Abstract
BACKGROUND AND OBJECTIVE:
Establish the surgical procedure for subretinal implantation of multiple photovoltaic arrays for the restoration of sight.
MATERIALS AND METHODS:
Multiple silicon photo-voltaic arrays of 1 mm in diameter and 30 μm in thickness were implanted subretinally via single retinotomy in rabbits. Ophthalmoscopic imaging and optical coherence tomography (OCT) were used to validate the implants’ placement.
RESULTS:
Vitrectomy, followed by subretinal fluid injection for retinal detachment and retinotomy, allowed accurate placement of seven modules in the bleb, covering approximately a 3.5-mm diameter area on the retina via a single 1.5-mm retinotomy. OCT confirmed complete reattachment of the retina over the implants.
CONCLUSION:
Subretinal implantation of multiple photovoltaic arrays via a single retinotomy, followed by their tiling, minimizes the scleral and retinal incisions and provides better fit to the spherical shape of the eye ball, compared to a single, larger module. Such minimally traumatic procedure can be performed with 20-gauge intraocular instruments.
INTRODUCTION
Patterned electrical stimulation of the retina with epiretinal or subretinal prostheses allows patients blinded by retinitis pigmentosa (RP) to regain light sensitivity and some visual shape recognition, primarily improving orientation and ambulation.1–3 Current retinal implants include transscleral cables connecting them to an extraocular power supply, which requires very difficult surgery and often leads to complications.1,4 We developed a completely wireless photovoltaic implant in which pixels directly convert pulsed near-infrared light projected from video goggles into electric current5 (Figure 1). The wireless nature of such an approach allows minimally traumatic implantation of multiple independent modules via small retinotomy and sclerotomy to cover a large visual field. In the past, we successfully implanted single modules to assess the characteristics of prosthetic vision in rats.6–8 However, implantation of multiple modules in a larger animal was never attempted. Here we describe the procedure for implantation of up to seven modules in the rabbit eye, which is very similar to the procedure expected in human patients.
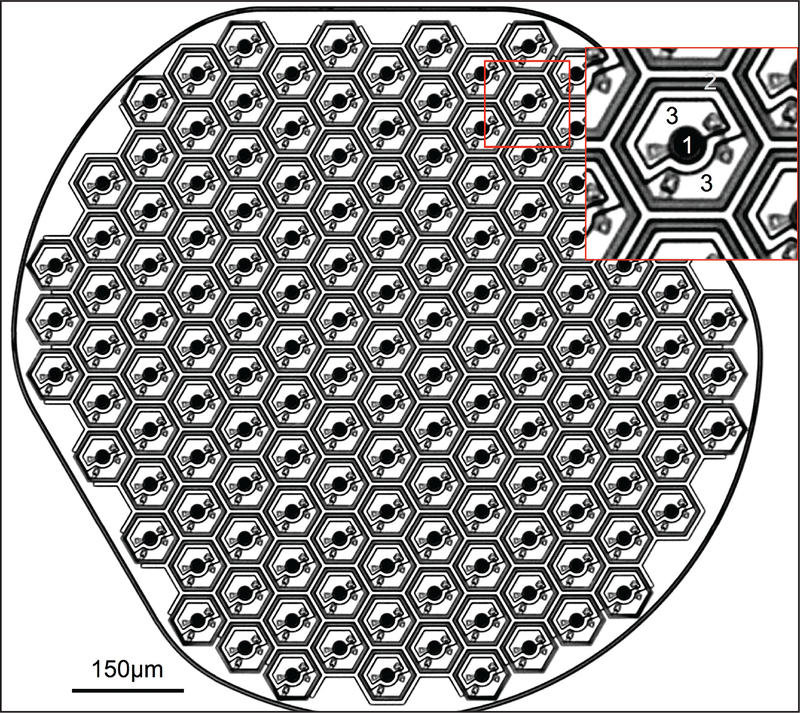
Figure 1.
The photovoltaic array of 1 mm in diameter and 30 μm in thickness. Each module is composed of 70-μm pixels, having a stimulating electrode (1) and a return electrode (2) connected to two photodiodes (3).
TECHNIQUE
All experiments were carried out in accordance with the ARVO guidelines for the Use of Animals in Ophthalmic and Vision Research and approved by the Stanford Administrative Panel on Laboratory Animal Care. Dutch belted rabbits (weight range: 2 kg to 2.5 kg) were anesthetized with intramuscular injection of ketamine (35 mg/kg) and xylazine (5 mg/kg). Pupillary dilation was achieved by one drop each of 1% tropicamide and 2.5% phenylephrine hydrochloride. Topical tetracaine 0.5% was instilled in the eye before and, as needed, during the procedure.
We performed pars plana vitrectomy9 using a three-port procedure and conventional vitrectomy equipment (SupraVit; Midlabs, San Leandro, CA). After triamcinolone acetonide injection and vitreous removal, a focal retinal detachment (5 mm in diameter) (Figure 2B) was obtained by subretinal injection of BSS (rate: 90 μL/min) using a 41-gauge (G) needle. A small retinotomy (1.5 mm) was performed with microscissors (Figure 2C). Implants were inserted one by one into the subretinal space with a microforceps (Figures 2D and 2E) and tiled in a hexagonal pattern by gentle pressing over the retina. After subretinal fluid resorption through the retinotomy site, the retina was reattached by injection of 2 mL to 3 mL of perfluorocarbon (Figure 2F). The success of the implantation was then confirmed with fundus examination (Figure 3A) and optical coherence tomography (Figure 3B).
Figure 2.
The surgical procedure. Vitrectomy (A) is followed by retinal detachment with fluid injection (B). A small (1.5 mm) retinotomy (C) allows insertion of the modules in subretinal space (D-E). Retina is reattached (F) after injection of perfluorocarbon.
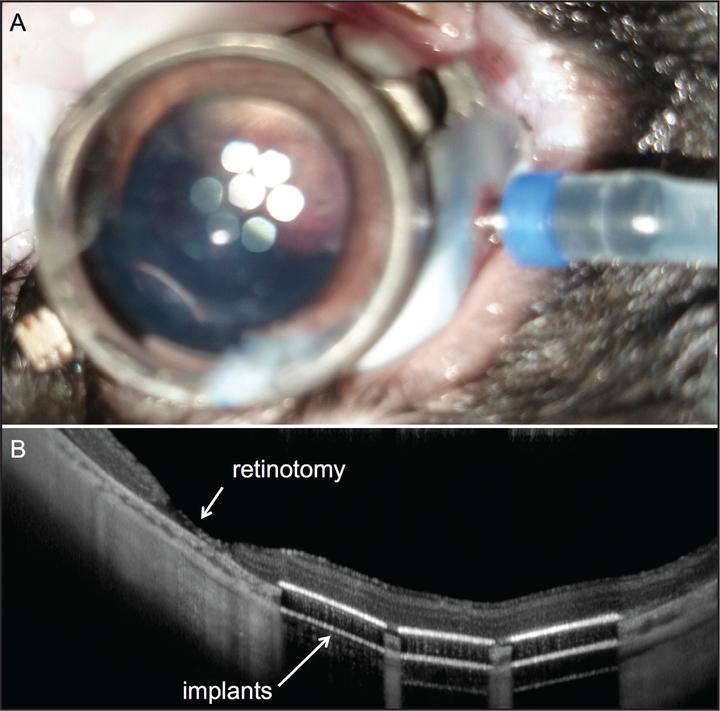
Figure 3.
Post-surgery imaging. (A) Fundus view after the implantation. (B) Optical coherence tomography demonstrates retinal reattachment. Modules follow the curvature of the eye globe.
DISCUSSION
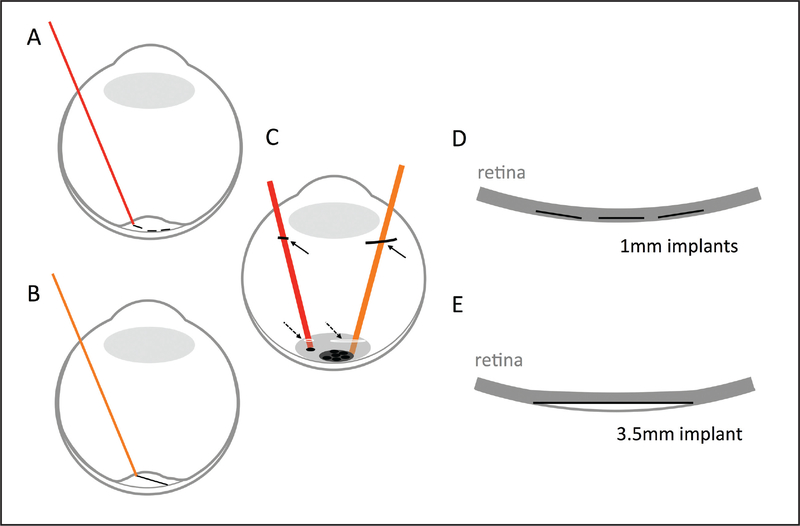
Successful implantation and tiling of seven modules of 1 mm in diameter in the subretinal space of a rabbit eye confirms feasibility of the proposed procedure. The use of 1-mm modules allows utilization of a 20-G intra ocular surgical instrumentation and makes the procedure minimally traumatic compared to implantation of a much larger implant in one piece (Figure 4). In addition, multiple small rigid modules better fit the spherical shape of the eyeball compared to a single, wider array (Figures 3B and 4D vs. Figure 4E). With seven modules, we covered around 3.5 mm of the retina, corresponding to 12° of the visual field (Figure 3A). Adding more would allow further expansion of the field in a desired direction. Air-fluid exchange, use of silicon oil, and endocoagulation in a few spots may be needed to ensure the long-term stability of the devices in human patients. We tried simplifying the surgery by attaching all modules to a soft polymer film, folding it, and inserting in one 1-mm wide piece to then unfold inside the bleb. However, unfolding it under the retina was quite difficult, and such manipulations led to additional retinal injury. We also tried attaching groups of two or three to straight polymer strips, but the alignment of such strips under the retina proved difficult. Therefore, we conclude that insertion and placement of individual modules one by one was the fastest and simplest procedure.
Figure 4.
Comparison between modular and single implant configurations with same total diameter, in the subretinal space of a human eye. (A-B) Side view of the placement of the seven 1-mm modules (A), compared to a single 3.5-mm implant (B). (C) Comparison of the sclerotomy (plain arrows) and retinotomy (dashed arrows) sizes for the two approaches. (D-E) Side view after retinal reattachment illustrates the curvature mismatch with a large single implant (E).
Acknowledgments
Funding was provided by NIH grant R01-EY-018608, by United States Department of Defense grant W81XWH-15-1-0009, and by Pixium Vision grant 1170660-200-UDERL.
Drs. Lorach and Palanker are consultants for Pixium Vision, and patents regarding the photovoltaic retinal prothesis are licensed by Stanford to Pixium Vision. The remaining authors report no relevant financial disclosures.
The authors would like to thank Gregory Orekhov for his help with development of the multimodular mounts and with surgeries.
REFERENCES
- 1.Humayun MS, Dorn JD, da Cruz L, et al. Interim results from the international trial of Second Sight’s visual prosthesis. Ophthalmology. 2012;119(4):779–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stingl K, Bartz-Schmidt KU, Besch D, et al. Subretinal Visual Implant Alpha IMS – Clinical trial interim report. Vision Res. 2015;111(Pt B):149–160. [DOI] [PubMed] [Google Scholar]
- 3.Ayton LN, Blamey PJ, Guymer RH, et al. First-in-human trial of a novel suprachoroidal retinal prosthesis. PLoS One. 2014;9(12):e115239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kitiratschky VB, Stingl K, Wilhelm B, et al. Safety evaluation of “retina implant alpha IMS” – a prospective clinical trial. Graefes Arch Clin Exp Ophthalmol. 2015;253(3):381–387. [DOI] [PubMed] [Google Scholar]
- 5.Wang L, Mathieson K, Kamins TI, et al. Photovoltaic retinal prosthesis: implant fabrication and performance. J Neural Eng. 2012;9(4):046014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mandel Y, Goetz G, Lavinsky D, et al. Cortical responses elicited by photovoltaic subretinal prostheses exhibit similarities to visually evoked potentials. Nat Commun. 2013;4:1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lorach H, Goetz G, Mandel Y, et al. Performance of photovoltaic arrays in-vivo and characteristics of prosthetic vision in animals with retinal degeneration. Vision Res. 2015;111(Pt B):142–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorach H, Goetz G, Smith R, et al. Photovoltaic restoration of sight with high visual acuity. Nat Med. 2015;21(5):476–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Machemer R The development of pars plana vitrectomy: a personal account. Graefes Arch Clin Exp Ophthalmol. 1995;233(8):453–468. [DOI] [PubMed] [Google Scholar]