Abstract.
Latent tuberculosis infection (LTBI) remains the main source of new active tuberculosis (TB) cases worldwide. Household close contacts (HCCs) are at high risk of acquiring LTBI and subsequent development of TB. In this study, we aim to identify risk factors associated with LTBI in HCCs of TB patients living in a low TB-incidence setting. Our results revealed that HCCs who are aged more than 50 years (OR = 4.05) and overweight (OR = 15.3) are at higher risk of acquiring LTBI. None of these LTBI household contacts progressed to active TB. These findings suggest that HCCs who are young adults and children with normal and low body mass index are less likely to acquire LTBI after exposure to TB patients, even in low TB-incidence settings.
Tuberculosis (TB) is considered a global health problem because of its high prevalence and morbidity and mortality rates. According to the WHO, in 2017, 10.4 million people became ill with TB and 1.8 million died from this disease.1 More than 95% of TB deaths occur in low- and middle-income countries, and TB remains the main cause of death in people infected with HIV.2 Unfortunately, one quarter of the world’s population suffers from latent tuberculosis infection (LTBI). The vast majority of these LTBI cases are unaware of their infection status, and 10% progress to active disease if not treated.3 Consequently, understanding risk factors for LTBI and disease progression remains key to ending the worldwide epidemic.
Interferon gamma release assays (IGRAs) and tuberculin skin tests (TSTs) have been proposed to identify individuals with LTBI in high-income countries with low TB incidence.4 Both tests are based on the adaptive immune response to Mycobacterium tuberculosis derivatives. A worldwide effort is underway to identify novel biomarker tests for LTBI diagnosis and disease progression.5 Despite their usefulness for LTBI monitoring and diagnosis, IGRA and TST outcomes are affected by the high TB burden across the world.6,7 In fact, the WHO has established differential guidelines for the management of LTBI in low TB-incidence settings.8 Consequently, identification of LTBI risk factors is essential for TB control even in low TB-burden regions. Our study aimed to determine the risk factors for acquiring LTBI among household close contacts (HCCs) of TB patients in a low TB-incidence setting within Panama. Our findings suggest older adults with a high body mass index (BMI) are more likely to acquire LTBI after exposure to positive sputum smear TB patients.
This pilot study was conducted in Cocle Province, which is located in the central region of Panama (Figure 1) and 150 km from Panama City. From January to December 2015, pulmonary TB patients were identified by acid-fast bacilli sputum smear. These TB patients were treated with anti-TB drugs for 6 months according to the national guidelines. Household close contacts living in the same house with smear-positive TB patients were invited to participate in our study. Those who provided informed written consent received a survey interview using a standardized questionnaire instrument. These HCCs donated blood samples and were encouraged to report any illness within a 2-year period. Only HIV-negative HCCs were included in our study. The study protocol was approved by the Institutional Review Board of Caja de Seguro Social Committee.
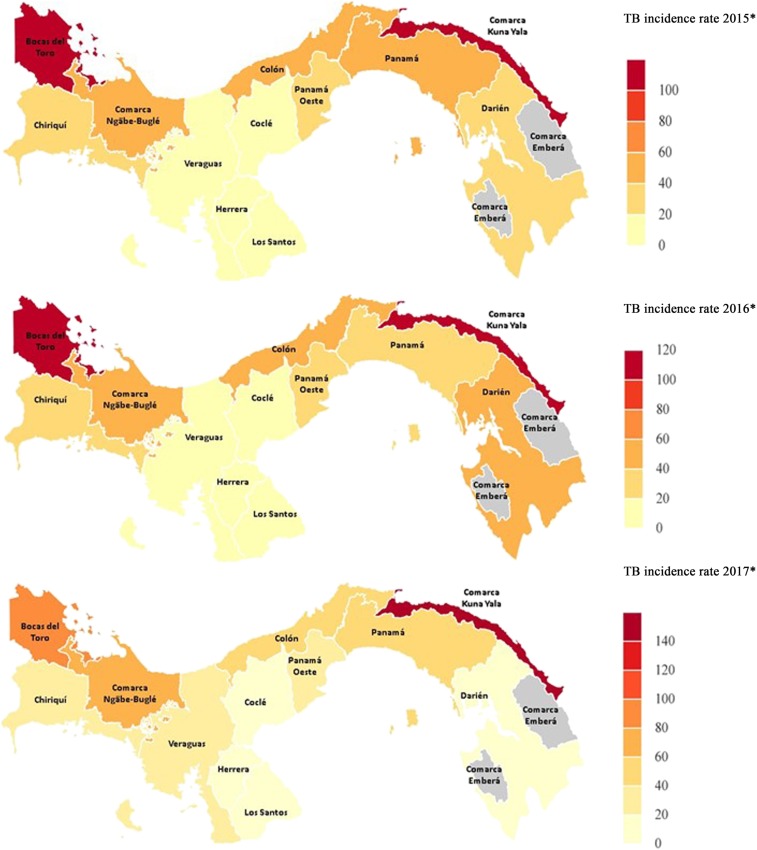
Figure 1.
Tuberculosis (TB) incidence changes in Panama during the 2015–2017 period: Country map shows the TB incidence per 100,000 inhabitants per year. Lighter colors indicate lower incidences and darker colors indicate high-incidence settings within Panama. The study site was Cocle Province. Source: Ministry of Health of the Republic of Panama. This figure appears in color at www.ajtmh.org.
Five milliliters of blood was collected from each HCC participant. We analyzed blood samples with the QuantiFERON-TB Gold In-Tube test (Cellestis Limited, Carnegie, Victoria, Australia) according the manufacturer’s instructions.9 All variables were described in percentages, and comparison between the IGRA-positive and IGRA-negative groups was completed using the Fischer exact test because of the small sample size. We used odds ratios and 95% CI to test all the potential associations between the risk factors and IGRA status. All statistical tests were carried out using STATA v12.1 (StataCorp LLC, College Station, TX) and Microsoft Excel software (Microsoft Coorporation, Redmond, WA).
A total of 61 HCCs were recruited to participate in our study during 2015. All participants approved and signed the consent/assent form. All participants were intimate HCCs (they lived with the patients during their treatment for a daily period of at least 6 hours). The province of Coclé had an average TB incidence of 13.5/100,000 during the collection year (2015) and the two follow-up years (2016–2017) (Figure 1). Therefore, we can assert that TB transmission to HCCs occurred at home and not at schools, in the community, or in the workplace. A total of four HCCs were excluded from the study: one died naturally, two participants declined to complete the survey, and one participant had respiratory symptoms not related to TB.
The analysis of HCC characteristics indicated an average family size of eight members, but 67% lived with more than five people per house. All the HCCs lived in rural or semi-urban areas in multifamily housing units, meaning household members shared common areas, such as kitchens, laundry rooms, and bathrooms with the members of other households. Table 1 shows the sociodemographic characteristics. Majority of the patients (34 [56%]) were male. Of the contacts interviewed, 32 (52%) had completed elementary school only; 27 (46%) identified as students and 17 (28%) identified as housewives. All 61 participants (100%) were Panamanians. Majority of the dwellings described by the participants were made of cement blocks (53 [85%]), with most only having one room. The degree of kinship between the patients and contacts was mostly 1st or 2nd degree of consanguinity (62%).
Table 1.
Description of the study population and univariate analysis of risk factors for latent tuberculosis infection
| Characteristic | Total | QGTB+ | QGTB− | OR | P-value* | |||
|---|---|---|---|---|---|---|---|---|
| n | % | N | % | n | % | |||
| Total | 61 | 100 | 7 | 11.5 | 54 | 88.5 | – | – |
| Age (years) | ||||||||
| ≤ 9 | 17 | 27.9 | 0 | 0 | 17 | 100 | Reference | – |
| 10–19 | 19 | 31.1 | 0 | 0 | 19 | 100 | NA | 0.26 |
| 20–29 | 4 | 6.6 | 0 | 0 | 4 | 100 | NA | 0.1 |
| 30–39 | 8 | 13.1 | 2 | 25 | 6 | 75 | 8.3 (0.45–348.5) | 0.08 |
| 40–49 | 6 | 9.8 | 1 | 16.7 | 5 | 83.3 | 5.2 (0.09–277.4) | 0.19 |
| ≥ 50 | 7 | 11.5 | 4 | 57.1 | 3 | 42.9 | 29.5 (1.65–2,351) | 0.01 |
| Gender | ||||||||
| Male | 24 | 39.3 | 3 | 12.5 | 21 | 87.5 | 1.18 (0.15–7.7) | > 0.99 |
| Female | 37 | 60.7 | 4 | 10.8 | 33 | 89.2 | Reference | – |
| Education | ||||||||
| Elementary school or less | 32 | 52.5 | 5 | 15.6 | 27 | 84.4 | Reference | – |
| Middle school | 19 | 31.1 | 2 | 10.5 | 17 | 89.5 | 0.64 (0.06–4.48) | 0.95 |
| High school or more | 10 | 16.4 | 0 | 0 | 10 | 100 | 0.65 (0.01–7.30) | > 0.99 |
| BMI† | ||||||||
| Underweight | 8 | 13.1 | 0 | 0 | 8 | 100 | 2.7 (0.05–150.5) | 0.27 |
| Normal | 22 | 36.1 | 0 | 0 | 22 | 100 | Reference | – |
| Overweight | 19 | 31.1 | 6 | 31.6 | 13 | 68.4 | 14.9 (1.23–972.3) | 0.014 |
| Obese | 12 | 19.7 | 1 | 8.3 | 11 | 91.7 | 3.2 (0.03–327.4) | 0.53 |
| Living in overcrowded conditions | ||||||||
| Yes | 52 | 85.2 | 4 | 7.7 | 48.0 | 92.3 | 0.17 (0.02–1.47) | 0.07 |
| No | 9 | 14.8 | 3 | 33.3 | 6.0 | 66.7 | Reference | – |
| BCG scar | ||||||||
| Yes | 57 | 93.4 | 4 | 7.0 | 53 | 93.0 | 0.03 (0.001–0.33) | 0.004 |
| No | 4 | 6.6 | 3 | 75.0 | 1 | 25.0 | Reference | – |
| Caregiver | ||||||||
| Yes | 17 | 27.9 | 3 | 17.6 | 14 | 82.4 | 2.14 (0.28–14.27) | 0.39 |
| No | 44 | 72.1 | 4 | 9.1 | 40 | 90.9 | Reference | – |
| Time of exposure | ||||||||
| ≥ 12 hours/day | 42 | 68.9 | 5 | 11.9 | 37 | 88.1 | 1.15 (0.17–13.1) | > 0.99 |
| < 12 hours/day | 19 | 31.1 | 2 | 10.5 | 17 | 89.5 | Reference | – |
| Smear status of source case | ||||||||
| Positive | 19 | 32.2 | 2 | 10.5 | 17 | 89.5 | 0.82 (0.07–5.71) | > 0.99 |
| Negative | 40 | 67.8 | 5 | 12.5 | 35 | 87.5 | Reference | – |
BCG = Bacillus Calmette-Guerin; BMI = body mass index; NA = not applicable; QGTB = quantiferon gold. Underweight: < 18.5 kg; normal: ≥ 18.5 kg and < 23 kg; overweight: ≥ 23 kg and < 27.5 kg; obese: ≥ 27.5 kg. Bold values resulted statistically significant at P < 0.005.
* Fisher exact test P-value (two-tailed).
† For ages 2–20 years, we used CDC growth charts for boys and girls.
The IGRA test, QuantiFERON-TB-Gold, identified 11.5% (7/61) of HCCs with LTBI, as shown in Table 1. By gender, the positive LTBI cases represented 10.8% of the female participants and 12.5% of the male participants. All participants were classified into six age groups. In the LTBI risk factor analysis, we found that HCCs aged more than 50 years had a significant OR of 29.5 (95% CI = 2.24–1,163). In this study, all positive LTBI HCCs were aged more than 30 years. The proportion of positive LTBI HCCs was higher among the group of participants with less than elementary school education than in the groups with at least middle or high school education. Although the association between education level and LTBI was not significant among all HCCs, the trend showed that higher levels of education could be a potential protective factor against LTBI. Body mass index was calculated and used as a proxy for adult nutritional status. For children, the BMI-for-age percentile tables for boys and girls developed by the CDC were used to classify the HCCs as underweight, normal, overweight, or obese.10 When using normal weight as a reference, we found that overweight significantly increased the risk for LTBI among HCCs (OR = 14.93, 95% CI = 1.57–483.3). Meanwhile, the presence of a Bacillus Calmette-Guerin vaccine scar proved to be a protective factor against LTBI among HCCs (OR = 0.029, 95% CI = 0.001–0.33).
Nearly 69% of participants reported being exposed to the source case for more than 12 hours per day and reported living in overcrowded conditions; however, these were not identified as significant risk factors. Similarly, the acid-fast smear status of the index TB patient was not related to the LTBI status among HCCs included in our study. Other health history information gathered from the 61 HCCs showed that all (100%) were nonsmokers, and three patients (4.9%) had coexisting diseases. When analyzed using a multivariable approach, age and overweight increased the risk of LTBI in HCCs (Table 2).
Table 2.
Exact logistic regression on risk factors for latent tuberculosis infection
| Variables | OR | Suff | P-value | 95% CI |
|---|---|---|---|---|
| Age (every 10 years) | 4.05 | 37 | 0.0008 | 1.49–26.92 |
| BMI (overweight) | 15.29 | 6 | 0.04 | 1.09–1,065.75 |
BMI = body mass index; normal and underweight used as reference.
The aforementioned results revealed an LTBI prevalence of 11.5% among HCCs in Cocle Province, Panama. This region holds the lowest TB incidence rate, and thus the HCCs were likely exposed to TB only at home. Our study also found that obese, overweight, and older HCCs have a higher risk of establishing LTBI. Recent systematic reviews have found that the opposite malnutrition status—low BMI—did not increase the yield of LTBI cases among household contacts.11 Others have indicated that malnutrition, in the form of excess intake of nutrients, could be a potential risk factor for LTBI.12 From a public health standpoint, obesity and overweight are risk factors for various other chronic diseases, including diabetes. Thus, malnutrition should not only be considered for individuals with a low BMI (underweight).13 Paradoxically, although obese adult HCCs are potentially more likely to harbor M. tuberculosis infection, they are less likely to progress to active TB.14,15 By contrast, bodyweight control in obese adults could lead to the development of TB. Future studies should evaluate whether malnutrition (either as an excess or deficiency of nutrients and energy) is related to LTBI. It is also necessary to clarify whether obesity induces an exaggerated immune response to a mycobacterial challenge and, thus, the clearance of M. tuberculosis or a pro-inflammatory response, which may result in establishing LTBI and stopping disease progression.14
Because of the sample size of our study, we were not able to adjust LTBI incidence for concomitant chronic diseases. The small number of participants precludes dividing them based on other risk factors. Our future plans include exploring the relationship between BMI and LTBI with the presence of other clinical conditions, such as diabetes, kidney diseases, immunological disorders, HIV, and autoimmune diseases, in both low and high TB-incidence settings. None of the participants in our study developed secondary TB after 2 years of follow-up. Thus, we could not estimate the OR of developing secondary TB after baseline LTBI. Further studies are necessary to investigate the role of overcrowding, exposure time, age, and/or BMI in developing secondary TB among overweight HCCs, especially in a low TB-incidence setting.
In summary, our findings support the notion that young HCCs with normal BMI are less likely to acquire LTBI after exposure to a positive sputum smear TB patient. A plausible explanation is that the immune response in lower BMI and/or older age individuals is impaired, and thus IGRA tests are negatively affected.11,16,17 Thus, LTBI screening among such an HCC group would result in minimal LTBI cases. Nevertheless, further studies using a much larger sample size are warranted to confirm the role of obesity and age in acquiring LTBI, possibly using a logistic regression with backward analysis adjusting for other variables. For now, we recommend providing close follow-up with HCCs who are aged more than 50 years and overweight in low TB-incidence settings.
Acknowledgments:
We thank Gladys Hidalgo and Maribel Ramos from the Cocle tuberculosis control program for providing access to TB case databases and Colleen Goodridge for critically reviewing this manuscript.
REFERENCES
- 1.WHO , 2018. Global Tuberculosis Report 2018. Geneva, Switzerland: World Health Organization, 243. [Google Scholar]
- 2.GBD Tuberculosis Collaborators , 2018. The global burden of tuberculosis: results from the Global Burden of Disease Study 2015. Lancet Infect Dis 18: 261–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salgame P, Geadas C, Collins L, Jones-Lopez E, Ellner JJ, 2015. Latent tuberculosis infection–revisiting and revising concepts. Tuberculosis (Edinb) 95: 373–384. [DOI] [PubMed] [Google Scholar]
- 4.Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K; IGRA Expert Committee ; Centers for Disease Control and Prevention (CDC) , 2010. Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection–United States, 2010. MMWR Recomm Rep 59: 1–25. [PubMed] [Google Scholar]
- 5.Walzl G, McNerney R, du Plessis N, Bates M, McHugh TD, Chegou NN, Zumla A, 2018. Tuberculosis: advances and challenges in development of new diagnostics and biomarkers. Lancet Infect Dis 18: e199–e210. [DOI] [PubMed] [Google Scholar]
- 6.Kang WL, et al. 2018. Interferon-gamma release assay is not appropriate for the diagnosis of active tuberculosis in high-burden tuberculosis settings: a retrospective multicenter investigation. Chin Med J (Engl) 131: 268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma SK, Vashishtha R, Chauhan LS, Sreenivas V, Seth D, 2017. Comparison of TST and IGRA in diagnosis of latent tuberculosis infection in a high TB-burden setting. PLoS One 12: e0169539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Getahun H, et al. 2015. Management of latent Mycobacterium tuberculosis infection: WHO guidelines for low tuberculosis burden countries. Eur Respir J 46: 1563–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoshiyama T, Harada N, Higuchi K, Saitou M, Kato S, 2015. Use of the QuantiFERON®-TB Gold in tube test for screening TB contacts and predictive value for active TB. Infect Dis (Lond) 47: 542–549. [DOI] [PubMed] [Google Scholar]
- 10.CDC , 2018. About Child & Teen BMI. Available at: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. Accessed November 19, 2018. [Google Scholar]
- 11.Saag LA, LaValley MP, Hochberg NS, Cegielski JP, Pleskunas JA, Linas BP, Horsburgh CR, 2018. Low body mass index and latent tuberculous infection: a systematic review and meta-analysis. Int J Tuberc Lung Dis 22: 358–365. [DOI] [PubMed] [Google Scholar]
- 12.Chen C, Zhu T, Wang Z, Peng H, Kong W, Zhou Y, Shao Y, Zhu L, Lu W, 2015. High latent TB infection rate and associated risk factors in the eastern China of low TB incidence. PLoS One 10: e0141511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan WC, 2018. Low body mass index and latent tuberculous infection: current evidence? Int J Tuberc Lung Dis 22: 355. [DOI] [PubMed] [Google Scholar]
- 14.Aibana O, et al. 2016. Nutritional status and tuberculosis risk in adult and pediatric household contacts. PLoS One 11: e0166333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leung CC, Lam TH, Chan WM, Yew WW, Ho KS, Leung G, Law WS, Tam CM, Chan CK, Chang KC, 2007. Lower risk of tuberculosis in obesity. Arch Intern Med 167: 1297–1304. [DOI] [PubMed] [Google Scholar]
- 16.Anuradha R, Munisankar S, Bhootra Y, Dolla C, Kumaran P, Babu S, 2016. High body mass index is associated with heightened systemic and mycobacterial antigen–specific pro-inflammatory cytokines in latent tuberculosis. Tuberculosis (Edinb) 101: 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bae W, et al. 2016. Comparison of the sensitivity of QuantiFERON-TB gold in-tube and T-SPOT.TB according to patient age. PLoS One 11: e0156917. [DOI] [PMC free article] [PubMed] [Google Scholar]