Abstract
Background
Depression is recognised as a major public health problem that has a substantial impact on individuals and on society. People with depression may consider using complementary therapies such as acupuncture, and an increasing body of research has been undertaken to assess the effectiveness of acupuncture for treatment of individuals with depression. This is the second update of this review.
Objectives
To examine the effectiveness and adverse effects of acupuncture for treatment of individuals with depression.
To determine:
• Whether acupuncture is more effective than treatment as usual/no treatment/wait list control for treating and improving quality of life for individuals with depression.
• Whether acupuncture is more effective than control acupuncture for treating and improving quality of life for individuals with depression.
• Whether acupuncture is more effective than pharmacological therapies for treating and improving quality of life for individuals with depression.
• Whether acupuncture plus pharmacological therapy is more effective than pharmacological therapy alone for treating and improving quality of life for individuals with depression.
• Whether acupuncture is more effective than psychological therapies for treating and improving quality of life for individuals with depression.
• Adverse effects of acupuncture compared with treatment as usual/no treatment/wait list control, control acupuncture, pharmacological therapies, and psychological therapies for treatment of individuals with depression.
Search methods
We searched the following databases to June 2016: Cochrane Common Mental Disorders Group Controlled Trials Register (CCMD‐CTR), Korean Studies Information Service System (KISS), DBPIA (Korean article database website), Korea Institute of Science and Technology Information, Research Information Service System (RISS), Korea Med, Korean Medical Database (KM base), and Oriental Medicine Advanced Searching Integrated System (OASIS), as well as several Korean medical journals.
Selection criteria
Review criteria called for inclusion of all published and unpublished randomised controlled trials comparing acupuncture versus control acupuncture, no treatment, medication, other structured psychotherapies (cognitive‐behavioural therapy, psychotherapy, or counselling), or standard care. Modes of treatment included acupuncture, electro‐acupuncture, and laser acupuncture. Participants included adult men and women with depression diagnosed by Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (DSM‐IV), Research Diagnostic Criteria (RDC), International Statistical Classification of Diseases and Related Health Problems (ICD), or Chinese Classification of Mental Disorders Third Edition Revised (CCMD‐3‐R). If necessary, we used trial authors' definitions of depressive disorder.
Data collection and analysis
We performed meta‐analyses using risk ratios (RRs) for dichotomous outcomes and standardised mean differences (SMDs) for continuous outcomes, with 95% confidence intervals (CIs). Primary outcomes were reduction in the severity of depression, measured by self‐rating scales or by clinician‐rated scales, and improvement in depression, defined as remission versus no remission. We assessed evidence quality using the GRADE method.
Main results
This review is an update of previous versions and includes 64 studies (7104 participants). Most studies were at high risk of performance bias, at high or unclear risk of detection bias, and at low or unclear risk of selection bias, attrition bias, reporting bias, and other bias.
Acupuncture versus no treatment/wait list/treatment as usual
We found low‐quality evidence suggesting that acupuncture (manual and electro‐) may moderately reduce the severity of depression by end of treatment (SMD ‐0.66, 95% CI ‐1.06 to ‐0.25, five trials, 488 participants). It is unclear whether data show differences between groups in the risk of adverse events (RR 0.89, 95% CI 0.35 to 2.24, one trial, 302 participants; low‐quality evidence).
Acupuncture versus control acupuncture (invasive, non‐invasive sham controls)
Acupuncture may be associated with a small reduction in the severity of depression of 1.69 points on the Hamilton Depression Rating Scale (HAMD) by end of treatment (95% CI ‐3.33 to ‐0.05, 14 trials, 841 participants; low‐quality evidence). It is unclear whether data show differences between groups in the risk of adverse events (RR 1.63, 95% CI 0.93 to 2.86, five trials, 300 participants; moderate‐quality evidence).
Acupuncture versus medication
We found very low‐quality evidence suggesting that acupuncture may confer small benefit in reducing the severity of depression by end of treatment (SMD ‐0.23, 95% CI ‐0.40 to ‐0.05, 31 trials, 3127 participants). Studies show substantial variation resulting from use of different classes of medications and different modes of acupuncture stimulation. Very low‐quality evidence suggests lower ratings of adverse events following acupuncture compared with medication alone, as measured by the Montgomery‐Asberg Depression Rating Scale (MADRS) (mean difference (MD) ‐4.32, 95% CI ‐7.41 to ‐1.23, three trials, 481 participants).
Acupuncture plus medication versus medication alone
We found very low‐quality evidence suggesting that acupuncture is highly beneficial in reducing the severity of depression by end of treatment (SMD ‐1.15, 95% CI ‐1.63 to ‐0.66, 11 trials, 775 participants). Studies show substantial variation resulting from use of different modes of acupuncture stimulation. It is unclear whether differences in adverse events are associated with different modes of acupuncture (SMD ‐1.32, 95% CI ‐2.86 to 0.23, three trials, 200 participants; very low‐quality evidence).
Acupuncture versus psychological therapy
It is unclear whether data show differences between acupuncture and psychological therapy in the severity of depression by end of treatment (SMD ‐0.5, 95% CI ‐1.33 to 0.33, two trials, 497 participants; low‐quality evidence). Low‐quality evidence suggests no differences between groups in rates of adverse events (RR 0.62, 95% CI 0.29 to 1.33, one trial, 452 participants).
Authors' conclusions
The reduction in severity of depression was less when acupuncture was compared with control acupuncture than when acupuncture was compared with no treatment control, although in both cases, results were rated as providing low‐quality evidence. The reduction in severity of depression with acupuncture given alone or in conjunction with medication versus medication alone is uncertain owing to the very low quality of evidence. The effect of acupuncture compared with psychological therapy is unclear. The risk of adverse events with acupuncture is also unclear, as most trials did not report adverse events adequately. Few studies included follow‐up periods or assessed important outcomes such as quality of life. High‐quality randomised controlled trials are urgently needed to examine the clinical efficacy and acceptability of acupuncture, as well as its effectiveness, compared with acupuncture controls, medication, or psychological therapies.
Plain language summary
Acupuncture for depression
Why is this review important?
Depression is widely experienced in our communities. People with clinical depression report lack of interest in life and activities that they otherwise normally enjoy. Some people who are depressed use complementary therapies, and some prefer these therapies over medication. Acupuncture treatment involves insertion of fine needles into different parts of the body to correct the imbalance of energy within the body.
Who will be interested in this review?
Adolescents and adults; healthcare practitioners, including general practitioners working with or involved in the treatment of individuals with depression; and providers and commissioners of healthcare services will be interested in this review.
What questions does this review aim to answer?
This review, which is an update of a previous Cochrane review (published in 2010), aims to answer the following questions.
• Is acupuncture better than no treatment or usual care?
• Is acupuncture better than control acupuncture (a treatment that looks similar to acupuncture)?
• Is acupuncture better than pharmacological therapies such as antidepressant medication?
• Is acupuncture combined with antidepressant medication better than antidepressant medication alone?
• Is acupuncture better than psychological therapies?
• Is acupuncture safer than other types of treatment for depression?
Which studies were included in the review?
Included were 64 randomised controlled trials (with 7104 participants) that measured changes in depression symptoms.
What does evidence from the review tell us?
Review authors rated the quality of evidence from most included studies as very low or low, and the effects described below should be interpreted with caution.
Acupuncture may result in a moderate reduction in the severity of depression when compared with treatment as usual/no treatment. Use of acupuncture may lead to a small reduction in the severity of depression when compared with control acupuncture. Effects of acupuncture versus medication and psychological therapy are uncertain owing to the very low quality of evidence. Risks of adverse events with acupuncture are also unclear, as most trials have not reported on adverse events.
What should happen next?
Review authors recommend that additional high‐quality randomised controlled trials should be undertaken. These trials should use suitable blinding (by which people do not know which treatment they are receiving) when appropriate and should incorporate quality of life measures, assessment of treatment acceptability, and medium‐ and long‐term follow‐up.
Summary of findings
Background
Description of the condition
Clinical depression is characterised by behavioural, cognitive, and emotional features. Depressed patients often exhibit signs of dysphoric mood, loss of interest in normally enjoyable pursuits, self‐neglect and social withdrawal, poor appetite or overeating, insomnia or hypersomnia, fatigue or loss of energy, low self‐esteem, poor concentration or difficulty making decisions, and feelings of hopelessness.
Depression is recognised as a major public health problem that has a substantial impact on individuals and on society. Depressive disorders are common in the general population. In the United States, the lifetime prevalence of a major depressive disorder (MDD) has been reported at 16.2% (Kessler 2007). The World Health Organization has described depression as an "unseen burden" (Murray 1996). MDD is associated with a significant loss of workdays (Kessler 2007), as well as substantial role impairment in relation to household responsibilities, social life, and personal relationships (Kessler 2003). It has been demonstrated that those in the community who have depressive disorders experience reduced physical and mental functioning ‐ similar to those seen with chronic diseases such as diabetes (Hays 1995; Wells 1989). In addition, mood disorders have been shown to have a greater impact on quality of life when compared with conditions such as hypertension and cardiac disease (Spitzer 1995). Depression is associated with considerable financial costs for health services and for society. The economic burden in England is estimated to exceed £9 billion per annum, with approximately £370 million accounting for direct costs of treatment (Thomas 2003).
Description of the intervention
Major depression is a discrete episode of severe depression; when it is gone, the person is described as being in remission and feeling completely normal. Dysthymia is a pervasive 'low‐level' depression that lasts a long time ‐ frequently for a few years. Treatment approaches are the same for both conditions. Most depressed patients are treated in primary care and do not require hospitalisation. In primary care, depression is most often managed with antidepressants (Goldman 1999). A range of psychological interventions, including cognitive‐behavioural therapies, interpersonal therapy, psychotherapy, and counselling, are also available. Surveys have shown that Australians report a preference for self‐help and complementary therapies for depression (Jorm 1997;Jorm 2000), and depressed persons in the United States report greater use of complementary therapies (Kessler 2000).
Acupuncture has a long history of use in China, Japan, and Korea. Contemporary acupuncture practice is commonly undertaken as part of the medical hospital system in modern China (Robinson 2012), as part of traditional Korean medicine in South Korea (Woo 2014), and as a mix of hospital and private practice in the United Kingdom (Hopton 2012). Traditional Chinese Medicine theory describes a state of health maintained by a balance of energy within the body. Acupuncture involves insertion of fine needles into different parts of the body to correct the imbalance of energy within the body. Styles of acupuncture range from traditional/classical acupuncture to auricular acupuncture, to trigger point acupuncture, to single‐point acupuncture. Acupuncture is practised under several theoretical frameworks. Traditional Chinese Medicine (TCM) and Classical Acupuncture are based on theoretical concepts of Yin and Yang and the Five Elements and explain disease and physiological function. A westernised medical application of acupuncture involves use of trigger points, segmental points, and commonly used formula points. Medical acupuncture may involve application of acupuncture based on the principles of neurophysiology and anatomy, rather than on TCM principles and philosophy. Auricular therapy involves using the ear to make a diagnosis and subsequent needling to points on the ear. Electro‐acupuncture is defined as application of a small current through acupuncture needles. Laser acupuncture is a non‐penetrative form of acupuncture that uses low‐power laser light to stimulate acupuncture points. The rationale for treatment will determine the needling details (e.g. selection of points, number of needles used) and the method of stimulation (e.g. manual acupuncture, electro‐acupuncture, laser acupuncture). Different styles of acupuncture may differ in their effectiveness, but little research has been conducted to directly examine effects on clinical outcomes when these parameters are changed (Armour 2016; Lin 2016).
Acupuncture is not entirely free of adverse events. Two large prospective surveys have been undertaken in the United Kingdom (MacPherson 2004; White 2001). White 2001 reported an incidence of 684 adverse events per 10,000 consultations. Most were minor events such as bleeding, needling pain, or aggravation of symptoms, and investigators have reported a low rate of significant adverse events (14 per 10,000). MacPherson 2004 reported a rate of 107 adverse events per 1000 participants (95% confidence interval (CI) 100 to 115). Three participants reported a serious adverse event. Events most commonly reported were severe tiredness and exhaustion, pain at the site of needling, and headache. White 2004 summarised the range and incidence of adverse events associated with acupuncture. Twelve prospective studies undertaken in the UK, Germany, Singapore, Japan, and Sweden surveyed more than a million treatments and found that risk of a serious adverse event with acupuncture was estimated to be 0.05 per 10,000 treatments, and 0.55 per 10,000 individual patients. Data from these studies suggest that the risks associated with acupuncture are few ‐ a point reinforced by Vincent 2001, which concluded that acupuncture is safe in competent hands.
How the intervention might work
The cause of depression appears to be multi‐factorial, and biological and psychosocial factors are involved (Davidson 2002). Various interdependent biological components have been implicated in the onset and maintenance of MDD. Current models suggest that changes in the hypothalamic‐pituitary‐adrenal (HPA) axis, dysfunction among stress hormones, and disequilibrium in neurotransmitters such as noradrenaline, serotonin, and dopamine may be key factors (Hou 2016).
Several mechanisms may explain the therapeutic effects of acupuncture within the current model of depression. Strong evidence obtained over the past three decades indicates that effects of acupuncture are mediated by various neurotransmitters, predominantly the endogenous opioid mechanism (EOM), catecholamines, and serotonin, and that an estimated 20 to 30 other neuropeptides are affected (Leung 2014). Results from animal experiments suggest that, similar to antidepressant medications, acupuncture is capable of affecting neurotransmitter levels of serotonin and noradrenaline, along with the adenylate cyclase‐cyclic adenosine monophosphate‐protein kinase A (AC‐cAMP‐PKA) cascade within the central nervous system (Leung 2014). In addition, acupuncture has produced structural and functional magnetic resonance imaging (fMRI) changes (as described by Huang 2012) in the default mode network, anterior cingulate cortex, and amygdala‐hippocampal formation (Liu 2009). Dysfunction in these areas of the brain has been previously implicated in depressive disorders (Hamilton 2015). Manual acupuncture causes a broad range of central nervous system responses involving the amygdala, hippocampus, hypothalamus, cerebellum, and other limbic structures as seen on fMRI and electroencephalography (EEG) (Napadow 2005). Electro‐acupuncture is thought to deliver a greater 'dose' of acupuncture compared with manual acupuncture, as a result of the duration and intensity of stimulation, and to cause greater activation of endogenous opoid mechanisms (Mayor 2013). This may or may not lead to greater clinical effects in non‐pain‐related conditions (Langevin 2015;Mayor 2013). The mechanism of laser acupuncture remains unclear, but proposed models involve changes in gene expression mediated via changes in nitric oxide (Chung 2012).
Why it is important to do this review
An increasing body of research is focussed on assessing the effectiveness of acupuncture. In 2005, we published the first version of this systematic review and concluded that evidence was insufficient for determination of the efficacy of acupuncture. An update was published in 2010. Since that time, new trials have been published and we have gained comprehensive access to a large body of relevant literature from China.
Objectives
To examine the effectiveness and adverse effects of acupuncture for treatment of individuals with depression.
To determine whether acupuncture is more effective than treatment as usual/no treatment/wait list control for treating and improving quality of life for individuals with depression.
To determine whether acupuncture is more effective than control acupuncture for treating and improving quality of life for individuals with depression.
To determine whether acupuncture is more effective than pharmacological therapies for treating and improving quality of life for individuals with depression.
To determine whether acupuncture plus pharmacological therapy is more effective than pharmacological therapy alone for treating and improving quality of life for individuals with depression.
To determine whether acupuncture is more effective than psychological therapies for treating and improving quality of life for individuals with depression.
To determine adverse effects of acupuncture compared with treatment as usual/no treatment/wait list control, control acupuncture, pharmacological therapies, and psychological therapies for treatment of individuals with depression.
Methods
Criteria for considering studies for this review
Types of studies
We sought to include all relevant published and unpublished randomised controlled trials (RCTs). We excluded cross‐over trials owing to uncertainty regarding the period allowed for washout before acupuncture treatment. We included cluster‐randomised trials and excluded quasi‐randomised trials that used non‐random methods of treatment assignment such as date of admission (see Differences between protocol and review).
Types of participants
Characteristics
We included studies of people of either gender and of any ethnicity, aged 16 years or older, with clinically diagnosed depression as the primary condition or as a comorbidity.
Diagnosis
We included studies in which investigators diagnosed depression using one or more of the following criteria: depression defined by the Diagnostic and Statistical Manual of Mental Disorders (Third Edition (DSM‐III), Fourth Edition (DSM‐IV), or Fifth Edition (DSM‐5); APA 2015), or the Research Diagnostic Criteria (RDC; Spitzer 1977), or the International Statistical Classification of Diseases and Related Health Problems (ICD; WHO 1993), or the Chinese Classification of Mental Disorders (Second Edition (CCMD‐2) or Third Edition (CCMD‐3); Chinese Psychiatric Society 2001). If necessary, we used trial authors' definitions of depressive disorder. We included both major depression and dysthymia.
Comorbidities
As long as depression was the main focus of the trial, studies that involve participants with comorbid physical or common mental disorders were eligible for inclusion.
Treatment setting
All settings ‐ primary, secondary, tertiary, and community ‐ were eligible for inclusion.
Types of interventions
Experimental interventions
Manual acupuncture: involves stimulation of anatomical points on the body through penetration of the skin with thin, solid, metallic needles that are manipulated by the hands. Also included is auricular acupuncture ‐ insertion of needles into points located on the ear
Electro‐acupuncture: involves passing a pulsed current through the body through acupuncture needles
Laser acupuncture: use of a low‐level laser beam instead of an acupuncture needle to stimulate an acupuncture point
Comparator interventions
We included in this review five main categories of trial comparison groups. We excluded trials that did not include one of the following comparison groups. We classified the comparator group in each study as follows.
Wait list control/treatment as usual/no treatment.
-
Control acupuncture.
-
Invasive acupuncture control.
Sham acupuncture, which consists of insertion of a needle into a non‐acupuncture point.
Minimal acupuncture, in which needles are inserted into non‐acupuncture points but more superficially, without stimulation or manipulation, to avoid the needling sensation known as 'de qi'.
Non‐invasive acupuncture control: includes use of the placebo needle, which is a blunted needle that looks as if it is piercing the skin yet does not; two forms are available (Park 2002;Streitberger 1998).
Mock electro‐acupuncture: involves using a de‐commissioned acupuncture stimulation unit and fixing electrodes to the skin with the switch turned off.
Mock laser acupuncture.
-
-
Antidepressants ‐ organised into classes for the purposes of this review.
Selective serotonin reuptake inhibitors (SSRIs): zimelidine, fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram, escitalopram.
Tetracyclic antidepressants (TCAs): amitriptyline, imipramine, trimipramine, doxepin, desipramine, protriptyline, nortriptyline, clomipramine, dothiepin, lofepramine.
Heterocyclic antidepressants: mianserin, trazodone, amoxapine, maprotiline.
Monoamine oxidase inhibitors (MAOIs): irreversible: phenelzine, tranylcypromine, izocarboxazid; reversible: brofaromine, moclobemide, tyrima.
Other antidepressants: noradrenaline reuptake inhibitors (NARIs): reboxetine, atomoxetine; norepinephrine‐dopamine reuptake inhibitors (NDRIs): amineptine, bupropion; serotonin‐norepinephrine reuptake inhibitors (SNRIs): trazodone; unclassified: agomelatine, vilazodone.
-
Combination therapy by which the same adjunct therapy was delivered to all study groups.
Acupuncture plus medication versus medication.
-
Psychological therapies.
Cognitive‐behavioural therapy (CBT).
Behavioural therapy (BT).
Psychotherapy.
Counselling.
Types of outcome measures
Primary outcomes
Reduction in the severity of depression, measured at the end of the intervention primarily as a continuous variable on self‐rating scales such as the Beck Depression Inventory (BDI) (Beck 1961), or on clinician‐rated scales, such as the Hamilton Depression Rating Scale (HAMD) ‐ as discussed in Hamilton 1960
Total numbers of adverse events
Secondary outcomes
Remission of depression as defined in trial reports and based on the HAMD or another clinician‐rated scale of depression severity and reported as a binary outcome
Quality of life indices (e.g. Short Form Health Survey (SF‐36); Ware 1994), with individual domains related to quality of life, for example, physical and emotional well‐being, reported
Change in use of medication or use of other support systems, measured as additional treatment provided, number of appointments attended, etc.
Dropouts from treatment, defined as failure to complete, including number of individuals leaving each study early and reasons for early dropout
Timing of outcome assessment
The primary time frame for reporting primary and secondary outcomes is at completion of the intervention. If a study reported several time points during the time frame (i.e. during treatment), we reported the last observation before treatment completion. We included all time frames and grouped them as follows.
During the treatment period.
At the conclusion of the treatment period.
Between zero and six months after conclusion of the treatment period (short term).
Between six and 12 months after conclusion of the treatment period (medium term).
Longer than 12 months after conclusion of the treatment period (long term).
Hierarchy of outcome measures
We treated equally five scales commonly used for assessment of depression: the Beck Depression Inventory (BDI; Beck 1961); the Hamilton Depression Rating Scale (HAMD; Hamilton 1960); the Patient Health Questionnaire (PHQ; Spitzer 1999); the Montgomery‐Asberg Depression Rating Scale (MADRS; Montgomery 1979); and the Clinical Global Impression‐Severity Scale (CGI‐S). We rated all other depression scales lower. If investigators used two or more of these scales, we applied the following hierarchy: (1) HAMD; (2) MADRS; (3) CGI‐S; (4) BDI; (5) PHQ; and (6) all other depression scales. Owing to the difficulty of participant blinding often seen in acupuncture trials, we gave preference to clinician‐rated scales when both clinician‐rated and self‐reported outcomes were provided.
If a study employed more than one quality of life measure, we applied the following hierarchy of scales: (1) World Health Organization Quality of Life (WHOQOL; WHO 1998); (2) Short Form Health Survey (SF‐36; Ware 1994); and (3) any other quality of life measures used.
We included both clinician‐rated and self‐reported outcomes in the same analysis; however, if investigators reported both, we used clinician‐rated scales in preference. If investigators presented no clinician‐rated outcomes, we used a self‐reported outcome. Each group did not include enough trials for these outcomes to be reported separately via subgroup analysis.
Search methods for identification of studies
Cochrane Specialised Registers: Cochrane Common Mental Disorders Clinical Trials Register (CCMD‐CTR)
The Cochrane Common Mental Disorders Group maintains a specialised register of randomised controlled trials ‐ the CCMD‐CTR. This register contains more than 39,000 reference records (reports of RCTs) on depression, anxiety, and other common mental disorders. A percentage of the reference records have been tagged to 12,500 individual, PICO‐coded study records (with coding based on the EU‐PSI (Evidence‐Based Treatment in Mental Health and Optimised Use of Databases) Coding Manual). Reports of RCTs for inclusion in the Register are collated from (weekly) generic searches of MEDLINE, Embase, and PsycINFO; quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); and review‐specific searches of additional databases. Reports of trials were also derived from international trial registries and drug companies; through handsearching of key journals; and via electronic searches of conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. Details of core CCMD search strategies can be found on the CCMD Group website.
Electronic searches
We searched the CCMD‐CTR (studies and references) (all years to 10 June 2016) using the following terms: ((acupunct* or acupress* or acupoints* or electroacupunct* or electro‐acupunct* or auriculotherap* or auriculoacupunct* or moxibust*) and (depress* or "affective disorder*" or "affective symptoms" or mood)):ti,ab,kw,ky,emt,mh,mc.
We did not systematically search Chinese language‐only databases for this version of the review; therefore trials meeting our selection criteria beyond those identified may exist. We identified a significant number of Chinese language trials through other search strategies (reported above), and a large number did not meet the inclusion criteria.
We searched the following eight electronic Korean medical databases using the same terms as above, without restricting language, from their respective inceptions up to June 2016: the Korean Studies Information Service System (KISS), Korean article database website (DBPIA), Korea Institute of Science and Technology Information, the Research Information Service System (RISS), Korea Med, the Korean Medical Database (KM Base), and the Oriental Medicine Advanced Searching Integrated System (OASIS). In addition, we searched the following Korean language journals: Journal of Korean Medicine, Korean Journal of Acupuncture, Journal of Pharmacopuncture, Journal of Acupuncture and Meridian Studies, Korean Journal of Joongpoong, Journal of Korean Acupuncture & Moxibustion Medicine Society, Journal of Korean Oriental Internal Medicine, Journal of Oriental Obstetrics and Gynecology, Journal of Society of Korean Medicine for Obesity Research, Journal of Oriental Neuropsychiatry, and Journal of Sasang Constitutional Medicine.
We applied no restrictions on publication date or status when conducting these searches.
We searched international trial registries via the World Health Organization trials portal (ICTRP), the Chinese clinical trial registry (www.chictr.org.cn), and the US National Library of Medicine database (ClinicalTrials.gov) to identify unpublished and ongoing studies.
Searching other resources
Grey literature
We searched sources of grey literature including dissertations and theses, clinical guidelines, and reports from regulatory agencies (when appropriate).
ProQuest Dissertations and Theses Database.
National Guideline Clearing House (http://guideline.gov).
OpenGrey (http://www.opengrey.eu/).
Handsearching
We handsearched relevant conference proceedings by referring to lists of publications in manuscripts.
Reference lists
We checked the reference lists of all included studies and relevant systematic reviews to identify additional studies missed by the original electronic searches (e.g. unpublished or in‐press citations). We conducted a cited reference search on the Web of Science.
Correspondence
We contacted trialists and subject experts to ask for information on unpublished or ongoing studies, or to request additional trial data.
Data collection and analysis
Selection of studies
Two review authors (of CS, MA, PH, HM, MS, L‐QW) reviewed all articles. Review authors independently screened titles and abstracts for potential inclusion of all studies identified as a result of the search and coded them as 'retrieve' (eligible or potentially eligible) or 'do not retrieve'. We retrieved full‐text study reports/publications, and two review authors (for all authors of the review) independently screened full‐texts, identified studies for inclusion, and identified and recorded reasons for exclusion of ineligible studies. We resolved disagreements through discussion or, if required, consulted a third review author (of PH, HM, CS). We identified and excluded duplicate records and collated multiple reports related to the same study, so that each study rather than each report is the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram.
Data extraction and management
Following assessment for inclusion, we assessed the methods used by each trial. All review authors independently extracted onto hard copy data sheets trial data on participants, methods, interventions, outcomes, and results. We sought missing data or clarification of study details from respective trial authors by mail or by email.
Main planned comparisons
Acupuncture versus wait list control/treatment as usual/no treatment
Acupuncture versus control acupuncture
Acupuncture versus pharmacological therapies
Acupuncture plus medication versus medication alone
Acupuncture versus psychological therapies (including counselling)
Assessment of risk of bias in included studies
Two or more review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion or by consultation with a third party, when necessary. We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
We judged each potential source of bias as high, low, or unclear and provided a supporting quotation from the study report together with a justification for our judgement in the 'Risk of bias' table. We summarised risk of bias judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes when necessary (e.g. for unblinded outcome assessment). When information on risk of bias was related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for studies that contributed to that outcome. For assessments of overall quality of the evidence for each outcome that included pooled data, we used the GRADE method to determine evidence quality, downgrading evidence from high quality by one level for serious (or two for very serious) issues with risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates, or potential publication bias.
Measures of treatment effect
We performed statistical analysis using Review Manager 5 (Revman 2014) software.
We undertook a statistical summary of the data and expressed dichotomous data as risk ratios (RRs) with corresponding 95% confidence intervals (95% CIs). We expressed continuous data as mean differences (MDs) with 95% CIs, or as standardised mean differences (SMDs) if outcomes were conceptually the same but were measured in different ways, for example, by using different instruments (e.g. BDI, HAMD).
Unit of analysis issues
Trials with multiple groups
We included trials with multiple groups and described them in the Characteristics of included studies table. For example, acupuncture might be compared with sham acupuncture, and with no acupuncture in another study group. If investigators included two acupuncture groups, we combined data from both treatment groups. For studies using a sham control and including no treatment control group, we evenly divided shared interventions between groups, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When outcomes were repeated measures, we conducted analysis of outcomes at completion of the intervention.
Cluster‐randomised trials
We included cluster‐randomised trials in analyses along with individually randomised trials. We adjusted their[sample sizes or standard errors] using methods described in the Cochrane Handbook for Systematic Reviews of Interventions [Section 16.3.4 or 16.3.6] and provided an estimate of the intracluster correlation coefficient (ICC) derived from trial data (if possible), from a similar trial, or from a study of a similar population. If we used ICCs from other sources, we reported this and conducted sensitivity analyses to investigate effects of variation in the ICC. If we identified both cluster‐randomised and individually randomised trials, we planned to synthesise relevant information. We considered it reasonable to combine results from both types of trials if we noted little heterogeneity between study designs, and if we considered interaction between effects of the intervention and choice of the randomisation unit unlikely. We also acknowledged heterogeneity in the randomisation unit and performed a subgroup analysis to investigate effects of the randomisation unit.
Dealing with missing data
We contacted investigators or study sponsors to verify key study characteristics and to obtain missing numerical outcome data when possible (e.g. when we identified a study in abstract format only). We documented all correspondence with trialists and reported in the full report which trialists responded. When it was unclear whether an intention‐to‐treat (ITT) analysis was performed, we contacted trial authors to request confirmation. In most cases, we obtained extracted data directly from the study itself; these data may represent available case data only. If possible, we calculated data using methods that enable this (e.g. if standard deviations are missing, it may be possible to calculate these from confidence intervals, standard errors, t values, or the like, using methods outlined in Higgins 2011, Section(s) 7.7.3.2 and 7.7.3.3). We sought statistical advice on imputation and attempted this only if most trials in the meta‐analysis provided complete statistics (Higgins 2011).
Assessment of heterogeneity
We investigated heterogeneity between studies by using the I2 statistic (I2 greater than or equal to 50% was considered indicative of heterogeneity). We formally tested heterogeneity by examining the P value of the I2 statistic. When determining the importance of heterogeneity, we took into account the magnitude and direction of effects; and the strength of evidence for heterogeneity (the P value from the Chi2 test or the width of the confidence interval for the I2 statistic).
We interpreted the I2 statistic as follows.
10% to 40%: might not be important.
30% to 60%: may represent moderate heterogeneity.
50% to 90%: may represent substantial heterogeneity.
75% to 100%: considerable heterogeneity.
When we detected heterogeneity greater than 75%, we rechecked the data and if necessary contacted study authors to confirm the accuracy of data as reported in the journal article.
Assessment of reporting biases
Reporting biases arise when dissemination of research findings is influenced by the nature and direction of results (Higgins 2011). We investigated potential biases of publication using the funnel plot or another analytical method (Egger 1997). If we included 10 or more studies in the meta‐analysis, we investigated reporting biases (such as publication bias) by assessing funnel plot asymmetry visually. If asymmetry was suggested by visual assessment, we explored possible reasons by performing the tests proposed in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Data synthesis
We used a random‐effects model to pool the results of all studies because this model is more conservative than a fixed‐effect model, and it incorporates both within‐study and between‐study variance. This change from the original protocol was due to the heterogeneity of studies.
If data were not reported in a form that would allow inclusion in the meta‐analysis, we reported the findings narratively.
Subgroup analysis and investigation of heterogeneity
Effects of acupuncture may be influenced by mode of stimulation and style of acupuncture administered. We planned to undertake prespecified subgroup analysis to examine effects of the mode of acupuncture stimulation used (i.e. manual, electro‐acupuncture, or laser); and different acupuncture styles applied (e.g. classical/traditional acupuncture vs single‐point therapy, auricular acupuncture). We also planned to conduct a subgroup analysis of different forms of acupuncture by using a classification of invasive and non‐invasive controls that may be influenced by bias derived from unblinding and physiological activity.
When we identified other psychological and pharmacological interventions, we planned to conduct subgroup analysis for the control groups (i.e. CBT vs BT or TCA vs SSRI). We planned to conduct other subgroup analyses to explore effects of treatment among people with different diagnoses (e.g. major depression, dysthymia) and people of different ages (< 65 years and ≥ 65 years).
We planned to conduct an a posteriori subgroup analysis to examine effects of the number of acupuncture treatment sessions provided (< 20 sessions and ≥ 20 sessions) and another analysis to examine outcomes of clinician‐rated versus self‐rated depression scales. We were unable to perform any of the subgroup analyses planned, as all subgroups included too few studies (fewer than five studies).
Sensitivity analysis
A priori, we planned to perform sensitivity analyses of results to look at the possible contribution of:
excluding trials that did not clearly report the randomisation process;
excluding trials with unclear concealment of random allocation; and
excluding trials reporting dropout greater than 20%.
We planned to perform an a posteriori sensitivity analysis to examine the contribution of overall trial quality by excluding trials rated as having overall high risk. We defined trials as having overall high risk if they had high risk of bias in any two or more domains. We defined trials as having overall low risk if they had low risk of bias for randomisation, allocation, and both performance and detection blinding.
'Summary of findings' tables
We prepared 'Summary of findings' tables using GRADEproGDT. These tables present the overall quality of the body of evidence for five comparisons reporting on primary review outcomes at completion of the intervention (severity of depression, adverse events), according to GRADE criteria (study limitations, consistency of effect, imprecision, indirectness, and publication bias). We justified, documented, and incorporated into reporting of results judgements about evidence quality (high, moderate, low) for each outcome.
Results
Description of studies
Results of the search
In total, we retrieved 559 articles through updated searches, and 559 remained after de‐duplication. Two review authors (CS, HM) read the titles and abstracts of all articles retrieved in English, one review author read those provided in Korean (MSL), and another review author read those written in Chinese (LQW). Another review author (PH) resolved discrepancies. We excluded 268 articles on the basis of title or abstract and retained 291 articles for inspection of the full‐text article for eligibility. We excluded a total of 227 studies after reading the full text; we have included in the Excluded studies section only studies reviewed on the basis of title or abstract that did not meet the review inclusion criteria. We included 34 new trials and excluded another 42 studies.
The previous version of this review included 30 trials and excluded 11 trials. See Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification, and Characteristics of ongoing studies. This update includes 64 studies with 7104 participants and excludes 53 studies. See Figure 1.
1.

Study flow diagram.
Included studies
Design
All trials used a parallel‐group design, 43 trials included two groups (acupuncture plus a control group), and 21 trials included three groups. We adjusted the unit of analysis for trials including multiple groups on the basis of the description of study methods provided.
Control groups varied between studies according to the research question. A total of 43 trials used medication alone, and four used control acupuncture combined with medication. Two trials used counselling, one trial usual care, and three trials a wait list. Control acupuncture groups included in four trials used sham inactive laser or electro‐acupuncture technique, four used the non‐invasive placebo sham needle, and three used both minimal and sham types of acupuncture.
Sample size
Sample sizes of studies included in this review ranged from 19 in Whiting 2008 to 755 in MacPherson 2013, with a median of 75 participants in each study.
Setting
A total of 51 studies were undertaken in China, three in the USA, three in Hong Kong, three in Germany, two in Australia, and two in the United Kingdom. Eleven studies recruited participants from both inpatient and outpatient hospital settings, 20 from inpatient settings, 16 from outpatient settings only, and six from the community via advertising or primary care settings; in 11 trials, the setting was unclear.
Participants
Trials recruited participants who met the diagnostic criteria for depression, or who had a clinical presentation of depression as defined by trial authors. Thirteen trials used the DSM (II, III, IV, or V), 33 used the CCMD (2 or 3), and eight used ICD Tenth Revision (ICD‐10) criteria. Ten trials recruited participants on the basis of a clinical presentation of depression. Two trials recruited participants only on the basis of BDI scores ≥ 12, and four used HAMD scores alone. Two trials used the Zung Self‐rating Depression Scale (SDS), one used the Clinical Interview Schedule Revised (CIS‐R; Whiting 2008), and one used Chinese Neuroscience Society diagnostic guidelines (He 2005). Inclusion criteria in addition to ICD‐10, DSM, or CCMD diagnosis were specified as HAMD score > 18 in 29 trials and HAMD score < 18 in five trials; remaining trials did not report a specific required HAMD score for entry.
Interventions
Trials delivered acupuncture that varied in terms of point selection, frequency of treatment, and total number of treatments administered. Most trials (46) used a standardised treatment protocol with a fixed selection of points administered at each acupuncture session. Selection of points varied and included acupuncture points located on arms, legs, abdomen, and head. Fourteen trials used a semi‐standardised treatment protocol consisting of a predefined set of acupuncture points used in combination with acupuncture points selected on the basis of diagnosis and identification of symptomatic patterns. Four trials administered individualised treatment for study participants on the basis of their diagnosis.
A total of 42 trials reported needling duration between 20 and 30 minutes. Needling duration was 30 to 60 minutes in 10 trials. Twelve trials provided no or unclear details.
Three trials provided fewer than 10 sessions, 19 trials between 12 and 18 sessions, and 38 trials between 21 and 60 sessions; four trials did not report the number of sessions. Included trials provided a median of 30 sessions.
One trial provided twice‐daily treatment (He 2007), and 12 trials reported daily treatment. Nineteen trials treated participants five or six days per week. Twenty‐six trials treated participants one to three times a week, and in six trials, treatment frequency was unclear. Some trials started with more frequent treatments before reducing frequency to weekly sessions.
Twenty‐five trials were of six weeks' duration, 17 were of six and a half to 12 weeks' duration, and 17 were of less than six weeks' duration. Duration of treatment was unclear in five trials.
Most trials (42) used manual acupuncture, 13 used electro‐acupuncture, seven used a combination of manual and electro‐acupuncture, and two used laser acupuncture.
Outcomes
Most trials assessed depression using HAMD as the primary outcome measure. Fifty‐four trials used HAMD as the primary outcome measure. Two trials used BDI as the primary outcome, two used CGI‐S, two used SDS, one used Symptom Checklist‐90 (SCL‐90), one used PHQ‐9, and two used a custom scale.
Excluded studies
We excluded 53 trials (see Characteristics of excluded studies). Fourteen studies did not meet the inclusion criteria for the control group (as specified in the methods) owing to a suboptimal dose of medication, lack of a suitable comparison group (as outlined under Types of interventions), or the fact that a non‐specified control group was used. Twenty trials provided data from participants who did not meet the diagnosis for depression. Three trials were duplicate publications in another language or used the same data set as included trials. One trial examined the effect of acupuncture on autonomic function in patients with depression or anxiety, and one trial examined the effect of acupuncture on menopausal symptoms in women with depression. Neither of these studies treated or evaluated the effect of acupuncture on depression. Three trials were quasi‐randomised; five used an intervention that was combined with another active intervention such as herbs; and six were identified as not randomised. We have presented further background information on these trials in the Characteristics of excluded studies section.
Ongoing studies
We identified 14 trials from clinical trial registries as ongoing (see Characteristics of ongoing studies).
Studies awaiting classification
We classified 17 trials as awaiting classification. Fourteen trials were awaiting confirmation of randomisation details, results of two studies were not available, the diagnosis was unclear in one study, and details of treatment required clarification in another trial (see Studies awaiting classification).
New studies found at this update
This update includes 34 new trials (Andreescu 2011;Bosch 2015;Chung 2015;Du 2005;Duan 2011;Fan 2013;Feng 2011;Fu 2006;He 2012;Huang 2013;Li 2008;Li 2011b;Lin 2012;Liu 2006;Liu 2013a; Liu 2015;Lv 2015;Ma 2011;Ma 2012;MacPherson 2013;Pei 2006;Qiao 2007;Qu 2013;Quah‐Smith 2013;Sun 2010;Sun 2013;Sun 2015b;Wang 2014;Wang 2015;Xiao 2014;Xu 2011;Yeung 2011b;Zhang 2005a;Zhang 2007a;Zhang 2009;Zhang 2012), for a total of 64 included trials. We excluded 42 trials since the last update (Arvidsdotter 2014; Bennett 1997; Bergmann 2014; Bin 2007; Carvalho 2013; Chang 2009; Chang 2010, Cocchi 1977; Deng 2013; Dormaemen 2011; Duan 2009;Fan 2015b;Guo 2009;He 2011; Hmwe 2015; Honda 2012; Hou 1996; Hu 2013; Huang 2003;Huo 2013; Khang 2002; Kim 2015; Li 2011; Liu 2013;Man 2014; Mischoulon 2012; Niu 2006; Shi 2014;Sun 2012; Tang 2003b; Tse 2010; Wang 2003; Wang 2006; Wang 2015; Wu 2010; Xie 2009; Xie 2012; Yeung 2011; Zhang 2004; Zhang 2004b; Zhao 2014; Zhou 2015), for a total of 53 excluded trials.
Risk of bias in included studies
See Figure 2 and Figure 3 for a graphical summary of risk of bias assessments performed by review authors for the 64 included studies, based on the seven risk of bias domains. Trial authors described three trials as having low risk of bias for all domains (Andreescu 2011;Chung 2015; Yeung 2011b). Four trials were at low risk of bias for five domains.
2.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.

Review authors' judgements about each 'risk of bias' domain for each included study.
Investigators described all trials as randomised.
Allocation
Using Cochrane criteria that rate the adequacy of random allocation concealment, we rated most trials as having low risk (75%; n = 48) and rated no trials as having high risk of bias.
A total of 22 trials used a randomisation sequence that was computer generated, 30 used random tables, two used lot drawing, and Quah‐Smith 2005 used coded beans.
A total of 18 trials assessed allocation concealment as being at low risk of bias; in most trials (46), this was unclear. Five trials performed central randomisation, and 11 trials reported using sealed opaque envelopes. Forty‐six trials did not report the method of allocation, or we assessed their risk as unclear.
Blinding
We assessed blinding as providing low risk of performance bias in 14 trials. Most trials involved comparisons of acupuncture versus medication and could not be blinded; this contributed to assessment of high risk. We assessed a total of 48 trials as having high risk for performance bias. For studies comparing acupuncture versus a sham or placebo acupuncture control, we sought evidence of verification of blinding of participants. We rated 10 trials as having low risk of detection bias. Most trials (35) did not report on blinding of the assessor/clinician or the analyst or used patient‐reported outcome measures.
Incomplete outcome data
We assessed most (37) trials as having low risk of bias for outcome reporting. Eight trials were at high risk owing to dropout or incomplete data ,and reporting bias was unclear in 19 trials. We rated trials as having high risk of bias if dropout rates were uneven between groups and the reason for dropout was related or suspected to be related to group allocation. We also rated trials as having high risk for bias if investigators reported a dropout rate > 20% and did not report how they dealt with this (e.g. ITT analysis, last observation carried forward).
Selective reporting
We rated risk of bias from selective reporting as unclear for most trials owing to no available study protocol. We rated two trials as having high risk of bias and found that Li 2007 did not report data on all included outcomes.
Other potential sources of bias
Risk of bias was unclear for most trials (31). We rated risk from other sources of bias as low for 29 trials. We assessed an imbalance at randomisation in eight trials (Allen 1998;Ding 2003;Fan 2005;Fu 2008;Luo 1988;Luo 1998;Whiting 2008;Xiujuan 1994). We rated trials at high risk of bias if we noted significant baseline imbalance between groups, and at unclear risk if trial authors did not report a baseline analysis.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
Summary of findings for the main comparison. Acupuncture compared with no treatment/wait list/treatment as usual for depression.
| Acupuncture compared with no treatment/wait list/treatment as usual for depression | ||||||
| Patient or population: clinical diagnosis of depression Setting: community/outpatient/inpatient Intervention: acupuncture Comparison: no treatment/wait list/treatment as usual | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no treatment/wait list/treatment as usual | Risk with acupuncture | |||||
| Severity of depression at the end of treatment assessed with various clinician‐rated and self‐rated outcome measures (lower score indicates less severe depression) | SMD 0.66 lower (1.06 lower to 0.25 lower) | ‐ | 488 (5 RCTs) | ⊕⊕⊝⊝ LOWa,b | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events | Study population | RR 0.89 (0.35 to 2.24) | 302 (1 RCT) | ⊕⊕⊝⊝ LOWc,d | ||
| 60 per 1000 | 53 per 1000 (21 to 134) | |||||
| Quality of life (physical) | ‐ | ‐ | ‐ | ‐ | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| Quality of life (emotional) | ‐ | ‐ | ‐ | ‐ | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level owing to high risk of performance bias across most included studies.
bDowngraded one level owing to substantial heterogeneity (I2 = 64%, Tau2 = 0.14, P = 0.02).
cDowngraded one level owing to high risk of performance bias.
dDowngraded one level owing to small sample size for detecting relatively rare events.
Summary of findings 2. Acupuncture compared with control acupuncture for depression.
| Acupuncture compared with control acupuncture for depression | ||||||
| Patient or population: clinical diagnosis of depression Setting: community/outpatient/inpatient Intervention: acupuncture Comparison: control acupuncture | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with control acupuncture | Risk with acupuncture | |||||
| Severity of depression at the end of the intervention as measured by the Hamilton Depression Rating Scale (HAMD) scored from 0 to 54 (lower score indicates less severe depression) | In the study population, average severity of depression at the end of treatment was 11.4 in clinician‐rated HAMD scores. | MD 1.69 lower (3.33 lower to 0.05 lower) | ‐ | 841 (14 RCTs) | ⊕⊕⊝⊝ LOWa,b | |
| Adverse events | Study population | RR 1.63 (0.93 to 2.86) | 300 (5 RCTs) | ⊕⊕⊕⊝ MODERATEc | ||
| 162 per 1000 | 264 per 1000 (151 to 463) | |||||
| Quality of life (physical) at the end of treatment (higher scores indicate greater quality of life) | Mean quality of life (physical) at the end of treatment was 37. | MD 5.12 lower (10.38 lower to 0.13 higher) | ‐ | 150 (1 RCT) | ⊕⊕⊝⊝ MODERATEd | |
| Quality of life (emotional) at the end of treatment (higher scores indicate greater quality of life) | Mean quality of life (emotional) at the end of treatment was 44.6. | MD 2.25 lower (5.89 lower to 1.39 higher) | ‐ | 167 (2 RCTs) | ⊕⊕⊕⊝ MODERATEe | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HAMD: Hamilton Depression Rating Scale; MD: mean difference; RCTs: randomised controlled trials; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level owing to high risk of bias in performance bias in five of the included studies and high risk of bias in at least one domain in most studies.
bDowngraded one level owing to substantial heterogeneity (I2 = 80%, Tau2 = 7.80, P < 0.001).
cDowngraded one level owing to small sample size for relatively rare events.
dDowngraded one level because only one small study contributed to this outcome.
eDowngraded one level for imprecision due to small sample size.
Summary of findings 3. Acupuncture compared with medication for depression.
| Acupuncture compared with medication for depression | ||||||
| Patient or population: clinical diagnosis of depression Setting: community/outpatient/inpatient Intervention: acupuncture Comparison: medication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with medication | Risk with acupuncture | |||||
| Severity of depression at the end of treatment assessed with various clinician‐rated and self‐rated outcome measures (lower score indicates less severe depression) | SMD 0.23 lower (0.4 lower to 0.05 lower) | ‐ | 3127 (31 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events (measured with Asberg Antidepressant Side Effect Scale) | Mean number of adverse events was 6.2. | MD 4.32 lower (7.41 lower to 1.23 lower) | ‐ | 481 (3 RCTs) | ⊕⊝⊝⊝ VERY LOWc,d | |
| Quality of life (physical) | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome | |
| Quality of life (emotional) | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCTs, randomised controlled trials; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels owing to very serious risk of bias. Of 31 trials, 30 were at high risk of bias owing to lack of blinding of participants, and 12 were at high risk of bias owing to lack of blinding of outcome assessors.
bDowngraded one level owing to substantial heterogeneity (I2 = 80%, Tau2 = 0.19, P < 0.0001).
cDowngraded two levels owing to very serious risk of bias in all three studies.
dDowngraded two levels owing to considerable heterogeneity (I2 = 97%, Tau2 = 7.22, P < 0.001).
Summary of findings 4. Acupuncture plus medication compared with medication for depression.
| Acupuncture plus medication compared with medication for depression | ||||||
| Patient or population: clinical diagnosis of depression Setting: community/outpatient/inpatient Intervention: acupuncture plus medication Comparison: medication | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with medication | Risk with acupuncture plus medication | |||||
| Severity of depression at the end of treatment assessed with various clinician‐rated and self‐rated outcome measures (lower score indicates less severe depression) | SMD 1.15 lower (1.63 lower to 0.66 lower) | ‐ | 813 (11 RCTs) | ⊕⊝⊝⊝ VERY LOWa,b | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events (measured with Asberg Antidepressant Side Effect Scale and Toxic Exposure Surveillance System) | SMD 1.32 lower (2.86 lower to 0.23 higher) | ‐ | 200 (3 RCTs) | ⊕⊝⊝⊝ VERY LOWc,d | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Quality of life (physical) at the end of treatment (higher scores indicate greater quality of life) | Quality of life (physical) score in the single included study was 14.9. | MD 1.19 higher (0.33 higher to 2.05 higher) | ‐ | 127 (1 RCT) | ⊕⊝⊝⊝ VERY LOWe,f | |
| Quality of life (emotional) at the end of treatment (higher scores indicate greater quality of life) | Mean quality of life (emotional) score was 17.2. | MD 0.25 higher (0.9 lower to 1.4 higher) | ‐ | 219 (2 RCTs) | ⊕⊝⊝⊝ VERY LOWf,g | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCTs: randomised controlled trials; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels owing to very serious risk of bias. Of 11 trials, nine were at high risk of bias owing to lack of blinding of participants, and 6 were at high risk of bias owing to lack of blinding of outcome assessors.
bDowngraded two levels owing to considerable heterogeneity (I2 = 89%, Tau2 = 0.70, P < 0.001). cDowngraded two levels owing to very serious risk of bias. dDowngraded two levels owing to considerable heterogeneity (I2 = 95%, Tau2 = 1.75, P < 0.001). eDowngraded one level owing to small sample size and only one study reporting on this outcome.
fDowngraded two levels owing to very serious risk of bias. gDowngraded one level owing to substantial heterogeneity (I2 = 71%, Tau2 = 0.97, P < 0.0001).
Summary of findings 5. Acupuncture compared with psychological therapy for depression.
| Acupuncture compared with psychological therapy for depression | ||||||
| Patient or population: clinical diagnosis of depression Setting: community Intervention: acupuncture Comparison: psychological therapy | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with psychological therapy | Risk with acupuncture | |||||
| Severity of depression at the end of treatment as measured by self‐rated depression scores (lower score indicates less severe depression) | SMD 0.5 lower (1.33 lower to 0.33 higher) | ‐ | 497 (2 RCTs) | ⊕⊕⊝⊝ LOWa,b | As a rule of thumb, 0.2 SMD represents a small difference, 0.5 moderate, and 0.8 large. | |
| Adverse events measured during study treatment | Study population | RR 0.62 (0.29 to 1.33) | 453 (1 RCT) | ⊕⊕⊝⊝ LOWc,d | ||
| 86 per 1000 | 53 per 1000 (25 to 115) | |||||
| Quality of life (physical) | ‐ | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| Quality of life (emotional) | ‐ | ‐ | ‐ | No studies reported on this outcome. | ‐ | Cannot estimate the effect of acupuncture as no studies reported on this outcome |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCTs: randomised controlled trials; RR: risk ratio; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for serious risk of bias; both included trials have high risk of performance bias. bDowngraded one level owing to substantial heterogeneity (I2 = 85%, Tau2 = 0.31, P = 0.01). cDowngraded one level for imprecision as only a single study reported on this rare outcome.
dDowngraded one level owing to high risk of performance bias.
Within each comparison, for each outcome, the overall treatment effect for acupuncture versus control is followed by the individual treatment effect for each mode of stimulation, presented as a series of subcomparisons. Primary endpoint data at the end of the intervention are presented. Data are presented for severity of depression during treatment, at the end of the intervention, and at follow‐up at zero to six months and at six to 12 months.
Comparison 1. Acupuncture versus no treatment/wait list/treatment as usual
Primary outcomes
1.1 Outcome: reduction in the severity of depression at the end of treatment
4.

Forest plot of comparison: 1 Acupuncture versus no treatment/wait list/TAU, outcome: 1.1 Severity of depression at the end of treatment.
1.1. Analysis.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 1 Severity of depression at the end of treatment.
Overall six trials of acupuncture provided low‐quality evidence that acupuncture reduced the severity of depression at the end of treatment (SMD ‐0.66, 95% CI ‐1.06 to ‐0.25, six trials, 488 participants, I2 = 64%). We downgraded the evidence for this comparison by two levels owing to high risk of performance bias in most included trials and substantial heterogeneity.
We explored possible reasons for substantial heterogeneity by examining the contributions of clinician‐rated versus self‐rated outcome measures. We found that two trials used self‐rated outcomes. Bosch 2015 and MacPherson 2013 contributed to a significant proportion of this heterogeneity; therefore we analysed clinician‐rated versus self‐reported outcomes separately. The three trials using clinician‐rated outcomes provided evidence of a reduction in the severity of depression at the end of the trial (SMD ‐0.97, 95% CI ‐1.34 to ‐0.60, three trials, 144 participants, I2 = 5%), and the two trials using self‐reported outcomes provided no evidence of a reduction in the severity of depression at the end of the trial (SMD ‐0.23, 95% CI ‐0.73 to 0.27, two trials, 334 participants, I2 = 68%).
Evidence suggested a reduction in depression for manual acupuncture compared with control (SMD ‐0.56, 95% CI ‐0.98 to ‐0.15, five trials, 458 participants, I2 = 62%) and electro‐acupuncture (SMD ‐1.26, 95% ‐2.10 to ‐0.43, one trial, 30 participants).
1.2 Outcome: adverse events
1.2. Analysis.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 2 Adverse events.
One study reported this outcome. This trial of manual acupuncture found low‐quality evidence of no difference in adverse event rates between groups (RR 0.89, 95% 0.35 to 2.24, one trial, 302 participants). We downgraded the evidence for this comparison by two levels owing to high risk of performance bias and the fact that only one trial reported on these relatively rare events.
Secondary outcomes
1.3 Outcome: reduction in the severity of depression during treatment
1.3. Analysis.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 3 Severity of depression during treatment.
Data show some evidence of reduction in the severity of depression during treatment (MD ‐6.75, 95% CI ‐9.12 to ‐4.38, two trials, 137 participants, I2 = 21%).
A trial of manual acupuncture found a reduction in the severity of depression (MD ‐7.04, 95% ‐11.08 to ‐3.00, two trials, 107 participants, I2 = 58%), as did a small trial of electro‐acupuncture (MD ‐6.24, 95% CI ‐9.12 to ‐4.38, one trial, 30 participants).
1.4 Outcome: reduction in the severity of depression zero to six months after treatment
1.4. Analysis.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 4 Severity of depression 0‐6 months after treatment.
Data show a reduction in depression from manual acupuncture at six months following completion of treatment (MD ‐1.90, 95% CI ‐3.01 to ‐0.79, one trial, 237 participants).
1.5 Outcome: reduction in the severity of depression six to 12 months after treatment
1.5. Analysis.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 5 Severity of depression 6‐12 months after treatment.
Researchers found no evidence of a reduction in depression from manual acupuncture at 12 months (MD ‐1.00, 95% CI ‐2.53 to 0.53, one trial, 235 participants).
1.6 Outcome: remission of depression
1.6. Analysis.
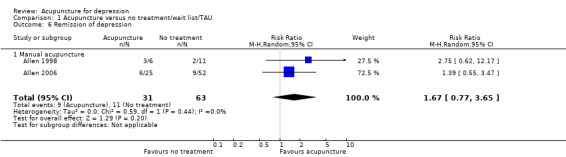
Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 6 Remission of depression.
Two small trials found no evidence of a difference in remission of depression from manual acupuncture (RR 1.67, 95% CI 0.77 to 3.65, two trials, 94 participants, I2 = 0%) (Allen 1998; Allen 2006).
1.7 Outcome: change in medication
1.7. Analysis.

Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 7 Change in use of medication at the end of treatment.
One trial found no evidence of a difference in medication change from manual acupuncture compared with control (RR 0.91, 95% CI 0.73 to 1.14, one trial, 302 participants) (MacPherson 2013).
1.8 Dropout from treatment
1.8. Analysis.
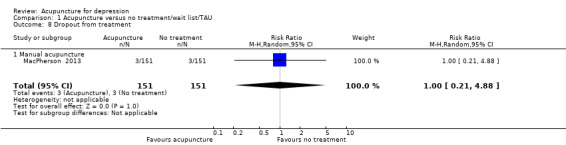
Comparison 1 Acupuncture versus no treatment/wait list/TAU, Outcome 8 Dropout from treatment.
One trial found no difference in dropout at the end of manual acupuncture treatment compared with control (RR 1.00, 95% CI 0.21 to 4.88, one trial, 302 participants) (MacPherson 2013).
Comparison 2. Acupuncture versus control acupuncture
Comparisons are made between invasive and non‐invasive controls. Invasive controls included non‐channel points (Andreescu 2011; Fan 2005; Fu 2006; Li 2008; Li 2011b), needling acupuncture points unrelated to depression (Allen 1998; Allen 2006), minimal insertion just into the skin layer (Fan 2013), different acupuncture points (Sun 2010; Sun 2013), and minimal insertion on specific non‐depression points (Chung 2015; Whiting 2008; Yeung 2011b). Non‐invasive controls included placebo needles (Chung 2015; Fan 2013; Yeung 2011b), mock electro‐acupuncture (Andreescu 2011; Yeung 2011b), and mock laser acupuncture (Quah‐Smith 2005; Quah‐Smith 2013).
Primary outcomes
2.1 Severity of depression at the end of treatment
2.1. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 1 Severity of depression at the end of the intervention.
5.

Forest plot of comparison: 2 Acupuncture versus control acupuncture, outcome: 2.1 Severity of depression at the end of the intervention.
Low‐quality evidence suggests a reduction in the severity of depression between acupuncture and control at the end of the trial; however, substantial heterogeneity can likely be explained by the mode of stimulation and activity from the control (MD ‐1.69, 95% CI ‐3.33 to ‐0.05, 14 trials, 841 participants, I2 = 80%). We downgraded evidence by one level in most studies for high risk of performance bias and high risk of bias in at least one other domain. We also downgraded evidence by one level on the basis of substantial heterogeneity.
2.1.1 Manual acupuncture versus invasive control
We found no evidence of a reduction in the severity of depression in the acupuncture group compared with an invasive control group (MD ‐2.97, 95% CI ‐6.26 to 0.31, seven trials, 418 participants, I2 = 81%). Clinical heterogeneity among types of invasive controls is likely a contributing factor. Fan 2013, using SCL‐90, found evidence suggesting that acupuncture reduced the severity of depression to a greater extent than the invasive control (MD ‐0.44, 95% CI ‐0.58 to ‐0.30, 95 participants).
2.1.2 Electro‐acupuncture versus invasive control
Trials provided no evidence of a difference between groups (MD 0.43, 95% ‐0.54 to 1.4, five trials, 251 participants, I2 = 0%).
2.1.3 Electro‐acupuncture versus non‐invasive control
Data show no evidence of a reduction in depression between groups (MD 0.17, 95% CI ‐2.14 to 2.48, two trials, 99 participants, I2 = 35%).
2.1.4 Laser acupuncture versus non‐invasive control
Researchers found evidence of reduced depression in the laser acupuncture group compared with the control group (MD ‐5.51, 95% CI ‐8.30 to ‐2.73, two trials, 73 participants, I2 = 0%).
2.2 Adverse events
2.2. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 2 Adverse events.
Overall moderate‐quality evidence shows no difference in the rate of adverse events between acupuncture groups and control groups (RR 1.63, 95% 0.93 to 2.86, five trials, 300 participants, I2 = 10%). We downgraded this evidence by one level owing to the small sample size and the relatively rare nature of adverse events.
2.2.1 Manual acupuncture versus invasive control
One trial reported on this outcome (Whiting 2008), providing no evidence of a difference between groups (RR 2.50, 95% CI 0.15 to 40.37, one trial,17 participants). One additional trial reported on this outcome using continuous data suggesting increased risk of adverse events from acupuncture (MD 8.30, 95% CI 6.88 to 9.72, one trial, 43 participants) (Li 2011b).
2.2.2 Electro‐acupuncture versus invasive control
Investigators found no evidence of a difference between groups (RR 1.79, 95% CI 0.99 to 3.25, four trials, 245 participants, I2 = 16%).
2.2.3 Electro‐acupuncture versus non‐invasive control
One trial reported on this outcome and provided no evidence of differences between groups (RR 0.40, 95% CI 0.05 to 3.08, one trial, 39 participants) (Yeung 2011b).
2.2.4 Laser acupuncture versus non‐invasive control
Quah‐Smith 2013 reported no difference in the rate of adverse events between laser and sham laser acupuncture. Researchers collected adverse event data on dizziness, aches, transient fatigue, prolonged fatigue, vagueness, and nausea. On a 0 to 6 scale (6 indicating maximum intensity), mean scores were as follows: minimal transient fatigue in the laser group ‐ 0.67, and in the sham laser group, aches 0.11, transient fatigue 1.0, days of fatigue 0.71, and vagueness 0.52.
Secondary outcomes
2.3 Severity of depression during treatment
2.3. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 3 Severity of depression during treatment.
Data show no evidence of a difference between groups in the severity of depression during treatment (MD 0.04, 95% CI ‐0.81 to 0.90, six trials, 413 participants, I2 = 0%).
2.3.1 Manual acupuncture versus invasive control
We found no evidence of a difference between manual acupuncture and control (MD 0.09, 95% CI ‐2.55 to 2.74, two trials, 117 participants, I2 = 2%).
2.3.2 Electro‐acupuncture versus invasive control
Trials provided no evidence of a difference between electro‐acupuncture and control (MD 0.16, 95% CI ‐0.92 to 1.24, four trials, 197 participants, I2 = 0%).
2.3.3 Electro‐acupuncture versus non‐invasive control
Data show no evidence of a difference between electro‐acupuncture and control (MD ‐0.45, 95% CI ‐2.71 to 1.80, two trials, 99 participants, I2 = 37%).
2.4 Severity of depression at zero to six months' follow‐up
2.4. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 4 Severity of depression at 0‐6 months' follow‐up.
2.4.1 Manual acupuncture versus invasive control
One trial reported on this outcome (Fan 2013), providing evidence of benefit at six months (MD ‐0.85, 95% CI ‐0.98 to ‐0.72, one trial, 95 participants).
2.5 Remission of depression
2.5. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 5 Remission of depression.
Overall evidence showed a greater remission rate following acupuncture (RR 1.91, 95% 1.14 to 3.21, 10 trials, 601 participants, I2 = 48%).
2.5.1 Manual acupuncture versus invasive control
Data show no evidence of improvement in remission rates between groups (RR 1.89, 95% CI 0.75 to 4.75, five trials, 368 participants, I2 = 63%).
2.5.2 Electro‐acupuncture versus invasive control
Trials provided no evidence of improvement in remission rates between groups (RR 1.23, 95% 0.35 to 4.29, two trials, 87 participants, I2 = 20%).
2.5.3 Electro‐acupuncture versus non‐invasive control
We found no evidence of improvement in remission rates between groups (RR 2.15, 95% CI 0.60 to 7.67, one trial, 73 participants).
2.5.4 Laser acupuncture versus non‐invasive control
Evidence suggests greater remission from laser acupuncture compared with control (RR 3.00, 95% CI 1.48 to 6.09, two trials, 73 participants, I2 = 0%).
2.6 Quality of life (emotional) during treatment
2.6. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 6 Quality of life (emotional) during treatment.
One trial reported on this outcome (Chung 2015), providing no evidence of a difference between groups (MD ‐1.98, 95% CI ‐5.41 to 1.45, one trial, 150 participants).
2.6.1 Electro‐acupuncture versus invasive control
Investigators provided no evidence of a difference between groups (MD ‐2.09, 95% CI ‐6.54 to 2.36, one trial, 90 participants).
2.6.2 Electro‐acupuncture versus non‐invasive control
Data show no evidence of a difference between groups (MD ‐1.81, 95% CI ‐7.18 to 3.56, one trial, 60 participants).
2.7 Quality of life (emotional) at the end of treatment
2.7. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 7 Quality of life (emotional) at the end of treatment.
Two trials reported on this outcome and provided moderate evidence of no difference in emotional quality of life between groups (MD ‐2.25, 95% CI ‐5.89 to 1.39, two trials, 167 participants, I2 = 0%). We downgraded the evidence for this comparison by one level owing to the small sample size.
2.7.1 Manual acupuncture versus invasive control
Researchers provided no evidence of a difference between groups (MD ‐5.0, 95% CI ‐36.47 to 26.47, one trial, 17 participants). One trial reported on changes from baseline between groups and described no difference between groups (acupuncture 6.2 (13.6) vs control 14.1 (17.5)) (Andreescu 2011).
2.7.2 Electro‐acupuncture versus invasive control
Data show no evidence of a difference between groups (MD ‐2.55, 95% CI ‐7.38 to 2.28, one trial, 90 participants).
2.7.3 Electro‐acupuncture versus non‐invasive control
We found no evidence of a difference between groups (MD ‐1.76, 95% CI ‐7.38 to 3.86, one trial, 60 participants).
2.8 Quality of life (physical) during treatment
2.8. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 8 Quality of life (physical) during treatment.
One trial reported on this outcome and found no differences between groups (MD ‐0.99, 95% CI ‐4.74 to 2.77, 150 participants) (Chung 2015).
2.8.1 Electro‐acupuncture versus invasive control
Investigators provided no evidence of a difference between groups (MD ‐2.62, 95% CI ‐7.07 to 1.83, one trial, 90 participants).
2.8.2 Electro‐acupuncture versus non‐invasive control
Data show no evidence of a difference between groups (MD 1.26, 95% CI ‐4.12 to 6.64, one trial, 60 participants).
2.9 Quality of life (physical) at the end of treatment
2.9. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 9 Quality of life (physical) at the end of treatment.
One trial reported on this outcome (Chung 2015), revealing that at the end of treatment, low‐quality evidence suggested no differences between groups in quality of life (MD ‐5.12, 95% CI ‐10.30 to 0.13, one trial, 150 participants). We downgraded the evidence for this comparison by one level because only one small study contributed data for this outcome.
2.9.1 Electro‐acupuncture versus invasive control
Trialists provided evidence of improved quality of life for the control group (MD ‐7.61, 95% CI ‐12.38 to ‐2.38, one trial, 90 participants). One trial reported on changes from baseline between groups and described no differences between groups (acupuncture 0.5 (6.9) vs control ‐1.7 (8.0)) (Andreescu 2011).
2.9.2 Electro‐acupuncture versus non‐invasive control
Data show no evidence of a difference between groups (MD ‐2.23, 95% ‐7.81 to 3.35, one trial, 60 participants).
2.10 Change in medication
2.10.1 Electro‐acupuncture versus non‐invasive control
Investigators provided no evidence of a difference between groups (MD ‐0.39, 95% CI ‐1.71 to 0.93, one trial, 70 participants).
2.11 Dropout from treatment
2.11. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 11 Dropout from treatment.
We found no difference in dropout between groups (RR 1.04, 95% CI 0.62 to 1.75, seven trials, 501 participants, I2 = 0%).
2.11.1 Manual acupuncture versus invasive control
Researchers presented no evidence of a difference between groups (RR 0.60, 95% CI 0.16 to 2.29, one trial, 60 participants).
2.11.2 Electro‐acupuncture versus invasive control
Data show no evidence of a difference between groups (RR 1.01, 95% CI 0.51 to 2.02, four trials, 224 participants, I2 = 0%).
2.11.3 Electro‐acupuncture versus non‐invasive control
Investigators provided no evidence of a difference between groups (RR 1.48, 95% CI 0.56 to 3.91, four trials, 217 participants, I2 = 0%).
Comparison 3. Acupuncture versus medication
Primary outcomes
3.1 Severity of depression at the end of treatment
3.1. Analysis.

Comparison 3 Acupuncture versus medication, Outcome 1 Severity of depression at the end of treatment.
6.

Forest plot of comparison: 3 Acupuncture versus medication, outcome: 3.1 Severity of depression at the end of treatment.
Overall very low‐quality evidence suggests small benefit from acupuncture compared with medication (SMD ‐0.23, 95% CI ‐0.40 to ‐0.05, 31 trials, 3127 participants, I2 = 80%). We explored possible reasons for substantial heterogeneity by examining the contribution of clinician‐rated versus self‐reported outcome measures. Only one study used a self‐reported outcome measure (Lv 2015). Removing this study from the analysis did not significantly reduce heterogeneity nor change the effect size (SMD ‐0.23, 95% CI ‐0.41 to ‐0.05, 30 trials, 3067 participants, I2 = 81%). We downgraded evidence for this comparison by two levels owing to very serious risk of bias, with 30 trials having high risk of bias owing to lack of blinding and 12 trials having high risk of bias owing to lack of blinding of outcome assessors. We also downgraded the evidence by one level because substantial heterogeneity was present.
3.1.1 Manual acupuncture versus SSRI
We found no evidence of benefit among groups (SMD ‐0.23, 95% CI ‐0.50 to 0.04, 16 trials, 1570 participants, I2 = 84%).
3.1.2 Electro‐acupuncture versus SSRI
Data show evidence of benefit from electro‐acupuncture compared with SSRI medication (SMD ‐0.47, 95% CI ‐0.85 to ‐0.10, five trials, 197 participants, I2 = 34%).
3.1.3 Manual acupuncture versus TCAs
Researchers provided no evidence of a reduction in the severity of depression between groups (SMD ‐0.28, 95% CI ‐1.25 to 0.69, three trials, 397 participants, I2 = 94%).
3.1.4 Electro‐acupuncture versus TCAs
Trials presented no evidence of a reduction in the severity of depression between groups (SMD ‐0.20, 95% CI ‐0.42 to 0.01, five trials, 801 participants, I2 = 34%).
3.1.5 Manual acupuncture versus other antidepressant
We found no evidence of a difference between groups (SMD ‐0.22, 95% CI ‐0.73 to 0.29, one trial, 60 participants).
3.1.6 Electro‐acupuncture versus heterocyclic antidepressants
Investigators provided no evidence of a difference between groups (SMD 0.30, 95% CI ‐0.21 to 0.80, one trial, 62 participants).
3.1.7 Electro‐acupuncture versus other antidepressant
We found no evidence of a difference between groups (SMD 0.09, 95% CI ‐0.52 to 0.70, one trial, 41 participants).
3.2 Adverse events
3.2. Analysis.

Comparison 3 Acupuncture versus medication, Outcome 2 Adverse events.
3.2.1 Manual acupuncture versus SSRI
All included studies used the Asberg side effect rating scale (SES). Data show very low‐quality evidence of an increase in adverse events reported by those taking SSRIs compared with manual acupuncture (MD ‐4.32, 95% CI ‐7.41 to ‐1.23, three trials, 481 participants, I2 = 97%). We downgraded the evidence by two levels owing to very serious risk of bias in all three studies, and by two levels owing to considerable heterogeneity.
Secondary outcomes
3.3 Severity of depression during treatment
3.3. Analysis.

Comparison 3 Acupuncture versus medication, Outcome 3 Severity of depression during treatment.
Overall evidence suggests benefit from acupuncture during treatment regardless of mode of stimulation, and reduced depression compared with medication (MD ‐1.67, 95% CI ‐2.91 to ‐0.43, nine trials, 552 participants, I2 = 55%).
3.3.1 Manual acupuncture versus SSRIs
Investigators provided no evidence of a difference between groups (MD ‐1.38, 95% CI ‐3.2 to ‐0.45, five trials, 340 participants, I2 = 66%).
3.3.2 Electro‐acupuncture versus SSRIs
Data show evidence of a reduction in the severity of depression during treatment from electro‐acupuncture compared with SSRIs (MD ‐2.58, 95% CI ‐4.38 to ‐0.78, three trials, 112 participants, I2 = 29%).
3.3.3 Manual acupuncture versus TCAs
Researchers provided no evidence of a reduction in the severity of depression between groups (MD ‐0.80, 95% CI ‐3.65 to 2.05, one trial, 100 participants).
3.4 Severity of depression zero to six months after treatment
3.4. Analysis.

Comparison 3 Acupuncture versus medication, Outcome 4 Severity of depression 0‐6 months after treatment.
3.4.1 Manual acupuncture versus other antidepressant
We found evidence of benefit derived from manual acupuncture compared with other antidepressant (MD ‐5.60, 95% CI ‐7.60 to ‐3.60, one trial, 60 participants).
3.5 Remission of depression
3.5. Analysis.

Comparison 3 Acupuncture versus medication, Outcome 5 Remission of depression.
Evidence suggests remission from acupuncture treatment when compared with medication only (RR 1.16, 95% CI 1.05 to 1.29, 27 trials, 2918 participants, I2 = 24%).
3.5.1 Manual acupuncture versus SSRI
Trialists reported no differences between groups (RR 1.16, 95% CI 0.98 to 1.37, 14 trials, 1332 participants, I2 = 11%).
3.5.2 Electro‐acupuncture versus SSRIs
Researchers described no differences between groups (RR 1.28, 95% CI 0.94 to 1.75, four trials, 188 participants, I2 =0 %).
3.5.3 Manual acupuncture versus TCAs
Investigators provided evidence of benefit in remission from manual acupuncture compared with TCAs (RR 1.32, 95% CI 1.03 to 1.69, four trials, 620 participants, I2 = 39%).
3.5.4 Electro‐acupuncture versus TCAs
Data show no evidence of differences between groups (RR 1.03, 95% CI 0.88 to 1.21, four trials, 778 participants, I2 = 25%).
3.6 Dropout from treatment
3.6. Analysis.

Comparison 3 Acupuncture versus medication, Outcome 6 Dropout from treatment.
Overall no evidence suggests differences in dropout between groups (RR 0.87, 95% CI 0.20 to 3.71, five trials, 246 participants, I2 = 43%).
3.6.1 Manual acupuncture versus SSRIs
Data show no evidence of differences in dropout between groups (RR 0.27, 95% CI 0.03 to 2.47, two trials, 134 participants, I2 = 41%).
3.6.2 Electro‐acupuncture versus SSRIs
Researchers provided no evidence of differences in dropout between groups (RR 1.82, 95% CI 0.43 to 7.79, three trials, 112 participants, I2 = 3%).
Comparison 4. Acupuncture and medication versus medication
Primary outcomes
4.1 Severity of depression at the end of treatment
4.1. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 1 Severity of depression at the end of treatment.
7.

Forest plot of comparison: 4 Acupuncture plus medication vs medication, outcome: 4.1 Severity of depression at the end of treatment.
Overall very low‐quality evidence suggests benefit from acupuncture plus medication compared with medication alone (SMD ‐1.15, 95% CI ‐1.63 to ‐0.66, 12 trials, 813 participants, I2 = 89%).
We explored another possible contribution to the considerable heterogeneity by examining the contributions of clinician‐rated versus self‐reported outcome measures. One study used a self‐rated scale (Qu 2013). Removing this study from analysis did not reduce heterogeneity, which remained considerable (SMD ‐1.25, 95% CI ‐1.83 to ‐0.67, 11 trials, 653 participants, I2 = 91%). We downgraded the evidence for this comparison by two levels owing to the very serious risk of bias present in most trials, and by another two levels for considerable heterogeneity.
4.1.1 Manual acupuncture plus SSRI versus SSRI
We found evidence of a reduction in the severity of depression at the end of treatment from manual acupuncture plus SSRIs compared with SSRIs alone (SMD ‐1.32, 95% CI ‐2.09 to ‐0.55, eight trials, 539 participants, I2 = 93%). We conducted a sensitivity analysis owing to high heterogeneity, possibly resulting from the very small standard deviations reported in one study (Wang 2014). We contacted the trial authors, who confirmed that the standard deviations were accurate. Removal of Wang 2014 from analysis resulted in no change in the direction of benefit but altered the effect size. Heterogeneity remained substantial (SMD ‐0.93, 95% CI ‐1.52 to ‐0.35, seven trials, 468 participants, I2 = 88%).
4.1.2 Electro‐acupuncture plus SSRIs versus SSRIs
Investigators provided evidence of a large effect reduction in the severity of depression during treatment from electro‐acupuncture plus SSRI compared with SSRIs alone (SMD ‐0.84, 95% CI ‐1.16 to ‐0.51, five trials, 274 participants, I2 = 33%).
4.1.3 Manual acupuncture plus TCAs versus TCAs
Trials provided evidence of a reduction in the severity of depression during treatment from manual acupuncture plus TCAs compared with TCAs alone (SMD ‐3.06, 95% CI ‐3.82 to ‐2.30, one trial, 60 participants).
4.2 Adverse events
4.2. Analysis.
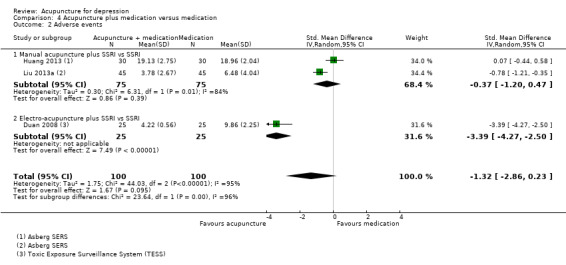
Comparison 4 Acupuncture plus medication versus medication, Outcome 2 Adverse events.
Two studies used the Asberg side effect scale (SES) (Huang 2013; Liu 2013a), and one study used the Toxic Exposure Surveillance System (TESS) (Duan 2008). We found very low‐quality evidence of no differences between groups in the numbers of adverse events recorded (SMD ‐1.32, 95% CI ‐2.86 to 0.23, three trials, 200 participants, I2 = 95%). We downgraded the evidence for this comparison by two levels owing to very serious risk of bias, and by another two levels owing to considerable heterogeneity.
4.2.1 Manual acupuncture plus SSRIs versus SSRis alone
We found no evidence of a difference between groups (SMD ‐0.37, 95% CI ‐1.20 to 0.47, two trials, 150 participants).
4.2.2 Electro‐acupuncture plus SSRIs versus SSRIs alone
Data provide evidence of a reduction in adverse events for electro‐acupuncture (SMD ‐3.39, 95% CI ‐4.27, to ‐2.50, one trial, 60 participants).
Secondary outcomes
4.3 Severity of depression during treatment
4.3. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 3 Severity of depression during treatment.
Overall evidence suggests a reduction in the severity of depression from acupuncture (SMD ‐1.60, 95% CI ‐2.45, to ‐0.76, six trials, 514 participants, I2 = 95%).
4.3.1 Manual acupuncture plus SSRIs versus SSRIs
Evidence suggests a reduction in the severity of depression during treatment from manual acupuncture plus SSRIs compared with SSRIs alone (SMD ‐1.81, 95% CI ‐2.83 to ‐0.80, six trials. 432 participants, I2 = 95%). We performed a sensitivity analysis owing to high heterogeneity, possibly resulting from the very small standard deviations presented in one study (Wang 2014). We contacted the trial authors, who confirmed that the standard deviations were accurate. Removal of Wang 2014 resulted in no change in the direction of benefit but altered effect size and heterogeneity (SMD ‐0.80, 95% CI ‐1.02 to ‐0.58, five trials, 361 participants, I2 = 0%).
4.3.2 Electro‐acupuncture plus SSRIs versus SSRIs
Overall data show evidence of a reduction in the severity of depression during treatment from electro‐acupuncture plus SSRIs compared with medication alone (SMD ‐0.70, 95% CI ‐1.19 to ‐0.21, one trial, 82 participants).
4.4 Remission of depression
4.4. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 4 Remission of depression.
Data show no evidence of a difference between groups (RR 1.21, 95% CI 0.85 to 1.73, nine trials, 618 participants, I2 = 61%).
4.4.1 Manual acupuncture plus SSRIs versus SSRIs
Data show no evidence of a difference between groups (RR 1.33, 95% CI 0.65 to 2.73, five trials, 299 participants, I2 = 76%).
4.4.2 Electro‐acupuncture plus SSRIs versus SSRIs
Researchers provided no evidence of a difference between groups (RR 1.17, 95% CI 0.75 to 1.80, four trials, 120 participants, I2 = 49%).
4.4.3 Manual acupuncture plus heterocyclic antidepressant versus heterocyclic antidepressant alone
Investigators provided evidence of an increase in remission in the acupuncture plus medication group (RR 4.36, 95% CI 0.53 to 36.12, one trial, 46 participants).
4.5 Quality of life (physical)
4.5. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 5 Quality of life (physical).
4.5.1 Manual acupuncture plus SSRIs versus SSRIs
Very low‐quality evidence suggests benefit from manual acupuncture in one small trial (MD 1.4, 95% CI 0.15 to 2.65, 64 participants). We downgraded the evidence for this comparison by one level because only one small study reported this outcome, and by two levels owing to very serious risk of bias.
4.5.2 Electro‐ acupuncture plus SSRIs versus SSRIs
Data show no differences between groups (MD 1.0, 95% CI ‐0.18 to 2.18, 63 participants).
4.6 Quality of life (emotional)
4.6. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 6 Quality of life (emotional).
Very low‐quality evidence suggests no differences between groups (MD 0.25, 95% CI ‐0.9 to 1.4, two trials, 219 participants, I2 = 71%). We downgraded the evidence for this comparison by two levels owing to very serious risk of bias, and by one level because of substantial heterogeneity.
4.6.1 Manual acupuncture plus SSRIs versus SSRIs
We found no evidence of a difference between groups (MD 0.10, 95% CI ‐1.46 to 1.65, two trials, 111 participants, I2 = 66%).
4.6.2 Electro‐acupuncture plus SSRIs versus SSRIs
Investigators provided no evidence of a difference between groups (MD 0.35, 95% CI ‐2.0 to 2.7, two trials, 108 participants, I2 = 86%).
4.7 Change in medication
4.7. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 7 Change in use of medication.
We found evidence of reduced risk of using medication in the acupuncture and SSRI group compared with the SSRI alone group (RR 0.39, 95% CI 0.22 to 0.67, three trials, 236 participants, I2 = 0%).
4.7.1 Manual acupuncture plus SSRIs versus SSRIs
Evidence suggests reduced medication use in the manual acupuncture plus medication group (RR 0.38, 95% CI 0.20 to 0.72, two trials, 154 participants, I2 = 0%).
4.7.2 Electro‐acupuncture plus SSRIs versus SSRIs
Data show no evidence of a difference between groups (RR 0.41, 95% CI 0.13 to 1.30, one trial, 82 participants).
4.8 Dropout from treatment
4.8. Analysis.

Comparison 4 Acupuncture plus medication versus medication, Outcome 8 Dropout from treatment.
Trials provided no evidence of a difference between groups (RR 0.70, 95% 0.35 to 1.42, six trials, 426 participants, I2 = 0%).
4.8.1 Manual acupuncture plus SSRIs versus SSRIs
Investigators provided no evidence of a difference between groups (RR 0.45, 95% CI 0.18 to 1.15, three trials, 234 participants, I2 = 0%).
4.8.2 Electro‐ acupuncture plus SSRIs versus SSRIs
Data show no differences between groups (RR 1.23, 95% CI 0.43 to 3.51, three trials, 192 participants, I2 = 0%).
Comparison 5. Acupuncture versus psychological treatment
Two trials reported on this outcome (MacPherson 2013;Wang 2015). Owing to significant differences in the psychological treatment delivered in these two trials, we did not combine them in the meta‐analysis. MacPherson 2013 used counselling, as delivered by a member of the British Association for Counselling and Psychotherapy, and Wang 2015 delivered an educational intervention with some participants receiving psychological guidance, but investigators did not specify the number or duration of sessions nor the content of these sessions.
Primary outcomes
5.1 Severity of depression at the end of treatment
5.1. Analysis.

Comparison 5 Acupuncture versus psychological therapy, Outcome 1 Severity of depression at the end of treatment.
5.1.1 Manual acupuncture
MacPherson 2013 found no evidence of a difference when comparing acupuncture with counselling alone (MD ‐0.80, 95% CI ‐1.92 to 0.32, one trial, 453 participants). Wang 2015 found evidence of benefit of acupuncture compared with the educational and psychological control (MD ‐6.49, 95% CI ‐10.33 to ‐2.65, one trial, 44 participants). Overall the quality of evidence for this comparison was low. We downgraded the evidence for this comparison by one level because both trials had high risk of performance bias, and by one level because results show substantial heterogeneity. However results for both studies show the same direction of effect.
5.2 Adverse events
5.2. Analysis.

Comparison 5 Acupuncture versus psychological therapy, Outcome 2 Adverse events.
5.2.1 Manual acupuncture
Trials provided low‐quality evidence suggesting no differences between groups (RR 0.62, 95% CI 0.29 to 1.33, one trial, 453 participants). We downgraded the evidence for this comparison by one level for risk of bias due to performance bias, and by one level because only one study contributed to this outcome.
Secondary outcomes
5.3 Severity of depression at zero to six months' follow‐up
5.3. Analysis.

Comparison 5 Acupuncture versus psychological therapy, Outcome 3 Severity of depression 0‐6 months after treatment.
5.3.1 Manual acupuncture
Data show no differences between groups (MD 0.50, 95% ‐0.51 to 1.51, one trial, 453 participants).
5.4 Severity of depression at six to 12 months
5.4. Analysis.

Comparison 5 Acupuncture versus psychological therapy, Outcome 4 Severity of depression 6‐12 months.
5.4.1 Manual acupuncture
Trialists found no differences between groups (MD 0.60, 95% CI ‐0.80 to 2.00, one trial, 453 participants).
5.5 Remission of depression
(Analysis 5.5)
5.5.1 Manual acupuncture
Data show no evidence of differences between groups (RR 1.50, 95% CI 0.81 to 2.79, one trial, 25 participants).
5.6 Change in use of medication
5.6. Analysis.

Comparison 5 Acupuncture versus psychological therapy, Outcome 6 Change in use of medication.
5.6.1 Manual acupuncture
Researchers provided no evidence of a difference between groups (RR 0.82, 95% CI 0.61 to 1.1, 453 participants).
5.7 Dropout
5.7. Analysis.

Comparison 5 Acupuncture versus psychological therapy, Outcome 7 Dropout from treatment.
5.7.1 Manual acupuncture
Evidence shows greater dropout from psychological treatment than from acupuncture (RR 0.27, 95% CI 0.08 to 0.90, one trial, 453 participants).
Comments on heterogeneity
Overall, the acupuncture trials were clinically highly heterogeneous and used a diverse range of acupuncture dosages. Electro‐acupuncture treatment duration ranged from three to six weeks, and treatment was administered two days per week to daily in treatment sessions lasting from 30 to 60 minutes, with a total course of treatment ranging from nine to 42 sessions. Ten trials used a standard point prescription, and four were semistandardised, allowing some variation based on diagnosis. Manual acupuncture trials were equally diverse, treatment duration ranged from two to 12 weeks, and acupuncture was administered from once a week to twice daily in treatment sessions lasting from 20 to 60 minutes, with a total course of treatment lasting 12 to 60 sessions. Twenty‐six trials used a standardised point prescription and eight used a semistandardised prescription; only three trials provided individualised treatment. Control acupuncture was also highly heterogeneous, with controls ranging from non‐channel points, to points unrelated to depression, minimal insertion, placebo needles, mock electro‐acupuncture, and mock laser acupuncture. Medication comparisons were less heterogeneous, with most trials describing administration of fluoxetine as the SSRI medication; however, investigators occasionally used other SSRIs such as paroxetine.
Sensitivity analysis
We proposed to undertake a sensitivity analysis of results to look at possible contributions of differences in risk of bias to robustness of the results, for example, by excluding trials with unclear concealment of random allocation; or excluding trials with greater than 20% dropout. Overall, we could not perform a sensitivity analysis for most comparisons because of lack of studies (fewer than five) in each group. When acupuncture was compared with medication, data show no significant change in the severity of depression when we removed studies unclearly describing randomisation (SMD ‐0.25, 95% CI ‐0.46 to ‐0.03, 21 trials, 1853 participants, I2 = 78%). Only two trials reported dropout greater than 20% (Allen 2006; Whiting 2008), and we could not perform a sensitivity analysis. We planned an a posteriori sensitivity analysis to examine the effects of studies undertaken in China; however, removal of these studies left one or two trials remaining in each comparison and therefore would not provide any additional useful information. We had also planned an a posteriori analysis on the effect of risk of bias (high‐risk vs low‐risk studies); however we identified insufficient trials with low risk of bias in each comparison to obtain any useful information.
Subgroup analyses
We planned several subgroup analyses to explore differences in effects of treatment among people with different diagnoses (e.g. major depression, dysthymia) and of different ages (< 65 years and ≥ 65 years) between psychological therapies and pharmacological interventions, effects of clinician‐rated versus self‐reported scales for depression, and effects of differing numbers of treatment sessions (< 20 and ≥ 20 sessions). We undertook none of these analyses because of paucity of data resulting in fewer than five studies in each subgroup.
Reporting bias
We inspected funnel plots for asymmetry in either of the primary outcome measures when 10 or more trials were included in the meta‐analysis (see Figure 8; Figure 9; Figure 10). We found no evidence of major asymmetry suggesting publication bias, especially in the light of true heterogeneity resulting from significantly different study interventions.
8.

Funnel plot of comparison: 2 Acupuncture versus control acupuncture, outcome: 2.1 Severity of depression at the end of the intervention.
9.

Funnel plot of comparison: 3 Acupuncture versus medication, outcome: 3.1 Severity of depression at the end of treatment.
10.
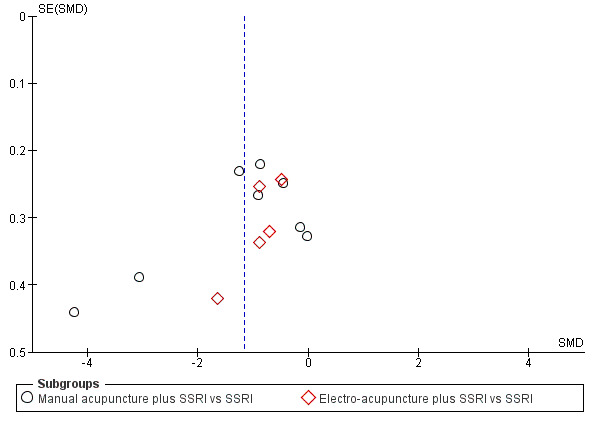
Funnel plot of comparison: 4 Acupuncture plus medication vs medication, outcome: 4.1 Severity of depression at the end of treatment.
Discussion
Summary of main results
We included in the meta‐analysis 63 trials with 7060 participants. Data show wide diversity among acupuncture interventions and comparators used to evaluate acupuncture for treatment of individuals with depression.
Acupuncture compared with no treatment/wait list/treatment as usual
For our primary outcome of severity of depression, we found low‐quality evidence from five trials of reduced severity of depression at the end of acupuncture treatment compared with no treatment/wait list/treatment as usual. Researchers found reduced severity of depression that was significant during treatment for acupuncture compared with no treatment/wait list/treatment as usual, and one trial reported that benefit was sustained at six months. We found no evidence of differences in adverse events between acupuncture and usual care and treatment as usual.
Acupuncture compared with control acupuncture
Fourteen trials examined the efficacy of acupuncture compared with an acupuncture control and found reduced severity of depression at the end of the acupuncture intervention (low‐quality evidence). Investigators found no difference in depression severity during treatment when acupuncture was compared with control acupuncture, and no evidence of a difference in adverse events between acupuncture and control acupuncture. Data show evidence of benefit from acupuncture, with increasing remission rates when compared with control acupuncture.
Acupuncture compared with medication alone
Acupuncture alone compared with medication alone reduced depression both during and at the end of treatment (very low‐quality evidence). We found evidence of greater side effects from medication than were noted with acupuncture. However, this outcome was not widely reported. Acupuncture compared with medication alone increased remission rates for depression.
Acupuncture plus medication compared with medication alone
Acupuncture plus medication compared with medication alone reduced depression both during and at the end of treatment (very low‐quality evidence). We found evidence of greater side effects from medication alone than were reported with a combination of acupuncture plus medication. However, this outcome was not widely reported. Data provide evidence of reduced use of medication and improved aspects of quality of life in the acupuncture plus medication groups, although only a small number of studies reported on these outcomes.
Acupuncture compared with psychological therapy
Researchers have provided no evidence of a difference in the severity of depression between acupuncture and a counselling intervention (low‐quality evidence). Psychological treatment was followed by a greater dropout rate than was reported with acupuncture, but data show no evidence of an effect on other outcomes. The effect of acupuncture on secondary outcomes, which included remission of symptoms, dropout, reduced use of medication, and quality of life, is limited in that fewer studies reported on these outcomes.
For both primary and secondary outcomes, evidence was of moderate to very low quality as assessed by the GRADE approach, and trial results were heterogeneous. Many comparisons are characterised as having significant clinical and substantial or considerable statistical heterogeneity. This relates to dosing characteristics of the intervention and the heterogeneity of controls, including dosages of medication and degree of physiological activity of acupuncture controls. Within comparisons, we presented data by mode of acupuncture stimulation (manual acupuncture, electro‐acupuncture, and laser acupuncture). The direction of effects within comparisons was similar, possibly suggesting that specific treatment effects may be similar. Although comparisons between acupuncture and different controls are not consistent in their findings, most comparisons suggest a beneficial effect from acupuncture, although the potential for bias exists. Owing to small numbers of identified studies, we have been unable to identify treatment dose parameters that may moderate and influence treatment outcomes.
We have highlighted additional sources of bias throughout the review, but participants' expectations and their often unblinded status may play a role. For trials that reported no blinding, the expectation of effects may be greater and the placebo effect larger. For trials of depression with a known placebo effect in mild to moderate depression, the larger placebo effects that might be expected from acupuncture may lead to methodological challenges and increased awareness of the need to design studies that may detect a beneficial treatment effect of true acupuncture. Overall we found no evidence of differences in depression severity when clinicians rather than participants rated depression, except in a comparison for which participants were unblinded to treatment between acupuncture and no treatment/wait list/usual care. The influence of lack of blinding and expectations may contribute to these findings. Fewer studies examined the role of acupuncture compared with a control such as a sham procedure or device. Placebo‐controlled trials included in this review show an overall small benefit derived from acupuncture compared with this control; however, heterogeneity is high and different controls may differ in terms of how inert or credible they are, or whether they produce a placebo effect. Addressing these differences is a priority suggested for future studies.
Overall completeness and applicability of evidence
Many styles of acupuncture may be provided, including individualised Traditional Chinese Medicine and approaches using standardised or semistandardised acupuncture points, as were used in most of the trials included in this review. This systematic review has documented wide variation in modes of stimulation, duration of needling, numbers of points used, depth of needling, and trial duration. Many studies administered suboptimal treatment doses of acupuncture. We also noted diversity in the clinical settings from which participants were recruited, and in trial inclusion and exclusion criteria. Most included trials were reported from China, and others were reported from Australia, Germany, United Kingdom, and United States. Trials from China recruited participants largely from an inpatient or mixed inpatient‐outpatient setting, and most of the studies conducted outside of China recruited participants from primary healthcare and community settings. It is unclear how treatment protocols used in this research may be generalisable to acupuncture as it is usually practised. We found insufficient reporting of the rationale for acupuncture used in the research setting. Variation may reflect the context in which acupuncture is practised. However, one pragmatic trial delivered a treatment intervention with high external validity and evidence of generalisability (MacPherson 2013).
Meta‐analyses of clinical trials of antidepressant medication, in particular the new‐generation antidepressants, show that treatment effects were clinically significant only with extremely depressed patients (Kirsch 2008), and suggest that the pattern of treatment response may be attributed to a decrease in response to placebo rather than to an increase in response to medication. A recent systematic review and meta‐analysis confirmed that the placebo response in major depressive disorder is large, regardless of the intervention provided (Brunoni 2009). Acupuncture has been described as a complex intervention, and some of the incidental components of the effects of treatment may contribute to the placebo effect. We discuss this further in the section describing Quality of the evidence.
It should also be noted that none of the primary studies of comparisons between acupuncture and medication have reported that the purpose of the research was to examine equivalence or non‐inferiority, nor superiority. Many trials did not report on outcomes other than depression and did not consistently report adverse events; among these studies, we found that long‐term follow up was scarce.
Many Chinese studies were poorly reported, and despite many attempts, we were unable to obtain complete details of study design features relevant to risk of bias assessment. Reporting on the primary outcome of severity of depression was high, although inclusion and reporting of other outcome measures was low. Follow‐up data after trial completion were rarely provided. It is important that future trials include medium‐ and long‐term follow‐up, given the burden of disease and costs to the individual and society arising from depression. Given the placebo effect associated with depression and its treatment arising from attention, it is important that future trials include follow‐up and provide data from follow‐up periods.
Trials involving comparisons with medication have provided no data on compliance; therefore it is unclear whether outcomes of these study groups could have been affected by suboptimal doses of medication. In some cases, trials used medications currently removed from the market in some countries owing to safety issues and queries about lack of efficacy (Lv 2015;Tang 2003).
Quality of the evidence
Overall the quality of evidence for most comparisons was very low to moderate, limiting our confidence in trial findings. We rated few trials as having low risk of bias, and for most trials, we assigned a rating of high risk of bias in at least one domain.
We rated 75% of trials as having low risk of bias related to sequence generation, although we assessed most trials as having unclear risk of bias in terms of allocation concealment.
High risk of bias was most frequently related to the domains of blinding. However for many comparisons, performance and detection bias is likely to be high because blinding of participants to the interventions provided was not feasible. This caused review authors to downgrade evidence by at least one level for most comparisons, and by two levels when both blinding domains were rated as high risk in at least a third of included studies. For several comparisons, we included only one clinical trial, causing a downgrade for lack of precision.
We rated more than half of trials as having low risk of bias for the domain of attrition bias. We assessed less than half of trials as having low risk of selective bias, and we were able to access published protocols for only a few trials. Adherence to treatment was not well reported, and only a few trials assessed the integrity of blinding among acupuncture controls.
Many comparisons showed substantial (I2 > 50%) heterogeneity, and several had I2 > 90%. Although some of the heterogeneity can be explained by heterogeneity among the interventions themselves, as well as among controls, this finding was often significant enough to result in downgrading of the level of evidence. We were unable to examine the effect of study quality through a sensitivity analysis because we found too few studies that were at low risk of bias. The quality of reporting remains poor in many trials.
The quality of evidence as assessed via GRADE was very low to low for severity of depression, and very low to moderate for adverse events (see Table 1; Table 2; Table 4; and Table 5).
Potential biases in the review process
We excluded cross‐over trials from this review owing to lack of clarity regarding the appropriate period of washout for acupuncture trials. We did not systematically search Chinese language‐only databases for this version of the review; therefore trials meeting our selection criteria beyond those identified may exist. We attempted to minimise publication bias, but such bias remains a possibility because we did not identify for inclusion any trials from China showing a negative treatment effect. We excluded quasi‐randomised controlled trials for this review update (these trials were included in previous versions) because the body of published trials has increased.
An author of the previous version of this review was an author of an included trial. Other review authors extracted data from and assessed the quality of this trial.
Agreements and disagreements with other studies or reviews
We utilised an extensive search strategy, and we identified and included a greater number of trials (64) for our updated review than were identified for five other systematic reviews, which included between seven and 35 trials. Our review update represents a comprehensive assessment of current evidence and is the largest review to date. Five other systematic reviews have examined acupuncture for treatment of individuals with depression (Chan 2015; Leo 2007; Mukaino 2005; Wang 2008;Zhang 2010). Our findings reflect a broader range of comparisons than were included in the Wang 2008 and Leo 2007 reviews, which combined all modes of acupuncture stimulation in their meta‐analyses and excluded all comparisons with medication. Our updated findings differ significantly from those of Mukaino 2005, which included seven trials and found no differences between acupuncture and a wait‐list comparison, between acupuncture and sham acupuncture, or between electro‐acupuncture and antidepressant medication. This difference is likely explained by the larger body of randomised controlled trials reported over time and by differences among trials meeting the inclusion criteria for our review.
One systematic review ‐ Zhang 2010 ‐ found that acupuncture was superior to antidepressant medication for patients who had experienced post‐stroke depression. We did not examine this specific comparison in our review. However, when review authors in Zhang 2010 compared acupuncture plus medication versus medication alone or acupuncture monotherapy versus medication alone, they found no benefit for individuals with major depressive disorder in comparisons with selective serotonin reuptake inhibitor (SSRI) medications. Our review includes 11 studies that became available after publication of Zhang 2010 and provides updated evidence.
Our findings are very similar to those of the most recent review ‐ Chan 2015 ‐ which included a meta‐analysis of trials comparing acupuncture plus medication versus medication alone. This meta‐analysis indicated that acupuncture combined with SSRI medication was superior to SSRI medication alone.
Authors' conclusions
Implications for practice.
The 64 trials included in this review compared acupuncture alone or in combination with pharmaceutical therapy versus a range of comparator interventions. The reduction in severity of depression at the end of treatment was smaller when acupuncture was compared with control acupuncture than when acupuncture was compared with no treatment control, although we rated both sets of results as providing low‐quality evidence. The possible benefit of acupuncture provided alone or in conjunction with pharmaceutical medication such as a selective serotonin reuptake inhibitor (SSRI) compared with pharmaceutical monotherapy is uncertain owing to the very low quality of available evidence. The effect of acupuncture compared with psychological therapy is unclear. The risk of adverse events with acupuncture is also unclear, as most trials did not report these adequately. However, in general, the risk of adverse events associated with acupuncture is low (Melchart 2004;Witt 2009). Few trials reported on dropout, reduced use of medication, and quality of life. Evidence is insufficient to show the optimal type of acupuncture or characteristics of acupuncture dosage. Lack of medium‐term and long‐term follow‐up in clinical trials represents a significant limitation of the evidence base.
Implications for research.
Further randomised controlled trials are required to evaluate the effectiveness of acupuncture for treatment of individuals with depression. All future randomised trials should consider other outcome measures such as adverse event reporting and changes in quality of life, in addition to clinical outcomes. Greater attention should be given to methodological design, including randomisation and blinding of practitioners (when appropriate), outcome assessors, and analysts. Using a combination of patient‐reported scales and blinded clinician‐reported scales may help to ameliorate some of the issues associated with lack of participant blinding. Future trials must be adequately powered and conducted in an appropriate setting, and must provide comprehensive adverse event reporting and medium‐ and long‐term follow‐up (for at least a year) if they are to provide outcome data that will increase the level of quality of the evidence base. Researchers must examine the effects of acupuncture treatment dosage on clinical outcomes as well as the efficacy and effectiveness of other modes of stimulation, including laser acupuncture.
What's new
| Date | Event | Description |
|---|---|---|
| 14 December 2016 | New citation required and conclusions have changed | The previous version of this review did not show evidence of benefit for acupuncture. Low‐quality evidence now suggests a small reduction in severity of depression with acupuncture compared with no treatment/wait list/treatment as usual and control acupuncture. |
| 12 October 2016 | New search has been performed | 34 new studies have been added. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 2, 2005
| Date | Event | Description |
|---|---|---|
| 14 December 2009 | Amended | Slight clarification and copyediting provided for the 'Acknowledgements' section of the review |
| 26 April 2009 | New citation required and conclusions have changed | New search undertaken and review updated |
| 1 November 2008 | Amended | Review converted to new format |
| 24 February 2005 | Amended | Minor updates provided |
| 17 March 2004 | New citation required and conclusions have changed | Substantive amendments made |
Acknowledgements
The review authors would like to acknowledge the Cochrane Common Mental Disorders team for assistance with preparation of the original review and its update, including the Trials Search Co‐ordinator for assistance in developing the search strategy; as well as editors, co‐editors, and other staff within the team. We also would like to thank the Chinese Cochrane Centre for assistance in searching databases for trials published in the Chinese literature for inclusion in the first version of this review (published 2005, Issue 2). We also acknowledge assistance in Chinese to English translation provided by Kelly Ho and Song Mei Wu, and we thank Michael Arnold for his contributions in development of the protocol. We wish to acknowledge the valuable contributions of Hugh MacPherson to this review and to previous versions.
Appendices
Appendix 1. Update search CCMD‐CTR ‐ June 2016
The CCMD‐CTR was searches (to 17 June 2016) using the following terms:
((acupunct* or acupress* or acupoints* or electroacupunct* or electro‐acupunct* or auriculotherap* or auriculoacupunct* or moxibust*) and (depress* or "affective disorder*" or "affective symptoms" or mood)):ti,ab,kw,ky,emt,mh,mc
An additional search of PubMed was also conducted at this time and new studies incorporated into the CCMD‐CTR.
#1 “Acupuncture”[MeSH] OR “Acupuncture Therapy”[MeSH] #2 (acupunct*[tw] or acupress*[tw] or acupoint*[tw] or electroacupunct*[tw] or electro‐acupunct*[tw] or auriculotherap*[tw] or auriculoacupunct*[tw] or moxibust*[tw]) #3 depress*[ti] #4 ("Depression"[Majr] OR "Depressive Disorder"[Majr:NoExp]) OR "Depressive Disorder, Major"[Majr]) #5 “Randomized Controlled Trials as Topic”[MeSH] #6 “Randomized Controlled Trial”[pt] #7 (randomized[tiab] OR randomised[tiab]) #8 (RCT[tiab] OR (random*[tiab] AND allocat*[tiab]) OR (random*[tiab] AND assign*[tiab])) #9 trial[ti] #10 placebo*[tiab] OR sham[tiab] #11 (#1 OR #2) AND (#3 OR #4) AND (#5 OR #6 OR #7 OR #8 OR #9 OR #10)
Appendix 2. Appendix 1 Risk of bias
Criteria for judging risk of bias in the Risk of bias assessment tool.
SEQUENCE GENERATION
Was the allocation sequence adequately generated?
Criteria for a judgement of ‘YES’ (i.e. low risk of bias)
The investigators describe a random component in the sequence generation process such as:
referring to a random number table;
using a computer random number generator;
coin tossing;
shuffling cards or envelopes;
throwing dice; and
drawing lots.
*Minimisation may be implemented without a random element, and this is considered equivalent to being random. Criteria for a judgement of ‘NO’ (i.e. high risk of bias) Investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example, sequence generated by odd or even date of birth; sequence generated by some rule based on date (or day) of admission; or sequence generated by some rule based on hospital or clinic record number. Other non‐random approaches happen much less frequently than the systematic approaches mentioned above and tend to be obvious. They usually involve judgement or some method of non‐random categorisation of participants, for example:
allocation by judgement of the clinician;
allocation by preference of the participant;
allocation based on the results of a laboratory or a series of tests; and
allocation by availability of the intervention.
Criteria for a judgement of 'UNCLEAR' (uncertain risk of bias)
Insufficient information about the sequence generation process to permit a judgement of 'Yes' or 'No'
ALLOCATION CONCEALMENT
Was allocation adequately concealed? (short form: allocation concealment?)
Criteria for a judgement of ‘YES’ (i.e. low risk of bias)
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation.
Central allocation (including telephone, Web‐based, and pharmacy‐controlled randomisation.
Sequentially numbered drug containers of identical appearance.
Sequentially numbered, opaque, sealed envelopes.
Criteria for a judgement of ‘NO’ (i.e. high risk of bias)
Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on:
using an open random allocation schedule (e.g. a list of random numbers);
using assignment envelopes without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or were not sequentially numbered);
alternation or rotation;
date of birth;
case record number; or
any other explicitly unconcealed procedure.
Criteria for a judgement of 'UNCLEAR' (uncertain risk of bias)
Insufficient information about the sequence generation process to permit judgement of 'Yes' or 'No'. This is usually the case if the method of concealment is not described or is not described in sufficient detail to allow a definitive judgement, for example, if use of assignment envelopes is described but it remains unclear whether envelopes were sequentially numbered, opaque, and sealed.
BLINDING OF PARTICIPANTS, PERSONNEL, AND OUTCOME ASSESSORS
Was knowledge of allocated interventions adequately prevented during the study? (short form: blinding)
Criteria for a judgement of ‘YES’ (i.e. low risk of bias)
Any one of the following.
No blinding, but review authors judge that the outcome and the outcome measurement are not likely to be influenced by lack of blinding.
Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken.
Either participants or key study personnel were not blinded, but outcome assessment was blinded and non‐blinding of others was unlikely to introduce bias.
Criteria for a judgement of ‘NO’ (i.e. high risk of bias)
Any one of the following.
No blinding or incomplete blinding, and the outcome or outcome measurement is likely to be influenced by lack of blinding.
Blinding of key study participants and personnel attempted, but likely that blinding could have been broken.
Either participants or some key study personnel were not blinded, and non‐blinding or others was likely to introduce bias.
Criteria for a judgment of 'UNCLEAR' (uncertain risk of bias)
Any one of the following.
Insufficient information to permit a judgement of 'Yes' or 'No'.
The study did not address this outcome.
INCOMPLETE OUTCOME DATA
Were incomplete outcome data adequately addressed? (short form: Incomplete outcome data addressed?)
Criteria for a judgement of ‘YES’ (i.e. low risk of bias)
Any one of the following.
No missing data.
Reasons for missing outcome data unlikely to be related to true outcomes (for survival data, censoring unlikely to introduce bias).
Missing outcome data balanced in numbers across intervention groups, and similar reasons for missing data were provided across groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk was not enough to have a clinically relevant impact on the intervention effect estimate.
For continuous outcome data, the plausible effect size (difference in means or standardised difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size.
Missing data have been imputed by appropriate methods.
Criteria for a judgment of ‘NO’ (i.e. high risk of bias)
Any one of the following.
Reasons for missing outcome data likely to be related to true outcomes, with imbalance in numbers or reasons for missing data across intervention groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in the intervention effect estimate.
For continuous outcome data, the plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to have a clinically relevant impact on observed effect size.
'As treated' analysis done with substantial departure of the intervention received from that assigned at randomisation.
Potentially inappropriate application of simple imputation.
Criteria for a judgement of 'UNCLEAR' (uncertain risk of bias)
Any one of the following.
Insufficient reporting of attrition/exclusions to permit judgement of 'Yes' or 'No' (e.g. number randomised not stated, no reasons for missing data provided).
The study did not address this outcome.
SELECTIVE OUTCOME REPORTING
Are reports of the study free of the suggestion of selective outcome reporting? (short form: free of selective reporting?)
Criteria for a judgement of ‘YES’ (i.e. low risk of bias)
Any one of the following.
The study protocol is available and all of the study's prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way.
The study protocol is not available but it is clear that published reports include all expected outcomes, including those that were prespecified (convincing test of this nature may be uncommon).
Criteria for a judgement of ‘NO’ (i.e. high risk of bias)
Any one of the following.
Not all of the study's prespecified primary outcomes have been reported.
One or more primary outcomes are reported via measurements, analysis methods, or subsets of data (subscales) that were not prespecified.
One or more reported primary outcomes were not prespecified (unless clear justification for their reporting is provided, such as an unexpected adverse effect).
One or more outcomes of interest in the review are reported incompletely so that they cannot be entered into a meta‐analysis.
The study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Criteria for a judgement of 'UNCLEAR' (uncertain risk of bias)
Insufficient information to permit a judgement of 'Yes' or 'No'. It is likely that most studies will fall into this category.
OTHER POTENTIAL THREATS TO VALIDITY
Was the study apparently free of other problems that could put it at risk of bias? (short form: free of other bias?)
Criteria for a judgement of ‘YES’ (i.e. low risk of bias)
The study appears free of other sources of bias.
Criteria for a judgement of ‘NO’ (i.e. high risk of bias)
At least one important risk of bias is present. For example, the study:
had a potential source of bias related to the specific design used;
was stopped early owing to some data‐dependent process (including a formal‐stopping rule);
had extreme baseline imbalance;
has been claimed to have been fraudulent; or
had some other problem.
Criteria for a judgement of 'UNCLEAR' (uncertain risk of bias)
Risk of bias may be present, but either:
information is iinsuffiecient for assessment of whether an important risk of bias exists; or
rationale or evidence is insufficient to suggest that an identified problem will introduce bias.
Data and analyses
Comparison 1. Acupuncture versus no treatment/wait list/TAU.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of depression at the end of treatment | 5 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.06, ‐0.25] |
| 1.1 Manual acupuncture | 5 | 458 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.98, ‐0.15] |
| 1.2 Electro‐acupuncture | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐2.10, ‐0.43] |
| 2 Adverse events | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.24] |
| 2.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.35, 2.24] |
| 3 Severity of depression during treatment | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐6.75 [‐9.12, ‐4.38] |
| 3.1 Manual acupuncture | 2 | 107 | Mean Difference (IV, Random, 95% CI) | ‐7.04 [‐11.08, ‐3.00] |
| 3.2 Electro‐acupuncture | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐6.24 [‐9.86, ‐2.62] |
| 4 Severity of depression 0‐6 months after treatment | 1 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.01, ‐0.79] |
| 4.1 Manual acupuncture | 1 | 237 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐3.01, ‐0.79] |
| 5 Severity of depression 6‐12 months after treatment | 1 | 235 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐2.53, 0.53] |
| 5.1 Manual acupuncture | 1 | 235 | Mean Difference (IV, Random, 95% CI) | ‐1.0 [‐2.53, 0.53] |
| 6 Remission of depression | 2 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.77, 3.65] |
| 6.1 Manual acupuncture | 2 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.77, 3.65] |
| 7 Change in use of medication at the end of treatment | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| 7.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.73, 1.14] |
| 8 Dropout from treatment | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.21, 4.88] |
| 8.1 Manual acupuncture | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.21, 4.88] |
Comparison 2. Acupuncture versus control acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of depression at the end of the intervention | 14 | 841 | Mean Difference (IV, Random, 95% CI) | ‐1.69 [‐3.33, ‐0.05] |
| 1.1 Manual acupuncture vs invasive control | 7 | 418 | Mean Difference (IV, Random, 95% CI) | ‐2.97 [‐6.26, 0.31] |
| 1.2 Electro‐acupuncture vs invasive control | 5 | 251 | Mean Difference (IV, Random, 95% CI) | 0.43 [‐0.54, 1.40] |
| 1.3 Electro‐acupuncture vs non‐invasive electro‐control | 2 | 99 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐2.14, 2.48] |
| 1.4 Laser acupuncture vs non‐invasive control | 2 | 73 | Mean Difference (IV, Random, 95% CI) | ‐5.51 [‐8.30, ‐2.73] |
| 2 Adverse events | 5 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.93, 2.86] |
| 2.1 Manual acupuncture vs invasive control | 1 | 17 | Risk Ratio (M‐H, Random, 95% CI) | 2.5 [0.15, 40.37] |
| 2.2 Electro‐acupuncture vs invasive control | 4 | 244 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.99, 3.25] |
| 2.3 Electro‐acupuncture vs non‐invasive control | 1 | 39 | Risk Ratio (M‐H, Random, 95% CI) | 0.4 [0.05, 3.08] |
| 3 Severity of depression during treatment | 6 | 413 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.81, 0.90] |
| 3.1 Manual acupuncture vs invasive control | 2 | 117 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐2.55, 2.74] |
| 3.2 Electro‐acupuncture vs invasive control | 4 | 197 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.92, 1.24] |
| 3.3 Electro‐acupuncture vs non‐invasive control | 2 | 99 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐2.71, 1.80] |
| 4 Severity of depression at 0‐6 months' follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Manual acupuncture vs invasive control | 1 | 95 | Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐0.98, ‐0.72] |
| 5 Remission of depression | 10 | 601 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [1.14, 3.21] |
| 5.1 Manual acupuncture vs invasive control | 5 | 368 | Risk Ratio (M‐H, Random, 95% CI) | 1.89 [0.75, 4.75] |
| 5.2 Electro‐acupuncture vs invasive control | 2 | 87 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.35, 4.29] |
| 5.3 Electro‐acupuncture vs non‐invasive electro‐control | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [0.60, 7.67] |
| 5.4 Laser acupuncture vs non‐invasive control | 2 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [1.48, 6.09] |
| 6 Quality of life (emotional) during treatment | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐1.98 [‐5.41, 1.45] |
| 6.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.09 [‐6.54, 2.36] |
| 6.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐7.18, 3.56] |
| 7 Quality of life (emotional) at the end of treatment | 2 | 167 | Mean Difference (IV, Random, 95% CI) | ‐2.25 [‐5.89, 1.39] |
| 7.1 Manual acupuncture vs invasive control | 1 | 17 | Mean Difference (IV, Random, 95% CI) | ‐5.0 [‐36.47, 26.47] |
| 7.2 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.55 [‐7.38, 2.28] |
| 7.3 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐7.38, 3.86] |
| 8 Quality of life (physical) during treatment | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐4.74, 2.77] |
| 8.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐2.62 [‐7.07, 1.83] |
| 8.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.26 [‐4.12, 6.64] |
| 9 Quality of life (physical) at the end of treatment | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐5.12 [‐10.38, 0.13] |
| 9.1 Electro‐acupuncture vs invasive control | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐7.61 [‐12.38, ‐2.84] |
| 9.2 Electro‐acupuncture vs non‐invasive control | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐2.23 [‐7.81, 3.35] |
| 10 Change in medication | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.71, 0.93] |
| 10.1 Electro‐acupuncture vs non‐invasive control | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.71, 0.93] |
| 11 Dropout from treatment | 7 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.62, 1.75] |
| 11.1 Manual acupuncture vs invasive control | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.6 [0.16, 2.29] |
| 11.2 Electro‐acupuncture vs invasive control | 4 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.51, 2.02] |
| 11.3 Electro‐acupuncture vs non‐invasive control | 4 | 217 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.56, 3.91] |
2.10. Analysis.

Comparison 2 Acupuncture versus control acupuncture, Outcome 10 Change in medication.
Comparison 3. Acupuncture versus medication.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of depression at the end of treatment | 31 | 3127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.40, ‐0.05] |
| 1.1 Manual acupuncture vs SSRI | 16 | 1570 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.50, 0.04] |
| 1.2 Electro‐acupuncture vs SSRI | 5 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.85, ‐0.10] |
| 1.3 Manual acupuncture vs TCAs | 3 | 397 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐1.25, 0.69] |
| 1.4 Electro‐acupuncture vs TCAs | 5 | 801 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.42, 0.01] |
| 1.5 Manual acupuncture vs other antidepressant | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.73, 0.29] |
| 1.6 Electro‐acupuncture vs heterocyclic antidepressants | 1 | 61 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [‐0.21, 0.80] |
| 1.7 Electro‐acupuncture vs other antidepressant | 1 | 41 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.52, 0.70] |
| 2 Adverse events | 3 | 481 | Mean Difference (IV, Random, 95% CI) | ‐4.32 [‐7.41, ‐1.23] |
| 2.1 Manual acupuncture vs SSRI | 3 | 481 | Mean Difference (IV, Random, 95% CI) | ‐4.32 [‐7.41, ‐1.23] |
| 3 Severity of depression during treatment | 9 | 552 | Mean Difference (IV, Random, 95% CI) | ‐1.67 [‐2.91, ‐0.43] |
| 3.1 Manual acupuncture vs SSRI | 5 | 340 | Mean Difference (IV, Random, 95% CI) | ‐1.38 [‐3.20, 0.45] |
| 3.2 Electro‐acupuncture vs SSRI | 3 | 112 | Mean Difference (IV, Random, 95% CI) | ‐2.58 [‐4.38, ‐0.78] |
| 3.3 Manual acupuncture vs TCAs | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐3.65, 2.05] |
| 4 Severity of depression 0‐6 months after treatment | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐7.60, ‐3.60] |
| 4.1 Manual acupuncture vs other antidepressant medication | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐5.60 [‐7.60, ‐3.60] |
| 5 Remission of depression | 25 | 2918 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.05, 1.29] |
| 5.1 Manual acupuncture vs SSRI | 14 | 1332 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.98, 1.37] |
| 5.2 Electro‐acupuncture vs SSRI | 4 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.94, 1.75] |
| 5.3 Manual acupuncture vs TCAs | 4 | 620 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.03, 1.69] |
| 5.4 Electro‐acupuncture vs TCAs | 4 | 778 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.88, 1.21] |
| 6 Dropout from treatment | 5 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.20, 3.71] |
| 6.1 Manual acupuncture vs SSRI | 2 | 134 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.03, 2.47] |
| 6.2 Electro‐acupuncture vs SSRI | 3 | 112 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.43, 7.79] |
Comparison 4. Acupuncture plus medication versus medication.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of depression at the end of treatment | 11 | 813 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐1.63, ‐0.66] |
| 1.1 Manual acupuncture plus SSRI vs SSRI | 8 | 539 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.09, ‐0.55] |
| 1.2 Electro‐acupuncture plus SSRI vs SSRI | 5 | 274 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.84 [‐1.16, ‐0.51] |
| 2 Adverse events | 3 | 200 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.86, 0.23] |
| 2.1 Manual acupuncture plus SSRI vs SSRI | 2 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.20, 0.47] |
| 2.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.39 [‐4.27, ‐2.50] |
| 3 Severity of depression during treatment | 6 | 514 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.60 [‐2.45, ‐0.76] |
| 3.1 Manual acupuncture plus SSRI vs SSRI | 6 | 432 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐2.83, ‐0.80] |
| 3.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.19, ‐0.21] |
| 4 Remission of depression | 9 | 618 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.85, 1.73] |
| 4.1 Manual acupuncture plus SSRI vs SSRI | 5 | 299 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.65, 2.73] |
| 4.2 Electro‐acupuncture plus SSRI vs SSRI | 5 | 273 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.75, 1.80] |
| 4.3 Manual acupuncture plus heterocyclic antidepressant vs medication alone | 1 | 46 | Risk Ratio (M‐H, Random, 95% CI) | 4.36 [0.53, 36.12] |
| 5 Quality of life (physical) | 1 | 127 | Mean Difference (IV, Fixed, 95% CI) | 1.19 [0.33, 2.05] |
| 5.1 Manual acupuncture plus SSRI vs SSRI | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.15, 2.65] |
| 5.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.18, 2.18] |
| 6 Quality of life (emotional) | 2 | 219 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.90, 1.40] |
| 6.1 Manual acupuncture plus SSRI vs SSRI | 2 | 111 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐1.46, 1.65] |
| 6.2 Electro‐acupuncture plus SSRI vs SSRI | 2 | 108 | Mean Difference (IV, Random, 95% CI) | 0.35 [‐2.00, 2.70] |
| 7 Change in use of medication | 2 | 236 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.22, 0.67] |
| 7.1 Manual acupuncture plus SSRI vs SSRI | 2 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.20, 0.72] |
| 7.2 Electro‐acupuncture plus SSRI vs SSRI | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.13, 1.30] |
| 8 Dropout from treatment | 5 | 426 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.35, 1.42] |
| 8.1 Manual acupuncture plus SSRI vs SSRI | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.18, 1.15] |
| 8.2 Electro‐acupuncture plus SSRI vs SSRI | 3 | 192 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.43, 3.51] |
Comparison 5. Acupuncture versus psychological therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of depression at the end of treatment | 2 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.33, 0.33] |
| 1.1 Manual acupuncture | 2 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.33, 0.33] |
| 2 Adverse events | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.29, 1.33] |
| 2.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.29, 1.33] |
| 3 Severity of depression 0‐6 months after treatment | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.51, 1.51] |
| 3.1 Manual acupuncture | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.5 [‐0.51, 1.51] |
| 4 Severity of depression 6‐12 months | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.80, 2.00] |
| 4.1 Manual acupuncture | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.80, 2.00] |
| 5 Remission of depression | 0 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Manual acupuncture | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Change in use of medication | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.10] |
| 6.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.10] |
| 7 Dropout from treatment | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.08, 0.90] |
| 7.1 Manual acupuncture | 1 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.08, 0.90] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allen 1998.
| Methods | Single‐blind randomised controlled trial of acupuncture, non‐specific acupuncture, and a wait‐list control | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV Age: 18 to 45 years Participant information: 38 women Location: United States (community) Inclusion/Exclusion: Exclusion criteria: dysthymia or chronic depression, history of psychosis or mania, substance abuse, current treatment, endocrine abnormalities, history of central nervous system lesions or any medical condition causing depression, pregnancy, suicide potential |
|
| Interventions |
(1) Duration: 8 weeks (12 sessions) Frequency of treatment: The intervention involved 2 sessions a week for the first 4 weeks, followed by 1 session a week thereafter. Treatment protocol: Acupuncture ‐ no details provided (2) Duration: 8 weeks (12 sessions) Frequency of treatment: The intervention involved 2 sessions a week for the first 4 weeks, followed by 1 session a week thereafter. Treatment protocol: Non‐specific acupuncture ‐ no details provided (3) Duration: 8 weeks Frequency of treatment: N/A Treatment protocol: The wait list control received acupuncture at 8 weeks. |
|
| Outcomes |
Time points for assessment: baseline, 8 and 16 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Beck Depression Inventory (BDI) |
|
| Notes | A power calculation was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was computer generated. |
| Allocation concealment (selection bias) | Low risk | Randomisation was undertaken centrally. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants in the 2 acupuncture groups and the therapist were blind. It remains possible that the acupuncture therapists developed some awareness between treatments. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The assessing clinician was blind. It was unclear whether the analyst was blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Five women dropped out (13%) ‐ 2 from the acupuncture group, 2 from non‐specific acupuncture, and 1 from wait‐list control. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Insufficient information was presented to examine other sources of bias, for example, imbalance at randomisation. |
Allen 2006.
| Methods | Single‐blind randomised controlled trial of acupuncture, non‐specific acupuncture, and a wait‐list control | |
| Participants |
Diagnosis: major depressive disorder (MDD) Method of diagnosis: DSM‐IV criteria and HAMD score > 14 Age: 18 to 65 years Participant information: 157 males and females Location: community setting, USA Inclusion/Exclusion: Exclusion criteria: dysthymia or a chronic MDD over longer than 2 years, seasonal pattern; current Axis I diagnosis besides MDD or Axis II cluster B disorder; history of psychosis or mania, substance abuse, or dependence within past 4 months; current relevant treatment; endocrine abnormalities; history of CNS involvement (seizures); medical condition believed to cause depression; active suicidal risk; pregnancy |
|
| Interventions | Acupuncture practitioners were NCCAOM board‐certified acupuncturists with a minimum of 4 years and in practice for 5 years. (1) Duration: 8 weeks (12 sessions) Frequency of treatment: Treatment was administered twice a week for 4 weeks, followed by once a week for 4 weeks. Treatment protocol: The acupuncture group received individualised TCM treatment. Point selection used unilateral and bilateral points and 10 to 16 needles; the depth of needle insertion was based on TCM principles; de qi sensation was obtained, and needles were retained for 20 minutes. No co‐interventions were allowed. (2) Duration: 8 weeks (12 sessions) Frequency of treatment: Treatment was administered twice a week for 4 weeks, followed by once a week for 4 weeks. Treatment protocol: The control group consisted of an active comparator involving non‐specific acupuncture. Valid acupuncture points were used but were not designed to treat depression. Points were needled as above. (3) Duration: 8 weeks Frequency of treatment: N/A Treatment protocol: Wait‐list control |
|
| Outcomes |
Time points for assessment: All patients completed the Beck Depression Inventory at weekly intervals. Blinded outcome assessors used the Hamilton Depression Rating Scale at 4‐weekly intervals. Outcomes: Hamilton Depression Rating Scale (HAMD) Beck Depression Inventory (BDI) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of generating randomisation schedule was not reported. |
| Allocation concealment (selection bias) | Low risk | The schedule was devised by the first trial author and was made available only on completion of assessments. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and treating acupuncturists were blind to the study hypothesis. The non‐specific intervention involved valid acupuncture points, and therapists administering acupuncture in this group would perceive that they were providing a valid treatment. Therapist expectations were assessed; the blinding strategy suggests that acupuncturists may have developed some awareness, but no evidence suggested that this influenced the clinical outcome. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessing clinicians were blind to study groups. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Six participants (3.8%) were post‐randomisation exclusions. Valid intention‐to‐treat sample acupuncture n = 50, non‐specific acupuncture n = 49, wait‐list control n = 52. Twenty (13%) participants terminated treatment before completion of the intervention, but this was not different between groups. A further 42 (28%) participants terminated treatment before 16 weeks. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | No imbalances were evident at randomisation. The study appears free of other sources of bias. |
Andreescu 2011.
| Methods | Acupuncture vs control acupuncture | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV and SCID with score > 14, mild to moderate depression Age: not stated Participant information: 53 participants Location: University of Pittsburgh Medical Center (UPMC) Shadyside, Center for Complementary Medicine, Pittsburgh, Pennsylvania, USA Inclusion/Exclusion: Exclusion criteria: severe MDD, suicidal, seizure disorder, psychosis, bipolar disorder, chronic MDD (i.e. duration > 2 years), treatment‐resistant MDD, history of substance abuse within past 6 months |
|
| Interventions | All medication was tapered before randomisation and participants remained free of psychotropic medication during the study. No other interventions were used. (1) Duration: 6 weeks (12 sessions) Frequency of treatment: 2/week Treatment protocol: Each session was administered over 30 minutes. Points Du 20 and Yingtang were needled. Electro‐acupuncture (EA) was administered. 0.22 × 30 mm needles were inserted. Electro‐stimulator 4C connected current 3 to 5 mA had a frequency of 2 Hz. Treatment was administered by a practitioner with 4 years of training who had completed Masters of Acupuncture and TCM and was certified by NCCAOM, had been in practice for 5 years, and had clinical practice with treatment of patients with anxiety and depression. (2) Duration: 6 weeks (12 sessions) Frequency of treatment: 2/week Treatment protocol: Control group: non‐scalp points with sham EA. Needles were inserted at 2 points away from classical points near channels, and no current was applied to the needle. Needles were inserted obliquely to 1 cm. |
|
| Outcomes |
Time points for assessment: unclear for HAMD, weekly for side effects rating scale; SF‐36 2 weeks post intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Comparison of responders in each group defined as a score ≤ 10 with relative decrease of 50% from baseline Side effects rating scale SF‐36 |
|
| Notes | ITT was undertaken. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Envelopes were sealed/opaque. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and key study personnel was ensured; it is unlikely that blinding could have been broken. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The trained research associate undertaking measurement was blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for missing outcome data were unlikely to be related to true outcomes (for survival data, censoring was unlikely to introduce bias). Treatment group: 4 were attrition, 1 could not be contacted, 2 preferred a different treatment regimen, 1 withdrew owing to physical health. Control group: All 3 could not be contacted. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
Bosch 2015.
| Methods | Randomised controlled trial of 50 participants comparing manual acupuncture vs wait‐list control | |
| Participants |
Diagnosis: depression Method of diagnosis: ICD F33.2 Age: 48.68 years (experimental), 46.32 years (control) Participant information: 3 males, 22 females (experimental), 2 males 23 females (control) Location: Germany (psychiatric clinic) Inclusion/Exclusion: Inclusion criteria: not specified, apart from the diagnosis of depression Exclusion criteria: addiction (other than nicotine), epilepsy or other neurological disorders, other co‐morbid psychiatric disorders |
|
| Interventions |
(1) Duration: 12 weeks (12 sessions) Frequency of treatment: 1/week Treatment protocol: TCM‐style acupuncture/manual acupuncture. Needles were retained for 60 minutes. Point selection was individualised with the following points being most common (% of all treatments): Hegu (LI4) (96%), Sanyinjiao (SP6) (96%), Yinlingquan (SP9) (96%), Shenmen (HT7) (95%), Taixi (KI3) (95%), Sishencong (EX‐HN1) (92%), Zusanli (ST36) (91%), Taichong (LR3) (78%), Quchi (LI11) (53%), Zhaohai (KI6) (53%), Guanyuan (CV4) (46%), Yanglingquan (GB34) (36%), Gongsun (SP4) (34%), Xuehai (SP10) (34%), and Lieque (LU7) (32%). All acupuncture was performed by a licensed Oriental medical practitioner with more than 5 years of clinical experience. (2) Duration: 12 weeks Frequency of treatment: N/A Treatment protocol: Wait‐list control |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Beck Depression Inventory (BDI) |
|
| Notes | ITT not undertaken | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Patient‐reported outcomes were used; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropout rate was high (> 20%). |
| Selective reporting (reporting bias) | Unclear risk | Insufficient details were provided. |
| Other bias | Unclear risk | Insufficient details were provided. |
Cheng 2007.
| Methods | Randomised controlled trial of abdominal acupuncture vs electro‐acupuncture and standard care | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: depression diagnosed by CCMD and DSM‐II Age: 60 to 85 years Participant information: 60 participants Location: inpatients at the Department of Neurology at the First Hospital Affiliated to Changchun China Inclusion/Exclusion: Inclusion criteria: cerebral infarction or cerebral haemorrhage; no history of depression or abuse of medication or alcohol and no known allergies to medications; no severe heart, lung, liver, or kidney disease; no loss of speech Exclusion criteria: history of mental disorders; taking antidepressants in past 2 weeks; severe depression; HAMD > 35; allergic to alcohol or medications; cardiovascular, cerebral, liver, kidney, or blood pathology conditions; do no meet inclusion criteria; not taking medication as advised or dropped out halfway; fainting during acupuncture; infection at acupuncture points |
|
| Interventions |
(1) Duration: 6 weeks (21 treatments) Frequency of treatment: every second day Treatment protocol: The treatment group received abdominal acupuncture, with stimulation to acupuncture points CV12 Zhong Wan, CV10 Xia Wan, CV6 Qi Hai, CV4 Guan Yuan, ST24 Hua Rou Men (on both sides), ST26 Wai Ling, and Tai Heng. Acupuncture needles were inserted perpendicular to a depth before the muscle layer. Needles were inserted quickly ‐ only twirling no lifting, and de qi sensation was not obtained. Needles were left in for 30 minutes. Needles used were of the Hwato brand and were manufactured at Suzhouby Tai xin san lI medical product company, H model, 0.35 mm × 40 mm, 0.30 mm × 25 mm, 0.30 mm × 50 mm. (2) Duration: 6 weeks (21 treatments) Frequency of treatment: every second day Treatment protocol: Electro‐acupuncture to points DU 20 Baihui, DU24 Shen Ting, M‐HN‐3 Yintang, M‐NH‐1 Shishenchong, LIV 3 Taichong, and HT 7 Shenmen. Baihui was needled 1 cun parallel to the skin, Shenting was needled 0.5 cun parallel to the skin, Yintang was needled 0.5 cun parallel to the skin, Shishenchong was needled parallel to the skin, Taichong was needled perpendicular 0.5 to 1 cun, Shenmen was needled perpendicular 0.5 cun. The electro‐acupuncture machine was connected to needles administered at a frequent pulse frequency at 4 Hz and intermittent pulse at 20 Hz. Positive pulse amplitude at 50 V and negative pulse amplitude at 35 V. During treatment, patients should feel an achey numbness, a sensation of fullness, or twitching of muscle. Needles were left in for 30 minutes. Electro‐machine model GD6805X, manufactured by Xia xi san yuan medical equipment company, was used. (3) Duration: 6 weeks Frequency of treatment: treatment administered every second day. Treatment protocol: The control was standard care for stroke rehabilitation. |
|
| Outcomes |
Time points for assessment: 2, 4, and 6 weeks after the start of the study Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No information could be obtained from trial authors. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether analysts and assessing clinicians were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up were reported. Data on all participants were analysed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance in randomisation at baseline between groups. The study appears free of other sources of bias. |
Chung 2015.
| Methods | Electro‐acupuncture vs minimal acupuncture vs control acupuncture controlled trial | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV and clinician assessment via structured interview Age: not stated Participant information: 150 participants Location: 4 regional psychiatric outpatient clinics in Hong Kong Inclusion/Exclusion: Inclusion criteria: age 18‐70 years, insomnia >3 nights /week for last 3 months, Insomnia severity index score >15, fixed dose of antidepressants in last 3 months Exclusion criteria: HAMD score > 18, apnoea hypopnoea index ≥ 10 or periodic limb movement disorder ≥ 15, significant suicidal risk, previous diagnosis of schizophrenia, psychotic disorder, bipolar disorder, alcoholism, substance abuse, pregnancy or breastfeeding, infection close to acupuncture points, serious illness, acupuncture in previous 12 months, CHM within 2 weeks before baseline measurements, increased dose of hypnotics within 4 weeks of baseline measures |
|
| Interventions | Acupuncture experience of person administering treatment: registered acupuncturist with at least 3 years' experience (1) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: TCM‐style acupuncture. Choice of points used: bilateral ear shenmen, Sishencong Anmian, PC6, Ht7, SP6 Yintang GV20 Mode of stimulation:depth of insertion 2 to 25 mm. De qi obtained if possible. Electro‐stimulator attached to all needles, current 0.4 ms at 4 Hz needles left for 30 minutes (2) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Minimal: at points thought to have no effect and avoidance of de qi. Points on forearm 1 inch lateral to HE3 and HE7, I inch lateral to Lu3, and 0.5 inch dorsal to GB29, pony forehead, and ear. Electro‐stimulator the same (3) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Placebo: Streitberger placebo needle placed at 1 inch beside acupuncture points used in acupuncture group connected to electro‐stimulator with no current |
|
| Outcomes |
Time points for assessment: Outcome assessment at 1 and 5 weeks post treatment Adverse events assessed after 3rd, 6th, and 9th treatments Outcomes: Hamilton Depression Rating Scale (HAMD) Secondary outcomes: quality of life based on SF‐36 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated assignment was used. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and key study personnel was ensured, and it is unlikely that the blinding could have been broken. Credibility and blinding of treatment were assessed. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Study personnel were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, with similar reasons provided for missing data across groups; 16 (10%) dropped out during treatment, and 18 (12%) withdrew at 5 weeks. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
Ding 2003.
| Methods | Acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: Diagnoses were based on DSM‐II‐R and HAMD scales. Age: not stated Participant information: 62 participants Location: Beijing Hospital of Integration of Chinese and Western Medicine, China Inclusion/Exclusion: Exclusion criteria: none specified |
|
| Interventions |
(1) Duration: unclear (40 sessions) Frequency of treatment: daily for 10 days, then 2‐ to 3‐day break Treatment protocol: Acupuncture points on the Du meridian were needles including DU 20 Baihui, DU 24 Shenting, DU 16 Feng fu. Additional points were used including PC6 Neiguan (both sides), LI4 Hegu (both sides), GB20 Feng chi (both sides). Needles of 30 gauge 1 to 1.5 cun (Chinese unit of measurement) long were used, needled to a depth of 0.5 to 1 cun. Needles were manipulation using reinforcing reducing method. Once de qi was obtained, needles were left in for 30 minutes. (2) Duration: 60 days Frequency of treatment: daily Treatment protocol: The control group received medication including fluoxetine 20 mg/d for 60 days. |
|
| Outcomes |
Time points for assessment: before treatment, 30 days into treatment, 60 days into treatment Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | Two participants dropped out owing to adverse effects. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No information could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The study participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether the assessing clinician(s) and the analyst were blind to the study group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two participants (1 from each group) were excluded post randomisation with no details reported. Data on primary outcome were available for 60 participants. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | It was unclear whether baseline characteristics were comparable. |
Dong 2007.
| Methods | Three‐arm randomised controlled trial of electro‐acupuncture vs acupuncture vs medication (fluoxetine) among participants with post‐stroke depression | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: depression according to DSM‐IV, CCMD‐3, and HAMD score > 20 Age: not stated Participant information: 108 participants Location: inpatients or day patients from the Heilongjiang Provincial Academy of TCM Hospitial, China Inclusion/Exclusion: Exclusion criteria: a severe health condition, pregnancy or breastfeeding, long‐term medication, plasma 5‐HT and SSRI‐type medications taken together in the past 2 weeks, lack of willingness or suitability to be participants in this clinical trial, severe suicidal ideation or behaviour not suitable for patient to be medicated, organic mental disorder, depression caused by psychoactive substances or non‐addictive medications |
|
| Interventions |
(1) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: Electro‐acupuncture. Points stimulated include GB5 Xuan Lu, DU17 Nao Hu, GV18 Qiang Jian, GB15 Tou lin qi, GB14 Yang Bai, GB 8 Shuai Gu, GB 7 Qu Bin, GV24 Shen Ting, M‐HN‐3 Yin Tang. Each acupuncture needle was inserted to a depth of 40 to 50 mm, stimulation used a fast but small angled twirling manipulation method, at 200 twirls per minute, with each needle manipulated for 1 minute. Needles were then connected to an electro‐acupuncture device, model G6805‐I. A continuous pulse was used, with frequency set at 120 to 250 pulse per minute. Intensity was set at a level tolerable to the participant. Stimulation was given over 30 minutes, with needles retained for 1 hour. (2) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: Manual acupuncture of non‐point‐through‐point (NON). Acupuncture was administered to points GV20 Baihui, M‐HN‐3 Yintang, M‐HN‐1 Shishencong, PC6 Neiguan, HT7 Shenmen, SP6 Sanyinjiao, LI4 Hegu, and LIV3 Taichong. Needles were inserted and de qi obtained, needles were manipulated using either lifting twirling reinforcing‐dispersing method or reinforcing‐dispersing manipulation methods. Needles were retained for 1 hour. Hwato acupuncture needles, manufactured by Suzhou medical product company, with dimensions 0.38 mm × 40 mm to 40 mm were used. (3) Duration: 30 days Frequency of treatment: daily Treatment protocol: The medication group received fluoxetine. Participants initially were given a 20‐mg/d dose; after 2 weeks with no severe side effects observed, the dose was increase to 80 mg/d. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were reported. |
| Allocation concealment (selection bias) | Unclear risk | No communication was received from trial authors in response to a letter requesting further details on study methods. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind to their group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details on the blinding status of the assessing clinician(s) and analyst were reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Exclusions and loss of data were not explained. Data on one primary outcome are complete. Data on secondary outcomes are incomplete. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Groups were comparable at baseline. The study appears free of other sources of bias. |
Du 2005.
| Methods | Randomised controlled trial comparing 2 types of manual acupuncture with medication (fluoxetine) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 20 Age: not stated Participant information: 103 women Location: outpatient setting, China Inclusion/Exclusion: Exclusion criteria: schizophrenia; interstitial disease; physical illness that can cause symptoms of depression; schizophrenia and other psychotic disorders; heart, liver, and kidney system diseases; glaucoma |
|
| Interventions |
(1) Duration: 6 weeks (42 sessions) Frequency of treatment: daily Treatment protocol: Harmonize spirit soothe liver acupuncture group Points needled: Baihui (DU20); Fengfu (DU16); Shuigou (DU26); Yintang (EX‐HN 3); Sishencong (EX‐HN 1);Taichong (LR 3); Ganshu (BL18) (2) Duration: 6 weeks (42 sessions) Frequency of treatment: daily Treatment protocol: Regular acupuncture group Points needled: Qimen (LV14); Taichong (LR 3); Yanglingquan (GB34); Zhigou (SJ6); Neiguan (PC6); Zusanli (ST36) (3) Duration: 6 weeks Frequency of treatment: daily treatment. Treatment protocol: Control group: fluoxetine 20 mg/d for 6 weeks |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) SDS SCL‐90 Cured rate based on HAMD score |
|
| Notes | No ITT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reason for missing outcome data is likely to be related to true outcomes, with imbalance in numbers or reasons for missing data across intervention groups. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was not provided. |
Duan 2008.
| Methods | Randomised controlled trial of electro‐acupuncture, medication (fluoxetine), and electro‐acupuncture plus medication | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3 and HAMD score of 20 to 35 Age: 18 to 60 years Participant information: 75 participants Location: inpatients or day patients at the Department of Neurology, PLA General Hospital, Beijing, China Inclusion/Exclusion: Inclusion criteria: history of severe neurological or physical disease, no history of mental illness; willingness to participate in this study Exclusion criteria: schizophrenia and other mental disorders; central nervous system organic disease; pregnancy or breastfeeding, or planning pregnancy during treatment; severe depression with HAMD score of 35; suicidal tendencies; known allergies to fluoxetine |
|
| Interventions |
(1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture plus medication. Acupuncture points Baihui DU 20, M‐HN‐3 Yintang were stimulated. Additional points were added based on differential patterns: Liver qi stagnation type add LIV3 Taichong, LI4 Hegu; Fire due to qi stagnation type add LIV2 Xing jian; Melancholy injuring the spirit type add Anmian, Shenmen HT7, Neiguan PC6; heart and spleen deficiency add SP6 Sanyinjiao, Zhusanl ST36; Yin deficiency with excess fire type add KD3 Taixi and KD6 Zhaohai. GV20 Baihu and DU24 Shen ting were connected to electro‐acupuncture machine model G 6805‐1, using continuous pulse, frequency set at 120 to 250 times per minute. Strength was set at a comfort level for the participant. Electro‐acupuncture was administered over 30 minutes, and needles were retained for 1 hour. Medication consisted of fluoxetine 20 mg per day, administered over 6 weeks. (2) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture only. Acupuncture points Baihui DU 20, M‐HN‐3 Yintang were stimulated. Additional points were added based on differential patterns: Liver qi stagnation type add LIV3 Taichong, LI4 Hegu; Fire due to qi stagnation type add LIV2 Xing jian; Melancholy injuring the spirit type add Anmian, Shenmen HT7, Neiguan PC6; heart and spleen deficiency add SP6 Sanyinjiao, Zhusanl ST36; Yin deficiency with excess fire type add KD3 Taixi and KD6 Zhaohai. GV20 Baihu and DU24 Shen ting were connected to electro‐acupuncture machine model G 6805‐1, using continuous pulse, frequency set at 120 to 250 times per minute. Strength was set at a comfort level for the participant. Electro‐acupuncture was administered over 30 minutes, and needles were retained for 1 hour. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Medication only, fluoxetine 20 mg per day |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was unclear. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind, but it was unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Five (6%) participants dropped out from the trial ‐ 2 in the medication group owing to side effects, 2 in the electro‐acupuncture group owing to work commitments and a family member death, and 1 in the acupuncture plus medication group owing to side effects attributed to the medication. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | No imbalances in randomisation were evident at baseline. The study appears free of other sources of bias. |
Duan 2011.
| Methods | Randomised controlled trial of electro‐acupuncture plus medication (fluoxetine) or medication only | |
| Participants |
Diagnosis: depression Method of diagnosis: ICD‐10 and HAMD score 18 to 30 Age: 18 to 50 years Participant information: 75 participants Location: outpatient setting recruited at the Chinese PLA General Hospital, The General Hospital of the People's Liberation Army, China Inclusion/Exclusion: Inclusion criteria: first onset, no serious cerebral organic disease, no other mental health history Exclusion criteria: schizophrenia or other mental disorders; organic diseases such as tumours and central nervous system diseases; pregnancy or lactation, or may be pregnant during treatment; severe depression or relapsed depression, or HAMD score 35 points or with suicidal tendencies; intolerant or hypersensitive to fluoxetine |
|
| Interventions |
(1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Acupuncture points: GV20 and Yintang. For insomnia, add Sishencong (Extra‐HN), Anmian Ⅰ (Extra 8), Sanyinjiao (SP6), Taixi (KI3), and Zhaohai (KI6), etc.; for headache or dizziness, Shenting (DU24), Benshen (GB13), and Fengchi (GB20), etc.; for digestion syndromes, Zhongwan (ZH12), Tianshu (ST25), Liangqiu (ST34), Fenglong (ST40), Zusanli (ST36), and Neiting (ST44), etc.; for cardio syndromes, Shenmen (H7), Neiguan (P6), and Sanyinjiao (SP6), etc.; for chronic pain, Back‐shu points for general malaise, Wushu points, etc. A good needle sensation was administered and described by participants as soreness, numbness, heaviness, or distension; was achieved when needling each point. After achieving the needling sensation, compulsory points were connected to a type G68052‐Ⅰ electro‐acupuncture apparatus. The output wave was continuous, with a frequency of 2 Hz; the output power was regulated according to each participant's tolerance. An electric stimulator was connected for 30 to 40 minutes, and needles were taken off after 1 hour. Participants were administered fluoxetine 20 mg per day in the morning (trade names: fluoxetine; common name: fluoxetine hydrochloride capsule, produced by the Eli Lilly Company (Suzhou) of the United States; specification: 20 mg for each pill) for a total of 6 weeks. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Participants were administered fluoxetine 20 mg per day in the morning (trade names: fluoxetine; common name: fluoxetine hydrochloride capsule, produced by the Eli Lilly Company (Suzhou) of the United States, specification: 20 mg for each pill) for a total of 6 weeks. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Symptom severity reduction rate and remission |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and study personnel were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment was blinded. HAMD scores of participants were assessed by 2 separate doctors in psychology who were blinded from grouping information; they were required to reach consistency at a level of at least 98%. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, with similar reasons provided for missing data across groups; 5 cases of attrition. 3 in control: 1 quit owing to dizziness and postural hypotension occurring after 2 weeks of treatment, another owing to panic and pyknosphygmia detected by EKG after 4 weeks of treatment, and the third for dysuria. Two in the EA group quit. The condition of 1 participant deteriorated and participant was hospitalised for combined therapy owing to the death of his mother; the other quit because of a heart attack. Statistical analysis was not performed for these 5 individuals |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available. |
| Other bias | Unclear risk | Reporting in the manuscript was insufficient. |
Eich 2000.
| Methods | Randomised placebo‐controlled trial of acupuncture vs control acupuncture | |
| Participants |
Diagnosis: minor depression Method of diagnosis: ICD‐10 F32.0, 32.1 Age: unclear Participant information: 56 participants with depression Location: inpatient and outpatient clinic setting in Germany Inclusion/Exclusion: Exclusion criteria: compulsory detained, alcohol or drug intoxication, subcutaneous long‐acting medication taken in the previous 30 days, mania, bipolar disorder, schizophrenia, blood clot disorder, impaired wound healing, organic disease, seizures, pregnancy or breastfeeding, study participation in the past 30 days, knowledge of acupuncture |
|
| Interventions | Before the intervention was commenced, a 2‐week washout was undertaken. A total of 11 points was used for both groups. (1) Duration: 2 weeks (14 sessions) Frequency of treatment: daily Treatment protocol: Participants were administered body acupuncture via acupuncture points known from the literature to have a regulating effect. These included Du20 Baihui, Bl62 Shenmai, PC6 Naiguan, HT 7 Shenman, and EX‐HN1 Sishencong. (2) Duration: 2 weeks (14 sessions) Frequency of treatment: daily Treatment protocol: The control group used sham points at non‐specific points with minimal insertion, located on the hand, head, and foot. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Global Clinical Improvement Scale |
|
| Notes | Reported results may have been limited because data were presented for depression combined with general anxiety. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of the randomisation schedule were reported. |
| Allocation concealment (selection bias) | Unclear risk | No details of the randomisation schedule were reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blind to group allocation, and therapists were aware of group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blinded. It is unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | No differences in baseline characteristics were evident. The study appears free of other sources of bias. |
Fan 2005.
| Methods | Randomised controlled trial of acupuncture, medication (Prozac), and control acupuncture | |
| Participants |
Diagnosis: depressive neurosis Method of diagnosis: CCMD‐2 Age: 18 to 65 years Participant information: 81 participants Location: Guangdong Hospital, Guangdong, China Inclusion/Exclusion: Inclusion criteria: needed not to have taken medication in the previous 2 weeks Exclusion criteria: liver, kidney, blood, gastrointestinal disorders; infectious diseases; current pregnancy or breastfeeding |
|
| Interventions |
(1) Duration: 3 months Frequency of treatment: unclear Treatment protocol: Acupuncture was administered to 4 acupuncture points, Baihi Du 20, M‐HN‐3 Yintang, 4 gates, ear seeds to auricular points liver and heart. These points were rotated between the left and right ear twice a week. Other points were retained for 30 minutes. (2) Duration: 3 months Frequency of treatment: daily Treatment protocol: The first control group received 20 mg of fluoxetine daily for 3 months. (3) Duration: 3 months Frequency of treatment: unclear Treatment protocol: The second control group received sham acupuncture at non‐acupuncture points; the ear points were administered. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | Randomisation was concealed by the use of opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind, and it is unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Four participants (5%) from the medication group withdrew from the study owing to side effects. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Reported information was insufficient for assessment of other sources of bias. |
Fan 2013.
| Methods | Randomised parallel controlled trial of acupuncture vs acupuncture with shallow needling vs acupuncture vs control | |
| Participants |
Diagnosis: depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 163 participants Location: outpatient at Guangdong Provincial Hospital of TCM, China Inclusion/Exclusion: Inclusion criteria: HAMD score < 20, meeting TCM criteria for stagnation of liver qi, qi depression transforming into fire, aged 18 to 70 years, not taking antidepressant medication in the past 2 weeks Exclusion criteria: organic somatic disease, e.g. psychosis, schizophrenia; HAMD score > 35; other TCM diagnostic criteria met; epilepsy; serious cerebro‐cardiovascular hepatic, renal gastrointestinal disease |
|
| Interventions |
(1) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Acupuncture delivered with the aim of soothing the liver and regulating the mind Acupuncture points: LI4 and LR3, GV20 and Yintang, GV29 Mode of stimulation: 0.35 mm × 25 mm needles, insertion 10 to 12 mm, even lifting, thrusting and rotating manipulation until arrival of de qi. Moxa on Bl17, Bl19, 5 cones/point interdermal needling Bl15, Bl18 (2) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Control group: non‐acupuncture points with invasive shallow needling 10 mm away from Li4, LR3, GV20 Gv29; shallow but same needling techniques Moxa 10 mm away from points; intradermal needles 10 mm away from points |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Symptom Checklist‐90 Adverse events Dropout from treatment |
|
| Notes | ITT not undertaken Groups 1 and 2 combined |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and some key study personnel were not blinded; non‐blinding of others was likely to introduce bias. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Patient‐reported outcomes were reported; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Six dropped out from acupuncture, 8 from shallow needling, 6 from control. Reasons for missing outcome data were unlikely to be related to true outcomes. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient, but no adverse events were reported. |
| Other bias | Unclear risk | No differences were evident between baseline characteristics. |
Feng 2011.
| Methods | Parallel randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: depression Method of diagnosis: SDS (Self‐rating Depression Scale) score > 50, Hamilton Depression Rating Scale (HAMD) score > 7, PSQI score ≥ 8 Age: 18 to 75 years Participant information: 80 participants Location: outpatient and inpatient ward of Traditional Chinese Medicine (TCM) Department or Acupuncture Department of Chinese PLA General Hospital, China, from October 2008 to October 2010 Inclusion/Exclusion: Inclusion criteria: no intellectual or mental disorders, ability to self‐judge the sleep condition and other common conditions, ability to accomplish the scale independently, expected survival time longer than 3 months Exclusion criteria: taking antidepressant drugs at the present time, Karnofsky score < 30 |
|
| Interventions |
(1) Duration: 30 days Frequency of treatment: daily Treatment protocol: In treatment group, participants were treated with acupuncture on the acupoints of Fenglong (ST 40), Yinlingquan (SP 9), Xuehai (SP 10), Sanyinjiao (SP 6), Yintang (EX‐HN3), Baihui (DU 20), Sishencong (EX‐HN1), Neiguan (PC 6), and Shenmen (TF 4). When needling, method of neutral supplementation and drainage was used. Participants were treated for 20 to 30 minutes, and the acupuncturist performed needling manipulation at intervals of 5 to 10 minutes. (2) Duration: 30 days Frequency of treatment: daily Treatment protocol: Participants in the control group received fluoxetine hydrochloride capsules (trade name: Prozac, produced by Patheon, in France) 20 mg per day. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: HAMD reduced rate (%) = (score before treatment - score after treatment)/score before treatment × 100% Cure rate (reduced rate > 75%), effective rate (reduced rate 50% to 75%), improved rate (reduced rate 25% to 49%), invalid rate (reduced rate < 25%) |
|
| Notes | ITT was not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding status was not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available and reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
Fu 2006.
| Methods | Three‐armed randomised controlled trial comparing acupuncture, medication, and control acupuncture for treatment of individuals with depression | |
| Participants |
Diagnosis: depression Method of diagnosis: CCMD‐2‐R Age: not stated Participant information: 201 participants were randomised into acupuncture group (n = 78), medication (Prozac) group (n = 82), and sham‐acupuncture group (n = 41). Location: outpatient, China Inclusion/Exclusion: Exclusion criteria: schizophrenia; physical diseases or organic diseases that can cause similar symptoms of depression; age > 65; severe cardiovascular, liver, kidney, haematopoietic system diseases; pregnancy; haematic disease; antidepressant drugs taken within the past 2 weeks |
|
| Interventions |
(1) Duration: 12 weeks (24 sessions) Frequency of treatment: twice per week Treatment protocol: TCM style of acupuncture. Acupoints used were Taichong (LR 3), Hegu (LI 4), Baihui (GV 20), Yintang (EX‐HN 3), to point Liver and Heart. For sham acupuncture group, punctured spots were those 0.5 cm to LR 3 and LI4 on the radial side, 0.5 cm to GV 20 on the left side, 0.5 cm to EX‐HN 3 on the left side. Manual acupuncture treatment lasted 30 minutes. (2) Duration: 12 weeks Frequency of treatment: daily Treatment protocol: Participants in medication group were ordered to take Prozac 20 mg/d, continuously for 12 weeks. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Self‐rating Depression Scale (SDS) |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Acupuncture and sham participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Details were insufficient; 28 were lost to follow‐up, but no details of group allocation were provided. |
| Selective reporting (reporting bias) | Unclear risk | Information presented was insufficient. |
| Other bias | Unclear risk | Information presented was insufficient. |
Fu 2008.
| Methods | Multi‐centred randomised controlled trial of acupuncture vs control acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: depression Method of diagnosis: CCMD‐2 and score > 20 on the HAMD Age: 18 to 65 years Participant information: 440 participants Location: mixed inpatients and outpatients from 4 different hospitals between October 2004 and December 2006, in China Inclusion/Exclusion: Inclusion criteria: conscious, no loss of speech, preserved intelligence, minimum primary education level, TCM diagnostic criteria of ‘yu bing’ depressive disease due to liver qi stagnation or qi stagnation causing fire, no antidepressant medication taken in the previous 2 weeks Exclusion criteria: schizophrenia; organic or somatic disease that can trigger depression; < 18 years or > 65 years of age; severe cardiovascular, neurological, liver, kidney, or blood function disease; pregnancy; non‐co‐operative during needling; not taking medication on time; antidepressants taken in the past 2 weeks |
|
| Interventions |
(1) Duration: 12 weeks (24 sessions) Frequency of treatment: twice per week Treatment protocol: Treatment group received acupuncture administered to LIV3 Taichong, LI 4 Hegu, DU 20 Baihui, and M‐HN‐3 Yin tang. The 4 gates were needled first, to a depth of 15 mm; the needle was stimulated by lifting twirling manipulation until de qi was obtained. Bai hui was needled at a 30º angle in a quick motion. Yintang was needled by pinching the skin, then inserting to a depth of 15 mm parallel to the skin surface. Baihui and Yintang were twirled until de qi was obtained. The needles were left in for 30 minutes. Two auricular acupuncture points were used ‐ liver and heart points. Ear press tacks were placed on points and secured with small strips of bandage. These points were left in for 3 days, then were repeated in alternate ears. (2) Duration: 12 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine 20 mg/d (Prozac capsule, manufactured by Eli Lilly and Company). These were taken orally once in the morning after meals for a total of 12 weeks. (3) Duration: 12 weeks (24 sessions) Frequency of treatment: twice per week Treatment protocol: The sham acupuncture group involved needling of points in the region of Taichong, Baihui, Yintang, but roughly 0.5 cun away from actual points. The needle was inserted and manipulated in the same way as for the acupuncture group. The auricular acupuncture points were used in the same way as in the active group. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Assessment of cure and marked effect > 75% change from baseline Reports of adverse events |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation allocation sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed with the use of opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of participants in acupuncture and sham groups was unclear, and no testing was reported. The therapist was not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind, and the blinding status of analysts was unclear. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | A total of 64 (15%) participants did not complete the trial. No further details were reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | High risk | Potential bias was evident with imbalance in characteristics at randomisation, including previous psychiatric medication use and history of psychiatric care, for which no adjustments were made in the analysis. |
Han 2002.
| Methods | Acupuncture vs standard medication (maprotiline) | |
| Participants |
Diagnosis: depression Method of diagnosis: ICD‐10 and score > 20 on the Hamilton Depression Rating Scale Age: 18 to 55 years Participant information: 66 men and women Location: outpatients from the Beijing University Mental Health Institute, China Inclusion/Exclusion: Exclusion criteria: none specified. |
|
| Interventions |
(1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture was administered for 45 minutes, 6 times a week, over 6 weeks, through unspecified numerous standardised points. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The medicated group received daily maprotiline at doses ranging from 75 to 250 mg for 6 weeks. |
|
| Outcomes |
Time points for assessment: baseline and 14, 28, and 42 days from trial entry Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Scale Ashberg Rating Scale for side effects |
|
| Notes | ITT was performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on how the allocation sequence was generated could be obtained from the trial author. |
| Allocation concealment (selection bias) | Unclear risk | No details on the method of concealment used could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The study participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blinded to the study group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up was obtained. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Baseline characteristics show no imbalance between groups. Intention‐to‐treat analysis was performed. The study appears free of other sources of bias. |
He 2005.
| Methods | Manual acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: Chinese Neuroscience Society diagnostic guidelines Age: not stated Participant information: 170 participants Location: inpatients from Zhongshan Chinese Medicine Hospital, China Inclusion/Exclusion: Exclusion criteria: serious heart, liver, kidney conditions; glaucoma |
|
| Interventions |
(1) Duration: 8 weeks (48 sessions) Frequency of treatment: 6/week Treatment protocol: The acupuncture intervention consisted of stimulation of the acupuncture points DU26 Ren Zhong, PC6 Neiguan, LIV3 Taichong, HT7 Shenmen, with xing nao kai qiao needling method, with dispersal and regulation of liver qi and calming shen. Additional acupuncture points were added according to the diagnosis. If liver stagnation, diagnosed points TH6 Zhi Gou, LIV 14 Qi men were added. Qi stagnation with stagnation fire, diagnosed points LIV 2 Xing Jian, GB43 Jai xi were used to clear liver and purge fire. Heart and spleen deficiency was diagnosed; points UB15 Xing Shu, UB20 Pi Shu, ST36 Zusanli, SP6 Sanyinjiao were used to strengthen the spleen and nourish the heart. If the spirit was depressed affecting shen, additional points ST36 Zusanli, SP6 Sanyinjiao, and tong li HT5 were used to nourish the heart and calm the shen. Ren zhong was needled towards the nose 5 fen deep using the pecking dispersing method. Zhigou and Neiguan were needled perpendicular 1 cun, via the lifting twirling dispersing method. Xing jian, Jaixi, and Taichong were needled perpendicular 0.5 cun via the twirling dispersing method. Tong li, Shenmen were needled perpendicular via the reinforcing‐reducing manipulation method. Qimen was needled perpendicular 1 cun with the twirling dispersing method. Xingshu and Pishu were needled towards the spine 1 cun, after de qi use of the twirling dispersing method. Zusanli and Sanyinjiao were needle perpendicular 1 cun via the lifting twirling reinforcing method. Needles were retained for 30 minutes. (2) Duration: 8 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine 20 mg/d, taken in the morning. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Rates of recovery reported as "cured" and "marked" effects |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation schedule was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No additional details could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The study participant and the therapist were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to study groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance at randomisation. The study appears free of other sources of bias. |
He 2007.
| Methods | Randomised controlled trial of acupuncture vs medication (amitriptyline) | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 256 participants Location: inpatients from The First Affiliated Hospital of Tianjin University of Chinese Medicine, China Inclusion/Exclusion: Inclusion criteria: dysphoria as the predominant symptom lasting a minimum of 2 weeks at the same time exhibiting at least 4 of the following symptoms: loss of interest, no feelings of pleasure; reduced concentration and feeling fatigued; slow psychomotor activity; low self‐evaluation or self‐blame or feelings of guilt; cognitive difficulties or self‐aware impairment of association; repetitive thoughts of suicide or inflicting injury to oneself; dyssomnia, e.g. insomnia, waking early, or oversleeping; reduction in appetite or obvious drop in body weight; hyposexuality Exclusion criteria: none stated |
|
| Interventions |
(1) Duration: 1 month (approximately 60 sessions) Frequency of treatment: twice daily Treatment protocol: Acupuncture points PC6 Neiguan, DU26 Shui guo, DU20 Baihui, M‐HN‐3 Yintang, SP6 Sanyinjiao were selected. Nei guan on both sides was needled perpendicular to a depth of 0.5 to 1 cun, manipulated via the lifting twirling dispersing method for 1 minute. For the first 3 days, needling of Shui guo was towards the mid of the nose to a depth of 5 fen, via the pecking manipulation method. After the first 3 days, Baihui and Yintang were used. Baihui was needled towards the posterior side, to a depth of 5 fen, by a quick twirling tonifying method for 1 minute. Yin tang was needled with the skin pinched, to a depth of 5 fen, via a quick twirling tonifying method, for 1 minute. Sanyinjiao was needled perpendicular to a depth of 0.5 to 1.2 cun by a lifting twirling tonifying method for 1 minute. Each needle was kept in for 20 minutes. (2) Duration: 1 month Frequency of treatment: daily Treatment protocol: The control group received amitriptyline. For the first day, amitriptyline 50 mg was taken orally at night. Subsequently, 1 tablet (25 mg per tablet) was added per day until 200 mg per day was reached. |
|
| Outcomes |
Time points for assessment: baseline and at 4 weeks Outcomes: Self‐rating Scale of Depression Hamilton Depression Rating Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No response was received from the trial author in reply to communication sent to request further information on randomisation. |
| Allocation concealment (selection bias) | Unclear risk | No response was received from the trial author in reply to communication sent to request further information on randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind to study groups. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The blinding status of assessing clinicians and analysts was unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported. All participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance at randomisation. The study appears free of other sources of bias. |
He 2012.
| Methods | Randomised trial of acupuncture or medication (fluoxetine) | |
| Participants |
Diagnosis: depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 80 participants Location: outpatient clinic of Rehabilitation Department at Fosan Shunde Jun’an Hospital, China, from August 2010 to June 2011 Inclusion/Exclusion: Inclusion criteria: aged 18 to 65 years, no schizophrenia; no history and family history of mental disorders. Exclusion criteria: family history of mental disorders; serious liver and kidney disease, heart failure, post‐schizophrenia depression, post‐cerebral apoplexy depression, post natal depression, depression related to the menopause. |
|
| Interventions |
(1) Duration: 6 weeks (45 sessions) Frequency of treatment: daily with a 2‐day interval every 15 days Treatment protocol: Acupuncture group received points: Bihui GV20, YinTang, Sanyinjaio SP6, Taichong LIV3, Neiguan PC6, and Hegu LI4. Acupuncture was given once per day; needles remained for 30 minutes. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control received fluoxetine once per day, 20 mg/time. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: HAMD Cured: reduced rate ≥ 75%; remarkably effective: reduced rate ≥ 50% and < 75%; improved: reduced rate ≥ 25% and < 50%; failed: reduced rate < 25% HAMD was classified into 7 categories of factor structures. Of them, a score < 8 indicated normal, in the range from 8 to 18 indicated mild depression, from 18 to 24 indicated moderate depression, and > 24 indicated serious depression. |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | High risk | Participants were divided into an acupuncture group (40 cases) and a western medicine group (40 cases). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Assessing clinicians undertook measurements by observation and communication, and therefore were unlikely to be blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Six cases: 2 in the acupuncture group, 4 in the control group |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
Huang 2013.
| Methods | 60 patients with depression were randomly assigned to the medication group (30 cases) and to the treatment plus medication group (30 cases). | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 60 men and women Location: inpatients in China Inclusion/Exclusion: Exclusion criteria: depression with psychotic symptoms and organic psychosis; depression caused by mental activity substance and non‐addiction substance; serious physical ailments, organic brain disorder, drug‐ and alcohol‐dependent individuals, and those with allergies |
|
| Interventions |
(1) Duration: 6 weeks (18 sessions) Frequency of treatment: once every other day, 3 out of 7 days Treatment protocol: Manual acupuncture was administered. Acupuncture points Baihui (GV 20), Yintang (EX‐HN 3), Fengfu (GV16), Dazhui (GV 14), Fengchi (GB 20), Neiguan (PC 6), and Sanyinjiao (SP 6) were administered. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control group: paroxetine hydrochloride 20 to 40 mg/d |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD), Self‐rating Depression Scale (SDS), Eisenberg Antidepressant Side Effects Scale (Asberg) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient details were reported. |
| Other bias | Unclear risk | Insufficient details were reported. |
Li 2004.
| Methods | Single‐blind randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: depression Method of diagnosis: CCMD‐3 and Hamilton Depression Rating Scale with score > 20 Age: not stated Participant information: 110 participants Location: inpatients at hospitals in the Tianjin District, China Inclusion/Exclusion: Exclusion criteria: a history of organic mental disorder; taking psychoactive drugs; schizophrenia and other mental disorders; any heart, liver, kidney, and glaucoma condition |
|
| Interventions |
(1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: The aim of treatment was to regulate mental activity and sooth the liver. Acupuncture points DU 20 Baihui, DU16 Fengfu, DU 26 Renzhong, M‐HN‐3 Yintang, M‐HN‐1 Shishengcong, LIV3 Taichong, and UB18 Ganshu were used. Baihui was needled towards anterior, until 1.67 to 2.66 cm of the needle was inserted. Fengfu was needled perpendicular to a depth of 1.67 to 3.33 cm. A reinforcing‐reducing method of needle manipulation was applied for 1 to 2 minutes. Renzhong was needled towards the nose to a depth of 1 to 1.67 cm via a twirling reducing needling method for 1 to 2 minutes. Shishengcong was needled towards Baihui 1.67 to 2.66 cm via twirling reinforcing method. Taichong was needled perpendicular to a depth of 1.67 to 3.33 cm, and Ganshu was needled to a depth of 1.67 to 2.66 cm and was stimulated via a twirling reducing method for 1 to 3 minutes. Needles were retained for 30 minutes each time. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The medication group received fluoxetine 20 mg/d, administered in the morning after meals. Details were not reported on the active control acupuncture group because this form of control did not meet eligibility criteria of the protocol. |
|
| Outcomes |
Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No details on concealment of the allocation were reported. No response was received from a letter sent to the trial author. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to the study group. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Seven (6.3%) participants dropped out of the trial. Acupuncture group ‐ 1 participant dropped out owing to work commitments. Second acupuncture group ‐ 1 participant was hospitalised owing to worsening of symptoms. Medication groups ‐ 5 participants dropped out owing to side effects of medication, high cost of treatment, and, in 1 case, for no stated reason. Participants were excluded from the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Group characteristics were similar at baseline. The study appears free of other sources of bias. |
Li 2007.
| Methods | Electro‐acupuncture vs standard medication (fluoxetine or paroxetine) | |
| Participants |
Diagnosis: mild, moderate, or severe depression Method of diagnosis: CCMD‐3, HAMD, BDI Age: not stated Participant information: 56 participants Location: inpatients at The First Teaching Hospital of Tianjin Traditional Chinese Medicine College, China Inclusion/Exclusion: Exclusion criteria: none specified |
|
| Interventions |
(1) Duration: variable ‐ from 2 to 6 weeks Frequency of treatment: daily Treatment protocol: Particpants were randomly allocated to receive electro‐acupuncture or fluoxetine or paroxetine (adequate dose defined). The following acupuncture points were used: GB20 Feng chi, Anmien, M‐HN‐1 Shishencong, M‐HN‐3 Yintang, DU20 Baihui, Ht 7 Shenmen, PC5 Jian Shi, LI4 Hegu, LIV3 Taichong, SP6 Sanyinjiao, GB40 Quixu, GB 8 Shuaigu, and ST36 Zhusanli. All needles were manipulated by a twirling method, with gentle insertion applied on Shenmen. Zhong wan used as a breathing purging method, and electro‐acupuncture was applied to Yintang and Baihui, with the level of stimulation determined by the participant. Needles were left in for 30 minutes, and participants were needled once a day. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received oral fluoxetine or paroxetine 20 mg once a day in the morning. |
|
| Outcomes |
Time points for assessment: 18 weeks Outcomes: Hamilton Depression Rating Scale Rates of recovery reported as "cured" and "marked" effects |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information could be obtained from the trial author on how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | The trial author did not respond to letters sent. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to the study group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported, and all participants were included in the analysis. |
| Selective reporting (reporting bias) | High risk | Data from the Hamilton Depression Rating Scale ‐ but not the Beck Depression Inventory ‐ were reported. |
| Other bias | Low risk | Data show no imbalance in participant characteristics at baseline. The study appears free of other sources of bias. |
Li 2008.
| Methods | Randomised controlled trial of TCM manual acupuncture (30 participants) vs control acupuncture (30 participants) via 'off channel' points | |
| Participants |
Diagnosis: depression Method of diagnosis: CCMD‐2‐R Age: not stated Participant information: 60 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: organic cause for depression including schizophrenia, psychosis, or reactive depression; epilepsy; cardiovascular, liver, kidney, circulatory, or gastrointestinal disorders; pregnancy or lactation; any ear infection or damage to the ear; long‐term use of benzodiazepines for insomnia |
|
| Interventions |
(1) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Verum acupuncture was performed at Taichong (LR3), Hegu (LI4), Baihui (GV20), and Yintang (EX‐HN3). Ear acupuncture was performed on liver and heart auricular points. Manual stimulation was used for all points and was retained for 30 minutes. (2) Duration: 12 weeks (24 sessions) Frequency of treatment: 2/week Treatment protocol: Sham acupuncture was performed at 'off channel' points, 1 cm to the side of LR3, LI4, GV20, and EX‐HN3, and was retained for 30 minutes. Ear acupuncture was performed on liver and heart auricular points. |
|
| Outcomes |
Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) "Cured" rate measured by HAMD reduction > 75% |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and key study personnel was ensured; it is unlikely that the blinding could have been broken. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Li 2011b.
| Methods | Acupuncture vs control acupuncture in a double‐blind controlled trial | |
| Participants |
Diagnosis: depression Method of diagnosis: DSM‐IV Age: not stated Participant information: 43 men and women (23 to acupuncture and 20 to sham acupuncture) Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: stroke patients with aphasia, language barrier, cognitive impairment, previous history of depression, needle phobia |
|
| Interventions | Both groups were able to continue taking fluoxetine. (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5 out of 7 days Treatment protocol: Acupuncture: TCM acupuncture. Each treatment lasted 30 minutes. Points Baihui (GV 20), Yintang (EX‐HN 3), Sishencong (EX‐HN 1), Taichong (LR 3), Shenmen (HT7), Neiguan (PC 6), Sanyinjiao (SP 6), Taixi (K 3), and Xinshu (BL 15) were administered. (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5 out of 7 days Treatment protocol: Sham acupuncture: applied to non‐acupoint points (5 mm lateral to acupoints) via shallow needling technique |
|
| Outcomes |
Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Asberg Antidepressant Side Effect Scale |
|
| Notes | ITT was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessing clinicians were blinded; it is unlikely that blinding would have been broken. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting of details was insufficient. |
| Other bias | Unclear risk | Reporting of details was insufficient. |
Lin 2012.
| Methods | Randomised controlled trial of medication, manual acupuncture plus medication, and electro‐acupuncture plus medication | |
| Participants |
Diagnosis: depression Method of diagnosis: ICD‐10 plus a score ≥ 17 on the Hamilton Depression Rating Scale Age: not stated Participant information: 102 men and women (34 cases allocated to each group) Location: China, unclear setting. Inclusion/Exclusion: Exclusion criteria: previous enrolment in other clinical studies within 4 weeks, currently using antidepressants or anxiolytics, suicidal behaviour, cognitive disorders, serious cerebrovascular disease, liver and kidney disease, pregnancy or lactation, inability to comply with research data requirements during intervention or follow‐up phases |
|
| Interventions | Both acupuncture groups received the medication. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: once every other day, 3 out of 7 days Treatment protocol: TCM‐style acupuncture was administered. Manual acupuncture to points Baihui (GV 20), Yintang (EX‐HN 3), Fengfu (GV16), Fengchi (GB 20), Dazhui (GV 14), Neiguan (PC 6), and Sanyinjiao (SP 6). Supplementary acupoints were combined according to syndrome differentiation. (2) Duration: 6 weeks (18 sessions) Frequency of treatment: once every other day, 3 out of 7 days Treatment protocol: Electro‐acupuncture stimulation to points Baihui (GV 20) and Yintang (EX‐HN 3) No other needling details were reported. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Medication group: Seroxat was prescribed for oral administration once per day. |
|
| Outcomes |
Time points for assessment: end of the intervention Outcomes: Clinical Global Impression Scale (CGI) Quality of life assessed by the WHOQOL |
|
| Notes | ITT was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10 participants dropped out, numbers were balanced across groups, reasons were not reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient to allow assessment. |
| Other bias | Unclear risk | Reporting was insufficient to allow assessment. |
Liu 2006.
| Methods | Randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R Age: not stated Participant information: 246 men and women (101 randomised to acupuncture, 145 randomised to control) Location: inpatient, China Inclusion/Exclusion: Exclusion criteria: dementia, deafness, cognitive disorders, communication disorders, family history of mental health disorders |
|
| Interventions |
(1) Duration: 6 weeks (30 sessions) Frequency of treatment: every other day, 5 out of 7 days Treatment protocol: TCM acupuncture was administered. Manual acupuncture to the following points: Sishengcong (EX‐HN1), Anmian (Extra 8), Neiguan (PC 6), Shenmen (H7), Zusanli (ST36), Sanyinjiao (SP 6), Taichong (Liv3), Zhaohai (K6), Shenmai (B 62) (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control group received medication: Prozac 20 mg/d for 6 weeks |
|
| Outcomes |
Time points for assessment: end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No other blinding was undertaken. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | None were reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Liu 2013a.
| Methods | Randomised controlled trial of acupuncture plus medication vs medication alone | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 17 Age: not stated Participant information: 90 men and women (45 in each group) Location: unclear, China Inclusion/Exclusion: Exclusion criteria: physical ailments, organic brain disorder, drug and alcohol addiction, pregnancy or lactation, serious adverse reactions and allergies to medication |
|
| Interventions |
(1) Duration: 4 weeks (14 sessions) Frequency of treatment: once every other day Treatment protocol: Treatment group comprised medication plus TCM‐style manual acupuncture to Baihui (GV20), Yintang (GV29), Shenting (Bl24), Sishencong (EX‐HN1), and Fengchi (GB20). Each session lasted 30 minutes. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Control group comprised SSRIs, with use of fluoxetine and paroxetine. |
|
| Outcomes |
Time points for assessment: end of 1st, 2nd, and 4th weeks of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) VAS for pain assessment Adverse events |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient for assessment. |
| Other bias | Unclear risk | Reporting was insufficient for assessment. |
Liu 2015.
| Methods | Randomised controlled trial comparing manual acupuncture with SSRI vs SSRI alone | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 90 male and female participants Location: inpatient setting in China Inclusion/Exclusion: Exclusion criteria: serious body disease, organic brain disease, alcohol or drug dependence, women in gestation or lactation period, inability to tolerate adverse drug reactions, allergic constitution, psychotic symptoms |
|
| Interventions |
(1) Duration: 4 weeks (14 sessions) Frequency of treatment: once every 2 days Treatment protocol: Manual acupuncture with an SSRI All participants received TCM‐style manual acupuncture for 30 minutes each session. Primary acupuncture points were Baihui (DU20), Yintang (EX‐HN3), Shenting (GV 24), Fengchi (G 20), Dazhui (GV 14), and Sishencong (EX‐HN 1). Supplementary acupoints were combined according to syndrome differentiation. All participants in group 1 also received SSRI treatment in the same fashion as the control group. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Control group: Participants randomly used 1 type of 5 medicines. Fluoxetine hydrochloride, first day 20 mg/d, other days 20 to 60 mg/d for 4 weeks Paroxetine hydrochloride, first day 20 mg/d, other days 20 to 60 mg/d for 4 weeks Citalopram hydrobromide, first day 20 mg/d, other days 20 to 60 mg/d for 4 weeks Sertraline hydrochloride, first day 20 mg/d, other days 50 to 200 mg/d for 4 weeks Fluvoxamine maleate, first day 20 mg/d, other days 50 to 300 mg/d for 4 weeks |
|
| Outcomes |
Time points for assessment: 1 week, 2 weeks, 4 weeks (end of treatment) Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ITT was not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was lacking. |
Luo 1985.
| Methods | Electro‐acupuncture vs amitriptyline | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: ≥ 20 on the Hamilton Depression Rating Scale Age: not stated Participant information: 47 men and women Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: not specified |
|
| Interventions |
(1) Duration: 5 weeks (30 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture: Two acupuncture points were stimulated: DU20 Baihui and M‐HN‐3 Yintang. Needles were stimulated via electro‐acupuncture. (2) Duration: 5 weeks Frequency of treatment: daily Treatment protocol: Medication (amitriptyline): initial dose 25 mg 3 times a day for 1 week; treatment dose then increased to average dose of 142 mg |
|
| Outcomes |
Time points for assessment: baseline and end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Chart Asberg Antidepressant Side Effect Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No details on randomisation were provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No other details were reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported; all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Baseline characteristics were similar between groups. The study appears free of other sources of bias. |
Luo 1988.
| Methods | Electro‐acupuncture vs amitriptyline | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: ≥ 20 on the Hamilton Depression Rating Scale Age: 32 to 64 years Participant information: 241 men and women Location: inpatients from 3 psychiatric hospitals in China Inclusion/Exclusion: Exclusion criteria: none specified |
|
| Interventions |
(1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture: Two acupuncture points were stimulated: DU20 Baihui and M‐HN‐3 Yintang. Needles were stimulated via electro‐acupuncture. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Medication (amitriptyline): initial dose 25 mg 3 times a day for 1 week; treatment dose then increased to 50 mg 3 times a day |
|
| Outcomes |
Time points for assessment: baseline and end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Chart Asberg Antidepressant Side Effect Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No details on randomisation were provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No other details were reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | It is unclear whether the study was free of other sources of bias. |
Luo 1998.
| Methods | Electro‐acupuncture plus placebo tablets vs amitriptyline versus electro‐acupuncture and amitriptyline | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: ≥ 20 on the Hamilton Depression Rating Scale Age: not stated Participant information: 29 men and women Location: closed ward at Beijing Medical University Hospital Inclusion/Exclusion: Inclusion criteria: drug free the week before start of the trial Exclusion criteria: none specified |
|
| Interventions |
(1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture group: Two acupuncture points were stimulated: DU20 Baihui and M‐HN‐3 Yintang. Needles were stimulated via electro‐acupuncture for 45 minutes; the current was 3 to 5 mA at a frequency of 2 Hz. (2) Duration: 6 weeks (36 sessions) Frequency of treatment: daily Treatment protocol: Amitriptyline group: Participants taking medication received an average dose of 161 mg per day. |
|
| Outcomes |
Time points for assessment: baseline and end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Chart Asberg Antidepressant Side Effect Scale |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on randomisation were provided. |
| Allocation concealment (selection bias) | Unclear risk | No details on randomisation were provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind to study groups; no other details were provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported; all participants were included in the analyses. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | It was unclear whether the study was free of other sources of bias. |
Lv 2015.
| Methods | Three‐armed randomised controlled trial comparing auricular acupuncture vs auricular acupuncture with TCM psychotherapy vs Deanxit | |
| Participants |
Diagnosis: depression after breast cancer surgery Method of diagnosis: CCMD‐3 and SDS score ≥ 53 Age: not stated Participant information: 90 participants Location: inpatient setting, China Inclusion/Exclusion: Exclusion criteria: patient major life events affected by mood change over recent 5 years; severe mental illness with self‐injury and recent suicidal behaviour; a history of alcohol or drug abuse within 3 months; severe heart, brain, vascular, liver, kidney, haematopoietic system diseases; breast cancer metastasis |
|
| Interventions |
(1) Duration: 4 weeks Frequency of treatment: unclear Treatment protocol: Auricular acupuncture with indwelling needles for 4 weeks. These were changed once a week, alternating between each ear. Each day, participants were instructed to press and stimulate the indwelling needles for 3 to 5 minutes each time, 3 to 5 times per day. Auricular points used were Xin (CO15), Shen (CO10), Gan (CO12), Shenmen (TF4), Pizhixia (AT4), and Neifenmi (CO18). In addition to auricular therapy, group 1 received a TCM emotion intervention, which was poorly described. (2) Duration: 4 weeks Frequency of treatment: unclear Treatment protocol: Group 2 received the same treatment as Group 1 without the additional emotion intervention. (3) Duration: 4 weeks Frequency of treatment: unclear Treatment protocol: Control group: Deanxit (flupentixol 0.5 mg and melitracen 10 mg): 1 tablet per day for 4 weeks Comparisons were made between group 2 and the control group. |
|
| Outcomes |
Time points for assessment: end of treatment and 4 weeks after end of treatment Outcomes: SDS score Cured rate based on changes in SDS score |
|
| Notes | ITT was not discussed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Patient‐reported outcomes were included; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was lacking. |
Ma 2011.
| Methods | Randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 60 participants (acupuncture ‐ 31, fluoxetine ‐ 29) Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: depression from an organic cause, "depression caused by mental activity substance" |
|
| Interventions |
(1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5 out of 7 days Treatment protocol: TCM‐style manual acupuncture was delivered for 30 minutes. Acupuncture points used on all participants included BL13, BL14, BL15, BL17, BL18, BL19, and BL20. LR3 and SP6 or HT7 and SP6 could be added based on TCM pattern differentiation. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine hydrochloride capsules, 20 mg per day for 6 weeks. |
|
| Outcomes |
Time points for assessment: 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Recovered vs not recovered based on Hamilton Depression Rating Scale Adverse event reporting |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reporting in the paper was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Ma 2012.
| Methods | Randomised controlled trial of paroxetine, verum acupuncture + paroxetine, and electroacupuncture + paroxetine | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: ICD‐10 and score ≥ 17 on the Hamilton Depression Rating Scale Age: 18 to 60 years Participant information: 157 participants (drug control (paroxetine, n = 48), verum acupuncture (verum acupuncture + paroxetine, n = 53), and electro‐acupuncture (electro‐acupuncture + paroxetine, n = 56)) Location: inpatient setting, China Inclusion/Exclusion: Exclusion criteria: bipolar depression, other clinical trial participation within last 4 weeks, taking or coming off antidepressant drugs, pregnant, lactating, planned suicide. |
|
| Interventions | The verum acupuncture and electro‐acupuncture groups were treated with paroxetine combined with acupuncture. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: every second day, 3/week Treatment protocol: Electro‐acupuncture group Baihui, Yintang, and bilateral Fengchi were stimulated with Han's acupoint nerve stimulator (LH202H; Beijing, China). The positive electrode of 1 set of electric wires was connected to Baihui, and the negative electrode was connected to Yintang; the other set of wires was connected to bilateral Fengchi, with positive and negative electrodes alternated between left and right sides at each treatment. A disperse‐dense wave ‐ 2/15 Hz ‐ was used, and the current was controlled within tolerance (skin micromovement). Each electro acupuncture lasted for 30 minutes. (2) Duration: 6 weeks (18 sessions) Frequency of treatment: every second day, 3/week Treatment protocol: Verum acupuncture group: The needle was left in place for 30 minutes at the other acupoints, with needling once after 15 minutes for 5 to 10 seconds. The principal points ‐ acupoints of co‐ordination, needles, acupuncture methods, and duration of treatment ‐ were the same as for both groups. Acupoints: Baihui and Yintang were the principal points; Fengfu (GV16), bilateral Fengchi (GB20), Dazhui (GV14), bilateral Neiguan (PC6), and bilateral Sanyinjiao (SP6) were the acupoints of co‐ordination, selected according to current data on acupoints for treatment of individuals with clinical depression. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Control: Participants in the drug control group were treated with paroxetine. The drug dose was 10 mg/d for the first 2 days, then 20 mg/d until the end of treatment, administered orally once per day after breakfast. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) WHOQOL Scale |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was performed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants was reported. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of assessing clinicians was reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Thirty participants withdrew from the study, leaving 127 cases (38 drug control, 45 verum acupuncture, and 44 electro‐acupuncture) in the final analysis. “Subjects who withdrew from the study were excluded”. “Treatment was terminated in subjects with poor compliance, who did not undergo acupuncture according to regulations, who experienced physiopathological changes, who was intolerant of or hypersensitive to paroxetine, who developed adverse effects or who may have become pregnant during the treatment". |
| Selective reporting (reporting bias) | Unclear risk | Insufficient details were reported. |
| Other bias | Unclear risk | Insufficient details were reported. |
MacPherson 2013.
| Methods | Randomised controlled 3‐arm parallel study of acupuncture plus usual care, counselling plus usual care, or usual care alone | |
| Participants |
Diagnosis: depression Method of diagnosis: Beck Depression Inventory scoring ≥ 20, diagnosed by the GP Age: over 18 years Participant information: 755 participants Location: community, United Kingdom Inclusion/Exclusion: Excluson criteria: receiving acupuncture or counselling at the time; terminal illness; significant learning disabilities; haemophilia; hepatitis; HIV; pregnancy; confounding psychiatric conditions (bipolar disorder, postpartum depression, adjustment disorder, psychosis, dementia, or personality disorder). Patients who had suffered a close personal bereavement or given birth during the previous 12 months were also excluded. |
|
| Interventions |
(1) Duration: 3 months (12 sessions) Frequency of treatment: approximately once per week Treatment protocol: Acupuncture: Traditional Chinese Medicine (TCM) style. On average, 13 needles were inserted per session (range 3 to 26). Average number of sessions per week, 0.74. Average number of weeks between sessions, 1.36. Average duration of session, 53 minutes (range 28 to 95 minutes). 246 different points were used. Common points were SP‐6, LIV‐3, ST‐36, and LI‐4, which were used within a course of treatment for 91%, 89%, 83%, and 74% of participants, respectively. Manual methods: tonifying (68%), reducing (43%), even method (55%). The response sought varied, most commonly, de qi by 96% of acupuncturists. Acupuncturist: British Acupuncture Council members, with more than 3 years' post‐qualification experience (2) Duration: 3 months Frequency of treatment: approximately once per week Treatment protocol: Counselling: Counseling will be provided by members of the British Association of Counseling and Psychotherapy, who used primarily a non‐directive approach. Counsellors will use empathy and advanced listening skills to help participants express feelings, clarify thoughts, and reframe difficulties, but they will not give advice or set homework. (3) Duration: 3 months Frequency of treatment: N/A Treatment protocol: Usual care: Usual GP care was available to all participants according to need. |
|
| Outcomes |
Time points for assessment: baseline and 3, 6, 9, and 12 months Outcomes: PHQ‐9 BDI‐II SF‐36 bodily pain subscale EQ‐5D Texted mood scores were collected weekly over the first 15 weeks. Medication and health service were used. |
|
| Notes | ITT was reported and performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation was provided by the York Trials Unit. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was performed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants was reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Patient‐reported outcomes were measured; therefore blinding was not applicable. Analysts were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed by appropriate methods. At 3 months, 3 withdrew from acupuncture, 21 from counselling, and 3 from usual care. |
| Selective reporting (reporting bias) | Low risk | Protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
Pei 2006.
| Methods | Randomised controlled trial of TCM‐style acupuncture vs medication (fluoxetine hydrochloride) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3‐R, HAMD score ≥ 18 Age: not stated Participant information: 120 participants (acupuncture ‐ 62, fluoxetine hydrochloride ‐ 58) Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: cardiovascular, liver, or kidney disease or falling sickness (as per Chinese translation); pregnancy or lactation; drug dependence; severe mental disorder |
|
| Interventions |
(1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: TCM‐style manual acupuncture was delivered for 30 minutes. Acupuncture points used on all participants were BL13, BL14, BL15, BL17, BL18, BL19,and BL20. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received fluoxetine hydrochloride capsules, 20 mg per day. |
|
| Outcomes |
Time points for assessment: baseline and 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Effectiveness rates based on changes in HAMD scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in paper was insufficient. |
| Other bias | Unclear risk | Reporting in paper was insufficient. |
Qiao 2007.
| Methods | Randomised controlled trial of manual acupuncture compared with fluoxetine (Prozac) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3 Age: not stated Participant information: 40 men and women Location: mixed inpatient and outpatient setting, China Inclusion/Exclusion: Exclusion criteria: none stated |
|
| Interventions |
(1) Duration: 60 sessions Frequency of treatment: unclear Treatment protocol: TCM acupuncture: Each session lasted 45 minutes. Manual acupuncture was administered with stimulation to points Baihui (GV20) and Shenmen (H7). Other auxiliary acupuncture points were used according to differentiation, although this was not stated. Method of stimulation included a technique of reinforcing deficiency and reducing excess. (1) Duration: unclear Frequency of treatment: daily Treatment protocol: Control: Prozac 20 mg/d over the course of the intervention |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ITT was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were reported, |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
Qu 2013.
| Methods | Randomsied controlled group of electro‐acupuncture, manual acupuncture, or medication (paroxetine) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: ICD‐10 diagnosis for depression with moderate to severe symptoms with score ≥ 17 on the Hamilton Depression Rating Scale Age: not stated Participant information: 160 participants Location: outpatient acupuncture clinic of Southern Medical University, First Affliated Hospital of Jinan University, and Guangdong 999 Brain Hospital, China Inclusion/Exclusion: Exclusion criteria: unstable medical condition; a history of brain injury or surgery; suicidal attempts or aggressive behaviour; a history of manic, hypomanic, or mixed episode illness; comorbidity with other neuropsychiatric disorders; a family history of mental illness; investigational drug treatment within the previous 6 months; a history of alcohol or drug abuse within the previous 12 months; pregnancy or lactation; current cognitive‐behavioural therapy or other behavioural therapies |
|
| Interventions | All groups received paroxetine. Acupuncture procedure was performed in the treatment room by experienced acupuncturists (JQC and GLL) who had received 5 years of undergraduate training in Chinese medicine and had practiced Chinese medicine over 3 years. To ensure consistency in the acupuncture procedure, acupuncturists attended a training workshop to establish the acupuncture protocol before the study began. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: Manual acupuncture: Manual manipulation was conducted and needling sensation was generally achieved within 2 minutes after the manipulation. After the needling sensation was achieved, needles were retained for 30 minutes and were manipulated once again during retaining to maintain needling sensation. Point selection: Baihui (GV20), Yintang (EXHN3), Fengfu (GV16), Dazhui (GV14), bilateral Fengchi (GB20), bilateral Neiguan (PC6), and bilateral Sanyinjiao (SP6) (2) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: Electro‐acupuncture: Electrical stimulation was delivered between Baihui (Du20) and Yintang (EX‐HN3) and bilateral Fengchi (GB20), with continuous waves at alternating low (2 Hz) and high (100 Hz) frequency via Han’s Acupuncture Nerve Stimulator (H.A.N.S., mode code: LH202H). Point selection: Baihui (GV20), Yintang (EXHN3), Fengfu (GV16), Dazhui (GV14), bilateral Fengchi (GB20), bilateral Neiguan (PC6), and bilateral Sanyinjiao (SP6) (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Paroxetine: The PRX dose was initiated at 10 mg/d and was escalated to 20 mg/d within 1 week based on individual participant response. The PRX dose would be further increased if psychiatrists believed that participants' symptoms were aggravated. The maximum dose was set at 40 mg/d. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) BDI Self‐reported depression Adverse events. |
|
| Notes | ITT was undertaken and reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Non‐sequential random numbers were generated in advance by a computer programme (SPSS version II). |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and acupuncturists were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The principal investigator, the data collector, and the analysts were blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data have been imputed by appropriate methods. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Reporting was insufficient. |
Quah‐Smith 2005.
| Methods | Single‐blind randomised controlled trial of laser acupuncture vs control laser acupuncture | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: clinical assessment of depression and BDI score of 12 to 30 Age: not stated Participant information: 30 men and women Location: community setting, Australia Inclusion/Exclusion: Exclusion criteria: chronic depression over 2 years; hypomania; psychosis or drug abuse; taking psychotropic drugs over the previous 3 months; pregnancy; a history of endocrine disorders; suicidal disorder |
|
| Interventions | Acupuncture was performed by a fellow of the Australian Medical Acupuncture College. A low‐level laser unit was used. A flick switch was installed ‐ numbered 1 and 2 by the manufacturer. The laser unit beeped and flashed for both groups. (1) Duration: 8 weeks (12 sessions) Frequency of treatment: twice weekly for first 4 weeks, then weekly Treatment protocol: Acupuncture treatment was administered on the basis of TCM diagnosis and was individualised and based on syndrome. Most common diagnosis pattern liver qi stagnation or liver qi deficiency. Treatment was individualised. Classical alarm points were used: Qi Men Liv 14 (on the right), CV14 Ju Que,15, HT 7 Shenmen, and LIV 8 Qu Quan Other points included Kd10 Yin Gu, LI4 Hegu, SP6 San Yin Jao, and GV20 Baihu. No co‐interventions were allowed. The laser was applied to each point for 5 seconds, delivering 0.5 J. Total delivered: 3 to 4 J per session (2) Duration: 8 weeks (12 sessions) Frequency of treatment: twice weekly for first 4 weeks, then weekly Treatment protocol: The control group received inactive laser. |
|
| Outcomes |
Time points for assessment: 4 and 8 weeks, with follow‐up BDI through a mail‐out at 12 and 20 weeks following randomisation Outcomes: BDI Hamilton Depression Rating Scale (HAMD) Adverse events questionnaire |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was generated from "lot drawing" based on equal numbers of red and green beans placed in a closed jar with a small hole in the lid. The research assistant randomly selected 1 bean to determine group allocation. |
| Allocation concealment (selection bias) | Low risk | Coding of group allocation was determined by a flip of the coin and was known only by the manufacturer until the data had been analysed. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and the acupuncturist were blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The research assistant and the analyst were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Four (13%) participants discontinued the intervention ‐ 2 in each group ‐ owing to illness, decreased mood, and relocation. One participant in the control group was lost to follow‐up. Data analysed: 14/16 treatment, 12/14 control |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalances at randomisation. The study had no other sources of bias. |
Quah‐Smith 2013.
| Methods | Randomised double‐blind RCT of laser acupuncture vs control laser | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV Age: 18 to 50 years Participant information: 47 participants Location: community setting, Sydney, Australia Inclusion/Exclusion: Inclusion criteria: need to be free of herbal medication and psychotropic drugs in the last 4 weeks. Exclusion criteria: duration of depression greater than 2 tears; a history of hypomania or mania, substance abuse disorders; known central nervous system lesions; known uncontrolled endocrine disorders; pregnancy or potential pregnancy; active suicidal tendencies. |
|
| Interventions | Both laser units had a concealed section with a flick switch numbered by the manufacturer as‘A’ and ‘B’ ‐ 1 of which was the placebo option, known only to the project manager (JAH) and the manufacturer. The control panel of the laser units beeped and a red light flashed when the laser probe button appeared on either A or B. Each unit was separately set up for placebo or laser options. (1) Duration: 8 weeks (12 sessions) Frequency of treatment: 2/week for 4 weeks, once a week for another 4 weeks Treatment protocol: Laser acupuncture: Laser acupuncture 100 Mw low‐intensity infrared (808 nm) units were produced and followed the Moxla protocol. The laser probe was fully in contact (perpendicular to the skin surface) to avoid scatter of the laser beam. Points used were LR14, CV14, LR8, HT7, and KI3. (2) Duration: 8 weeks (12 sessions) Frequency of treatment: 2/week for 4 weeks, once a week for another 4 weeks Treatment protocol: Control laser acupuncture: The placebo group received inactive laser. Points used were LR14, CV14, LR8, HT7, and KI3. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Remission defined as score ≤ 7 on HAMD or ≤ 5 on QIDS |
|
| Notes | ITT analysis was undertaken and reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Sealed and opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and key study personnel was ensured, and it is unlikely that the blinding could have been broken. Blinding of participants: The percentages of participants in the active group that offered guess ‘active’, ‘placebo’, and ‘unsure’ were 65.2%, 30.4%, and 4.3%. In the placebo group, corresponding percentages were 60.0%, 30.0%, and 10.0%. These differences between groups were not statistically significant. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessing clinicians and analysts were blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Three in the treatment group and 1 in the control group discontinued. Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups; plausible effect size (difference in means or standardised difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size. |
| Selective reporting (reporting bias) | Low risk | Study protocol was available. |
| Other bias | Unclear risk | Available information was insufficient for assessment. |
Roschke 2000.
| Methods | Single‐blind placebo‐controlled trial of medication vs acupuncture plus medication vs medication plus control acupuncture | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: DSM‐IV, score > 18 on the Hamilton Depression Rating Scale Age: 20 to 70 years Participant information: 70 participants Location: inpatient setting, Germany Inclusion/Exclusion: Exclusion criteria: suicidal behaviour, diagnosis of schizophrenia or bipolar affective disorder or delusions; coagulation disease; wound healing disease; emphysematous thorax; abnormal blood cell count; serious liver and kidney disease; epilepsy |
|
| Interventions | Up to 20 mg/d diazepam was allowed if required in all groups. (1) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Mianserin (90 to 120 mg/d) (2) Duration: 4 weeks Frequency of treatment: daily medication, 3/week acupuncture Treatment protocol: Mianserin (90 to 120 mg/d) plus verum acupuncture. A standardised acupuncture treatment was applied 3 times a week over 4 weeks. Points included were U.B.15, U.B.17, BL.18, H7, P6, St40, Sp5, Sp6, and Lu1. Needles were retained for 30 minutes. (3) Duration: 4 weeks Frequency of treatment: daily medication, 3/week acupuncture Treatment protocol: Mianserin (90 to 120 mg/d) plus control acupuncture |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Global Assessment Scale Melancholia Scale Clinical Global Impressions Scale Mean dosage of medication collected Self‐reported improvement |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on how the allocation sequence was generated could be obtained from the trial author. |
| Allocation concealment (selection bias) | Unclear risk | No details could be obtained from the trial author. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study participants may have been blinded. No data were provided to verify whether participants were blind to being allocated to acupuncture or placebo acupuncture. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind, and it is unclear whether the analyst was blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up were reported. All participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance in baseline characteristics between groups. The study appears free of other sources of bias. |
Shen 2005.
| Methods | Single‐blind randomised controlled trial of manual acupuncture vs medication (amitriptyline) | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: CCMD Age: not stated Participant information: 256 participants Location: inpatients from a hospital setting in Tian jin, China Inclusion/Exclusion: Exclusion criteria: impaired speech, impaired consciousness, history of organic metal illness |
|
| Interventions |
(1) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: The intervention of manual acupuncture points used points PC6 Nei guan, GV26 Shui guo, DU20 Baihui, M‐Hn‐3 Yintang, and SP6 Sanyinjiao. The form of needling stimulation was described as locating Neiguan on both sides, perpendicular insertion of the needle to a depth of 13 to 25 mm; the needles were manipulated with twirling lifting method for 1 minute. For the first 3 days, the acupuncture point Shui Gou was used, with needling towards the nose, via a pecking method of needle manipulation. The following 3 days, the acupuncture points Yintang and Baihui were stimulated. These points were needled towards the posterior side to a depth of 13 mm. Manipulation of the needle used the frequent twirling reinforcing method for 1 minute. Sanyinjiao was needled to a depth of 13 to 44 mm with a twirling reinforcing method for 1 minute. Needles were left in for 20 minutes. (1) Duration: 30 days Frequency of treatment: daily Treatment protocol: The control group received amitriptyline. A dose of 50 mg/d was taken orally at night; 3 days later, the dose was increased by 25 mg every day until a dose of 200 mg was administered. |
|
| Outcomes |
Time points for assessment: 8 weeks Outcomes: Improvement was assessed as cured, marked effect, improved, or no effect. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation sequence was computer generated. |
| Allocation concealment (selection bias) | Unclear risk | The trial author did not respond to a letter sent to request further details on trial methods. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and the therapist were not blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available. Data on study outcomes were reported; however the instrument used was unclear. |
| Other bias | Low risk | Baseline characteristics were similar. The study had no other major sources of bias. |
Sun 2010.
| Methods | Randomised controlled trial comparing 2 different types of electro‐acupuncture vs medication (fluoxetine hydrochloride) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐2, HAMD score ≥ 17 Age: not stated Participant information: 90 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: diagnosis of depression, with HAMD scores < 17; other serious primary diseases, such as heart disease, hepatic disease, renal disease, and haematopoietic system disease; psychiatric patients; pregnancy or lactation; non‐co‐operative patients; definitive diagnosis of infectious disease |
|
| Interventions |
(1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Group 1 received TCM‐style electro‐acupuncture. Acupuncture points used were Baihui (DU20) and Sanyinjiao (SP6). (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Group 2 also received TCM‐style electro‐acupuncture in a similar manner to group 1 but using Taichong (LR 3),Sanyinjiao (SP 6), Neiguan (PC 6), and Shenmen (HT 7). (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received Prozac (fluoxetine) 20 mg/d. |
|
| Outcomes |
Time points for assessment: 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Recovered vs not recovered scores calculated on the basis of changes in HAMD |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Sun 2013.
| Methods | Propective randomised controlled trial of acupuncture vs medication (fluoxetine) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: DSM‐IV via a standard clinical interview and score ≥ 20 on the Hamilton Depression Rating Scale Age: 18 to 70 years Participant information: 75 participants Location: outpatients in the Department of Acupuncture, Beijing Hospital of Traditional Chinese Medicine, China Inclusion/Exclusion: Exclusion criteria: psychiatric illness, mental retardation, alcohol or drug abuse, severe somatic illness, positive medical history for cerebral disease, obesity, history of infection, known autoimmune disease, electroconvulsive therapy, immunosuppressive agents or immunostimulants used within 6 months, pregnancy or breastfeeding |
|
| Interventions | Acupuncture interventions for treatment and control groups were manipulated by the same acupuncturists, who had 5 years of training in acupuncture and TCM and more than 2 years of clinical experience. For both groups 1 and 2, the needles at Baihui (DU20) and Zusanli (ST36) or of Taichong (LR3) and Sanyinjiao (SP6) were connected to an electro‐acupuncture apparatus (KWD‐808 II Acupuncture Stimulator; Great Wall brand, Shanghai, China), with a frequency of 3 Hz and continuous waves based on patient tolerance. EA was applied for 30 minutes at a time. (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Electro‐acupuncture at the acupoints of Baihui (DU20) and Zusanli (ST36) (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Electro‐acupuncture control group at the acupoints of Taichong (LR3), Sanyinjiao (SP6), Neiguan (PC6), and Shenmen (HT7) (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: Fluoxetine (20 mg/d) for 6 weeks |
|
| Outcomes |
Time points for assessment: 0 (baseline) and 2, 4, and 6 weeks after treatment Outcomes: Hamilton Depression Rating Scale (HAMD) Treatment response was defined as ≥ 50% reduction in HAMC score, and great improvement was defined as final HAMD score ≤ 15. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated list was used. |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes with information describing group allocation were transferred to another nurse, who was not involved in the study; these were sequentially numbered. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blind; no other details were provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No other details were provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 14 participants dropped out: 5 from the EA treatment group and 9 from the EA control group. Among the 5 dropouts from the EA treatment group, 4 had no reason for refusing to participate in the study, and 1 refused because she was scared of having blood drawn. Among 9 dropouts from the EA control group, 4 had no reason for refusing to participate in the study, and the other 5 refused owing to fear of drawing blood for testing. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Unclear risk | Reporting was insufficient. |
Sun 2015b.
| Methods | Randomised controlled trial examining effects of manual acupuncture plus medication (fluoxetine) vs medication alone for treatment of individuals with post‐stroke depression | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: CCMD‐3, HAMD ≥ 8 Age: not stated Participant information: 63 men and women Location: inpatient setting, China Inclusion/Exclusion: Exclusion criteria: serious disuse; aphasia; memory loss; impaired hearing or understanding or cognitive issues; cerebral hernia or severe heart, liver, kidney, or haematopoietic system disease; depression, anxiety, and a history of mental illness or suicidal disorder before stroke; taking all kinds of calming, psychotropic drugs; a history of alcohol dependence; obvious cognitive impairment by MMSE |
|
| Interventions |
(1) Duration: 4 weeks (24 sessions) Frequency of treatment: 6/week Treatment protocol: TCM‐style manual acupuncture for 40 minutes each session. Acupuncture points used were primary point: Baihui (DU20); Fengfu (DU16); Shenting (GV 24); Shuigou (DU26); Dazhui (DU14); and Shendao (DU11). Supplementary acupoints were combined according to syndrome differentiation. All participants in group 1 received the same medication as the control group. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: Control group: fluoxetine 20 mg/d for 4 weeks |
|
| Outcomes |
Time points for assessment: 2 weeks and at end of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) Cured rate based on HAMD scores |
|
| Notes | ITT was not mentioned. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number generator was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not stated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | High risk | Sample size calculation was lacking. |
Tang 2003.
| Methods | Randomised controlled trial comparing manual TCM acupuncture vs medication (Deanxit (Flupentixol + Melitracen)) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 20 Age: not stated Participant information: 41 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: not reported in the paper |
|
| Interventions |
(1) Duration: 20 days (20 sessions) Frequency of treatment: daily Treatment protocol: TCM‐style manual acupuncture was delivered for 20 minutes. Acupuncture points used were Baihui (GV20), Yintang (EX‐HN3), Taiyang (EX‐HN5), Shuaigu (GB8), Fengchi (GB20), Fengfu (GV16), Shuigou (DU26), Hegu (LI4), Neiguan (PC6), Quchi (LI11), Sanyinjiao (SP6), Taichong (LR3), and Zusanli (ST36). (2) Duration: 20 days Frequency of treatment: daily Treatment protocol: The medication control group received Deanxit (Flupentixol + Melitracen) 1 tablet twice per day for 10 days, then 1 tablet daily for another 10 days. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Cured rates also reported, but source of these unclear |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawing of lots was described. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Wang 2014.
| Methods | Randomised controlled trial comparing manual acupuncture plus medication (SSRI) vs an SSRI alone | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: ICD‐9, HAMD score ≥ 18 Age: not stated Participant information: 76 participants Location: inpatient department of medical psychology at Nanjing Brain Hospital between April and November 2006 Inclusion/Exclusion: Exclusion criteria: SSRI or acupuncture treatment for depression in the past 3 months; severe medical disease; a history of brain stroke or other mental health disorders; pregnancy or breastfeeding |
|
| Interventions | Both acupuncture and medication control groups received an SSRI ‐ fluoxetine (20 mg once per day), paroxetine (20 mg once per day), or duloxetine (40 mg twice daily). (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Acupuncture treatment: Acupuncture points used for all participants were GV24 (Shenting), GV20 (Baihui), GV14 (Dazhui), and GV4 (Mingmen). Additional points were used according (TCM) differentiation for depression with the 4 diagnostic methods including tongue and pulse once a week, and additional points were changed accordingly: Liver depression and Spleen deficiency, add LR3 (Taichong), SP9 (Yinlingquan); Liver Qi stagnation, add LR3, LR14 (Qimen); Heart and Spleen deficiency, add HT7 (Shenmen) and ST36 (Zusanli); Liver and Kidney Yin deficiency, add KI3 (Taixi) and LR3; Spleen and Kidney Yang deficiency, add CV4 and CV6. In addition, according to individual symptoms, extra points could be applied: insomnia and forgetfulness, add HT7 and An’mian (Ext); palpitations and chest tightness, add PC6 (Neiguan); constipation, add ST25 (Tianshu) and ST37 (Shangjuxu). After achieving de qi needling sensation, the Dao qi technique was used. Acupuncture was applied at the 4 key acupuncture points. This manipulation involved lifting‐thrusting and rotating the needle with light and smooth stimulation. The amplitude was 1 to 2 mm; the needle rotation angle was < 90°, and frequency was 60 to 100 times per minute for 1 to 2 minutes. GV14 and GV4 were needled in a sitting position, with 5 minutes of retention before the needles were removed. All acupuncture treatments were delivered by a senior acupuncturist (TW) with 15 years’ clinical experience and certified by the China Association of Acupuncture and Moxibustion. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The medication control group received the SSRI alone. |
|
| Outcomes |
Time points for assessment: 1, 2, 4, and 6 weeks after the start of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Low risk | Randomisation was conducted via sequentially numbered and sealed opaque envelopes, prepared in advance. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Healthcare staff, apart from the acupuncturist, were blinded to group allocation before each participant was enrolled. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All assessments were carried out by trained psychiatrists who were blinded to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | High risk | The study report fails to include results for a key outcome that would be expected to have been reported for such a study. |
| Other bias | Low risk | The study appears free of other sources of bias. |
Wang 2015.
| Methods | Randomised controlled trial comparing manual acupuncture vs psychological intervention and health education | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: SDS score between 50 and 70 Age: not stated Participant information: 44 participants Location: outpatient setting, China Inclusion/Exclusion: Exclusion criteria: severe heart, lung, liver, or kidney disease; osteoarthritis; rheumatoid arthritis; gouty arthritis; a cardiac pacemaker; stroke followed by haemorrhagic infarction, moyamoya disease, subarachnoid haemorrhage, cerebral haemorrhage, brain tumour, brain trauma, etc.; not completing the self‐rating depression scale; low compliance with treatment |
|
| Interventions |
(1) Duration: 8 weeks (16 sessions) Frequency of treatment: 2/week Treatment protocol: Group 1 received TCM‐style manual acupuncture and moxibustion. Treatment was given for 30 minutes per session. Acupuncture points used were Baihui (DU20); Shenting (GV 24); Sishencong (EX‐HN 1); Hegu (LI4); Zusanli (ST36); Taichong (LR3); Guanyuan(CV4); Zhongwan(CV12); and Shenque(CV8). Indirect moxibustion was used above Guanyuan (CV4); Zhongwan (CV12); and Shenque (CV8) for 5 minutes. (2) Duration: 8 weeks Frequency of treatment: unclear Treatment protocol: Group 2 was given unspecified health maintenance education and psychological intervention. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: SDS score |
|
| Notes | ITT was not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence was computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes were used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Patient‐reported outcomes were reported; therefore blinding was not applicable. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reporting was insufficient. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Low risk | The study appears free of other sources of bias. |
Wenbin 2002.
| Methods | Randomised controlled trial of acupuncture vs medication (fluoxetine hydrochloride) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R, HAMD score > 17 Age: 19 to 51 years Participant information: 62 participants with duration of depression ranging from 6 months to 6½ years Location: inpatient and outpatient departments of the Second Clinical Medical College of Guanzhou University of TCM, China Inclusion/Exclusion: Exclusion criteria: severe organic disease |
|
| Interventions |
(1) Duration: 8 weeks (56 sessions) Frequency of treatment: daily Treatment protocol: Acupuncture based on TCM syndrome differentiation. The main syndromes were Heart and Spleen deficiency, Spleen and Kidney Yang deficiency, and a disorder of the Chong and Ren meridians. The main acupuncture points were Hegu LI4, Taichong LR 3, Baihui GV 20, and Yintang EX‐HN‐3. Other adjunct points included Xinshu (Bl15) or Jueyinshu BL14 (implanted intradermal needle). Ear points were Xin (MA‐IC), Dannang (EX‐LE 6), and Ershenmen (MA‐TF 1) implanted ring headed thumbtack needle for insomnia. Shenmen HT7, Sanyinjiao (SP6) was added for Heart and Spleen deficiency. Shenmen (HT 7) and Qiuxu (GB 40) was used for timidity due to heart qi deficiency. Sanyinjiao (SP 6) was added for liver qi stagnation and spleen deficiency. Taixi (KI 3), Daling (PC7), and Yinbai (SP1) were used for a disturbance of the mind by accumulated phlegm. Gongsun (SP4) and Lieque (LU7) supplemented a disorder of the Chong and Ren meridians. Qi was obtained. Needles were retained for 30 minutes. (2) Duration: 8 weeks Frequency of treatment: daily Treatment protocol: The control group was administered fluoxetine hydrochloride 20 mg per day. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) A score of cured was defined as greater than 75% improvement. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated by the study statistician, who produced a computer‐generated list. |
| Allocation concealment (selection bias) | Unclear risk | No details on allocation were reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It was not feasible to blind participants and therapists. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details were provided on the blinding status of assessing clinicians and analysts. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up; all participants were analysed. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no imbalance in baseline characteristics. The study appears free of other sources of bias. |
Whiting 2008.
| Methods | Pilot randomised controlled trial of acupuncture vs control acupuncture | |
| Participants |
Diagnosis: mixed anxiety and depression Method of diagnosis: clinical interview schedule revised Age: > 18 years Participant information: 19 participants Location: 7 general practices in the UK Inclusion/Exclusion: Exclusion criteria: a history of substance abuse, brain damage, other psychiatric disorder preceding the onset of depression, in receipt of concurrent alternative treatment, talking therapy for repression, pharmacological treatments for more than 3 months in the past year |
|
| Interventions |
(1) Duration: 12 sessions Frequency of treatment: unclear Treatment protocol: Manual acupuncture: delivered by a TCM practitioner with 10 years' clinical experience. A formula of points plus 2 discretionary points was used. Choice of points and needle depth were individualised according to TCM principles and body mass of the participant. Needles were retained for 20 minutes. (2) Duration: 12 sessions Frequency of treatment: unclear Treatment protocol: The control group received sham acupuncture. Sham acupuncture involved actual shallow needling but at sites unrelated to depression. Points were reported on the Web appendix. No needle stimulation was provided, and de qi was avoided. Needles were retained for 20 minutes. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Beck Depression Inventory Rand 36‐Item Survey |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the randomisation sequence was generated. |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed via off‐site central randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and researchers were blind to group allocation. Participants were asked about their perception of the group to which they were allocated. Blinding was maintained. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind to group allocation. It is unclear whether analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Five (26%) participants did not complete all acupuncture sessions. Three (50%) participants in the sham group did not comply with treatment. Two participants in the sham group were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | High risk | Data show imbalances between groups at randomisation with regard to age and BDI. No other sources of bias are evident. |
Xiao 2014.
| Methods | Randomised controlled trial of TCM‐style manual acupuncture vs medication (paroxetine) | |
| Participants |
Diagnosis: breast cancer with comorbid depression Method of diagnosis: CCMD‐3, SDS score between 50 and 69 Age: not stated Participant information: 60 women Location: mixed inpatient and outpatient setting, China Inclusion/Exclusion: Exclusion criteria: pregnancy or breastfeeding, organic cause for depression such as schizophrenia, severe infection, or abuse of/dependence on psychoactive substances |
|
| Interventions |
(1) Duration: 8 weeks (40 sessions) Frequency of treatment: 5/week Treatment protocol: TCM‐style manual acupuncture was delivered for 30 minutes. Acupuncture points used included Taichong (LIV3), Hegu (LI4), and Baihui (DU20) with the even‐reinforcing method, and Zusanli (ST36) and Qihai (REN6) with the twirling reinforcing method. Auricular acupressure with Semen Vaccariae was also applied to liver, spleen, and endocrine points unilaterally, alternating sides every 4 days. (2) Duration: 8 weeks Frequency of treatment: daily Treatment protocol: The medication control group received paroxetine hydrochloride capsules, 20 mg per day. |
|
| Outcomes |
Time points for assessment: 4 and 8 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Reported effectiveness rates based on changes in HAMD scores |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Xiujuan 1994.
| Methods | Single‐blind randomised controlled trial of acupuncture vs medication (amitriptyline) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: Hamilton Depression Rating Scale (HAMD) Age: not stated Participant information: 41 participants Location: inpatient and outpatient clinics at Beijing Medical University, China Inclusion/Exclusion: Exclusion criteria: none reported |
|
| Interventions |
(1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Mixed manual acupuncture and electro‐acupuncture: Acupuncture points DU 24 Shenting, DU20 Baihui, DU14 Dazhui, DU12 Shenzhu, Conception Vessel 17 Shanzong, CV14 Juque Ren, GB 20 Fengchi, and PC6 Neiguan. Additional acupuncture points were used depending on the Chinese medical diagnosis. For stagnation of Liver Qi ST23 Taiyi, SP6 Sanyinjiao and LIV3 Taichong were used. For Stagnation of Liver Blood LI4 Hegu, LIV3 Taichong and SP10 Xuehai were used. For Spleen and Heart Deficiency, HT7 Shenmen, PC7 Daling, SP6 Sanyinjiao, and ST36 Zusanli were used. For Spleen and Kidney Yang Deficiency, KD3 Taixi, SP6 Sanyinjiao, ST36 Zusanli, and CV4 Guanyuan were used. Needles were inserted bilaterally and were stimulated manually, except for DU 24 and DU 20, which were stimulated by electro‐acupuncture (frequency 80 to 100/s). (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received 25 mg of amitriptyline on the first day; the dose was increased by 25 to 50 mg each day up to 150 mg. In the second week, the dose was adjusted according to response and side effects but ranged from 150 mg to 300 mg daily. |
|
| Outcomes |
Time points for assessment: weekly until the end of the intervention Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | It is unclear whether concealment of the randomisation schedule was adequate. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is unclear whether assessing clinicians and analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Follow‐up was complete; all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Unclear risk | Information was insufficient for judgement. |
Xu 2011.
| Methods | Randomised controlled trial comparing manual acupuncture and electro‐acupuncture in combination with medication (SSRI) vs SSRI alone | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score ≥ 17 Age: not stated Participant information: 75 participants Location: unclear setting, China Inclusion/Exclusion: Exclusion criteria: physical ailments, organic brain disorders, substance dependence, had taken hormones, nerve blockers or immunomodulating drugs in the past month |
|
| Interventions | All groups received an SSRI such as citalopram, paroxetine, or fluoxetine at the standard daily oral dose. (1) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: A manual TCM‐style acupuncture intervention was delivered for 30 minutes. Acupuncture points included Baihui (GV20), Yintang (EX‐HN3), Shenting (GV24), Fengchi (GB20), Dazhui (GV14), Shengdao (GV11), and Zhiyang (GV9). (2) Duration: 6 weeks (18 sessions) Frequency of treatment: 3/week Treatment protocol: The electro‐acupuncture intervention was identical to the manual acupuncture intervention except that electro‐acupuncture was performed between GV20 and EX‐HN‐3. (3) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control medication group received only the SSRI. |
|
| Outcomes |
Time points for assessment: 1, 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Reported effectiveness scores based on changes in HAMD |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study did not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Yan 2004.
| Methods | Single‐blind randomised controlled trial of electro‐acupuncture vs medication (amitriptyline) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD, HAMD score > 20 Age: not stated Participant information: 30 participants Location: inpatients at Anning Hospital, Tianjin, China Inclusion/Exclusion: Exclusion criteria: none reported |
|
| Interventions |
(1) Duration: 30 days (30 sessions) Frequency of treatment: daily Treatment protocol: Electro‐acupuncture: administered to 2 acupuncture points: DU20, Baihui, and M‐NH‐3 Yingtang. Needles were Inserted to a depth of 1 cun and were connected to the electro‐acupuncture machine, Model G605. A strong current was delivered to generate visible observation of muscle pulsation, with a threshold of frequency of 80 to 90 times/min. Needles were retained for 1 hour. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received amitriptyline. For the first week, 250 mg per day was administered, medication was taken 3 times a day according to severity and side effects reported by the participant, and dosage was adjusted accordingly. The. average dose was 130 mg a day (suboptimal dose). |
|
| Outcomes |
Time points for assessment: 6 weeks post trial entry Outcomes: Hamilton Depression Rating Scale (HAMD) Improvement in depression measured subjectively by reporting on the number of participants cured |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the randomisation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | No response was received from the trial author when further details of randomisation were requested. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessing clinicians were blind to group allocation; it is unclear whether analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported. All participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Groups were comparable at baseline. No other sources of bias were apparent. |
Yeung 2011b.
| Methods | Randomised controlled trial comparing electro‐acupuncture, minimal acupuncture, and control acupuncture | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV, HAMD score ≤ 18 Age: not stated Participant information: 78 Chinese participants recruited through referrals from psychiatrists and advertisements at the clinic Location: outpatient clinic of the Department of Psychiatry at Queen Mary Hospital, a regional teaching hospital in Hong Kong Inclusion/Exclusion: Inclusion criteria: (1) ethnic Chinese; (2) age 18 to 65 years; (3) chief complaint of insomnia; (4) previous diagnosis of MDD based on DSM‐IV criteria, as assessed by a clinician; (5) 17‐item Hamilton Depression Rating Scale (HAMD17) score ≤ 18 at screening and baseline; (6) taking the same antidepressants at a fixed dose for 12 weeks before baseline Exclusion criteria: (1) symptoms suggestive of specific sleep disorders, as assessed by the Insomnia Interview Schedule, a semistructured face‐to‐face interview; (2) significant risk of suicide; (3) previous diagnosis of schizophrenia, other psychotic disorders, bipolar disorder, or alcohol or substance use disorder; (4) pregnancy or breastfeeding, or woman of childbearing potential not using adequate contraception; (5) valvular heart defects or bleeding disorders or taking anticoagulant drugs; (6) infection or abscess close to the site of selected acupoints; (7) any serious physical illness; (8) taking Chinese herbal medicine or over‐the‐counter drugs intended for insomnia. Also, an apnoea‐hypopnoea index ≥ 10 or a periodic limb movement disorder index with arousal ≥ 15, as assessed by overnight polysomnography in a subgroup of participants who consented to the investigation |
|
| Interventions | Participants were advised to continue the same type and dosage of antidepressants throughout the study period. Sedatives, anxiolytics, and hypnotics could be continued during the study period, but dose escalation was disallowed. All acupuncture treatments were performed in a quiet treatment room by the same acupuncturist. (1) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Electroacupuncture group: needled for 30 minutes at Yintang (EX‐HN3) and Baihui (GV20), and bilateral Ear Shenmen, Sishencong (EX‐HN1), and Anmian (EX), with disposable acupuncture needles. De qi was achieved if possible. Needles were held in place with surgical tape or hair pins. Electro‐acupuncture was delivered via a constant‐current, 0.45‐ms square wave pulse at 4 Hz. (2) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Minimal acupuncture group: needled superficially at bilateral “Deltoideus” (in the middle of the line of insertion of Binao LI14 and acromion), “Forearm” (1 inch lateral to the middle point between Shaohai HE3 and Shenmen HE7), “Upper arm” (1 inch lateral to Tianfu LU3), and “Lower leg” (0.5 inch dorsal to Xuanzhong GB39) De qi was avoided during needling. Acupuncturist, setting, number of points needled, electrostimulation, treatment frequency, and duration of treatment were the same as in the electro‐acupuncture group. (3) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Placebo acupuncture group: treated at the same acupoints as the electro‐acupuncture group with placebo needles. Placebo needles were placed 1 inch beside the acupoints to avoid acupressure effect. The needles were then connected to the electric stimulator, but with zero frequency and amplitude. Treatment frequency and duration of treatment were the same as in the electro‐acupuncture group. |
|
| Outcomes |
Time points for assessment: 1 and 4 weeks post treatment Outcomes: Hamilton Depression Rating Scale (HAMD) Recorded changes in quality of life and adverse events from acupuncture |
|
| Notes | ITT analysis was used. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence was used. |
| Allocation concealment (selection bias) | Low risk | Central randomisation was used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were blinded to group allocation, but no data on the success of blinding were collected; therefore it is possible that blinding was not successful. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessment of depressive symptoms, past psychiatric history, and antidepressant treatment history was conducted by a clinician. Analysis of questionnaires, sleep diaries, and actigraphy results was conducted by independent investigators, who were blinded to participants' group allocation. The HAMD was administered by an experienced psychiatrist (KCT), who was blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups; 7 participants (9.0%) dropped out during the treatment period, and 3 participants (3.8%) withdrew from the study at 4‐week follow‐up. Data show no difference in attrition rates among groups at 1‐week and 4‐week follow‐up (P > 0.05; Fisher exact test). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no significant between‐group differences in sociodemographic and clinical features, nor in pharmacotherapy. |
Zhang 2003.
| Methods | Randomised trial of electro‐acupuncture or medication (amitriptyline) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐2, HAMD score > 20 Age: 12 to 50 years Participant information: 460 participants. The duration of depression ranged from 6 months to 4 years. Location: inpatients and outpatients from Sichuan Province, China Inclusion/Exclusion: Exclusion criteria: none reported |
|
| Interventions |
(1) Duration: 3 weeks (unclear) Frequency of treatment: 6/week Treatment protocol: Two primary groups of acupuncture points were administered to participants. First, Baihui DU20, Laogong PC8, and Yongquan KI 1. Other points included Shuugou DU26, Hegu LI 4, and Taichong LIV3. Additional combined points were administered. For participants with palpitations, insomnia, and vexation, Xinshu Bl15, Fengchi GB20, Neiguan PC6, and Shenmen HT7 were added. For participants with stomach ache, poor appetite, and abdominal distension, Zusanli ST36, Pishu BL20, and Weishu BL21 were added. The 2 groups of acupuncture points were used alternatively. Acupuncture needles were inserted to a depth 0.5 to 1.0 cun. An ML8804 electro‐acupuncture unit was applied with output of 50 to 100 Hz, wave width 200 micros, and a current of 2 to 3 mA. The needles were stimulated until muscles trembled slightly, then were manipulated by a reinforcing‐reducing technique for 30 to 60 minutes. (2) Duration: 3 weeks Frequency of treatment: daily Treatment protocol: For the medication group, amitriptyline was given at 25 mg 3 times a day in the first week. Subsequent doses were modified after the first week, with an average dose of 150 mg per day administered over 3 weeks. All participants received psychological treatment for 3 weeks. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) The following outcomes were also described. Cured clinical symptoms disappeared with no sign of relapse after 2 to 3 weeks. Marked effect: Clinical symptoms were eased with occasional emotional fluctuation. Improvement: Clinical symptoms improved with some mental fluctuation. Failure: no improvement was seen. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details on the method of randomisation were reported. |
| Allocation concealment (selection bias) | Unclear risk | Details on randomisation were not confirmed by the trial author. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind to group allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It was unclear whether assessing clinicians and analysts were blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up was reported, and all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Groups were comparable at baseline. The study appears free of other sources of bias. |
Zhang 2005a.
| Methods | Randomised controlled trial of TCM‐style acupuncture vs medication (paroxetine) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R, HAMD score ≥ 17 Age: not stated Participant information: 86 participants Location: outpatient setting, China Inclusion/Exclusion: Exclusion criteria: depression due to organic causes |
|
| Interventions |
(1) Duration: 30 to 40 days (30 to 40 sessions) Frequency of treatment: daily Treatment protocol: TCM‐style manual acupuncture was delivered for 20 to 30 minutes. Acupuncture points included Baihui (GV20), Yintang (EX‐HN3), Shenmen (HT7), Neiguan (PC6), and Taichong (LR3). Other points were added on the basis of syndrome differentiation. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control medication group received paroxetine at 20 mg once per day for 6 weeks. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Reported effectiveness scores based on changes in HAMD |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number table was used. |
| Allocation concealment (selection bias) | Unclear risk | This was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No data were missing. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Zhang 2007.
| Methods | Single‐blind randomised controlled trial of electro‐acupuncture plus medication (paroxetine) vs medication for participants with clinical depression | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐3, HAMD score > 17 Age: not stated Participant information: 42 participants Location: inpatients at hospital in Hubei, China Inclusion/Exclusion: Exclusion criteria: previous suicide attempts, pregnancy or breastfeeding, dependence on drugs or alcohol |
|
| Interventions | Both groups received medication. (1) Duration: 6 weeks (36 sessions) Frequency of treatment: 6/week Treatment protocol: Electro‐acupuncture group: Dominant acupoints were Baihui (DU20) and Yintang (EXHN3). Bilateral auxiliary points were Neiguan (PC6), Waiguan (SJ5), Shenmen (HT7), Hegu (LI4), Taichong (LR3), Zusanli (ST36), Fenglong (ST40), Sanyinjiao(SP6), Taiyuan (LU9), etc. (sic). Needles were connected to the electro‐acupuncture machine ‐ type g6805 ‐ and needle stimulation was administered at 2 Hz frequency, with sparse‐dense wave, 6 volts, applied to produce stimulation within the participant's comfort level. EA was applied for 30 minutes. (2) Duration: 6 weeks Frequency of treatment: daily Treatment protocol: The control group received paroxetine 10 to 40 mg daily. |
|
| Outcomes |
Time points for assessment: 2, 4, and 6 weeks Outcomes: Hamilton Depression Rating Scale (HAMD) Side effects ratings |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | It is unclear how the randomisation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | It was not reported whether concealment of the allocation sequence was adequate. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is unclear whether assessing clinicians and analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up were reported. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | Data show no differences between groups at baseline. The study appears free of other sources of bias. |
Zhang 2007a.
| Methods | Randomised controlled trial comparing TCM‐style manual acupuncture vs medication (amitriptyline) | |
| Participants |
Diagnosis: clinical depression Method of diagnosis: CCMD‐2‐R, HAMD ≥ 20 Age: not stated Participant information: 100 participants Location: China, outpatient setting. Inclusion/Exclusion: Exclusion criteria: immune modulators or hormone preparations within the past 6 months, acute or chronic infection, trauma, recent inflammation or fever, known food or drug allergy |
|
| Interventions |
(1) Duration: 28 sessions Frequency of treatment: not stated Treatment protocol: TCM‐style manual acupuncture was delivered for 20 minutes. Acupuncture points used were Neiguan (PC6), Fengchi (GB20), Sanyinjiao (SP6), and Baihui (GV20). (2) Duration: not stated Frequency of treatment: daily Treatment protocol: The control medication group received amitriptyline 25 mg 3 times per day for 7 days. The dosage was then altered based on symptoms and adverse reactions. The average dosage was 150 mg per day. |
|
| Outcomes |
Time points for assessment: 2 and 4 weeks of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | High risk | An open allocation sequence was used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding was attempted. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding was attempted. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The study does not address this outcome. |
| Selective reporting (reporting bias) | Unclear risk | Reporting in the paper was insufficient. |
| Other bias | Unclear risk | Reporting in the paper was insufficient. |
Zhang 2009.
| Methods | Randomised controlled trial of acupuncture plus medication (fluoxetine) vs control acupuncture plus medication | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV, HAMD score > 14 Age: 18 and 60 years Participant information: 80 men and women Location: outpatient recruitment from psychiatric hospital and general hospital, China Inclusion/Exclusion: Exclusion criteria: acute suicidality; substance abuse or dependence; receiving electroconvulsive treatment; previous acupuncture experience; diagnosis of schizoaffective or bipolar affective disorder, coagulation disease, abnormal blood cell count, pregnancy, serious liver or kidney disease; epilepsy history |
|
| Interventions | Before administration of fluoxetine, a minimum 1‐week placebo washout was required, with 3 weeks for patients receiving monoamine oxidase inhibitors; then all patients were reevaluated, with HRSD as the baseline depressive score. Two licensed acupuncturists with 3 months of formal research training, in practice 3 to 5 years, delivered the intervention. Fluoxetine and placebo (sugar) tablets were identical in appearance and taste, and were administered as a morning dose. During the 6‐week randomised phase, the dose regimen guideline was 1 fluoxetine pill (10 mg) plus 1 placebo pill a day in group 1, or 2 fluoxetine pills (20 mg) a day in group 2, for the first 2 weeks, followed by 1 fluoxetine pill (10 mg) plus 2 placebo pills a day in group 1, or 3 fluoxetine pills (30 mg) a day in group 2, for the next 4 weeks. Zolpidem (up to 10 mg prn at bedtime) for insomnia was permitted during the trial. (1) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Acupuncture treatment based on TCM standardised protocol via published books/relevant literature: Acupuncture points were GV20, ExHN1 Sishencong, Yintang Ex HN3, GV26 Shuogou, PC6 Neiguan, H7 Shen men, Liv3, and LI4. 15 needles were inserted. Needle manipulation included manual reinforcing reducing, de qi with needling of each point retained for 30 minutes. (2) Duration: 6 weeks (30 sessions) Frequency of treatment: 5/week Treatment protocol: Sham: needled at non‐specific locations in the neighbourhood (1 to 3 cm, not recognised as true acupoints or meridians) of the loci cited above, merely pricking the skin superficially (1 to 4 mm deep). The same sham points were used during each treatment session. Shallow superficial insertion of the needle along with a minimum of needle sensation was emphasized. Minimum manual stimulation was applied to the needles. |
|
| Outcomes |
Time points for assessment: baseline and 2, 4, and 6 weeks of treatment Outcomes: Hamilton Depression Rating Scale (HAMD) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation schedule was based on severity of depression (HRSD score < 21 or ≥ 21). Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | These assignments were generated from a closed list of random numbers by a biostatistician not involved in conducting the trial, and were transmitted to a psychiatric nurse not otherwise involved in the clinical trial |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | All participants were informed that they would receive 2 indistinguishable but different‐style acupuncture treatments for depression. Although the 2 interventions were described to participants as ‘‘traditional acupuncture’’ or ‘‘non‐traditional acupuncture’’ on informed consent forms, participants were not told to which group they were assigned. For the sake of blinding, each participant was required to lie in bed completely relaxed, with eyes closed during the treatment process. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The treatment group was concealed from psychiatrists, other care providers, and research raters. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data were balanced between groups. Treatment: 1 physical disease, 1 lack of response. Sham: 1 given herbs, 2 lack of response, 1 arrhythmia. |
| Selective reporting (reporting bias) | Unclear risk | Reporting was insufficient. |
| Other bias | Low risk | No differences in baseline or power analysis were reported. |
Zhang 2012.
| Methods | Parallel RCT of acupuncture vs acupuncture control | |
| Participants |
Diagnosis: major depressive disorder Method of diagnosis: DSM‐IV, HAMD score > 18 and Clinical Global Impression‐Severity (CGI‐S) score > 4 Age: 25 to 65 years Participant information: 70 participants Location: outpatient setting, Hong Kong Inclusion/Exclusion: Exclusion criteria: (1) unstable medical conditions; (2) suicide attempts or aggressive behaviours; (3) history of manic, hypomanic, or mixed episode; (4) family history of bipolar or psychotic disorder; (5) a history of substance abuse within the previous 12 months; (6) investigational drug treatment in the previous 6 months; (7) current psychotropic treatment exceeding 1 week; (8) needle phobia |
|
| Interventions | Unmedicated participants in both groups received orally administered fluoxetine for 3 weeks in an open manner. The dose was initiated at 10 mg/d and was escalated to an optimal dose within 1 week on the basis of individual participants' responses, with a maximum dose of 40 mg/d. Those currently treated with fluoxetine for no longer than 1 week continued their medication at the same dose. Those currently treated with other psychotropic medications for no longer than 1 week were required to be switched to the fluoxetine regimen by gradual withdrawal of drugs within 1 week to wash out potential ‘‘carryover’’ effects. Concomitant use of other psychotropic drugs was not allowed. To ensure consistency in acupuncture procedures, the principal investigator (Z.J.Z.) provided a training workshop on the acupuncture protocol. Acupuncture intervention was performed by registered acupuncturists (W.W. and S.C.M.) who had received 5‐year undergraduate training in Chinese medicine and had practiced Chinese medicine over 3 years. (1) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Dense cranial electro‐acupuncture stimulation (DCEAS) is a novel stimulation mode by which electrical stimulation is delivered through dense acupoints located on the forehead mainly innervated by the trigeminal nerve, efficiently modulating multiple central transmitter systems via the trigeminal sensory‐brainstem NA and 5‐HT neuronal pathways. For DCEAS, the following 6 matches of forehead acupoints innervated by the trigeminal nerve via inserted or non‐inserted needles were used: Baihui (Du‐20) and Yintang (EXHN3), left Sishencong (EX‐HN1) and Toulinqi (GB15), right Sishencong (EX‐HN1) and Toulinqi (GB15), bilateral Shuaigu (GB8), bilateralTaiyang (EX‐HN5), and bilateral Touwei (ST8). Electrical stimulation was delivered to the 6 points. Electrical stimulation with continuous waves at 2 Hz and constant current and voltage (9 V) was delivered via an acupuncture stimulation instrument (Hwarto, SDZ‐II) for 30 minutes (pulse width could not be determined by this model instrument). Selection of this stimulation mode was based on the fact that low frequency could exert broader effects on central neurochemical systems compared with high frequency; this mode has been widely introduced into treatment for those with neuropsychiatric disorders. The intensity of stimulation was adjusted to a level at which participants felt most comfortable. (2) Duration: 3 weeks (9 sessions) Frequency of treatment: 3/week Treatment protocol: Non‐invasive electro‐acupuncture (n‐EA) control procedure with Streitberger’s non‐invasive needle was used. The needles with blunt tips were quickly put onto the same acupoints used in DCEAS without insertion into the skin. These needles were then affixed with plastic O‐rings and adhesive tapes. Electrical stimulation was delivered based on the same parameters as were used in DCEAS. Participants felt the stimulation via blunt tips touched on the skin. |
|
| Outcomes |
Time points for assessment: baseline and days 3, 7, 14, and 21 Outcomes: Hamilton Depression Rating Scale (HAMD) Clinical Global Impression Scale (CGI) Safety assessed by the TESS |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly assigned to n‐EA or DCEAS treatment at a ratio of 1:1, via a random block scheme from an automatic computer programme (SPSS version 2). |
| Allocation concealment (selection bias) | Unclear risk | Assignment was done in a single‐blind manner, by which random codes were known only by the acupuncturists. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The validity of the participant‐blind design was ensured by a sham acupuncture procedure performed at the forehead acupoints, which were outside the visual field of participants. To minimise expected effects, participants were not told during random assignment about potential responses to control and DCEAS procedures. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Raters were blind to treatment allocation; it is unclear whether analysts were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. Three withdrew from the control group ‐ 1 medical emergency, 1 loss to follow‐up, and 1 severe headache. Seven withdrew from treatment ‐ 2 losses to follow‐up, 3 medical emergencies, and 2 intolerance to acupuncture. |
| Selective reporting (reporting bias) | Low risk | The 3 primary measures from the protocol were reported. |
| Other bias | Low risk | The study appears free of other sources of bias. |
Zhuang 2004.
| Methods | Single‐blind randomised controlled trial of acupuncture plus massage vs medication | |
| Participants |
Diagnosis: post‐stroke depression Method of diagnosis: CCMD‐R, HAMD > 8 Age: not stated Participant information: 62 participants with post‐stroke depression for longer than 1 year Location: day patients and inpatients at the Guangzhou Hospital, China Inclusion/Exclusion: Exclusion criteria: serious cardiovascular disease, allergy to a sedative named “Dai an shen” containing flupentixol and melitracen |
|
| Interventions |
(1) Duration: 4 weeks (15 sessions) Frequency of treatment: every second day Treatment protocol: “ZhisanZhen” included a combination of points such as GB13 Ben Shen, DU24 Shenting, PC6 Neiguan, and SP4 Gongsun. The “Zhisanzhen” was needled with 25‐mm needles. PC6 was needled with 50‐mm needles, with deep needling. SP4 was needled towards SP3 Taibai, with de qi obtained and the sensation of qi sensation moving towards the chest. Needles were retained for 30 minutes. In addition, the group received finger point pressure and massage, which consisted of head massage, that is, massage on Tianmen points press Yingtang and stroke towards Shenting, repeated 5 times. Pressure was applied to acupuncture points DU20 Baihui, M‐NH‐3 Yingtang, DU26 Shuigou, and M‐HN‐9 Taiyang 5 times. Points GB20 Fengchi and DU16 Feng fu were pressed 3 times. Abdominal massage: In a circular clockwise motion, massage was applied to the abdomen 10 times. Pressure massage was applied to acupuncture points CV8 Shenque, CV4 Guanyuan, CV6 Qihai, and CV17 Shanzhong 3 to 5 times. Tendon separating pressure was applied to acupuncture points ST36 Zhusanli, SP6 Sanyinjiao 3 times. Massage via a kneading technique was applied to KD3 Taixi, LIV3 Taichong, SP6 Sanyinjiao, and PC6 Neiguan 3 times. Massage was applied once every second day for 15 treatments. (2) Duration: 4 weeks Frequency of treatment: daily Treatment protocol: The control group received medication consisting of Dai an shen (contains flupenthixol and melitracen). Two tablets were taken once a day in the morning for 1 month continuously. Note: Flupenthixol is a antipsychotic drug, and melitracen is a tricyclic antidepressant. |
|
| Outcomes |
Time points for assessment: end of intervention Outcomes: Hamilton Depression Rating Scale (HAMD) Data on participants cured, or showing a marked effect |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random table was used to generate the allocation sequence. |
| Allocation concealment (selection bias) | Unclear risk | No response was received from the trial author when further details of randomisation were requested. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and therapists were not blind. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | It is unclear whether assessing clinicians and analysts were blind to study group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition or exclusions were reported; no data are missing; all participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available. |
| Other bias | Low risk | The study appears free of other sources of bias. |
BDI: Beck Depression Inventory.
CCMD: Chinese Classification of Mental DIsorders.
CGI: Clinical Global Impression Scale.
CGI‐S: Clinical Global Impression‐Severity Scale.
CHM: Chinese herbal medicine.
CNS: central nervous system.
DCEAS: dense cranial electro‐acupuncture stimulation.
DSM: Diagnostic and Statistical Manual of Mental Disorders.
EA: electro‐acupuncture.
EQ‐5D: EuroQoL quality of life questionnaire based on five dimensions.
GP: general practitioner.
HAMD: Hamilton Depression Rating Scale.
ICD: International Statistical Classification of Diseases and Related Health Problems.
ITT: intention‐to‐treat.
MDD: major depressive disorder.
MMSE: Mini‐Mental State Examination.
N/A: not applicable.
NCCAOM: National Certification Commission for Acupuncture and Oriental Medicine.
n‐EA: non‐invasive electro‐acupuncture.
PHQ: Patient Health Questionnaire.
QIDS: Quick Inventory for Depression Self Reporting.
RCT: randomised controlled trial.
SCID: Structured Clinical Interview for DSM.
SCL‐90: Symptom Checklist‐90.
SDS: Self‐rating Depression Scale.
SF‐36: Short Form Health Survey.
SPSS: Statistical Package for the Social Sciences.
SSRI: selective serotonin reuptake inhibitor.
TCM: Traditional Chinese Medicine.
TESS: Toxic Exposure Surveillance System.
UPMC: University of Pittsburgh Medical Center.
VAS: visual analogue scale.
WHOQOL: World Health Organization quality of life questionnaire.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agelink 2003 | This trial of depression and anxiety aimed to evaluate the effect of acupuncture on cardiac autonomic nervous system function. Thirty‐six participants were randomly allocated to acupuncture or control sham acupuncture. No clinically meaningful data were reported. Data on cardiovascular outcomes (e.g. heart rate variability) were reported. |
| Arvidsdotter 2014 | Inability to confirm clinical diagnosis of depression |
| Bennett 1997 | Clinical diagnosis of depression not made |
| Bergmann 2014 | Clinical diagnosis of depression not made |
| Bin 2007 | Inability to confirm clinical diagnosis |
| Carvalho 2013 | Clinical diagnosis of depression not made |
| Chang 2009 | Inability to establish clinical diagnosis of depression |
| Chang 2010 | Study intervention involved use of TENS stimulation. |
| Chang‐du 1994 | In this trial of acupuncture, participants had experienced a stroke and reported post‐stroke depression. Depression was diagnosed as per our protocol and did not meet trial criteria. Details on randomisation could not be confirmed. Participants were allocated into 3 groups: Xingnao acupuncture method, routine acupuncture plus medication (doxepin), and routine acupuncture. No other details were reported. The outcome measure was unclear. |
| Cocchi 1977 | Observational study |
| Deng 2013 | Clinical diagnosis of depression not made |
| Dormaemen 2011 | The intervention focussed primarily on reducing menopausal ‐ not depressive ‐ symptoms. |
| Duan 2009 | Duplicate publication of Duan 2011 |
| Fan 2015b | Duplicate publication of Fan 2013 |
| Gallagher 2002 | Study population, intervention, and outcomes are the same as those reported in Allen 1998. This study reported follow‐up data at 12 months for an earlier trial (Allen 1998). However data reported separately by group cannot be obtained. |
| Guo 2009 | Clinical diagnosis of depression not made |
| He 2007b | Sixty‐one participants from China were given a diagnosis of depression based on the CCMD. Participants were given acupuncture or Chinese herbal medicine. The control group was administered Chinese herbs that did not meet our definition of standard care. Details on randomisation were unclear. The outcome measure was assessed by the Hamilton Depression Rating Scale. |
| He 2011 | The comparator group did not meet inclusion criteria. |
| Hmwe 2015 | Clinical diagnosis of depression not made |
| Honda 2012 | Clinical diagnosis of depression not made |
| Hou 1996 | The intervention did not meet the inclusion criteria because electro‐acupuncture was compared with manual acupuncture. |
| Hu 2013 | The intervention did not meet the inclusion criteria because acupuncture and Chinese herbal medicine were combined. |
| Huang 2003 | Acupuncture plus electro‐acupuncture vs manual acupuncture did not meet inclusion criteria for comparator groups. |
| Huang 2004 | Eighty‐five participants with post‐stroke depression were recruited in China. Participants were allocated to acupuncture and point injection groups every second day for 12 days. The control group received amitriptyline 25 to 50 mg 2 to 3 times per day. Outcome assessment was based on the Hamilton Depression Rating Scale. The study evaluated point injection therapy with a parental solution of breviscapine, and this did not our criteria for inclusion. |
| Huang 2005 | Ninety inpatients from a hospital in China were recruited to the trial. Participants met DSM‐II‐R diagnostic criteria for depression and were randomly allocated to scalp acupuncture or routine acupuncture, administered 6 days a week for 6 weeks.The Hamilton Depression Rating Scale was used to measure outcomes. This study was excluded owing to use of acupuncture as the control. |
| Huo 2013 | Clinical diagnosis of depression not made |
| Khang 2002 | Participants quasi‐randomised by day of admission |
| Kim 2015 | Clinical diagnosis of depression not made |
| Li 2011 | Clinical diagnosis of depression not made |
| Liu 2013 | The intervention did not meet inclusion criteria because acupuncture and Chinese herbal medicine were combined. |
| Lu 2004 | Sixty‐six participants with a diagnosis of depression based on CCMD‐3. Participants were inpatients from a hospital in China and were randomised to acupuncture plus medication or medication only. Electro‐acupuncture was administered 5 times a week for 6 weeks. Details on the dose of medication were insufficient as reported in the manuscript. We were unable to confirm details despite extensive efforts to reach trial authors. Outcome assessment was based on the Hamilton Depression Rating Scale. |
| Man 2014 | Clinical diagnosis of depression not made |
| Mischoulon 2012 | Study not randomised |
| Niu 2006 | The intervention did not meet inclusion criteria because acupuncture and Chinese herbal medicine were combined. |
| Shi 2014 | The study compared tongue acupuncture vs body acupuncture. |
| Song 1999 | 142 participants with stroke and depression (score > 7 on HAMD). Intervention group received scalp acupuncture once a day for 30 days ‐ Prozac 0.5 mg administered once per day. Outcome measures were based on HAMD. A suboptimal dose of medication was administered in the control group ‐ 0.5 mg once a day. Clarification was sought from the trial author but no response was received after extensive efforts. |
| Sun 2012 | The intervention did not meet inclusion criteria because acupuncture and Chinese herbal medicine were combined. |
| Tang 2003b | Clinical diagnosis of depression not made |
| Tse 2010 | Clinical diagnosis of depression not made |
| Wang 2003 | Clinical diagnosis of depression not made |
| Wang 2004 | Participants had depression following a stroke, and depression was diagnosed by the Hamilton Depression Rating Scale. Participants in the intervention group received acupuncture 5 times a week for 4 weeks. Participants in the control group received diazepam 2.5 mg once a day, or clozapine 25 mg once a day, for 4 weeks. Neither medication was prescribed for the control group to treat depression. Outcomes were measured on the Hamilton Depression Rating Scale. |
| Wang 2005 | Thirty‐four participants were recruited as inpatients from a hospital in Malta. Diagnosis for depression did not meet our criteria. This study compared acupuncture vs standard medication for depression. Participants received electro‐acupuncture twice a week for 5 weeks. The control group received Deanxit; during the first 3 weeks, 2 tablets a day were given, and during the past 2 weeks, 1 tablet a day was given. No details on dosage are available. However, we were unable to confirm through correspondence with the trial author whether this was a randomised controlled trial. |
| Wang 2006 | Participants were quasi‐randomised via case number. |
| Wu 2010 | Clinical diagnosis of depression not made |
| Xie 2009 | Inability to establish method of randomisation despite efforts to contact trial author |
| Xie 2012 | The intervention did not meet inclusion criteria because acupuncture and blood letting were combined. |
| Yeung 2011 | This was a non‐randomised observational study. |
| Zhang 2004 | The intervention did not meet inclusion criteria because acupuncture and control acupuncture were combined. |
| Zhang 2004b | This was a non‐randomised study. |
| Zhao 2014 | Participants were quasi‐randomised ‐ allocated by case number. |
| Zhou 2007 | Participants had depression associated with menopause. This trial did not provide a clear definition and used the HAMD to classify depression. This study defined a subcategory of depression in post‐menopausal women ‐ a group not recognised in the West. The intervention consisted of acupuncture given once per day 6 days a week for 6 weeks. The control group received fluoxetine 20 mg once per day for 6 weeks. Outcomes were measure by the HAMD. |
| Zhou 2015 | The intervention did not meet the inclusion criteria because acupuncture and moxibustion were combined. |
CCMD: Chinese Classification of Mental Disorders.
DSM‐II‐R: Diagnostic and Statistical Manual of Mental Disorders, Second Edition, Revised.
HAMD: Hamilton Depression Rating Scale.
TENS: transcutaneous electrical nerve stimulation.
Characteristics of studies awaiting assessment [ordered by study ID]
Fu 2003.
| Methods | Randomised study of acupuncture vs fluoxetine |
| Participants | 62 participants with depression diagnosed by the CCMD‐2R |
| Interventions | Fluoxetine 20 mg daily for 8 weeks Acupuncture LV 3, LI 4, GV20, Yintang, with adjunctive points BL15, BL14, ear points, HT7, GB 40, once daily twice a week |
| Outcomes | Recovery HAMD > 75% |
| Notes | Awaiting response from trial authors on details of randomisation |
Guo 2012.
| Methods | Acupuncture plus paroxetine vs medication only |
| Participants | 72 inpatients and outpatients with major depression |
| Interventions | Acupuncture plus paroxetine, electro‐acupuncture, and paroxetine vs paroxetine only |
| Outcomes | HAMD, SDS |
| Notes | Paper presented at conference, manuscript in preparation |
Guo 2015.
| Methods | Evaluation of therapeutic effects of early interventions and comparison of advantages of electro‐acupuncture (EA), cognitive‐behaviour therapy (CBT), and their combination in ameliorating depressive symptoms |
| Participants | 33 patients in depressive status included via the Hamilton Depression Rating Scale‐17 (HAMD‐17) and the Mini International Neuropsychiatric Interview (MINI) |
| Interventions | Electro‐acupuncture vs cognitive‐behavioural therapy (CBT) vs a combination of CBT and electro‐acupuncture vs observation only |
| Outcomes | HAMD |
| Notes | Conference paper (ICCMR 2015). Manuscript requested from trial author |
Haiyan 2004.
| Methods | Investigation of the change in signal transduction system among patients with major depressive disorder and the effect on signal transduction of electro‐acupuncture for treatment of individuals with depression |
| Participants | Patients with DSM‐IV or ICD‐10 major depressive disorder (MDD) recruited |
| Interventions | Under a double‐blind, acupuncture‐controlled, randomised pattern, participants were divided into 3 groups and were given different treatments for 6 weeks: electro‐acupuncture (n = 20), fluoxetine (n = 21), and needle punching (n = 21). |
| Outcomes | For each participant, blood samples were collected before and after treatment. |
| Notes | Unable to establish details of randomisation and any other outcome measures assessed |
Han 2002b.
| Methods | Randomised study of the effect of electrical acupuncture on serum cytokines in depressive patients |
| Participants | 61 patients with depression, 30 healthy controls |
| Interventions | Electro‐acupuncture, medication |
| Outcomes | Depression, anxiety, IL‐6, IL‐1ß, TNF‐alpha |
| Notes | Unable to determine method of randomisation and details of clinical diagnosis |
Han 2006.
| Methods | Randomised trial of electro‐acupuncture compared with medication (no details on randomisation reported) |
| Participants | 61 participants with depression meeting criteria for ICD‐10 |
| Interventions | Electro‐acupuncture 6 sessions per week for 6 weeks, or 174 mg of medication per day |
| Outcomes | Hamilton Depression Rating Scale, self‐rating scale for depression, self‐rating scale for anxiety, Clinical Global Impression scale |
| Notes | Wrote to trial authors seeking clarification of randomisation |
Li 2003.
| Methods | Randomised controlled trial of acupuncture vs fluoxetine |
| Participants | 69 patients with depression diagnosed by CCMD‐2‐R |
| Interventions | Manual acupuncture plus fluoxetine vs fluoxetine |
| Outcomes | Hamilton Depression Rating Scale (HAMD) and CGI used to evaluate efficacy |
| Notes | Unable to establish method of randomisation |
Lin 2004.
| Methods | Acupuncture vs medication |
| Participants | Patients with diagnosis of depression based on CCMD‐3 |
| Interventions | Manual acupuncture plus paroxetine vs paroxetine |
| Outcomes | HAMD scores |
| Notes | Unable to establish whether the trial was randomised |
Lin 2005.
| Methods | Acupuncture compared with medication, parallel design |
| Participants | 53 patients with depression diagnosed by CCMD‐3 |
| Interventions | Manual acupuncture vs paroxetine |
| Outcomes | HAMD and adverse events |
| Notes | Wrote to trial author seeking clarification of randomisation details |
Lu 2009.
| Methods | Controlled trial of electro‐acupuncture vs fluoxetine |
| Participants | 41 participants met diagnostic criteria for depression according to the Chinese Classification and Diagnostic Criteria for Mental Diseases, and scored > 17 on the Hamilton Depression Rating Scale. |
| Interventions | Electro‐acupuncture administered to points Baihui (GV 20), Shenting (GV 24), and Yintang (EX‐HN3). Additional points given based on Traditional Chinese Medicine diagnosis |
| Outcomes | Treatment Emergent Symptom Scale after 1 week, 2 weeks, 4 weeks, and 6 weeks of treatment |
| Notes | Unable to establish whether the trial was randomised |
Song 2007.
| Methods | Randomised controlled trial (RCT) divided into 3 groups treated with fluoxetine, EA, and control EA, respectively |
| Participants | 90 patients with MDD meeting DSM‐IV criteria |
| Interventions | Participants in the fluoxetine treatment group received 20 mg fluoxetine per day and sham EA (a needle punctured under the skin at the side of 1 cm far from Yintang, Baihui points without electrical current). Participants in the EA treatment group received the real EA (a needle punctured in the Yintang, Baihui point with electrical current of 10 to 40 mA) for 45 minutes in the morning of every weekday and 20 mg placebo. Sham EA treatment group received sham EA and 20 mg placebo. |
| Outcomes | HAMD |
| Notes | Wrote to trial author seeking clarification of randomisation details |
Song 2009.
| Methods | Depressed patients were randomly and blindly assigned to 3 groups of treatment: (1) EA and placebo capsules; (2) fluoxetine and control EA; or (3) control EA and placebo capsules. |
| Participants | 95 patients were recruited from outpatient clinics of the Beijing Mental Health Institute. Patients were assessed via the Structured Clinical Interview for DSM‐IV (SCID) and met DSM‐IV (Diagnostic and Statistical Manual of Mental Disorders) criteria for major depressive disorder. |
| Interventions | EA treatment was performed by placing needles at Bai Hui and at Yin Tang acupuncture points on the forehead. The acupuncture needles (0.30 mm × 33 mm) were then connected to an electro‐acupuncture machine with an antidepression sequence of waves for 45 minutes 3 times a week. Sham acupuncture was performed by placing the needles at non‐therapeutic points: 1 cm beside the Bai Hiu and Yin Tang acupoints. The needles were connected via the same EA machine that simulated the same oscillation waves as the active EA. The treatment procedure was the same as for the EA group. Fluoxetine (20 mg) or matched placebo capsules (supplied by Eli Lilly Pharmaceutical Company, USA) were taken after breakfast, 1 per day for 6 weeks. |
| Outcomes | Hamilton Depression Rating Scale (HAMD) 21 item scores (15) and Clinical Global Impression Scale (CGI) |
| Notes | Trial author did not confirm that the study was randomised. |
Sun 2015.
| Methods | Acupuncture vs Prozac vs acupuncture plus Prozac |
| Participants | 93 participants with post‐stroke depression |
| Interventions | Four‐week intervention |
| Outcomes | HAMD |
| Notes | Unable to confirm whether participants had received a clinical diagnosis of depression |
Vázquez 2011.
| Methods | Double‐blind control acupuncture vs real acupuncture clinical trial |
| Participants | Major depression as diagnosed by DSM‐IV. A total of 42 participants were recruited from the university primary care centre in Mexico. |
| Interventions | Electro‐acupuncture vs sham control |
| Outcomes | Carroll Rating Scale for Depression |
| Notes | Trial author did not confirm that the study was randomised. |
Zhang 1996.
| Methods | Control study of laser acupuncture vs medication. Method of randomisation unclear |
| Participants | 62 patients with depressive neurosis based on Chinese criteria of diagnosis |
| Interventions | Laser acupuncture or doxepin administered over 21 days |
| Outcomes | HAMD, CGI |
| Notes | Wrote to trial author seeking clarification of the method of randomisation |
Zhang 2005.
| Methods | Randomised trial with no details reported (divided into 2 groups) |
| Participants | 90 patients |
| Interventions | Acupuncture vs medication ‐ fluoxetine |
| Outcomes | HAMD scale |
| Notes | Contacted trial authors; no response received |
Zhao 2006.
| Methods | Acupuncture vs fluoxetine |
| Participants | 60 patients with HAMD score ≥ 20 |
| Interventions | Acupuncture administered once daily for 30 days. Fluoxetine administered 2 tablets for first 10 days, then 2 tablets for 20 days |
| Outcomes | HAMD scale |
| Notes | Unable to establish whether study was truly randomised |
CBT: cognitive‐behavioural therapy.
CCMD: Chinese Classification of Mental Disorders.
CGI: Clinical Global Impression Scale.
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
EA: electro‐acupuncture.
HAMD: Hamilton Depression Rating Scale.
ICCMR: International Congress of Complementary Medicine Research.
ICD‐10: International Statistical Classification of Diseases and Related Health Problems, Tenth Edition.
IL: interleukin.
MDD: major depressive disorder.
MINI: Mini International Neuropsychiatric Interview.
RCT: randomised controlled trial.
SCID: Structured Clinical Interview for DSM.
SDS: Self‐rating Depression Scale.
TNF: tumour necrosis factor.
Characteristics of ongoing studies [ordered by study ID]
Deng 2015.
| Trial name or title | Effect of acupuncture on the DMN of brain in patients with major depressive disorder: a resting‐state fMRI study |
| Methods | Case control study |
| Participants | 60 patients with depression as diagnosed by DSM‐IV. Patients are included if they are having their first depressive episode, are drug naive, are aged between 18 and 60 years, are right handed, and have an HAMD score ≥ 18 |
| Interventions | Acupuncture at Baihui (GV20) for 20 minutes |
| Outcomes | Activity in brain regions (ALFF, ReHo) |
| Starting date | January 2011 |
| Contact information | Study leader: Demao Deng (demaodeng@163.com) |
| Notes | Recruitment is complete. |
Fan 2015.
| Trial name or title | Clinical study of acupuncture for mild and moderate depressive episodes |
| Methods | Randomised controlled trial comparing a comprehensive intervention vs drug treatment |
| Participants | 200 patients aged 18 to 75 with diagnosis of mild to moderate depression according to CCMD‐3. Patients are excluded if they have an organic mental disorder or psychoactive substances and non‐addictive substance‐induced depression; are younger than 18 years of age or older than 75 years; cannot comprehend the meaning of self‐report of patients; are pregnant women; have epilepsy or serious disorders of the heart and brain blood vessels, liver, kidney, haematopoietic system, or gastrointestinal system; or cannot follow through with treatment. |
| Interventions | Comprehensive intervention programme plus placebo acupuncture Drug treatment plus sham acupuncture |
| Outcomes | Hamilton Depression Rating Scale, SF‐36 |
| Starting date | February 2015 |
| Contact information | Study leader: Ling Fan (546624680@qq.com) |
| Notes | Currently recruiting |
Fu 2011.
| Trial name or title | Clinical study on acupuncture treating insomnia with depression |
| Methods | Randomised controlled trial of 2 styles of acupuncture |
| Participants | 140 patients aged between 18 and 65 with depression diagnosed according to CCMD‐3 with a chief complaint of insomnia. HAMD scores between 20 and 35. Patients able to give informed consent. Patients are excluded if depression is a result of mental disease, active substances, or non‐addiction medicine, as are pregnant or lactating women; patients with serious heart, brain, or kidney disease or other major medical disorder; patients with cancer; and patients unable to co‐operate with their doctor |
| Interventions |
Conventional acupuncture treatment: Hegu (LI4), Tai Chong (LIV3), Yintang (EX‐HN‐3), Bai hui (GV20). Needles retained 30 minutes. While needles are inserted, patients are advised to take 6 deep breaths, then rest and repeat this every minute until the needles are removed. Optimised acupuncture treatment: Same as the conventional group but with Lie Qie (LU7) and Zhao Hai (KID6) added. Embedded needles (2 to 3 mm long) are used for 2 alternating groups of points: Xin Shu (BL‐15) and Shen Shu (Bl‐23) or Dan Shu (Bl19) and An Mian (N‐HN‐54). These embedded needles are retained until the start of subsequent treatment. |
| Outcomes | PSQI and HAMD are the primary outcome measures. |
| Starting date | September 2011 |
| Contact information | Trial leader: Wenbin Fu (drfwb63@21cn.com) |
| Notes |
Li 2015.
| Trial name or title | Acupuncture for ischemic post‐stroke depression |
| Methods | Multi‐centre, single‐blind, randomised controlled clinical trial in patients with ischaemic post‐stroke depression comparing verum acupuncture plus placebo medication vs control acupuncture plus true medication |
| Participants | 208 patients aged 45 to 80 years with a diagnosis of ischaemic stroke per International Classification of Diseases‐10 163 (ICD‐10 163: diagnosis of a major depressive episode according to the depression module of the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM‐IV), or the Chinese Classification and Diagnostic Criteria of Mental Disorders‐3 (CCMD‐3)). Onset of ischaemic post‐stroke depression is recent (< 6 months); patient is conscious, co‐operative, and without aphasia and has severe cognitive impairment; and has the capacity to provide written consent for both research assessment and treatment. |
| Interventions |
Experimental: Traditional acupuncture and placebo: Participants will be treated at Renzhong (Du26), Yintang (EX‐HN3), acupuncture Shangxing (DU23), penetrate to Baihui (DU20), Sishencong (EX‐HN1), Neiguan (PC6), Sibai (ST2), Fengchi (GB20), and Sanyinjiao (SP6) in bilateral; Jianyu (LI15), Quchi (LI11), Shousanli (LI10), Hegu (LI 4), Fengshi (GB31), Xuehai (SP10), Zusanli (ST36), and Taichong (LR 3) on the hemiplegia side. Another 6 groups use acupoints in bilateral. The acupuncturist will choose 1 group of acupoints according to the participant's syndrome: Zhigou (SJ6), Qimen (LR14), Xingjian (LR2), Xiaxi (GB43), Fenglong (ST40), Lianquan (RN23), Tongli (HT5), Xinshu (BL15), Xinshu (BL15), Pishu (BL20), Shenshu (BL23), and Taixi (KI3). Acupoints are inserted at a depth of 20 to 30 mm, except Renzhong (Du26), Sibai (ST2), and Sishencong (EX‐HN1), which are inserted at a depth of 5 to 10 mm. The needles will be left for 30 minutes and then removed. Acupuncture treatment will consist of 3 sessions per week for 12 consecutive weeks. Drug: placebo Placebo was given for 12 consecutive weeks. Sham‐acupoint acupuncture and fluoxetine: Participants will be treated at Jianliao (SJ14), Tianquan (PC2), Xiabai (LU4), Xiaoluo (SJ12), Shouwuli (LI13), Sidu (SJ9), Huizong (SJ7), Wenliu (LI7), Zhouliao (LI12), Quze (PC3), Kongzui (LI6), Zhigou (SJ6), Zhongzhu (SJ3), Futu (ST32), Jimen (SP11), Yinshi (ST33), Liangqiu (ST34), Shangjuxu (ST37), Xiajuxu (ST39), Xiyangguan (GB33), Ligou (LR5), Pucan (BL61), Jinggu (BL64), Rangu (KI2), Ligou (LR5), and Neiting (ST44) on the hemiplegia side. Acupoints are inserted at a depth of 20 to 30 mm, except Pucan (BL61), Jinggu (BL64), Rangu (KI2), and Neiting (ST44), which are inserted at a depth of 5 to 10 mm. The needles will be left for 30 minutes and then removed. Acupuncture treatment will consist of 3 sessions per week for 12 consecutive weeks. Drug: fluoxetine Fluoxetine was given at a dose of 20 mg/d for 12 consecutive weeks. |
| Outcomes | HAMD‐17 |
| Starting date | March 2016 |
| Contact information | Menghan Li, State Administration of Traditional Chinese Medicine of the People's Republic of China, The First Affiliated Hospital of Tianjin University of Traditional Chinese Medicine |
| Notes | Not yet recruiting |
Prater 2015.
| Trial name or title | Adjunctive treatment of major depression utilizing auricular acupuncture |
| Methods | Randomised, single‐blind study of 6 weeks' duration involving the use of auricular acupuncture or control acupuncture for adjunctive treatment of college students with depression |
| Participants | 40 college students presenting for care at Counseling and Psychological Services who meet Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM‐V) criteria for major depression single episode or recurrent will be included in the trial. Patients must have been symptomatic with depression for 2 months or longer or less than 18 months. Participants will be randomised into a sham auricular acupuncture group or a treatment acupuncture group. All patients who meet inclusion criteria will be treated with the selective serotonin reuptake inhibitor (SSRI) Lexapro 10 mg daily, which will be increased to 20 mg daily at week 2. Some participants will be treated twice weekly during their follow‐up visits with sham auricular acupuncture, others in the auricular acupuncture group will be treated with microcurrents of electricity. Trial duration will be 6 weeks. |
| Interventions |
Experimental: Auricular acupuncture + Lexipro: Participants will be treated with the SSRI Lexapro 10 mg daily, which will be increased to 20 mg daily at week 2. Participants in this group will be treated twice weekly during their follow‐up visits with microcurrents of electricity through auricular acupuncture. Sham comparator: Sham auricular acupuncture + Lexapro: Participants will be treated with the SSRI Lexapro 10 mg daily, which will be increased to 20 mg daily at week 2. Participants will be treated twice weekly during their follow‐up visits with sham auricular acupuncture (no microcurrent). |
| Outcomes | Change from baseline score of the Behavioral Health Measure‐20 through 6 weeks |
| Starting date | August 2015 |
| Contact information | Principal investigator: John Prater (jprater@fgcu.edu) |
| Notes | Currently recruiting |
Tai 2013.
| Trial name or title | Acupuncture based on five elements of body characteristics in the treatment of patients with post‐stroke depression |
| Methods | Randomised control trial comparing body acupuncture, 5‐element body acupuncture, and western medicine for post‐stroke depression |
| Participants | 150 patients aged 30 to 70 years who meet both Chinese medicine and conventional medicine diagnostic criteria for post‐stroke depression, who are able to understand and complete the depression scale, whose lesion is confirmed by head CT or MRI examination, and whose lesions are located in the anterior cerebral circulation |
| Interventions |
Observation group: 5 pedestrian body dialectical acupuncture Acupuncture group: conventional acupuncture Western medicine control group: no acupuncture |
| Outcomes | Changes in HAMD scale score |
| Starting date | July 2013 |
| Contact information | Study leader: Liu Tai (liutai590216@163.com) |
| Notes | Recruitment complete |
Wang 2014a.
| Trial name or title | Abdominal acupuncture on moderate and severe depression female patients: a randomised controlled blind clinical trial |
| Methods | Randomised controlled trial comparing a combination of acupuncture and fluoxetine vs another combination of acupuncture and fluoxetine |
| Participants | 40 female patients aged 23 to 60 years with depression, able to understand and read Chinese, with SDS < 53 or MADRE score > 14 |
| Interventions | Acupuncture and fluoxetine treatment group Acupuncture and fluoxetine control group |
| Outcomes | Self‐Rating Depression Scale (SDS), Montgomery‐Asberg Depression Rating Scale (MADRS) |
| Starting date | September 2014 |
| Contact information | Study leader: Xiaoyun Wang (jiaoshouw@163.com) |
| Notes | Currently recruiting |
Weidong 2015.
| Trial name or title | Clinical evaluation of depression treated by disease and syndrome combined method |
| Methods | Randomised parallel controlled trial comparing low‐resistance‐state thought induction psychotherapy vs cognitive‐behavioural therapy vs low‐resistance‐state thought induction psychotherapy and acupuncture and herbs |
| Participants | 225 patients aged 18 to 60 with depression diagnosed by SCID and HAMD score of 25 to 36, with education level higher than junior high school and no suicidal ideation. Patients would be excluded if they had schizophrenia and substance addiction; had organic brain disease or endocrine disease; were pregnant or lactating women; had had a manic attack; or had serious physical disease. |
| Interventions |
TIP group: low‐resistance‐state thought induction psychotherapy CBT group: cognitive‐behavioural treatment Comprehensive group: low‐resistance‐state thought induction psychotherapy and acupuncture and herbs |
| Outcomes | Hamilton Depression Rating Scale, Beck Depression Inventory |
| Starting date | May 2015 |
| Contact information | tcmtip@126.com |
| Notes | Recruitment pending |
Weidong 2016.
| Trial name or title | A clinical evaluation research for the treatment of major depression by integrated disease with Zheng of TCM method |
| Methods | Randomised parallel controlled trial of acupuncture, herbal medicine, and escitalopram vs escitalopram alone |
| Participants | 160 patients aged 18 to 45 with depression diagnosed in accordance with conventional disease diagnosis and TCM treatment in Shanghai (second edition) and DSM‐IV psychiatric diagnostic standard in the United States, and Hamilton Depression Rating Scale score ≥ 20 points, namely, the clinical‐severe type; who at least 1 week before treatment have not used antidepressant drugs (including western medicine and TCM) or other psychiatric drugs or have used them with cleaning at least 1 week; after 2 different types of antidepressants or at least more than 6 weeks, nearly 1 week is invalid, can maintain the original drug dosage into the group; has a cultural degree for junior high school above; available for the course of more than 2 weeks; right‐handed; has no contraindications to MRI scanning; with the approval of the hospital ethics committee, volunteer to participate in, and sign the informed consent. |
| Interventions | Acupuncture, liver depression resolving particles, and escitalopram vs escitalopram alone |
| Outcomes | HAMD |
| Starting date | April 2016 |
| Contact information | Study leader: Wang Weidong (prof_wwd@126.com) |
| Notes | Currently recruiting |
Wenben 2015.
| Trial name or title | Effectiveness and safety of electro‐acupuncture for mild to moderate perimenopausal depression |
| Methods | Randomised controlled trial to compare effects of electro‐acupuncture and escitalopram oxalate tablets on mild to moderate perimenopausal depression, and to evaluate the safety of electro‐acupuncture stimulation |
| Participants | 252 women aged 45 to 55 years, meeting the diagnostic standard of STRAW‐10 for perimenopause, conforming to the diagnostic standard of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5), for depression, and conforming to the diagnostic standard of the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD‐10) F32.0 (mild depression) or F32.1 (moderate depression), with HAMD‐17 score > 7 and < 23, with first episode of depression during the perimenopausal period, not on hormone replacement therapy (HRT), and taking no antidepressant 3 months before the study begins |
| Interventions |
Experimental: Electro‐acupuncture: Baihui, Yintang, Guanyuan (dual), Zigong (dual), Sanyinjiao (dual), Hegu (dual), and Taichong (dual). Insert needles to the acupoints mentioned above after sterilised. Needle handles of Baihui and Yintang are connected with the electro‐acupuncture instrument wire. Needle handles of bilateral Zigong are connected with the electro‐acupuncture instrument wire. Needle handles of bilateral Tianshu are connected with the electro‐acupuncture instrument wire. Density wave, frequency of 10/50 Hz, and current intensity of 0.5˜1.0 mA for 30 minutes. 3 times per week. Each treatment interval > 24 hours, continuous treatment for 12 weeks. Active comparator: escitalopram oxalate tablets 0.5 hour after breakfast, oral 10 mg escitalopram oxalate tablets, continuous treatment for 12 weeks |
| Outcomes | Change from baseline in scores of the 17‐item Hamilton Depression Rating Scale (HAMD‐17) at 4th week, 8th week, 12th week, 16th week, and 24th week |
| Starting date | September 2013 |
| Contact information | Study leader: Wenben Fu (fuwenbin@139.com) |
| Notes | Estimated completion: December 2015 |
Ya 2008.
| Trial name or title | The clinical study of the best treatment option in acupuncture on depression |
| Methods | Randomised controlled trial comparing manual acupuncture, electro‐acupuncture, and medication (paroxetine HCL) |
| Participants | 480 patients aged 18 to 60 with depression diagnosed by ICD‐10 (excluding bipolar disorder), HAMD score ≥ 17 who are able to give informed consent. Patients are excluded if they have joined another clinical examination within 4 weeks of starting the trial, are taking antidepressants, are pregnant or lactating women, have other serious diseases, have caught brain disease, or have suicidal ideation. |
| Interventions |
Manual acupuncture group: Baihui, Yintang, Fengfu, Fengchi, Da Zhui, Neiguan, Sanyinjiao Electro‐acupuncture group: Baihui, Yintang, Fengfu, Fengchi, Da Zhui, Neiguan, Sanyinjiao Medication control group: paroxetine HCL, 10 mg/d for the first 2 days, then 20 mg/d |
| Outcomes | SDS, HAMD, CGI |
| Starting date | October 2007 |
| Contact information | Study leader: Tu Ya (tuyab@263.net) |
| Notes | Recruitment complete |
Ya 2015.
| Trial name or title | The clinical curative effect of acupuncture treatment in depression |
| Methods | Randomised parallel controlled trial of electro‐acupuncture vs SSRI antidepressants |
| Participants | 80 patients aged 18 to 65 with mild and moderate depression as diagnosed by ICD‐10 and HAMD score ≥ 17 and ≤ 22, diagnosed for the first time, without current systemic treatment, with depression starting within the past 2 weeks to 1 year. Patients are excluded if 4 weeks before the start of this study they participated in other clinical trials; if they are taking or 2 weeks before the start of the study were taking antidepressant medication; if they have brain disease or abnormal judgement ability (Wechsler Adult Intelligence Scale < 90 points); if they have other serious diseases that need to be treated, have apparent suicide intent, or suffer from other mental disorders. |
| Interventions |
Electro‐acupuncture: Yintang and Baihui, Taichong, Neiguan, Zusanli, Shenmen, Sanyinjiao. Treatment 2 times a week, 30 minutes per session. Electro‐acupuncture frequency 20 Hz Medication: SSRIs, antidepressants including fluoxetine, paroxetine, fluvoxamine, sertraline, and citalopram. Dosage was based on physician advice. |
| Outcomes | fMRI; ACTH; CORT; IL‐6; TNF‐alpha; IL‐1; HAMD scale |
| Starting date | July 2015 |
| Contact information | Study leader: Tu Ya (tuyab@263.net) |
| Notes | Recruitment status unknown |
Yan 2012.
| Trial name or title | Comparison of treatment effect of Chinese medicine and western medicine on depression in China and America |
| Methods | Randomised controlled trial comparing Chinese medicine, acupuncture, traditional Chinese medicine psychology and physical treatment for treatment of individuals with depression |
| Participants | 160 patients aged 16 to 70 with depression diagnosed by ICD‐10 criteria; antidepressants and other psychiatric drugs were not taken 2 weeks before the trial, or the drugs above were used but have a cleaning period of 2 weeks; level of education is higher than junior middle school; course of disease is longer than 2 weeks, and informed consent is given. |
| Interventions |
Experimental: Chinese herb: Chinese herbs special for depression Experimental: Acupuncture: acupuncture at DU20, EX HN3, EX HN1, PC6, HT7, SP6, special point for depression Experimental: Psychotherapy: thought imprint psychotherapy under lower resistance state Experimental: Physiotherapy: transcranial magnetic stimulation on the head |
| Outcomes | Psychological questionnaires at 1 week, 2 weeks, 4 weeks, 6 weeks, and 12 weeks post treatment |
| Starting date | March 2012 |
| Contact information | Study leader: Xue Yan (snowater27@hotmail.com) |
| Notes | Estimated completion date: March 2014 |
Yanli 2015.
| Trial name or title | Wrist‐ankle acupuncture combined with Prozac in the treatment of post‐stroke depression |
| Methods | Randomised controlled trial comparing 3 different styles of wrist‐ankle needling in conjunction with fluoxetine |
| Participants | 105 patients aged 30 to 75 years with a diagnosis of post‐stroke depression according to TCM syndrome diagnostic criteria, with HAMD score ≥ 18 in the post‐acute phase (2 weeks after stroke), with vital signs that are stable. Patient is conscious, has certain expression and communication skills, and is able to sign informed consent or has immediate family members who will sign informed consent. |
| Interventions |
Group 1: Thick needle+Prozac Group 2: Fine needle+Prozac Group 3: Sham needle+Prozac |
| Outcomes | Hamilton Depression Rating Scale (HAMD), Self‐rating Depression Scale (SDS) |
| Starting date | June 2015 |
| Contact information | Study leader: You Yanli (youyanli2005@163.com) |
| Notes | Recruitment pending |
ACTH: adrenocorticotropic hormone.
ALFF: amplitude of spontaneous low‐frequency fluctuation.
CBT: cognitive‐behavioural therapy.
CCMD: Chinese Classification of Mental DIsorders.
CGI: Clinical Global Impression Scale.
CORT: Cortisol.
CT: computed tomography.
DMN: default mode network.
DSM‐5: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
fMRI: functional magnetic resonance imaging.
HAMD: Hamilton Depression Rating Scale.
HRT: hormone replacement therapy.
ICD‐10: International Statistical Classification of Diseases and Related Health Problems, Tenth Edition.
IL: interleukin.
MADRS: Montgomery‐Asberg Depression Rating Scale.
MRI: magnetic resonance imaging.
PSQI: Pittsburg Sleep Quality Index.
ReHo: regional homogeneity.
SCID: Structured Clinical Interview for DSM.
SDS: Self‐rating Depression Scale.
SF‐36: Short Form Health Survey.
SSRI: selective serotonin reuptake inhibitor.
STRAW‐10: Stages of Reproductive Aging Workshop.
TCM: Traditional Chinese Medicine.
TNF: tumour necrosis factor.
Differences between protocol and review
Review authors used a random‐effects model to pool the results of all studies because this model is more conservative than a fixed‐effect model and incorporates both within‐study and between‐study variance. This decision reflects a change from the original protocol. The statement that data on at least one primary outcome must be reported for inclusion has been removed because outcome measures do not serve as the basis for inclusion.
In updating this review, we made the following changes to the protocol: (1) excluded quasi‐randomised controlled trials owing to the large number of randomised trials now published; (2) performed an a posteriori subgroup analysis to examine the effect of the number of treatment sessions undertaken (< 20 sessions vs ≥ 20 sessions); (3) added a new comparison of acupuncture plus medication versus medication alone to bring this update in line with others from the CCMD Group; (4) reported individual quality of life domains in the absence of an overall score; (5) if data were not reported in a form that could be included in the meta‐analysis, provided a narrative report of the findings; (6) performed an a posteriori sensitivity analysis to examine the effects of overall risk of bias; and (7) planned to perform an a posteriori subgroup analysis to examine effects of using self‐reported versus clinician‐rated scales. We could not undertake this analysis owing to the small number of included studies. We instead explored the impact of this factor on each outcome when we encountered a mixture of self‐reported and clinician‐rated depression outcomes.
Contributions of authors
Caroline Smith conceptualised and took the lead in writing the protocol and review, performed initial searches of databases for trials, was involved in selecting trials for inclusion, performed data extraction and quality assessment of included trials, and was responsible for statistical analysis and interpretation of trial data.
Mike Armour performed data extraction and quality assessments of the included trials, assisted with statistical analysis and interpretation of the data, and edited the updated review.
Myeong Soo Lee performed data extraction and quality assessments of the included trials, assisted with statistical analysis and interpretation of the data, and edited the updated review.
Li‐Qiong Wang performed data extraction and quality assessment of the included trials, assisted with interpretation of data, and commented on drafts of the updated review.
Phillipa Hay was involved in selecting trials for inclusion, performed data extraction and quality assessment of the included trials, assisted with interpretation of the data, and commented on drafts of the protocol and the review.
Sources of support
Internal sources
Western Sydney University, Australia.
University of York, UK.
External sources
-
National Institute for Health Research, Department of Health, UK.
Department of Health’s 2008 Cochrane Review Incentive Scheme
Declarations of interest
CS, LQW, MSL, PH: none known.
MA is not currently in clinical practice but remains the director of a private acupuncture and physiotherapy practice.
CA and MA as members of NICM declare that as a medical research institute, NICM receives research grants and donations from foundations, universities, government agencies, and industry. Sponsors and donors provide untied funding for work done to advance the vision and mission of the Institute. In general, NICM respects confidentiality in these arrangements, so as to avoid any likelihood of generating unwelcome further solicitations to the donor or sponsor from outside parties.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Allen 1998 {published data only}
- Allen JB, Schyner RN, Hitt SK. The efficacy of acupuncture in the treatment of major depression in women. Psychological Science 1998;9(5):397‐401. [Google Scholar]
Allen 2006 {published data only}
- Allen JJ, Schyner RN, Chambers AS, Hitt SK. Acupuncture for depression: a randomised controlled trial. Journal of Clinical Psychiatry 2006;67(11):1665‐73. [DOI] [PubMed] [Google Scholar]
Andreescu 2011 {published data only}
- Andreescu C, Glick RM, Emeremni CA, Houck PR, Mulsant BH. Acupuncture for the treatment of major depressive disorder: a randomised controlled trial. Journal of Clinical Psychiatry 2011;72(8):1129‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bosch 2015 {published data only}
- Bosch P, Noort M, Yeo S, Lim S, Coenen A, Luijtelaar G. The effect of acupuncture on mood and working memory in patients with depression and schizophrenia. Journal of Integrative Medicine 2015;13:380‐90. [DOI] [PubMed] [Google Scholar]
Cheng 2007 {published data only}
- Cheng Y, Tang QS. Abdominal acupuncture in treating liver‐qi stagnation and spleen deficiency in the elderly with post‐stroke depression: a randomized and controlled observation. Chinese Journal of Clinical Rehabilitation Tissue Engineering Research 2007;11(39):7791‐4. [Google Scholar]
Chung 2015 {published data only}
- Chung KF, Yeung WF, Yu YM, Yung K‐P, Zhang S‐P, Zhang Z‐J, et al. Acupuncture for residual insomnia associated with major depressive disorder: a placebo and sham controlled subject and assessor blind randomised trial. Journal of Clinical Psychiatry 2015;76(6):752‐60. [DOI] [PubMed] [Google Scholar]
Ding 2003 {published data only}
- Ding Z, Yu X‐G. Clinical study on treatment of post‐stroke depression with acupuncture of Du meridian as main therapy. Journal of Beijing University of TCM (Clinical Medicine) 2003;10(3):31‐3. [Google Scholar]
Dong 2007 {published data only}
- Dong JP, Sun WY, Wang S, Wu ZQ, Liu F. Clinical observation on head point‐through‐point electroacupuncture for treatment of post stroke depression. Chinese Acupuncture and Moxibustion 2007;27(4):241‐4. [PubMed] [Google Scholar]
Du 2005 {published data only}
- Du YH, Li GP, Yan H, Zhang XJun, Huang LF. Clinical study on needling method for regulating mental activities and soothing liver for treatment of melancholia. Chinese Acupuncture and Moxibustion 2005;25:151‐4. [PubMed] [Google Scholar]
Duan 2008 {published data only}
- Duan M, Tu Y, Chen LP. Assessment of effectiveness of electroacupuncture and fluoxetine for treatment of depression with physical symptoms. Chinese Acupuncture and Moxibustion 2008;28(3):167‐70. [PubMed] [Google Scholar]
Duan 2011 {published data only}
- Duan DM, Tu Y, Liao S, Qin W. The relevance between symptoms and magnetic resonance imaging analysis of the hippocampus of depressed patients given electro‐acupuncture combined with fluoxetine intervention: a randomized controlled trial. Chinese Journal of Integrative Medicine 2011;17(3):190‐9. [DOI] [PubMed] [Google Scholar]
Eich 2000 {published data only}
- Eich H, Agelink MW, Lehman E, Lemmer W, Kliesser E. Acupuncture in patients with minor depression or generalized anxiety disorders ‐ results of a randomized study. Fortschritte Der Neurologie Psychiatrie 2000;68:137‐44. [DOI] [PubMed] [Google Scholar]
Fan 2005 {published data only}
- Fan L, Fu WB, Meng CR, Zhu XP, Mi JP, Li WX, et al. Effect of acupuncture at routine acupoint and no‐acupoint on depressive neurosis evaluated by Hamilton Depression Scale. Chinese Journal of Clinical Rehabilitation 2005;9(28):14‐6. [Google Scholar]
Fan 2013 {published data only}
- Fan L, Fu WB, Xu NG, Liu JH, Li ZP, Ou AH. Impact of acupuncture and moxibustion on outcome indices of depression patients subjective reports. World Journal of Acupuncture‐Moxibustion 2013;23(2):22‐8. [PubMed] [Google Scholar]
Feng 2011 {published data only}
- Feng Y, Wang XY, Li SD, Zhang Y, Wang HM, Li M, et al. Clinical research of acupuncture on malignant tumour patients for improving depression and sleep quality. Journal of Traditional Chinese Medicine 2011;31(3):199‐202. [DOI] [PubMed] [Google Scholar]
Fu 2006 {published data only}
- Fu WB, Fan L, Zhu XP, He Q, Wang L, Zhang LX, et al. Clinical research on acupuncture treatment of depressive neurosis by using liver‐function‐regulating method. Acupuncture Research 2006;31:355‐8. [Google Scholar]
Fu 2008 {published data only}
- Fu WB, Fan L, Zhu XP, He Q, Wang L, Zhuang LX, et al. Acupuncture for treatment of depressive neurosis: a multi‐centred randomized controlled trial. Chinese Acupuncture and Moxibustion 2008;28(1):3‐6. [PubMed] [Google Scholar]
- Fu WB, Fan L, Zhu XP, He Q, Wang L, Zhuang LX, et al. Depressive neurosis by acupuncture for regulating the liver ‐ a report of 176 cases. Journal of Traditional Chinese Medicine 2009;29(2):83‐6. [DOI] [PubMed] [Google Scholar]
Han 2002 {published data only}
- Han C, Li XW, Luo HC. Comparative study of electro‐acupuncture and maprotiline in treating depression. Combined Chinese/Western Journal 2002;22(7):512‐4. [PubMed] [Google Scholar]
He 2005 {published data only}
- He XJ, Tan JL, Wang BH, et al. Effects of acupuncture using Xingnao Kaiqiao (consciousness restoring resuscitation) needling method on acupuncture with post stroke depression. Chinese Journal of Rehabilitation Theory and Practice 2005;11(6):467‐8. [Google Scholar]
He 2007 {published data only}
- He J, Shen PF. Clinical study on the therapeutic effect of acupuncture in the treatment of post‐stroke depression. Acupuncture Research 2007;32:58‐61. [PubMed] [Google Scholar]
He 2012 {published data only}
- He YS, Wu YS, Oufang MF, Li GX, Li HJ, Xie HE. Efficacy of observation of depression in nicotine withdrawal treatment with acupuncture. World Journal of Acupuncture‐Moxibustion 2012;22(1):13‐7. [Google Scholar]
Huang 2013 {published data only}
- Huang Y, Wang XJ, Wang LL, Lu SF, Zhu BM, Xu L. Effect of acupuncture on selective serotonin reuptake inhibitors. Chinese Journal of Integrative Medicine 2013;33:1341‐4. [PubMed] [Google Scholar]
Li 2004 {published data only}
- Li GP, Du YH, Yan H, Zhang XiJ, Huang LF. Clinical effect of Tiaoshen Shugan acupuncture on depression (clinical observation on regulating mental activity and soothing liver (tiao shen su gan) needling method for treatment of depression). Tianjin Journal of Traditional Chinese Medicine 2004;21(4):382‐5. [Google Scholar]
Li 2007 {published data only}
- Li SJ, Liu T. Clinical observation on treatment of melancholia by acupuncture following principle of relieving depression and regulating mentality. Chinese Journal of Integrated Traditional and Western Medicine 2007;27:155‐7. [PubMed] [Google Scholar]
Li 2008 {published data only}
- Li YW, Fu WB, Zhu XP. Clinical observation on acupuncture for depressive of 27 cases. Journal of Traditional Chinese Medicine 2008;49:431‐3. [Google Scholar]
Li 2011b {published data only}
- Li HJ, Zhong BL, Fan YP, Hu HT. Acupuncture for post stroke depression:a randomized controlled trial. Chinese Acupuncture and Moxibusion 2011;31:3‐6. [PubMed] [Google Scholar]
Lin 2012 {published data only}
- Lin WR, Huang Y, Chen JQ, Wang SX. Global improvement in agitated depression treated with the alliance therapy of acupuncture and seroxat and the observation of the quality of life. Chinese Acupuncture and Moxibusion 2012;32:1063‐9. [PubMed] [Google Scholar]
Liu 2006 {published data only}
- Liu SK, Zhao XM, Xi ZM. Incidence rate and acupuncture‐moxibustion treatment of post‐stroke depression. Chinese Acupuncture and Moxibustion 2006;26:472‐4. [PubMed] [Google Scholar]
Liu 2013a {published data only}
- Liu Y, Zhang YH, Jin M, Liu WJ. Study on clinical effect of enhancement of acupuncture for depression with chronic pain treated with SSRI antidepressants. Chinese Acupuncture and Moxibustion 2013;13:689‐91. [PubMed] [Google Scholar]
Liu 2015 {published data only}
- Liu Y, Feng H, Mao H, Mo Y, Yin Y, Liu W, et al. Impact on serum 5‐HT and TH1/TH2 in patients of depressive disorder at acute stage treated with acupuncture and western medication. Chinese Acupuncture and Moxibustion 2015;35:539‐43. [PubMed] [Google Scholar]
Luo 1985 {published data only}
- Luo HC, Yunkui J, Zhan L. Electro‐acupuncture versus amitriptyline in the treatment of depressive states. Journal of Traditional Chinese Medicine 1985;5(1):3‐8. [PubMed] [Google Scholar]
Luo 1988 {published data only}
- Luo HC, Shen YC, Jia YK, Zhou D. Clinical study of electro‐acupuncture on 133 patients with depression in comparison with tricyclic amitriptyline. Chinese Journal of Modern Developments in Traditional Medicine 1988;8(2):77‐80. [PubMed] [Google Scholar]
Luo 1998 {published data only}
- Luo H, Meng F, Jia Y, Zhao X. Clinical research on the therapeutic effect of the electro‐acupuncture treatment in patients with depression. Psychiatry and Clinical Neurosciences 1998;52:338‐40. [DOI] [PubMed] [Google Scholar]
Lv 2015 {published data only}
- Lv X, Wang B, Chen J, Ye J. Clinical observation of depression after breast cancer operation treated with auricular point sticking therapy. Chinese Acupuncture and Moxibustion 2015;35:447‐50. [PubMed] [Google Scholar]
Ma 2011 {published data only}
- Ma Q, Zhou DA, Wang LP. Clinical curative effect and factor analysis of depression treated by acupuncture. Chinese Acupuncture and Moxibustion 2011;31:875‐8. [PubMed] [Google Scholar]
Ma 2012 {published data only}
- Ma S, Qu S, Huang Y, Chen J, Lin R, Wang C, et al. Improvement in quality of life in depressed patients following verum acupuncture or electroacupuncture plus paroxetine. Neural Regeneration Research 2012;7(27):2123‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
MacPherson 2013 {published data only}
- MacPherson H, Richmond S, Bland M, Brealey S, Gabe R, Hopton A, et al. Acupuncture and counselling for depression in primary care: a randomised controlled trial. PloS Medicine 2013;10(9):e1001518. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pei 2006 {published data only}
- Pei Y, Zhang J, Chen J, Qiao J. Clinical observation of acupuncture in treating depression on Wang‐Shi Back‐shu points of five‐zang. Chinese Journal of Information on TCM 2006;13:62‐3. [Google Scholar]
Qiao 2007 {published data only}
- Qiao YX, Cheng WP. Clinical observation of acupuncture in treating depression at Baihui (GV20) and Shenmen (H 7). Journal of Clinical Acupuncture and Moxibustion 2007;23:52‐4. [Google Scholar]
Qu 2013 {published data only}
- Qu SS, Huang Y, Zhang ZJ, Chen JQ, Lin RY, Wang CQ, et al. A 6 week randomised controlled trial with 4 week follow up of acupuncture combined with paroxetine in patients with major depressive disorder. Journal of Psychiatric Research 2013;47:726‐32. [DOI] [PubMed] [Google Scholar]
Quah‐Smith 2005 {published data only}
- Quah‐Smith JI, Tang WM, Russell J. Laser acupuncture for mild to moderate depression in a primary care setting. Acupuncture in Medicine 2005;23(3):103‐11. [DOI] [PubMed] [Google Scholar]
Quah‐Smith 2013 {published data only}
- Quah‐Smith I, Smith C, Crawford JD, Russell J. Laser acupuncture for depression: a randomised double blind controlled trial using low intensity laser intervention. Journal of Affective Disorders 2013;148(2‐3):179‐87. [DOI] [PubMed] [Google Scholar]
Roschke 2000 {published data only}
- Roschke J, Wolf C, Muller MJ, Wagner P, Mann K, Grozinger M, et al. The benefit from whole body acupuncture in major depression. Journal of Affective Disorders 2000;57:73‐81. [DOI] [PubMed] [Google Scholar]
Shen 2005 {published data only}
- Shen PF, Shi XM. Study on clinical therapeutic effect of activating brain and regaining consciousness needling method on post‐stroke depressing and the mechanism. Chinese Acupuncture and Moxibustion 2005;25:11‐3. [PubMed] [Google Scholar]
Sun 2010 {published data only}
- Sun H, Zhao H, Zhang J, Bao F, Wei J, Wang DH, et al. Effect of acupuncture at Baihui (GV 20) and Zusanli (ST36) on the level of serum inflammatory cytokines in patients with depression. Chinese Acupuncture and Moxibustion 2010;30:195‐9. [PubMed] [Google Scholar]
Sun 2013 {published data only}
- Sun H, Zhao H, Ma C, Bao F, Zhang J, Wang DH, et al. Effects of electroacupuncture on depression and the production of glial cell line–derived neurotrophic factor compared with fluoxetine: a randomized controlled pilot study. Journal of Alternative and Complementary Medicine 2013;19(9):733‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2015b {published data only}
- Sun P, Chu H, Li P, Wang T, Pu F, Wu J, et al. The effect of the acupuncture intervention of dredging Governor Vessel and regulating mentality for the medication treatment of post‐stroke depression. Chinese Acupuncture and Moxibustion 2015;35:753‐7. [PubMed] [Google Scholar]
Tang 2003 {published data only}
- Tang SX, Xu ZH, Tang P, Li FP. Clinical study on acupuncture treatment of depressive neurosis. Chinese Acupuncture and Moxibustion 2003;23:585‐6. [Google Scholar]
Wang 2014 {published data only}
- Wang T, Wang L, Tao W, Chen L. Acupuncture combined with an antidepressant for patients with depression in hospital: a pragmatic randomised controlled trial. Acupuncture in Medicine 2014;32:308‐12. [DOI] [PubMed] [Google Scholar]
Wang 2015 {published data only}
- Wang C, Liu M, Lv J, Li N. Effect of acupuncture and moxibustion on depressive states of stroke patients' spouses. Chinese Acupuncture and Moxibustion 2015;35:223‐6. [PubMed] [Google Scholar]
Wenbin 2002 {published data only}
- Wenbin F. Clinical research on acupuncture treatment of depressive psychosis. World Journal of Acupuncture‐Moxibustion 2002;12(3):13‐6. [Google Scholar]
Whiting 2008 {published data only}
- Whiting M, Leavey G, Scammell A, Au S, King M. Using acupuncture to treat depression: a feasibility study. Complementary Therapies in Medicine 2008;16:87‐91. [DOI] [PubMed] [Google Scholar]
Xiao 2014 {published data only}
- Xiao B. Liu ZH. Efficacy on depression in breast cancer treated with acupuncture and auricular acupressure. Chinese Acupuncture and Moxibustion 2014;34:956‐60. [PubMed] [Google Scholar]
Xiujuan 1994 {published data only}
- Xiujuan Y. Clinical observation on needling extrachannel points in treating mental depression. Journal of Traditional Chinese Medicine 1994;14(1):14‐8. [PubMed] [Google Scholar]
Xu 2011 {published data only}
- Xu L, Wang LL. Clinical observation on depression treated by electroacupuncture combined with western medicine. Chinese Acupuncture and Moxibustion 2011;31:779‐82. [PubMed] [Google Scholar]
Yan 2004 {published data only}
- Yan M, Mao X, Wu JL. Comparison of electroacupuncture and amitriptyline in treating depression. Chinese Journal of Clinical Rehabilitation 2004;18:3548‐9. [Google Scholar]
Yeung 2011b {published data only}
- Yeung MF, Chung KF, Tso KC, Zhang SP, Zhang ZJ, Ho LM. Electroacupuncture for residual insomnia associated with major depressive disorder: a randomised controlled trial. Sleep 2011;34(6):807‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2003 {published data only}
- Zhang H, He J. Clinical observation of electro‐acupuncture in treating depression. Journal of Acupuncture and Tuina Science 2003;1(4):24‐6. [Google Scholar]
Zhang 2005a {published data only}
- Zhang DL. Application of acupuncture in patients with depression. Chinese Journal of Clinical Rehabilitation 2005;9:217‐8. [Google Scholar]
Zhang 2007 {published data only}
- Zhang GJ, Shi ZY, Liu S, Gong SH, Liu JQ. Clinical observation of treatment of depression by electro‐acupuncture combined with paroxetine: clinical observations. Chinese Journal of Integrative Medicine 2007;13(3):228‐30. [DOI] [PubMed] [Google Scholar]
Zhang 2007a {published data only}
- Zhang LJ, Zhao H. Clinical observation of acupuncture in treating depression and effect on serum cell factors. Chinese Journal of Information on TCM 2007;14:15‐7. [Google Scholar]
Zhang 2009 {published data only}
- Zhang WJ, Yang X‐B, Zhong B‐L. Combination of acupuncture and fluoxetine for depression: a randomised double blind sham controlled trial. Journal of Alternative and Complementary Medicine 2009;15(8):837‐44. [DOI] [PubMed] [Google Scholar]
Zhang 2012 {published data only}
- Zhang ZJ, Ng R, Man SC, Li TYJ, Wong W, Tan QR, et al. Dense cranial electro‐acupuncture stimulation for major depressive disorder: a single blind, randomized controlled study. PLoS One 2012;7(1):e29651. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhuang 2004 {published data only}
- Zhuang ZQ, Wang CR. Treatment of poststroke depression by Zhisanzhen combined with digital point pressure and massage. Chinese Acupuncture and Moxibustion 2004;24:800‐2. [Google Scholar]
References to studies excluded from this review
Agelink 2003 {published data only}
- Agelink MW, Sanner D, Elch H, Pach J, Bertling R, Lemmer W, et al. Does acupuncture influence cardiac autonomic nervous system in patients with minor depression or anxiety disorders. Fortschritte der Neurologie und Psychiatrie 2003;71:141‐9. [DOI] [PubMed] [Google Scholar]
Arvidsdotter 2014 {published data only}
- Arvidsdotter T, Bertil Marklund B, Taft C. Six‐month effects of integrative treatment, therapeutic acupuncture and conventional treatment in alleviating psychological distress in primary care patients ‐ follow up from an open,pragmatic randomized controlled trial. BMC Complementary and Alternative Medicine 2014;14:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bennett 1997 {published and unpublished data}
- Bennett CF. Treatment effects of acupuncture on anxiety and depression in working women. Dissertation Abstracts International 1998;58(11B):5886. [Google Scholar]
Bergmann 2014 {published data only}
- Bergmann N, Ballegaard S, Hjalmarson A, Krogh J, Gyntelberg F, Faber J. The effect of daily self‐measurement of pressure pain sensitivity followed by acupressure on depression and quality of life versus treatment as usual in ischemic heart disease: a randomised controlled trial. PLoS One 2014;9(5):e97553. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bin 2007 {published data only}
- Bin F, Lanying L, Fangzhong X, Jiong C, Peirong W, Wensong C, et al. Thirty cases of obsession treated by point‐stimulation and with small dose of chlorimipramine. Journal of Traditional Chinese Medicine 2007;27(1):3‐6. [PubMed] [Google Scholar]
Carvalho 2013 {published data only}
- Carvalho F, Weires K, Ebling M, Padiha MSR, Ferrao YA, Vercelino R. Effects of acupuncture on the symptoms of anxiety and depression by premenstrual dysphoric disorder. Acupuncture in Medicine 2013;31:358‐63. [DOI] [PubMed] [Google Scholar]
Chang 2009 {published data only}
- Chang Y. The effect on serotonin and MDA levels in depressed patients with insomnia when Far‐Infared rays are applied to acupoints. American Journal of Chinese Medicine 2009;37(5):837‐42. [DOI] [PubMed] [Google Scholar]
Chang 2010 {published data only}
- Chang SH, Fang MC, Yang YS. Effectiveness of transcutaneous electrical acupoint stimulation for improving depressive mood status among nursing home elders in Taiwan: a pilot study. Geriatric Nursing 2010;31:324‐30. [DOI] [PubMed] [Google Scholar]
Chang‐du 1994 {published data only}
- Chang‐du L, Yong H, Ying‐kun L, Ka‐ming H, Zhen‐ya J. Treating post stroke depression with "mind refreshing antidepressive": acupuncture therapy: a clinical study of 21 cases. International Journal of Clinical Acupuncture 1994;5(4):389‐93. [Google Scholar]
Cocchi 1977 {published data only}
- Cocchi R, Fusari A, Lorini G, Roccia L. Agopuntura, farmaci vitali e psicofarmaci nel trattamento di pazienti psichiatrici a struttura depressiva di fondo. Minerva Medica 1977;68:23092314. [PubMed] [Google Scholar]
Deng 2013 {published data only}
- Deng G, Chan Y, Sjoberg D, Vickers A, Yeung KS, Kris M, et al. Acupuncture for the treatment of post‐chemotherapy chronic fatigue: a randomized, blinded, sham controlled trial. Supportive Cancer Care 2013;21:1735‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dormaemen 2011 {published data only}
- Dormaemen A, Heimdal MR, Wang CFA, Grimsgaard AS. Depresion in postmenopause: a study on a subsample of the Acupuncture on Hot Flushes Among Menopausal Women (ACUFLASH) study. Menopause 2011;18(5):525‐30. [DOI] [PubMed] [Google Scholar]
Duan 2009 {published data only}
- Duan D, Chen LP, Wu ZJ. Efficacy evaluation for depression with somatic symptoms treated by electroacupuncture combined with fluoxetine. Journal of Traditional Chinese Medicine 2009;29(3):167‐73. [DOI] [PubMed] [Google Scholar]
Fan 2015b {published data only}
- Fan L, Gong J, Fu W, Chen Z, Xu N, Liu J, et al. Gender‐related differences in outcomes on acupuncture and moxibustion treatment among depression patients. Journal of Alternative and Complementary Medicine 2015;21(11):673‐80. [DOI] [PubMed] [Google Scholar]
Gallagher 2002 {published data only}
- Gallagher SM, Allen JJB, Hitt SK, Schyner RN, Manber R. Six month depression relapse rates among women treated with acupuncture. Complementary Therapies in Medicine 2002;9:216‐8. [DOI] [PubMed] [Google Scholar]
Guo 2009 {published data only}
- Guo RY, Su L, Liu L, Wang CX. Effects of Linggui Bafa on the therapeutic effect and quality of life in patients of post‐stroke depression. Chinese Acupuncture and Moxibustion 2009;29:785‐90. [PubMed] [Google Scholar]
He 2007b {published data only}
- He Q, Zhang J, Tang Y. A controlled study on treatment of mental depression by acupuncture plus TCM medication. Journal of Traditional Chinese Medicine 2007;27(3):166‐9. [PubMed] [Google Scholar]
He 2011 {published data only}
- He LL, Zheng Z, Cai DJ, Zou K. Randomized controlled trial on comorbid anxiety and depression treated with electroacupuncture combined with rTMS. Chinese Acupuncture and Moxibustion 2011;31:294‐8. [PubMed] [Google Scholar]
Hmwe 2015 {published data only}
- Hmwe NTT, Subramanian P, Tan LP, Chong WK. The effects of acupressure on depression, anxiety and stress in patients with hemodialysis: a randomized controlled trial. International Journal of Nursing Studies 2015;52(2):509–18. [DOI] [PubMed] [Google Scholar]
Honda 2012 {published data only}
- Honda Y, Tsuda A, Horiuchi S. Four week self administered acupressure improves depressive mood. Psychology 2012;3:802‐4. [Google Scholar]
Hou 1996 {published data only}
- Hou DF, Lo HC. Clinical observation of therapeutic effect of baihui (GV20)‐yintang (EX‐HN3) electro‐acupuncture in 30 cases of post‐apoplectic depression. Chinese Acupuncture and Moxibustion 1996;16(8):432‐3. [Google Scholar]
Hu 2013 {published data only}
- Hu J, Chen C, Bi X, Yu Z, Yang P, Fan Z, et al. Effect of early intervention of liver‐smoothing and blood‐activating decoction combined with acupuncture on patients with post‐stroke depression. China Journal of Chinese Materia Medica 2013;38(14):2403‐5. [PubMed] [Google Scholar]
Huang 2003 {published data only}
- Huang Y, Xia D, Zhou J. Clinical observation on treating 46 cases of post‐windstroke depression by scalp‐electrical acupuncture. China Journal of Basic Medicine in Traditional Chinese Medicine 2003;9:60‐2. [Google Scholar]
Huang 2004 {published data only}
- Huang DH, Wang CY, Huang JH, Ye Y, Chen XH. Point injection therapy combining baihui acupuncture with parental solution of breviscapine for post cerebral infarction depression. Chinese Journal of Chinese Rehabilitation 2004;28(8):6132‐3. [Google Scholar]
Huang 2005 {published data only}
- Huang Y, Jing C, Jun Z. Effect of scalp acupuncture on post stroke depression. Chinese Journal of Clinical Rehabilitation 2005;9(40):172‐3. [Google Scholar]
Huo 2013 {published data only}
- Huo ZJ, Guo J, Li D. Effects of acupuncture with meridian acupoints and three anmian acupoints on insomnia and related depression and anxiety state. Chinese Journal of Integrative Medicine 2013;19(3):187‐91. [DOI] [PubMed] [Google Scholar]
Khang 2002 {published data only}
- Kang B, Zhang PG, Xiong SC, et al. Control observation on electroacupuncture and amitriptyline for treatment of depression. Chinese Acupuncture and Moxibustion 2002;22(6):383‐4. [Google Scholar]
Kim 2015 {published data only}
- Kim JE, Seo BK, Choi JB, Kim HJ, Kim TH, Lee MH, et al. Acupuncture for chronic fatigue syndrome and idiopathic chronic fatigue: a multicenter, nonblinded, randomized controlled trial. Trials 2015;16:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2011 {published data only}
- Li H, Zhong B, Fan Y, Hu H. Acupuncture for post‐stroke depression: a randomized controlled trial. Chinese Acupuncture and Moxibustion 2011;31:3‐6. [PubMed] [Google Scholar]
Liu 2013 {published data only}
- Liu Y, Zhang YH, Jin M, Liu WJ. Study on clinical effect enhancement of acupuncture for depression with chronic pain treated with SSRI antidepressants. Chinese Acupuncture and Moxibustion 2013;33(6):689‐91. [PubMed] [Google Scholar]
Lu 2004 {published data only}
- Lu M, Wang LL, Lui LY, Maho L. Clinical research on treatment of depression with electroacupuncture and SSRI. Journal of Nanjing University of Traditional Chinese Medicine 2004;20:149‐51. [Google Scholar]
Man 2014 {published data only}
- Man SC, Hung BH, Ng RMK, Yu XC, Cheung H, Fung MPM, et al. A pilot controlled trial of a combination of dense cranial electro‐acupuncture stimulation and body acupuncture for post stroke depression. BMC Complementary and Alternative Medicine 2014;14:255. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mischoulon 2012 {published data only}
- Mischoulon D, Brill CD, Ameral V, Fava M, Yeung AS. A pilot study of acupuncture monotherapy in patients with major depressive disorder. Journal of Affective Disorders 2012;141:469‐73. [DOI] [PubMed] [Google Scholar]
Niu 2006 {published data only}
- Niu SY, Li N, You H, Shi SX, Liu CM. Effect of integrated therapy of Chinese and western medicine on differentiation of symptoms and signs of patients with depression. Chinese Journal of Clinical Rehabilitation 2006;10:7‐9. [Google Scholar]
Shi 2014 {published data only}
- Shi X, Wang H, Wang L, Zhao Z, Litscher D, Tao J, et al. Can tongue acupuncture enhance body acupuncture? First results from heart rate variability and clinical scores in patients with depression. Evidence‐Based Complementary and Alternative Medicine 2014;2014:329746. [DOI] [PMC free article] [PubMed] [Google Scholar]
Song 1999 {published data only}
- Song Y, Liang HR. Observation of the curative effect of scalp acupuncture on cerebral postapoplectic depression. Shanghai Journal of Acupuncture‐Moxibustion 1999;18(1):8‐9. [Google Scholar]
Sun 2012 {published data only}
- Sun ZG, Lian F, Zhang JW. Effects of acupuncture combined Chinese materia medica for tonifying shen and soothing gan on the anxiety and depression of patients with in vitro fertilization and embryo transplantation and on the treatment outcomes. Chinese Journal of Integrated Traditional and Western Medicine 2012;32(8):1023‐7. [PubMed] [Google Scholar]
Tang 2003b {published data only}
- Tang JX, Guan NH, Li L, Liu JF. Influence of electroacupuncture on the quality of life in patients with post apoplectic depression. Shanghai Journal of Acupuncture and Moxibustion 2003;22:12‐4. [Google Scholar]
Tse 2010 {published data only}
- Tse M, Au J. The effects of acupressure in older adults with chronic knee pain: depression, pain, activities of daily living and mobility. Journal of Pain Management 2010;3(4):399‐410. [Google Scholar]
Wang 2003 {published data only}
- Wang H. Clinical observation on acupuncture for treatment of depression after apoplexy. Chinese Acupuncture and Moxibustion 2003;23:442‐4. [PubMed] [Google Scholar]
Wang 2004 {published data only}
- Wang Y, Zhao ZF, Wu Y. Clinical therapeutic effect of acupuncture on post stroke depression with insomnia. Chinese Acupuncture and Moxibustion 2004;24(9):603‐6. [Google Scholar]
Wang 2005 {published data only}
- Wang TJ. Clinical observation on acupuncture for treatment of depression. Chinese Acupuncture and Moxibustion 2005;25:107‐10. [PubMed] [Google Scholar]
Wang 2006 {published data only}
- Wang J. Clinical observation on Governor Vessel Daoqi method for treatment of dysomnia in the patient of depression. Chinese Acupuncture and Moxibustion 2006;26:328‐30. [PubMed] [Google Scholar]
Wu 2010 {published data only}
- Wu JP. Clinical observation on acupuncture treatment of 150 cases of post‐stroke depression according to syndrome differentiation. Acupuncture Research 2010;35:303‐6. [PubMed] [Google Scholar]
Xie 2009 {published data only}
- Xie YC, Li YH. Observation on therapeutic effect of acupuncture at Zhongwan (CV 12) and Si‐guan points combined with reinforcing‐reducing manipulation of respiration for treatment of depression. Chinese Acupuncture and Moxibustion 2009;29:521‐4. [PubMed] [Google Scholar]
Xie 2012 {published data only}
- Xie HW, Bai CY, Yi Y, Xu FM, Song YE, Li LM, Tang X. Observation on therapeutic effect of acupuncture of five Shu‐points of the liver meridian combined with bloodletting for depression patients and concomitant changes of blood rheology. Acupuncture Research 2012;37:140‐44. [PubMed] [Google Scholar]
Yeung 2011 {published data only}
- Yeing AS, Ameral VE, Chuzi SE, Fava M, Mischoulon D. A pilot study of acupuncture augmentation therapy in antidepressant partial and non‐responders with major depressive disorder. Journal of Affective Disorders 2011;130:285‐9. [DOI] [PubMed] [Google Scholar]
Zhang 2004 {published data only}
- Zhang J, Liu X, Zhang H. A controlled study of electro‐acupuncture and amitriptyline in the treatment of depression. Journal of Clinical Psychosomatic Diseases 2004;19:98‐9. [Google Scholar]
Zhang 2004b {published data only}
- Zhang Y. Study of acupuncture on depression after apoplexy and rehabilitation effect of nerve function. Modern Journal of Integrated Traditional Chinese and Western Medicine 2004;13:864. [Google Scholar]
Zhao 2014 {published data only}
- Zhao YD, Han DY, Guo X. Warming‐promotion acupuncture for post‐earthquake depression: a randomized controlled study. Chinese Acupuncture and Moxibusion 2014;34:755‐8. [PubMed] [Google Scholar]
Zhou 2007 {published data only}
- Zhou SH. Acupuncture in the treatment of female climacteric depression in 60 cases. Journal of Clinical Rehabilitation Tissue Engineering Research 2007;11(39):7817‐9. [Google Scholar]
Zhou 2015 {published data only}
- Zhou X, Li Y, Zhou Z, Pan S. Clinical observation of acupuncture in patients with depression and its impact on serum 5‐HT. Chinese Acupuncture and Moxibustion 2015;35:123‐6. [PubMed] [Google Scholar]
References to studies awaiting assessment
Fu 2003 {published data only}
- Fu WB. Observations on the curative effect of acupuncture on depressive neurosis. Journal of Acupuncture and Tuina Science 2003;1(4):15‐7. [Google Scholar]
Guo 2012 {published data only (unpublished sought but not used)}
- Guo T, Wang Y, Sun L, Zhang W, Ma W. Acupuncture combined with an antidepressant has a better effect on major depression: a multi‐centre, randomized controlled clinical trial. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):P155. [Google Scholar]
Guo 2015 {published data only (unpublished sought but not used)}
- Guo T, Ya T, Guo Z, Zhang W, Yang X, Ma W, et al. Are early interventions beneficial for depressive status? A pragmatic randomized controlled trial. Integrative Medicine Research 2015;4. [Google Scholar]
Haiyan 2004 {published data only}
- Haiyan L, Dongfeng Z, Yuqing S. Effect of platelet protein kinase C of electro‐acupuncture and fluoxetine treatment in patients with major depressive disorder. Chinese Mental Health Journal 2004;18:688‐91. [Google Scholar]
Han 2002b {published data only}
- Han C, Wang L, Li X. Dynamic study of electrical acupuncture on serum cytokines in depressive patients. Journal of Beijing University of Traditional Chinese Medicine 2002;11:277‐9. [Google Scholar]
Han 2006 {published data only}
- Han C. Randomsied clinical trial comparing the effects of electro‐acupuncture and maprotiline in treating depression. International Journal of Clinical Acupuncture 2006;15(1):7‐14. [Google Scholar]
Li 2003 {published data only}
- Li X. Clinical effect of acupuncture and moxibustion as accessory treatment of depressive patients. Health Psychology Journal 2003;11:363‐4. [Google Scholar]
Lin 2004 {published data only}
- Lin H, Gen‐Qi U, Zhou Z. Clinical study on treatment of depression with combined acupuncture and antidepressant. Journal of Clinical Acupuncture and Moxibustion 2004;20:17‐9. [Google Scholar]
Lin 2005 {published data only}
- Lin H, Li GQ, Zhou ZB, Liu JX. Observation on therapeutic effect of combination of acupuncture with drug on depression. Chinese Acupuncture and Moxibustion 2005;25:27‐9. [PubMed] [Google Scholar]
Lu 2009 {published data only}
- Liu LY, Lu Q, Wang LL. Influence of electro‐acupuncture on the side effects of fluoxetine on depression patients. Journal of Traditional Chinese Medicine 2009;29(4):271‐4. [DOI] [PubMed] [Google Scholar]
Song 2007 {published data only}
- Song YQ, Zhou DF, Fan JH, Luo H, Halbreich U. Effects of electroacupuncture and fluoxetine on the density of GTP‐binding‐proteins in platelet membrane in patients with major depressive disorder. Journal of Affective Disorders 2007;98:253‐7. [DOI] [PubMed] [Google Scholar]
Song 2009 {published data only}
- Song C, Halbreich U, Han C, Leonard BE, Luo H. Imbalance between pro‐and anti‐inflammatory cytokines, and between Th1 and Th2 cytokines in depressed patients: the effect of electro‐acupuncture or fluoxetine treatment. Pharmacopsychiatry 2009;42:182‐8. [DOI] [PubMed] [Google Scholar]
Sun 2015 {published data only}
- Sun Y, Bao Y, Wang S, Chu J, Li L. Efficacy on post‐stroke depression treated with acupuncture at the acupoints based on ziwuliuzhu and Prozac. Chinese Acupuncture and Moxibustion 2015;35:119‐22. [PubMed] [Google Scholar]
Vázquez 2011 {published data only}
- Vázquez RD, González‐Macías L, Berlanga C, Aedo FJ. Effect of acupuncture treatment on depression: correlation between psychological outcomes and salivary cortisol levels. Salud Mental 2011;34:21‐6. [Google Scholar]
Zhang 1996 {published data only}
- Zhang B, Wenyou M, Baoting Z, Shuling L. A control study of clinical therapeutic effects of laser acupuncture on depressive neurosis. World Journal of Acupuncture and Moxibustion 1996;6(2):12‐7. [Google Scholar]
Zhang 2005 {published data only}
- Zhang C. The brain resuscitation acupuncture method for treatment of post wind stroke mental depression: a report of 45 cases. Journal of Traditional Chinese Medicine 2005;25:243‐6. [PubMed] [Google Scholar]
Zhao 2006 {published data only}
- Zhao J, Peng S. Clinical observation on acupuncture treatment of depressive neurosis in 30 cases. Journal of Traditional Chinese Medicine 2006;26(3):191‐2. [PubMed] [Google Scholar]
References to ongoing studies
Deng 2015 {published data only}
- ChiCTR‐OPC‐15005873. Effect of acupuncture on the DMN of brain in patients with major depressive disorder: a resting‐state fMRI study. chictr.org.cn/showproj.aspx?proj=10316 (first received 21 January 2015).
Fan 2015 {published data only}
- ChiCTR‐ICR‐15005935. Clinical study of acupuncture for mild and moderate depressive episodes. chictr.org.cn/showproj.aspx?proj=10394 (first received 2 April 2015). [Google Scholar]
Fu 2011 {published data only}
- ChiCTR‐TRC‐00000481. Clinical study on acupuncture treating insomnia with depression. chictr.org.cn/showproj.aspx?proj=7943 (first received 13 May 2011). [Google Scholar]
Li 2015 {published data only}
- NCT02472613. Comparison of Acupuncture and Fluoxetine for of Ischemic Post‐stroke Depression:A Multicentre Randomized Controlled Trial. clinicaltrials.gov/show/NCT02472613 (first received 8 June 2015). [Google Scholar]
Prater 2015 {published data only}
- NCT02579343. Adjunctive treatment of major depression utilizing auricular acupuncture. clinicaltrials.gov/show/NCT02579343 (first received 5th October 2015). [Google Scholar]
Tai 2013 {published data only}
- ChiCTR‐TRC‐13003434. Acupuncture based on five elements body characteristics in the treatment of patients with post‐stroke depression. chictr.org.cn/showproj.aspx?proj=6125 (first received 25th July 2013). [Google Scholar]
Wang 2014a {published data only}
- ChiCTR‐TRC‐14005228. Abdominal acupuncture on moderate and severe depression female patients: a randomized controlled blind clinical trial. chictr.org.cn/showproj.aspx?proj=4348 (first received 1st September 2014). [Google Scholar]
Weidong 2015 {published data only}
- ChiCTR‐ICR‐15006455. Clinical evaluation of depression treated by disease and syndrome combined method. chictr.org.cn/showproj.aspx?proj=10994 (first received 17 May 2015). [Google Scholar]
Weidong 2016 {published data only}
- ChiCTR‐IOR‐16008327. A clinical evaluation research for the treatment of major depression by integrated disease with Zheng of TCM method. chictr.org.cn/showproj.aspx?proj=14018 (first received 20th April 2016). [Google Scholar]
Wenben 2015 {published data only}
- NCT02423694. Effectiveness and safety of electro‐acupuncture for mild‐to‐moderate perimenopausal depression. clinicaltrials.gov/show/NCT02423694 (received 11th April 2014). [Google Scholar]
Ya 2008 {published data only}
- ChiCTR‐TRC‐08000297. The clinical study of the best treatment option in acupuncture on depression. chictr.org.cn/showproj.aspx?proj=9233 (first received 26th December 2008). [Google Scholar]
Ya 2015 {published data only}
- ChiCTR‐IPR‐15006503. The clinical curative effect of acupuncture treatment in depression. chictr.org.cn/showproj.aspx?proj=11116 (first received 4th June 2014). [Google Scholar]
Yan 2012 {published data only}
- NCT01558154. Comparison of treatment effect of Chinese Medicine and Western Medicine on depression in China and America. clinicaltrials.gov/show/NCT01558154 (first received 2nd March 2012. [Google Scholar]
Yanli 2015 {published data only}
- ChiCTR‐IOR‐15006313. Wrist‐ankle acupuncture combined with Prozac in the treatment of post‐stroke depression: clinical research. chictr.org.cn/showproj.aspx?proj=10820 (first received 21st April 2015). [Google Scholar]
Additional references
APA 2015
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th Edition. Washington, DC: American Psychiatric Association, 2013. [Google Scholar]
Armour 2016
- Armour M, Smith CA. Treating primary dysmenorrhoea with acupuncture: a narrative review of the relationship between acupuncture ‘dose’ and menstrual pain outcomes. Acupuncture in Medicine 2016;Online First 14 November 2016. [DOI: 10.1136/acupmed-2016-011110] [DOI] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Medelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Brunoni 2009
- Brunoni AR, Lopes M, Kaptchuk TJ, Freni F. Placebo response of non‐pharmacological and pharmacological trials in major depression: a systematic review and meta‐analysis. PLoS One 2009;4(3):e4824. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan 2015
- Chan YY, Lo WY, Yang SN, Chen YH, Jaung GL. The benefit of combined acupuncture and antidepressant medication for depression: a systematic review and meta‐analysis. Journal of Affective Disorders 2015;176:106‐17. [DOI] [PubMed] [Google Scholar]
Chinese Psychiatric Society 2001
- Chinese Psychiatric Society. The Chinese classification of mental disorders (3rd ed. [CCMD‐3]).. The Chinese Classification of Mental Disorders (CCMD‐3). 3rd Edition. Shandong: Shandong Publishing House of Science and Technology, 2001. [Google Scholar]
Chung 2012
- Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low‐level laser (light) therapy. Annals of Biomedical Engineering 2012; Vol. 40, issue 2:516‐33. [DOI: 10.1007/s10439-011-0454-7] [DOI] [PMC free article] [PubMed]
Davidson 2002
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldman 1999
- Goldman LS, Nielsen NH, Champion HC. Awareness, diagnosis and treatment of depression. Journal of General Internal Medicine 1999;14(9):569‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEproGDT [Computer program]
- McMaster University (developed by Evidence Prime). GRADEproGDT [GRADEproGDT]. Version accessed June 2017. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurosurgery & Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 2015
- Hamilton JP, Farmer M, Fogelman P, Gotlib IH. Depressive rumination, the default‐mode network, and the dark matter of clinical neuroscience. Biological Psychiatry 2015; Vol. 78, issue 4:224‐30. [DOI: 10.1016/j.biopsych.2015.02.020] [DOI] [PMC free article] [PubMed]
Hays 1995
- Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K. Functioning and well‐being outcomes of patients with depression compared with chronic general medical illnesses. Archives of General Psychiatry 1995;52:11‐9. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hopton 2012
- Hopton AK, Curnoe S, Kanaan M, Macpherson H. Acupuncture in practice: mapping the providers, the patients and the settings in a national cross‐sectional survey. BMJ Open. England, 2012; Vol. 2, issue 1:e000456. [2044‐6055] [DOI] [PMC free article] [PubMed]
Hou 2016
- Hou Z, Jiang W, Yin Y, Zhang Z, Yuan Y. The current situation on major depressive disorder in China: research on mechanisms and clinical practice. Neuroscience Bulletin 2016; Vol. 32, issue 4:389‐97. [DOI: ] [DOI] [PMC free article] [PubMed]
Huang 2012
- Huang W, Pach D, Napadow V, et al. Characterizing acupuncture stimuli using brain imaging with FMRI ‐ a systematic review and meta‐analysis of the literature. PLoS One 2012;7(4):e32960. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jorm 1997
- Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy: a survey of the public's ability to recognise mental disorders and their belief about the effectiveness of treatment. Medical Journal of Australia 1997;166:182‐6. [DOI] [PubMed] [Google Scholar]
Jorm 2000
- Jorm AF, Medway J, Christensen H, Korten AE, Jacomb PA, Rodgers B. Public beliefs about the helpfulness of interventions for depression: effects on actions taken when experiencing anxiety and depression symptoms. Australia and New Zealand Journal of Psychiatry 2000;34:619‐26. [DOI] [PubMed] [Google Scholar]
Kessler 2000
- Kessler RC, Soukup J, Davis RB. The use of complementary and alternative therapies to treat anxiety and depression in the Unites States. American Journal of Psychiatry 2000;158:289‐94. [DOI] [PubMed] [Google Scholar]
Kessler 2003
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas MR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS‐R). JAMA 2003;289:3095‐105. [DOI] [PubMed] [Google Scholar]
Kessler 2007
- Kessler RC, Merikangas KR, Wang PS. Prevalence, comorbidity and service utilisation for mood disorders in the United States at the Beginning of the twenty first century. Annual Review of Clinical Psychology 2007;3:137‐58. [DOI] [PubMed] [Google Scholar]
Kirsch 2008
- Kirsch I, Deacon BJ, Huedo‐Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and anti‐depressant benefits: a meta‐analysis of data submitted to the Food and Drug Administration. PLoS Medicine 2008;5(2):260‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Langevin 2015
- Langevin H, Schnyer R, MacPherson H, Davis R, Harris RE, Napadow V, et al. Manual and electrical needle stimulation in acupuncture research: pitfalls and challenges of heterogeneity. Journal of Alternative and Complementary Medicine 2015; Vol. 21, issue 3:113‐28. [1557‐7708] [DOI] [PMC free article] [PubMed]
Leo 2007
- Leo RJ, Ligot JS Jr. A systematic review of randomized controlled trials of acupuncture in the treatment of depression. Journal of Affective Disorders 2007;97:13‐22. [DOI] [PubMed] [Google Scholar]
Leung 2014
- Leung MC, Yip KK, Ho YS, et al. Mechanisms underlying the effect of acupuncture on cognitive improvement: a systematic review of animal studies. Journal of Neuroimmune Pharmacology 2014;9(4):492‐507. [DOI] [PubMed] [Google Scholar]
Lin 2016
- Lin Y‐J, Kung Y‐Y, Kuo W‐J, Niddam DM, Chou C‐C, Cheng C‐M, et al. Effect of acupuncture ‘dose’ on modulation of the default mode network of the brain. Acupuncture in Medicine 2016; Vol. 34, issue 6:113‐28. [DOI] [PMC free article] [PubMed]
Liu 2009
- Liu P, Qin W, Zhang Y, et al. Combining spatial and temporal information to explore function‐guide action of acupuncture using fMRI. Journal of Magnetic Resonance Imaging 2009;30:41‐6. [DOI] [PubMed] [Google Scholar]
MacPherson 2004
- MacPherson H, Scullion A, Thomas KJ, et al. Patient reports of adverse events associated with acupuncture treatment: a prospective national survey. Quality and Safety in Health Care 2004;13:349‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mayor 2013
Melchart 2004
- Melchart D, Weidenhammer W, Streng A, Reitmayr S, Hoppe A, Ernst E, et al. Prospective investigation of adverse effects of acupuncture in 97,733 patients. Archives of Internal Medicine 2004;164(1):104‐5. [DOI] [PubMed] [Google Scholar]
Montgomery 1979
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry 1979;134:382‐9. [DOI] [PubMed] [Google Scholar]
Mukaino 2005
- Mukaino Y, Park J, White A, Ernst E. The effectiveness of acupuncture for depression: a systematic review of randomised controlled trials. Acupuncture in Medicine 2005;23(2):70‐6. [DOI] [PubMed] [Google Scholar]
Murray 1996
- Murray CJ, Lopez AD. The Global Burden of Disease. Geneva: World Health Organization and Harvard University Press, 1996. [Google Scholar]
Napadow 2005
- Napadow V, Makris N, Liu J, et al. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by MRI. Human Brain Mapping 2005;24:193‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2002
- Park J, White A, Stevinson C, et al. Validating a new non‐penetrating sham acupuncture device: two randomised controlled trials. Acupuncture in Medicine 2002;20(4):168‐74. [DOI] [PubMed] [Google Scholar]
Revman 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5) Version 5.3. Cophenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robinson 2012
Spitzer 1977
- Spitzer RL, Endicott J, Robins E. Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders. 3rd Edition. New York, NY: Biometric Research, 1977. [Google Scholar]
Spitzer 1995
- Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JB, deGruy FV 3rd, et al. Health‐related quality of life in primary care patients with mental disorders. Results from the PRIME‐MD 1000 study. JAMA 1995;274:1511‐7. [PubMed] [Google Scholar]
Spitzer 1999
- Spitzer RL, Kroenke K, Williams JBW. Patient Health Questionnaire Study Group. Validity and utility of a self‐report version of PRIME‐MD: the PHQ Primary Care Study. JAMA 1999;282:1737‐44. [DOI] [PubMed] [Google Scholar]
Streitberger 1998
- Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352:364‐5. [DOI] [PubMed] [Google Scholar]
Thomas 2003
- Thomas C, Morris S. Cost of depression among adults in England in 2000. British Journal of Psychiatry 2003;183:154‐9. [DOI] [PubMed] [Google Scholar]
Vincent 2001
- Vincent C. The safety of acupuncture. BMJ 2001;323:4467‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2008
- Wang H, Qi H, Wang BS, Cui YY, Zhu L, Rong ZX, Chen HZ. Is acupuncture beneficial in depression: a meta analysis of 8 randomized controlled trials. Journal of Affective Disorders 2008;111(2‐3):125‐34. [DOI] [PubMed] [Google Scholar]
Ware 1994
- Ware JE, Kosinski M, Keller SD. SF‐36 Physical and Mental Health Summary Scales: A User Manual. Boston, MA: Health Institute, New England Medical Centre, 1994. [Google Scholar]
Wells 1989
- Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, et al. The functioning and well being of depressed patients: results from the Medical Outcomes Study. JAMA 1989;262:914‐9. [PubMed] [Google Scholar]
White 2001
- White A, Hayhoe S, Hart A, et al. Survey of adverse events following acupuncture (SAFA): a prospective study of 32,000 consultations. Acupuncture in Medicine 2001;19:84‐92. [DOI] [PubMed] [Google Scholar]
White 2004
- White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupuncture in Medicine 2004;22(3):122‐33. [DOI] [PubMed] [Google Scholar]
WHO 1993
- World Health Organization. The ICD‐10 Classification of Mental and Behavioural Disorders. Diagnostic Criteria for Research. Geneva, Switzerland: World Health Organization, 1993. [Google Scholar]
WHO 1998
- World Health Organization. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Social Science and Medicine 1998;46:1569‐85. [DOI] [PubMed] [Google Scholar]
Witt 2009
- Witt CM, Pach D, Brinkhaus B, Wruck K, Tag B, Mank S, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forschende Komplementarmedizin 2009;16(2):91‐7. [DOI] [PubMed] [Google Scholar]
Woo 2014
- Woo JM, Park EJ, Lee M, Ahn M, Kwon S, Koo KH. Changes in attitudes toward and patterns in traditional Korean medicine among the general population in South Korea: a comparison between 2008 and 2011. BMC Complementary and Alternative Medicine 2014; Vol. 14:436. [DOI: 10.1186/1472-6882-14-436] [DOI] [PMC free article] [PubMed]
Zhang 2010
- Zhang ZJ, Chen HY, Yip K, Ng R, Wong VT. The effectiveness and safety of acupuncture therapy in depressive disorders: systematic review and meta‐analysis. Journal of Affective Disorders 2015;124:9‐21. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Smith 2005
- Smith CA, Hay PP, M Arnold. Acupuncture for depression. Cochrane Database of Systematic Reviews 2003. [DOI: 10.1002/14651858.CD004046] [DOI] [PubMed] [Google Scholar]


