ABSTRACT
Influenza is a leading cause of respiratory tract infections worldwide and there is limited information on the impact of the influenza A(H1N1)pdm virus on mortality after the 2009 pandemic. Using national mortality register data through 1998–2015 in Mexico, influenza-associated mortality was estimated for respiratory, cardiovascular, and all-cause events. The proportion of influenza-associated respiratory and cardiovascular deaths among different age groups were compared. There were 8,853,986 death registries included for the 1998–2015 winter seasons, average influenza-associated respiratory, cardiovascular, and all-cause mortality rates were 5.2, 6.3, and 19.6 deaths/100,000 population, respectively. The largest number of respiratory influenza-associated deaths occurred in adults 60 years of age and older, followed by children <5 years of age; during the 2009 pandemic, 2011–2012, and 2013–2014 winter seasons there was a larger number of deaths in the 20–59 years old group. Influenza-associated mortality rates showed a continuous reduction in children <5 years of age. After the 2009 pandemic, influenza A(H1N1)pdm09 virus-associated mortality in Mexico showed a persistent change in the demographic pattern of the most severely affected population, particularly during the 2013–2014 season. Influenza associated-mortality has decreased in children <5 years of age and continue to be elevated in adults >60 years of age.
KEYWORDS: Influenza, mortality, pandemic, influenza A(H1N1)pdm09, respiratory infections, pneumonia
Introduction
Starting in April 2009, a novel influenza A H1N1 virus caused human infection and severe respiratory disease around the world [1,2]. Mexico was one of the countries where widespread of this infection, and severe acute respiratory infections (SARI) were reported [3,4]. Mortality in Mexico during the pandemic was higher compared to other countries [5]. Historically, after the emergence of pandemic influenza viruses, subsequent post-pandemic waves have been observed; for example, two post-pandemic waves occurred during the five years that followed the 1957 influenza A(H2N2) pandemic [6]. To better understand the impact of the 2009 pandemic, assessment of influenza-associated mortality during the years following the pandemic is required. In Mexico, after the 2009 pandemic period, an additional pandemic wave was observed during the 2013–2014 winter season; during that year an increase in hospitalizations caused by influenza A(H1N1)pdm09 was observed, but country-wide estimates of influenza-associated mortality have not been reported [7–10]. The impact of influenza on mortality is difficult to establish if only reports of pneumonia and influenza are relied on, because influenza is not suspected or influenza testing is not carried out in many patients [5,11]. In order to evaluate the impact of pandemic and post-pandemic waves, age and cause-specific excess mortality are useful parameters that reflect the burden of and changes in age groups most severely affected by pandemic viruses. The aims of this study were to analyze excess respiratory, cardiovascular, and all-cause mortality rates by age groups before, during, and after the pandemic period (1998 through 2015) in Mexico.
Material and methods
In this study, we used national mortality data available at the General Direction of Health Information website (Ministry of Health, Mexico) for the period between 1998 and 2015 (General Mortality Datbases) [12]. The number of deaths that occurred during each epidemiological week were obtained by analysis of mortality registers and analyzed for different age groups (0–<5 years, 5–19 years, 20–59 years, 60 and more years, and all ages). In addition, separate analyses were carried out for all-cause deaths (all ICD-10 codes), and cause-specific respiratory (J00-J99 ICD-10 codes) and cardiovascular (I00-I99 ICD-10 codes) deaths. Information on the Mexican population by year and age group was obtained from data generated by the Consejo Nacional de Población (CONAPO) [13]. Time series for weekly mortality rates were elaborated for each age group, and for each mortality cause (respiratory, cardiovascular, and all-cause).
Influenza-attributable mortality was calculated for each winter season, which included the period between week 27 of a given year and week 26 of the following year (starting in 1998 and ending in 2015). The only exception was the 2008–2009 and 2009–2010 (pandemic) seasons which were shorter (2008–2009) and longer (2009–2010), due to the appearance of the influenza A(H1N1)pdm09 virus in April 2009. As such, the 2008–2009 season included only 40 weeks (ending on week 13 of 2009), and the 2009–2010 season included 65 weeks (starting on week 14 of 2009 and ending on week 26 of 2010). Mortality attributed to influenza was estimated using Serfling cyclical regression models, as previously described [14,15]. Baseline mortality was established through analysis of the periods without influenza activity using regression methods to establish α, β1, β2, β3 for the following equation Y = α + β1t + β2 sin(2πt/52.14) + β3 cos(2πt/52.14) + ε and the weekly recorded death numbers. Influenza epidemic periods were defined based on pneumonia and influenza mortality (J09-J18 ICD-10 codes) for the Mexican population. The onset of the epidemic period was defined as the first of three consecutive weeks in which pneumonia and influenza mortality was greater than the upper 95% confidence limit of the mean mortality for the winter season, and the end of the epidemic period was defined as the last week when pneumonia and influenza mortality was above the upper 95% confidence limit of the mean which was followed by three consecutive weeks with mortality lower than the 95% confidence limit, as previously described [11].
Excess mortality was calculated as the observed minus predicted mortality rates during the weeks included in each influenza epidemic period. The number of influenza-attributable deaths for each season was calculated based on the excess mortality rate and the Mexican population at the beginning of each year (mid-point for each season). These calculations were carried out for each age group, and for every mortality cause of death (all-cause, respiratory, and cardiovascular).
To assess the predominant influenza strains during a particular season, data available from FluNet was used. The total number of influenza detections during a winter season was recorded, as well as the number of influenza A and B viruses, to determine which type predominated during a particular season. In addition, the number of influenza A(H1N1), (H3N2), and (H1N1)pdm09 viruses detected were also registered to define the predominant influenza A subtype for each season.
Results
There were 8,853,986 death registries included in the study period (average 520,823 deaths per season); overall, cardiovascular deaths accounted for 2,074,869 (23.4%) deaths, while there were 762,334 (8.6%) deaths due to respiratory causes. The number of all-cause, respiratory, and cardiovascular deaths (and death rates) for each season are shown in Table 1. Over the study period, there was an increase in the number of deaths. This is a result of an increase in the total population in Mexico (from a total population of 99,017,196 in 1999 to 120,285,088 in 2015), as well as due to aging of the country’s population: in 1999, persons 20 years of age and older comprised 55.3% of the country’s population, while in 2015 this age group accounted for 62.9% of the population.
Table 1.
Respiratory, cardiovascular, and all-cause mortality and mortality rates in Mexico between epidemiological week 27 of 1998 and epidemiological week 26 of 2015.
| Season | Respiratory mortality | Respiratory mortality rate | Cardiovascular mortality | Cardiovascular mortality rate | All-cause mortality | All-cause mortality rate |
|---|---|---|---|---|---|---|
| 1998–1999 | 40,354 | 40.8 | 96,374 | 97.3 | 435,722 | 440.0 |
| 1999–2000 | 40,176 | 40.1 | 97,804 | 97.6 | 436,282 | 435.2 |
| 2000–2001 | 35,798 | 35.3 | 97,221 | 95.8 | 431,631 | 425.4 |
| 2001–2002 | 39,647 | 38.6 | 102,154 | 99.4 | 451,453 | 439.5 |
| 2002–2003 | 37,461 | 36.0 | 104,287 | 100.3 | 457,194 | 439.6 |
| 2003–2004 | 42,286 | 40.2 | 108,466 | 103.0 | 472,434 | 448.8 |
| 2004–2005 | 40,543 | 38.1 | 107,904 | 101.3 | 475,680 | 446.6 |
| 2005–2006 | 42,480 | 39.4 | 111,198 | 103.2 | 490,048 | 454.7 |
| 2006–2007 | 42,982 | 39.4 | 116,627 | 106.9 | 503,261 | 461.2 |
| 2007–2008 | 44,678 | 40.4 | 121,961 | 110.3 | 527,821 | 477.5 |
| 2008–2009* | 35,232 | 31.5 | 98,356 | 87.8 | 419,522 | 374.6 |
| Pandemic** | 61,899 | 54.6 | 167,658 | 147.8 | 708,768 | 624.7 |
| 2010–2011 | 50,993 | 44.4 | 141,070 | 122.8 | 590,968 | 514.4 |
| 2011–2012 | 46,306 | 39.8 | 140,395 | 120.7 | 584,691 | 502.8 |
| 2012–2013 | 51,533 | 43.8 | 149,074 | 126.7 | 609,058 | 517.7 |
| 2013–2014 | 55,205 | 46.4 | 154,092 | 129.5 | 620,641 | 521.6 |
| 2014–2015 | 54,761 | 45.5 | 160,228 | 133.2 | 638,812 | 531.1 |
*There were only 40 weeks included in the 2008–2009 season due to the start of the 2009 influenza pandemic.
**The Pandemic period included 65 weeks due to the start of the first pandemic wave in April 2009 (week 14, 2009).
As expected, all-cause, respiratory, and cardiovascular mortality showed a seasonal pattern, with the highest mortality during the winter months, and lower mortality during the summer (Figure 1). The duration of the influenza season, excluding the pandemic period, varied from 12 to 22 weeks; the 2009 pandemic included 29 weeks with excess mortality (four during the first spring wave, and 25 during the summer-fall waves).
Figure 1.
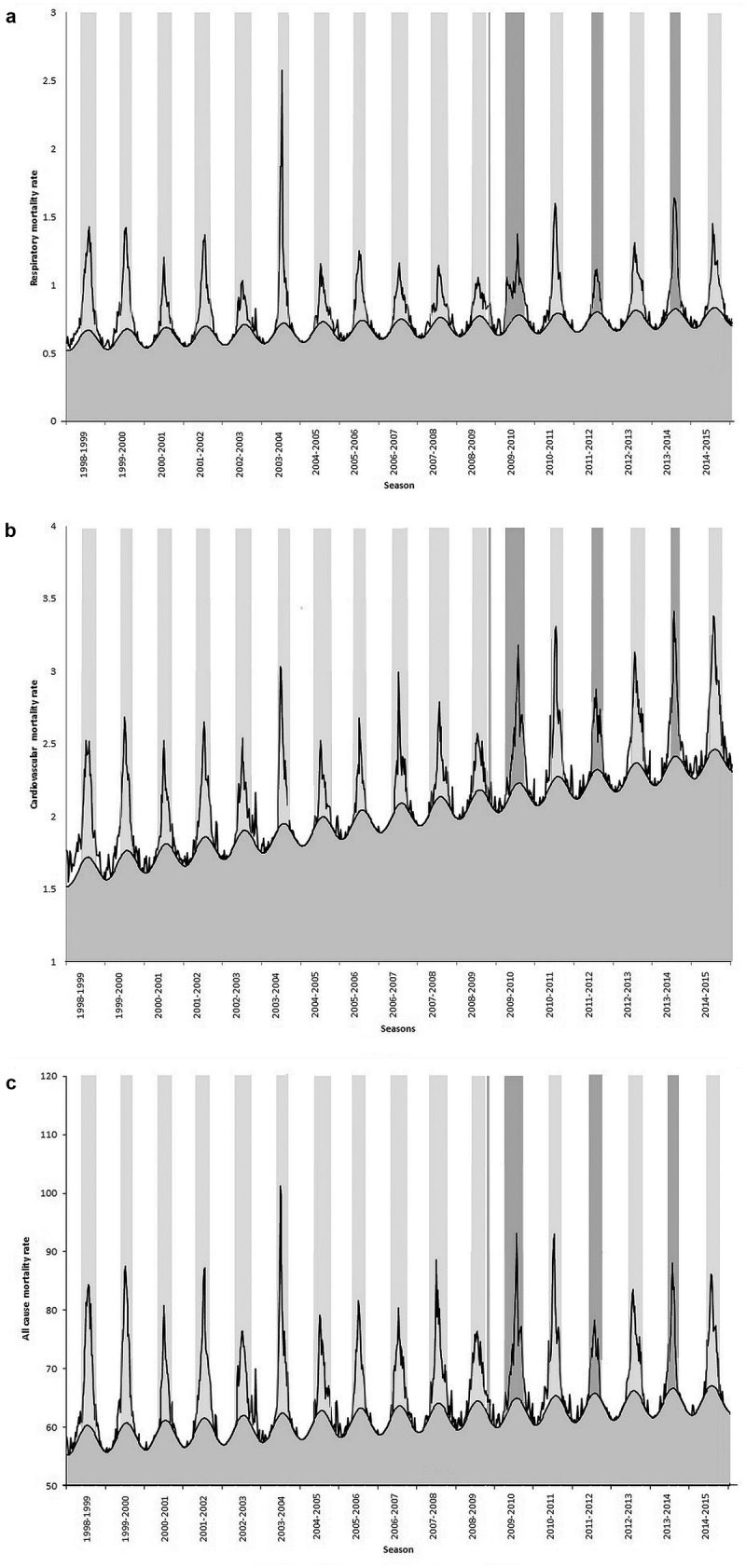
Weekly respiratory (panel A), cardiovascular (panel B), and all-cause (panel C) mortality rates in Mexico between epidemiological week 27 of 1998 and epidemiological week 26 of 2015.
Virological data was available from FluNet from the end of 1999 onward. Between the 1999–2000 and 2008–2009, influenza A(H3N2) was the predominant virus type/subtype in most seasons. Influenza A(H1N1) was the most frequently detected virus during the 2000–2001 and 2002–2003 seasons, while influenza B was the influenza virus reported most frequently during the 2004–2005 season; of note, influenza A(H3N2) was the predominant influenza A strain during that season. Between 2009 and 2014–2015 an alternating pattern was observed with influenza A(H1N1)pdm09 virus predominating during the 2009–2010, 2011–2012, and 2013–2014 seasons, and influenza A(H3N2) predominating during the 2010–2011, 2012–2013, and 2014–2015 seasons.
Influenza-attributable mortality varied widely throughout the study period (Table 2). The lowest all-cause mortality rates were observed during the 2000–2001 and 2004–2005 seasons, when the predominant influenza strains were influenza A(H1N1) and influenza B, respectively. The latter was also the season with the lowest influenza-attributable cardiovascular death rate. In contrast, the lowest influenza-attributable respiratory mortality rate was observed during the 2011–2012 season, when influenza A(H1N1)pdm09 was the predominant influenza strain.
Table 2.
Influenza-attributable respiratory, cardiovascular, and all-cause mortality and mortality rates in Mexico between epidemiological week 27 of 1998 and epidemiological week 26 of 2015.
| Season | Predominant influenza type/influenza A subtype | Respiratory influenza-associated mortality | Respiratory influenza-associated mortality rate | Cardiovascular influenza-associated mortality | Cardiovascular influenza-associated mortality rate | All-cause influenza-associated mortality | All-cause influenza-associated mortality rate |
|---|---|---|---|---|---|---|---|
| 1998–1999 | No data | 7,581.6 | 7.7 | 8,707.6 | 8.8 | 28,342.2 | 28.6 |
| 1999–2000 | No data | 6,696.6 | 6.7 | 7,805.6 | 7.8 | 24,267.4 | 24.2 |
| 2000–2001 | A/(H1N1) | 3,350.5 | 3.3 | 5,185.0 | 5.1 | 13,342.4 | 13.1 |
| 2001–2002 | A/(H3N2) | 5,734.2 | 5.6 | 6,866.8 | 6.7 | 21,546.2 | 21.0 |
| 2002–2003 | A/(H1N1) | 3,234.1 | 3.1 | 5,529.2 | 5.3 | 14,680.3 | 14.1 |
| 2003–2004 | A/(H3N2) | 8,373.6 | 8.0 | 7,268.1 | 6.9 | 24,513.7 | 23.3 |
| 2004–2005 | B/(H3N2) | 4,221.2 | 4.0 | 4,134.2 | 3.9 | 13,949.4 | 13.1 |
| 2005–2006 | A/(H3N2) | 4,897.9 | 4.5 | 4,259.0 | 4.0 | 15,793.9 | 14.7 |
| 2006–2007 | A/(H3N2) | 4,198.6 | 3.8 | 5,690.0 | 5.2 | 15,345.9 | 14.1 |
| 2007–2008 | A/(H3N2) | 4,230.4 | 3.8 | 5,694.3 | 5.2 | 21,768.9 | 19.7 |
| 2008–2009* | A/(H3N2) | 3,578.7 | 3.2 | 4,667.7 | 4.2 | 16,480.5 | 14.7 |
| Pandemic** | A/(H1N1)pdm09 | 8,842.6 | 7.8 | 10,200.2 | 9.0 | 34,771.2 | 30.6 |
| 2010–2011 | A/(H3N2) | 6,880.3 | 6.0 | 8,679.1 | 7.6 | 27,872.0 | 24.3 |
| 2011–2012 | A/(H1N1)pdm09 | 3,046.0 | 2.6 | 5,495.6 | 4.7 | 16,469.8 | 14.2 |
| 2012–2013 | A/(H3N2) | 5,568.8 | 4.7 | 8,316.3 | 7.1 | 24,553.6 | 20.9 |
| 2013–2014 | A/(H1N1)pdm09 | 7,116.5 | 6.0 | 7,760.2 | 6.5 | 23,489.3 | 19.7 |
| 2014–2015 | A/(H3N2) | 6,346.8 | 5.3 | 10,675.5 | 8.9 | 27,049.8 | 22.5 |
*There were only 40 weeks included in the 2008–2009 season due to the start of the 2009 influenza pandemic.
**The Pandemic period included 65 weeks due to the start of the first pandemic wave in April 2009 (week 14, 2009).
The season with the highest influenza-attributable respiratory death rate was the 2003–2004 season, when influenza A(H3N2) virus was the predominant strain; the 1998–1999 season and the pandemic period also showed high influenza-associated mortality rates. In addition, these two seasons were the ones with the highest influenza-attributable all-cause mortality rates.
Overall, the period between 2004 and 2009 showed lower mortality rates compared to the period encompassed between 1998 and 2004 (Supplementary Table 1). Of note, during the post-pandemic period (2010–2015) influenza mortality rates are similar to those observed between 1998 and 2004.
To better understand the impact of pandemic influenza on mortality, we analyzed the influenza-attributable respiratory and cardiovascular mortality rates in different age groups (Tables 3 and 4). While a continuous downward trend in influenza-attributable respiratory mortality was seen in children <5 years of age, this was less apparent in adults 60 years of age and older (Table 3). The 5–19 years of age group had a low mortality rate throughout the study period (0.04–0.3 respiratory deaths/100,000 population), except during the 2009 pandemic, where a significant increase was noted (0.9 respiratory deaths/100,000 population). The 20–59 years of age group also had a high respiratory mortality rate during the pandemic period (6 respiratory deaths/100,000 population) compared to the previous years (when mortality rate was usually <1 respiratory deaths/100,000 population). In addition, during the 2011–2012 and 2013–2014 winter seasons this age group also showed a significant increase in respiratory mortality (1.2 and 4.1 respiratory deaths/100,000 population, respectively).
Table 3.
Influenza-attributable respiratory mortality and mortality rates in Mexico between epidemiological week 27 of 1998 and epidemiological week 26 of 2015, according to age group.
| Season | Predominant influenza type/influenza A subtype | Influenza-attributable respiratory mortality 0–<5 years | Influenza-attributable respiratory mortality rate 0–<5 years | Influenza-attributable respiratory mortality 5–19 years | Influenza-attributable respiratory mortality rate 5–19 years | Influenza-attributable respiratory mortality 20–59 years | Influenza-attributable respiratory mortality rate 20–59 years | Influenza-attributable respiratory mortality 60 and more years | Influenza-attributable respiratory mortality rate 60 and more years |
|---|---|---|---|---|---|---|---|---|---|
| 1998–1999 | No data | 1,840 | 15.7 | 91 | 0.3 | 571 | 1.2 | 4,981 | 69.1 |
| 1999–2000 | No data | 1,293 | 11.1 | 37 | 0.1 | 560 | 1.2 | 4,767 | 64.2 |
| 2000–2001 | A/(H1N1) | 965 | 8.3 | 46 | 0.1 | 345 | 0.7 | 2,018 | 26.4 |
| 2001–2002 | A/(H3N2) | 1,127 | 9.8 | 47 | 0.1 | 374 | 0.7 | 4,216 | 53.6 |
| 2002–2003 | A/(H1N1) | 794 | 6.9 | 49 | 0.1 | 189 | 0.4 | 2,323 | 28.7 |
| 2003–2004 | A/(H3N2) | 1,296 | 11.3 | 111 | 0.3 | 655 | 1.3 | 6,403 | 76.7 |
| 2004–2005 | B/(H3N2) | 858 | 7.5 | 29 | 0.1 | 194 | 0.4 | 3,339 | 38.8 |
| 2005–2006 | A/(H3N2) | 720 | 6.4 | 28 | 0.1 | 337 | 0.6 | 3,929 | 44.3 |
| 2006–2007 | A/(H3N2) | 743 | 6.6 | 58 | 0.2 | 264 | 0.5 | 3,281 | 35.9 |
| 2007–2008 | A/(H3N2) | 581 | 5.2 | 55 | 0.2 | 466 | 0.8 | 3,276 | 34.8 |
| 2008–2009* | A/(H3N2) | 520 | 4.6 | 18 | 0.1 | 304 | 0.5 | 2,844 | 29.3 |
| Pandemic** | A/(H1N1)pdm09 | 765 | 6.8 | 309 | 0.9 | 3,535 | 6.0 | 4,349 | 43.3 |
| 2010–2011 | A/(H3N2) | 570 | 5.1 | 53 | 0.2 | 499 | 0.8 | 5,753 | 55.5 |
| 2011–2012 | A/(H1N1)pdm09 | 303 | 2.7 | 47 | 0.1 | 705 | 1.2 | 1,916 | 17.9 |
| 2012–2013 | A/(H3N2) | 472 | 4.2 | 35 | 0.1 | 344 | 0.6 | 4,506 | 40.6 |
| 2013–2014 | A/(H1N1)pdm09 | 313 | 2.8 | 59 | 0.2 | 2,587 | 4.1 | 3,907 | 34.1 |
| 2014–2015 | A/(H3N2) | 312 | 2.8 | 14 | 0.0 | 478 | 0.7 | 5,099 | 42.9 |
*There were only 40 weeks included in the 2008–2009 season due to the start of the 2009 influenza pandemic.
**The Pandemic period included 65 weeks due to the start of the first pandemic wave in April 2009 (week 14, 2009).
Table 4.
Influenza-attributable cardiovascular mortality and mortality rates in Mexico between epidemiological week 27 of 1998 and epidemiological week 26 of 2015, according to age group.
| Season | Predominant influenza type/influenza A subtype | Influenza-attributable cardiovascular mortality 0–<5 years | Influenza-attributable CV mortality rate 0–<5 years |
Influenza-attributable cardiovascular mortality 5–19 years | Influenza-attributable CV mortality rate 5–19 years |
Influenza-attributable cardiovascular mortality 20–59 years | Influenza-attributable CV mortality rate 20–59 years | Influenza-attributable cardiovascular mortality 60 and more years | Influenza-attributable CV mortality rate 60 and more years |
|---|---|---|---|---|---|---|---|---|---|
| 1998–1999 | No data | 38 | 0.32 | 51 | 0.16 | 1,094 | 2.30 | 7,212 | 100.03 |
| 1999–2000 | No data | 7 | 0.06 | 39 | 0.12 | 1,038 | 2.14 | 6,625 | 89.24 |
| 2000–2001 | A/(H1N1) | 12 | 0.11 | 23 | 0.07 | 816 | 1.65 | 4,350 | 56.91 |
| 2001–2002 | A/(H3N2) | 23 | 0.20 | 25 | 0.08 | 838 | 1.66 | 6,142 | 78.04 |
| 2002–2003 | A/(H1N1) | 9 | 0.08 | 19 | 0.06 | 757 | 1.47 | 4,995 | 61.62 |
| 2003–2004 | A/(H3N2) | 11 | 0.09 | 23 | 0.07 | 781 | 1.49 | 6,713 | 80.38 |
| 2004–2005 | B/(H3N2) | 10 | 0.08 | 31 | 0.09 | 523 | 0.98 | 4,075 | 47.37 |
| 2005–2006 | A/(H3N2) | 16 | 0.14 | 20 | 0.06 | 439 | 0.81 | 4,180 | 47.16 |
| 2006–2007 | A/(H3N2) | 13 | 0.12 | 38 | 0.11 | 675 | 1.22 | 5,438 | 59.53 |
| 2007–2008 | A/(H3N2) | 59 | 0.53 | 47 | 0.14 | 952 | 1.69 | 5,153 | 54.70 |
| 2008–2009* | A/(H3N2) | 49 | 0.43 | 41 | 0.12 | 581 | 1.01 | 4,462 | 45.91 |
| Pandemic** | A/(H1N1)pdm09 | 105 | 0.94 | 86 | 0.25 | 1,932 | 3.30 | 8,697 | 86.66 |
| 2010–2011 | A/(H3N2) | 43 | 0.39 | 33 | 0.10 | 1,052 | 1.76 | 7,726 | 74.52 |
| 2011–2012 | A/(H1N1)pdm09 | 45 | 0.40 | 21 | 0.06 | 968 | 1.59 | 4,457 | 41.59 |
| 2012–2013 | A/(H3N2) | 65 | 0.59 | 53 | 0.16 | 941 | 1.52 | 6,987 | 63.03 |
| 2013–2014 | A/(H1N1)pdm09 | 14 | 0.13 | 17 | 0.05 | 1,605 | 2.56 | 5,718 | 49.84 |
| 2014–2015 | A/(H3N2) | 16 | 0.14 | 20 | 0.06 | 1,369 | 2.15 | 8,371 | 70.48 |
*There were only 40 weeks included in the 2008–2009 season due to the start of the 2009 influenza pandemic.
**The Pandemic period included 65 weeks due to the start of the first pandemic wave in April 2009 (week 14, 2009).
The largest number of influenza-attributable respiratory deaths occurred in the 60 years and older age group. The 0–<5 years old was the group with the second largest number of respiratory deaths; however, during the 2009 pandemic, as well as during the 2011–2012 and 2013–2014, when influenza A(H1N1)09pdm virus was the predominant strain, there was a larger number of deaths in the 20–59 years old group than in children 0–<5 years of age. The proportion of influenza-attributable respiratory deaths, according to age group, is shown in Figure 2. The distinctive pattern of increased mortality in young adults can be readily appreciated, not only for the 2009 pandemic period but also for the two subsequent influenza seasons in which influenza A(H1N1)09pdm virus predominated.
Figure 2.
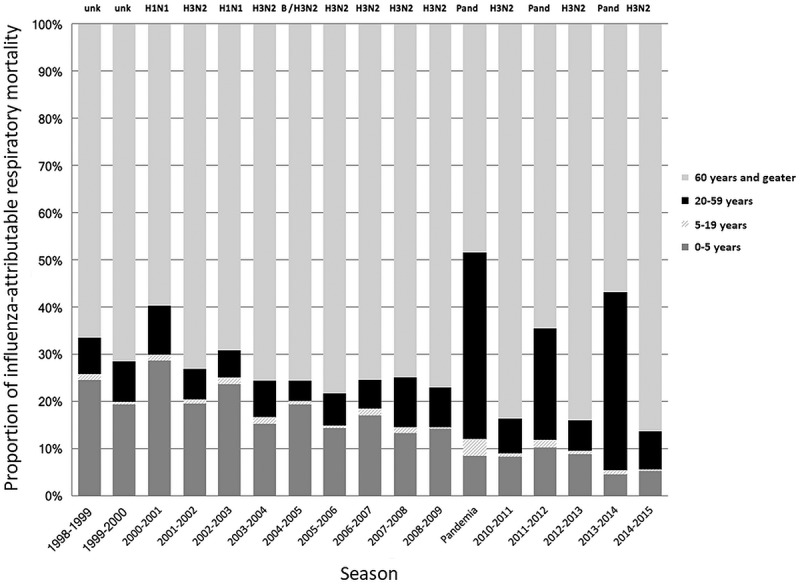
Proportion of influenza-attributable respiratory deaths per age group in Mexico between epidemiological week 27 of 1998 and epidemiological week 26 of 2015. The predominant influenza virus subtype is noted on top of each season. During the 2004–2005 season the predominant influenza virus reported in Mexico was influenza B, followed by influenza A(H3N2).
Overall, despite year to year variability, influenza-attributable cardiovascular mortality in children and adolescents (0–19 years old) during the post-pandemic period were similar to those observed prior to the pandemic period (Table 4). In contrast, adults (20 years of age and older) showed high influenza-attributable cardiovascular mortality in the post-pandemic period; of note, high mortality rates in this age group were observed regardless if influenza A(H1N1)pdm09 or influenza A(H3N2) was the predominant virus. The mean cardiovascular mortality rate during seasons where A(H3N2) virus predominated was higher (7.8 deaths/100,000) than during seasons when A(H1N1)pdm09 virus predominated (5.6 deaths/100,000).
Discussion
This study analyses the mortality attributed to influenza during a period of 17 years in Mexico. This allowed to assess post-pandemic respiratory, cardiovascular, and all-cause mortality attributed to influenza. During prior pandemics, changes in influenza epidemiology have been observed, leading to increased excess mortality several years after the emergence of a pandemic virus [6]. As such, assessment of the impact of influenza in the years following the 2009 pandemic is required. During the 2013–2014 winter season a large number of young adults required hospitalization due to severe influenza infection in Mexico and other countries [7–10,16–19]. Consistent with those observations, we observed a notable increase in respiratory and cardiovascular excess mortality for adults 20–59 years of age (Tables 3 and 4). This also was reflected in a large proportion of influenza-respiratory mortality occurring in this age group, a signature of pandemic influenza behavior. Of note, although excess mortality was not increased during the 2011–2012 season, when influenza A(H1N1)pdm09 virus also predominated, the age distribution of respiratory deaths associated to influenza was very similar in that season to the distribution observed during the pandemic and the 2013–2014 season. This distribution in age groups mostly affected by influenza reflects the continuing effect of a pandemic virus during the post-pandemic period. Post-pandemic waves have been documented several years after other influenza pandemics; during the 1957 influenza A(H2N2) pandemic a similar behavior was noted, with three waves reported during the five years following the emergence of the pandemic virus [6,20]. Also, a similar pattern was reported during the 1918 pandemic in London, where two different waves of increased hospital mortality were documented 3 and 5 years after the pandemic [20]. Different reasons have been advocated to explain these waves: virus and host adaptation, the extent of immunity developed in the population, as well as differences in geographic and demographic circumstances [6,21]. The latter factors have changed dramatically in recent years in comparison to the circumstances surrounding previous pandemics; current demographic patterns (largest world population and longer life expectancy), global mobility, and globalization of information are likely to significantly affect the dynamics of seasonal and pandemic influenza.
During the pre-pandemic period, most seasons were dominated by influenza A(H3N2) virus. During the pre-pandemic seasons when influenza A(H1N1) predominated, mortality rates tended to be lower. Also, mortality rates during the seasons encompassed between 2004 and 2009 tended to be lower than in previous seasons. Of note, influenza vaccination in young children was included in the Mexican immunization schedule in 2004, and a reduction in influenza-associated mortality was observed subsequently in children younger than 5 years of age [11]. In contrast, during the post-pandemic period, influenza A(H3N2) and influenza A(H1N1)pdm09 viruses have been present in alternating seasons in Mexico, and similar influenza-attributable respiratory mortality rates have been observed, independently of the predominant virus. Based on the experience during previous pandemics, an increase in excess mortality associated with influenza A(H1N1)pdm09 virus is not surprising; however, high influenza-associated mortality rates were also observed during seasons where influenza A(H3N2) virus predominated. This was notable for respiratory and cardiovascular deaths particularly in adults 60 years of age and older. In previous pandemics (1918, 1957, and 1968), the pandemic virus became the dominant virus, whereas currently both H1N1 and H3N2 virus continue to co-circulate. This alternation of two influenza virus strains could be explained by a dynamic balance between antigenic drift and population immunity to circulating viruses, as well as increasing vaccination recommendations in diverse age groups. For instance, the 2011–2012 season showed a low influenza-attributable respiratory mortality rate (2.6/100,000; Table 2) compared to other post-pandemic seasons, despite circulation of the pandemic virus; a low mortality could be explained by acquired immunity in the population given the recent presence of the novel influenza virus and large-scale vaccination during previous years.
Similar influenza-attributable all-cause and cardiovascular mortality rates were observed in seasons (1998–2004) and post-pandemic seasons (2010–2015), while in the period 2004–2009 this mortality rates remained significantly lower (Supplementary Table 1). Most of these deaths occur in the >60 years old age group. Whether these differences reflect temporal changes in virulence of circulating influenza strains, or changes in vaccine efficacy remain open questions.
Of interest, during post-pandemic years (2011–2015) cardiovascular mortality tended to be higher in older adults in seasons where strain A(H3N2) predominated (Table 4). This could be explained by low vaccine efficacy against this strain reported in recent years [22]. Vaccine efficacy after the 2009 influenza pandemic has varied in different age groups (24–43%) and through different seasons (7–46%); low vaccine efficacies have been notable in older adults (24%) [22].
A limitation in our study is that the contribution of other viruses, particularly respiratory syncytial virus, to winter excess mortality was not carried out. Unfortunately, no national virological surveillance data for non-influenza respiratory viruses that includes the complete study period is available, precluding inclusion of this factor in the analysis. In a previous study limited to San Luis Potosi state, the effect of respiratory syncytial virus in addition to influenza on winter excess mortality has been considered [23]. The results obtained in the present study are comparable, in general, to those of that study, as well as to other estimates of influenza-associated mortality in Mexico [5]. The estimates obtained in our analysis also correlate with those reported recently for Mexico in a global analysis of seasonal influenza-associated mortality [24]. The influenza-associated respiratory mortality rate for the period between 2002 and 2009, calculated based on the results reported in that study, was 3.86 deaths/100,000 population, while the estimated respiratory rate for the same period in our study was 3.8 deaths/100,000 population. Our results for seasonal influenza mortality are also comparable to those reported for Mexico by Cheng et al. [25].
As for post-pandemic influenza mortality estimates, several studies have been published in recent years [26–29]. Estimates for respiratory influenza-associated mortality are comparable in these studies, ranging between 2.74 and 4.59 deaths/100,000 population, and are similar to our estimates for Mexico (4.65/100,000). In contrast, all-cause mortality estimates have been more variable, and range between 6.94 and 16.25 deaths/100,000 population. Our estimate for Mexico for this period was 20.3 deaths/100,000; this figure is comparable to previously reported pre-pandemic (17.9/100,000) and pandemic (24.6/100,000) all-cause influenza-associated mortality in Mexico [5]. The observed differences between studies may be the result of several factors including the method used to estimate influenza mortality, the predominant influenza type/subtype in the study region, the population structure of each country, as well as the prevalence of underlying risk factors for severe infection.
In summary, influenza-associated mortality after the 2009 pandemic in Mexico demonstrates a persistent change in demographic patterns of the most affected population by the H1N1 virus, particularly during the 2013–2014 season. Although influenza associated-mortality has decreased in children <5 years of age in Mexico, influenza-associated mortality rates in adults >60 years of age continue to be elevated.
Disclosure statement
D. E. Noyola has participated as a member of the speakers’ bureau of AbbVie and speakers’ bureau and the advisory board for Sanofi Pasteur. All other authors report no potential conflict of interest.
Supplementary material
Supplementary data for this article can be accessed here.
References
- [1].Novel swine-origin influenza A (H1N1) virus investigation team Emergence of a novel swine-origin influenza A (H1N1) virus in humans. New Engl J Med. 2009;360:2605–2615. [DOI] [PubMed] [Google Scholar]
- [2].Writing Committee of the WHO consultation on clinical aspects of pandemic (H1N1) 2009 influenza Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med. 2010;362:1708–1719. [DOI] [PubMed] [Google Scholar]
- [3].Perez-Padilla R, de la Rosa-Zamboni D, Ponce de Leon S, et al. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361:680–689. [DOI] [PubMed] [Google Scholar]
- [4].Echeverría-Zuno S, Mejía-Aranguré JM, Mar-Obeso AJ, et al. Infection and death from influenza A H1N1 virus in Mexico: a retrospective analysis. Lancet. 2009;47:565–574. [DOI] [PubMed] [Google Scholar]
- [5].Charu V, Chowell G, Palacio Mejia LS, et al. Mortality burden of the A/H1N1 pandemic in Mexico: a comparison of deaths and years of life lost to seasonal influenza. Clin Infect Dis. 2011;53:985–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Miller MA, Viboud C, Balinska M, et al. The signature features of influenza pandemics. Implications for policy. N Engl J Med. 2009;360:2595–2598. (Erratum, N Engl J Med 2012; 366: 771). [DOI] [PubMed] [Google Scholar]
- [7].Gómez-Gómez A, Magaña-Aquino M, Bernal-Silva S, et al. Risk factors for severe influenza A virus pneumonia in adult cohort, Mexico, 2013–14. Emerg Infect Dis. 2014;20:1553–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Dávila-Torres J, Chowell G, Borja-Aburto VH, et al. Intense seasonal A/H1N1 influenza in Mexico, Winter 2013–2014. Arch Med Res. 2015;46:63–70. [DOI] [PubMed] [Google Scholar]
- [9].Martínez-Briseño D, Torre-Bouscoulet L, Herrera-Zamora Jde J, et al. Clinical characteristics and mortality of influenza A H1N1 and influenza-like illness in Mexico city in the 2013–2014 winter season. Rev Invest Clin. 2016;68:147–153. [PubMed] [Google Scholar]
- [10].Albarrán-Sánchez A, Ramírez-Rentería C, Huerta-Montiel F, et al. Clinical features of patients with influenza-like illness who went to a third level center in the winter of 2013–2014. Rev Med Inst Mex Seguro Soc. 2016;54(Suppl 2):S162–S167. Spanish. [PubMed] [Google Scholar]
- [11].Sánchez-Ramos EL, Monárrez-Espino J, Noyola DE.. Impact of vaccination on influenza mortality in children < 5 years old in Mexico. Vaccine. 2017;35:1287–1292. [DOI] [PubMed] [Google Scholar]
- [12].Dirección General de Información en Salud Bases de datos sobre defunciones [Databases regarding deaths]. México: Secretaría de Salud; cited 2018 March19 Available from: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/std_defunciones.html [Google Scholar]
- [13].Consejo Nacional de Población (CONAPO) Datos de Proyecciones [Projections data]. México: Consejo Nacional de Población; cited 2018 March19 Available from: http://www.conapo.gob.mx/es/CONAPO/Proyecciones_Datos [Google Scholar]
- [14].Serfling RE. Methods for current statistical analysis of excess pneumonia- influenza deaths. Public Health Rep. 1963;78:494–506. [PMC free article] [PubMed] [Google Scholar]
- [15].World Health Organization A practical guide for designing and conducting influenza disease burden studies. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- [16].World Health Organization Severe atypical pneumonia outbreak associated with influenza A (H1N1) pdm09 in Egypt, 2013–2014 season. Wkly Epidemiol Rec. 2014;89:161–164. [PubMed] [Google Scholar]
- [17].Bednarska K, Hallmann-Szelińska E, Kondratiuk K, et al. Evaluation of the activity and influenza-like viruses in the epidemic season 2013/2014. Adv Exp Med Biol. 2015;857:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].DeMarcus LS, Parms TA, Thervil JW. The DoD global, laboratory-based, influenza surveillance program: summary for the 2013–2014 influenza season. MSMR. 2016;23: 2–5. PMID: 2703092. [PubMed] [Google Scholar]
- [19].Puig-Barberá J, Natividad-Sancho A, Trushakova S, et al. Epidemiology of hospital admissions with influenza during the 2013/2014 northern hemisphere influenza season: results from the global influenza hospital surveillance network. PLoS One. 2016;11:e0154970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Oxford JS. Influenza A pandemics of the 20th century with special reference to 1918: virology, pathology and epidemiology. Rev Med Virol. 2000;10:119–133. [DOI] [PubMed] [Google Scholar]
- [21].Wu NC, Wilson IA. A perspective on the structural and functional constraints for immune evasion: insights from influenza virus. J Mol Biol. 2017;429:2694–2709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Belongia EA, Simpson MD, King JP, et al. Variable influenza vaccine effectiveness by subtype: a systematic review and meta-analysis of test-negative design studies. Lancet Infect Dis. 2016;16:942–951. [DOI] [PubMed] [Google Scholar]
- [23].Comas-García A, García-Sepúlveda CA, Méndez-de Lira JJ, et al. Mortality attributable to pandemic influenza A (H1N1) 2009 in San Luis Potosí, Mexico. Influenza Other Respir Viruses. 2011;5:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Iuliano AD, Roguski KM, Chang HH, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 2018;391:1285–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Cheng PY, Palekar R, Azziz-Baumgartner E, et al. Burden of influenza-associated deaths in the Americas, 2002–2008. Influenza Other Respir Viruses. 2015;9(Suppl 1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cohen C, Walaza S, Treurnicht FK, et al. In- and out-of-hospital mortality associated with seasonal and pandemic influenza and respiratory syncytial virus in South Africa, 2009–2013. Clin Infect Dis. 2018;66:95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Freitas AR, Francisco PM, Donalisio MR. Mortality associated with influenza in tropics, state of São Paulo, Brazil, from 2002 to 2011: the pre-pandemic, pandemic, and post-pandemic periods. Influenza Res Treat. 2013;2013:696274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Liu XX, Qin G, Li X, et al. Excess mortality associated with influenza after the 2009 H1N1 pandemic in a subtropical city in China, 2010–2015. Int J Infect Dis. 2017;57:54–60. [DOI] [PubMed] [Google Scholar]
- [29].Zhang H, Xiong Q, Wu P, et al. Influenza-associated mortality in Yancheng, China, 2011–15. Influenza Other Respir Viruses. 2018;12:98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


