Conflict of Interset
The authors declare no conflict of interest.
Atlantoaxial dislocation (AAD) rarely leads to vertebral artery dissection (VAD). There have only been 10 cases of VAD caused by AAD been reported. We report one case of VAD caused by AAD. Based on three‐dimensional computed tomography angiography (CTA) results, we speculate on the mechanism of VA injury and propose a rational treatment plan.
An 18‐year‐old man presented with a history of sudden severe headache, neck pain, unconsciousness, and irritating cough with no obvious inducing factors in July 2010. Neck magnetic resonance imaging (MRI) revealed atlanto‐occipital fusion, AAD with a 6‐mm atlanto‐dental interval. Head MRI showed fresh infarction lesions located on the right occipital lobe, bilateral cerebellar hemispheres, and the right medulla oblongata. The patient received whole cerebral digital subtraction angiography (DSA) in our hospital. DSA showed the V3 segment of the right VA dissection with distal occlusion, and development of the posterior inferior cerebellar artery (PICA) and basilar artery (BA) was absent (Figure 1). He was prescribed anti‐coagulant with adoptable warfarin dose to sustain the international normalized ratio between 2 and 3. After 1 week, he was alert and oriented, and his headache gradually improved. Three months later, neck 3D‐CTA was performed, which showed a smooth recanalized and free‐flowing right VA without thrombosis (Figure 2A), and the 3D‐CT and 3D‐CTA showed the right VA was compressed at the anterior border of the transverse formen of C2 (Figure 2B). He then received posterior occipito‐cervical reduction and fusion surgery as Jian et al. 1 had described. After operation, the recovery of the patient was smooth. He was discharged from hospital on the 5th day after the operation.
Figure 1.

Cerebral digital subtraction angiography displays the left vertebrobasilar artery without any abnormalities, but the V3 segment of the right VA shows dissection with distal occlusion (↑), and development of the posterior inferior cerebellar artery and basilar artery was absent.
Figure 2.
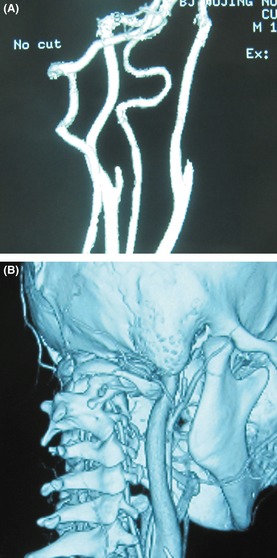
The cervical 3D‐computed tomography angiography (CTA) and 3D‐CT of the patient 3 months after the symptoms onset. (A) The cervical 3D‐CTA showed a smooth recanalized and free‐flowing right VA without thrombosis. (B) Cervical 3D‐CT and 3D‐CTA shows the transverse foramen of C1 moved forward as a result of atlas dislocation. This led to the foramina of C1 and C2 retracting the VAs and made them compressed around the C2 foramen (↑).
Cervical arterial dissections merely account for about 2% of ischemic strokes. However, it is a crucial etiological factor inducing stroke in young and middle‐aged people 2, and VAD has an estimated incidence of approximately 1.0 per 100,000. VAD can be secondary to blunt cervical trauma or can be spontaneous. Endothelial injury and decreased blood flow velocity encourage thrombus formation, with the inevitable emboli causing brain stem and cerebellar infarctions. The mortality rate of VAD is <5%, and approximately three‐quarters of the patients who suffered strokes could recover well 3. Approximately 51% of VADs emerge between the atlas and the axis. In this region, it is speculated that the atlanto‐occipital and atlantoaxial joints exhibit such a great range of motion during activity of the head and neck that the VA is vulnerable to the retraction strength of bone structures. As a result, the endomembrane of the VA will be injured, which consequently causes the dissection 4.
In AAD patients, atlantoaxial stability is lost, which intensifies the retraction force on the VA, which lies between the atlas and axis, and this can enable the VA to be compressed by bone structures, even causing VAD. To date, only 10 cases have been reported regarding AAD patients whose first symptom was posterior cerebral ischemia, nine of whom had atlantoaxial instability associated with os odontoideum, and the left one was associated with basilar invagination 5, 6, 7, 8, 9, 10. Fukuda et al. 7 used 3D‐CTA to view the VA running through the transverse foramina of C1 and C2 in one patient. They proposed that the mechanism of VA injury caused by AAD was because the VA in this region was hyper‐curved. The 3D‐CT and 3D‐CTA could also demonstrate the mechanism of VAD formation induced by bone compression; in this case, the transverse foramen of the C1 moved forward, the foramina of C1 and C2 retracted the right VA, and the right VA was compressed at the anterior border of the transverse formen of C2. The abnormal movement between C1 and C2 increased the compression of the VA and injured the VA, leading to the development of VAD.
Determining the mechanism of VAD caused by atlanto‐occipital malformation could help provide a basis for rational treatment. During the VAD, acute‐phase anticoagulation therapy should be adopted to encourage the recanalization of the dissected VA. After the recanalization of the VA and when the endomembrane is stable, usually 3 months after the onset of VAD, surgery was considered to reduce the C1‐C2 luxation with internal fixation system. After displaced C1 and C2 foramina reduction, the retraction strength upon the VA sharply decreased, which combined with avoidance of dynamic injury because the fusion of the AO joint reduced the AVD recurrent risk.
Acknowledgment
The diagnosis and treatment of this patient were under the direction of the chairman of the department of neurosurgery, Professor Feng Ling.
References
- 1. Jian FZ, Chen Z, Wrede KH, Samii M, Ling F. Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery 2010;66:678–687. [DOI] [PubMed] [Google Scholar]
- 2. Kim YK, Schulman S. Cervical artery dissection: pathology, epidemiology and management. Thromb Res 2009;123:810–821. [DOI] [PubMed] [Google Scholar]
- 3. Fusco MR, Harrigan MR. Cerebrovascular dissections–a review part I: spontaneous dissections. Neurosurgery 2011;68:242–257. [DOI] [PubMed] [Google Scholar]
- 4. Saeed AB, Shuaib A, Al‐Sulaiti G, Emery D. Vertebral artery dissection: warning symptoms, clinical features and prognosis in 26 patients. Can J Neurol Sci 2000;27:292–296. [DOI] [PubMed] [Google Scholar]
- 5. Panda S, Ravishankar S, Nagaraja D. Bilateral vertebral artery dissection caused by atlantoaxial dislocation. J Assoc Physicians India 2010;58:187–189. [PubMed] [Google Scholar]
- 6. Kikuchi K, Nakagawa H, Watanabe K, Kowada M. Bilateral vertebral artery occlusion secondary to atlantoaxial dislocation with os odontoideum: implication for prophylactic cervical stabilization by fusion–case report. Neurol Med Chir (Tokyo) 1993;33:769–773. [DOI] [PubMed] [Google Scholar]
- 7. Fukuda M, Aiba T, Akiyama K, Nishiyama K, Ozawa T. Cerebellar infarction secondary to os odontoideum. J Clin Neurosci 2003;10:625–626. [DOI] [PubMed] [Google Scholar]
- 8. Sasaki H, Itoh T, Takei H, Hayashi M. Os odontoideum with cerebellar infarction: a case report. Spine (Phila Pa 1976) 2000;25:1178–1181. [DOI] [PubMed] [Google Scholar]
- 9. Takakuwa T, Hiroi S, Hasegawa H, Hurukawa K, Endo S, Shimamura T. Os odontoideum with vertebral artery occlusion. Spine (Phila Pa 1976) 1994;19:460–462. [DOI] [PubMed] [Google Scholar]
- 10. Miyata I, Imaoka T, Masaoka T, Nishiura T, Ishimitsu H. Pediatric cerebellar infarction caused by atlantoaxial subluxation–case report. Neurol Med Chir (Tokyo) 1994;34:241–245. [DOI] [PubMed] [Google Scholar]


