Summary
Objective
To assess the management of low‐density lipoprotein cholesterol (LDL‐C) in patients suffering from ischemic stroke within 6–12 months and explore the predictors of the achievement of LDL‐C target.
Methods
This study was a nation‐wide, multicenter, cross‐sectional study conducted from July 2013 to August 2013 in mainland China. Patients who had an ischemic stroke within 6–12 months and were more than 18 year old were consecutively included into this study. All data referred to personal information, medical history, medication and results from laboratory tests were collected by face‐to‐face questionnaires, physical examination and blood tests. The predictors for the achievement of LDL‐C target (<1.8 mmol/L or <70 mg/dL) were analyzed by the multivariate analysis.
Results
A total of 3956 cases from 56 centers who suffered from ischemic stroke within 6–12 months were finally included into this study. The average serum level of LDL‐C in all patients was 2.42 ± 0.91 mmol/L with a median of 2.30 mmol/L and the total LDL‐C goal achievement rate was 27.4% (95% CI: 26.0%‐28.8%). Lipid‐lowering therapy (odds ratio [OR] = 3.54, 95% CI: 2.879–4.388) was the most significant predictor for LDL‐C target achievement and female (OR = 0.64, 95% CI: 0.526–0.777), current smoking (OR = 0.714, 95% CI: 0.571–0.892), and the history of dyslipidemia (OR = 0.577, 95% CI: 0.497–0.668) were other three important negative factors for the LDL‐C goal achievement.
Conclusion
Although lipid modulation is recommended as an important intervention for stroke patients in the international guidelines, the goal achievement of LDL‐C is still very low in this population in mainland China. The modifiable predictors including the use of lipid‐lowering medication and smoking cessation should be improved in secondary prevention of stroke.
Keywords: Goal achievement rate, LDL‐C, Lipid‐lowering therapy, Stroke
Introduction
Stroke is the leading cause of death worldwide and is also recognized as a leading cause of serious physical and cognitive long‐term disability in adults 1. It has an extremely high rate of recurrence and risk factor management in stroke patients has been proved to be an important intervention for secondary prevention of stroke. Just as published, a body of evidence indicated that dyslipidemia is an important risk factor for stroke and modification of low‐density lipoprotein cholesterol (LDL‐C), a primary serum lipid biomarker, is an effective treatment in the secondary stroke prevention 2. Recent studies have shown that the reduction of per 1.0 mmol/L LDL‐C could bring about a risk reduction of 16%, 21%, and 23% in all of strokes, ischemic stroke, and first nonfatal ischemic stroke, respectively 3. Results from SPARCL trial showed that achievement of LDL‐C level <70 mg/dl was related to a risk reduction of stroke recurrence by 28% 4. In secondary prevention of noncardioembolic stroke, intense reduction of LDL‐C by statins also significantly reduced the risk of recurrent stroke (relative risk, 0.84) 5. Therefore, the American Heart Association (AHA)/American Stroke Association (ASA) stroke guideline 2014 recommended that high‐intensity statins should be used to reduce the risk of stroke and cardiovascular events among patients with ischemic stroke or transient ischemic attack (TIA) and the Chinese stroke secondary guidelines (2014) recommend the LDL‐C of <1.8 mmol/L (<70 mg/dL) as the treatment goal in patients with ischemic stroke or TIA 6, 7.
Actually, more and more attention is given to the dyslipidemia management in China. A cross‐sectional study on the levels of lipid and lipoprotein in Chinese adults launched by He and colleagues 8 revealed a high proportion of subjects with an increased level of total cholesterol (TC) and LDL‐C as well as a low rate of awareness, treatment, and management in the population. The second survey of dyslipidemia management (2006) revealed an overall LDL‐C goal achievement rate of 34% after treatment 9. The goal achievement rate is decreased along with the increased risk stratification and the population at very high risk had only a rate of 22%. Results from another survey about the dyslipidemia management in the outpatient of cardiology revealed that the goal achievement rates for the populations at high risk and very high risk were 19.9% and 21%, respectively 10. Results from DYSIS‐China have shown that the rate of LDL‐C attainment of <1.8 mmol/L in patients with or without metabolic syndrome is 26.1% and 27.4%, respectively 11. However, none of these studies provide the information about LDL‐C management condition in patients with stroke.
There are more than 7 million stroke patients and almost 2.5 million residents experience an incident or recurrent stroke each year in China 12, 13. Therefore, a cross‐sectional survey about dyslipidemia management in stroke patients is needed to assess the management of LDL‐C and to explore the predictors of the achievement of LDL‐C target in patients suffering from ischemic stroke.
Methods
Study Design
This study was designed as a multicenter, cross‐sectional, observational investigation, aiming to investigate the prevalence and management condition of dyslipidemia in adults suffering from ischemic stroke within 6–12 months. This study was conducted from July 2013 to August 2013 in mainland China and a total of 56 registry hospitals representing 12 provinces and 4 municipalities had been selected as registry hospitals. Among them, there were 52 tertiary hospitals and 4 secondary urban hospitals. Patients were screened consecutively, and eligible subjects were interviewed by investigators and finished a questionnaire during the visit. Investigators collected relevant medical history, physical examination results, and laboratory test results including serum lipids.
Patient Recruitment
This was a noninterventional project which did not require any specific treatment. Patients (aged ≥18 years old) suffering from ischemic stroke within 6–12 months were consecutively recruited. The exclusion criteria were listed as follows: (a) patients with significant medical or psychological condition that incapacitates patients for finishing the questionnaire independently or with the aids of legal representatives, (b) double enrollment in the present study, (c) engagement in other clinical studies, (d) no information about serum LDL‐C level, and (e) patients’ refusal. All the written informed consent forms were obtained from patients or his proxy. All study procedures including informed consent forms were approved by the ethics committee in accordance with laws and regulations.
Data Collection
Information of all cases about medical history and physical examination was recorded. All hospitals obtained the levels of blood lipids (total cholesterol, triglycerides, LDL‐C, high‐density lipoprotein cholesterol) and glucose (glycated hemoglobin, if any) for enrolled patients by laboratory testing, respectively. The information about gender, age, history of coronary artery diseases (CAD), and other characteristics was obtained by questionnaire. Dyslipidemia was defined as LDL‐C ≥130 mg/dL, high‐density lipid (HDL) <40 mg/dL, TC≥200 mg/dL, or triglycerides (TG) ≥150 mg/dL 14. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg or receiving medications for hypertension 15. Definition of diabetes was based on self‐reported diabetes history or current hypoglycemic agent usage. LDL‐C goal achievement was defined as LDL‐C < 1.8 mmol/L (70 mg/dL) 7.
Statistical Analysis
Statistical analysis was executed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA). Continuous variables were described using mean ± SD and categorical variables were described using the percentage. The goal achievement rates were described using proportions. The odds ratio (OR) in the group was analyzed and the difference was examined using chi‐square statistics for categorical variables and one‐way analysis of variance for continuous variables. To evaluate the independent associations between the control of LDL‐C and other factors, multivariate logistic regression analysis was performed. The statistically significant differences were inferred when the P value was <0.05 and all confidence intervals were computed at the 95% level.
Results
A total of 4117 patients with ischemic stroke were consecutively recruited from 56 centers from July 2013 to August 2013. After excluding 7 cases for double enrollment in different centers and 154 cases for being without lipid data, 3956 cases were finally included into full analysis set (FAS) and 161 cases were excluded (Figure 1).
Figure 1.
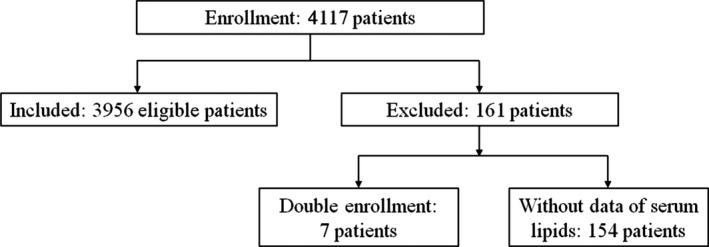
The reasons for exclusion of recruited patients.
Patient Characteristics
The characteristics of the included patients were summarized in Table 1 and were refined according to the LDL‐C goal achievement or not. The average LDL‐C level for FAS was 2.42 ± 0.91 mmol/L. For groups with or without LDL‐C goal achievement, the average LDL‐C levels were 1.42 ± 0.27 mmol/L and 2.79 ± 0.77 mmol/L, respectively. There were 2044 cases (51.7%) with a history of dyslipidemia including 2023 cases with one or more serum lipids out of range and 21 cases with a lack of detailed history. For these 2023 cases, there were 832 (41.1%) with elevated total cholesterol, 1148 (56.8%) with elevated TC, 549 (27.1%) with decreased HDL, and 948 (46.9%) with elevated LDL‐C.
Table 1.
Patients’ characteristics grouped by LDL‐C goal achievement or not
| Characteristics | Result (n, %) | |||
|---|---|---|---|---|
| Total (n = 3956) | With LDL‐C goal achievement (n = 1082) | Without LDL‐C goal achievement (n = 2874) | ||
| Gender | Male, n (%) | 2696 (68.15%) | 796 (73.57%) | 1900 (66.11%) |
| Age (year) | ≥18,≤45 | 179 (4.52%) | 58 (5.36%) | 121 (4.21%) |
| ≥46,≤65 | 1956 (49.44%) | 524 (48.43%) | 1432 (49.83%) | |
| ≥66,≤75 | 1014 (25.63%) | 266 (24.58%) | 748 (26.03%) | |
| ≥76 | 798 (20.17%) | 232 (21.44%) | 566 (19.69%) | |
| Unknown | 9 (0.23%) | 2 (0.18%) | 7 (0.24%) | |
| Race | Han | 3921 (99.12%) | 1071 (99.00%) | 2850 (99.16%) |
| Others | 35 (0.88%) | 11 (1.00%) | 24 (0.84%) | |
| Education | College and above | 392 (9.9%) | 112 (10.4%) | 280 (9.7%) |
| High school | 1047 (26.5%) | 295 (27.3%) | 752 (26.2%) | |
| Middle school | 1145 (28.9%) | 312 (28.8%) | 833 (29.0%) | |
| Primary school | 878 (22.2%) | 239 (22.1%) | 639 (22.2%) | |
| Illiteracy | 313 (7.9%) | 98 (9.1%) | 215 (7.5%) | |
| Unknown | 181 (4.6%) | 26 (2.4%) | 155 (5.4%) | |
| Smokinga | Never | 2048 (51.77%) | 548 (50.64%) | 1500 (52.19%) |
| Current | 799 (20.20%) | 330 (30.50%) | 759 (26.41%) | |
| Past | 1089 (27.53%) | 198 (18.30%) | 601 (20.91%) | |
| Unknown | 20 (0.5%) | 6 (0.55%) | 14 (0.49%) | |
| Alcohol intakeb | Yes | 950 (24.01%) | 282 (26.06%) | 668 (23.24%) |
| No | 2955 (74.7%) | 783 (72.37%) | 2172 (75.57%) | |
| Unknown | 51 (1.29%) | 17 (1.57%) | 34 (1.19%) | |
| Physical activityc | ≤1/week | 1378 (34.83%) | 380 (35.12%) | 998 (34.73%) |
| 2–3/week | 977 (24.70%) | 277 (25.60%) | 700 (24.36%) | |
| ≥3/week | 1499 (37.89%) | 386 (35.67%) | 1113 (38.73%) | |
| Unknown | 102 (2.58%) | 39 (3.60%) | 63 (2.19%) | |
| CVDd | Yes | 747 (18.88%) | 187 (17.28%) | 560 (19.49%) |
| No | 2967 (75.00%) | 837 (77.36%) | 2130 (74.11%) | |
| Unknown | 242 (6.12%) | 58 (5.36%) | 184 (6.40%) | |
| TIAd | Yes | 256 (6.47%) | 73 (6.75%) | 183 (6.37%) |
| Once | 138 (3.49%) | 36 (3.33%) | 102 (3.55%) | |
| 2 times | 48 (1.21%) | 16 (1.48%) | 32 (1.11%) | |
| ≥3 times | 70 (1.77%) | 21 (1.94%) | 49 (1.70%) | |
| No | 3612 (91.30%) | 989 (91.40%) | 2623 (91.27%) | |
| Unknown | 88 (2.22%) | 20 (1.85%) | 68 (2.37%) | |
| Carotid artery stenosis | Yes | 956 (24.17%) | 269 (24.86%) | 687 (23.90%) |
| No | 2639 (66.71%) | 747 (69.04%) | 1892 (65.83%) | |
| Unknown | 361 (9.13%) | 66 (6.10%) | 295 (10.26%) | |
| CADd | Yes | 786 (19.87%) | 198 (18.30%) | 588 (20.46%) |
| No | 3071 (77.63%) | 866 (80.04%) | 2205 (76.72%) | |
| Unknown | 99 (2.50%) | 18 (1.66%) | 81 (2.82%) | |
| Hypertension | Yes | 3058 (77.30%) | 851 (78.65%) | 2207 (76.79%) |
| No | 881 (22.27%) | 230 (21.26%) | 651 (22.65%) | |
| Unknown | 17 (0.43%) | 1 (0.09%) | 16 (0.56%) | |
| Diabetes | Yes | 1210 (30.59%) | 346 (31.98%) | 864 (30.06%) |
| No | 2729 (68.98%) | 732 (67.65%) | 1997 (69.49%) | |
| Unknown | 17 (0.43%) | 4 (0.37%) | 13 (0.45%) | |
| Dyslipidemia | Yes | 2044 (51.67%) | 472 (43.62%) | 1572 (54.70%) |
| No | 1911 (48.31%) | 610 (56.38%) | 1301 (45.27%) | |
| Unknown | 1 (0.03%) | 0 (0.00%) | 1 (0.03%) | |
| Type of stroke | Cerebral infarction | 3955 (99.97%) | 1082 (100%) | 2873 (72.62%) |
| Intracerebral hemorrhage | 83 (2.10%) | 29 (2.68%) | 54 (1.37%) | |
| Subarachnoid brain hemorrhage | 1 (0.03%) | 0 (0.00%) | 1 (0.03%) | |
| Time from stroke onset | n (missing) | 3956 (0) | 1082 (0) | 2874 (0) |
| Mean ± SD (day) | 275.1 ± 55.5 | 269.62 ± 55.77 | 277.15 ± 55.27 | |
| Median (min, max) | 274 (182, 366) | 265.00 (183, 366) | 278.00 (182, 366) | |
| Lipid‐lowering drugs | Statins | 3072 (77.65%) | 967 (89.37%) | 2105 (73.24%) |
| Fibrates | 25 (0.63%) | 6 (0.55%) | 19 (0.66%) | |
| Cholesterol absorption inhibitor | 24 (0.61%) | 8 (0.74%) | 16 (0.56%) | |
| Nicotinic acid and its derivatives | 1 (0.03%) | 0 (0.00%) | 1 (0.03%) | |
| Others | 79 (2.00%) | 14 (1.29%) | 65 (1.26%) | |
| Anticoagulant | Yes | 203 (5.1%) | 77 (7.1%) | 126 (4.4%) |
| No | 3753 (94.9%) | 1005 (92.9%) | 2748 (95.6%) | |
| Antihypertension | Yes | 2691 (68.0%) | 756 (69.9%) | 1935 (67.3%) |
| No | 1265 (32.08%) | 326 (30.1%) | 939 (32.7%) | |
| Antidiabetes | Yes | 1048 (26.5%) | 303 (28.0%) | 745 (25.9%) |
| No | 2908 (73.5%) | 779 (72.0%) | 2129 (74.1%) | |
| Medication compliance | Never missed | 2389 (60.39%) | 796 (73.56%) | 1593 (55.43%) |
| Rarely (missed ≤once/week) | 459 (11.60%) | 137 (12.66%) | 322 (11.20%) | |
| Occasionally (missed 2–3 times/week) | 151 (3.82%) | 17 (1.57%) | 133 (4.63%) | |
| Frequently (missed≥ 4 times/week) | 150 (3.79%) | 28 (2.59%) | 123 (4.28%) | |
| LDL‐C | 2.42 ± 0.91 mmol/L | 1.42 ± 0.27 mmol/L | 2.79 ± 0.77 mmol/L | |
Smoking at least one cigarette per day with a total duration of at least 6 months.
Drinking (white wine, red wine, millet wine, or beer) at 3 drinks per week with a total duration of at least 6 months.
30 min or more each time.
Abbreviations: CAD, coronary artery disease; TIA, transient ischemic attack; CAD, coronary artery disease.
The Lipid‐Lowering Therapy
In all of 3956 cases, 3149 (79.6%) received the therapy of lipid‐lowering drugs. Among them, 97.6% (3072 cases) used statins for the lipid‐lowering drugs and the average doses for statins are shown in Table 2. For patients with lipid‐lowering therapy, approximately 75.9% of them (2389 cases) were with strict medication compliance. The reasons for missed doses included forgetting (42.2%), fearing of side effects (14.3%), paying little attention to this therapy (24.2%), and others (20.3%). Moreover, 20.4% of them (807 cases) did not receive lipid‐lowering treatment due to several reasons as follows: no prescription (57.9%), economic considerations (5.8%), no treatment motivation (18.3%), and others (19.1%).
Table 2.
The doses of lipid‐lowering therapy and the LDL‐C goal achievement
| Drug name (main ingredient) | Mean daily (mg, mean ± SD) (%) | The number of patients | |
|---|---|---|---|
| High‐intensity statinsa | Moderate‐/low‐intensity statinsb | ||
| Pitavastatin Calcium | 2.0 ± 0.0 (0.1%) | 0 (0.0%) | 2 (100%) |
| Rosuvastatin Calcium | 9.8 ± 2.6 (31.9%) | 38 (3.9%) | 942 (96.1%) |
| Atorvastatin Calcium | 18.5 ± 4.9 (56.1%) | 29 (1.7%) | 1693 (98.3%) |
| Lovastatin | 20.5 ± 3.2 (1.3%) | 0 | 39 (100%) |
| Pravastatin Sodium | 22.3 ± 7.7 (3.6%) | 0 | 110 (100%) |
| Simvastatin | 23.7 ± 10.2 (6.5%) | 0 | 199 (100%) |
| Fluvastatin Sodium | 66.1 ± 24.0 (0.6%) | 0 | 18 (100%) |
High‐intensity statins: rosuvastatin ≥20 mg; atorvastatin 40–80 mg.
Moderate‐/low‐intensity statins: atorvastatin 10–20 mg; rosuvastatin 5–10 mg; pitavastatin 1–4 mg; lovastatin 20–40 mg; pravastatin 10–80 mg; simvastatin 10–40 mg; fluvastatin 20–80 mg.
LDL‐C Goal Attainment
In the FAS, there were 1082 patients (27.4%, 95% CI: 26.0%‐28.8%) who achieved the LDL‐C goal of 1.8 mmol/L or <70 mg/dL. The group with lipid‐lowering drugs has a goal attainment rate of 31.1% which is significantly higher than that (13.0%) in the group without lipid‐lowering drugs and the odds ratio (OR) is 3.045 (95% CI: 2.456–3.810, P < 0.0001) (Table 3).In particular, the goal attainment rate of LDL‐C in the group without missed dose is 33.7% and the OR is 3.393 (95% CI: 2.750–4.220) compared with that in the group without lipid‐lowering drugs. Other factors including smoking, dyslipidemia, and low medication compliance were shown to statistically impair the goal achievement of LDL‐C (Table 3).
Table 3.
The analysis of variables with LDL‐C goal achievement
| Number under control (Total) | Control rate | OR (95% CI) | P value | |
|---|---|---|---|---|
| Lipid‐lowering drug | ||||
| Yes | 978 (3149) | 31.1% | 3.045 (2.456, 3.810) | <.0001 |
| No (control) | 104 (807) | 12.9% | ||
| Compliance | ||||
| Frequently missed | 17 (145) | 11.7% | 0.888 (0.500, 1.490) | <.0001 |
| Occasionally missed | 28 (147) | 19.1% | 1.573 (0.982, 2.453) | |
| Rarely missed | 136 (445) | 30.6% | 2.943 (2.223, 3.903) | |
| Never | 786 (2335) | 33.7% | 3.393 (2.750, 4.220) | |
| No use (control) | 115 (884) | 13.0% | ||
| Gender | ||||
| Female | 286 (1260) | 22.7% | 0.701 (0.599, 0.818) | <.0001 |
| Male (control) | 796 (2696) | 29.5% | ||
| Age (yrs) | ||||
| ≥76 | 232 (798) | 29.1% | 0.855 (0.606, 1.217) | 0.2192 |
| ≥66, ≤75 | 266 (1014) | 26.2% | 0.742 (0.529, 1.051) | |
| ≥46, ≤65 | 524 (1956) | 26.8% | 0.763 (0.552, 1.067) | |
| ≥18, ≤45 (control) | 58 (179) | 32.4% | ||
| Smoking | ||||
| Past | 330 (1089) | 30.3% | 1.190 (1.012, 1.399) | 0.0204 |
| Current | 198 (799) | 24.8% | 0.902 (0.746, 1.087) | |
| Never (control) | 548 (2048) | 26.8% | ||
| Alcohol intake | ||||
| Yes | 282 (950) | 29.7% | 1.171 (0.996, 1.375) | 0.0552 |
| No (control) | 783 (2955) | 26.5% | ||
| Physical activity | ||||
| ≥3/week | 386 (1499) | 25.8% | 0.911 (0.772, 1.075) | 0.3145 |
| 2–3/week | 277 (977) | 28.4% | 1.039 (0.866, 1.247) | |
| ≤1/week (control) | 380 (1378) | 27.6% | ||
| CVD | ||||
| Yes | 187 (747) | 25.0% | 0.850 (0.706, 1.020) | 0.0827 |
| No (control) | 837 (2967) | 28.2% | ||
| TIA | ||||
| Yes | 73 (256) | 28.5% | 1.059 (0.795, 1.395) | 0.6911 |
| No (control) | 989 (3612) | 27.4% | ||
| Carotid artery stenosis | ||||
| Yes | 269 (956) | 28.1% | 0.992 (0.841, 1.168) | 0.9213 |
| No (control) | 747 (2639) | 28.3% | ||
| CHD | ||||
| Yes | 198 (786) | 25.2% | 0.857 (0.715, 1.024) | 0.0924 |
| No (control) | 866 (3071) | 28.2% | ||
| Hypertension | ||||
| Yes | 851 (3058) | 27.8% | 1.091 (0.922, 1.295) | 0.3130 |
| No (control) | 230 (881) | 26.1% | ||
| Diabetes | ||||
| Yes | 346 (1210) | 28.6% | 1.093 (0.939, 1.270) | 0.2499 |
| No (control) | 732 (2729) | 26.8% | ||
| Dyslipidemia | ||||
| Yes | 472 (2044) | 23.1% | 0.640 (0.556, 0.737) | <.0001 |
| No (control) | 610 (1911) | 31.9% | ||
The relationship of the goal attainment with all variables was further analyzed by multivariate logistic regression. The most significant independent determinant for achieving the treatment target was the lipid‐modifying therapy (OR = 3.540, 95% CI: 2.879–4.388). Other determinants of the LDL‐C target achievement included body mass index (BMI, OR = 0.953, 95% CI: 0.929–0.976), gender (OR = 0.640, 95% CI: 0.526–0.777), dyslipidemia (OR = 0.577, 95% CI: 0.497–0.888), and smoking status (OR = 0.714, 95% CI: 0.571–0.892). The age, hypertension, or diabetes was shown not to be associated with the LDL‐C target achievement (Figure 2).
Figure 2.
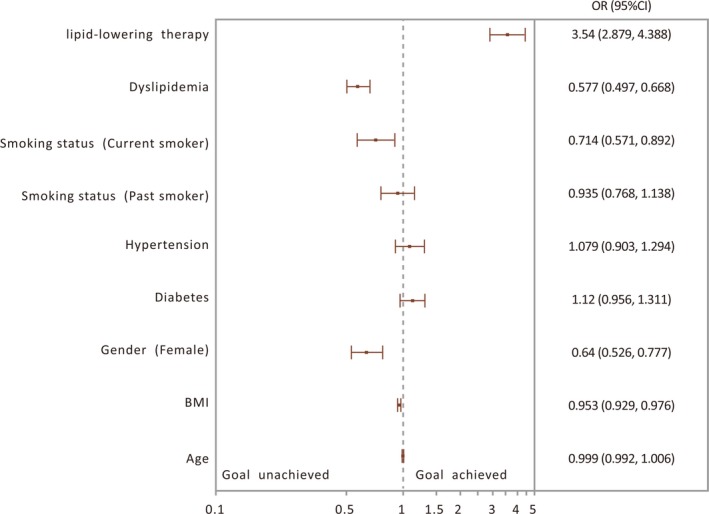
Multivariate analysis for predictors of LDL‐C goal achievement.
Discussion
In this study, we performed a national survey of the LDL‐C management in stroke patients by a large‐scale investigation in China and reveal a low goal achievement rate of LDL‐C in stroke patients as well as the predictors of LDL‐C goal achievement. In fact, previous studies demonstrated that up to 80% of recurrent stroke may be prevented by the intervention of the modifiable risk factors such as dyslipidemia, which mostly attributes to the better recognition, treatment options, and secondary prevention in addition to changes in lifestyles 1, 6, 16. Therefore, our results will help the improvement of the LDL‐C management for the secondary prevention of stroke.
Currently, lowering LDL‐C remains the primary target of lipid‐modifying therapy and the LDL‐C goal achievement can reduce the risk of stroke recurrence. Previous studies show that patients with a history of ischemic stroke or TIA could benefit from lipid‐lowering therapy 17. Our results indicate that the use of lipid‐modifying agents is independently associated with and a robust predictor of LDL‐C goal achievement. In this study, there are 79.6% of poststroke cases with the use of lipid‐lowering drugs and only 27.4% achieved the goal achievement. There might attributes to several patient‐ and physician‐associated factors. There was 20.4% of stroke patients without lipid‐lowering therapy and 57.9% of those did not receive prescription. Also, 19.2% of stroke patients did not have a rigorous medication adherence. In fact, the LDL‐C goal of 1.8 mmol/L is considered to be difficult to achieve, which might require a single maximal dose or a combination regimen of lipid‐lowering agents 18, 19. In this study, the median daily doses of atorvastatin and rosuvastatin, two major statins used in stroke patients, were 20 mg and 10 mg, respectively, which are lower than those used in Western clinical outcome studies. Therefore, the improvement of the awareness of dyslipidemia, appropriate statin dosing, and medication adherence for stroke patients and the education about the latest lipid guidelines for physicians will obtain a high LDL‐C goal achievement rate to reduce stroke recurrence rate.
The variables were also analyzed by the multivariate analysis for predictors of LDL‐C goal attainment and these predictors included BMI, dyslipidemia, smoking status, and gender. Our results showed that BMI is an independent determinant for achieving LDL‐C goal attainment. In fact, previous epidemiologic studies have demonstrated a direct correlation between increasing BMI and elevated LDL‐C 20. Also, the goal achievement in patients with dyslipidemia is lower than in those without dyslipidemia. Although smoking has not been shown to directly impact of LDL‐C level, it appears to have an independent association with goal achievement in this study and has been shown to be an independent stroke risk factor 21, 22. It is possible that current smokers might attach little importance to lipid‐lowering therapy and therefore had low medication compliance. Our previous studies showed that female patients had a lower medication compliance rate than that of the male 23. Additionally, male gender is shown to be associated with an increased goal achievement, which is consistent with previous studies that show that females are less likely to achieve goal LDL than males 24, 25. The lower medication compliance rate in female patients might result in a lower goal achievement rate since medication compliance is important for the achievement of LDL‐C goal. Therefore, smoking cessation should be encouraged and intensive lipid treatment for females should be boosted for the attainment of the lipid treatment target in clinical practice.
However, the improvement of the LDL‐C goal achievement is a challenge for stroke patients to reduce the stroke recurrence in China. Over the last decade in China, there is an increasing prevalence of dyslipidemia. Results from a recent systemic analysis have demonstrated a total dyslipidemia prevalence of 41.9% in China 26. Also, there is an increasing stroke incidence as well as a high recurrence rate of stroke in China 27. Results from the Chinese National Stroke Registry showed a recurrence rate of 16% in patients with ischemic stroke in the first year 28. According to European Society of Cardiology ESC/European Atherosclerosis Society (EAS) guidelines for the management of dyslipidemia (2011) and the Chinese dyslipidemia management guidelines for adults, patients with ischemic stroke are considered subjects at a high or very high risk. Our results also revealed a high proportion of dyslipidemia (51.6%) in stroke patients, which is consistent with previous reports that patients with dyslipidemia have a high risk for stroke. Although lipid‐lowering therapies are effective at reducing LDL‐C level, our results indicate a low LDL‐C goal attainment rate (27.4%) in stroke patients, which highlights a gap between recommendations and clinical practice. Therefore, the development of a practical LDL‐C manage strategy is still required for the secondary prevention of stroke.
However, there are still several limitations that should be addressed. First, it was an observational cross‐sectional trial that did not assess long‐term outcomes. A prospective follow‐up study is required to evaluate medical treatment and LDL‐C goal attainment in relation to stroke recurrence in patients treated with lipid‐lowering agents. Second, lipid parameters were not measured in a central core laboratory and were obtained from direct medical records. Third, there were only 4 secondary urban hospitals as registry hospitals in this study, and therefore, the LDL‐C goal achievement rate might not represent the actual one in rural area. The LDL‐C goal achievement rate in rural area might be much lower than that obtained in this study.
In conclusion, there is a low percentage of the LDL‐C goal attainment in stroke patients and improvement of the LDL‐C goal achievement is still an important task for secondary prevention of stroke in China. More effort should be put into enhancing the awareness of lipid‐lowering therapy and the lifestyle changes in stroke patients. The emphasis of guideline adherence for stroke patients and physicians will help to promote dyslipidemia management.
Conflicts of Interest
The authors declare that we have no conflict of interests.
Acknowledgments
This study was funded by the Ministry of Science and Technology of China (2011BAI08B02, 2013BAI09B03, 2015BAI12B04) and funded by Astra Zeneca.
References
- 1. Kuklina EV, Tong X, George MG, Bansil P. Epidemiology and prevention of stroke: A worldwide perspective. Expert Rev Neurother 2012;12:199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tziomalos K, Athyros VG, Karagiannis A, Mikhailidis DP. Dyslipidemia as a risk factor for ischemic stroke. Curr Top Med Chem 2009;9:1291–1297. [DOI] [PubMed] [Google Scholar]
- 3. Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta‐analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Amarenco P, Goldstein LB, Szarek M, et al. Effects of intense low‐density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke 2007;38:3198–3204. [DOI] [PubMed] [Google Scholar]
- 5. Amarenco P, Labreuche J. Lipid management in the prevention of stroke: Review and updated meta‐analysis of statins for stroke prevention. Lancet Neurol 2009; 8: 453–463.6. [DOI] [PubMed] [Google Scholar]
- 6. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:2160–2236. [DOI] [PubMed] [Google Scholar]
- 7. Wang Y, Wang C, Miu Z, et al. Chinese guidelines for the secondary prevention of stroke in patients with stroke and transient ischemic attack. Chin J Neurol 2014;48:258–273. [Google Scholar]
- 8. He J, Gu D, Reynolds K, et al. Serum total and lipoprotein cholesterol levels and awareness, treatment, and control of hypercholesterolemia in China. Circulation 2004;110:405–411. [DOI] [PubMed] [Google Scholar]
- 9. Wu YF. The second multi‐center survey of dyslipidemia management in China: Goal attainment rate and related factors. Zhonghua xin xue guan bing za zhi 2007;35:420–427. [PubMed] [Google Scholar]
- 10. Gao F, Zhou YJ, Hu DA, et al. Contemporary management and attainment of cholesterol targets for patients with dyslipidemia in China. PLoS ONE 2013;8:e47681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang F, Ye P, Hu D, et al. Lipid‐lowering therapy and lipid goal attainment in patients with metabolic syndrome in China: Subgroup analysis of the Dyslipidemia International Study‐China (DYSIS‐China). Atherosclerosis 2014;237:99–105. [DOI] [PubMed] [Google Scholar]
- 12. Mi D, Jia Q, Zheng H, et al. Metabolic syndrome and stroke recurrence in Chinese ischemic stroke patients–the ACROSS‐China study. PLoS ONE 2012;7:e51406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu X, Zhu B, Fu L, et al. Prevalence, incidence, and mortality of stroke in the chinese island populations: A systematic review. PLoS ONE 2013;8:e78629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults , et al. Zhonghua xin xue guan bing za zhi 2007;35:390–419. [PubMed] [Google Scholar]
- 15. Wang J, Zhang L, Wang F, Liu L, Wang H, China National Survey of Chronic Kidney Disease Working Group . Prevalence, awareness, treatment, and control of hypertension in China: Results from a national survey. Am J Hypertens 2014;27:1355–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): A prospective population‐based sequential comparison. Lancet 2007;370:1432–1442. [DOI] [PubMed] [Google Scholar]
- 17. Stroke Council Stroke Council, American Heart Association, American Stroke Association . Statins after ischemic stroke and transient ischemic attack: An advisory statement from the Stroke Council, American Heart Association and American Stroke Association. Stroke 2004;35:1023. [DOI] [PubMed] [Google Scholar]
- 18. Kennedy AG, MacLean CD, Littenberg B, Ades PA, Pinckney RG. The challenge of achieving national cholesterol goals in patients with diabetes. Diabetes Care 2005;28:1029–1034. [DOI] [PubMed] [Google Scholar]
- 19. Maron DJ, Hartigan PM, Neff DR, Weintraub WS, Boden WE, Investigators CT. Impact of adding ezetimibe to statin to achieve low‐density lipoprotein cholesterol goal (from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation [COURAGE] trial). Am J Cardiol 2013;111:1557–1562. [DOI] [PubMed] [Google Scholar]
- 20. Shirasawa T, Ochiai H, Ohtsu T, Nishimura R, et al. LDL‐cholesterol and body mass index among Japanese schoolchildren: A population‐based cross‐sectional study. Lipids Health Dis 2013;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bhat VM, Cole JW, Sorkin JD, et al. Dose‐response relationship between cigarette smoking and risk of ischemic stroke in young women. Stroke 2008;39:2439–2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ho LT, Yin WH, Chuang SY, et al. Determinants for achieving the LDL‐C target of lipid control for secondary prevention of cardiovascular events in Taiwan. PLoS One 2015;10:e0116513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ji R, Liu G, Shen H, et al. Persistence of secondary prevention medications after acute ischemic stroke or transient ischemic attack in Chinese population: Data from China National Stroke Registry. Neurol Res 2013;35:29–36. [DOI] [PubMed] [Google Scholar]
- 24. Reibis RK, Bestehorn K, Pittrow D, Jannowitz C, Wegscheider K, Voller H. Elevated risk profile of women in secondary prevention of coronary artery disease: A 6‐year survey of 117,913 patients. J Womens Health 2009;18:1123–1131. [DOI] [PubMed] [Google Scholar]
- 25. Singh M, Chin SH, Crothers D, Giles P, Al‐Allaf K, Khan JM. Time trends of gender‐based differences in lipid goal attainments during secondary prevention of coronary artery disease: Results of a 5‐year survey. Am J Ther 2013;20:613–617. [DOI] [PubMed] [Google Scholar]
- 26. He H, Yu YQ, Li Y, et al. Dyslipidemia awareness, treatment, control and influence factors among adults in the Jilin province in China: A cross‐sectional study. Lipids Health Dis 2014;13:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Liu L, Wang D, Wong KS, Wang Y. Stroke and stroke care in China: Huge burden, significant workload, and a national priority. Stroke 2011;42:3651–3654. [DOI] [PubMed] [Google Scholar]
- 28. Wang Y, Cui L, Ji X, et al. The China National Stroke Registry for patients with acute cerebrovascular events: Design, rationale, and baseline patient characteristics. Int J Stroke 2011;6:355–361. [DOI] [PubMed] [Google Scholar]


