Abstract
Healthcare delivery has been dramatically changing in recent times with advances in technology. One area of expansion has been the use of telemedicine due to progression in communication technologies. Telemedicine offers the opportunity to overcome barriers of access, improve patient satisfaction, improve healthcare outcomes and streamline communication between patients and providers. The primary modalities of telemedicine can be grouped into categories of ‘remote monitoring,’ ‘store and forward’ and ‘interactive telemedicine.’ These modalities of telemedicine have been practiced and explored within the scope of hepatology such as in liver transplantation, hepatocellular carcinoma and management of chronic hepatitis C (CHC). There are numerous telemedicine‐based CHC management studies and programs that have developed in New Mexico, the Department of Veterans Affairs, as well as globally in Australia and Canada. In Northern California, the University of New Mexico telemedicine‐based model of ‘ECHO’ has been extended to develop community‐based champions to screen‐link‐treat CHC patients with the goal to eliminate hepatitis C. Despite the advantages to telemedicine, there are still many barriers to seamless integration due to reimbursement and up‐front cost. Nevertheless, it remains an essential part in providing world‐class care to liver patients across geographic and economic barriers.
Abbreviations
- CHC
chronic hepatitis C
- DAA
direct‐acting antiviral
- ECHO
Extension for Community Healthcare Outcomes
- HCV
hepatitis C virus
- PCP
primary care physician
- SVR
sustained virologic response
- UC
University of California
- VA
Veterans Affairs
In the world of smartphones, applications, social media, and electronic health record portals, delivery and communication in health care have drastically changed. Telemedicine is a rapidly expanding area of health care delivery. The term itself denotes “healing at a distance” and was coined in the 1970s. According to the World Health Organization, telemedicine needs to have four elements: provide clinical support, overcome geographic barriers to connect individuals that are not in the same physical location, involve various communication technologies, and improve health outcome.1 The greatest driving force for the advancement of telemedicine has been the rapid advancement and availability of mobile communication technologies along with expansion of wireless broadband technology. Telemedicine deviates from the traditional patient–physician office visit. Importantly, it can overcome barriers to access as many patients are unable to travel to see a specialist or provider due to distance, financial reasons, or simply inconvenience. With specialized care typically limited to larger urban areas, there is a significant need for advancements of telemedicine to connect patients in remote or rural areas with health care providers in urban areas. Ultimately, if telemedicine can enhance patient access to providers and/or provide improved continuity of care, there is an opportunity to improve health care outcomes. In this article, we delve into how telemedicine can impact hepatology practice and help in the understanding of challenges and future directions.
A Primer of Telemedicine Terminology
Telemedicine and telehealth are used interchangeably. The primary modalities of telehealth or telemedicine can be grouped into three categories: “remote monitoring,” “store and forward,” and “interactive telemedicine” (Fig. 1). These different modalities contribute to improving patient health in different but overlapping ways.
Figure 1.
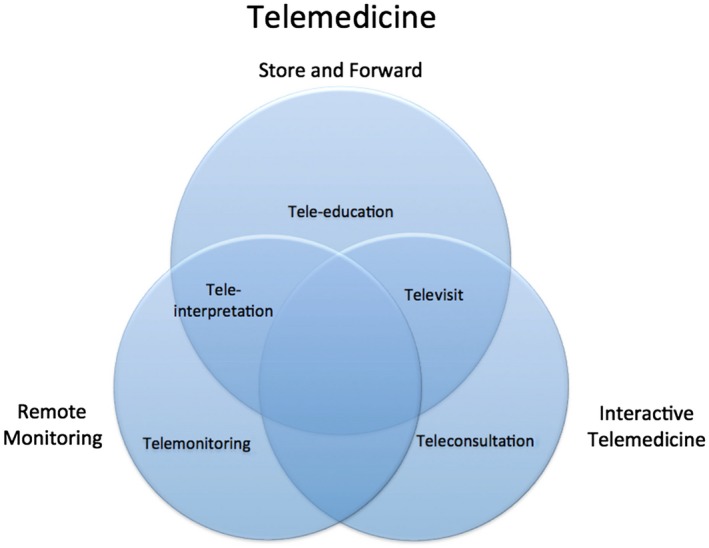
Different modalities of telemedicine.
Remote Monitoring
Telemonitoring generally refers to tracking various patient parameters, usually through mobile devices or reporting by telephone. An example is home monitoring of daily weights, blood pressure, and pulse in patients with congestive heart failure; the data are then transmitted to a monitoring database. Tele‐interpretation often uses asynchronous telemedicine that requires remote monitoring and interpretation of medical data by distant medical professionals; this is commonly used in radiology or pathology and can be seen in practice with interpretation of electrocardiograms by remote cardiologists.
Interactive Telemedicine
Interactive telemedicine is synchronous real‐time patient management. It includes teleconsultation in collaboration with specialists who are available at tertiary centers but unable to be physically present at community and rural hospitals. Commonly, community hospitals have access to pulmonary critical care doctors at a tertiary care center through teleconsultation; these doctors can guide on‐site hospitalists in critical care medical decisions. Televisits are conventional patient–provider office visits that use video and audio conferencing due to distance; televisits are a form of interactive telemedicine or store and forward. With advents in digital diagnostic tools, such as digital stethoscopes and otoscopes, televisits can be as comprehensive as an in‐person clinic visit.
Store and Forward
Store and forward is also known as asynchronous telemedicine and refers to storing a patient's information, which is then later analyzed by a medical professional. This contrasts with real‐time communication seen in interactive telemedicine where a clinician interacts with a patient in real time by video and audio conferencing. Tele‐education generally uses the concept of store and forward and has been practiced for many years through online teaching didactics and interactive videos for patients as well as providers.
Telemedicine and Hepatitis C
Early management of chronic hepatitis C (CHC) was challenging and generally restricted to academic medical centers or specialty care. The advent of telemedicine and innovative methodology from New Mexico helped transform the treatment of CHC. The telemedicine‐based CHC management studies and programs are summarized in Table 1. One of the most well‐known studies in hepatology is the Extension for Community Healthcare Outcomes (ECHO) project created at the University of New Mexico Health Sciences Center to delivery CHC treatment in rural and underserved populations in New Mexico.2 In this single‐site, prospective, cohort study, primary care physicians/providers (PCPs) undertook weekly videoconferences with specialists as well as short didactic sessions along with discussions of patient treatment plans. The study comprised 407 subjects in the ECHO study arm that received CHC interferon treatment administered by PCPs and 146 controlled subjects that received the same CHC treatment at the University of New Mexico hepatitis C virus (HCV) clinic. Results showed that sustained virologic responses (SVRs) or viral eradication were similar in the ECHO study arm (58.2%) and controlled arm (57.5%; no significant difference). Over the years, ECHO has transformed many practices for CHC treatment nationally and internationally and has also percolated through multiple different specialties.
Table 1.
Summary of Various Telemedicine‐Based CHC Programs
| Article | Type of TM Subjects | Number of Subjects | Study Design | SVR | Treatment Type | Country |
|---|---|---|---|---|---|---|
| Arora et al.2 | Rural | TM n = 261 | Prospective cohort study | TM 58% | Interferon and ribavirin | USA |
| Clinic n = 146 | Clinic 58% | |||||
| Nazareth et al.11 | Rural | TM n = 50 | Prospective cohort study | TM 71% | Interferon and ribavirin | Australia |
| Clinic n = 559 | Clinic 59% | |||||
| Rossaro et al.12 | Rural | TM n = 40 | Retrospective cohort study | TM 55% | Interferon and ribavirin | USA |
| Clinic n = 40 | Clinic 43% | |||||
| Beste et al.3 | Rural veterans | TM n = 6,431 | Prospective cohort study | TM 58% | Interferon +/– ribavirin, DAA | USA |
| Clinic n = 32,322 | Clinic 54% | |||||
| Cooper et al.4 | Rural | TM n = 157 | Retrospective cohort study | TM 95% | DAA | Canada |
| Clinic n = 1,130 | Clinic 95% | |||||
| Sterling et al.13 | Incarcerated | TM n = 84 | Prospective cohort study | TM 95% | DAA | USA |
| Clinic n = 240 | Clinic 94% | |||||
| Talal et al.14 | OST | TM n = 62 | Prospective cohort study | TM 93% | DAA | USA |
| Papaluca et al.15 | Incarcerated | TM n = 313 | Prospective cohort study | TM 96% | DAA | Australia |
Abbreviations: OST, opioid substitution therapy; TM, telemedicine.
The Department of Veterans Affairs (VA) adopted a similar model for treatment of CHC called the VA Extension for Community Health Outcomes (VA‐ECHO) to reach the rural VA patient population. VA‐ECHO was implemented in 152 PCP sites nationwide. PCPs received videoconferencing with specialists every 1‐2 weeks with collaborative discussions of patient treatment plans. In the study, 4,173 subjects were exposed to VA‐ECHO and 32,322 subjects were unexposed. Subjects were treated with direct antiviral drugs for treatment of CHC with no difference in rate of SVR in the two populations. However, the study noted that the rate of PCP‐initiated antiviral treatment was much higher in subjects exposed to VA‐ECHO compared to patients who were unexposed (21.4% versus 2.5%, respectively). This study suggests that further implementation of VA‐ECHO will improve rates of initiation of CHC treatment in the VA population.3 Similarly, comparison of telehealth‐based care of the rural patient population versus the urban population having access to direct clinical care had similar rates of SVR (94.7% versus 94.8%, respectively) when using new‐generation antivirals for CHC (direct‐acting antivirals [DAAs]).4
The University of California (UC) San Francisco uses the ECHO model to expand CHC treatment capacity in northern California. More than 50 providers in over 20 counties are actively engaged in HCV management. Although this made significant roadway into the management of hepatitis C, an expanded version of ECHO was launched in 2018, called ECHO‐plus, in collaboration with UC Davis and their telemedicine program. While ECHO takes a one‐to‐many (specialist hub with PCP spokes) approach, UC Davis telemedicine is one‐to‐one telementoring with the HCV specialist–provider–patient. A unique aspect of the program is the ability to tailor the training based on the provider or practice needs. To further provide a comprehensive service to the providers, ECHO‐plus includes pharmacist‐driven training of the DAAs and their approval, a clinical management support tool, and access to a “warm line” (Fig. 2). The joint program has already enrolled PCPs from 30 centers across rural northern California in the past year.5 Telemedicine is a vital tool for the goal of elimination of hepatitis C. Continual efforts in innovations of telemedicine to cater to the local needs will be essential for the treatment of hepatitis C.
Figure 2.
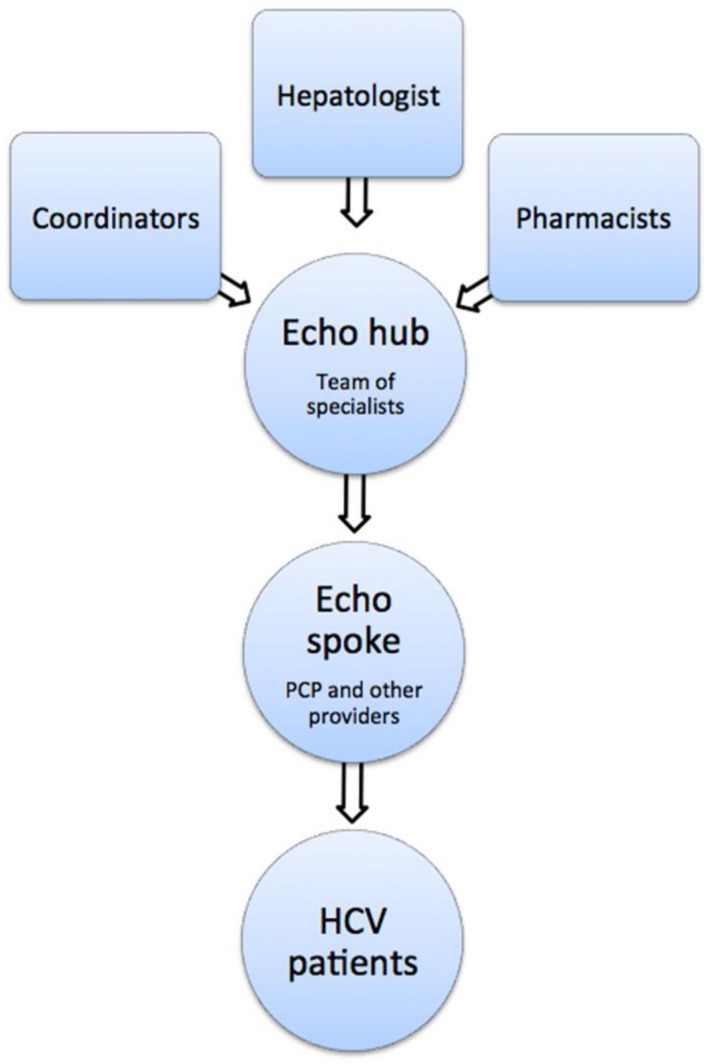
Model of ECHO‐plus at UC San Francisco and UC Davis.
Telemedicine for Hepatocellular Carcinoma
In patients with hepatocellular carcinoma who are cared for at institutions without tumor board forums, virtual tumor boards can expedite the process of multidisciplinary evaluation. At the VA, patients enrolled in virtual tumor boards received high rates of comprehensive multidisciplinary evaluation within a shorter amount of time.6
Telemedicine Expanding Into Other Areas of Hepatology
Telemedicine has also gained traction in other areas of hepatology (Table 2). In populations before and after liver transplant, telehealth‐based approaches have been shown to improve patient satisfaction.7 The innovative telemedicine‐based approach also streamlined communication between transplant surgeons for allocation of grafts in split liver transplantation.8 In patients with alcoholic cirrhosis, frequent teleconsultations appeared to prevent relapse, reduce hospitalization, and increase quality of life. A recent pilot study showed an automated telephone monitoring system could be used to predict future hospitalizations in patients with decompensated cirrhosis.9
Table 2.
Use of Telemedicine in Different Areas of Hepatology
| Condition | Articles | Conclusion |
|---|---|---|
| HCV |
|
|
| Hepatocellular carcinoma |
|
|
| Cirrhosis |
|
|
| Liver transplantation |
|
Challenges With Telemedicine Implementation
Numerous challenges remain in the integration of telemedicine into clinical practice. One of the significant barriers is restriction on reimbursements. At this time, there are stringent rules to be eligible for Medicare reimbursement for telemedicine services.10 Patients must be located outside a metropolitan statistical area. Patients also need to be located within approved “originating sites,” such as office, clinic, or nursing home, with interactive audio and video telecommunication systems for real‐time communication in order to quality for reimbursements. Clinicians often need to be licensed with malpractice insurance at the originating sites to receive reimbursement.10 Reimbursement process and rates have also been confusing across insurers. Private payer reimbursements for telemedicine services are variable. Currently, there are different state policies regarding reimbursement for telehealth services. The lack of guidelines and uniformity of reimbursement create varying degrees of incentive to invest in telemedicine.
Although telemedicine holds significant potential, telemedicine is not ubiquitous. It requires large upfront costs to the institution to implement, along with additional support for legal liabilities, security of data, and training. Thus, it will require significant cultural change, including modifications to teaching and management techniques. Telemedicine has been studied in many specialties and clinical settings; yet, few studies have analyzed its cost effectiveness.
Concluding Remarks
Telehealth offers unique opportunities to patients and providers. As the field of medicine progresses, disparities in health care and access remain through all specialties. Evolving technological advances can help address some of these challenges by integrating care and increasing access while maintaining or reducing costs. Telemedicine is certainly reaching prime time, thus providing world‐class care to all our liver patients across geographic and economic barriers. Telehealth should be the logical extension of clinical care for all academic and tertiary medical centers.
Supported by Gilead Sciences through ECHO‐plus (grant no. IN‐US‐342‐4311 to N.T.)
Potential conflict of interest: Dr. Sarkar received grants from Gilead. Dr. Terrault received grants from Gilead, Bristol Myers Squibb, AbbVie, Merck, and Allergan; she consults for Dova. Dr. Piao has nothing to report.
References
- 1. World Health Organization . Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. https://www.who.int/goe/publications/goe_telemedicine_2010.pdf. Published 2009. Accessed January 2019.
- 2. Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med 2011;364:2199‐2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beste LA, Glorioso TJ, Ho PM, Au DH, Kirsh SR, Todd‐Stenberg J, et al. Telemedicine specialty support promotes hepatitis C treatment by primary care providers in the Department of Veterans Affairs. Am J Med 2017;130:432‐438.e3. [DOI] [PubMed] [Google Scholar]
- 4. Cooper CL, Hatashita H, Corsi DJ, Parmar P, Corrin R, Garber G. Direct‐acting antiviral therapy outcomes in Canadian chronic hepatitis C telemedicine patients. Ann Hepatol 2017;16:874‐880. [DOI] [PubMed] [Google Scholar]
- 5. Terrault N, Kanner R, Gailloux K, Slepin J, Catalli L, McKinney J, et al. Elimination of Hepatitis C in California: The Year‐One ECHO‐PLUS Report Card. MetaECHO 2019. URL: https://www.cvent.com/events/metaecho-2019-conference/agenda-2e603b603a8b4422906c13682e59feb9.aspx.
- 6. Salami AC, Barden GM, Castillo DL, Hanna M, Petersen NJ, Davila JA, et al. Establishment of a regional virtual tumor board program to improve the process of care for patients with hepatocellular carcinoma. J Oncol Pract 2015;11:e66‐e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ertel AE, Kaiser T, Shah SA. Using telehealth to enable patient‐centered care for liver transplantation. JAMA Surg 2015;150:674‐675. [DOI] [PubMed] [Google Scholar]
- 8. Reddy MS, Bhati C, Neil D, Mirza DF, Manas DM. National Organ Retrieval Imaging System: results of the pilot study. Transpl Int 2008;21:1036‐1044. [DOI] [PubMed] [Google Scholar]
- 9. Thomson M, Volk M, Kim HM, Piette JD. An automated telephone monitoring system to identify patients with cirrhosis at risk of re‐hospitalization. Dig Dis Sci 2015;60:3563–3569. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Medicare & Medicaid Services . Telehealth. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/index.html. Published January 3, 2014. Accessed January 31, 2019.
- 11. Nazareth S, Kontorinis N, Muwanwella N, Hamilton A, Leembruggen N, Cheng WS. Successful treatment of patients with hepatitis C in rural and remote Western Australia via telehealth. J Telemed Telecare 2013;19:101‐106. [DOI] [PubMed] [Google Scholar]
- 12. Rossaro L, Torruellas C, Dhaliwal S, Botros J, Clark G, Li CS, et al. Clinical outcomes of hepatitis C treated with pegylated interferon and ribavirin via telemedicine consultation in Northern California. Dig Dis Sci 2013;58:3620‐3625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sterling RK, Cherian R, Lewis S, Genther K, Driscoll C, Martin K, et al. Treatment of HCV in the Department of Corrections in the era of oral medications. J Correct Health Care 2018;24:127‐136. [DOI] [PubMed] [Google Scholar]
- 14. Talal AH, Andrews P, Mcleod A, Chen Y, Sylvester C, Markatou M, et al. Integrated, co‐located, telemedicine‐based treatment approaches for hepatitis C virus (HCV) management in opioid use disorder patients on methadone. Clin Infect Dis 2018; 10.1093/cid/ciy899. [DOI] [PubMed] [Google Scholar]
- 15. Papaluca T, McDonald L, Craigie A, Gibson A, Desmond P, Wong D, et al. Outcomes of treatment for hepatitis C in prisoners using a nurse‐led, state‐wide model of care. J Hepatol 2019; 10.1016/j.jhep.2019.01.012. [DOI] [PubMed] [Google Scholar]


