Conflict of Interest
The authors declare no conflict of interest.
Although it is known that infections can increase risk of exacerbation of relapsing‐remitting multiple sclerosis (MS), some microbial products trigger a regulatory function and provide a link between microbial recognition and suppression of autoimmune diseases 1. The family of Toll‐like receptors (TLRs) has been shown to play the crucial role in developing and directing the response of DCs to microbial invasion 2. TLR‐9 is of particular interest, because it is expressed constitutively on pDCs and B lymphocytes, and its ligands, the unmethylated cytosine–phosphate–guanosine oligodeoxynucleotides (ODN‐CpG), act as very effective activators of these cells 3. pDCs and B cells may present important functions in the pathogenic and regulatory mechanisms in MS 4, 5. Recent studies have demonstrated that ODN‐CpG may also reduce the severity of some autoimmune diseases 6. The beneficial effect of the ODN‐CpG may be due to the activation of the tolerogenic properties of the pDC and B lymphocytes. In the present study, we aimed to investigate the role of pDCs and B lymphocytes in the beneficial effect of ODN‐CpG treatment in MS experimental model, experimental autoimmune encephalomyelitis (EAE). As far we know this is the first work with in vivo administration of ODN‐CpG in EAE.
Experimental autoimmune encephalomyelitis was actively induced in the C57Bl/6 mice by immunization with MOG35‐55 peptide (Appendix S1). To test whether administration of the CpG oligonucleotide can modulate the evolution of EAE, we treated mice with five consecutive subcutaneous doses (−5 to 0 days) before immunization with the MOG peptide. The CpG‐treated (5 μg/dose) mice had significantly less severe EAE than the control group (Figure 1A). The reduction of the disease was accompanied by significant reduction of specific proliferative response of encephalitogenic T lymphocytes in the lymph node (Figure 1B) and a decrease of encephalitogenic cells infiltrated in the CNS (data not shown). Very interestingly, in vitro depletion of pDCs abrogates the inhibition of the specific proliferative response, suggesting the tolerogenic effect of these cells (Figure 1B). Our results are in agreement with previous study that clearly demonstrated that TLR9 −/− C57Bl/6 mice exhibited more severe EAE symptoms than wild‐type mice, suggesting the regulatory effect of the stimulation of TLR9 7. As both pDCs and B lymphocytes present the TLR9, we investigate the activation of tolerogenic functions in these two cells population. Flow cytometry analysis demonstrated that the percentage of both pDCs and B lymphocytes did not alter with the treatment in the spleen or lymph nodes (Figure 1C and D). However, qPCR demonstrated that the expression of IDO was significantly increased in pDCs sorted from lymph nodes of ODN‐CpG‐treated animals, while the B lymphocytes express more IL‐10 in the same group (Figure 1E). Interestingly, the adoptive transfer of both pDCs (Figure 2B) and B lymphocytes (Figure 2C) significantly reduces the severity of EAE confirming that suppressive functions were activated in the two cells populations. The enhancement of IL‐10 and IDO expression, in B lymphocytes and pDCs, respectively, may trigger the conversion/expansion of regulatory T cells 8. Indeed, our results show a slightly increase of CD4+Foxp3+ T cells in the spleen and a significant increase of these cells in the lymph nodes of ODN‐CpG‐treated animals (Figure 1F and G). The increase of Foxp3 was confirmed by the expression of the Foxp3 mRNA (Figure 1H). The major mechanism of Foxp3+ regulatory T cells is the expression and release of IL‐10 and TGFβ. These cytokines can modulate the autoaggressive response during EAE evolution and other autoimmune pathologies 8, 9. The Figure 1H demonstrated that the treatment with ODN‐CpG significantly increases the expression of IL‐10 and TGFβ, which may explain the reduction of the disease with the transfer of these cells.
Figure 1.
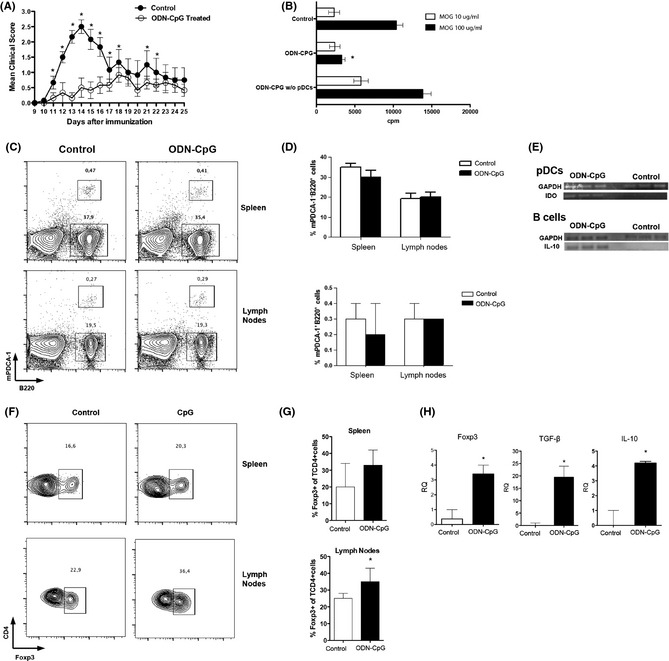
Clinical evolution of EAE in C57BL/6 mice, which were subcutaneously treated with ODN‐CpG at 5 μg/dose during 5 consecutive (−5 to 0) days (black circle). The control group (white circle) received the same dose of ODN alone during the same period (A). Specific proliferative response of T lymphocytes from lymph nodes of ODN‐CpG treated with or without pDCs and treated with ODN alone (control), and stimulated with 1 (white bars) or 10 μg/mL (black bars) of MOG35–55 peptide (B). Flow cytometry analysis of pDCs (B220+ mPDCA‐1+) and B lymphocytes (B220+ mPDCA‐1−) in spleen and lymph node from CpG‐treated (black bars) and CpG‐untreated (white bars) mice (C, representative plot; D, mean of 5 independent experiments). qPCR of IDO and IL‐10 of sorted pDCs and B cells (RQ = relative quantification) (E). Flow cytometry analysis of CD4+CD25+Foxp3+ (CD25, plot not presented; up to 95% of CD4+Foxp3+ cells) cells in spleen and lymph node from CpG‐treated (black bars) and CpG‐untreated (white bars) mice (F, representative plot; G, mean of five independent experiments). qPCR of Foxp3, IL‐10, and TGFβ of lymph nodes from CpG‐treated (black bars) and CpG‐untreated (white bars) mice (H).
Figure 2.
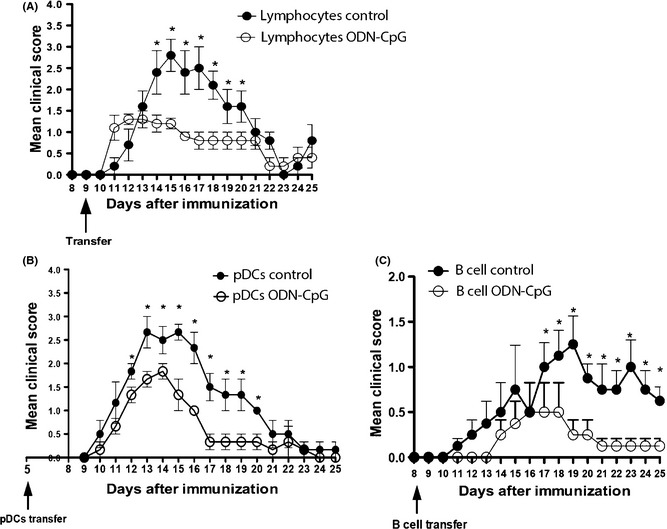
Adoptive transfer of T lymphocytes (CD3+) from CpG‐treated (white circles) and CpG‐untreated (black circles) mice, 9 days after the immunization (A). Adoptive transfer of pDCs (B220+ mPDCA‐1+) from CpG‐treated (white circles) and CpG‐untreated (black circles) mice, 5 days after the immunization (B). Adoptive transfer of B lymphocytes (B220+ mPDCA‐1−) from CpG‐treated (white circles) and CpG‐untreated (black circles) mice, 9 days after the immunization (C).
To confirm the activation of regulatory T cells by the treatment with ODN‐CpG, T lymphocytes from treated mice and control group treated, only with ODN, were transferred (9d.a.i.) to mice immunized with MOG35–55 before the onset of the disease. The Figure 2A showed that the mice that received T lymphocytes from the CpG‐treated ones developed a less severe EAE than those that received T lymphocytes from mice untreated with CpG.
In the EAE model, after successful T cell priming, autoaggressive lymphocytes subsequently migrate into the CNS causing tissue damage 10. The normal immune responses depend on appropriate levels of immunosuppression. In pathological situation such as in autoimmune disease, the immunosuppression is essential to return the inflammatory response to normal levels. Here, we demonstrated that pDCS and B lymphocytes acquire a tolerogenic profile upon the administration of an agonist of TLR 9, ODN‐CpG, which significantly reduces the severity of EAE. The enhancement of immunomodulatory molecules, such as IDO, IL‐10, and TGFβ, contributes to build a tolerogenic environment in the peripheral immune organs. This tolerogenic environment favors the conversion/expansion of regulatory T cells. Foxp3+ regulatory T cells also release IL‐10 and TGFβ, which will contribute to maintain the tolerogenic environment.
Taken together, we demonstrated that the activation of a tolerogenic profile of pDCs and B lymphocytes via TLR9 by ODN‐CpG resulted in increase of immunosuppressive mechanisms, which lead to a significant reduction of EAE.
Supporting information
Appendix S1. Methods.
Acknowledgment
This work was supported by grants from FAPESP (#2011/18728‐5; 2012/04565‐0).
References
- 1. Farias AS, Talaisys RL, Blanco YC, et al. Regulatory T cell induction during Plasmodium chabaudi infection modifies the clinical course of experimental autoimmune encephalomyelitis. PLoS ONE 2011;6:e17849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhang Z, Wang FS. Plasmacytoid dendritic cells act as the most competent cell type in linking antiviral innate and adaptive immune responses. Cell Mol Immunol 2005;2:411–417. [PubMed] [Google Scholar]
- 3. Moseman EA, Liang X, Dawson AJ, et al. Human plasmacytoid dendritic cells activated by CpG oligodeoxynucleotides induce the generation of CD4+CD25+ regulatory T cells. J Immunol 2004;173:4433–4442. [DOI] [PubMed] [Google Scholar]
- 4. Longhini AL, von Glehn F, Brandão CO, et al. Plasmacytoid dendritic cells are increased in cerebrospinal fluid of untreated patients during multiple sclerosis relapse. J Neuroinflammation 2011;8:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Franciotta D, Salvetti M, Lolli F, Serafini B, Aloisi F. B cells and multiple sclerosis. Lancet Neurol 2008;7:852–858. [DOI] [PubMed] [Google Scholar]
- 6. Lobell A, Weissert R, Eltayeb S, et al. Presence of CpG DNA and the local cytokine milieu determine the efficacy of suppressive DNA vaccination in experimental autoimmune encephalomyelitis. J Immun 1999;163:4754–4762. [PubMed] [Google Scholar]
- 7. Bettelli E, Das MP, Howard ED, et al. IL‐10 is critical in the regulation of autoimmune encephalomyelitis as demonstrated by studies of IL‐10‐ and IL‐4‐deficient and transgenic mice. J Immunol 1998;161:3299–3306. [PubMed] [Google Scholar]
- 8. Farias AS, Spagnol GS, Bordeaux‐rego P, et al. Vitamin D3 induces IDO+ tolerogenic DCs and enhances treg, reducing the severity of EAE. CNS Neurosci Ther 2013;19:269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pradella F, Moraes AS, Santos M, et al. Granulocyte–colony‐stimulating factor treatment enhances Foxp3+ T lymphocytes and modifies the proinflammatory response in experimental autoimmune neuritis. CNS Neurosci Ther 2013;19:529–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bartholomäus I, Kawakami N, Odoardi F, et al. Effector T cell interactions with meningeal vascular structures in nascent autoimmune CNS lesions. Nature 2009;462:94–98. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Methods.


