Abstract
Purpose of review
Epidemiological studies associate city living with an elevated psychosis risk. Urban (social/economic) stress and exposure to environmental toxins, pollution or disease agents have been proposed to underlie this association. This review provides an update on the recent evidence (May 2017 – November 2018).
Recent findings
Of 647 screened studies, 17 on: urbanicity–psychosis associations in worldwide high, middle and low-income countries; explanatory mechanisms, including nature exposure, social and economic stressors and genetic risk; urbanicity effects on the brain and coping; and urbanicity and resources, were included. The reviewed evidence revealed complex patterns of urbanicity–psychosis associations with considerable international variation within Europe and between low, middle and high-income countries worldwide. Social and economic stressors (e.g. migration, ethnic density and economic deprivation), nature exposure and access to resources could only explain part of the urbanicity effects. Risk factors differed between countries and between affective and non-affective psychosis.
Summary
Urbanicity–psychosis associations are heterogeneous and driven by multiple risk and protective factors that seem to act differently in different ethnic groups and countries. Interdisciplinary research combining approaches, for example from experimental neuroscience and epidemiology, are needed to unravel specific urban mechanisms that increase or decrease psychosis risk.
Keywords: green space, psychosis, schizophrenia, social determinants, urbanicity
INTRODUCTION
Well-controlled epidemiological studies show elevated rates of psychotic disorders in densely populated areas [1,2]. Fifty-five per cent of today's world population lives in urban areas and further urbanization is expected in the next decades [3]. The topic of urbanicity and mental health is therefore vital and timely [4▪,5,6]. Previous research associated psychosis risk with urban birth [7,8] upbringing [9,10], and current city living [11,12]. Explanations were sought in characteristics of the urban environment that reflect social stressors and socio-environmental adversity [1], which are increased by low social cohesion and high deprivation (e.g. low income, employment and education), inequality and social fragmentation [13–19]. In addition, lack of green space in itself or as proxy for urban stress, environmental pollution and toxin exposure has been suggested to increase risk [20]. Urban factors may do most harm in individuals with a genetic liability for psychosis. Yet, it has also been proposed that particularly those at risk might be drawn toward city living [21]. Knowledge about urban risk factors is crucial to enable urban designs that mitigate risk. Here we review the recent literature on the link between urbanicity and psychosis.
Box 1.
no caption available
MATERIAL AND METHODS
Search strategy and study selection
We conducted a systematic literature search in the online databases PsycINFO, Embase and PubMed, covering May 2017 until November 2018. Search terms were: ‘urbanicity’ or ‘urban population’ or ‘green space’ or ‘nature’ or ‘urban area’ or ‘urbanisation/urbanization’ or ‘population density’ and ‘psychosis’ or ‘psychoses’ or ‘psychotic disorder’ or ‘schizophrenia’ or ‘schizophrenia spectrum disorder’ or ‘delusion’ or ‘hallucination’ or ‘paranoia’.
Reference lists of key studies were inspected for additional articles. Studies were included if they: were written in English; peer-reviewed; included patients with a self-reported or clinically assessed diagnosis of a (non-affective or affective) psychotic disorder; and assessed urbanicity effects (i.e. associations with population density). Studies were excluded if they were reviews, doctoral theses/dissertations or book chapters or reported only subclinical psychotic experiences/subclinical symptoms in the general population. We identified 647 unique articles. Titles and abstracts were screened by I.L.J. Eighty-five articles were eligible and the full text was assessed by I.L.J. and was discussed by I.L.J. and A.K.F., resulting in 17 included studies (see Fig. 1).
FIGURE 1.
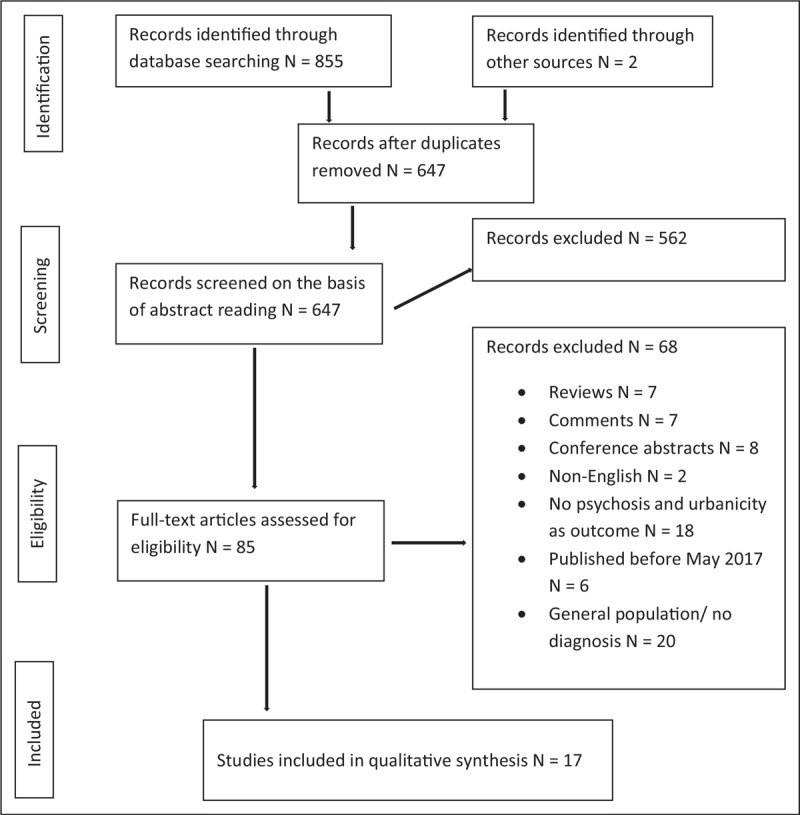
Flow diagram for the inclusion of articles for this review.
RESULTS
Urbanicity and psychosis risk
Five studies on worldwide urbanicity–psychosis associations yielded mixed findings. Data from a large Danish, male-only sample associated urban birth and moving toward higher urbanicity before age 10 with elevated risk for schizophrenia spectrum disorders in adulthood [22]. The association with urban birth was most robust and remained significant after adjustment for IQ, social class, parental education, familial psychiatric history and second-generation migrant status. Schofield et al.[23] confirmed the association between urbanicity exposure at age 15 and the risk for non-affective psychosis in native Danes, but not in migrants from Africa, Asia, Europe or the Middle East. A European multicentre study by Jongsma et al.[24▪▪] showed no significant overall association between urbanicity and the incidence of psychosis. However, analyses by country revealed significant associations between urbanicity and higher psychosis risk in the United Kingdom and the Netherlands, but not in France, Italy and Spain [24▪▪]. Data from the United Kingdom also indicated that individuals with first episode psychosis (FEP) are more likely to reside in urban areas compared to the general population [25]. Urban living was also found to be associated with elevated schizophrenia risk in China [26] and WHO Survey data from several low and middle-income countries (LMIC) revealed a higher risk for psychotic disorders (self-report) with urbanicity in Estonia. However, a lower psychosis risk with higher urbanicity was present in Mali, Senegal and the Philippines. The overall association was nonsignificant [27▪▪].
Urbanicity, symptoms and hospitalization
Across different European sites, urban living was associated with higher general, negative, disorganized, and manic symptoms in FEP. Interestingly, urbanicity was associated with higher positive and negative symptoms in the United Kingdom and lower positive and negative symptoms in Spain. No such associations were present in the Netherlands, France or Italy [28]. On the Italian island of Sardinia, lower hospitalization rates for schizophrenia and other psychiatric disorders have been found for individuals from towns with more than 10,000 residents than for individuals from smaller municipalities (7.1 vs. 9.3/1,000) [29].
Explaining the urbanicity–psychosis association
Twelve studies examined possible explanatory mechanisms of the urbanicity–psychosis link. Two studies investigated coping with urbanicity and the associations between urbanicity and the brain.
Urbanicity, social and economic mechanisms
Several social and economic mechanisms might account for the urbanicity–psychosis link. Four studies showed that migrants/ethnic minorities have a higher psychosis incidence than native populations [23,24▪▪,25,30]. Although migrant or ethnic minority status has been suggested as underlying factor of urbanicity effects, Schofield et al.'s [23] findings implicate a more complicated relationship. Only after ethnic density (i.e. concentration of a particular group in an area) was included in the analysis, psychosis risk was elevated for European and the Middle Eastern, but not for Asian or African migrants. Thus in some groups, urbanicity–psychosis associations appear when ethnic density is low [23]. Kirkbride et al.[25] showed that regardless of urbanicity, Black-Caribbean, African and Pakistani, but not Arabic or Bangladeshi minorities have a higher psychosis risk. Another investigation [30] used the same data to disentangle effects of urbanicity, racial/ethnic diversity, – density and – fragmentation, economic deprivation and social isolation on psychosis risk. Economic deprivation, social isolation and urbanicity emerged as independent risk factors when ethnicity was accounted for. Some patterns of urban risk differed for affective and non-affective psychosis, with increased risk in rural areas for some groups (see Table 1) [25,30]. In the European multicentre study [24▪▪], psychosis risk was not significantly associated with urbanicity when ethnic minority status, owner occupancy of housing, household status (single person) and unemployment were accounted for; with similar patterns for affective and non-affective psychosis.
Table 1.
Key characteristics of the included studies
| References | Country | Urban factor | Diagnosis | Sample | Covariates | Methods | Results | |
| 1 | Bocchetta and Traccis [29] | Italy | Population size of the municipalities | Schizophrenic syndromes; paranoia and delusional syndromes; bipolar and depression | 16,305 hospital records (between 1901 and 1964) | Lower hospitalisation rates (schizophrenia, depression, bipolar) in towns with more than 10,000 inhabitants (7.1/1,000) as compared to smaller villages (9.3/1,000) | ||
| 2 | Boers et al. [35] | The Netherlands | Green and blue space in % within a circular buffer of 300 m centred on patient's home address | Schizophrenia spectrum and other psychotic disorders, DSM-IV | 1,245,294 inhabitants in Utrecht area, 0.4% with diagnosis of schizophrenia; 623 hospitalised cases with inpatient visits between 2008 and 2016, male 70% mean age 38; age range 11–94 | Age, sex, urbanicity (address density), socio-economic status (residential property value) | χ2 for group differences, multivariate regression analysis on length of hospital stay | Ca. 65% of patients had no green space near their home. Patients had a significantly lower amount of green space in their neighbourhoods compared to the general population. No differences regarding blue space. Green or blue space in neighbourhood was not associated with length of hospital stay of patients |
| 3 | DeVylder et al. [27▪▪] | 42 countries (17 low income, 25 middle income) | Urban or rural residence (dichotomized, in line with united nations urbanization prospects report) | Self-reported lifetime history of a psychotic disorder | 215,682 (86,437 low and 129,245 middle); 49.2% male, mean age 37.9 (SD 15.7); individuals with psychotic disorder (0.9%) | Age, sex and country | Multivariable logistic regression | Positive association between urban residence and psychosis in Estonia (OR = 12.17). Negative association between urban residence and psychosis in Mali, Senegal and the Philippines (OR = 0.28–0.42). Overall, no significant association of urban residence with psychosis in low and middle-income countries (OR = 0.92) |
| 4 | Engemann et al. [34▪▪] | Denmark | Green space (based on normalised difference vegetation index), urbanization: capital, capital suburb, provincial city, provincial town, or rural areas | Schizophrenia spectrum disorders (ICD-8, ICD-10) | 943,027 (born 1985–2003 followed until 2013); 7,609 schizophrenia spectrum disorder; 3,748 schizophrenia | Urbanization, year of birth, sex, SES (parents’ education, income and employment status) | IRR estimated using Cox regression | Incidence ratio of schizophrenia spectrum disorder was higher with lower mean green space exposure at age 10 (IRR = 1.52). Effects sizes were smaller when adjusted for urbanization and socioeconomic status. The strongest protective association was observed during early childhood |
| 5 | Frissen et al. [38▪] | The Netherlands, (including some Belgian participants) | Average population density per square kilometre (three levels low, medium and high) conform Dutch Central Bureau for statistics and equivalent Belgian database urbanicity rating, urban exposure from 0–14 years | Non-affective psychosis (diagnosed by clinician) | 89 patients, 95 siblings and 87 control subjects, mean age 29.5; age range 16–50, male 38–67% | Sex, age, educational level, cannabis use, childhood trauma total intracranial volume and scan type | Multilevel random linear regression analyses and MRI | Only male patients showed a negative association between grey matter volume and urbanicity exposure during childhood |
| 6 | He et al. [31] | China | Rural-urban dichotomy | Schizophrenia diagnosis self-report/family members’ reports and on-site psychiatrist diagnosis (ICD-10) | 387,093 adults born 1956–1965. Rural: 239,055; Urban: 148,038, male: 50.1 vs. 50.3% | Sex, ethnicity (minority), marital status, education, annual family income per capita | Logistic regression | Schizophrenia rates were 0.45% in the rural group and 0.42% in the urban group. Famine cohorts (1959–1962) had significantly higher odds (OR = 1.84) of schizophrenia than reference cohort of 1965 in the rural population, even after adjusting for multiple covariates (OR = 1.82). No statistically significant differences between famine and reference cohort were found in the urban population |
| 7 | Hou et al. [32] | China | Rural–urban dichotomy based on care in metropolitan and small town primary care services | Schizophrenia DSM-IV or ICD-10 | 1,365,742 rural and 623 urban patients, male 61% vs. 57%, age = 39.9 vs. 49.1 | χ2 for group differences | More patients in rural than urban areas were antipsychotic free (35.4 vs. 17.5%) | |
| 8 | Jongsma et al. [24▪▪] | England, The Netherlands, France, Italy, Spain and Brazil | Population density based on pp/km2 | First episode nonorganic psychotic disorders (affective and nonaffective), ICD-10 | European network of national Schizophrenia networks studying Gene–Environment Interactions (EU-GEI): 2,774 cases (78.7% non-affective psychosis, 19.9% affective psychosis), age range 18–64; male 49.5%, 23.9% ethnic minority background | Age, sex, racial/ethnic minority status, setting level variables | Poisson regression | Substantial variation in incidence of FEP with no overall effect of urbanicity (IRR = 1.01). Ethnic minorities had a higher incidence of psychosis than the majority group (IRR = 1.59). Psychosis risk was not significantly associated with population density when ethnic minority status, owner occupancy of housing, household status (single person) and unemployment were accounted for (IRR = 1.01, 1.59, 0.76, 1.06, 0.90). Separate analysis for affective and non-affective psychosis showed that population density did not predict psychosis risk when minority status, unemployment and owner-occupancy were included in the statistical models. Analysis by country associated urbanicity with increased risk for psychosis in Northern European but not Southern European countries (IRR = England 1.17; the Netherlands 1.89; Spain 1.01; France 1.01; Italy 0.72; adjusted for age, sex, their interaction, minority status and owner-occupancy) |
| 9 | Kirkbride et al. [25] | United Kingdom (East Anglia) | Rural–urban dichotomy defined as less or more than 8,000 pp/km2 | FEP, ICD-10 | Social Epidemiology of Psychoses in East Anglia (SEPEA), 687 (identified between 2009 and 2013, 83.4% non-affective psychosis, 50.9% schizophrenia), age range 16–35 years, male 66.8%, white British 74.8% | Age, sex, age × sex, SES, population density, deprivation | Poisson regression | Cases more likely to reside in urban areas than population at risk. Increased rates of non-affective psychosis and schizophrenia in ethnic minorities adjusted for population density and other confounders (IRR = Pakistani 2.31; Black African 4.06, Black Caribbean 4.63, mixed 1.71). No urban–rural risk differences in these or non-British white or other ethnic groups after adjustment for confounders. Patterns for overall psychosis and non-affective psychosis were similar. For some groups (Pakistani, Bangladeshi, non-British white and other ethnicities) with affective psychosis a higher risk was present in rural areas |
| 10 | Paksarian et al. [37▪] | Denmark | Urbanicity at birth and at age 15. Five levels urbanicity: capital, capital suburb, provincial city (>100,000 residents), provincial town (>10,000 residents), and rural areas | Schizophrenia ICD-8 and ICD-10 | Urban birth (1981–2000): 1,549 matched pairs of cases and controls; median age 20 (IQR = 3.9), male 55.5%; urbanicity at age 15: 1,456 complete pairs | Age, sex, date of birth, PRS/10 principal components, parental psychiatric history | Conditional logistic regression | After adjustment for confounders PRS not associated with greater odds of being born in the capital vs. rural area (OR = 1.09), but associated with odds of residing in the capital at age 15 (OR = 1.19). Adjustment for PRS did not change association between schizophrenia and urbanicity at birth (IRR = 1.67) and slightly attenuated association with urbanicity at age 15 (IRR = 1.47). After confounders were controlled, the association between urban birth and schizophrenia remained significant (IRR = 1.54) |
| 11 | Quattrone et al. [28] | The Netherlands, England, France, Italy, Spain and Brazil | Population density based on pp/km2 | ICD-10/RDC: schizoaffective disorder (35%), schizophrenia spectrum (38.6%), unspecified psychotic disorder (16.3%), affective psychosis (10.1%) | EU-GEI study; 2,182 incident cases recruited between 2010 and 2015, mean age 32.1 (SD 11.2); age range 18–64, male 57%, white 57.1% | Sex, age-at-first-contact, ethnicity, diagnosis and assessment method | Multiple linear regression with urbanicity as continuous variable | Urbanicity was associated higher general symptoms, negative symptoms and disorganized symptoms. Analysis by country showed that in the United Kingdom urbanicity was associated with more positive/negative symptoms, whereas in Spain it was associated with less positive/negative symptoms |
| 12 | Richardson et al. [30] | United Kingdom | Urbanicity variable based on factor analysis with positive load on population density, and negative load on green space, nondomestic building and travel times | Non-affective and affective psychosis, ICD-10 | SEPEA study, 631, age range 16–35, male 65.9%, non-affective psychosis (n = 573) 87.2%, affective psychosis (n = 84) 12.8%, white British 74.6%, median age 23.8 (IQR 19.6–27.6) | Age, sex, race/ethnicity and socio-economic status | Multilevel Poisson regression | Deprivation, social isolation and urbanicity were associated with elevated psychosis risk for psychotic disorders (IRR = 1.12, 1.09 and 1.11). Deprivation and social isolation were associated with greater risk for non-affective psychosis (IRR = 1.13 and 1.11) and racial and ethnic diversity with a lower risk (IRR = 0.94). Racial and ethnic density and lower intragroup fragmentation were also associated with a lower risk for affective psychoses (IRR = 0.98 and 0.97) |
| 13 | Schofield et al. [23] | Denmark | Urbanicity based on pp/km2 at age 15 | Non-affective psychosis, ICD-10 and 8 | Population based cohort of 2,224,464 born between 1965 and 1997 and followed until 2013, individuals of which 58,616 (2.6%) diagnosed, first and second-generation migrants | Age, sex, age × sex, calendar time, history of parental psychiatric disorder, parental income, ethnic density in neighbourhood at age 15 | Multilevel Poisson regression; the relation with urbanicity/ethnic density tested in cross-level interaction | Risk for non-affective psychosis higher for native Danes in urban environments (IRR = 1.13). All migrant groups showed elevated IRRs when age, sex and calendar period were adjusted for. After adjustment for ethnic density only migrants from Europe and the Middle East had an elevated psychosis risk in more urban areas (IRR = 1.09 and 1.12) |
| 14 | Söderström et al. [36▪▪] | Switzerland | Lausanne 3400 pp/km2, urban walks | Schizophrenia or non-affective psychoses | Twenty FEP, age 18–35 | Ethnographic, coding of experiences and behaviour | Participants indicated they preferred the countryside, urban areas being associated with stress, caused by density, sensory stimulations, obstacles to mobility and uncertainty about role management in public situations. Patients used three coping tactics: regulating mobility; creating ‘bubbles’ of isolation or atmosphere of comfort | |
| 15 | Thirthalli et al. [33] | India | District headquarters were considered urban, the remaining places were considered rural | Non-affective psychosis, ICD-10 | 551 first admissions, mean age 31.6, 54.4% male | t-tests, Mann–Whitney U test and Kruskal–Wallis test, Spearman's correlation | Education and income were higher in urban compared to rural populations. Patients from urban areas were more often unemployed. Duration of untreated psychosis did not differ between urban and rural patients | |
| 16 | Toulopoulou et al. [22] | Denmark | Urban birth, moving to a more urban area at age 10 vs. not based on five urbanization categories: capital, capital suburb, provincial city, provincial town and rural; 5,220, 845, 470, 180, and 55 pp/km2 | Schizophrenia spectrum disorder ICD-8, ICD-10 | 153,170 individuals born in Denmark between 1955 and 1993, 578 were later diagnosed, male only | Period, birth cohort, parental age, education and occupation (social class), familial psychiatric history and second-generation migrant status | Cox regression | Being born in the capital and an increase in urbanicity before age 10 was associated with higher adult schizophrenia risk (IRR = 1.69 and 1.45). The effect for the latter became nonsignificant when we adjusted for confounders |
| 17 | Wang and Zhang [26] | China | Rural–urban residency | Schizophrenia, ICD-10 | 2,108,410 respondents, 11,790 (0.56%) with schizophrenia | Age, years of education, provincial infant mortality rate, provincial gross domestic product, season of birth, region (north vs. south) | Discrete time hazard models | Urban residents had the highest risk for developing schizophrenia (OR = 1.09). Further analysis showed an elevated risk only for males (OR = 1.23 vs. 0.97 in females). Birth seasonality effects on psychosis risk were only present in rural areas |
DSM, Diagnostic and Statistical Manual; EU-GEI, European network of national Schizophrenia networks studying Gene–Environment Interactions; FEP, first episode psychosis, ICD, international classification of diseases; IQR, interquartile range; IRR, incident rate ratio; OR, odds ratio; PRS, polygenic risk scores; RDC, research diagnostic criteria; SEPEA, Social Epidemiology of Psychoses in East Anglia; SES, Socio-economic status.
Urbanicity, resources and treatment
Urbanicity can be a proxy for risk-increasing factors, but can also signify risk-reducing factors, such as healthcare or resource access. Individuals who were prenatally exposed to the Chinese famine in 1959–1962 showed significantly elevated schizophrenia rates in rural, but not urban areas. The urban population received food from state grain stores, showing how urbanicity can affect resource access [31]. Another Chinese study showed that patients in rural compared to urban areas were less likely to take antipsychotics (35.4 vs. 17.5%) [32]. Lower education, living alone and number of admissions were predictors of not taking antipsychotics in urban areas, whereas female sex, low BMI, higher positive symptoms, lower anxiety and insight emerged as predictors in rural areas. These patterns could reflect urban variation in status associated with sex, care and family structures. Research from India on rural–urban differences in time to treatment (indicated by duration of untreated psychosis) showed that despite greater proximity to psychiatric care, better education and income of families, urban patients did not access care earlier than rural patients [33].
Urbanicity and nature
Green space might reduce psychosis risk through stress reduction and reduced exposure to pollution. A Danish register study showed increased psychosis risk in those who during childhood (at age 10) lived in the least green compared to those who lived in the greenest areas. Risk decreased with accumulated green space exposure. The effects of green space were attenuated, but still significant when urbanicity and socio-economic factors were taken into account [34▪▪]. Evidence from the Netherlands showed that patients with psychotic disorders tend to reside in less green neighbourhoods than the general population. Yet, greener living was unrelated to the duration of psychiatric admissions [35].
Coping with urbanicity
Swiss research showed that FEP patients prefer rural to urban environments and that they perceive density of people and buildings; levels of sensory stimulation; mobility obstacles and difficult role management in public situations as stressors. Coping strategies included planning and regulating mobility to avoid crowded areas; creating isolation from the environment through technology (e.g. headphones), close social contact (e.g. friends) or internal dialogue and creating atmospheres of comfort (e.g. in nature) [36▪▪].
Urbanicity and genetic risk
One study examined whether the genetic risk for psychosis, indicated by polygenic risk scores, accounts for city living and associations between schizophrenia and urbanicity at birth and during upbringing (i.e. at age 15). Urbanicity was associated with increased schizophrenia risk. Adjustment for polygenic risk scores did not change the association between schizophrenia and urban birth and slightly attenuated the association with urban upbringing [37▪].
Urbanicity and the brain
A Dutch investigation on total grey matter volume (GMV) and urban upbringing in individuals with non-affective psychosis, healthy siblings and control participants [38▪], associated urban upbringing with reduced GMV in male patients only.
DISCUSSION
This review shows that urban environments do not increase the risk for psychosis by default, but that their effects are conditional on multiple factors. For instance, city living can offer benefits, like access to healthcare or resources, especially in less developed countries [31,32]. However, it is also characterized by lack of green space and high-intensity social encounters that might be particularly stressful for individuals with an increased liability for psychosis [36▪▪,39].
The North European findings support previously established urbanicity–psychosis associations [22,25,40,41], with most robust effects for urban birth and childhood urbanicity [22]. Danish population register data show that the urbanicity–psychosis link cannot be explained by the genetic risk for psychosis, which could lead to a tendency for urban living [37▪]. Interestingly, South European data did not support the link between urbanicity and psychosis (in Italy urbanicity emerged as protective factor) and a North–South divide also appeared for associations between urbanicity and psychotic symptoms [28,29]. Thus, even in relatively homogenous western, high-income countries (e.g. comparable drug use, religion, education and healthcare standards), urbanicity effects are diverse and it is unclear why international differences occur. Possible explanatory factors include differences in social cohesion, control and isolation in rural areas; differential pressures of modern urban life or geographic variations in diet, climate or exposure to disease agents. Clear-cut urbanicity effects could not be identified in LMIC either [27▪▪]. It is possible that in some LMIC positive urbanicity effects, such as the availability of resources counteract negative urbanicity effects. Alternatively, some negative effects of (northern) high-income societies, such as migration/racial discrimination and social economic disparities might not play a large role in LMIC. Overall, this review reveals heterogeneity and complex variation. In Estonia, China, Denmark, the Netherlands and the United Kingdom urbanicity was associated with a higher psychosis risk. In Mali, Senegal, the Philippines, Spain, Italy and France urbanicity was associated with a lower psychosis risk or unrelated to risk. There is no obvious common denominator unifying the two lists of culturally and geographically diverse countries. In the search for explanations, it is important to consider that definitions of urbanicity varied between studies. Pooled analysis covers interesting and potentially important international patterns of variation and future research will need to analyze data by country to identify shared risk factors and protective factors.
Numerous social and economic mechanisms may account for urbanicity effects [42]. Among others, the reviewed studies investigated migrant/ethnic minority status, racial/ethnic diversity, – density and – fragmentation, socio-economic status and social isolation. Migrant/minority status has been viewed as particularly important, because migrants often leave poor living conditions with limited opportunities to seek improvement in urban areas [43]. This exposes them to multiple factors that can increase psychosis risk [44]. For instance, residential mobility itself has been associated with an increased risk, suggesting harmful effects of social instability [25,45]. The current findings support an elevated psychosis risk for some (e.g. African, Caribbean, Middle Eastern/Pakistani, European non-Scandinavian and Asian), but not all migrant groups (e.g. Arabic, non-British White) [23,24▪▪,25,30]. Migrant status did not explain urbanicity effects in the United Kingdom and Denmark [23,25,30], but did so across multiple other European countries [24▪▪]. Interestingly, ethnic density, for example living in areas with others from the same cultural background, appears to mitigate psychosis risk in European and Middle Eastern groups [23]. Protective effects could be social support networks and reduced discrimination [46]. It remains unclear why this effect has been found only for specific migrant groups. Future research needs to consider time (e.g. childhood vs. adulthood) and reasons for migration (e.g. war refugees, economic migration within or between culturally (dis)similar countries), as well as the different conditions people encounter in their new homes (e.g. attitudes towards migrants) as possible explanations. Also with regard to urbanicity and other socio-economic factors, the current evidence is mixed. In the United Kingdom economic deprivation, social isolation and urbanicity (but not racial/ethnic diversity, – density or – fragmentation) emerged as independent predictors of psychosis risk when ethnicity was accounted for [30]. However, across Europe [24▪▪] no significant associations between urbanicity and psychosis risk were found when minority status and socio-economic indicators (e.g. owner occupancy of housing, single-person household and unemployment) were considered.
Exposure to green space during childhood reduced psychosis risk, independent of urbanicity effects [34▪▪]. Effects of nature might be particularly salient during childhood, where a calmer and less polluted environment with opportunities for outdoor activities may enhance resilience and/or protect the developing brain. Such effects are supported by research that linked urban upbringing to reductions in GMV in males with psychosis [38▪]. Urban upbringing may increase psychosis risk through stress sensitization, mediated by gene–environment interactions with dopamine genes [47] and stress during development has previously been associated with reduced GMV [48]. Still, it remains unclear why this effect would be specific to males. Further research will be necessary to show how the city affects the developing brain [49]. Research that investigated current green space exposure showed that individuals with a psychotic disorder tend to live in less green neighbourhoods. Although this was unrelated to clinical outcomes [35], recent evidence suggests positive effects of nature on well-being [50] and that FEP patients use nature to cope with urban stressors [36▪▪]. Thus, exposure to nature could still impact positively on patients’ well-being if directly integrated in treatment during admission.
CONCLUSION
Diverse social, economic and environmental factors combine to explain urban risk with regard to incidence, prevalence and the course of psychotic disorders in ways we are only starting to understand. This review highlights the need for global, multidisciplinary investigations that incorporate epidemiology, neuroscience, experimental psychology, sociology and urban planning, an approach which was recently presented as ‘neurourbanism’ [49]. This research needs to pinpoint toxic (e.g. pollution, disease exposure, unemployment, social fragmentation or migration), as well as protective urban effects (e.g. resources, political freedom and low social control) and their interactions. Sensitive periods of maximum risk (e.g. urban birth, upbringing and current urbanicity) should be systematically investigated, while considering effects of cumulative urban exposure. The newly generated knowledge will be paramount for urban design that mitigates risk and the understanding of the cause of psychosis.
Acknowledgements
None.
Financial support and sponsorship
A.K.F. was supported by a NARSAD Young Investigator Grant from the Brain & Behaviour research Foundation (24138). L.K. was supported by a VICI grant from the Netherlands Organization for Scientific Research (NWO) [452-07-007,453-11-005]; and an ERC Consolidator grant (648082 SCANS).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Radua J, et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 2018; 17:49–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Os J, Pedersen CB, Mortensen PB. Confirmation of synergy between urbanicity and familial liability in the causation of psychosis. Am J Psychiatry 2004; 161:2312–2314. [DOI] [PubMed] [Google Scholar]
- 3.United Nations DoE, Social A. World Urbanization Prospects: The 2018 Revision, Highlights. 2018. [Google Scholar]
- 4▪.Kirkbride JB, Keyes KM, Susser E. City living and psychotic disorders: implications of global heterogeneity for theory development. JAMA Psychiatry 2018; 75:1211–1212. [DOI] [PubMed] [Google Scholar]; An interesting viewpoint on DeVylder et al.[27▪▪] outlining the need for new theories on the urbanicity–psychosis association, as well as the investigation of urbanicity effects across different worldwide contexts.
- 5.Coid JW, Zhang Y, Li T. Urbanicity and psychosis. JAMA Psychiatry 2018; 75:1301–11301. [DOI] [PubMed] [Google Scholar]
- 6.Plana-Ripoll O, Pedersen CB, McGrath JJ. Urbanicity and risk of schizophrenia: new studies and old hypotheses. JAMA Psychiatry 2018; 75:687–688. [DOI] [PubMed] [Google Scholar]
- 7.Mortensen PB, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med 1999; 340:603–608. [DOI] [PubMed] [Google Scholar]
- 8.Laursen TM, et al. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a Danish population-based cohort. J Clin Psychiatry 2007; 68:1673–1681. [DOI] [PubMed] [Google Scholar]
- 9.Pedersen CB, Mortensen PB. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch Gen Psychiatry 2001; 58:1039–1046. [DOI] [PubMed] [Google Scholar]
- 10.Krabbendam L, Van Os J. Schizophrenia and urbanicity: a major environmental influence: conditional on genetic risk. Schizophr Bull 2005; 31:795–799. [DOI] [PubMed] [Google Scholar]
- 11.Sundquist K, Frank G, Sundquist J. Urbanisation and incidence of psychosis and depression. Br J Psychiatry 2004; 184:293–298. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie K, Murray A, Booth T. Do urban environments increase the risk of anxiety, depression and psychosis? An epidemiological study. J Affect Disord 2013; 150:1019–1024. [DOI] [PubMed] [Google Scholar]
- 13.Kirkbride JB, et al. Neighbourhood-level effects on psychoses: re-examining the role of context. Psychol Med 2007; 37:1413–1425. [DOI] [PubMed] [Google Scholar]
- 14.Michail M, Birchwood M. Social anxiety disorder in first-episode psychosis: incidence, phenomenology and relationship with paranoia. Br J Psychiatry 2009; 195:234–241. [DOI] [PubMed] [Google Scholar]
- 15.van Os J, Kenis G, Rutten BP. The environment and schizophrenia. Nature 2010; 468:203. [DOI] [PubMed] [Google Scholar]
- 16.Drukker M, et al. Social disadvantage and schizophrenia. A combined neighbourhood and individual-level analysis. Soc Psychiatry Psychiatr Epidemiol 2006; 41:595–604. [DOI] [PubMed] [Google Scholar]
- 17.Kirkbride JB, et al. Testing the association between the incidence of schizophrenia and social capital in an urban area. Psychol Med 2008; 38:1083–1094. [DOI] [PubMed] [Google Scholar]
- 18.O’donoghue B, et al. Neighbourhood characteristics and the incidence of first-episode psychosis and duration of untreated psychosis. Psychol Med 2016; 46:1367–1378. [DOI] [PubMed] [Google Scholar]
- 19.Zammit S, et al. Individuals, schools, and neighborhood: a multilevel longitudinal study of variation in incidence of psychotic disorders. Arch Gen Psychiatry 2010; 67:914–922. [DOI] [PubMed] [Google Scholar]
- 20.Attademo L, Bernardini F. Air pollution and urbanicity: common risk factors for dementia and schizophrenia? Lancet Planet Health 2017; 1:e90–e91. [DOI] [PubMed] [Google Scholar]
- 21.Selten JP, Cantor-Graae E, Kahn RS. Migration and schizophrenia. Curr Opin Psychiatry 2007; 20:111–115. [DOI] [PubMed] [Google Scholar]
- 22.Toulopoulou T, et al. IQ, the urban environment, and their impact on future schizophrenia risk in men. Schizophr Bull 2017; 43:1056–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schofield P, et al. Ethnic density, urbanicity and psychosis risk for migrant groups: a population cohort study. Schizophr Res 2017; 190:82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24▪▪.Jongsma HE, et al. Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatry 2018; 75:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]; The large multicentre study shows substantial heterogeneity of the urbanicity–psychosis link in FEP in Southern and Northern European urban settings, highlighting the need for further investigation of underlying mechanisms.
- 25.Kirkbride JB, et al. Ethnic minority status, age-at-immigration and psychosis risk in rural environments: evidence from the SEPEA study. Schizophr Bull 2017; 43:1251–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C, Zhang Y. Season of birth and schizophrenia: evidence from China. Psychiatry Res 2017; 253:189–196. [DOI] [PubMed] [Google Scholar]
- 27▪▪.DeVylder JE, et al. Association of urbanicity with psychosis in low- and middle-income countries. JAMA Psychiatry 2018; 75:678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]; The international population-based study shows no association between urban residence and self-reported diagnoses of psychotic disorders across 42 low and middle-income countries. Considerable heterogeneity at county level highlights the need for fine-grained investigations.
- 28.Quattrone D, et al. Transdiagnostic dimensions of psychopathology at first episode psychosis: findings from the multinational EU-GEI study. Psychol Med 2018; 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bocchetta A, Traccis F. The sardinian puzzle: concentration of major psychoses and suicide in the same sub-regions across one century. Clin Pract Epidemiol Ment Health 2017; 13:246–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Richardson L, et al. Association of environment with the risk of developing psychotic disorders in rural populations: findings from the social epidemiology of psychoses in East Anglia study. JAMA Psychiatry 2018; 75:75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He P, et al. Long-term effect of prenatal exposure to malnutrition on risk of schizophrenia in adulthood: evidence from the Chinese famine of 1959–1961. Eur Psychiatry 2018; 51:42–47. [DOI] [PubMed] [Google Scholar]
- 32.Hou CL, et al. Antipsychotic-free status in community-dwelling patients with schizophrenia in China: comparisons within and between rural and urban areas. J Clin Psychiatry 2018; 79: [DOI] [PubMed] [Google Scholar]
- 33.Thirthalli J, et al. Rural-urban differences in accessing mental health treatment in patients with psychosis. Int J Soc Psychiatry 2017; 63:694–698. [DOI] [PubMed] [Google Scholar]
- 34▪▪.Engemann K, et al. Childhood exposure to green space: a novel risk-decreasing mechanism for schizophrenia? Schizophr Res 2018; 199:142–148. [DOI] [PubMed] [Google Scholar]; Using novel satellite-based technology, this study suggests particular benefits of green space exposure during childhood on the risk for psychosis.
- 35.Boers S, et al. Does residential green and blue space promote recovery in psychotic disorders? A cross-sectional study in the Province of Utrecht, The Netherlands. Int J Environ Res Public Health 2018; 15: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36▪▪.Söderström O, et al. Emplacing recovery: how persons diagnosed with psychosis handle stress in cities. Psychosis 2017; 9:322–329. [Google Scholar]; This study on the experience of urban environments gives important insights into key coping mechanisms that individuals with psychosis use to deal with urban stressors.
- 37▪.Paksarian D, et al. The role of genetic liability in the association of urbanicity at birth and during upbringing with schizophrenia in Denmark. Psychol Med 2018; 48:305–314. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study shows that the genetic liability for psychosis does not account for the association between early urbanicity exposure and psychosis risk later in life.
- 38▪.Frissen A, et al. Evidence that reduced gray matter volume in psychotic disorder is associated with exposure to environmental risk factors. Psychiatry Res Neuroimaging 2018; 271:100–110. [DOI] [PubMed] [Google Scholar]; An interesting study that suggests that urbanicity exposure during childhood may impact on psychosis risk through effects on grey matter density of the developing brain.
- 39.Glaeser E. Cities, productivity, and quality of life. Science 2011; 333:592–594. [DOI] [PubMed] [Google Scholar]
- 40.Vassos E, et al. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull 2012; 38:1118–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.March D, et al. Psychosis and place. Epidemiol Rev 2008; 30:84–100. [DOI] [PubMed] [Google Scholar]
- 42.Manning N. Sociology, biology and mechanisms in urban mental health. Soc Theory Health 2018; 1–22. [Google Scholar]
- 43. Eurostat, ed. People in the EU: who are we and how do we live? 2015, Publications Office of the European Union, 2015: Luxembourg. [Google Scholar]
- 44.Cantor-Graae E, Pedersen CB. Full spectrum of psychiatric disorders related to foreign migration: a Danish population-based cohort study. JAMA Psychiatry 2013; 70:427–435. [DOI] [PubMed] [Google Scholar]
- 45.Price C, et al. Association of residential mobility over the life course with nonaffective psychosis in 1.4 million young people in Sweden. JAMA Psychiatry 2018; 75:1128–1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bécares L, Dewey ME, Das-Munshi J. Ethnic density effects for adult mental health: systematic review and meta-analysis of international studies. Psychol Med 2017; 48:2054–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reed JL, et al. Interaction of childhood urbanicity and variation in dopamine genes alters adult prefrontal function as measured by functional magnetic resonance imaging (fMRI). PloS One 2018; 13:e0195189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tyborowska A, et al. Early-life and pubertal stress differentially modulate grey matter development in human adolescents. Sci Rep 2018; 8:9201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adli M., et al. Neurourbanism: towards a new discipline. (2215-0374 (Electronic)) [Google Scholar]
- 50.Bakolis I, et al. Urban mind: using smartphone technologies to investigate the impact of nature on mental well being in real time. BioScience 2018; 68:134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]


