Conflict of Interest
A patent application on bpv therapeutic effects in stroke has been filed to China Intellectual Property Office.
Pneumonia, the most common complication following stroke, severely increases mortalities and exacerbates outcomes following both human and experimental stroke 1, 2. To prevent poststroke pneumonia, antibiotic therapies are currently under clinical investigation 1. However, extensive use of antibiotics leads to resistance, which in turn substantially compromises the effectiveness of antibiotics. Thus, new therapeutic strategies are needed for the treatment of stroke‐associated pneumonia.
PTEN is a dual specificity phosphatase, exhibiting high phosphatase specificity toward 3‐phosphorylated phosphoinositides. By dephosphorylating 3‐phosphorylated phosphoinositides, PTEN inhibits Akt activation. Indeed, PTEN inhibitors confer acute neuroprotection by activating Akt when administered before or immediately after experimental stroke 3. Using a potent PTEN inhibitor bpv, our recent findings show that delayed PTEN inhibition improves long‐term functional recovery in a well‐established mouse middle cerebral artery occlusion model (MCAO) 4. Unexpectedly, we also observe that delayed bpv treatment significantly improves survival of stroke mice during 3–7 days following MCAO despite the fact that bpv does not reduce acute infarction 4.
Since the major cause for mouse death during 3–7 days following MCAO is spontaneous lung bacterial infection 5, 6, this study investigated if delayed administration of bpv improved survival of stroke mice by suppressing post‐stroke spontaneous lung infection. We also investigated if cerebral ischemia impaired the local Akt cascade in the lung and if bpv restored the lung Akt signaling following MCAO.
Middle cerebral artery occlusion model was induced in adult male CD‐1 mice (30 ± 2 g) via the intraluminal suture technique 4. Bpv or vehicle saline was administered at 24 h (0.2 mg/kg/day) after MCAO. First, we investigated if bpv treatment, starting at 24 h after MCAO, reduced lung bacterial infection at 96 h after MCAO. Remarkably, lower bacterial loads were detected in the lungs of bpv‐treated mice than in those of saline‐treated mice (Figure 1A). Histological examination further revealed typical signs of bacterial pneumonia, that is, thickening of alveolar walls and intraalveolar neutrophil infiltrates, in all saline‐treated mice but not in sham‐operated or bpv‐treated mice at 96 h after MCAO (Figure 1B).
Figure 1.
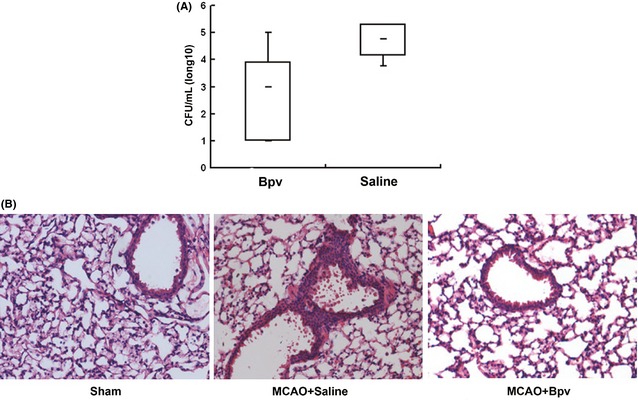
The PTEN inhibitor bpv suppressed spontaneous lung bacterial infection following MCAO. (A) Significantly lower bacterial loads in the lung were detected in bpv‐ vs. saline‐treated mice at 4 days after MCAO (n = 8). (B) Thickening of alveolar walls and neutrophilic infiltrates were observed in the lungs of MCAO mice treated with saline but not in those of sham‐operated or bpv‐treated mice at 96 h after MCAO (Representative images of three animals/group).
There is evidence that PTEN gene deletion increases mouse survival by activating Akt and enhancing phagocytosis of lung macrophages following pneumonia infection 7. Thus, we investigated if cerebral ischemia activated PTEN and consequently impaired local Akt signaling in the lung following MCAO. As shown in Figure 2A, compared to sham‐operated mice, MCAO mice displayed significantly reduced levels of phosphorylated (inactivated) PTEN while maintained comparable levels of total PTEN in the lung, suggesting that PTEN activation was enhanced in the lung following MCAO. As a PTEN inhibitor, bpv restored the levels of phosphorylated (inactivated) PTEN/total PTEN in the lung following MCAO. In line with enhanced activation of PTEN, Akt activation (phosphorylation), a cascade downstream inhibited by PTEN, was significantly reduced in the lung of MCAO mice (Figure 2A). As expected, bpv restored akt activation in the lung following MCAO, as evidenced by the increased ratios of p‐Akt/Akt. Our data suggested that Akt phosphorylation (activation) in the lung was impaired by MCAO‐induced activation of PTEN and that bpv could block the MCAO‐induced local impairment of Akt activation in the lung.
Figure 2.
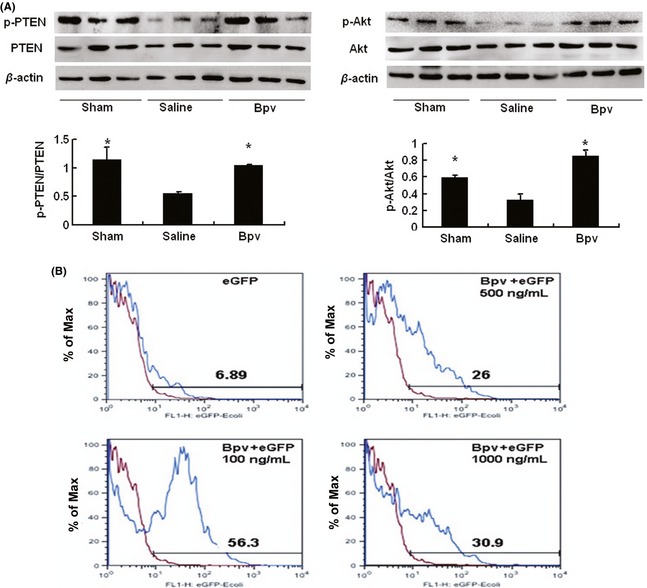
Bpv attenuated MCAO‐induced local PTEN activation and Akt inactivation in the lung and increased macrophage phagocytosis in vitro. (A) Compared to sham‐operated mice, saline‐treated MCAO mice displayed reduced PTEN phosphorylation (inactivation, p‐PTEN) and Akt phosphorylation (activation, p‐Akt) while maintained comparable levels of total PTEN and Akt in the lung at 4 days after MCAO. Bpv treatment significantly attenuated MCAO‐induced decrease in PTEN inactivation (phosphorylation) and Akt activation (phosphorylation) in the lung. *P < 0.05 compared to saline‐treated MCAO mice. (B) Uptake of Escherichia coli expressing enhanced green fluorescence protein (eGFP) by primary macrophages was quantified with FACS. Macrophage phagocytosis was enhanced by bpv at the concentrations of 100, 500, and 1000 ng/mL Results were representative images of three independent experiments. The numbers labeled in the figure 2B were the percentage of eGFP + macrophages.
Macrophages from PTEN‐deficient mice displayed enhanced phagocytic ability, which accounts for prolonged survival of the mice subjected to Streptococcus pneumoniae challenge 7. Thus, we examined bpv effects on macrophage phagocytosis using the FACS‐based assay. Primary intraperitoneal macrophages were isolated and incubated with bpv or saline overnight. Macrophages were then incubated with Escherichia coli expressing enhanced green fluorescence protein (eGFP) at a multiplicity of infection of 100 for 30 min at 37°C. After washing with PBS extensively, uptake of E. coli was assessed by quantifying eGFP positive cells with FACS Calibur. Uptake of E. coli expressing eGFP by primary macrophages was enhanced by bpv at the concentration of 100, 500, and 1000 ng/mL, indicating that the phagocytosis of macrophage was enhanced by bpv treatment (Figure 2B).
This study presented two major findings. First, post‐ischemic administration of a potent PTEN inhibitor, bpv, starting at 24 h after stroke onset, reduced mortalities by suppressing lung bacterial infection following cerebral ischemia. Second, for the first time, our results suggested that stroke impaired local PI3K/Akt cascade in the lung through PTEN activation and that the impaired local PI3K/Akt cascade contributed to stroke‐associated pneumonia.
On the basis of following reasons, we interpreted that bpv improved the survival of MCAO mice by suppressing post‐ischemic lung bacterial infection rather than by conferring acute neuroprotection. First, PTEN inhibitors confer acute neuroprotection only when they are administered prior to or immediately after stroke onset 3, 8, 9. Consistently, we found that bpv, administered at 24 h after MCAO, does not reduce acute infarction at 4 days after MCAO 4. Second, it is during 3–7 days after MCAO that bpv reduces mortalities, a period during which the major cause for death of MCAO mice has been attributed to lung infection 5. Third, we observed that delayed bpv treatment reduced bacterial loads and ameliorated tissue damage in the lung at 4 days following MCAO. Collectively, we concluded that bpv inhibitory effects on lung infection rather than its acute neuroprotective effects accounted for better survival of bpv‐treated mice following MCAO.
Pneumonia is the most common complication following stroke, which not only increases mortality but also exacerbates brain infarct damage 2. In addition to the antibiotic approach, several strategies, such as selective immunomodulation, the blockade of sympathetic activation and inhibition on spleen atrophy, substantially reduce post‐stroke lung infection in experimental stroke 5, 6, 10. However, these strategies are effective only when they are applied before or immediately after cerebral ischemia 5, 6. Since bpv effectively suppressed post‐stroke lung infection within a clinically relevant therapeutic window, PTEN inhibition represents a valuable approach for the treatment of post‐stroke pneumonia.
Acknowledgments
The study is supported by National Science Foundation of China (81041094, 81371278, 81070959 and 81130023) and Priority Academic Program Development of Jiangsu Higher Education Institutes (PAPD).
The first two authors contributed equally to this study.
References
- 1. Harms H, Prass K, Meisel C, et al. Preventive antibacterial therapy in acute ischemic stroke: A randomized controlled trial. PLoS One 2008;3:e2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Meisel C, Prass K, Braun J, et al. Preventive antibacterial treatment improves the general medical and neurological outcome in a mouse model of stroke. Stroke 2004;35:2–6. [DOI] [PubMed] [Google Scholar]
- 3. Li D, Qu Y, Mao M, et al. Involvement of the PTEN‐AKT‐FOXO3a pathway in neuronal apoptosis in developing rat brain after hypoxia‐ischemia. J Cereb Blood Flow Metab 2009;29:1903–1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mao L, Jia J, Zhou X, et al. Delayed administration of a PTEN inhibitor BPV improves functional recovery after experimental stroke. Neuroscience 2013;231:272–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Prass K, Meisel C, Hoflich C, et al. Stroke‐induced immunodeficiency promotes spontaneous bacterial infections and is mediated by sympathetic activation reversal by poststroke T helper cell type 1‐like immunostimulation. J Exp Med 2003;198:725–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Braun JS, Prass K, Dirnagl U, Meisel A, Meisel C. Protection from brain damage and bacterial infection in murine stroke by the novel caspase‐inhibitor Q‐VD‐OPH. Exp Neurol 2007;206:183–191. [DOI] [PubMed] [Google Scholar]
- 7. Schabbauer G, Matt U, Gunzl P, et al. Myeloid PTEN promotes inflammation but impairs bactericidal activities during murine pneumococcal pneumonia. J Immunol 2010;185:468–476. [DOI] [PubMed] [Google Scholar]
- 8. Liu B, Li L, Zhang Q, et al. Preservation of GABAA receptor function by PTEN inhibition protects against neuronal death in ischemic stroke. Stroke 2010;41:1018–1026. [DOI] [PubMed] [Google Scholar]
- 9. Shi GD, OuYang YP, Shi JG, Liu Y, Yuan W, Jia LS. PTEN deletion prevents ischemic brain injury by activating the mTOR signaling pathway. Biochem Biophys Res Commun 2011;404:941–945. [DOI] [PubMed] [Google Scholar]
- 10. Wong CH, Jenne CN, Lee WY, Leger C, Kubes P. Functional innervation of hepatic iNKT cells is immunosuppressive following stroke. Science 2011;334:101–105. [DOI] [PubMed] [Google Scholar]


