Abstract
SIGNIFICANCE
Pregnancy-induced hypertension is a unique yet common complication in pregnant women and may cause retinopathy. Optical coherence tomography (OCT) may help find the features of retinopathy that are difficult to observe through fundus examination. Not all patients can fully recover from retinopathy.
PURPOSE
This report describes a case of pregnancy-induced hypertension with retinopathy and represents the features of retinopathy in OCT and fundus fluorescein angiography.
CASE REPORT
A 29-year-old pregnant woman presented with bilateral blurred vision and xanthopsia 2 days before her induced labor; she was also diagnosed as pre-eclamptic in the obstetrics department. The vision in her right eye was 20/33, and that in her left eye was 20/20. Fundus fluorescein angiography showed scattered-dot hypofluorescence around the disc at an early stage, and needle-like hyperfluorescence gradually appeared near the disc with late-stage fluorescein leakage in both eyes. Optical coherence tomography revealed multiple shallow retinal detachments with hyperreflective bright spots in the outer retina and clumped hyperreflective materials on the retinal pigment epithelium (RPE).
CONCLUSIONS
Typical findings and some tiny changes in the outer retina and RPE can be observed through spectral-domain OCT. The clumped hyperreflective deposits in the outer retina may be by-products of RPE swelling and necrosis that lead to barrier dysfunctions and fluid leakage. These described features may help diagnose retinopathy from pregnancy-induced hypertension. Although it is a self-limited disease, the disruptions in the ellipsoid and interdigitation zones may not fully recover and result in reduced visual dysfunction. Therefore, control of hypertension is indicated.
Pregnancy-induced hypertension is a common complication in pregnant women and occurs in 5 to 10% of pregnancies, with 32.5% of these patients developing retinopathy.1 It may take one of four forms, including chronic hypertension that predates pregnancy, pre-eclampsia/eclampsia, chronic hypertension with superimposed pre-eclampsia, and nonproteinuric gestational hypertension. Clinical and experimental studies suggest endothelial dysfunction as a major mechanism in pregnancy-induced hypertension.2
The manifestation of retinopathy in pregnancy-induced hypertension, such as thinning arteries, hemorrhage, exudation, and even retinal detachment, often occurs during late pregnancy.3 Optical coherence tomography may help to find subretinal fluid, photoreceptor irregularities, and lesions at the retinal pigment epithelium level, all of which are features that are difficult to observe through fundus examination.4
The purposes of this study were to report a case of pregnancy-induced hypertension with retinopathy and to present the features of retinopathy in optical coherence tomography and fundus fluorescein angiography. No identifiable health information was included in this case report.
CASE REPORT
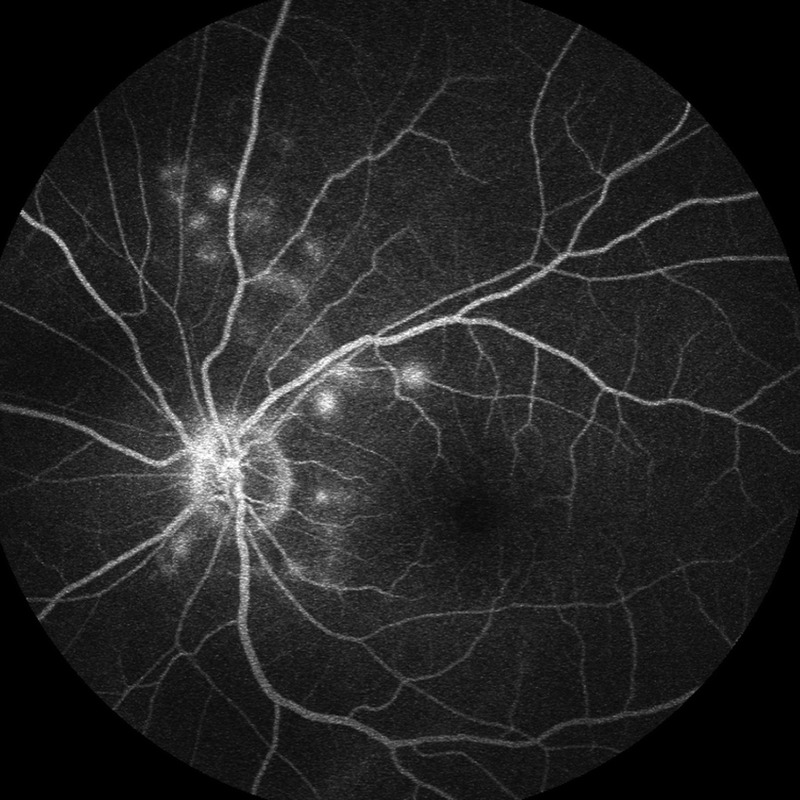
A 29-year-old pregnant Chinese woman presented with bilateral blurred vision and xanthopsia 2 days before induced labor at a gestational age of 22 weeks and 5 days. She was diagnosed as pre-eclamptic and admitted for an induced labor in the obstetrics department at First Affiliated Hospital of Dalian Medical University in China. Three days after her induced labor, this patient came to our department for ophthalmic examination. Her blood pressure was 150/100 mmHg. Her visions were 20/33 in the right eye and 20/20 in the left eye. The anterior segment examination results were normal. There was thinning of the retinal arteries with artery-to-vein ratios of 1:3 (Fig. 1).
FIGURE 1.
Clinical timeline: a 29-year-old Chinese pregnant woman diagnosed as having, and pharmaceutically treated for, retinopathy of PIH after induced labor. FFA = fundus fluorescein angiography; OCT = optical coherence tomography; PIH = pregnancy-induced hypertension; RPE = retinal pigment epithelium.
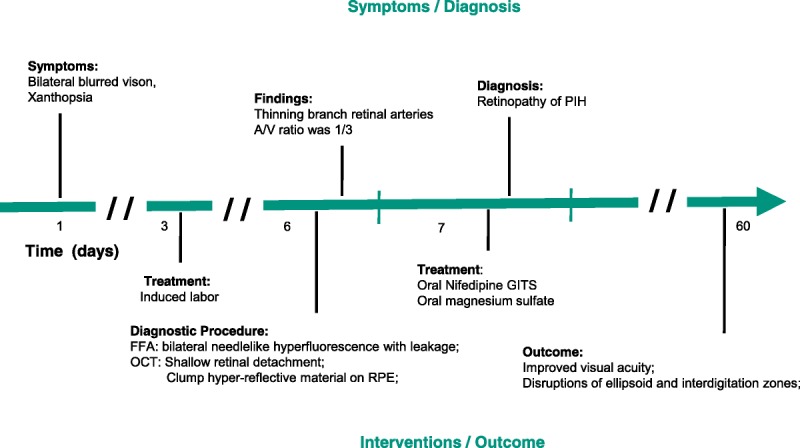
Fundus fluorescein angiography showed early-stage scattered-dot hypofluorescence (Fig. 2A) around the disc and needle-like hyperfluorescence gradually starting to appear in later stages in the right eye (Fig. 2B). The fluorescein angiography findings were similar in the left eye (Figs. 2C, D). Spectral-domain optical coherence tomography revealed multiple shallow retinal detachments with hyperreflective bright spots in the outer retina and clumped hyperreflective materials on the retinal pigment epithelium, consistent with the lesions in both eyes (Figs. 3A, C). No abnormalities were seen in a computed tomographic examination of the head.
FIGURE 2.
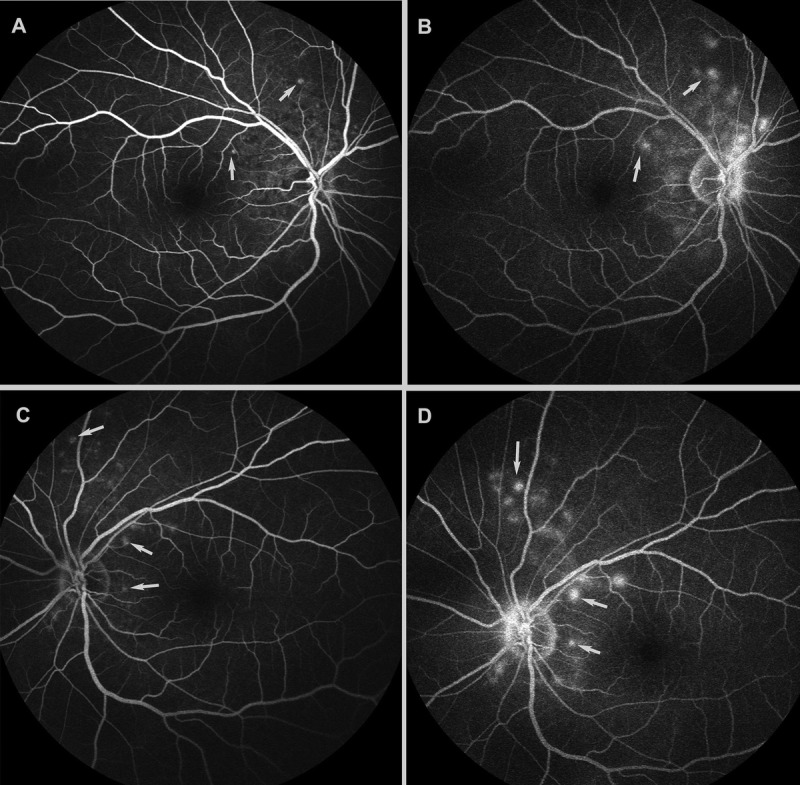
(A) Fundus fluorescein angiography showed scattered-dot hypofluorescence and needle-like early-stage hyperfluorescence (arrow) around the disc in the right eye. (B) Late-stage fluorescein leakage (arrow) in the right eye. (C) Fundus fluorescein angiography showed needle-like early-stage hyperfluorescence (arrow) around the disc in the left eye. (D) Late-stage fluorescein leakage (arrow) in the left eye.
FIGURE 3.
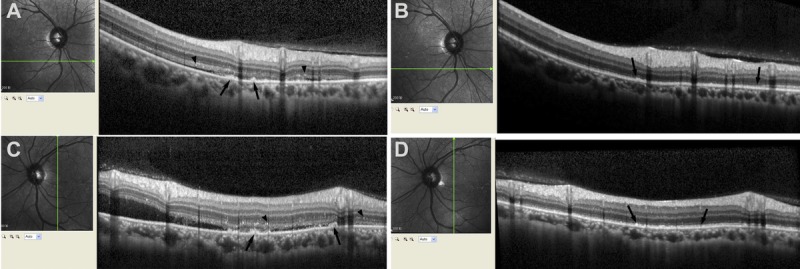
(A) Special-domain optical coherence tomography revealed shallow retinal detachment with hyperreflective bright spots (arrowheads) in the outer retina and clumped hyperreflective material (long arrow) on the retinal pigment epithelium in the right eye. (B) Disruptions in the ellipsoid and interdigitation zones (long arrow) in the right eye that persisted after treatment. (C) Special-domain optical coherence tomography revealed shallow retinal detachment with hyperreflective bright spots (arrowheads) in the outer retina and clumped hyperreflective material (long arrow) on the retinal pigment epithelium in the left eye. (D) Disruptions in the ellipsoid and interdigitation zones (long arrow) in the left eye that persisted after treatment.
The results of laboratory tests, including those for rheumatoid immune antibody, syphilis antibodies, human immunodeficiency virus, herpes simplex virus, hepatitis, and autoantibody such as antinuclear antibody, antimitochondrial antibody, and smooth muscle antibody, were normal. Urine protein quantitation was 11,294 mg/24 h. Serum albumin was 28.4 g/L, and total protein was 45.1 g/L, with serum b-type natriuretic peptide at 133.60 pg/mL and procalcitonin at 1.69 ng/mL. Serum D-dimer was 1180 μg/L.
The patient was clinically diagnosed as having pregnancy-induced hypertension and treated with nifedipine gastrointestinal therapeutic system and magnesium sulfate to control her blood pressure. She was followed up every 2 weeks, and the vision in her right eye improved to 20/25 after 1 month of therapy. Although the serous subretinal fluid resolved, the ellipsoid and interdigitation zones remained disorganized (Figs. 3B, D).
DISCUSSION
Pregnancy-induced hypertension is characterized by a blood pressure elevation after 20 weeks of gestation and is often accompanied by proteinuria.5 It may cause retinopathy, including arteriolar narrowing, hemorrhage, exudates, and even retinal detachment during late pregnancy.3 Researchers believed that retinal pigmented epithelial lesions and serous retinal detachments were secondary to choroidal ischemia.6,7 The optical coherence tomography features of this retinopathy have not been completely clarified. Researchers have found that patients with pregnancy-induced hypertension may have a circulation disorder that results in ischemia within the choroid. With fluorescein angiography, less or no choroidal fluorescence is seen.4 The present study discusses the tiny changes in the outer retina and retinal pigmented epithelium as observed in patients with pregnancy-induced hypertension through spectral-domain optical coherence tomography.
We speculate that the clumped hyperreflective deposits (Figs. 3A, C) in the outer retina may be secondary to retinal pigmented epithelial swelling and necrosis leading to deficiencies in their barrier functions. These pathological abnormalities ultimately lead to fluid leakage and shallow retinal detachment. Sato and Takeuchi4 believe that the multiple subretinal and epiretinal pigmented epithelium deposits with high brightness were proliferation and migration of the retinal pigmented epithelial cells as in uveal effusion syndrome. Similar to our case, these authors also state that malignant hypertension-induced ischemic retinal pigmented epithelial necrosis compromises the outer blood-retinal barrier leading to localized retinal pigmented epithelial detachment and serous retinal detachment.4 Altalbishi et al.8 report that the focal elevations of a thick, highly reflective retinal pigmented epithelium band, also called Elschnig spots, were believed to be a gradient of retinal pigmented epithelial damage where the cells were totally necrotic: as an ischemic retinal pigmented epithelium becomes edematous and necrotic, the outer blood-retinal barrier is disrupted, allowing for fluid leakage from the choroid into the subretinal space. These features, as found by optical coherence tomography, may help diagnose retinopathy from pregnancy-induced hypertension and potentially become one of the diagnostic criteria (Fig. 3).
Although most cases in the literature report a good visual prognosis, our patient had persistent disruption in the ellipsoid and interdigitation zones after treatment. These changes may not completely heal and result in a permanent loss of visual function. We advise aggressive treatment to preserve vision.
CONCLUSIONS
Both typical and small unusual outer retinal findings in pregnancy-induced hypertensive retinopathy may be imaged with spectral-domain optical coherence tomography. The clumped hyperreflective deposits in the outer retina may be secondary to retinal pigmented epithelial swelling and necrosis leading to altered barrier dysfunction and fluid leakage. These described features may help diagnose retinopathy from pregnancy-induced hypertension. Although this is a self-limited disease, the disruptions in the ellipsoid and interdigitation zones may not fully recover and result in reduced visual dysfunction. Therefore, control of hypertension is indicated.
Footnotes
Funding/Support: Foundation of Liaoning Educational Committee (LQ2017016; to XQ) and National Natural Science Foundation of China (81300779; to ZZ).
Conflict of Interest Disclosure: None of the authors have reported a financial conflict of interest.
Author Contributions: Data Curation: JL; Funding Acquisition: ZZ, XQ; Resources: XQ; Writing – Original Draft: ZZ; Writing – Review & Editing: JL, XQ.
REFERENCES
- 1.Rasdi AR, Nik-Ahmad-Zuky NL, Bakiah S, et al. Hypertensive Retinopathy and Visual Outcome in Hypertensive Disorders in Pregnancy. Med J Malaysia 2011;66:42–7. [PubMed] [Google Scholar]
- 2.Possomato-Vieira JS, Khalil RA. Mechanisms of Endothelial Dysfunction in Hypertensive Pregnancy and Preeclampsia. Adv Pharmacol 2016;77:361–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Errera MH, Kohly RP, da Cruz L. Pregnancy-associated Retinal Diseases and their Management. Surv Ophthalmol 2013;58:127–42. [DOI] [PubMed] [Google Scholar]
- 4.Sato T, Takeuchi M. Pregnancy-induced Hypertension Related Chorioretinitis Resembling Uveal Effusion Syndrome: A Case Report. Medicine 2018;97:e11572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Furuya M, Ishida J, Aoki I, et al. Pathophysiology of Placentation Abnormalities in Pregnancy-induced Hypertension. Vasc Health Risk Manag 2008;4:1301–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saito Y, Tano Y. Retinal Pigment Epithelial Lesions Associated with Choroidal Ischemia in Preeclampsia. Retina 1998;18:103–8. [DOI] [PubMed] [Google Scholar]
- 7.Sathish S, Arnold JJ. Bilateral Choroidal Ischaemia and Serous Retinal Detachment in Pre-eclampsia. Clin Exp Ophthalmol 2000;28:387–90. [DOI] [PubMed] [Google Scholar]
- 8.Altalbishi A, Khateb S, Amer R. Elschnig's Spots in the Acute and Remission Stages in Preeclampsia: Spectral-domain Optical Coherence Tomographic Features. Eur J Ophthalmol 2015;25:e84–7. [DOI] [PubMed] [Google Scholar]


