Supplemental digital content is available in the text.
Abstract
SIGNIFICANCE
The successful uptake, integration, and use of vision rehabilitation devices with speech output depend to a large part on their audibility. However, individuals with combined vision and hearing impairments are at a disadvantage when using devices that do not consider multiple impairments.
PURPOSE
Sensory rehabilitation for individuals with combined vision and hearing impairment often relies on the use of assistive technology devices that use speech outputs (e.g., talking clock), but in individuals with dual impairment, their use is likely compromised by a concurrent hearing loss. The goal of this study was to evaluate the audibility of these devices in a population of individuals with acquired dual sensory impairment.
METHODS
We measured the ability to correctly repeat speech output presented by three assistive technology devices (talking watch, calculator, scanner) and confidence levels in response accuracy in 24 participants with visual impairment only and in 22 individuals with dual sensory loss. Stimuli were presented at three volumes that were repeated one or four times. Participants were placed at a fixed distance of 74 cm from the sound source.
RESULTS
The pattern of results was similar across the different devices, whereby an interaction of volume and repetition indicated that participants' accuracy to repeat a phrase and their confidence in their response improved with increasing volume, but more so at higher numbers of repetition (P < .05; ω2, from 0.005 to 0.298). Participants with dual sensory loss generally had lower accuracy and confidence.
CONCLUSIONS
Scores and confidence levels being very low across devices and users suggest that even participants with normal hearing for their age experienced a certain level of difficulty understanding speech output, confirming the need for better assistive technology device design.

Interest in combined vision and hearing loss (dual sensory impairment) as comorbidity in the aging population has gained increasing attention in gerontology research agendas across the globe in recent years, given the dramatic increase in the number of older adults who are affected with both sensory impairments. The proportion of older adults 65 years or older who are affected by dual sensory impairment has been reported to be as high as 34%, and recent data revealed that 26% of older adults receiving home care and an additional 30% of long-term-care residents report both impairments of vision and hearing.1,2 With the general population aging, the prevalence of dual sensory impairment is expected to increase drastically in the coming decades, along with an increased need for the rehabilitation services dispensed to these individuals. The use of assistive technology devices constitutes an important part of sensory rehabilitation interventions, and these devices are often used as part of the compensation strategies for the disability. For example, auditory assistive technology often uses visual cues, such as warning lights for battery life, whereas visual assistive devices frequently use auditory signals, such as text-to-speech in reading devices. However, because dual sensory impairment is characterized by the loss of both modalities (vision and hearing), the use of such devices can be compromised because most of them rely on one ability to compensate for the loss of the other. A closer look at the literature confirms that very few data concerning the usability of assistive technology devices in the dual sensory impairment population exist. More specifically, we are unaware of any research that has assessed the audibility of low vision assistive technology devices that have an auditory component (e.g., speech output) in individuals affected with dual sensory impairment, a gap the present study aims to fill.
COMMON AGE-RELATED CHANGES IN HEARING
Age-related changes in hearing may be related to a variety of factors.3 Changes in the inner ear are have the most effect on speech understanding. As a person ages, the effects of environmental exposures (e.g., noise) are cumulative and may cause permanent damage to the cochlea (inner ear), the sensory organ that allows sound transmission to the auditory nerve. The hallmark of age-related hearing loss (presbycusis) is worsening of high-frequency thresholds. There are also age-related changes in the auditory nervous system that can affect the clarity of sound even if thresholds remain normal. Age-related hearing loss of high frequencies may thus result in reduced audibility and clarity of speech.3,4 Importantly, the effects of auditory aging can cause communication difficulties in everyday life that may eventually lead to social isolation and reduction of quality of life, resulting in the need for rehabilitation.5 Hearing rehabilitation aims to limit these effects induced by hearing loss and may consists of sensory management, perceptual training, counseling and use of assistive technology.6
COMMON AGE-RELATED CHANGES IN VISION
Normal age-related changes in vision include presbyopia, decreasing light transmission, and decreasing pupil size.4 The four most frequent causes of age-related visual impairment are cataracts, age-related macular degeneration, glaucoma, and diabetic retinopathy.7,8 Cataracts are characterized by the metabolic processes linked to aging processes that result in a clouding of the lens, causing blurred vision and poorer contrast sensitivity.4,9 Fortunately, when the cataract becomes an obstacle to vision, it can be extracted surgically, and visual function is generally restored.7,10 Age-related macular degeneration is characterized by an accumulation of extracellular deposits accelerated by risk factors such as smoking or sunlight exposure, which prevents the retina from receiving proper nutrition. As a result of this accumulation, retinal atrophy and tissue disorganization develop, and central vision for details becomes progressively affected. Glaucoma, a complex set of diseases that is not yet completely understood, is linked to the inability to maintain the balance between produced and evacuated aqueous humor in the anterior chamber of the eye.8 This can increase intraocular pressure and eventually cause damage to the optic nerve either by direct pressure or by cutting off the blood supply to the nerve and thus creating atrophy.9 The main visual consequence is a progressive reduction of the visual field, as well as loss in visual acuity and contrast sensitivity in the late stages of the disease.9 Diabetic retinopathy is a disease affecting the small blood vessels in the retina.8 It can cause, among other problems, retinal hemorrhages, microaneurysms, and diabetic macular edema.9 Because of the variety of symptoms linked to this disease, visual consequences may also vary from a central deficit (macular edema) to Swiss cheese vision, where some parts of the retina become unusable, whereas others remain healthy.10 However, regardless of the cause, age-acquired diseases of the eye may result in reduced visual acuity and contrast sensitivity, which are not only important vision capacities in daily functioning but also important features to consider for speech reading.11
DUAL SENSORY IMPAIRMENT
The term “deafblindness” characterizes individuals with different levels of residual vision or hearing; therefore, it is often referred to as dual sensory impairment and includes early onset of either visual or hearing impairment and late development of the other and late onset of both impairments. The present study focused on acquired dual sensory impairment, which is often related to aging processes.12 This category represents indeed the greater part of individuals affected by dual sensory impairment, the most common causes being age-related macular degeneration in combination with presbycusis.13,14 Age-related changes in hearing may induce the loss of high frequencies, leading to poor speech recognition. In addition, age-acquired visual impairment may result in reduced visual acuity and contrast sensitivity. The combination of these two impairments frequently co-occurs with increased age and can create a very challenging reality for the individuals affected. For example, the use of simple everyday devices, such as a telephone, can be compromised, as its use requires both hearing skills to understand the person on the other end of the call and visual skills to be able to use the keypad. Some authors agree that dual sensory impairment may even represent a distinct disability, considering that the loss of one type of sensory input cannot be compensated by the other.1,4
Together, these two types of impairment can have a tremendous negative effect on people's functionality and social interactions. Guthrie et al.1 recently conducted a study that aimed to compare demographics and functional and psychological characteristics of individuals with dual sensory impairment using a database that contained data from four countries (Canada, the United States, Belgium, and Finland). The authors found that individuals with deafblindness had higher rates of depression, communication difficulties, and cognitive loss compared with participants with only one or without any sensory impairment. Also, cognition seemed to decline faster in individuals with dual sensory impairment living in long-term facilities compared with residents with a single-modality impairment. A study performed among 102 American older adults demonstrated that vision and hearing loss were moderately related to depression and anxiety among this population if the access to social and caregiving support was less than average.15 McDonnall16 obtained similar results for depression rate over time. Indeed, among the 2689 individuals composing the study sample, those who developed dual sensory impairment with age had higher rates of depression. In addition, in a cross-sectional study conducted by Viljanen et al.,17 27,536 participants older than 50 years were recruited to evaluate the impact of dual sensory impairment on social participation. Among the individuals tested, two-thirds of the participants with dual sensory impairment were not participating socially compared with one-half of the participants who did not report sensory impairment. The authors calculated an odds ratio of 1.21 of reduced social participation within the dual sensory impairment group compared with the control group. Guthrie et al.1 suggest that people with dual sensory impairment may experience an array of other illnesses, and therefore, this particular type of impairment needs to be addressed specifically to ensure the best quality of life.
DUAL SENSORY IMPAIRMENT REHABILITATION
Dual sensory impairment rehabilitation uses not only assistive technology devices such as hearing aids or other systems designed to help discriminate speech (e.g., frequency modulation systems, pocket talker, and infrared systems for television), or magnifiers and talking devices to help with reading, but also technologies and strategies such as cochlear implants or tactile recognition.18 Environmental adaptations and communication strategies are used to ensure best quality of life. Among assistive technology devices, environmental devices can be used, such as vibrotactile or light signals for the doorbell, the telephone, or the fire alarm. In addition, cochlear implants are frequently used in individuals with dual sensory impairment and have been associated with improved communication.19 Cochlear implants are also used with older adults who have acquired dual sensory impairment and have been shown to adequately restore speech recognition with stable results over time.20 Special environmental adaptations can be made, for example, enhanced contrast and lighting, to facilitate daily activities and movement for those with low vision.3 Communication strategies such as lip/speech reading are also taught to individuals with dual sensory impairment, even those with moderate to severe visual impairment.11 Indeed, these authors reported the benefits of paired auditory and visual speech for recognition and noted that these paybacks could also be beneficial for older visually impaired patients with a visual acuity as low as 6/120. Rehabilitation has been shown to be effective in terms of social interaction and prevention of depression in individuals with dual sensory impairment, although very few studies have addressed the subject.18,21,22
DUAL SENSORY IMPAIRMENT REHABILITATION CHALLENGES
Assistive technology devices represent a priority in dual sensory impairment rehabilitation; however, their uptake, use, and abandonment rate have not been fully documented.18 Because many rehabilitation strategies are based on compensating for the missing ability by a second one, dual loss may create very specific challenges. This is particularly true because many assistive technology devices used in low vision rehabilitation are devices that use speech output. Wittich and Gagné10 suggested that the auditory signals used in assistive technology devices should be optimized to be easily detected, discriminated, and recognized by its users. With regard to low vision devices, this means that auditory components should be easily understood whether individuals have normal auditory threshold, have age-related diminished high-frequency sensibility, or have a moderate to profound hearing impairment. These specific devices are clearly not designed to be used by a population with age-acquired dual sensory impairment, considering the related hearing loss, but are still used because they are the only aids currently available. However, to date, no data examining their usability within this population exist. Considering that around 46% of the population older than 65 years affected by vision impairment also has a concurrent hearing loss, the need to investigate the use of appropriate assistive technology devices for the older population with dual sensory impairment is more than justified.23
RESEARCH AIM
Members of this research team have previously investigated the usability of auditory assistive technology devices among a low vision population.24 Sixty adults 60 years or older were asked to use three different devices with either minimal or no instructions at all. The main outcome measure was successful device use, defined as the proper execution of the consecutive steps required to use the assistive technology devices. The goal of the present study is to reverse this previous approach and evaluate the audibility of low vision devices (talking watch, calculator, and scanner) with an auditory or speech component in a population of individuals with acquired dual sensory impairment. We investigated whether these specific devices could be understood by their users. In addition to the success in correctly hearing a device as an outcome measure for our study, we considered the accuracy of the responses as the ability to repeat the sound output of a device correctly, whether it corresponds to words or numbers, and the confidence level toward the repetition of the output. The ultimate goal was to establish clinical guidelines to inform the choice of assistive technology devices for this specific clientele as a part of rehabilitation, based on the audibility of each device.
METHODS
The study protocol was approved by the Centre de recherche interdisciplinaire en réadaptation du Montréal métropolitain's institutional review board (CRIR-1165-0716) in accordance with the Declaration of Helsinki for research with human participants.
Participants
The participant group with dual sensory impairment included individuals with a vision impairment that was characterized by a visual acuity worse than 6/60 in the better eye with best standard correction, concurrent to at least a moderate hearing loss corresponding to an average pure-tone hearing threshold across four frequencies (500, 1000, 2000, and 4000 Hz) of 26-dB hearing loss or more in the better ear without hearing aid, as required for hearing rehabilitation eligibility in Quebec, Canada.13 The vision criteria and a hearing screening were used to define the study group of individuals with normal hearing and visual impairment only. All participants were recruited by either the CRIR/Centre de réadaptation MAB-Mackay du CIUSSS du Centre-Ouest-de-l'Île-de-Montréal or the CRIR/Institut Nazareth et Louis-Braille du CIUSSS de la Montérégie-Centre. The cause of either sensory impairment was irrelevant, as long as visual acuity was impaired sufficiently due to some defect of central vision (e.g., age-related macular degeneration and diabetic retinopathy), resulting in decreased acuity.
Materials
The devices used in this study were a Tel-Time Talking Watch (MaxiAids, Farmingdale, NY; Appendix Fig. A1, available at http://links.lww.com/OPX/A394), a 10-digit Talking Calculator (MaxiAids; see Appendix Fig. A2, available at http://links.lww.com/OPX/A395), and an Optelec ClearReader+ Basic talking scanner (Optelec, Longueuil, Quebec, Canada; see Appendix Fig. A3, available at http://links.lww.com/OPX/A396). These assistive device technologies are all found among the aids available through the Régie de l'assurance maladie du Québec, the third-party payer for assistive technology devices in Quebec, Canada, and were chosen because they are among the most frequently recommended devices at the rehabilitation centers where this study was conducted. For reasons of availability, only female voices were used. The outputs of these three assistive technology devices were recorded using the Audacity software, along with a Blue Yeti (Logitech, Newark, CA) microphone in a soundproof room, whereby each device was 30 cm away from the microphone. Recorded audio was cleaned by applying a noise reduction in Audacity based on an ambient sound recording in the soundproof room, to maintain the sound quality for the purpose of volume magnification, without creating distortions of the sound. This procedure allowed us to maintain the most realistic sound profile of each recording.
The iTunes software (Apple Inc., Cupertino, CA) was used to play back the pre-recorded tracks corresponding to each device as WAVE files through a single speaker (Logitech Z130, Logitech, Newark, CA) attached to a MacBook Air laptop (Apple Inc.). The speech outputs from the devices varied between words or numbers, depending on the device (e.g., spoken time when using a watch). Three sound components for each device were recorded and played at three different intensity levels whereby the lowest volume represented the intensity at which the device's output would normally be presented at 30-cm distance during, for example, a demonstration of the device; the lowest volume for the watch was 50 dBA, and for the calculator and the scanner, it was 60 dBA, with volumes each increasing by 10 dB at each step. The choices of these starting volumes were based on the volume capacities and the volume range of each device. Please note that for all three devices the maximal volume created in this experimental setup was beyond the volume ability of the device. The targets for the talking watch consisted of three different times. For the calculator, three five-digit numbers were presented. For the scanner, three short phrases, varying from two to four words, were played.
Procedure
After obtaining informed written consent, the participants were placed at a fixed distance of 74 cm from the sound source (from the middle of the speaker to the middle of the outer ear). Participants who owned and brought their hearing aid wore the device during testing, and its functionality was confirmed by the research assistant. A practice target was presented to familiarize the participant. A photograph of the device and its name were presented to the participant before each sound series. Phrases were presented at the three volumes specified previously and were repeated first once and then four times for each volume. Participants were asked to repeat each phrase (either after the one or the four consecutive repetitions of the target) and rate their level of confidence in their answer on a scale from 1 to 10. No feedback was given during testing as to whether each response was correct. Testing was conducted under controlled conditions with a background noise of 37.7 dBA.
When visual acuity and hearing threshold were not available, a vision and hearing screening was performed using the Freiburg Visual Acuity Test and the method for hearing screening by Davis et al.,25 comprising the presentation of a 35-dB hearing loss pure tone at 3000 Hz one ear at a time, as well as two questions related to hearing difficulties. In the absence of a positive response in the better ear or with a positive response to one of the two questions, the participant was classified in the dual sensory impairment group. Additional information was collected, such as perceived hearing handicap (Hearing Handicap Inventory for the Elderly–validated questionnaire26) and cognitive screening (blind version of the Montreal Cognitive Assessment27), the administration order of which was alternated to be either at the beginning or at the end of the protocol.
RESULTS
Sample
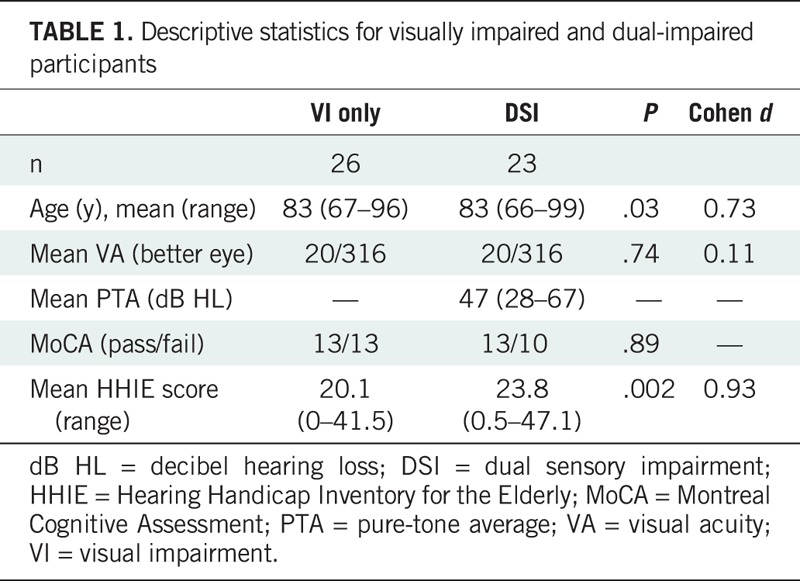
We measured the ability to correctly repeat speech output presented by the assistive technology devices as well as participants' confidence levels in their response accuracy in 26 participants with visual impairment only (visual acuity from 20/50 to no light perception in the better eye) and in 23 participants with dual sensory loss (visual acuity from 20/40 to no light perception; unaided mean pure-tone threshold ranging from 28- to 75-dB hearing loss). Analyses were conducted using the mean score of three trials per person per condition. Summary descriptive statistics and group comparisons are provided in Table 1. The proportion of individuals who failed the Montreal Cognitive Assessment in each group was similar. The Hearing Handicap Inventory for the Elderly scores, although statistically significantly higher in the dual sensory impairment group (t47 = 3.25, P = .002, d = 0.93), indicated that a wide range of individuals subjectively experienced hearing difficulties in both groups.
TABLE 1.
Descriptive statistics for visually impaired and dual-impaired participants
Success
The success of a task corresponded to the ability of a participant to repeat a target sentence without any mistakes (e.g., nine forty-one for the time 0941 hours). Fig. 1 presents the overall percentage of participants who were able to complete at least one of the tasks correctly. Success rates were low, ranging from 0 to 38%, depending on the condition, the device, and the participant group.
FIGURE 1.
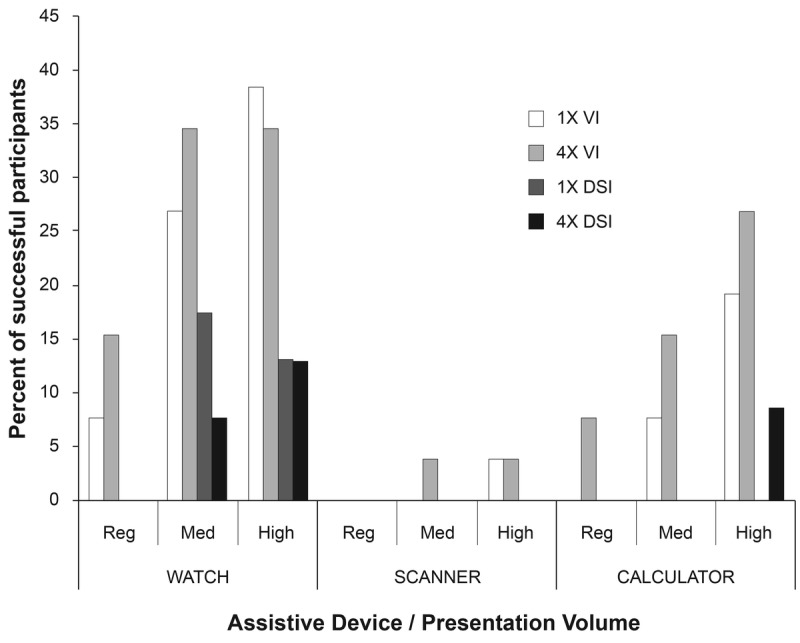
Proportion of visually impaired and dual-impaired participants who could complete at least one of the tasks without mistakes. Success increased with increasing volume and with increasing repetition; however, overall success rates were extremely low and never exceeded 40%. 1× = one stimulus presentation; 4× = four stimulus presentations; DSI = dual sensory impairment; VI = visual impairment.
Accuracy and Confidence
Accuracy was defined as the ratio of correct words or numbers as a function of the total target number of words or numbers. In addition, the participants were asked to rate their confidence level in their response for each device and each task difficulty by rating their confidence on a scale from 1 to 10, with 10 being very confident. Both dependent variables were statistically significantly correlated, whereby increased accuracy indicated increased confidence across all conditions. Pearson correlation coefficients ranged from r = 0.53 to 0.72 for the watch, r = 0.52 to 0.63 for the calculator, and r = 0.49 to 0.65 for the scanner. Correlations between accuracy and Hearing Handicap Inventory for the Elderly scores ranged from r = 0.50 to 0.38 for the watch, r = 0.49 to 0.23 for the calculator, and r = 0.33 to 0.17 for the scanner. Correlations between confidence and Hearing Handicap Inventory for the Elderly scores ranged from r = 0.44 to 0.39 for the watch, r = 0.34 to 0.16 for the scanner, and r = 0.56 to 0.39 for the calculator. Correlations between pure-tone averages and the dependent variables were similar in size but not statistically significant, given the reduced sample size of individuals where audiograms were available.
Statistics
Analyses of covariance were conducted using both Hearing Handicap Inventory for the Elderly and visual acuity scores as potential covariates. For acuity, arbitrary values of 2.3, 3, and 3.1 as suggested by Schulze-Bonsel et al.28 were used to allow acuity reports of hand motion, light perception, and no light perception to be included in the analysis; however, no statistically significant effects were detected. Analyses of covariance are therefore only reported hereinafter for those analyses where Hearing Handicap Inventory for the Elderly scores emerged as a significant covariate.
Watch
A three-way mixed within-between analysis of covariance was conducted to examine differences in accuracy across levels of volume and repetition in both visually impaired participants and individuals with dual sensory impairment. After controlling for the Hearing Handicap Inventory for the Elderly survey scores (F1,46 = 6.81, P = .01, η2 = 0.12), an interaction of volume and repetition emerged (F2,92 = 5.78, P = .004, η2 = 0.10), suggesting that scores improved with increased number of repetitions but more so at lower volumes (Fig. 2). However, scores did not differ significantly between the two groups, suggesting that individuals with normal hearing for their age had the same results as individuals with dual sensory impairment when the Hearing Handicap Inventory for the Elderly score was taken into consideration. For the confidence level reported by the participants, main effects of volume (F2,90 = 32.98, P < .001, η2 = 0.42), repetition (F1,45 = 21.85, P < .001, η2 = 0.32), and category (F1,45 = 9.71, P = .003, η2 = 0.16) emerged after controlling for the Hearing Handicap Inventory for the Elderly score, indicating that the confidence was higher in the visually impaired group compared with the dual sensory impairment participants at higher volumes and with increased number of repetitions (Fig. 3).
FIGURE 2.
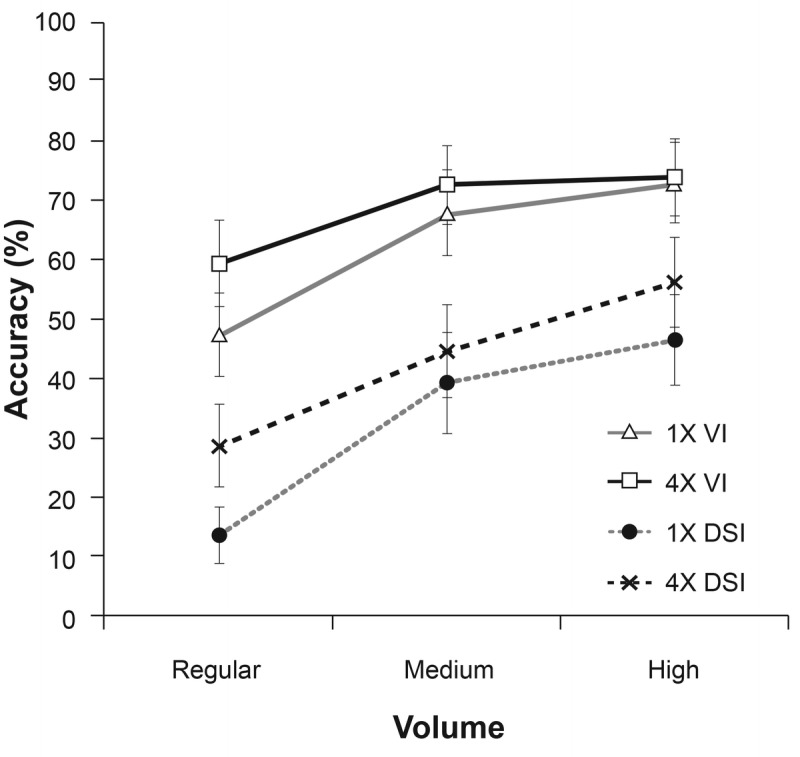
Accuracy of responses in visually impaired and dual-impaired participants using the talking watch. Because the patterns were similar in other devices, results for the calculator or the scanner are not presented here. Accuracy improves with an increased number of repetitions but more so at lower volumes. 1× = one stimulus presentation; 4× = four stimulus presentations; DSI = dual sensory impairment; VI = visual impairment.
FIGURE 3.
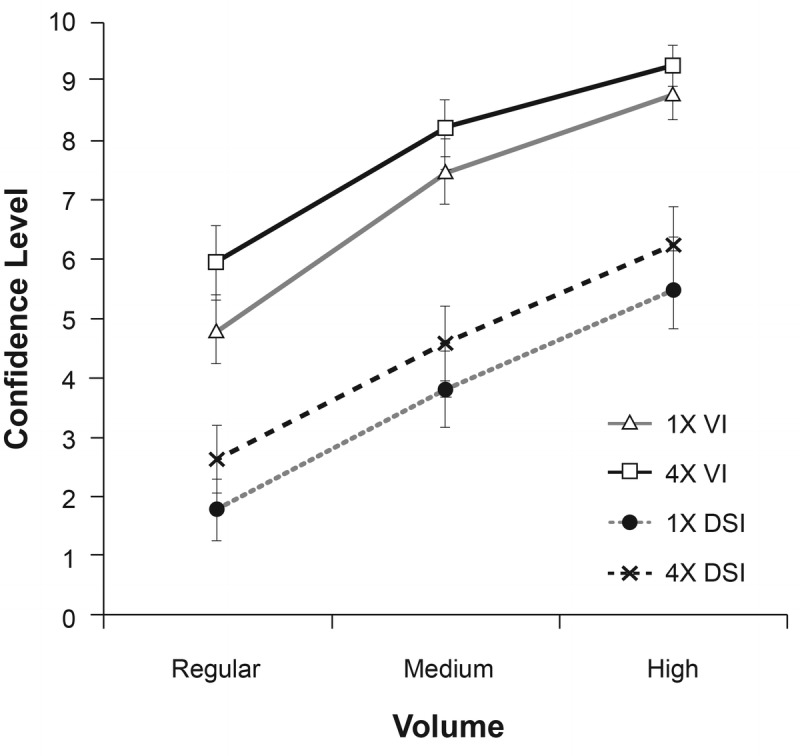
Confidence level of responses in visually impaired and dual-impaired participants using the talking watch. Because the patterns were similar in other devices, results for the calculator or the scanner are not presented here. The confidence was higher in the visually impaired group compared with the dual sensory impairment participants at higher volumes and with increased number of repetitions. 1× = one stimulus presentation; 4× = four stimulus presentations; DSI = dual sensory impairment; VI = visual impairment.
Calculator
A three-way mixed within-between analysis of covariance was conducted to examine difference in accuracy across levels of volume and repetition in both visually impaired participants and individuals with dual sensory impairment, after controlling for survey scores. An interaction of volume and repetition was obtained for the accuracy (F2,74 = 13.55, P < .001, η2 = 0.27), demonstrating that the scores improved with an increased number of repetitions, and more importantly at lower volumes. Scores did not differ significantly between the two groups. For confidence scores, an interaction of volume and repetitions was obtained (F2,70 = 7.10, P = .002, η2 = 0.16) after controlling for the Hearing Handicap Inventory for the Elderly scores, indicating that confidence improved with an increased number of repetitions and at higher volumes. Confidence did not differ between the two groups after controlling for the Hearing Handicap Inventory for the Elderly scores.
Scanner
An interaction of volume and repetition was obtained for accuracy (F2,94 = 4.78, P = .01, η2 = 0.09), indicating that the score improves with an increased number of repetitions, this effect being more important at lower volumes. A main effect of the category was also noted, indicating that the accuracy was overall lower in participants with dual sensory impairment (F1,47 = 4.74, P = .04, η2 = 0.09). An interaction of volume and repetition was obtained for confidence scores (F2,94 = 18.05, P < .001, η2 = 0.27), indicating that the score improved with an increased number of repetitions, this effect being more pronounced at higher volumes. A main effect of category was noted, indicating that the confidence was overall lower in participants with dual sensory impairment (F1,47 = 4.74, P = .02, η2 = 0.11). A complete summary of all pairwise comparisons is provided in Appendix Table A1, the pairwise comparisons, available at http://links.lww.com/OPX/A397.
DISCUSSION
The main goal of the present study was to investigate the audibility of three low vision assistive technology devices with speech output (watch, calculator, and scanner) in a population of older adults with acquired visual or dual sensory impairment. We measured the ability to complete a series of tasks, asking participants to repeat what they heard when using these devices at increasing levels of volume and repetition of the signal. In addition, we measured the accuracy of their answers and their confidence in responding correctly. The proportion of all participants who were able to complete our tasks under conditions that resemble device use because it is often observed in a client's home with the regular volume output of the device (i.e., either one or four repetitions at the lower volume) ranged from 0 to 15% in the visually impaired group and was 0% in the dual sensory impairment group. These results indicate that not only were individuals with dual sensory impairment unable to complete the tasks, but visually impaired individuals with age-normal hearing experienced difficulty as well. The audibility of the low vision assistive technology devices tested is compromised in older individuals with visual impairment, and these devices might not be the most suitable aids to be prescribed to this population or would require additional volume adjustment options. In addition, we demonstrated that increased volume and number of repetitions lead to better accuracy and confidence among both groups. Therefore, we propose that individuals with dual sensory impairment would benefit from aids with larger volume control options. However, the results seemed to reach a plateau, giving the impression that increasing volume can only improve results up to a point. We speculate that, given the nature of the hearing loss, the sounds presented remain distorted for the listener, and the tasks still present a challenge. Interestingly, the observed differences in audibility between the two groups were rendered nonsignificant in some conditions when controlling for participants' subjective judgment of their own hearing difficulties using the Hearing Handicap Inventory for the Elderly questionnaire. This finding leads us to believe that the self-perceived level of hearing difficulty is an important factor to consider during the device recommendation process. Rehabilitation professionals may benefit from systematically evaluating subjective hearing difficulty when choosing vision rehabilitation devices that use speech output.
Accessibility and Technology
Previous studies examined the usability of a device by focusing on the interaction between the user, the device, and the environment.29–31 The International Standards Organisation defines the usability of a device through three elements: effectiveness (accuracy and completion of the task), efficiency (ratio between benefit of use and time, effort, effectiveness, and cost), and satisfaction (as subjectively reported by the user).29 In addition, the concept of universal accessibility stipulates that an aid should be usable and accessible to people of all ages and abilities (with their respective disabilities) and with little adaptation.30 These principles were created specifically to achieve universal accessibility with the ultimate goal to design and create aids that can be used by a heterogeneous population in terms of disability type and severity. Some authors suggested that, instead of applying the concept of universal accessibility, developers should use a more dynamic approach, therefore adapting the design of systems and interfaces to an evolving population with different needs, abilities, and degree of disability.31 This new concept is called the “user-sensitive inclusive design” and encourages devices to be made for a population with a wider range of characteristics instead of targeting a category of disability.31
In the case of the devices used in our study, these assistive technology devices should be able to present spoken information that is perceivable and comprehensible by everyone. In general, the number of systematic and rigorous studies that have addressed the interaction between assistive technology devices and the users (usability and/or effectiveness) remains very limited, whereby those that specifically examine vision and hearing impairment technology are even sparser.18,32 One such study reviewed assistive technology devices in the context of Internet access for the population with dual sensory impairment.33 The main conclusion was that the devices and approaches that are currently available were not fully adequate, although they improved access. Another concern was that all the studies reviewed simulated dual sensory impairment to test for the effectiveness of the assistive technology devices (e.g., individuals with normal vision and hearing thresholds were tested) instead of directly considering and involving the users themselves.33 This problem has previously been reported qualitatively by individuals with dual sensory impairment who feel excluded and want to be consulted in the development of technology that can benefit their needs.34 In addition, members of this research team have previously investigated the usability of auditory assistive technology devices among a low vision population.24 Their conclusions were that the usability varied widely depending on the device, the instructions provided to use the device, and the complexity of the task. The authors not only suggested several adaptations to the devices themselves but also proposed improvements to the rehabilitation process and device introduction by clinicians to devices users. For example, they suggested additional practice, task repetition, and proper instructions as winning strategies.
Confidence
Usability is generally tested separately from the user's satisfaction with the use of a device, and confidence in its use is rarely addressed. As for satisfaction, subjective measures of usability have mostly been investigated through validated satisfaction questionnaires, which was not the case in the present study.32 However, confidence in using an aid could contribute to better satisfaction. In the present study, success, accuracy, and confidence levels were investigated whereby confidence generally increased with accuracy in both groups; we can thus expect a better confidence level with effective use of assistive technology devices. From a clinical standpoint, this might translate into a decrease in the abandonment rate of an assistive technology device and an increase in general satisfaction levels with a device. Future studies should include measures of confidence in the outcome of a device and its use, to better reflect the user experience and guide future device development.
Aging and Technology
Technology is developing fast, but very little information on the interaction between new technology and its target users is available. In the present study, most users were older adults with acquired sensory impairment. The normal aging process is characterized by changes in the physical, mental/cognitive, and sensory states, which can modify the interaction with technology.10 Previous research has indicated that engineers and designers should be able to not only understand the functionality and usability of a product but also better comprehend users' capacities and confidence in using any given product.31 Older adults of today are more likely to abandon a product or an aid that is too demanding.31 Research has shown that among the predictors of assistive technology device abandonment are poor performance of the device and changes in the needs or priorities of the user.35 Poor success in using an aid and little accuracy and confidence are thus more likely to lead to aid abandonment in older adults.
A recent study investigated the approach and use of technology by older hearing-impaired individuals.36 The authors suggested adapting the approach depending on the clients' attitudes toward technology; however, attitudes of the participants were generally positive toward the use of technology for their rehabilitation. In addition, the authors noticed that aids that required a certain level of hearing ability, such as music players or home security systems with an auditory modality, were less likely to be used by their hearing-impaired participants. The authors concluded that one should not use a universal but more client-centered approach that is individualized and oriented toward the needs and priorities of each user. These results might not generalize to an older population with age-related hearing loss because most participants in their study had been hearing impaired since childhood. They indeed could have been exposed to assistive technology devices at a younger age, and this likely influenced their attitudes toward and experience with technology.
Limitations and Future Directions
The present findings need to be considered within certain limitations. Originally, it was intended to compare the outcome of devices with female and/or male artificial voices. It is indeed known that higher pitches are generally more difficult to understand by individuals with age-related acquired hearing impairment, given their predominant loss in the upper frequencies.37 However, only assistive technology devices with female voices were chosen because the study was conducted both in French and in English, and the only assistive technology devices available in both languages were those with female voices. Therefore, it is possible that the use of devices with male voices may result in improved success, accuracy, and confidence. The calculator voice was not available in French, and therefore, the available data were reduced for this particular device. In addition, the texts used for the scanner were very short phrases, devoid of context, making the task more difficult and highlighting the importance of contextual cues for comprehension. Future investigations should include a control group whose sensory capacities are within age-expected norms and should include a group of individuals with hearing loss only. In addition, our findings may not generalize to younger individuals with sensory loss, those with lifelong impairments, and other assistive technologies with speech output. Finally, we had intended to test the devices in a context that would compare to everyday use. However, to facilitate the testing and manipulation of the sound output, we decided to record the devices, speculating that having access to visual cues would not affect our results. For example, none of our devices provided facial information on a screen to facilitate speech recognition. Numerous studies have shown that adding a visual component, such as a video of the person speaking, could have a tremendous benefit for understanding speech, both in adults with normal hearing and in those with hearing impairment who were using cochlear implants.38–40 Individuals with profound hearing loss do not seem to benefit as much of auditory-visual speech perception.39 The impact of visual cues in speech perception has also been shown to be more important when the sound is distorted, for example, with background noise, or when the target is unfamiliar.39 However, these studies seem to consider normally sighted individuals only. An alternative strategy might be to provide a scrolling text display on a device in addition to speech output; however, we are not aware of any research comparing hearing abilities when additional written information is provided.
CONCLUSIONS
The results indicated that the audibility of vision rehabilitation assistive technology devices with speech output used in this study depended on whether participants had concurrent hearing loss. In addition, scores and confidence levels being very low in both participant groups suggest that even those with normal hearing for their age experienced a certain level of difficulty understanding artificial speech output. Future device design needs to improve audibility for assistive technology devices whose usefulness depends on speech output comprehension. We hope that this study will raise awareness among researchers and clinicians alike when choosing and referring aids for older low vision patients who have a concurrent hearing loss. Our data suggest that the specific aids tested here are only of limited use for older individuals with dual sensory impairment. Accuracy and confidence will need to be tested during the rehabilitation process to confirm the usability of a device. Clinicians and researchers should also keep in mind that hearing is naturally reduced as a result of the aging process, specifically in the higher frequencies, and even individuals with age-normal hearing abilities can potentially experience difficulty in using low vision aids with speech output.
Supplementary Material
Footnotes
Supplemental Digital Content: Appendix Figure A1, an image of the Tel Time Talking Watch, is available at http://links.lww.com/OPX/A394.
Appendix Figure A2, an image of the 10-digit Talking Calculator, is available at http://links.lww.com/OPX/A395.
Appendix Figure A3, and image of the Optelec ClearReader+ Basic talking scanner, is available at http://links.lww.com/OPX/A396.
Appendix Table A1, the Pairwise Comparisons, is available at http://links.lww.com/OPX/A397.
Funding/Support: Centre for Interdisciplinary Research in Rehabilitation (to WW).
Conflict of Interest Disclosure: None of the authors have reported a financial conflict of interest.
Study Registration Information: CRIR-11650716.
Author Contributions and Acknowledgments: Conceptualization: LS-A, WW; Data Curation: LS-A, JJ; Formal Analysis: LS-A, JJ, WW; Funding Acquisition: WW; Investigation: LS-A, WW; Methodology: LS-A, JJ, WW; Project Administration: JJ, WW; Resources: WW; Software: JJ, WW; Supervision: WW; Writing – Original Draft: LS-A, WW; Writing – Review & Editing: WW.
We would like to thank Jonathan Jarry, Alexandre Beaulieu, and Jérémie Voix, as well as the Institut Raymond-Dewar, the Institut Nazareth et Louis Braille, and the MAB-Mackay Rehabilitation Centre.
Supplemental Digital Content: Direct URL links are provided within the text.
REFERENCES
- 1.Guthrie DM, Declercq A, Finne-Soveri H, et al. The Health and Well-being of Older Adults with Dual Sensory Impairment (DSI) in Four Countries. PLoS One 2016;11:e0155073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guthrie DM, Davidson JGS, Williams N, et al. Combined Impairments in Vision, Hearing and Cognition Are Associated with Greater Levels of Functional and Communication Difficulties than Cognitive Impairment Alone: Analysis of interRAI Data for Home Care and Long-term Care Recipients in Ontario. PLoS One 2018;13:e0192971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry P, Mascia J, Steinman BA. Vision and Hearing Loss in Older Adults: “Double Trouble.” Care Manag J 2004;5:35–40. [DOI] [PubMed] [Google Scholar]
- 4.Saunders G, Echt KV. An Overview of Dual Sensory Impairment in Older Adults: Perspectives for Rehabilitation. Trends Amplif 2007;11:243–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalton DS, Cruickshanks KJ, Klein BE, et al. The Impact of Hearing Loss on Quality of Life in Older Adults. Gerontologist 2003;43:661–8. [DOI] [PubMed] [Google Scholar]
- 6.Boothroyd A. Adult Aural Rehabilitation: What Is It and Does It Work? Trends Amplif 2007;11:63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klaver CC, Wolfs RC, Vingerling JR, et al. Age-specific Prevalence and Causes of Blindness and Visual Impairment in an Older Population. Arch Ophthalmol 1998;116:653–8. [DOI] [PubMed] [Google Scholar]
- 8.Congdon NG, Friedman DS, Lietman T, et al. Important Causes of Visual Impairment in the World Today. JAMA 2003;290:2057–60. [DOI] [PubMed] [Google Scholar]
- 9.Bowling B. Kanski's Clinical Ophtalmology: A Systematic Approach. 8th ed Philadelphia: Elsevier; 2016. [Google Scholar]
- 10.Wittich W, Gagné JP. Perceptual Aspects of Gerontechnology. In: Kwon S, ed. Gerotechnology: Research, Practice and Principles in the Field of Technology and Aging. New York: Springer Publishing Company; 2016:13–34. [Google Scholar]
- 11.Gagné JP, Wittich W. Visual Impairment and Audiovisual Speech-perception in Older Adults with Acquired Hearing Loss. In: Hickson L, ed. PHONAK Conference on Hearing Care for Adults 2009—The Challenge of Aging. Stafa, Switzerland: Phonak; 2010:165–77. [Google Scholar]
- 12.Brennan M, Bally SJ. Psychosocial Adaptations to Dual Sensory Loss in Middle and Late Adulthood. Trends Amplif 2007;11:281–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wittich W, Watanabe DH, Gagné JP. Sensory and Demographic Characteristics of Deafblindness Rehabilitation Clients in Montréal, Canada. Ophthalmic Physiol Opt 2012;32:242–51. [DOI] [PubMed] [Google Scholar]
- 14.Chia E-M, Mitchell P, Rochtchina E, et al. Association between Vision and Hearing Impairments and their Combined Effects on Quality of Life. Arch Ophthalmol 2006;124:1465–70. [DOI] [PubMed] [Google Scholar]
- 15.Oppegard K, Hansson RO, Morgan T, et al. Sensory Loss, Family Support, and Adjustment among the Elderly. J Soc Psychol 1984;123:291–2. [PubMed] [Google Scholar]
- 16.McDonnall MC. The Effects of Developing a Dual Sensory Loss on Depression in Older Adults: A Longitudinal Study. J Aging Health 2009;21:1179–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Viljanen A, Törmäkangas T, Vestergaard S, et al. Dual Sensory Loss and Social Participation in Older Europeans. Eur J Ageing 2013;11:155–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wittich W, Jarry J, Groulx G, et al. Rehabilitation and Research Priorities in Deafblindness for the Next Decade. J Vis Impair Blind 2016;110:219–31. [Google Scholar]
- 19.Damen GW, Pennings RJ, Snik AF, et al. Quality of Life and Cochlear Implantation in Usher Syndrome Type I. Laryngoscope 2006;116:723–8. [DOI] [PubMed] [Google Scholar]
- 20.Jolink C, Helleman HW, van Spronsen E, et al. The Long-term Results of Speech Perception in Elderly Cochlear Implant Users. Cochlear Implants Int 2016;17:146–50. [DOI] [PubMed] [Google Scholar]
- 21.Gaylord-Ross R, Park H-S, Johnston S, et al. Individual Social Skills Training and Co-worker Training for Supported Employees with Dual Sensory Impairment. Two Case Examples. Behav Modif 1995;19:78–94. [DOI] [PubMed] [Google Scholar]
- 22.McDonnall MC. The Effect of Productive Activities on Depressive Symptoms among Older Adults with Dual Sensory Loss. Res Aging 2011;33:234–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Statistique Canada. Bizier C, Contreras R. Visual Disabilities among Canadians Aged 15 and Over. 2012. Available at: https://www150.statcan.gc.ca/n1/pub/89-654-x/89-654-x2016001-fra.htm. Accessed July 10, 2018.
- 24.Wittich W, Southall K, Johnson A. Usability of Assistive Listening Devices by Older Adults with Low Vision. Disabil Rehabil Assist Technol 2016;11:564–71. [DOI] [PubMed] [Google Scholar]
- 25.Davis A, Smith P, Ferguson M, et al. Acceptability, Benefit and Costs of Early Screening for Hearing Disability: A Study of Potential Screening Tests and Models. Health Technol Assess 2007;11:1–294. [DOI] [PubMed] [Google Scholar]
- 26.Lichtenstein MJ, Bess FH, Logan SA. Validation of Screening Tools for Identifying Hearing-impaired Elderly in Primary Care. JAMA 1988;259:2875–8. [PubMed] [Google Scholar]
- 27.Wittich W, Phillips N, Nasreddine Z, et al. Sensitivity and Specificity of the Montreal Cognitive Assessment Modified for Individuals Who Are Visually Impaired. J Vis Impair Blind 2010;360–9. [Google Scholar]
- 28.Schulze-Bonsel K, Feltgen N, Burau H, et al. Visual Acuities “Hand Motion” and “Counting Fingers” Can Be Quantified with the Freiburg Visual Acuity Test. Invest Ophthalmol Vis Sci 2006;47:1236–40. [DOI] [PubMed] [Google Scholar]
- 29.International Standards Organisation (ISO). Ergonomic Requirements for Office Work with Visual Display Terminals (VDTs)—Part 11: Guidance on Usability: ISO 9241-11:1998. Geneva, Switzerland: ISO; 1998. [Google Scholar]
- 30.Story MF. Maximizing Usability: The Principles of Universal Design. Assist Technol 1998;10:4–12. [DOI] [PubMed] [Google Scholar]
- 31.Chong Lim CS, Newell AF. User-sensitive Inclusive Design for Technology in Everyday Life. In: Kwon S, ed. Gerontechnology. New York: Springer Publishing Company; 2017:157–79. [Google Scholar]
- 32.Lenker JA, Scherer MJ, Fuhrer MJ, et al. Psychometric and Administrative Properties of Measures Used in Assistive Technology Device Outcomes Research. Assist Technol 2005;17:7–22. [DOI] [PubMed] [Google Scholar]
- 33.Perfect E, Jaiswal A, Davies TC. Systematic Review: Investigating the Effectiveness of Assistive Technology to Enable Internet Access for Individuals with Deafblindness. Assist Technol 2018:doi:10.1080/10400435.2018.1445136. Available at: https://www.tandfonline.com/doi/full/10.1080/10400435.2018.1445136. Accessed March 29, 2019. [DOI] [PubMed] [Google Scholar]
- 34.Lejeune BJ. Aging with Dual Sensory Loss: Thoughts from Consumer Focus Groups. AER J 2010;3:146–52. [Google Scholar]
- 35.Phillips B, Zhao H. Predictors of Assistive Technology Abandonment. Assist Technol 1993;5:36–45. [DOI] [PubMed] [Google Scholar]
- 36.Singleton JL, Remillard ET, Mitzner TL, et al. Everyday Technology Use among Older Deaf Adults [published online March 2018]. Disabil Rehabil Assist Technol 2018. doi:10.1080/17483107.2018.1447609. Available at: https://www.tandfonline.com/doi/abs/10.1080/17483107.2018.1447609. Accessd February 15, 2019. [DOI] [PubMed] [Google Scholar]
- 37.Pisoni D, Remez R. The Handbook of Speech Perception. Malden: Blackwell Publishing; 2006. [Google Scholar]
- 38.MacDonald J, McGurk H. Visual Influences on Speech Perception Processes. Percept Psychophys 1978;24:253–7. [DOI] [PubMed] [Google Scholar]
- 39.Grant KW, Walden BE, Seitz PF. Auditory-visual Speech Recognition by Hearing-impaired Subjects: Consonant Recognition, Sentence Recognition, and Auditory-visual Integration. J Acoust Soc Am 1998;103:2677–90. [DOI] [PubMed] [Google Scholar]
- 40.Taitelbaum-Swead R, Fostick L. Audio-visual Speech Perception in Noise: Implanted Children and Young Adults versus Normal Hearing Peers. Int J Pediatr Otorhinolaryngol 2017;92:146–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


