Summary
Parkinson's disease is a neurodegenerative disorder. Parkinson's clinical feature is characterized by its motor manifestations, although its many nonmotor symptoms occur earlier and have more profound impact on the quality of patient's life. Acupuncture has been increasingly popular and has been used to treat patients with Parkinson's. In this article, we have studied the clinical reports of acupuncture treatment for Parkinson's, which were listed in Medline, PubMed, EMBASE, CNKI, and CINAHL databases in the past 15 years. It was found that acupuncture either manual or electroacupuncture stimulation at specific acupoints relieved some motor symptoms in patients with Parkinson's and markedly improved many nonmotor symptoms such as psychiatric disorders, sleep problems, and gastrointestinal symptoms. When it was used as an adjunct for levodopa, acupuncture improved therapeutic efficacy and reduced dosage and the occurrence of side effects of levodopa. However, the results were constrained by small sample sizes, methodological flaws, and blinding methods of studies. Although the evidence for the effectiveness of acupuncture for treating Parkinson's is inconclusive, therapeutic potential of acupuncture seems quite promising. More studies, either comparative effectiveness research or high‐quality placebo‐controlled clinical studies are warranted.
Keywords: Acupuncture, Motor symptoms, Nonmotor symptoms, Parkinson's disease
Introduction
Parkinson's disease (PD) is an age‐related, progressive neurodegenerative disorder. It affects one in a thousand people over 60 years of age and is a substantial source of economic cost. Although both genetic and environmental factors are implicated in the development of PD, the cause of disease is still unclear. The clinical manifestation of PD motor symptoms includes bradykinesia, resting tremor, rigidity of muscles and joints, gait, and posture imbalance. The occurrence of motor symptoms is mainly caused by the severe loss of dopaminergic neurons in the substance nigra of middle brain and subsequent depletion of dopamine in the striatum 1, 2. The nonmotor symptoms of PD are found in the vast majority of patients with PD, consisting of autonomic dysfunction, neuropsychiatric disturbance, sleep disorders, gastrointestinal symptoms, and many others 3, 4, 5. The nonmotor symptoms of PD and related disorders usually respond poorly to dopaminergic treatment. This indicates, in addition to the loss of dopamine, the changes in other neurotransmitters, such as serotonin, norepinephrine, and gamma‐aminobutyric acid (GABA) and glutamate, in the different brain regions and peripheral nervous systems, are involved in the pathogenesis of many nonmotor symptoms 6. There is currently no cure for PD. The prevalence medication for motor symptoms, such as dopamine replacement therapy, in particular levodopa treatment, is only symptomatic relief with limited effect, but has many adverse effects, for example, dyskinesia 7, 8, 9.
Acupuncture has been used to treat many conditions in China for more than 3000 years. Acupuncture is now one of the most popular complementary medicines and is used for the treatment of a variety of disorders worldwide. In general, acupuncture needle inserted at the specific acupoint stimulates nerve receptors both directly or indirectly, through mechanical coupling via the connective tissues surrounding the needle, then through the local reflex and the central nervous system, induces endocrine, neuroendocrine, autonomic, and systemic behavioral responses 10, 11. This suggests that acupuncture therapy beneficially affects a whole body even if it stimulates, through the fine needles, only limited sites on the body. Within past a few decades, acupuncture has become increasingly popular with both public and medical professionals, and it has been reported to be a very safe and well‐tolerated therapy with only minor side effects 12, 13, 14. Many patients with PD are reported using acupuncture as an alternative treatment at some points of their life. Indeed, it has been estimated that more than a quarter of patients with PD in the United States (40%), Britain (38.7%), Sweden (34.5%), Singapore (61%), and Argentina (25.7%) have used at least one form of complementary medicine, while 7–49% of them have used acupuncture as an alternative therapy 15, 16, 17, 18, 19. Many patients with PD experienced improvement of their conditions after acupuncture.
Recently, we have assessed the recent research development regarding the effects and mechanisms of acupuncture on PD models 20. In this article, we have reviewed the clinical acupuncture studies of Parkinson's and evaluated the effect of acupuncture therapy on motor and nonmotor symptoms in patients with PD.
Materials and Methods
Criteria for Considering Studies for Review
This review included the clinical studies that focused on the effect of penetrating acupuncture, with either manual or electrical stimulation, on patients with PD, without limitation on age, gender, duration of condition, and medication. The control included placebo, medication, or no treatment. Outcome measures included (1) PD motor symptom impairment rating scales; (2) PD nonmotor symptom impairment rating scales; (3) PD activity of daily living rating scales; (4) quality‐of‐life measures for PD; (5) changes in levodopa dose; and (6) alterations in functional neuroimaging and biochemical studies. Language restrictions were applied to English and Chinese.
Search Methods for Identification of Studies
The following electronic databases were searched in December 2014 for publications between 2000 and 2014: (1) PubMed; (2) MEDLINE; (3) EMBASE; (4) CNKI, and (5) CINAHL. The reference list of relevant studies and reviews was manually searched to identify more potential papers. The search term used in the studies was cross‐referenced acupuncture and its proprietary names, and PD and with its derivations.
Study Selection and Data Extraction
The titles and abstracts of collected studies were scanned to select potential reference. Relevant articles with potential for eligible studies were selected after reviewing full text, and then, data describing patients, duration and severity of condition, treatment, control groups, and outcomes were extracted.
A total of 176 studies were identified from the electronic databases and hand searching. After searching titles and abstracts, 142 studies were excluded due to the following reasons: (1) the studies were nonclinical; (2) the studies were irrelevant to PD; (3) the studies were irrelevant to acupuncture; (4) the studies were case report; (5) patients included were not typical idiopathic PD; and (6) the studies did not show valid outcome measures. Having evaluated full text of remaining 34 literatures, 14 were selected for this study based on predefined criteria. Among the selected studies, four were conducted in the United States, two originated from Korea, and eight were from China (Table 1). The screen process was summarized in a flow diagram (Figure 1).
Table 1.
Summary of included acupuncture clinical studies
| Study | Design, Sample size, Study duration | Characteristics | Acupoints | Intervention | Control | Outcome measures: Motor symptoms | Nonmotor symptoms | Others |
|---|---|---|---|---|---|---|---|---|
| Shulman, 2002 |
Uncontrolled open label, N = 20 (1) N = 7, 5 weeks (2) N‐13, 8 weeks |
Age: 68 years Duration: 8.5 years H&Y: 2.2 UPDRS: 38.7 Medication: N/A |
Body AP: LI4, GB34, ST36, K3, K7, SP6, SI3, TB5 Scalp AP: chorea trembling control area |
PD medication + body AP + scalp AP 60 min, twice a week for 5 or 8 weeks | N/A | UPDRS I to IV+, Total UPDRS+ H&Y+ | Sleep and rest+++ | |
| Cristian, 2005 |
Randomized Controlled Double blind, N = 14, 2 weeks |
Age: 72–74 years Duration: N/A H&Y: 2–4 UPDRS: N/A |
Body AP: K3, K10, L3, ST41 ST36, GB34, Bafeng points, MH6, LI4, GV20 | PD medication + body EA, 4 Hz for 20 min, 5 sessions, for 2 weeks (n = N/A) | PD medication + stimulation of nonacupoints, for 20 min, 5 sessions for 2 weeks (n = N/A) | UPDRS III+ to ++ | ADLs, PDQ‐8 Summary Index score++; depression, nausea, sleep problems++; orthostasis‐ | |
| Eng, 2006 |
Uncontrolled open label, N = 23, 24 weeks |
Age: 69.3 years Duration: 6.4 years H&Y: 2.1 UPDRS: 37.8 Medication: N/A |
Body AP: ST 42, SP 3, LI11, LI15, LI20, ST7, ST36 | PD medication + energy massage (tui na) + AP for 7–10 min, Once a week for 24 weeks + Qigong machine (n = 23) | N/A | UPDRS III‐ | PDQ‐39 + ++, BDI+++ | |
| Jiang, 2006 |
Randomized controlled, N = 30, 6 weeks |
Age: 65.6 years Duration: 6.0 years UPDRS: N/A Webster: 16.4 (AP), 15.3 (C) |
Scalp AP: MS4, MS6, MS8, MS9, MS14 | Madopar + scalp EA, 100 Hz, for 30 min, 5 times/week, total 6 weeks | Medopar 125–250 mg/each, 3–4 times/day | UPDRS III+++ | Constipation+++, Sweating+++ | |
| Yang, 2006 |
Controlled open label, N = 38, 68 days |
Age: N/A Duration: N/A UPDRS: N/A Medication: Prolopa |
Body AP: LI4, SI3, LI5, SI6, LI11, PC3, LU5, LR3, ST41, KI3, GB34, SP9, BL40, GB30 Scalp AP: MS1, MS5, MS6 | Prolopa + body AP + scalp AP 30 min, 1 course = 5 AP, once every 2nd day for 10 days, 7 days interval, then next course, total 4 courses | Prolopa 62.5–500 mg/each, 2–4 times/day | Total UPDRS+++ | N/A |
SOD↑+++ LPO↓+++ |
| Zou, 2006 |
Uncontrolled open label, N = 30, 6 months |
Age: 47–81 Duration: 1–16 H&Y: II=6, III=9, IV=12, V = 3 Medication: Madopar 0.5–1.25 g |
Body AP: GV14, GV20, GV26, GB20, TE17, ST36, ST40, SP6, KI3, LR3 Scalp AP: dance and tremor zone |
Madopar + body AP + scalp AP, 1 course = 5 AP, once every 2nd day for 10 days, 7 days interval, then next course for total 6 months | N/A |
Webster scores +++ (n = 4), ++ (n = 16), +‐0 (10), total effective rate: 66.7%. Madopar reduction+ |
Constipation+++ | Madopar dosage reduced after AP |
| Ren 2008 |
Controlled, N = 80, 4 weeks |
Age: N/A Duration: N/A UPDRS: N/A |
Body AP: TE4, LI5, PC7, SI6, LI11, LU5, PC3, HT3, TE14, LI15, SI9, LR4, KI3, ST41, SP9, GB34, BL40, GB30, BL36 | Madopar 752 mg ± 159 + AP 30 min, once a day for 10 days as a session, interval 3–5 days, and another session | Madopar 749 ± 169 |
Tremor++, Gait++ |
N/A |
Madopar dosage: AP: 504 ± 179 Control: 726 ± 261 |
| Chae, 2009 |
Randomized single blind uncontrolled, N = 10, 1 time |
Age: 45–66 years Duration: 3.0 ± 2.0 years H&Y: 1.6 ± 0.2 UPDRS: 33.0 ± 15.5 |
GB34 | AP for 9 min | Placebo | Finger‐tapping task+++ | N/A | fMRI showed AP increased activation in the putamen and the motor cortex |
| Chen, 2012 |
Randomized Controlled, N = 60 6 weeks |
Age: N/A Duration: N/A UPDRS: N/A |
GV20, EX‐HN 3, EX‐HN 1 |
AP + Madopar + Tolterodin e 1 mg, 2 times/day |
Madopar + Tolterodine 2 mg, 2times/day |
UPDRS III+++ | Bladder function+++ | |
| Cho, 2012 |
Randomized single blind controlled, N = 22, 8 weeks |
Age: 55–57 years Duration: 5–6 years H&Y: 1.6–3.0 UPDRS: 33.0 ± 15.5 |
GB20, LI11, GB34, ST36, LR3 |
(1) PD medication + VA, 2 times weekly for 8 weeks (n = 13) (2) PD medication + AP (rotated at 2 Hz for 10s, and maintained for 20 min), 2 times weekly for 8 weeks (n = 13) |
PD medication only (n = 9) |
Total UPDRS+++ UPDRS III+++ |
BDI+++ | |
| Xia, 2012 |
Randomized Controlled, N = 60, 12 weeks |
Age: N/A Duration: N/A UPDRS: N/A |
GV20, EX‐HN 3, EX‐HN 1, LR3, SP6 | Madopar+fluoxetine + AP for 12 weeks | Madopar+fluoxetine | N/A | Depression+++ | Serum BDNF+++ |
| Lei, 2014 |
Randomized Controlled, N = 13, 3 weeks |
Age: N/A Duration: N/A UPDRS: N/A |
N/A | EelctroAP 30 min, once a week for 3 weeks | Sham |
Balance+++, gait+++, postural transitions+++ |
N/A | |
| Yuan, 2014 |
Controlled, Open label, N = 49, 3–6 weeks |
Age: N/A Duration: N/A UPDRS: N/A |
DU15, bilateral BL10, GB20, GB12 | EelctroAP 30 min, 3 times a week for 3 to 6 weeks + Madopar | Madopar 250 mg, 3 times/day | Webster scale ++ to +++ | N/A | 87% of patients stopped medication for 2 weeks after AP |
| Liang, 2014 |
Controlled, Open label, N = 70, 24 weeks |
Age: 48–73 years Duration: 3–7 years H&Y: 1.0–3.0 UPDRS: 33.0 ± 15.5 |
Bilateral GB20, GB12, BL10; GV15 | (1) AP, 30 min/each time, 3 times weekly for 24 weeks (n = 35) | Madopar 250 mg, 3 times/day, for 24 weeks (n = 35) | PDQ‐39 + ++ | UPDRSII+++ PDSS+++ PDQ‐39 + ++ |
AP, acupuncture; N, numbers; UPDRS, Unified Parkinson's Disease Rating Scale; N/A, not available; min, minute; S&E ADLs, Schwab and England Activities of Daily Living; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; PDQ‐39, Parkinson's Disease Questionnaire; PDSS, Parkinson's disease sleep scale; H&Y, Hoehn and Yahr stage; fMRI, functional magnetic resonance imaging; SOD, superoxide dismutase; LPO, lipid peroxides; BDNF, brain‐derived neurotrophic factor. ↑, increase; ↓, decrease; +, indicates minor improvement; ++, indicates median improvement; +++, indicates significant improvement. ‐, indicates worsening effect.
Figure 1.
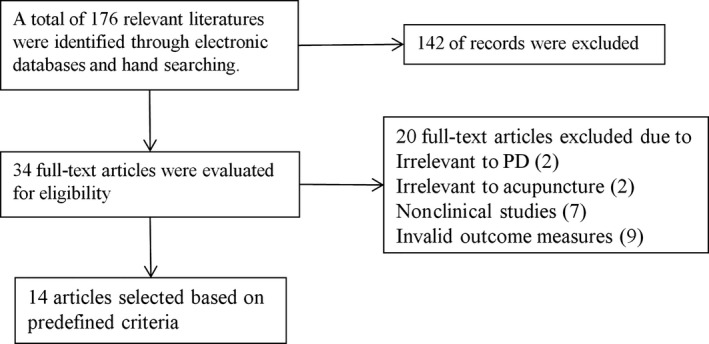
Flowchat of study selection.
Effect of Acupuncture on Motor Symptoms of Parkinson's Disease
During past 15 years, there are an increasing number of clinical studies of acupuncture therapy in PD (Table 1). Cristian et al. 21 conducted a randomized controlled blind study with 14 PD patients. The patients were treated with electroacupuncture, 20 min/day, five sessions a week for 2 weeks. The data showed a trend toward significant improvement in motor scores on the Unified Parkinson's Disease Rating Scores (UPDRS) III (motor function assessment). This was accompanied by the improved activities of daily living and decreased body discomfort compared to the nonelectroacupuncture group. Using scalp acupuncture, Jiang et al. 22 carried out a randomized controlled clinical study in which 30 patients with PD were divided into two groups. Patients in treatment group were given scalp electroacupuncture for 30 min, once a day, 5 times a week for total 6 weeks, plus medication Madopar. Patients in control group were only given Madopar. The UPDRS and Webster scores were used to assess the functional changes before and after acupuncture treatment. It was found that tremor, rigidity, and bradykinesia were improved compared with base lines in both groups, respectively. However, patients in scalp acupuncture group showed more significant improvement in motor function than those of control group judged by UPDRSIII scores 22. In another study, 38 patients with PD were divided into acupuncture plus drug group and drug control group. Patients in acupuncture group were treated with scalp acupuncture and body acupuncture for 30 min, once every 2 days, 10 times as a course and four courses in total, plus medication Prolopa. Patients in control group were only given Prolopa. At the end of treatment, total UPDRS scores were significantly reduced in acupuncture group compared with baseline scores and with scores of control group 23. In a long‐term study, 30 PD subjects, with diminished therapeutic effect and drug‐induced complications, were treated with combination of scalp acupuncture and body acupuncture 24. Acupuncture was given once every second day for 10 days as one course of the treatment, after 7 days interval, next course of treatment was followed and total treatment was for 6 months. By the end of treatment, Webster score assessment showed that acupuncture produced a remarkable effect in four cases, effective in 16 cases, and failed to show improvement in 10 cases and total effective rate was 66.7% compared with baseline scores. Further, therapeutic effects of levodopa were enhanced, while its dose and complications being reduced 24.
In a large clinical study 25, 80 PD subjects were divided into treatment group (n = 50) and control group (n = 30), it was found that acupuncture treatment for 4 weeks produced a significant improvement in motor function including tremor and gait disturbance compared to control group; however, the study did not mention how the motor functions were assessed 25. Using functional magnetic resonance imaging (fMRI) technique, Chae et al. 26 explored the neural mechanism of specific effect of acupuncture stimulation on the motor function of patients with PD. When acupuncture stimulation at acupoint GB34 on patients with PD, fMRI revealed the activation of the putamen and primary motor cortex. The patients experienced a significant improvement of motor function, finger‐tapping tasks of affected hand following acupuncture 26. This suggested that acupuncture exerted its beneficial effect via its ability to modulate neuronal activities in the specific motor‐related brain regions in patients with PD.
Recently, Chen et al. 27 conducted a clinical study of acupuncture treatment with PD patients. Sixty PD subjects were randomly divided into two groups: patients in treatment group were treated with electroacupuncture once a day plus Madopar for 6 weeks; patients in control group were given Madopar only. By the end of 6‐week treatment, the UPDRSIII assessment showed that acupuncture produced a significant improvement in motor function with reduced adverse effect compared to Madopar alone group 27. Similarly, Cho et al. 28 reported, in a randomized controlled clinical study with 43 PD patients, that acupuncture treatment twice a week for 8 weeks significantly improved UPDRS total scores and UPDRSIII scores in patients with PD, while control group did not show any significant improvement in any outcome.
Very recently, a small randomized controlled clinical study was conducted to evaluate the efficacy of electroacupuncture for improving gait and balance in patients with PD using objective modalities based on innovative body worn sensors technology 29. Thirteen patients with PD were randomly treated with real acupuncture (n = 10) or sham acupuncture (n = 3) for 30 min, once weekly for 3 weeks. Assessments, measured before and after treatment, include gait, balance, and postural transitions. By the end of treatment, acupuncture group showed a significant improvement in gait, balance, and UPDRSIII compared to baseline. No difference was found in control group compared to baseline. Group comparison revealed that balance, gait speed, and stride length during all conditions was significantly improved in acupuncture group compared to control group 29.
The acupuncture technique called “the seven acupoints of cranial base” (SACB) was used as the adjunct to treat patients with PD in China recently and showed some interesting results. The SACB consists of DU15, bilateral BL10, GB20, and GB12 which are believed to be located at the very place of cranial bottom 30. In an uncontrolled open labeled clinical study, 49 patients with PD were recruited and categorized as early (<10 scores, n = 4), moderate (11–20 scores, n = 43), and advanced stage (21–25 scores, n = 2) according to the Webster scores. All patients were treated with electroacupuncture at the “seven acupoints” for 30 min, 3 times a week. Then, the courses of acupuncture treatment were decided according to the severity of condition. After the initial three acupuncture treatments, patients with early stage were asked to stop medication, then treated with acupuncture for further 6 times (total nine treatments within 3 weeks). Patients with moderate stage, after the first three acupuncture treatments, were asked to reduce medication to half dose; after given further three acupuncture treatments, they were asked to stop medication, then given further six acupuncture treatments (total 12 treatments within 4 weeks). For advanced stage, patients, after the initial three acupuncture treatments, were asked to reduce the dose of medication by one‐third, then after further six acupuncture treatments, were asked to reduce the dose by half on the base of first reduced dose; after one further treatment, patients were asked to stop the medication and were given further nine acupuncture treatments (total 19 treatment within 6 and half weeks). Before acupuncture, the average of Webster score was 16.74 ± 3.35, and it was significantly reduced to 11.50 ± 4.17 after acupuncture treatment. Approximately 87% of patients with PD stopped medication for two weeks after last acupuncture treatment and maintained good improvement of their symptoms 30. It would be very interesting to know the outcome of the follow‐up study.
Taken together, the studies mentioned above demonstrated that acupuncture including scalp acupuncture ameliorated motor symptoms in patients with PD. How does acupuncture exert its motor function improvement is not well studied in clinical setting. However, many basic studies shed light on the mechanism of acupuncture on motor function, review see 20. It has been reported that acupuncture stimulation at specific acupoints markedly reduced rotational behavioral, significantly reduced the loss of dopaminergic neurones, and significantly elevated expression of TrkB in the lesioned substantia nigra 31, 32. Acupuncture also significantly increased tyrosine Hydroxylase‐immunoreactive fiber density in the lesioned striatum 33 and markedly reversed decrease in superoxide dismutase and glutathione peroxidize, while decreased the increase in the levels of malondialdehyde, tumor necrosis factor‐alpha and interleukin‐1 in the brain nigrostriatal system 32, 34. These studies indicated that acupuncture protected dopaminergic neurons against toxic insults and increase dopamine production in the brain by inducing release of neurotrophic factor, enhancing antioxidant agents, and inhibit inflammatory.
Effect of Acupuncture on Nonmotor Symptoms of Parkinson's Disease
Nonmotor symptoms (NMSs) of PD are common but are often under‐recognized in clinic practice due to the lack of spontaneous complaints from patients. NMS in PD was systematically reviewed for the first time by Chaudhuri et al. 3. NMS ranges from autonomic dysfunction, neuropsychiatric disorders, sleep disturbance, sensory symptoms to gastrointestinal syndromes, fatigue, and many others and are often under‐treated 3. NMS occurs throughout the course of the disease. Some of them, such as depression, fatigue, and smelling dysfunction, may appear at the earliest stage of the disease in un‐treated patients. Others appear at the advanced stage of the disease. At the time of diagnosis, the prevalence of NMS among patients with PD was 21% (pain, urinary symptoms, depression, and anxiety) and went up to 88% after 7‐year disease progression 14, 35. Indeed, nonmotor aspects of PD had greater impact on quality of life and cause higher institutionalization rates and healthcare cost 36.
Psychiatric Disorders
Depression was one of the most common psychiatric symptoms in nonmotor features in PD 37. Studies indicated that approximately 17–50% of patients with PD had depression 4, 38. Patients with depression felt sad, anxiety, irritable, and restless and might lose interest in activities once enjoyable. The cause of depression in PD was not clear, but the altered levels of serotoninergic, noradrenergic, and dopaminergic neurotransmission in brain were implicated as relevant factors 39, 40, 41. In acupuncture clinical studies, one of the prominent responses to acupuncture in patients with PD was the reported therapeutic effect on depression 21, 28, 42, 43. Many patients experienced great alleviation in their symptoms. This was reflected on the results of Beck Depression Inventory, one of the most widely used instruments for measuring severity of depression, which showed a significant decrease in the scores in patients after acupuncture therapy compared with control groups 21, 28, 42, 43. Acupuncture is very effective in treating depression in patients without PD. Clinical studies showed that acupuncture was superior to drug treatment in reducing depression, anxiety in non‐PD patients with psychiatric disorders 44, 45.
Sleep Disorders
Excessive daytime somnolence (EDS) and insomnia are common symptoms of sleep disturbance of NMS in PD, affecting up to 50% or even higher proportion of patients 4, 46. Sleep disorders are more frequent in patients with advanced stage of disease and have large impact on the quality of life of patients. The occurrence of EDS is often associated with long‐term medication of dopamine agonist, in particular, levodopa 47. Acupuncture was reported to effectively improve sleep disorders in patients with PD. Acupuncture study with 20 PD patients showed that 85% of patients treated with acupuncture reported a subjective improvement in sleep problems and this was confirmed by the improvement in the sleep and rest category of the Sickness Impact Profile scores 14. In another randomized controlled double‐blind study, patients with PD receiving electroacupuncture showed a significant improvement in sleep problems 21. Very recently, a controlled clinical study with 70 PD patients reported that “the Seven Acupoints of the Cranial Base” acupuncture technique significantly improved sleep in patients judged by Parkinson Disease Sleep Scale (PDSS) compared with control group 48. In non‐PD patients, intradermal acupuncture on HT7 and PC6 stabilized the sympathetic activities and improved insomnia in stroke patients 49. Acupuncture stimulation at PC6, HT7, and ST36 acupoints, commonly used to treat insomnia in clinic, increased GABA levels and elevated the expression of GABA(A) receptor in hypothalamic neurons of insomnia rats 50. This may explain the insomnia‐relieving effect of acupuncture. The results of those studies suggest that improvement of sleep disorders by acupuncture is potentially mediated by a variety of neurotransmitters including GABA, norepinephrine, melatonin, and beta endorphin, (for review, see 51).
Gastrointestinal Symptoms
Gastrointestinal dysfunctions in PD included dysphagia, nausea, bloating, constipation, and many others 3, 52. Nausea occurred the most often due to dopaminergic therapy; however, it may occur in untreated patients 53. Constipation is the most prominent manifestation of lower gastrointerestinal dysfunction in PD, and it may precede the development of motor symptoms of PD by many years 53, 54. Many studies showed that acupuncture treatment to patients with PD improved gastrointestinal symptoms, such as nausea and constipation without inducing any adverse effect 21, 22, 24. It was reported that the effect of acupuncture on gastrointestinal dysfunction was related to its activation of various brain nuclei, such as the nucleus tractus solitaries, dorsal motor nucleus of vagus, and periaqueductal gray, through modulating the imbalance between sympathetic and parasympathetic activity of those nuclei 55. Similarly, acupuncture markedly relieved gastrointestinal symptoms such as constipation, irritable bowel syndrome, and functional dyspepsia in patients without PD 56, 57, 58.
Autonomic Symptoms
Bladder dysfunction (urinary urgency/frequency) was one of the most common autonomic symptoms, and it occurred in 55–80% of patients with PD 59. Urinary disturbance can appear early in the disease, and symptoms get worse with increased motor disability 35. Recently, a clinical acupuncture study of Parkinson's with overactive bladder syndrome was conducted to assess the therapeutic effect of acupuncture as an adjunctive on bladder function 27. It was found that at the end of 6‐week treatment, acupuncture significantly improved the average frequency urination of 24 h, frequency of incontinence of 24 h, and average urine volume at a time, compared with the scores obtained prior to treatment; the improvement of urinary function in acupuncture plus drug treatment group was significantly better than those of drug alone group 27. It was suggested that the therapeutic effect of acupuncture on bladder dysfunction might be attributed to its modulation on autonomic system and central cholinergic activity 60. In non‐PD patients, electroacupuncture treatment significantly improved chronic bladder dysfunction in patients with traumatic spinal cord injury 61 and had a long‐lasting reduction of blood pressure in patients with mild‐to‐moderate hypertension 62.
Many clinical and basic studies reported that acupuncture including manual and electroacupuncture modulated the transmission of dopamine, noradrenalin, serotonin, glutamate, GABA; and the activation of hypothalamic–pituitary–adrenal axis within central nervous system and peripheral nervous system 51, 55, 63. These effects may be attributed to the improvement of PD nonmotor symptoms by acupuncture.
Discussion
Present study reviewed the data of 519 patients with PD from 14 clinical studies. The results from some of the included studies showed the potential benefits of acupuncture for treating PD, especially nonmotor symptoms seems to be more beneficial from acupuncture treatment. However, many methodological flaws presented in most studies limited the reliability of results. Therefore, the results included in this study should be interpreted with cautious.
Outcome measures for motor symptoms differed among the included studies. For example, seven studies used the UPDRS, two studies used Webster scale, and another five studies only described changes in individual motor symptom. Among seven studies used UPDRS, four studies showed moderate to marked improvement in UPDRS III motor scores before and after acupuncture, between acupuncture plus medication and medication alone groups. One study showed negative outcome in UPDRS III motor scores 42, and two studied presented minor to moderate improvement in total UPDRS scores. Two studies used Webster scale presented marked improvement in motor symptoms. Five of 14 studies described changes in individual motor symptom following acupuncture treatment. For example, Lei et al. 29 described the improvement in balance, gait, and postural transition following acupuncture. It is difficult to draw a valid comparative conclusion based on inconsistent outcome measures. Suitable outcome measures such as UPDRS should be applied as a standard outcome measure and full data on outcome measures including mean and standard deviation should be presented.
Although many of included studies showed a moderate to marked improvement in motor function, one study 42 reported a worsening in UPDRS motor scores (24.0 vs. 26.4, P = 0.018). In this study, patients with PD were given acupuncture treatment for 7–10 min, once a week for 6 months 42. However, patients in majority of included studies were given acupuncture for 20–60 min, 2–3 times a week. This implied that duration and frequency of intervention might play an important role in the outcome of treatment.
Although many nonmotor symptoms occur even before the appearance of motor symptoms, only 9 of 14 studies reported presence of the nonmotor symptoms. This is not surprise as patients do not spontaneously complain their nonmotor symptoms to doctors 3. Within nine studies, depression was the most reported symptom, followed by sleep disorder, constipation, and bladder dysfunction. This is consistent with other studies showing depression is one of the most complained nonmotor symptoms from patients with PD 37, 38. All studies reported that acupuncture significantly improved depression of patients with PD. Beck's Depression Inventory (BDI), PDQ‐39, and PDQ8 were applied to rate the changes in depression within different studies. This led to difficult for comparison as each instrument covered different aspect of item and made the data less reliable. Similarly, the outcome of sleep disorder was measured by PDSS and ISI scores between studies. Outcome measures for other NMS were barely mentioned by relevant studies. Indeed, there is a need to achieve an agreement on what are the accepted outcome measures for NMS in PD.
Complete lack of control group occurred in 3 of 14 included studies. It has been known that the demonstration of efficacy of new treatment is based on comparing the response in the treated group with that of control group receiving placebo or another treatment. Without control group, it is very unlikely to have a reliable comparison of different treatments. Within other 11 studies, one used placebo control and another one used sham control and the remaining nine studies chosen PD medication as controls. It has been suggested that comparing acupuncture plus drug treatment with drug only may generate false favorable therapeutic effect, because it did not demonstrate specific therapeutic effects without a placebo control 64. Further, a sham control is necessary to eliminate any nonspecific physiological effect. Alternatively, comparative effectiveness research might be a good way to assess the effectiveness of acupuncture, because it compares more than two different interventions which have clinical evidence and relevance to clinical settings 65.
Discrepancy in acupoints used in the studies made it difficult to interpret the results and compare the studies. Within 14 studies, approximately 40 body acupoints were used, only LR3, GB34, ST36, and K3 were repeatedly chosen by 5 or 6 studies, while majority of acupoints were used for only in 1 or 2 times. Currently, there was unknown validated treatment protocol of acupuncture for PD, and there was no consensus regarding acupoint selection in the previous studies. Recently, many PD model studies suggest that stimulation at acupoint GB34 and ST36 could enhance motor function and promote dopaminergic cells against toxic insults 31, 32, 33, 34. Studies of fMRI on human subjects found that stimulation on GB34 activated motor‐related brain regions such as the putamen, caudate nucleus and thalamus and cerebellum 66. The efficacy of other acupoints used in the studies was barely investigated. In the future, acupuncture research in PD needs to identify more acupoints that are effective in PD treatment and achieve an agreement on the selection of acupoints in PD acupuncture treatment.
All included studies except one 25 evaluated the patients immediately before and after acupuncture treatment, whereas results of long‐term duration of any improvement after acupuncture were not available. Sustainable therapeutic effect is an important part of assessment of effectiveness of any treatment so follow‐up evaluation should be conducted in a reasonable time period after completing treatment.
Many methodology flaws were found within included studies. For example, 8 of 14 included studies did not show proper diagnostic criteria for recruitment, and disease severity of the patients eligible to participate the treatment was not disclosed in most studies. Although 7 of 14 studies stated as randomized, only two were single blind controlled and one was double‐blind controlled studies. There was a lack of well‐design randomized, double‐blind, and placebo‐controlled studies. Although acupuncture is safe and well‐tolerated, majority of studies did not mention the adverse effect and any dropout and withdraw during treatment.
Future clinical acupuncture study should follow accepted standards of methodology such as CONSORT and STRICTA checklists. In particular, studies should have sufficiently large sample sizes, should be based on data from appropriate pilot studies, and to ensure reproducibility. Even if further clinical studies confirm acupuncture to be therapeutic valuable more evidence should be required on whether it has matched the effectiveness of conventional medicine or has significant advantage over conventional medicine. Further, some common practical settings should help improve the quality of future clinical studies. So we propose that (1) comprehensive assessment of patients with PD, not only about motor symptoms also nonmotor symptoms, should be conducted. (2). Using the well‐established and universally recognized measures for motor and nonmotor symptoms assessment, such as UPDRS in which the scores of each part should be reported. (3). Acupuncture treatment should include obligatory acupoints and optional acupoints. The former should include proven motor‐related acupoints such as GB34 and ST36 for motor symptom treatment 32, 66. The selection of latter is dependent on the nonmotor symptoms and other conditions. (4). Needle duration should be expected to maintain at least 20 min each time for acupuncture to produce a certain level of therapeutic effect. (5). A proper follow‐up to evaluate the sustainable therapeutic effect of acupuncture. We hope that this will help reduce the discrepancy between the studies and improve the quality of treatment.
In conclusion, although the evidence for the effectiveness of acupuncture for treating PD is inclusive, data from the reviewed studies showed that therapeutic potential of acupuncture in treating Parkinson's seems rather promising. More studies, either comparative effectiveness research or high‐quality placebo‐controlled clinical studies should be conducted.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgment
We thank the IT support from King's College London.
References
- 1. Hornykiewicz O. Chemical neuroanatomy of the basal ganglia – normal and in Parkinson's disease. J Chem Neuroanat 2001;22:3–12. [DOI] [PubMed] [Google Scholar]
- 2. Obeso JA, Marin C, Rodriguez‐Oroz C, et al. The basal ganglia in Parkinson's disease: Current concepts and unexplained observations. Ann Neurol 2008;64(Suppl 2):S30–S46. [DOI] [PubMed] [Google Scholar]
- 3. Chaudhuri KR, Healy DG, Schapira AH. Non‐motor symptoms of Parkinson's disease: Diagnosis and management. Lancet Neurol 2006;5:235e45. [DOI] [PubMed] [Google Scholar]
- 4. Chaudhuri KR, Odin P, Antonini A, Martinez‐Martin P. Parkinson's disease: The non‐motor issues. Parkinsonism Relat Disord 2011;17:717–723. [DOI] [PubMed] [Google Scholar]
- 5. Garcia‐Ruiz PJ, Chaudhuri KR, Martinez‐Martin P. Non‐motor symptoms of Parkinson's disease A review…from the past. J Neurol Sci 2014;338:30–33. [DOI] [PubMed] [Google Scholar]
- 6. Ferrer I. Neuropathology and neurochemistry of non motor symptoms in Parkinson's disease. Parkinsons Dis 2011;2011:708404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Olanow CW, Schapira AH. Therapeutic prospects for Parkinson disease. Ann Neurol 2013;74:337–347. [DOI] [PubMed] [Google Scholar]
- 8. Salat D, Tolosa E. Levodopa in the treatment of Parkinson's disease: Current status and new developments. J Parkinsons Dis 2013;3:255–269. [DOI] [PubMed] [Google Scholar]
- 9. Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: A review. JAMA 2014;311:1670–1683. [DOI] [PubMed] [Google Scholar]
- 10. Dong Q, Dong X, Li H, et al. The influence of electroacupuncture on the activity of deep body receptors. Shanghai J Acupunct 2002;21:38–40. [Google Scholar]
- 11. Langevin HM, Churchill DL, Wu J, et al. Evidence of connective tissue involvement in acupuncture. FASEB J 2002;16:872–874. [DOI] [PubMed] [Google Scholar]
- 12. Posadzki P, Alotaibi A, Ernst E. Prevalence of use of complementary and alternative medicine (CAM) by physicians in the UK: A systematic review of surveys. Clin Med 2012;12:505–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rabinstein AA, Shulman LM. Acupuncture in clinical neurology. Neurologist 2003;9:137–148. [DOI] [PubMed] [Google Scholar]
- 14. Shulman LM, Wen X, Weiner WJ, et al. Acupuncture therapy for the symptoms of Parkinson's disease. Mov Disord 2002;17:799–802. [DOI] [PubMed] [Google Scholar]
- 15. Ferry P, Johnson M, Wallis P. Use of complementary therapies and non‐prescribed medication in patients with Parkinson's disease. Postgrad Med J 2002;78:612–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pecci C, Rivas MJ, Moretti CM, et al. Use of complementary and alternative therapies in outpatients with Parkinson's disease in Argentina. Mov Disord 2010;25:2094–2098. [DOI] [PubMed] [Google Scholar]
- 17. Rajendran PR, Thompson RE, Reich SG. The use of alternative therapies by patients with Parkinson's disease. Neurology 2001;57:790–794. [DOI] [PubMed] [Google Scholar]
- 18. Tan LC, Lau PN, Jamora RD, Chan ES. Use of complementary therapies in patients with Parkinson's disease in Singapore. Mov Disord 2006;21:86–89. [DOI] [PubMed] [Google Scholar]
- 19. Lökk J, Nilsson M. Frequency, type and factors associated with the use of complementary and alternative medicine in patients with Parkinson's disease at a neurological outpatient clinic. Parkinsonism Relat Disord 2010;16:540–544. [DOI] [PubMed] [Google Scholar]
- 20. Zeng BY, Salvage S, Jenner P. Current development of acupuncture research in Parkinson's disease. Int Rev Neurobiol 2013;111:141–158. [DOI] [PubMed] [Google Scholar]
- 21. Cristian A, Katz M, Cutrone E, Walker RH. Evaluation of acupuncture in the treatment of Parkinson's disease: A double‐blind pilot study. Mov Disord 2005;20:1185–1188. [DOI] [PubMed] [Google Scholar]
- 22. Jiang XM, Huang Y, Zhuo Y, Gao YP. Therapeutic effect of scalp electroacupuncture on Parkinson disease. Nan Fang Yi Ke Da Xue Xue Bao 2006;26:114–116. [PubMed] [Google Scholar]
- 23. Yang DH, Shi Y, Jia YM. Influence of acupuncture plus drug in the amelioration of symptoms and blood antioxidant system of patients with Parkinson's disease. Chin J Chin Rehabil 2006;10:14–16. [Google Scholar]
- 24. Zou Y. Clinical observation on acupuncture treatment of Parkinson's syndrome. J Acupunct Tuina Sci 2006;4:211–212. [Google Scholar]
- 25. Ren XM. Fifty cases of Parkinson's disease treated by acupuncture combined with madopar. J Tradit Chin Med 2008;28:255–257. [DOI] [PubMed] [Google Scholar]
- 26. Chae Y, Lee H, Kim H, et al. Parsing brain activity associated with acupuncture treatment in Parkinson's diseases. Mov Disord 2009;24:1794–1802. [DOI] [PubMed] [Google Scholar]
- 27. Chen YL, Feng WJ, Zhang XL. Parkinson's disease combined with overactive bladder syndrome treated with acupuncture and medication. Zhongguo Zhen Jiu 2012;32:215–218. [PubMed] [Google Scholar]
- 28. Cho SY, Shim SR, Rhee HY, et al. Effectiveness of acupuncture and bee venom acupuncture in idiopathic Parkinson's disease. Parkinsonism Relat Disord 2012;18:948–952. [DOI] [PubMed] [Google Scholar]
- 29. Lei H, Toosizadeh N, Schwenk M, et al. Objective assessment of electro‐acupuncture benefit for improving balance and gait in patients with Parkinson's disease. Neurology 2014;82(Suppl 10):P3.074. [Google Scholar]
- 30. Yuan Y, Chen F, Yang JS. Forty‐nine cases of Parkinson's disease treated by acupuncture adjunctive therapy. Zhongguo Zhen Jiu 2014;34:53–54. [PubMed] [Google Scholar]
- 31. Park HJ, Lim S, Joo WS, et al. Acupuncture prevents 6‐hydroxydopamine‐induced neuronal death in the nigrostriatal dopaminergic system in the rat Parkinson's disease model. Exp Neurol 2003;180:93–98. [DOI] [PubMed] [Google Scholar]
- 32. Yu YP, Ju WP, Li ZG, Wang DZ, Wang YC, Xie AM. Acupuncture inhibits oxidative stress and rotational behaviour in 6‐hydroxydopamine lesioned rat. Brain Res 2010;1336:58–65. [DOI] [PubMed] [Google Scholar]
- 33. Kim YK, Lim HH, Song YK, et al. Effect of acupuncture on 6‐hydroxydopamine‐induced nigrostratal dopaminergic neuronal cell death in rats. Neurosci Lett 2005;384:133–138. [DOI] [PubMed] [Google Scholar]
- 34. Liu XY, Zhou HF, Pan YL, et al. Electroacupuncture stimulation protects dopaminergic neurons from inflammation‐mediated damage in medial forebrain bundle‐transected rats. Exp Neurol 2004;189:189–196. [DOI] [PubMed] [Google Scholar]
- 35. O'Sullivan SS, Williams DR, Gallagher DA, Massey LA, Silveira‐Moriyama L, Lees AJ. Nonmotor symptoms as presenting complaints in Parkinson's disease: A clinicopathological study. Mov Disord 2008;23:101–106. [DOI] [PubMed] [Google Scholar]
- 36. Chaudhuri KR, Martinez‐Martin P, Brown RG, et al. The metric properties of a novel non‐motor symptoms scale for Parkinson's disease: Results from an international pilot study. Mov Disord 2007;22:1901–1911. [DOI] [PubMed] [Google Scholar]
- 37. Gallagher DA, Schrag A. Psychosis, apathy, depression and anxiety in Parkinson's disease. Neurobiol Dis 2012;46:581–589. [DOI] [PubMed] [Google Scholar]
- 38. Reijnders JS, Ehrt U, Lousberg R, Aarsland D, Leentjens AF. The association between motor subtypes and psychopathology in Parkinson's disease. Parkinsonism Relat Disord 2009;15:379–382. [DOI] [PubMed] [Google Scholar]
- 39. Frisina PG, Haroutunian V, Libow LS. The neuropathological basis for depression in Parkinson's disease. Parkinsonism Relat Disord 2009;15:144–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Politis M, Wu K, Loane C, et al. Depressive symptoms in PD correlate with higher 5‐HTT binding in raphe and limbic structures. Neurology 2010;75:1920–1927. [DOI] [PubMed] [Google Scholar]
- 41. Walter U, Hoeppner J, Prudente‐Morrissey L, Horowski S, Herpertz SC, Benecke R. Parkinson's disease‐like midbrain sonography abnormalities are frequent in depressive disorders. Brain 2007;130:1799–1807. [DOI] [PubMed] [Google Scholar]
- 42. Eng ML, Lyons KE, Greene MS, Pahwa R. Open‐label trial regarding the use of acupuncture and yin tui na in Parkinson's disease outpatients: A pilot study on efficacy, tolerability, and quality of life. J Altern Complement Med 2006;12:395–399. [DOI] [PubMed] [Google Scholar]
- 43. Xia Y, Wang HD, Ding Y, Kang B, Liu WG. Parkinson's disease combined with depression treated with electroacupuncture and medication and its effect on serum BDNF. Zhongguo Zhen Jiu 2012;32:1071–1074. [PubMed] [Google Scholar]
- 44. Arvidsdotter T, Marklund B, Taft C. Six‐month effects of integrative treatment, therapeutic acupuncture and conventional treatment in alleviating psychological distress in primary care patients–follow up from an open, pragmatic randomized controlled trial. BMC Complement Altern Med 2014;14:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhang ZJ, Ng R, Man SC, et al. Dense cranial electroacupuncture stimulation for major depressive disorder–a single‐blind, randomized, controlled study. PLoS ONE 2012;7:e29651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bonnet AM, Jutras MF, Czernecki V, Corvol JC, Vidailhet M. Nonmotor symptoms in Parkinson's disease in 2012: Relevant clinical aspects. Parkinsons Dis 2012;2012:198316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chaudhuri KR, Logishetty K. Dopamine receptor agonists and sleep disturbances in Parkinson's disease. Parkinsonism Relat Disord 2009;15(Suppl 4):S101–S104. [DOI] [PubMed] [Google Scholar]
- 48. Liang X, Chen F. The effects of the Seven Acupoints of the Cranial Base on health related quality of life for patients with Parkinson's disease: A randomized controlled trial. Int J Trad Chin Med 2014;36:613–616. [Google Scholar]
- 49. Lee SY, Baek YH, Park SU, et al. Intradermal acupuncture on shen‐men and nei‐kuan acupoints improves insomnia in stroke patients by reducing the sympathetic nervous activity: A randomized clinical trial. Am J Chinese Med 2009;37:1013–1021. [DOI] [PubMed] [Google Scholar]
- 50. Zhou YL, Gao XY, Wang PY, Ren S. Effect of acupuncture at different acupoints on expression of hypothalamic GABA and GABA(A) receptor proteins in insomnia rats. Zhen Ci Yan Jiu 2012;37:302–307. [PubMed] [Google Scholar]
- 51. Zhao K. Acupuncture for the treatment of insomnia. Int Rev Neurobiol 2013;111:217–234. [DOI] [PubMed] [Google Scholar]
- 52. Pfeiffer RF. Gastrointestinal dysfunction in Parkinson's disease. Parkinsonism Relat Disord 2011;17:10–15. [DOI] [PubMed] [Google Scholar]
- 53. Edwards L, Pfeiffer RF, Quigley EMM, Hofman R, Baluff M. Gastrointestinal symptoms in Parkinson's disease. Mov Disord 1991;6:151–156. [DOI] [PubMed] [Google Scholar]
- 54. Abbott RD, Ross GW, Petrovitch H, et al. Bowel movement frequency in late‐life and incidental Lewy bodies. Mov Disord 2007;22:1581–1586. [DOI] [PubMed] [Google Scholar]
- 55. Takahashi T. Mechanism of acupuncture on neuromodulation in the gut–a review. Neuromodulation 2011;14:8–12. [DOI] [PubMed] [Google Scholar]
- 56. MacPherson H, Tilbrook H, Bland JM, et al. Acupuncture for irritable bowel syndrome: Primary care based pragmatic randomised controlled trial. BMC Gastroenterol 2012;24:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lima FA, Ferreira LE, Pace FH. Acupuncture effectiveness as a complementary therapy in functional dyspepsia patients. Arq Gastroenterol 2013;50:202–207. [DOI] [PubMed] [Google Scholar]
- 58. Wu JN, Zhang BY, Zhu WZ, Du RS, Liu ZS. Comparison of efficacy on functional constipation treated with electroacupuncture of different acupoint prescriptions: A randomized controlled pilot trial. Zhongguo Zhen Jiu 2014;34:521–528. [PubMed] [Google Scholar]
- 59. Sakakibara R, Uchiyama T, Yamanishi T, Shirai K, Hattori T. Bladder and bowel dysfunction in Parkinson's disease. J Neural Transm 2008;115:443–460. [DOI] [PubMed] [Google Scholar]
- 60. Hotta H, Uchida S. Aging of the autonomic nervous system and possible improvements in autonomic activity using somatic afferent stimulation. Geriatr Gerontol Int 2010;10(Suppl 1):S127–S136. [DOI] [PubMed] [Google Scholar]
- 61. Liu Z, Wang W, Wu J, Zhou K, Liu B. Electroacupuncture improves bladder and bowel function in patients with traumatic spinal cord injury: Results from a prospective observational study. Evid Based Complement Alternat Med 2013;2013:543174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Li P, Tjen‐A‐Looi SC, Cheng L, et al. Long‐lasting reduction of blood pressure by electroacupuncture in patients with hypertension: Randomized controlled trial. Med Acupunct 2015;27:253–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Longhurst JC, Tjen‐A‐Looi S. Acupuncture regulation of blood pressure: Two decades of research. Int Rev Neurobiol 2013;111:257–271. [DOI] [PubMed] [Google Scholar]
- 64. Lee MS, Shin BC, Kong JC, Ernst E. Effectiveness of acupuncture for Parkinson's disease: A systematic review. Mov Disord 2008;23:1505–1515. [DOI] [PubMed] [Google Scholar]
- 65. Golub RM, Fontanarosa PB. Comparative effectiveness research: Relative successes. JAMA 2012;307:1643–1645. [DOI] [PubMed] [Google Scholar]
- 66. Na BJ, Jahng GH, Park SU, et al. An fMRI study of neuronal specificity of an acupoint: Electroacupuncture stimulation of Yanglingquan (GB34) and its sham point. Neurosci Lett 2009;464:1–5. [DOI] [PubMed] [Google Scholar]


