Supplemental Digital Content is available in the text.
Abstract
Introduction:
Bowel and bladder dysfunction (BBD) is a common pediatric condition that describes a constellation of lower urinary tract symptoms (LUTS) associated with constipation. Many children with BBD have comorbid neuropsychiatric and psychosocial concerns that are not routinely assessed. The aim of quality improvement (QI) was to establish a comprehensive assessment for BBD by developing and evaluating (1) a standardized clinician assessment form and (2) parent-reported questionnaire.
Methods:
From July 2017 to April 2018, a prospective QI study was conducted in the BBD network. A standardized assessment form was developed based on literature review and expert opinions, with targeted sections for LUTS, constipation, and psychosocial history. Before clinic, families of children referred for BBD were given a questionnaire to clarify voiding, stooling, and dietary patterns. Physicians utilized the assessment form for new referrals. Afterward, both physicians and parents evaluated the assessment process anonymously.
Results:
A total of 15 physicians and 45 parents responded, with 67% of patients being between 4 and 10 years old and 51% male. Physicians responded that the assessment form reminded them to ask about specific LUTS (93%), constipation (87%), and psychosocial history (87%). Parents responded positively by agreeing that they felt included in care decisions (96%) and had questions answered appropriately (100%). Only 47% found the previsit package easy to complete.
Conclusions:
In pediatric BBD consultations, a standardized assessment form can guide clinicians to efficiently gather a comprehensive history and screen for psychosocial risk factors. It can empower more pediatricians to evaluate BBD in the future.
INTRODUCTION
Background
Bowel and bladder dysfunction (BBD) is a common yet underdiagnosed condition that describes a spectrum of lower urinary tract symptoms (LUTSs) associated with constipation, with or without encopresis.1 LUTSs include dysuria, urgency, daytime incontinence, enuresis, urinary retention, and straining. Although the cause of BBD is multifactorial, nonbiological factors including stressful or adverse life events, such as parental separation and abuse, have been well associated with BBD.2,3 There is also known correlation between BBD and neuropsychiatric symptoms, such as inattention, hyperactivity, and anxiety.4 The stigma associated with BBD symptoms may negatively impact the self-esteem and quality of life of patients and their families, and further, hinder their adherence to treatment recommendations.5
Problem Identified
BBD represents up to 40% of pediatric urology consults, with long wait times of up to a year for consultation in tertiary centers.6 Most children with BBD will improve with conservative management, such as bladder retraining and constipation treatment.1 As most BBD-related issues are functional, most children are best initially evaluated by a general pediatrician, with referral to a pediatric urologist in severe or refractory cases. Unfortunately, many general clinicians are uncomfortable with the initial assessment of BBD patients. Due to an even fewer number of pediatric urologists, long wait times are homogeneous among pediatric urology centers across Canada, with wait times averaging between 6 months and 1 year for consultations.
With a specific aim to improve access to quality care and reduce wait times for children with BBD, a unique and collaborative network was developed by the Urology Division at the Hospital for Sick Children (HSC) and a group of general pediatricians in the Greater Toronto Area (GTA) in Canada in 2016.7,8 Based on central triage and support from the HSC Urology team, patients referred for BBD can be seen across 8 pediatric community sites. Since initiation in June 2016, the BBD network has seen over 1,000 patients. Although the network has standardized the management approach through the use of common educational materials and following treatment guidelines,1,9,10 there is a lack of standardized approach and method in the initial assessment of BBD between sites. In assessing urinary and constipation history, patient-recorded symptom diaries have been found in prior studies to be more accurate and efficient in the gathering of LUTS history compared with direct recall in the clinical visit.11,12 Given the complexity of BBD referrals, comprehensive initial assessment, specifically for the presence of neuropsychiatric symptoms and psychosocial risk factors, has not been evaluated. There is presently no standardized published questionnaire nor assessment form for the clinical evaluation of BBD.
Aims
The primary aim of this quality improvement (QI) project is to develop and evaluate a standardized comprehensive clinician assessment form for patients with BBD. The assessment form includes a guided clinical history with specific screening questions for psychosocial risk factors and neuropsychiatric symptoms, along with a physical examination checklist. Second, we aim to improve the efficiency and accuracy of BBD consultations through implementing a previsit questionnaire that collects information on patients’ dietary habits, fluid intake, voiding, and stooling patterns. Ultimately, we aim to empower pediatricians to perform efficient and thorough assessments of BBD in the community.
METHODS
Clinical Setting
The HSC QI Review Board reviewed and approved the study before initiation. The QI study took place in the GTA BBD network, which includes the HSC pediatric urology department and 8 pediatric community sites. Referrals to the BBD network generally arise from primary care providers in the GTA catchment, such as family physicians and general pediatricians. After a referral is made to the network, it is triaged to be seen by a BBD network–affiliated physician based on the patient’s geographical location within the GTA.
Intervention
Two interventions for BBD assessment were developed based on a review of literature and consultation with local experts. These were (1) a standardized clinician assessment form and (2) a parent-reported previsit questionnaire. The standardized clinician assessment form included sections with questions to target LUTS, constipation, diet, medical history, neuropsychiatric symptoms, psychosocial risk factors, and a physical examination checklist for neurologic red flags (BBD Clinician Assessment Form, Supplemental Digital Content, available at http://links.lww.com/PQ9/A72). The parent-reported previsit questionnaire included 4 sections: voiding symptoms, 7-day voiding diary, stool patterns, and dietary/fluid intake (Previsit Questionnaire, Supplemental Digital Content, available at http://links.lww.com/PQ9/A73). Specifically, the dysfunctional voiding scoring system was used to assess baseline dysfunctional voiding symptoms and parental report of stressful events.13 Stool history was assessed using the Bristol stool scale.14 The clinician assessment form and previsit questionnaire were both pilot-tested for usability.
QI Study Design
The study was conducted between July 2017 and April 2018, with recruitment procedures shown in Figure 1. Approximately 1 month before the first clinic visit, families of newly referred patients for BBD were mailed a previsit questionnaire and were reminded to bring the completed form to the clinic. If they did not bring in the form, they were given one in the clinic to fill out while waiting for the appointment. All GTA BBD network–affiliated physicians (from the 8 community sites) were invited to participate in the QI project voluntarily. A standardized assessment form was subsequently provided to participants. On the day of the clinic appointment, physicians were asked to review the patient’s completed previsit questionnaire and utilize the standardized assessment form during their consultation. At the end of the clinic visit, both physicians and parents were given anonymous experience surveys to evaluate their perspectives of the assessment process and previsit or assessment forms. Following the QI data collection period, the assessment forms were refined through 3 extensive reviews based on feedback from patients and physicians.
Fig. 1.
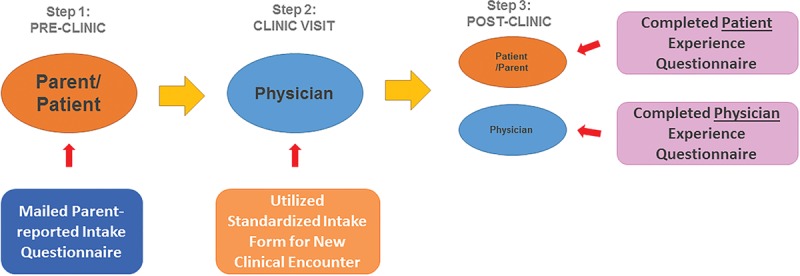
Study design and process of QI intervention.
Data Collection and Analysis
The physician experience survey included 3 sections: patient visit information, assessment form feedback, and overall experience. Physicians provided basic visit information such as site, estimated duration of the appointment, and, if any, parental previsit questionnaires that were utilized during the consultation. Next, physicians were asked specific questions regarding clarity and utility of the assessment form using a 6-point Likert scale (from strongly agree, agree, neither, disagree, strongly disagree, and nonapplicable). Finally, they were asked to respond to a short-answer question on how the form can be improved and used a global rating scale (from 0 to 10) to rate their overall perception of supporting the implementation of a standardized BBD assessment form.
The patient experience survey included 3 sections; demographic information, coordination of care and education, and overall experience. Basic nonidentifying demographic information was collected, such as age range and sex. Also, patients/parents were asked questions using a 6-point Likert scale on the coordination of appointment and information received. Finally, they were asked to provide written feedback on how the visit could be improved and used a global rating scale to rate their likelihood of recommending the BBD network to a friend or family member.
Statistical analysis was completed using SPSS 23 (IBM, Armonk, NY, United States of America). In data analysis, from the 6-point Likert scale, strongly agree and agree were categorized as responding “agree,” and disagree and strongly disagree were categorized as responding “disagree.”
RESULTS
A total of 15 physicians from 5 BBD network sites responded to the experience survey after using the BBD assessment form, including 2 pediatric urologists and 13 general pediatricians. A total of 45 patients/parents from 3 network sites completed the experience survey after their clinic visit. The majority of patients (67%) were between 4 and 10 years old at the time of the first consultation, 24% were between 11 and 17 years old, and 9% were younger than 4 years old. Further, 51% were male, and 49% were females.
Physician Experience
Using the assessment form, the median time spent for each new BBD consultation was 45 minutes (interquartile range, 15; lower limit is 30 minutes, and upper limit is 60 minutes), compared with previously BBD physician-reported time of 60–90 minutes per visit. Participants (93% of physicians) agreed that the assessment form reminded them to ask specific questions on history about urinary symptoms. Also, 87% of physicians agreed that the assessment form reminded them to ask specific questions about constipation and psychosocial history. Further, 40% of physicians agree that the form reminded them to perform specific parts of the physical examination. Overall, 90% of physicians agreed that they would use the assessment form again and on average rated 7.6 out of 10 (SD, 1.7) in support of implementing the standardized assessment forms in the BBD network. Written feedback varied but generally included suggestions on formatting such as shortening the form, changing the specific wording of questions, and including more blank space for writing.
Patient Experience
Before the visit, although 84% of parents agreed that the scheduling process to book the appointment was smooth, 42% had to wait a long time for the visit. All parents (100%) agreed that physicians adequately answered their questions during the visit, and 96% agreed that physicians clearly explained the treatment plan to them and that they felt included in care decisions. Only 47% of parents found the previsit questionnaire easy to complete before the clinic. Some commented that the voiding diary was particularly difficult to fill out and hard to keep track of voids. Overall, parents rated 9.3 out of 10 (SD, 1.3) that they would recommend the BBD network. Many parents stated that they were satisfied with their appointment, but several commented about the need to decrease wait time.
DISCUSSION
In the evaluation of BBD, a standardized assessment form helped guide physicians to gather a comprehensive medical history and complete documentation in an efficient manner. The most useful aspect of the BBD assessment form was the reminder to ask about urinary symptoms. The BBD assessment form has 1 page dedicated to urinary symptoms including voiding patterns, LUTS, urinary tract infections, daytime incontinence, and nocturnal enuresis. Based on recent unpublished data from a provincial survey of pediatricians, urinary problems have been identified as an area of weakness in clinical competency (J. Dos Santos, MD, email communication, June 2017). Using the Miller’s Pyramid learning model in assessing clinical competency, the first 2 stages of “know” and “know how” involve knowledge transmission and application.15 In BBD clinical encounters, the standardized clinician assessment form has been shown to increase self-reported knowledge in asking appropriate questions during visits. It has the potential to help learners progress through these first 2 knowledge stages as an education tool in professional development and in teaching medical trainees. Following Miller’s Pyramid, the third stage of “shows how” involves demonstrating learning in practice settings, and the final stage “does” apply to integration into practice.15 Although physicians in this study were not directly observed nor evaluated for the upper 2 stages in their clinical assessments, using the assessment form did help to indirectly improve performance efficiency in reducing the time spent for visits by 15–30 minutes. Consistent use of the BBD assessment form has the potential to enable greater clinical capacity and subsequently reduce wait times ultimately.
A significant proportion (87%) of physicians were reminded through the assessment form to ask about details regarding psychosocial history. It is critical to identify nonbiological determinants of health, such as personal, familial, and environmental factors, as they are known to impact the severity and outcome of BBD.2,16 The majority of physicians were also reminded by the assessment form to ask about details of constipation and specific prior treatments tried. Gaining a thorough understanding of both above clinical histories is essential in the management of BBD, as behavioral modifications through bladder retraining and constipation treatment are first-line strategies.1,17 As such, using the BBD assessment form can help physicians to gain situational awareness of the individual patient and psychosocial concerns. Future research can explore whether or not management strategies are affected as a result of changes in assessment.
Also, 40% of physicians responded that the assessment form reminded them to perform specific parts of the physical examination. Neurological examination and careful inspection for spinal anomalies, such as a sacral dimple or hair tuft, are crucial to exclude an underlying neurologic cause of BBD.18 Performing a genital examination can help to identify anatomical urinary tract anomalies such as ectopic ureter19 and evaluate for sexual abuse as potential causes for voiding dysfunction.20 The BBD physical examination checklist helps guide physicians through a detailed assessment to rule out important red flags that may delay the proper diagnosis if not otherwise identified.
Although most parents were satisfied with the BBD clinic visit, long wait time was the most negative aspect of the experience. However, wait time for BBD referrals before the BBD network ranged from 6 months to 1 year. Currently, it has since been reduced to approximately 1–2 months. Nonetheless, healthcare capacity for BBD assessment remains an important barrier to patient access to time-sensitive care and may be secondary to systemic and training factors. Common conditions in the BBD spectrum including voiding postponement, urge incontinence, and dysfunctional voiding are recommended to be initially treated and followed by the primary care practitioner or general pediatrician.1,6 However, most BBD cases are directly sent to pediatric urologists with long wait times.1 Future medical education and standardization of BBD consultations, such as through using a clinician assessment form, have the potential to empower more general pediatricians to be comfortable, thorough, and efficient with evaluating BBD.
Only about half of the parents found the preclinic package easy to complete, as many cited difficulties filling out the voiding diary. Although the voiding diary is an important diagnostic tool for determining the type and severity of urinary symptoms, the process of filling out a voiding diary has been recognized as a burden for families and may result in incomplete or inaccurate diaries.21 Utilizing a different mode of data entry, such as electronic diaries, can be helpful in increasing compliance, as seen in other pediatric populations with chronic pain.22 Mobile voiding tracking devices have further been evaluated in adult urology patients with improved sensitivity in results.23,24 To date, there has only been 1 pediatric study evaluating the feasibility of a mobile voiding diary for LUTS, which showed nonsuperiority in comparison to a paper diary.25 Given the overall advantages of electronic diaries in other populations and pervasiveness of mobile devices,26 further evaluation of electronic voiding diaries is needed in the pediatrics BBD population because it has the potential to improve data quality.
This QI study is the first to develop and evaluate a clinician assessment form for BBD. Given the overall positive global rating score supporting the implementation of a standardized BBD assessment form, this is a future direction for the BBD network. Based on physician users’ feedback, the assessment form has been refined and can be distributed in the pediatrics community and beyond through online format. Several proposed models of integration are being considered, such as through paper format or incorporation into electronic medical records (EMRs).27 In an EMR system, users can add the BBD assessment form as a template. Further, if the patient’s previsit questionnaire can also be securely collected electronically, it could be integrated directly into the EMR upon completion, summarized and available for clinical review during the encounter. Future aims in the BBD network will involve evaluating clinical competence and assessing whether patient outcomes are improved in this novel model of care.
CONCLUSIONS
Implementation of a standardized assessment form for pediatric BBD can help guide clinicians to efficiently gather a comprehensive medical history, specifically for urinary symptoms and psychosocial factors, and rule out red flags on physical examination. With further education of the clinical approach and management of BBD, it has the potential to empower more general pediatricians to evaluate and manage BBD in the future.
ACKNOWLEDGMENTS
The authors thank Megan Saunders for assistance with the study.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online March 27, 2019.
Poster presentation at Canadian Paediatrics Society Meeting, May 30, 2018, Quebec City, Toronto, Ontario, Canada.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Wang R, Kanani R, El Bardisi Y, Mistry N, Dos Santos J. Development of a Standardized Approach for the Assessment of Bowel and Bladder Dysfunction. Pediatr Qual Saf 2019;2:e144.
REFERENCES
- 1.Dos Santos J, Lopes R, Koyle M. Bladder and bowel dysfunction in children: an update on the diagnosis and treatment of a common, but underdiagnosed pediatric problem. CUAJ. 2017;11:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Logan BA, Correia K, McCarthy J, et al. Voiding dysfunction related to adverse childhood experiences and neuropsychiatric disorders. J Pediatr Urol. 2014;10:634–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.von Gontard A. Does psychological stress affect LUT function in children? ICI-RS 2011. Neurourol Urodyn. 2012;31:344–348. [DOI] [PubMed] [Google Scholar]
- 4.Wolfe-Christensen C, Veenstra AL, Kovacevic L, et al. Psychosocial difficulties in children referred to pediatric urology: a closer look. Urology. 2012;80:907–912. [DOI] [PubMed] [Google Scholar]
- 5.Van Herzeele C, Dhondt K, Roels SP, et al. Neuropsychological functioning related to specific characteristics of nocturnal enuresis. J Pediatr Urol. 2015;11:208.e1–208.e6. [DOI] [PubMed] [Google Scholar]
- 6.Dos Santos J, Varghese A, Williams K, et al. Recommendations for the management of bladder bowel dysfunction in children. Pediatr Ther. 2014;4:191. [Google Scholar]
- 7.Ming J, Rockman R, Mistry N, et al. Improving the management of bladder and bowel dysfunction in children. Paper presented at: 68th Annual Meeting of the Northeastern Section of the American Urological Association; September 29, 2016; Buffalo, N.Y Available at http://www.abstractsonline.com/pp8/#!/4174/presentation/115. Accessed September 25, 2018. [Google Scholar]
- 8.Dos Santos J, Rockman R, Mistry N, et al. P40: Improving the management of bladder and bowel dysfunction in children. Can Urol Assoc J. 2016; 10(9–10S4): S173. [Google Scholar]
- 9.SickKids – About Kids Health. Bladder retraining website. Available at https://www.aboutkidshealth.ca/Article?contentid=49&language=English. Updated July 9, 2009. Accessed July 15, 2018.
- 10.Issenman RM, Filmer RB, Gorski PA. A review of bowel and bladder control development in children: how gastrointestinal and urologic conditions relate to problems in toilet training. Pediatrics. 1999;103(6 Pt 2):1346–1352. [PubMed] [Google Scholar]
- 11.De Gennaro M, Niero M, Capitanucci ML, et al. Validity of the international consultation on incontinence questionnaire-pediatric lower urinary tract symptoms: a screening questionnaire for children. J Urol. 2010;184(4 Suppl):1662–1667. [DOI] [PubMed] [Google Scholar]
- 12.Nevéus T, Gontard A, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the standardization committee of the International Children’s Continence Society (ICCS). Neurourol Urodyn. 2006;26:90–102. [DOI] [PubMed] [Google Scholar]
- 13.Farhat W, Bägli DJ, Capolicchio G, et al. The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol. 2000;164(3 Pt 2):1011–1015. [DOI] [PubMed] [Google Scholar]
- 14.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920–924. [DOI] [PubMed] [Google Scholar]
- 15.Wass V, Van der Vleuten C, Shatzer J, et al. Assessment of clinical competence. Lancet. 2001;357:945–949. [DOI] [PubMed] [Google Scholar]
- 16.Martins G, Minuk J, Varghese A, et al. Non-biological determinants of paediatric bladder bowel dysfunction: a pilot study. J Pediatr Urol. 2016;12:109.e1–109.e6. [DOI] [PubMed] [Google Scholar]
- 17.Yagci S, Kibar Y, Akay O, et al. The effect of biofeedback treatment on voiding and urodynamic parameters in children with voiding dysfunction. J Urol. 2005;174:1994–1997; discussion 1997. [DOI] [PubMed] [Google Scholar]
- 18.Sutherland RS, Mevorach RA, Baskin LS, et al. Spinal dysraphism in children: an overview and an approach to prevent complications. Urology. 1995;46:294–304. [DOI] [PubMed] [Google Scholar]
- 19.Heuser M, Zöller G, Seseke F, et al. Bladder dysfunction in children with bilateral single ectopic ureters. J Pediatr Surg. 2002;37:15–17. [DOI] [PubMed] [Google Scholar]
- 20.Ellsworth PI, Merguerian PA, Copening ME. Sexual abuse: another causative factor in dysfunctional voiding. J Urol. 1995;153(3 Pt 1):773–776. [PubMed] [Google Scholar]
- 21.Tincello DG, Williams KS, Joshi M, et al. Urinary diaries: a comparison of data collected for three days versus seven days. Obstet Gynecol. 2007;109(2 Pt 1):277–280. [DOI] [PubMed] [Google Scholar]
- 22.Palermo TM, Valenzuela D, Stork PP. A randomized trial of electronic versus paper pain diaries in children: impact on compliance, accuracy, and acceptability. Pain. 2004;107:213–219. [DOI] [PubMed] [Google Scholar]
- 23.Pereira-Azevedo N, Carrasquinho E, Cardoso de Oliveira E, et al. mHealth in urology: a review of experts’ involvement in app development. PLoS One. 2015;10:e0125547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quinn P, Goka J, Richardson H. Assessment of an electronic daily diary in patients with overactive bladder. BJU Int. 2003;91:647–652. [DOI] [PubMed] [Google Scholar]
- 25.Johnson EK, Estrada CR, Johnson KL, et al. Evaluation of a mobile voiding diary for pediatric patients with voiding dysfunction: a prospective comparative study. J Urol. 2014;192:908–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johansen MA, Berntsen GK, Schuster T, et al. Electronic symptom reporting between patient and provider for improved health care service quality: a systematic review of randomized controlled trials. part 2: methodological quality and effects. J Med Internet Res. 2012;14:e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen-Silver J, Laher N, Freeman S, et al. Family fIRST, an interactive risk screening tool for families in a school-based pediatric clinic. Clin Pediatr (Phila). 2017;56:217–225. [DOI] [PubMed] [Google Scholar]


