of visiting the emergency department between 1.5 and 2.5 years of age. Mothers who had depressive symptoms also had an increased probability of reporting that their children had sustained injuries. The second study130 highlighted that depressed women differed significantly from women who had not experienced depression in their use of health services for their child. Depressed women were less likely to complete expected well-health visits for their child. The relative risk (RR) of inadequate well-child visits was two times greater for depressed women than for women who had never experienced depression. Children of depressed women were also less likely to complete immunizations within the expected time frame, and they had significantly more visits to the emergency department for acute care. The third study98 demonstrated that infants of mothers with PPD were more likely to have ⩾6 sick or emergency visits and had an increased risk of hospitalization compared to infants of mothers without depression. The fourth study37 reported that most depressed women sought some form of professional help for their child compared to nondepressed women. The fifth study showed that women with PPD consulted more with family physicians and pediatricians than nondepressed mothers did.63 In addition, the rate of PPD was significantly higher in women who consulted health services for medical reasons (nonroutine care) than for those who visited for routine care only.57
Another study26 demonstrated that women with PPD had an increased likelihood of bringing their babies for emergency room visits than women without PPD; however, this association was no longer significant in the adjusted model. Finally, one study142 did not demonstrate a significant effect of maternal PPD on infant health care practices and utilization measures. This study showed that a high risk of maternal depression did not have a negative impact on the completion of routine immunizations in Zambia. However, clinic location and older infant age were significantly associated with incomplete vaccinations.
Maternal perceptions of infants’ patterns
Postpartum depressive symptoms appear to lead to negative maternal perceptions of infant patterns (Table 17). One study showed that mothers with depressive symptoms had a higher perception of their children’s temperament as “more difficult” than nondepressed mothers.40 Another study highlighted that mothers with elevated depressive symptoms were more inclined to report infant crying/fussing, sleeping and temperament problems than mothers without PPD.58 The third study reported that mothers who suffered from PPD were more likely to rate negative infant faces shown for a longer period more negatively than mothers without PPD.50 The authors of this third study concluded that their results highlighted the difficulties that these mothers have in responding to their own infants’ signals. A fourth study demonstrated that the only difference between mothers with and without PPD was their assessment of babies’ faces; neutral baby faces were judged to be less neutral by depressed mothers than by nondepressed mothers.80 Mothers with PPD were also less likely to accurately identify happy infant faces (no differences regarding sad faces were identified) than mothers without PPD.46
Risk of maltreatment
The studies included in the evaluation of the risk of maltreatment are presented in Table 17. One study found that depressed women had a significantly higher risk (4.2 times greater) for spanking their child compared with nondepressed women.130 Another study did not identify a direct effect of maternal PPD on abusive behaviors; however, it demonstrated that PPD strongly influenced worries about how to parent and concerns about how their parenting affected the fear of being abusive.144 This study also highlighted that poor maternal care influenced difficulty with bonding, which also affected abusive behaviors.
Discussion
The purpose of this study was to evaluate the maternal and infant consequences of maternal PPD.
First, as expected, maternal PPD was associated with more negative maternal physical and psychological health and with a worse quality of life. Surprisingly, there were very few results regarding maternal physical health. Only three studies included in the present systematic review showed that depressed mothers presented more PPWR35,67 and lower scores on all SF-36 domains,88 while a systematic review conducted in 2014 evaluated the impact of sleep, stress, and depression on PPWR and found conflicting results, as follows: of seven studies that examined PPD and weight retention, three studies reported nonsignificant associations and four studies reported positive associations.18 As it was decided to reject the systematic and nonsystematic review of this research, this previous systematic review18 was not included. In addition, based on the inclusion criteria of our systematic review, only one67 of the studies included in this previous systematic review18 could be considered in our results (of seven studies, two were published before 2005 and four were rejected based on the title and abstract). Indeed, this study excluded treated PPD, while the previous systematic review18 did not. This is an important difference between the two studies, and it could explain many of the discrepancies between our findings and those of this previous review. The two studies included in the examination of PPWR were both cohort studies and seemed to be of good quality: one study included 75 women followed for 14 months,35 and the other study included 850 women followed for 18 months.67 In addition, both studies used the EPDS to screen for PPD. However, they did not use the same cut-off values: one study used a cut-off value of ⩾1035 and the other study used a cut-off of >12.67 Given this information, we can assert that our results seem to support the risk of PPWR among depressed mothers. As previously observed in cases of women’s health, depressed mothers appeared to be more likely to consult general practitioners, pediatricians, or mental health professionals for medical reasons (nonroutine care) than for routine care.57,63,78 These results suggest that depressed women had more health expenditures than nondepressed women.
Depressed mothers also seemed to experience more difficulties in their social relationships (including relationships with their partners)37,44 and to feel that they received lower quality social support85 than nondepressed mothers. These results are consistent with the qualitative study of Rodrigues et al.,148 who reported poor marital relationships and a lack of practical help and emotional support among depressed mothers. Depressed mothers seemed to have more risky behaviors (including the risk of start smoking again after pregnancy55,84 and an increased prevalence of suicidal ideations).30,33,76,81,85 These results are consistent with a review conducted in 2013, which showed that women who had high depressive symptom scores were also more likely than those with lower scores to engage in risky behaviors (alcohol, illicit drug, or other substances use).20 Nevertheless, according to the inclusion criteria of our systematic review, none of the studies included in this previous review20 could be considered in our analyses (of 12 studies, 5 were published before 2005 and 7 were rejected after reading the title and abstract). PPD therefore appeared to be associated with higher risk behaviors, regardless of whether the women were treated for these symptoms.
Concerning the outcomes of children aged 0 to 3 years, it seemed that the anthropometric consequences of maternal PPD differed between high- and low-income countries. Maternal PPD seemed to have few associations with the weight and length of infants in high-income countries100,113 except during the transient period at the beginning of the newborn’s life.125 However, in low-income populations, maternal PPD seemed to be associated with less infant weight gain and stunting.97,104,110,131,140,142 Moreover, many studies indicated significant and negative associations between maternal postpartum depressive symptoms and infant cognitive development,94,95,99,101,102,107,141,147 language development,94,102,105,116,117,131,132,139 infant behaviors,49,52,110,114,120,121,131,133 overall infant health concerns,48,104,119,122–124,135,136,138 and quality of sleep.104,108
In contrast, the impact of maternal PPD on infant motor development seemed to be controversial: some studies94,95,97 demonstrated a clear effect of PPD on children’s gross and fine motor development, while other studies66,103,107 did not demonstrate this effect. Regardless of whether they showed an effect, all but one study (60 subjects)66 that evaluated the effect of PPD on child motor development were cohort studies and included large samples of subjects (from 360103 to 652 subjects).97 Four of the six studies used the EPDS as a screening tool for depression; the two other studies used the Aga Khan University Anxiety and Depression Scale (AKUADS) or the BDI-II. The studies that used the EPDS did not use the same cut-off values: the two studies that used the EPDS that did not find an effect of PPD on motor development used a cut-off value of ⩾12,103,107 while the two studies that used the EPDS and found evidence in favor of this relationship used cut-off values of ⩾1395 and ⩾10.97 Regarding these conflicting results, there may be a confounding factor. We suggest that PPD could affect the life and home environments66,94,103,117,141 of the infants, which could impact their development, particularly through a lack of caregiving from the mother. Similarly, maternal PPD did not seem to have a direct effect on child social development.66,143
Concerning mother–infant interaction, the majority of studies found a significant association between maternal PPD and the care that mothers provide their children. Therefore, it is reasonable to assume that maternal PPD has a real impact on how a mother cares for her child. Maternal PPD seemed to be associated with poor maternal care, which influenced bonding difficulties and insecure attachments.31,34 Although physical contact does not appear to be necessary for the development of a healthy bond,149,150 difficulty with mother–infant bonding could originate from (early) physical separation or a lack of maternal emotional availability.151 In addition, difficulties in mother-to-infant bonding could reduce the quality of parenting practices37,53,130,137,145,146 and could affect the rates of abusive behavior.144 The quality of the mother–infant relationship seemed to have an influence on the overall development of these infants; however, it was also affected by the way mothers cared for their child. Maternal PPD seemed to have a negative effect on these parameters, which created a vicious circle around the mother–child couple. It is interesting to note that successful treatment of PPD may not be sufficient to improve infants’ attachment, temperament, and cognitive development.5 In addition, many studies identified a significantly negative effect of maternal depressive symptoms on breastfeeding and/or its parameters (e.g. discontinued breastfeeding, less-healthy feeding practices, breastfeeding problems, lower satisfaction, or reduced confidence).25,41,45,59,62,77,89,90,118,119,137 These results are consistent with a systematic review published in 2014 that also showed negative effects of PPD on breastfeeding.22 In this systematic review, PPD was associated with a shorter breastfeeding duration in almost all studies; therefore, PPD appeared to be associated with more breastfeeding problems, regardless of whether women were treated for PPD symptoms. The authors of several studies noted that PPD predicted and was predicted by breastfeeding cessation.22 Many studies found a significant and negative association between maternal PPD and the duration of breastfeeding and a positive association between maternal PPD and breastfeeding problems. The Dias and Figueiredo’s22 systematic review included 48 studies, 14 which were included in the present systematic review (the other studies were published before 2005 (n = 17) or rejected based on the title and abstract (n = 17)).
Some studies64,108,121 compared the impact of chronic depression versus transient depression on child development and found that chronic maternal depression seemed to have a more serious impact on child development. In addition, some studies highlighted the importance of other environmental factors on the delay in child development, such as the infants’ life environment66,94,103,117,141 or maternal sensitivity.115,127,147 Therefore, maternal PPD could also indirectly impact a child’s development via a demonstrated lack of caregiving. The quality of the mother–infant relationship is critical for infant development, and maternal PPD could have a negative effect. Moreover, the relationship a mother develops with her child is dependent on the mother’s own emotional health.94 One study explained that a potential implication of the results was that the infants of mothers with PPD reacted to negative maternal nonverbal engagement by displaying negative behaviors, and they showed less interest in interacting.49 Infants’ dissatisfaction with their environment or their relationship with their mothers could explain their more difficult temperaments, greater display of internalization or communication problems, more problems relating to their mothers, and more difficulties in social development, particularly in their ability to relate to other individuals. In addition, lower socioeconomic groups seemed to be at a higher risk. Thus, an unfavorable environment should be a warning signal for caregivers. Therefore, in these subgroups (including populations from low-income countries), the prevention and early recognition of maternal PPD may improve the optimal development of children and the care their mothers provide.
In conclusion, maternal PPD seems to have many negative effects on both child and maternal health; however, it is important to highlight that the studies included were heterogeneous in their designs, the tools they used to assess PPD and the large group of confounding factors that was considered (even though adjusted results were used when they were available). Nevertheless, efforts to screen and prevent maternal PPD are critical.
Need for a consensus regarding PPD diagnosis
A difficulty emerged during the evaluation of the maternal and infant consequences of untreated PPD as a result of the heterogeneity of the PPD diagnosis. While PPD is not a recent pathology, a consensus regarding the “best diagnostic tool” does not exist. The prevalence of maternal depression therefore depends on the definition and/or the tool used to diagnose PPD.3,6–8 In addition, the prevalence of PPD may depend on the cut-off values used with the same diagnostic tool.
The 122 studies included in this systematic review also used different diagnostic tools. PPD was mainly diagnosed using the EPDS (68 studies); however, it was also assessed using various other questionnaires, such as the BDI (10 studies), the CES-D (10 studies), the MINI (4 studies), the SCID (4 studies), the DSM-IV (2 studies), the PHQ-9 (3 studies), the PHQ-8 (1 study), the PHQ-D (1 study), the CIDI (3 studies), the PDSS (3 studies), the BSI (2 studies), the SQR-20 (2 studies), the GAD-Q (2 studies), and the HDRS (1 study). Therefore, the prevalence of PPD varied among these studies, from 2.7% in a population of Pakistani mothers at 18 months postpartum94 to 68.8% in a population of Australian mothers at 4 months postpartum.64
Concerning the cut-off values, there were also several disparities. For example, as shown Tables 1–17, among the studies that used the EPDS, the authors used different cut-off values to establish the diagnosis of PPD; cut-off values of 8,57 9,40 10,44 11,132 12,31 13,34 or 1465 were used to screen for postnatal depression. Cox et al.4 showed that a cut-off point of 13 or more on the EPDS indicates a probable depression with a sensitivity of 86% and a specificity of 78% in the postnatal period. Another study indicated that the optimal cut-off for probable major depression during the antenatal period may be higher (15 or more).152 Some authors used different cut-off values to classify depression as mild/moderate (e.g. EPDS ⩾ 886 or EPDS ⩾ 10 and ⩽12108) or severe (EPDS ⩾ 1286 or EPDS ⩾ 13108). Other authors considered the EPDS a screening tool that measures probable depression and does not provide a clinical diagnosis of depression; these authors considered an EPDS score of 13 indicative of PPD.112
Although previous research conducted a receiver operating characteristic curve (ROC) analysis comparing the EPDS, BDI, and HRSD scores with the SCID Mood Module and showed that these scales were highly predictive of a major depressive episode,153 future studies should develop a consensus to standardize the tools researchers use to diagnose depression during the postpartum period. The EPDS4 seems to be the most commonly used PPD diagnostic tool. Nevertheless, researchers must agree on cut-off values to ensure the validity and reliability of the tool. For example, in 2006, Matthey et al.154 recommended the use of a validated score of 13 or higher on the EPDS when reporting probable major depression during the postnatal period and a score of 15 or higher during the antenatal period (particularly for English-speaking women). However, it seems that these recommendations are not always followed. In any case, it is sometimes difficult to compare the outcomes of PPD because of the heterogeneity of its diagnosis. It is important to be careful given that in some cases, the results of this systematic review combined results from studies that were heterogeneous in terms of design (cross-sectional vs cohort studies) and methodology (e.g. screening tools used for PPD or length of follow-up).
Implications for practice
Social support seems to have a protective effect against postnatal depression.8,155,156 However, depressed mothers presented lower perceived social support than nondepressed mothers.66 Social support also seems to stimulate maternal self-efficacy,157 which plays a key role in the process of constructing parenthood.158 A study showed that mothers who had a strong belief in their maternal abilities had better outcomes in terms of emotional well-being, attachment to the child and adaptation to their new role.159 In addition, maternal self-efficacy is positively associated with the mothers’ coping strategies.
Even when everything seems to be going well, the majority of women seem to feel fears or anxiety at the beginning of maternity given the sudden changes in their role.160 It is normal for mothers to be worried about the safety and well-being of their child. Nevertheless, given all the identity disturbances related to the arrival of a baby, it is not uncommon for women to encounter episodes of psychological distress of varying duration and degrees of severity during the postnatal period. Childbirth may be a traumatic experience for a woman.161 A lack of social support, pain during the first stage of labor, feelings of powerlessness, unfulfilled expectations, and negative interactions with medical personnel are examples of factors that can influence the perception of a traumatic experience following childbirth. These findings suggest several intervention points for health care practitioners, including opportunities to discuss the birth during the postpartum period.161
Nevertheless, one study indicated a discrepancy between professionals’ perceptions of maternal needs and the needs that mothers actually had.162 Professionals seemed to be more concerned about needs during pregnancy than during the postpartum period. Moreover, they seemed to identify very few unmet needs during the postnatal period, while the mothers tend to feel neglected during this period.162 However, many studies have shown that mothers have important physical and emotional needs during the year after childbirth.155,158,160,162–179 In addition, the present systematic review shows that the health of infants and children is intimately associated with the health of their mothers.
These elements suggest that the promotion of maternal health by professionals cannot end at the birth of the newborn or at the 6-week postpartum visit.164 The needs of mothers take longer than 6 weeks to resolve. Fahey and Shenassa164 noted that a healthy postnatal period depends on a woman’s ability to effectively employ her own skills to satisfy her own needs and those of her family. Thus, postnatal care providers must understand that women’s health needs during this transition period are not limited to physical recovery, and they must identify care strategies that will help women develop the required skills to appropriately meet their needs.
The recommendations in terms of maternal health promotion are increasingly moving toward a holistic vision of women’s health. It is necessary to go beyond health care itself to meet the complete needs of mothers;164,180–182 this is even more true as maternity leave is increasingly shortened, thus presenting additional risks of insufficient education and health promotion models for mothers.183 It is important that professionals implement rigorous follow-up procedures outside the hospital to continue to support parents during this life event.184
Strengths and limitations of the study
To our knowledge, this study is the first systematic review in several decades to evaluate the consequences of untreated maternal PPD in both mothers and their children from 0 to 3 years of age. Our study included 122 studies and encompassed all outcomes for mothers and children that have been described since January 2005. The limitations of this study are that given the number of abstracts initially included in the review, study selection and data extraction were not performed using a double-blinded method, and an assessment of the studies’ methodological quality was not performed. Nevertheless, the inclusion and exclusion criteria were rigorously discussed and defined at the beginning of the study by the two researchers who performed the review. In addition, if there was doubt regarding an abstract or an article, the article was discussed, and the researchers reached a consensus regarding its inclusion or exclusion. Another limitation of this study is that given the substantial number of maternal PPD outcomes, the present review compares heterogeneous studies that used various designs (cohort vs cross-sectional studies) and tools to assess PPD. Therefore, it is important to consider that potential confounding factors could be present.
Conclusion
We conclude that maternal postnatal depression has negative consequences for both mothers who suffer from this pathology and their children up to 3 years of age. PPD has important impacts, mainly on mothers’ psychological health, quality of life, and interactions with their infant, partner, and relatives. Depressed women are caught in a vicious circle in which they become sadder and angrier and have increasingly lower perceptions of their competence. The accumulation of these elements creates an environment that is not conducive to the personal development of mothers or the optimal development of a child. The present systematic review shows that the health of infants and children is intimately associated with the health of their mothers. In addition, severe or chronic maternal depression seems to present a higher risk to children’s development than milder depression. Thus, maternal PPD has many direct and indirect negative effects on the development of a child, including lower quality of the home environment and decreased maternal sensitivity and caregiving. It therefore seems important to detect and treat depression in the postnatal period as early as possible to avoid harmful consequences. The risks are greater for children in low-income populations. Consequently, more attention should be paid to these areas.
Acknowledgments
The author would like to thank all the co-authors of this article, especially Germain Honvo for helping in the data extraction.
Appendix
Appendix 1.
Search strategy and search terms used for this systematic research.
| 1. Postpartum depression.mp 2. Depression, Postpartum/ 3. Post partum depression.mp 4. Post-partum depression.mp 5. OR/1-4 6. Postnatal depression.mp 7. Post natal depression.mp 8. Post-natal depression.mp 9. OR/6-8 10. Puerperal depression.mp 11. Exp postpartum depression/ 12. Exp postanal depression/ 13. OR/11-12 14. OR/5,9-10,13 15. Limit to English language 16. Limit 15 to yr =”2005-Current” 17. Limit 16 to humans |
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Olivier Bruyère  https://orcid.org/0000-0003-4269-9393
https://orcid.org/0000-0003-4269-9393
References
- 1. Cristescu T, Behrman S, Jones SV, et al. Be vigilant for perinatal mental health problems. Practitioner 2015; 259(1780): 19–232. [PubMed] [Google Scholar]
- 2. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
- 3. O’Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol 2014; 28(1): 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987; 150: 782–786. [DOI] [PubMed] [Google Scholar]
- 5. Pearlstein T, Howard M, Salisbury A, et al. Postpartum depression. Am J Obstetr Gynecol 2009; 200(4): 357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gavin NI, Gaynes BN, Lohr KN, et al. Perinatal depression: a systematic review of prevalence and incidence. Obstetr Gynecol 2005; 106(5 Pt. 1): 1071–1083. [DOI] [PubMed] [Google Scholar]
- 7. Halbreich U, Karkun S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord 2006; 91(2–3): 97–111. [DOI] [PubMed] [Google Scholar]
- 8. Norhayati MN, Nik Hazlina NH, Asrenee AR, et al. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord 2014; 175: 34–52. [DOI] [PubMed] [Google Scholar]
- 9. Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Arch Womens Ment Health 2005; 8(3): 141–153. [DOI] [PubMed] [Google Scholar]
- 10. Misri S, Reebye P, Kendrick K, et al. Internalizing behaviors in 4-year-old children exposed in utero to psychotropic medications. Am J Psychiatry 2006; 163(6): 1026–1032. [DOI] [PubMed] [Google Scholar]
- 11. Carter AS, Garrity-Rokous FE, Chazan-Cohen R, et al. Maternal depression and comorbidity: predicting early parenting, attachment security, and toddler social-emotional problems and competencies. J Am Acad Child Adolesc Psychiatry 2001; 40(1): 18–26. [DOI] [PubMed] [Google Scholar]
- 12. Sohr-Preston SL, Scaramella LV. Implications of timing of maternal depressive symptoms for early cognitive and language development. Clin Child Fam Psychol Rev 2006; 9(1): 65–83. [DOI] [PubMed] [Google Scholar]
- 13. Oberlander TF, Reebye P, Misri S, et al. Externalizing and attentional behaviors in children of depressed mothers treated with a selective serotonin reuptake inhibitor antidepressant during pregnancy. Arch Pediatr Adolesc Med 2007; 161(1): 22–29. [DOI] [PubMed] [Google Scholar]
- 14. Weissman MM, Pilowsky DJ, Wickramaratne PJ, et al. Remissions in maternal depression and child psychopathology: a STAR*D-child report. JAMA 2006; 295(12): 1389–1398. [DOI] [PubMed] [Google Scholar]
- 15. Hay DF, Pawlby S, Angold A, et al. Pathways to violence in the children of mothers who were depressed postpartum. Dev Psychol 2003; 39(6): 1083–1094. [DOI] [PubMed] [Google Scholar]
- 16. Weissman MM, Wickramaratne P, Nomura Y, et al. Offspring of depressed parents: 20 years later. Am J Psychiatry 2006; 163(6): 1001–1008. [DOI] [PubMed] [Google Scholar]
- 17. Society CP. Maternal depression and child development. Paediatr Child Health 2004; 9(8): 575–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Xiao RS, Kroll-Desrosiers AR, Goldberg RJ, et al. The impact of sleep, stress, and depression on postpartum weight retention: a systematic review. J Psychosom Res 2014; 77(5): 351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Milgrom J, Skouteris H, Worotniuk T, et al. The association between ante- and postnatal depressive symptoms and obesity in both mother and child: a systematic review of the literature. Women’s Health Issues 2016; 22(3): e319–e328. [DOI] [PubMed] [Google Scholar]
- 20. Chapman SLC, Wu L-T. Postpartum substance use and depressive symptoms: a review. Women Health 2013; 53(5): 479–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jones E, Coast E. Social relationships and postpartum depression in South Asia: a systematic review. Int J Soc Psychiatry 2013; 59(7): 690–700. [DOI] [PubMed] [Google Scholar]
- 22. Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. J Affect Disord 2014; 171: 142–154. [DOI] [PubMed] [Google Scholar]
- 23. Vliegen N, Casalin S, Luyten P. The course of postpartum depression: a review of longitudinal studies. Harv Rev Psychiatry 2016; 22(1): 1–22. [DOI] [PubMed] [Google Scholar]
- 24. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mallan KM, Daniels LA, Wilson JL, et al. Association between maternal depressive symptoms in the early post-natal period and responsiveness in feeding at child age 2 years. Matern Child Nutr 2015; 11(4): 926–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Balbierz A, Bodnar-Deren S, Wang JJ, et al. Maternal depressive symptoms and parenting practices 3-months postpartum. Matern Child Health J 2015; 19(6): 1212–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Curtis MA, Corman H, Noonan K, et al. Maternal depression as a risk factor for family homelessness. Am J Public Health 2014; 104(9): 1664–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kim JJ, La Porte LM, Saleh MP, et al. Suicide risk among perinatal women who report thoughts of self-harm on depression screens. Obstetr Gynecol 2015; 125(4): 885–893. [DOI] [PubMed] [Google Scholar]
- 29. Dubber S, Reck C, Muller M, et al. Postpartum bonding: the role of perinatal depression, anxiety and maternal–fetal bonding during pregnancy. Arch Womens Ment Health 2015; 18(2): 187–195. [DOI] [PubMed] [Google Scholar]
- 30. Pope CJ, Xie B, Sharma V, et al. A prospective study of thoughts of self-harm and suicidal ideation during the postpartum period in women with mood disorders. Arch Womens Ment Health 2013; 16(6): 483–488. [DOI] [PubMed] [Google Scholar]
- 31. Orün E, Yalcin SS, Mutlu B. Relations of maternal psychopathologies, social-obstetrical factors and mother-infant bonding at 2-month postpartum: a sample of Turkish mothers. World J Pediatr 2013; 9(4): 350–355. [DOI] [PubMed] [Google Scholar]
- 32. Kawano A, Emori Y. The relationship between maternal postpartum psychological state and breast milk secretory immunoglobulin A level. J Am Psychiatr Nurses Assoc 2015; 21(1): 23–30. [DOI] [PubMed] [Google Scholar]
- 33. Do T, Hu Z, Otto J, et al. Depression and suicidality during the postpartum period after first time deliveries, active component service women and dependent spouses, U.S. Armed Forces, 2007-2012. MSMR 2013; 20(9): 2–7. [PubMed] [Google Scholar]
- 34. O’Higgins M, Roberts IS, Glover V, et al. Mother-child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Arch Womens Ment Health 2013; 16(5): 381–389. [DOI] [PubMed] [Google Scholar]
- 35. Biesmans K, Franck E, Ceulemans C, et al. Weight during the postpartum period: what can health care workers do. Matern Child Health J 2013; 17(6): 996–1004. [DOI] [PubMed] [Google Scholar]
- 36. Prenoveau J, Craske M, Counsell N, et al. Postpartum GAD is a risk factor for postpartum MDD: the course and longitudinal relationships of postpartum GAD and MDD. Depress Anxiety 2013; 30(6): 506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Vliegen N, Casalin S, Luyten P, et al. Hospitalization-based treatment for postpartum depressed mothers and their babies: rationale, principles, and preliminary follow-up data. Psychiatry 2013; 76(2): 150–168. [DOI] [PubMed] [Google Scholar]
- 38. Faisal-Cury A, Huang H, Chan Y-F, et al. The relationship between depressive/anxiety symptoms during pregnancy/postpartum and sexual life decline after delivery. J Sex Med 2013; 10(5): 1343–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Taylor J, Johnson M. The role of anxiety and other factors in predicting postnatal fatigue: from birth to 6 months. Midwifery 2013; 29(5): 526–534. [DOI] [PubMed] [Google Scholar]
- 40. Kerstis B, Engstrom G, Edlund B, et al. Association between mothers’ and fathers’ depressive symptoms, sense of coherence and perception of their child’s temperament in early parenthood in Sweden. Scand J Public Health 2013; 41(3): 233–239. [DOI] [PubMed] [Google Scholar]
- 41. Stuebe AM, Grewen K, Meltzer-Brody S. Association between maternal mood and oxytocin response to breastfeeding. J Womens Health (Larchmt) 2013; 22(4): 352–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gollan JK, Hoxha D, Getch S, et al. Affective information processing in pregnancy and postpartum with and without major depression. Psychiatry Res 2013; 206(2–3): 206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Muzik M, Bocknek EL, Broderick A, et al. Mother–infant bonding impairment across the first 6 months postpartum: the primacy of psychopathology in women with childhood abuse and neglect histories. Arch Womens Ment Health 2013; 16(1): 29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lilja G, Edhborg M, Nissen E. Depressive mood in women at childbirth predicts their mood and relationship with infant and partner during the first year postpartum. Scand J Caring Sci 2012; 26(2): 245–253. [DOI] [PubMed] [Google Scholar]
- 45. Gagliardi L, Petrozzi A, Rusconi F. Symptoms of maternal depression immediately after delivery predict unsuccessful breast feeding. Arch Dis Child 2012; 97(4): 355–357. [DOI] [PubMed] [Google Scholar]
- 46. Arteche A, Joormann J, Harvey A, et al. The effects of postnatal maternal depression and anxiety on the processing of infant faces. J Affect Disord 2011; 133(1–2): 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Edhborg M, Nasreen H-E, Kabir ZN. Impact of postpartum depressive and anxiety symptoms on mothers’ emotional tie to their infants 2-3 months postpartum: a population-based study from rural Bangladesh. Arch Womens Ment Health 2011; 14(4): 307–316. [DOI] [PubMed] [Google Scholar]
- 48. Darcy JM, Grzywacz JG, Stephens RL, et al. Maternal depressive symptomatology: 16-month follow-up of infant and maternal health-related quality of life. JABFM 2016; 24(3): 249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Reissland N, Burt M. Bi-directional effects of depressed mood in the postnatal period on mother-infant non-verbal engagement with picture books. Infant Behav Dev 2010; 33(4): 613–618. [DOI] [PubMed] [Google Scholar]
- 50. Stein A, Arteche A, Lehtonen A, et al. Interpretation of infant facial expression in the context of maternal postnatal depression. Infant Behav Dev 2010; 33(3): 273–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ngai F-W, Wai-Chi Chan S, Ip WY. Predictors and correlates of maternal role competence and satisfaction. Nurs Res 2010; 59(3): 185–193. [DOI] [PubMed] [Google Scholar]
- 52. Lanzi RG, Bert SC, Jacobs BK. Depression among a sample of first-time adolescent and adult mothers. J Child Adolesc Psychiatr Nurs 2009; 22(4): 194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Cowley-Malcolm ET, Fairbairn-Dunlop TP, Paterson J, et al. Child discipline and nurturing practices among a cohort of Pacific mothers living in New Zealand. Pac Health Dialog 2009; 15(1): 36–45. [PubMed] [Google Scholar]
- 54. Korja R, Savonlahti E, Haataja L, et al. Attachment representations in mothers of preterm infants. Infant Behav Dev 2009; 32(3): 305–311. [DOI] [PubMed] [Google Scholar]
- 55. Park ER, Chang Y, Quinn V, et al. The association of depressive, anxiety, and stress symptoms and postpartum relapse to smoking: a longitudinal study. Nicotine Tob Res 2009; 11(6): 707–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Korja R, Savonlahti E, Ahlqvist-Bjorkroth S, et al. Maternal depression is associated with mother-infant interaction in preterm infants. Acta Paediatr 2008; 97(6): 724–730. [DOI] [PubMed] [Google Scholar]
- 57. Chee CYI, Chong Y-S, Ng TP, et al. The association between maternal depression and frequent non-routine visits to the infant’s doctor—a cohort study. J Affect Disord 2008; 107(1–3): 247–253. [DOI] [PubMed] [Google Scholar]
- 58. Orhon FS, Ulukol B, Soykan A. Postpartum mood disorders and maternal perceptions of infant patterns in well-child follow-up visits. Acta Paediatr 2007; 96(12): 1777–1783. [DOI] [PubMed] [Google Scholar]
- 59. Dennis C-L, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes. Acta Paediatr 2007; 96(4): 590–594. [DOI] [PubMed] [Google Scholar]
- 60. McCarter-Spaulding D, Horowitz JA. How does postpartum depression affect breastfeeding? MCN 2017; 32(1): 10–17. [DOI] [PubMed] [Google Scholar]
- 61. Moehler E, Brunner R, Wiebel A, et al. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother-child bonding. Arch Womens Ment Health 2006; 9(5): 273–278. [DOI] [PubMed] [Google Scholar]
- 62. Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics 2006; 118(2): 659–668. [DOI] [PubMed] [Google Scholar]
- 63. Eilat-Tsanani S, Merom A, Romano S, et al. The effect of postpartum depression on women’s consultations with physicians. Isr Med Assoc J 2006; 8(6): 406–410. [PubMed] [Google Scholar]
- 64. McMahon CA, Barnett B, Kowalenko NM, et al. Maternal attachment state of mind moderates the impact of postnatal depression on infant attachment. J Child Psychol Psychiatry 2006; 47(7): 660–669. [DOI] [PubMed] [Google Scholar]
- 65. Hatton DC, Harrison-Hohner J, Coste S, et al. Symptoms of postpartum depression and breastfeeding. J Human Lactat 2005; 21(4): 444–449, quiz 450–454. [DOI] [PubMed] [Google Scholar]
- 66. Wang S-Y, Chen C-H, Chin C-C, et al. Impact of postpartum depression on the mother-infant couple. Birth 2005; 32(1): 39–44. [DOI] [PubMed] [Google Scholar]
- 67. Herring SJ, Rich-Edwards JW, Oken E, et al. Association of postpartum depression with weight retention 1 year after childbirth. Obesity 2008; 16(6): 1296–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Jagodzinski T, Fleming MF. Postpartum and alcohol-related factors associated with the relapse of risky drinking. J Stud Alcohol Drugs 2007; 68(6): 879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Feldens CA, Vitolo MR, Rauber F, et al. Risk factors for discontinuing breastfeeding in southern brazil: a survival analysis. Matern Child Health J 2012; 16(6): 1257–1265. [DOI] [PubMed] [Google Scholar]
- 70. Annagür A, Annagür BB, Sahin A, et al. Is maternal depressive symptomatology effective on success of exclusive breastfeeding during postpartum 6 weeks. Breastfeed Med 2013; 8(1): 53–57. [DOI] [PubMed] [Google Scholar]
- 71. Nishioka E, Haruna M, Ota E, et al. A prospective study of the relationship between breastfeeding and postpartum depressive symptoms appearing at 1-5 months after delivery. J Affect Disord 2011; 133(3): 553–559. [DOI] [PubMed] [Google Scholar]
- 72. Figueiredo B, Canario C, Field T. Breastfeeding is negatively affected by prenatal depression and reduces postpartum depression. Psychol Med 2014; 44(5): 927–936. [DOI] [PubMed] [Google Scholar]
- 73. Dagher RK, Hofferth SL, Lee Y. Maternal depression, pregnancy intention, and return to paid work after childbirth. Women’s Health Issues 2014; 24(3): e297–e303. [DOI] [PubMed] [Google Scholar]
- 74. Khajehei M, Doherty M, Tilley PJM, et al. Prevalence and risk factors of sexual dysfunction in postpartum Australian women. J Sex Med 2015; 12(6): 1415–1426. [DOI] [PubMed] [Google Scholar]
- 75. Kohlhoff J, Barnett B. Parenting self-efficacy: links with maternal depression, infant behaviour and adult attachment. Early Hum Dev 2013; 89(4): 249–256. [DOI] [PubMed] [Google Scholar]
- 76. Tavares D, Quevedo L, Jansen K, et al. Prevalence of suicide risk and comorbidities in postpartum women in Pelotas. Br J Psychiatry 2012; 34(3): 270–276. [DOI] [PubMed] [Google Scholar]
- 77. Kondo N, Suda Y, Nakao A, et al. Maternal psychosocial factors determining the concentrations of transforming growth factor-beta in breast milk. Pediatr Allergy Immunol 2011; 22(8): 853–861. [DOI] [PubMed] [Google Scholar]
- 78. McCallum SM, Rowe HJ, Gurrin L, et al. Unsettled infant behaviour and health service use: a cross-sectional community survey in Melbourne, Australia. J Paediatr Child Health 2011; 47(11): 818–823. [DOI] [PubMed] [Google Scholar]
- 79. De l’Etoile SK, Leider CN. Acoustic parameters of infant-directed singing in mothers with depressive symptoms. Infant Behav Dev 2011; 34(2): 248–256. [DOI] [PubMed] [Google Scholar]
- 80. Gil S, Teissedre F, Chambres P, et al. The evaluation of emotional facial expressions in early postpartum depression mood: a difference between adult and baby faces. Psychiatry Res 2011; 186(2–3): 281–286. [DOI] [PubMed] [Google Scholar]
- 81. Paris R, Bolton RE, Weinberg MK. Postpartum depression, suicidality, and mother-infant interactions. Arch Womens Ment Health 2009; 12(5): 309–321. [DOI] [PubMed] [Google Scholar]
- 82. Figueiredo B, Costa R, Pacheco A, et al. Mother-to-infant emotional involvement at birth. Matern Child Health J 2009; 13(4): 539–549. [DOI] [PubMed] [Google Scholar]
- 83. Reissland N, Hopkins B, Helms P, et al. Maternal stress and depression and the lateralisation of infant cradling. J Child Psychol Psychiatry 2009; 50(3): 263–269. [DOI] [PubMed] [Google Scholar]
- 84. Allen AM, Prince CB, Dietz PM. Postpartum depressive symptoms and smoking relapse. Am J Prev Med 2009; 36(1): 9–12. [DOI] [PubMed] [Google Scholar]
- 85. Posmontier B. Functional status outcomes in mothers with and without postpartum depression. J Midwifery Womens Health 2008; 53(4): 310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. De Tychey C, Briançon S, Lighezzolo J, et al. Quality of life, postnatal depression and baby gender. J Clin Nurs 2007; 17: 312–322. [DOI] [PubMed] [Google Scholar]
- 87. Whitaker RC, Orzol SM, Kahn RS. The co-occurrence of smoking and a major depressive episode among mothers 15 months after delivery. Prev Med 2007; 45(6): 476–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Da Costa D, Dritsa M, Rippen N, et al. Health-related quality of life in postpartum depressed women. Arch Womens Ment Health 2006; 9(2): 95–102. [DOI] [PubMed] [Google Scholar]
- 89. Dunn S, Davies B, McCleary L, et al. The relationship between vulnerability factors and breastfeeding outcome. J Obstet Gynecol Neonatal Nurs 2006; 35(1): 87–97. [DOI] [PubMed] [Google Scholar]
- 90. Thome M, Alder EM, Ramel A. A population-based study of exclusive breastfeeding in Icelandic women: is there a relationship with depressive symptoms and parenting stress. Int J Nurs Stud 2006; 43(1): 11–20. [DOI] [PubMed] [Google Scholar]
- 91. Flores-Quijano ME, Cordova A, Contreras-Ramirez V, et al. Risk for postpartum depression, breastfeeding practices, and mammary gland permeability. J Hum Lact 2008; 24(1): 50–57. [DOI] [PubMed] [Google Scholar]
- 92. Zubaran C, Foresti K. The correlation between breastfeeding self-efficacy and maternal postpartum depression in southern Brazil. Sex Reprod Healthc 2013; 4(1): 9–15. [DOI] [PubMed] [Google Scholar]
- 93. Barr JA, Beck CT. Infanticide secrets: qualitative study on postpartum depression. Can Fam Physician 2008; 54(12): 1716.e5–1717.e5. [PMC free article] [PubMed] [Google Scholar]
- 94. Ali NS, Mahmud S, Khan A, et al. Impact of postpartum anxiety and depression on child’s mental development from two peri-urban communities of Karachi, Pakistan: a quasi-experimental study. BMC Psychiatry 2013; 13: 274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Koutra K, Chatzi L, Bagkeris M, et al. Antenatal and postnatal maternal mental health as determinants of infant neurodevelopment at 18 months of age in a mother-child cohort (Rhea Study) in Crete, Greece. Soc Psychiatry Psychiatr Epidemiol 2013; 48(8): 1335–1345. [DOI] [PubMed] [Google Scholar]
- 96. Walker MJ, Davis C, Al-Sahab B, et al. Reported maternal postpartum depression and risk of childhood psychopathology. Matern Child Health J 2013; 17(5): 907–917. [DOI] [PubMed] [Google Scholar]
- 97. Nasreen H-E, Kabir ZN, Forsell Y, et al. Impact of maternal depressive symptoms and infant temperament on early infant growth and motor development: results from a population based study in Bangladesh. J Affect Disord 2013; 146(2): 254–261. [DOI] [PubMed] [Google Scholar]
- 98. Farr SL, Dietz PM, Rizzo JH, et al. Health care utilisation in the first year of life among infants of mothers with perinatal depression or anxiety. Paediatr Perinat Epidemiol 2013; 27(1): 81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Azak S. Maternal depression and sex differences shape the infants’ trajectories of cognitive development. Infant Behav Dev 2012; 35(4): 803–814. [DOI] [PubMed] [Google Scholar]
- 100. Ertel KA, Kleinman K, van Rossem L, et al. Maternal perinatal depression is not independently associated with child body mass index in the Generation R Study: methods and missing data matter. J Clin Epidemiol 2012; 65(12): 1300–1309. [DOI] [PubMed] [Google Scholar]
- 101. McManus BM, Poehlmann J. Parent-child interaction, maternal depressive symptoms and preterm infant cognitive function. Infant Behav Dev 2012; 35(3): 489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Kaplan PS, Danko CM, Kalinka CJ, et al. A developmental decline in the learning-promoting effects of infant-directed speech for infants of mothers with chronically elevated symptoms of depression. Infant Behav Dev 2012; 35(3): 369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Piteo AM, Yelland LN, Makrides M. Does maternal depression predict developmental outcome in 18 month old infants. Early Hum Dev 2012; 88(8): 651–655. [DOI] [PubMed] [Google Scholar]
- 104. Gress-Smith JL, Luecken LJ, Lemery-Chalfant K, et al. Postpartum depression prevalence and impact on infant health, weight, and sleep in low-income and ethnic minority women and infants. Matern Child Health J 2012; 16(4): 887–893. [DOI] [PubMed] [Google Scholar]
- 105. Quevedo LA, Silva RA, Godoy R, et al. The impact of maternal post-partum depression on the language development of children at 12 months. Child Care Health Dev 2012; 38(3): 420–424. [DOI] [PubMed] [Google Scholar]
- 106. Tharner A, Luijk MPCM, van Ijzendoorn MH, et al. Maternal lifetime history of depression and depressive symptoms in the prenatal and early postnatal period do not predict infant-mother attachment quality in a large, population-based Dutch cohort study. Attach Human Dev 2012; 14(1): 63–81. [DOI] [PubMed] [Google Scholar]
- 107. Sutter-Dallay AL, Murray L, Dequae-Merchadou L, et al. A prospective longitudinal study of the impact of early postnatal vs. chronic maternal depressive symptoms on child development. Eur Psychiatry 2011; 26(8): 484–489. [DOI] [PubMed] [Google Scholar]
- 108. Tavares Pinheiro KA, Pinheiro RT, Silva RA, et al. Chronicity and severity of maternal postpartum depression and infant sleep disorders: a population-based cohort study in southern Brazil. Infant Behav Dev 2011; 34(2): 371–373. [DOI] [PubMed] [Google Scholar]
- 109. Ertel KA, Koenen KC, Rich-Edwards JW, et al. Maternal depressive symptoms not associated with reduced height in young children in a US prospective cohort study. PLoS ONE 2010; 5(10): e13656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Avan B, Richter LM, Ramchandani PG, et al. Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch Dis Child 2010; 95(9): 690–695. [DOI] [PubMed] [Google Scholar]
- 111. Bagner DM, Pettit JW, Lewinsohn PM, et al. Effect of maternal depression on child behavior: a sensitive period. J Am Acad Child Adolesc Psychiatry 2010; 49(7): 699–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Ertel KA, Koenen KC, Rich-Edwards JW, et al. Antenatal and postpartum depressive symptoms are differentially associated with early childhood weight and adiposity. Paediatr Perinat Epidemiol 2010; 24(2): 179–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Grote V, Vik T, von Kries R, et al. Maternal postnatal depression and child growth: a European cohort study. BMC Pediatr 2010; 10: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Hanington L, Ramchandani P, Stein A. Parental depression and child temperament: assessing child to parent effects in a longitudinal population study. Infant Behav Dev 2010; 33(1): 88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Feldman R, Granat A, Pariente C, et al. Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. J Am Acad Child Adolesc Psychiatry 2009; 48(9): 919–927. [DOI] [PubMed] [Google Scholar]
- 116. Paulson JF, Keefe HA, Leiferman JA. Early parental depression and child language development. J Child Psychol Psychiatry 2009; 50(3): 254–262. [DOI] [PubMed] [Google Scholar]
- 117. Stein A, Malmberg L-E, Sylva K, et al. The influence of maternal depression, caregiving, and socioeconomic status in the post-natal year on children’s language development. Child Care Health Dev 2008; 34(5): 603–612. [DOI] [PubMed] [Google Scholar]
- 118. Hasselmann MH, Werneck GL, Silva CVC. Symptoms of postpartum depression and early interruption of exclusive breastfeeding in the first two months of life. Cad Saude Publica 2008; 24(Suppl. 2): S341–S352. [DOI] [PubMed] [Google Scholar]
- 119. Adewuya AO, Ola BO, Aloba OO, et al. Impact of postnatal depression on infants’ growth in Nigeria. J Affect Disord 2008; 108(1–2): 191–193. [DOI] [PubMed] [Google Scholar]
- 120. Gao W, Paterson J, Abbott M, et al. Maternal mental health and child behaviour problems at 2 years: findings from the Pacific Islands Families Study. Aust N Z J Psychiatry 2007; 41(11): 885–895. [DOI] [PubMed] [Google Scholar]
- 121. Moehler E, Kagan J, Parzer P, et al. Childhood behavioral inhibition and maternal symptoms of depression. Psychopathology 2007; 40(6): 446–452. [DOI] [PubMed] [Google Scholar]
- 122. Rahman A, Bunn J, Lovel H, et al. Maternal depression increases infant risk of diarrhoeal illness: a cohort study. Arch Dis Child 2007; 92(1): 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Moscardino U, Axia G, Altoe G. The role of maternal depressed mood and behavioural soothing on infant response to routine vaccination. Acta Paediatr 2006; 95(12): 1680–1684. [DOI] [PubMed] [Google Scholar]
- 124. Akman I. Mothers’ postpartum psychological adjustment and infant colic. Arch Dis Child 2006; 91(5): 417–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Wright CM, Parkinson KN, Drewett RF. The influence of maternal socioeconomic and emotional factors on infant weight gain and weight faltering (failure to thrive): data from a prospective birth cohort. Arch Dis Child 2006; 91(4): 312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Tomlinson M, Cooper PJ, Stein A, et al. Post-partum depression and infant growth in a South African peri-urban settlement. Child Care Health Dev 2006; 32(1): 81–86. [DOI] [PubMed] [Google Scholar]
- 127. Tomlinson M, Cooper P, Murray L. The mother-infant relationship and infant attachment in a south African peri-urban settlement. Child Dev 2005; 76(5): 1044–1054. [DOI] [PubMed] [Google Scholar]
- 128. Minkovitz CS, Strobino D, Scharfstein D, et al. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics 2005; 115(2): 306–314. [DOI] [PubMed] [Google Scholar]
- 129. Friedman DD. 4-month infant vocal quality in mother-infant face-to-face interaction: 6-week maternal postpartum depressive symptomatology and infant gender. PhD Thesis, New York University, New York, 2005. [Google Scholar]
- 130. Zajicek-Farber ML. Postnatal depression and infant health practices among high-risk women. J Child Fam Stud 2008; 18(2): 236–245. [Google Scholar]
- 131. Kalita KN. Developmental profile of infants born to mothers with postpartum depression and anxiety: a comparative study. J Indian Assoc Child Adolesc Ment Health 2009; 6(1): 3–12. [Google Scholar]
- 132. Zajicek-Farber ML. The contributions of parenting and postnatal depression on emergent language of children in low-income families. J Child Fam Stud 2009; 19(3): 257–269. [Google Scholar]
- 133. Conroy S, Pariante CM, Marks MN, et al. Maternal psychopathology and infant development at 18 months: the impact of maternal personality disorder and depression. J Am Acad Child Adolesc Psychiatry 2012; 51(1): 51–61. [DOI] [PubMed] [Google Scholar]
- 134. Evans J, Melotti R, Heron J, et al. The timing of maternal depressive symptoms and child cognitive development: a longitudinal study. J Child Psychol Psychiatry 2012; 53(6): 632–640. [DOI] [PubMed] [Google Scholar]
- 135. Guo N, Bindt C, TeBonle M, et al. Association of antepartum and postpartum depression in Ghanaian and Ivorian women with febrile illness in their offspring: a prospective birth cohort study. Am J Epidemiol 2013; 178(9): 1394–1402. [DOI] [PubMed] [Google Scholar]
- 136. Weobong B, tenAsbroek AH, Soremekun S, et al. Association between probable postnatal depression and increased infant mortality and morbidity: findings from the DON population-based cohort study in rural Ghana. BMJ Open 2015; 5(8): e006509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. McLearn KT, Minkovitz CS, Strobino DM, et al. Maternal depressive symptoms at 2 to 4 months post partum and early parenting practices. Arch Pediatr Adolesc Med 2006; 160(3): 279–284. [DOI] [PubMed] [Google Scholar]
- 138. Okronipa HET, Marquis GS, Lartey A, et al. Postnatal depression symptoms are associated with increased diarrhea among infants of HIV-positive Ghanaian mothers. AIDS Behav 2012; 16(8): 2216–2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Kaplan PS, Danko CM, Everhart KD, et al. Maternal depression and expressive communication in one-year-old infants. Infant Behav Dev 2014; 37(3): 398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Bakare MO, Okoye JO, Obindo JT. Introducing depression and developmental screenings into the national programme on immunization (NPI) in southeast Nigeria: an experimental cross-sectional assessment. Gen Hosp Psychiatry 2016; 36(1): 105–112. [DOI] [PubMed] [Google Scholar]
- 141. Chen H-H, Hwang F-M, Wang K-L, et al. A structural model of the influence of immigrant mothers’ depressive symptoms and home environment on their children’s early developmental outcomes in Taiwan. Res Nurs Health 2013; 36(6): 603–611. [DOI] [PubMed] [Google Scholar]
- 142. Ndokera R, MacArthur C. The relationship between maternal depression and adverse infant health outcomes in Zambia: a cross-sectional feasibility study. Child Care Health Dev 2011; 37(1): 74–81. [DOI] [PubMed] [Google Scholar]
- 143. Hartley C, Pretorius K, Mohamed A, et al. Maternal postpartum depression and infant social withdrawal among human immunodeficiency virus (HIV) positive mother-infant dyads. Psychol Health Med 2010; 15(3): 278–287. [DOI] [PubMed] [Google Scholar]
- 144. Choi H, Yamashita T, Wada Y, et al. Factors associated with postpartum depression and abusive behavior in mothers with infants. Psychiatry Clin Neurosci 2010; 64(2): 120–127. [DOI] [PubMed] [Google Scholar]
- 145. Hibino Y, Takaki J, Kambayashi Y, et al. Relationship between the Noto-Peninsula earthquake and maternal postnatal depression and child-rearing. Environ Health Prev Med 2009; 14(5): 255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Bank AM, Barr R, Calvert SL, et al. Maternal depression and family media use: a questionnaire and diary analysis. J Child Fam Stud 2012; 21(2): 208–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Kaplan PS, Danko CM, Cejka AM, et al. Maternal depression and the learning-promoting effects of infant-directed speech: roles of maternal sensitivity, depression diagnosis, and speech acoustic cues. Infant Behav Dev 2015; 41: 52–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Rodrigues M, Patel V, Jaswal S, et al. Listening to mothers: qualitative studies on motherhood and depression from Goa, India. Social Sci Med 2003; 57(10): 1797–1806. [DOI] [PubMed] [Google Scholar]
- 149. Klaus M, Kennell J, Ballard R. Parent-infant bonding, 1982, https://sjwd4iadz01.storage.googleapis.com/MDgwMTYyNjg1NA==01.pdf
- 150. Kennell JH, Klaus MH. Bonding: recent observations that alter perinatal care. Pediatr Rev 1998; 19(1): 4–12. [PubMed] [Google Scholar]
- 151. Kinsey CB, Baptiste-Roberts K, Zhu J, et al. Birth-related, psychosocial, and emotional correlates of positive maternal-infant bonding in a cohort of first-time mothers. Midwifery 2014; 30(5): e188–e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EDDS). J Reprod Infant Psychol 1990; 8(2): 99–107. [Google Scholar]
- 153. Ji S, Long Q, Newport DJ, et al. Validity of Depression Rating Scales during pregnancy and the postpartum period: impact of trimester and parity. J Psychiatr Res 2011; 45(2): 213–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Matthey S, Henshaw C, Elliott S, et al. Variability in use of cut—off scores and formats on the Edinburgh Postnatal Depression Scale—implications for clinical and research practice. Arch Womens Ment Health 2006; 9(6): 309–315. [DOI] [PubMed] [Google Scholar]
- 155. Negron R, Martin A, Almog M, et al. Social support during the postpartum period: mothers’ views on needs, expectations, and mobilization of support. Matern Child Health J 2013; 17(4): 616–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Cheng C-Y, Pickler RH. Effects of stress and social support on postpartum health of Chinese mothers in the United States. Res Nurs Health 2009; 32(6): 582–591. [DOI] [PubMed] [Google Scholar]
- 157. Zheng X, Morrell J, Watts K. A quantitative longitudinal study to explore factors which influence maternal self-efficacy among Chinese primiparous women during the initial postpartum period. Midwifery 2017; 59: 39–46. [DOI] [PubMed] [Google Scholar]
- 158. Razurel C. Comment l’éducation dispensée par les professionnels peut-elle influencer le sentiment de compétence parentale chez les mères primipares? Rouen: Université de Rouen, 2010. [Google Scholar]
- 159. Williams TM, Joy LA, Travis L, et al. Transition to motherhood: a longitudinal study. Infant Ment Health J 1987; 8(3): 251–265. [Google Scholar]
- 160. Forster DA, McLachlan HL, Rayner J, et al. The early postnatal period: exploring women’s views, expectations and experiences of care using focus groups in Victoria, Australia. BMC Pregnancy Childbirth 2008; 8: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Soet JE, Brack GA, Di Iorio C. Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth 2003; 30(1): 36–46. [DOI] [PubMed] [Google Scholar]
- 162. Slomian J, Emonts P, Vigneron L, et al. Identifying maternal needs following childbirth: a qualitative study among mothers, fathers and professionals. BMC Pregnancy Childbirth 2017; 17(1): 213–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Stainton C, Murphy B, Higgins PG, et al. The needs of postbirth parents: an international, multisite study. J Perinat Educ 1999; 8: 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: the perinatal maternal health promotion model. J Midwifery Womens Health 2013; 58(6): 613–621. [DOI] [PubMed] [Google Scholar]
- 165. Forster DA, McLachlan HL, Davey M-A, et al. Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BMC Pregnancy Childbirth 2016; 16: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Rayner J-A, McLachlan HL, Peters L, et al. Care providers’ views and experiences of postnatal care in private hospitals in Victoria, Australia. Midwifery 2013; 29(6): 622–627. [DOI] [PubMed] [Google Scholar]
- 167. Brown SJ, Davey M-A, Bruinsma FJ. Women’s views and experiences of postnatal hospital care in the Victorian Survey of Recent Mothers 2000. Midwifery 2005; 21(2): 109–126. [DOI] [PubMed] [Google Scholar]
- 168. Jenkins MG, Ford JB, Todd AL, et al. Women’s views about maternity care: how do women conceptualise the process of continuity. Midwifery 2015; 31(1): 25–30. [DOI] [PubMed] [Google Scholar]
- 169. Emmanuel E, Creedy D, Fraser J. What mothers want: a postnatal survey. Aust J Midwifery 2001; 14(4): 16–20. [DOI] [PubMed] [Google Scholar]
- 170. Carolan M. Health literacy and the information needs and dilemmas of first-time mothers over 35 years. J Clin Nurs 2007; 16(6): 1162–1172. [DOI] [PubMed] [Google Scholar]
- 171. Malata A, Chirwa E. Childbirth information needs for first time Malawian mothers who attended antenatal clinics. Malawi Med J 2011; 23(2): 43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Sword W, Watt S. Learning needs of postpartum women: does socioeconomic status matter. Birth 2005; 32(2): 86–92. [DOI] [PubMed] [Google Scholar]
- 173. Deave T, Johnson D, Ingram J. Transition to parenthood: the needs of parents in pregnancy and early parenthood. BMC Pregnancy Childbirth 2008; 8: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Javadifar N, Majlesi F, Nikbakht A, et al. Journey to motherhood in the first year after child birth. J Family Reprod Health 2016; 10(3): 146–153. [PMC free article] [PubMed] [Google Scholar]
- 175. Nystrom K, Ohrling K. Parenthood experiences during the child’s first year: literature review. J Adv Nurs 2004; 46(3): 319–330. [DOI] [PubMed] [Google Scholar]
- 176. Nicolson P. Loss, happiness and postpartum depression: the ultimate paradox. Can Psychol 1999; 40(2): 162–178. [Google Scholar]
- 177. McKellar LV, Pincombe JI, Henderson AM. Insights from Australian parents into educational experiences in the early postnatal period. Midwifery 2006; 22(4): 356–364. [DOI] [PubMed] [Google Scholar]
- 178. Hildingsson IM. New parents’ experiences of postnatal care in Sweden. Women Birth 2007; 20(3): 105–113. [DOI] [PubMed] [Google Scholar]
- 179. Fishbein EG, Burggraf E. Early postpartum discharge: how are mothers managing. J Obstet Gynecol Neonatal Nurs 1998; 27(2): 142–148. [DOI] [PubMed] [Google Scholar]
- 180. Fowles ER, Cheng H-R, Mills S. Postpartum health promotion interventions: a systematic review. Nurs Res 2012; 61(4): 269–282. [DOI] [PubMed] [Google Scholar]
- 181. Cheng C-Y, Fowles ER, Walker LO. Continuing education module: postpartum maternal health care in the United States: a critical review. J Perinat Educ 2006; 15(3): 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Nelson AM. Transition to motherhood. JOGNN 2003; 32(4): 465–477. [DOI] [PubMed] [Google Scholar]
- 183. Benahmed N, Devos C, San Miguel L, et al. KCE Reports 232B: caring for mothers and newborns after uncomplicated delivery: towards integrated postnatal care, 2014, https://www.kindengezin.be/img/KCE-report-232-postpartumcare.pdf
- 184. Nilsson I, Danbjørg DB, Aagaard H, et al. Parental experiences of early postnatal discharge: a meta-synthesis. Midwifery 2015; 31(10): 926–934. [DOI] [PubMed] [Google Scholar]