Retinal “macrocysts” have been reported in association with chronic retinal detachments,1,2 but their pathologic characteristics remain poorly understood. We report a case of chronic retinal detachment with large macular and peripheral retinal pseudocysts and discuss the histologic features of such retinal macro-pseudocysts and their implications.
Report of a Case
A man in his mid-20s with a remote history of blunt injury to his left eye presented with a 10-year history of chronic blurred vision in the left eye. Results of an examination of the left eye showed visual acuity of counting fingers, a normal anterior segment, and an inferior retinal detachment involving the macula (Figure 1A). A retinal tear 2 clock-hours in size was noted in the inferotemporal quadrant near the ora serrata. Two large retinal macro-pseudocysts, posterior to the retinal break, were confirmed by ultrasonography to be contiguous with the detached retina (Figure 1B). Optical coherence tomography through a separate foveal retinal macro-pseudocyst revealed a schisis-like cavity (Figure 1C). The patient underwent surgical repair with 23-gauge pars plana vitrectomy, scleral buckle placement, inferior retinectomy, endolaser, and injection of per-fluoropropane. Intraoperatively, the peripheral retinal macro-pseudocysts (Figure 1D) and a small area of the adjacent detached retina were aspirated, then resected en bloc and sent for pathologic examination. At the patient’s 6-month postoperative visit, the retina remained attached, and his visual acuity showed a slight improvement at Snellen 20/400 OS.
Figure 1. Multimodal Imaging.
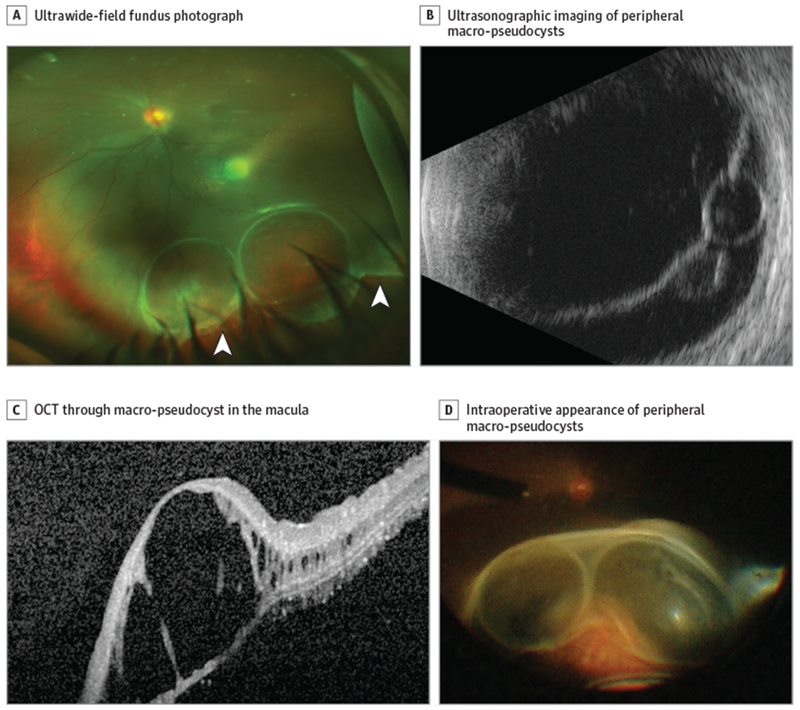
A, Ultrawide-field fundus photograph showing a retinal tear (arrowheads), peripheral retinal macropseudocysts, and an inferior retinal detachment involving the macula. B, Ultrasonographic imaging of the peripheral retinal macro-pseudocysts within the detached retina. C, Optical coherence tomography (OCT) through the macular macro-pseudocyst showing splitting of the retinal layers. D, Intraoperative appearance ofthe peripheral retinal macro-pseudocysts on scleral depression.
Discussion
To our knowledge, this is the first reported case with multimodal imaging of concurrent macular and peripheral retinal macro-pseudocysts associated with chronic retinal detachment. By comparing the peripheral retinal macropseudocyst with the adjacent detached retina, we conclude that the peripheral retinal macro-pseudocyst is a localized splitting of the detached retina, with an anterior portion consisting of atrophied inner retinal layers (Figure 2A and B) and a posterior portion consisting of disorganized outer retinal layers (Figure 2C and D). The anterior portion of the pseudocyst contained blood vessels that stained positive with CD34 antibody and periodic acid-Schiff, and ganglion cells and cells of the inner nuclear layer that stained positive with NeuN, a neuronal nuclear antigen (Figure 2B). The posterior portion of the pseudocyst stained negative for the CD34 antigen and NeuN (Figure 2D). In addition, immunohistochemical staining for keratin was negative in our specimen, indicating the absence of epithelial cells. Few pathologic reports of retinal macro-pseudocysts exist, and our observation is consistent with pathologic specimens obtained by Zimmerman and Spencer3 and Marcus and Aaberg,4 who indicated that these pseudocysts were located in the outer plexiform layer, although their reports lacked immunohistochemical confirmation. In addition, optical coherence tomography through the macular macro-pseudocyst also revealed splitting of the retina in the patient, similar to that reported by Tripathy et al.5 Our histologic findings, together with ultrasonographic and optical coherence tomographic findings, suggest that what is commonly referred to as a macrocyst in this clinical context is a misnomer.
Figure 2. Histologic and Immunohistochemistry Findings.
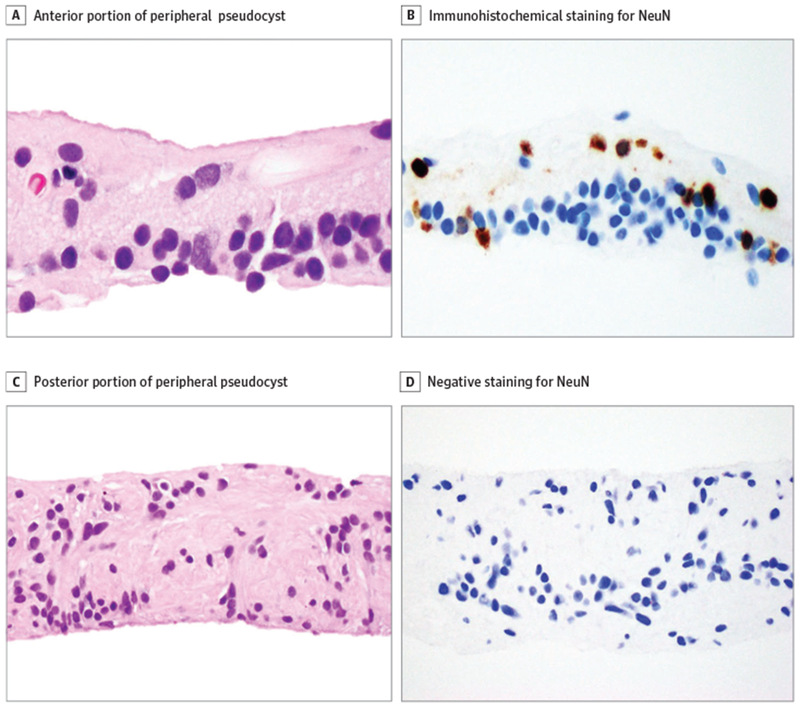
A, Anterior portion of the peripheral pseudocyst. B, Immunohistochemical staining for NeuN was positive, highlighting ganglion cells and scattered cells of the inner nuclear layer. C, Posterior portion of the peripheral pseudocyst, showing disorganized glioneuronal tissue. D, Posterior portion of the peripheral pseudocyst, showing negative staining for NeuN. All parts, immunohistochemical stain, original magnification x400.
The inner wall of a cyst, by definition, is lined by epithelium. Classic teaching dictates that drainage of a cyst without removal of the cyst wall en bloc will lead to the reaccumulation of fluid. In the clinical context of retinal macro-pseudocysts associated with chronic retinal detachment, it is important to understand the pathogenesis of these pseudocysts, which has surgical implications. Specifically, because these macro-pseudocysts are not real cysts, they need not be resected en bloc during surgical retinal reattachment, thus allowing for the preservation of wide areas of the retina.
Conclusions
Retinal macro-pseudocysts canbe seen in the setting of chronic retinal detachments. Our histologic, optical coherence tomographic, and ultrasonographic findings suggest that these macro-pseudocysts are not real cysts but are formed by the splitting of the retinal layers instead. This observation is important for choosing the optimal surgical approach in this clinical setting.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
References
- 1.Kumar V,Vivek K, Chandra P, Kumar A. Ultrawidefield imaging of multiple intraretinal cysts in old rhegmatogenous retinal detachment. Oman J Ophthalmol. 2016;9(3):191–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verdaguer P, Nadal J. Intraretinal cyst secondary to longstanding retinal detachment. Eur J Ophthalmol. 2012;22(3):506–508. [DOI] [PubMed] [Google Scholar]
- 3.Zimmerman LE, Spencer WH. The pathologic anatomy of retinoschisis with a report of two cases diagnosed clinically as malignant melanoma. Arch Ophthalmol. 1960;63:10–19. [DOI] [PubMed] [Google Scholar]
- 4.Marcus DF, Aaberg TM. Intraretinal macrocysts in retinal detachment. Arch Ophthalmol. 1979;97(7):1273–1275. [DOI] [PubMed] [Google Scholar]
- 5.Tripathy K, Bypareddy R, Chawla R, Kumawat B. Optical coherence tomography follow-up of an unusual case of old rhegmatogenous retinal detachment with a hemorrhagic macrocyst atthe macula. Ophthalmic Surg Lasers Imaging Retina. 2015;46(10):1058–1060. [DOI] [PubMed] [Google Scholar]


