Abstract
To clarify dynamic change of quality of life (QOL) in patients with stroke after treatment, and to explore the predictors associated with return to work (RTW) within 48 weeks.
Patients diagnosed with stroke were enrolled. All patients enrolled were asked to fill in the Short Form 36 Health Survey. For patients with stroke, SF-36 questionnaires were measured repeatedly 4 weeks after treatment. We used phone call to find out if the patient was RTW. The investigation time was 48 weeks.
Patients with stroke had lower scores in terms of physiological dimensions, such as physical functional, role limitations due to physical problems, and general health (P < .001). While patients with strokes scored significantly lower in all mental dimensions including vitality, social functioning, role limitations due to emotional problems, and mental health (P < .001). After 4-weeks treatment, we found that, except for bodily pain, scores in dimensions like physical functioning, role limitations due to physical problems, and general health had increased significantly (P < .001). Multivariate logistic regression analysis was conducted, and the result showed that older age (P = .04) and singleness (P = .03) were risk factors associated with QOL improvement in stroke patients after treatment. Outcomes of stroke patients within 48 weeks were explored. The results showed that 108 out of 136 patients RTW within 48 weeks. Average days it took for patients with cerebral infarction to return to work were 77 ± 79, significantly less than patients with cerebral hemorrhage (206 ± 159 days) and patients with subarachnoid hemorrhage (117 ± 113 days, P < .001). Multivariate analysis indicated that only QOL improvement (P = .04) and subtype of stroke (P = .01) were independent factors associated with RTW within 48 weeks.
QOL of stroke patients was significantly reduced. After treatments, the physiological quality of stroke patients increased, but the psychological quality remained low. In addition, patients with cerebral hemorrhage and patients with no significant improvement in QOL are independent risk factors for RTW. Therefore, for this subgroup of the population, early diagnosis, close follow-up and monitor of the psychological state should be provided to avoid the occurrence of adverse events.
Keywords: psychological state, quality of life, return to work, risk factor, stroke
1. Introduction
Cerebrovascular disease is one of the main heath issues that affect the life expectancy worldwide.[1] At least 7 million people in China suffer from stroke annually.[2,3] The morbidity and recurrence rate of stroke is high. With the increase of aging population in China, cardiovascular and cerebrovascular diseases, including stroke, are becoming the main causes of death.[2–5] Patients with stroke bring about physical, psychological, social and economic burdens, and health related quality of life (QOL) of the patients are low.[6–8]
Despite the remarkable progression in the treatment of stroke, the life quality and social-related events caused by stroke received limited attentions. Most studies have shown that the QOL in stroke patients were decreased.[9–11] However, there is still no report about the dynamic change of QOL in patients with stroke after treatment. Chronic diseases, such as stroke, are related to deteriorated QOL.
Another important issue is the related social event caused by stroke. The direct cost of strokes is medical care services and the indirect cost includes loss of productivity, which imposes huge personal and societal healthcare burdens. Therefore, it is becoming more and more important for patients to be able to return to work (RTW) after strokes.[12,13] The RTW is an important stroke-related outcome in occupations.
Hence, the purpose of this study is to clarify the dynamic change of QOL in patients with stroke after treatment, and to explore the predictors associated with RTW within 48 weeks. Our study may help to increase QOL in patients with stroke and improve health care policies to provide greater support for stroke survivors and their families.
2. Subjects and methods
2.1. Subjects
Patients diagnosed with stroke were enrolled in our center. A total of 86 people who underwent a physical examination at the same time were selected as healthy controls.
There were 3 subtypes of strokes, including cerebral infarction, cerebral haemorrhage, and subarachnoid hemorrhage. All patients enrolled had full-time job before diagnosis. Exclusion criteria were: drug taker or heavy alcohol abusers or patients with other illnesses (e.g., psychiatric diagnosis) that could affect the possibility of RTW. The Institutional Review Board of The Affiliated Yantai Yuhuangding Hospital of Qingdao University Institution had approved the study. Sociodemographic information, such as gender, age, ethnicity, education level, and income were collected. The information about job before stroke, including company size, company area, and occupational type (desk worker or manual worker), were also recorded.
2.2. Follow-up
All patients enrolled were asked to fill in the Short Form 36 Health Survey (SF-36). For patients with stroke, the SF-36 questionnaire was measured twice in total (before treatment and after 4 weeks of treatment). We analyses the changes in quality of life by comparing the results of the SF-36 questionnaire before and after treatment. The patients enrolled were received physical therapy. All of the subjects finished the questionnaires in a quiet room without any disruptions. They could get help from professional staff if they had problem in understanding the questions. We used phone call to find out if the patient was RTW. The investigation time was 48 weeks. The patient was told to inform the investigator by phone when they RTW. If the patients did not tell if they had returned to work in 48 weeks after diagnosis, the investigator telephoned to ask about the specific situation.
2.3. Questionnaires
The SF-36 is a brief self-administered HRQoL instrument commonly used for patients with a variety of diseases.[14,15] It includes 8 items: physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH)). In addition, there are 2 summary measures: physical component summary (PCS) and mental component summary (MCS) scales. Higher scores mean better healthy conditions. The Chinese versions of SF-36 questionnaire were available and provided by the developer. The tool's validity and screening ability have been shown in various samples in China.[16]
2.4. Statistical analysis
Continuous variables were expressed as mean and standard deviation, and categorical variables were expressed as percentages. The Chi-square test and t test were applied to determine whether the results were statistically different. Univariate and multivariate analysis were used to explore the factor associated with outcomes. The statistical significance of all tests was set as P < .05 by 2-tailed tests. Data analyses and quality control procedures were performed using SPSS for Windows, version 13.0 (SPSS Inc. 233 South Wacker Drive, 11th Floor, Chicago).
3. Results
3.1. Demographic data and QOL in stroke patient
A total of 136 patients and 86 health controls were included in this study and all of the participants had completed the SF-36 questionnaire. The characteristics of the subjects were shown in Table 1. No significant differences were found between the 2 groups in terms of gender, age, marital status, education level, and income level. We further compared the scores of QOL between the 2 groups of patients. We found that in the physical component summary and mental component summary, the healthy controls performed significantly better than the stroke patients. Patients with stroke had lower scores in terms of physiological dimensions, such as physical functional, role limitations due to physical problems and general health. Patients with strokes scored significantly lower in all mental dimensions including vitality, social functioning, role limitations due to emotional problems, and mental health, as shown in Figure 1.
Table 1.
Characteristics of patients in stroke group and control group.
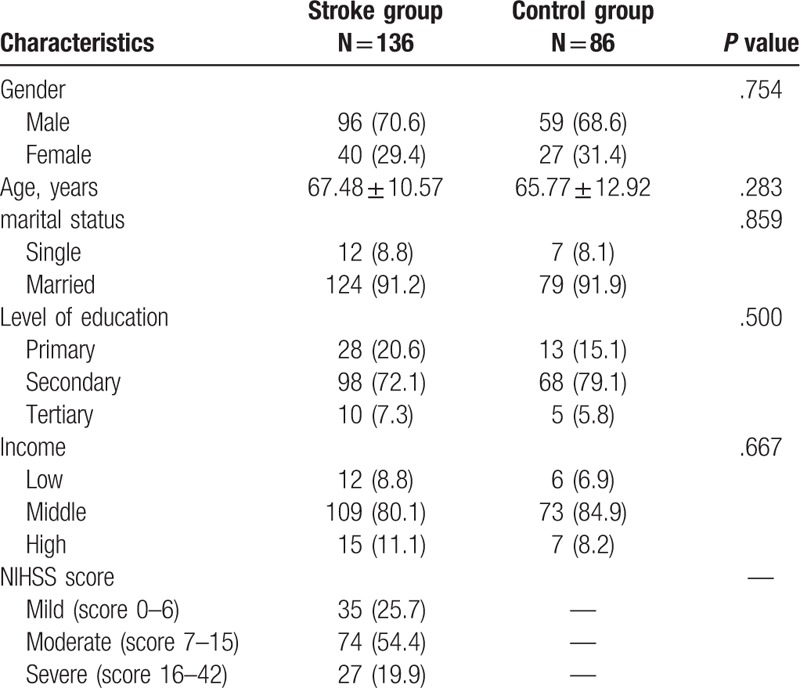
Figure 1.

SF-36 scores in stroke patients and controls. Patients with stroke had lower scores in terms of physiological dimensions, such as physical functional, role limitations due to physical problems and general health (P < .001). While patients with strokes scored significantly lower in mental dimensions including vitality, social functioning, role limitations due to emotional problems and mental health (P < .001). BP = bodily pain, ERF = emotional role functioning, GHP = general health perceptions, MH = mental health, PF = physical functioning, PFR = physical role functioning, SRF = social role functioning, VIT = vitality,.
3.2. Dynamic change of QOL in stoke patients after treatment
Four weeks after the treatment, we investigated the QOL of the stroke patients repeatedly. Interestingly, we found that at the physiological level, except for bodily pain, scores in dimensions like physical functioning, role limitations due to physical problems, and general health had increased significantly. This result demonstrated that the physiological aspect of the patient's QOL had improved. However, at the mental level, except for vitality, scores in dimensions including social functioning, role limitations due to emotional problems, and mental health did not show significant increases. The results were shown in Figure 2.
Figure 2.

SF-36 Scores for patient before and after treatment. We investigated the QOL of the stroke patients repeatedly 4 weeks after the treatment. We found that at the physiological level, except for bodily pain, scores in dimensions like physical functioning, role limitations due to physical problems and general health had increased significantly (P < .001). BP = bodily pain, ERF = emotional role functioning, GHP = general health perceptions, PF = physical functioning, PFR = physical role functioning SRF = social role functioning, MH = mental health, VIT = vitality.
3.3. Factors associated with QOL improvement after treatment
To explore the relationships between baseline characteristics and QOL improvement after intervention, the univariate analysis was performed and the result showed that age (P = .03) and marital status (P = .02) were the predictors for the life quality improvement. Furthermore, a multivariate logistic regression analysis was conducted and the result showed that older age (P = .04) and singleness (P = .03) were risk factors associated with QOL improvement in stroke patients after treatment (Table 2).
Table 2.
Factors associated with QOL improvement after treatment.

3.4. Outcomes of stoke patients within 48 weeks from diagnosis of stoke
The outcomes of 136 stroke patients enrolled within 48 weeks were explored. The results showed that 108 out of 136 patients returned to work within 48 weeks. Among them, 72 were from companies with <500 employees, 73 were from companies in rural areas and 39 were desk workers. Among those 108 who returned to work, 61 were diagnosed with cerebral infarction, 28 were diagnosed with cerebral hemorrhage and 19 were diagnosed with subarachnoid hemorrhage, as shown in Table 3.
Table 3.
Outcomes 48 weeks after initial day of diagnosis with stroke.
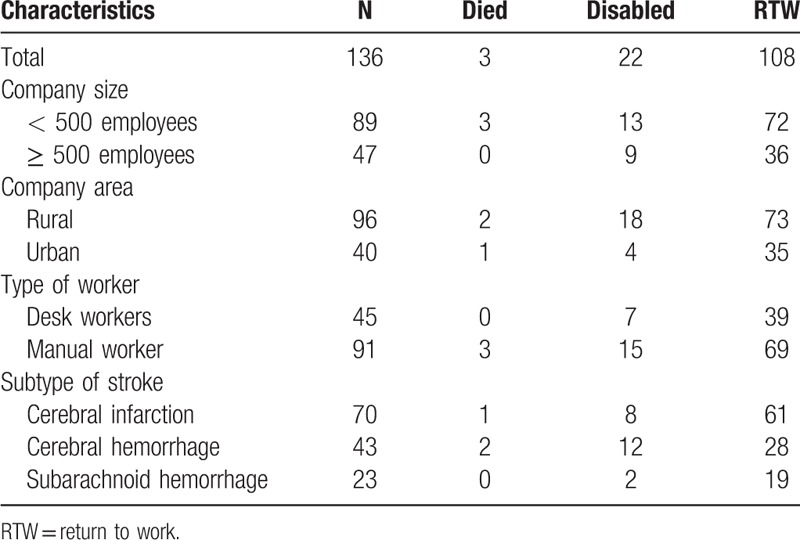
The days from diagnosis to RTW were also analyzed. Interestingly, the average days it took for patients with cerebral infarction to return to work were 77 ± 79, significantly less than patients with cerebral hemorrhage (206 ± 159 days) and patients with subarachnoid hemorrhage (117 ± 113 days, P < .001). The results were shown in Figure 3.
Figure 3.
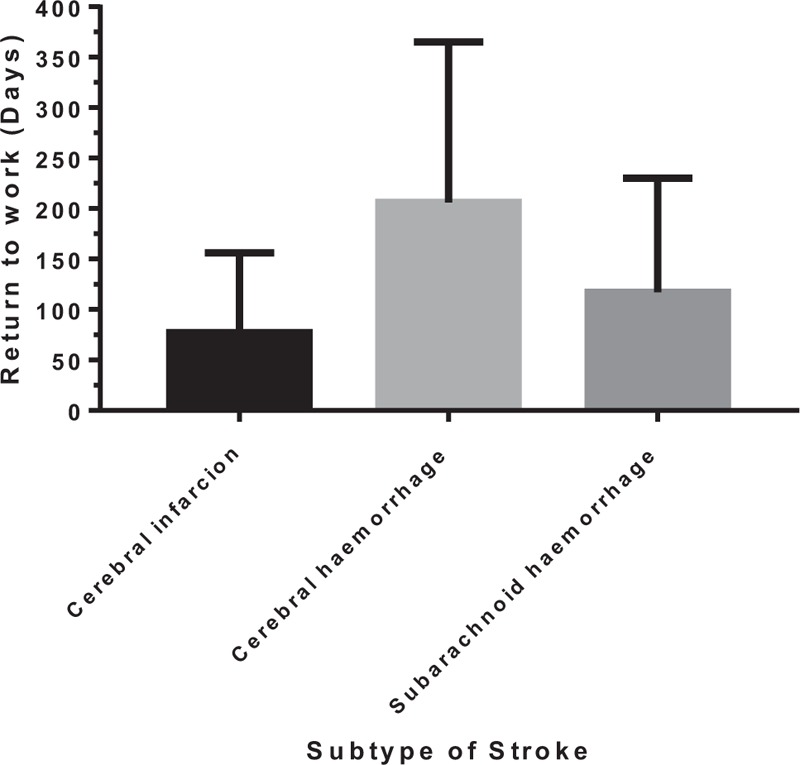
The days from diagnosis to RTW in stokes patients. The average days it took for patients with cerebral infarction to return to work were 77 ± 79 days, significantly less than patients with cerebral hemorrhage (206 ± 159 days) and patients with subarachnoid hemorrhage (117 ± 113 days, P < .001). RTW = return to work.
3.5. Factors associated with RTW in stroke patients after treatment
We further analyzed relationships between characteristics of patients and RTW within 48 weeks. The univariate analysis showed that QOL improvement at week 4 (P = .03), type of work (P = .03), and subtype of stroke (P = .01) were the predictors for RTW. While multivariate analysis indicated that only QOL improvement (P = .04) and subtype of stroke (P = .01) were independent factors associated with RTW within 48 weeks among stroke patients, as shown in Table 4.
Table 4.
Factors associated with return to work after treatment.

4. Discussion
In addition to suffering from a decline in QOL, patients with stroke are also prone to loss of productivity, which imposes both personal and social losses.[12] This is very common for patients with chronic diseases.[17–19] Previous studies have reported that chronic diseases, such as viral infections, metabolic diseases, and cardiovascular diseases, can cause a decline in the QOL of patients.[16,20,21] This study showed that the QOL of stroke patients was significantly lower than that of healthy controls. This is consistent with previous reports.[7,10] The study also found that after 4 weeks of treatment, although the physiological quality of the patients increased significantly, the patient's mental QOL did not show significant improvement. This suggests that in the clinical management of stroke patients, more attention should be paid to improving the psychological conditions of the patients. Stroke is a chronic condition that requires long-term management.[22,23] The lack of improvement in the psychological aspect of stroke patients will reduce patients’ compliance in the long term, which may lead to recurrence of the disease. The study also found that there was a significant difference in RTW rates among patients with different stroke types. The RTW rate of patients with cerebral infarction was significantly higher. Patients with cerebral infarction were more likely to return to work 4 weeks after treatment than patients with cerebral hemorrhage. To the best of our knowledge, this is the first study to report the predictive factors associated with RTW in China.
In this study, we found that there was no significant increase in QOL at the mental level after 4 weeks of treatment in stroke patients. Further multivariate analysis suggested that being single and older ages were factors associated with improvement of QOL. Previous reports suggest that age is closely related to the improvement of QOL.[24,25] The reason why the QOL of single patients do not improve significantly is an interesting question. It may be associated with the lack of family care and support for a single person. In addition, communication between people is also an effective way to improve emotional function. Family care and emotional support all contribute to improving the QOL of patients after stroke. In clinical practice, more emphasis should be placed on monitoring the QOL of stroke patients. Timely and psychological intervention is necessary for people at risk of having difficulty in improving QOL, especially for single and elderly patients. Chronic diseases like stroke requires long-term management, low quality of life, and poor psychological conditions can lead to decreased treatment compliance in patients, which in turn will lead to recurrence of stroke.[26–28] A study reported that effective psychological intervention can significantly reduce stress in stroke patients and increase adherence with treatment.[29,30] Therefore, psychological interventions are necessary for these high-risk groups in clinical practice.
Few studies have investigated the predictors of RTW in stroke patients and the differences in RTW rates among stroke subtypes. According to our study, patients with cerebral infarction are more likely to return to work, and they also return to work earlier. This is consistent with previous reports.[13,31] Study pointed out that patients with cerebral hemorrhage are often more prone to suffering from dysfunction than cerebral infarction.[32,33] We also found that the improvement in QOL 4 weeks after treatment was an independent predictor of RTW in patients. Since chronic disease needs regular follow-up and timely intervention.[34–36] The result suggests that patients who have not improved QOL 4 weeks after diagnosis may need to be closely monitored and psychological counseling should be considered. It may help to increase the likelihood of RTW within 48 weeks.
This article has some limitations. First, the sample size of this study is small, which may cause some bias. Secondly, all patients were enrolled from a single medical center. To explore the relationship between changes in the QOL of stroke patients and RTW, a prospective multicenter clinical study is warranted to confirm our results
In summary, this study found that the QOL of stroke patients was significantly reduced. The physiological quality of stroke patients increased, but the psychological quality remained low after treatments. Therefore, psychological monitoring and interventions are important in improving QOL for patients with stroke, especially for single and elderly patients. In addition, patients with cerebral hemorrhage and patients with no significant improvement in QOL are independent risk factors for RTW. Therefore, for this subgroup of the population, early diagnosis, close follow-up and monitor of the psychological state should be provided to avoid the occurrence of adverse events.
Author contributions
Conceptualization: Qi Chen, Li Gong, yanxiang zhang.
Data curation: Qi Chen, yanxiang zhang.
Formal analysis: Qi Chen, Chunni Cao.
Investigation: Qi Chen, Chunni Cao.
Methodology: Chunni Cao.
Project administration: Chunni Cao.
Software: Li Gong.
Supervision: Li Gong.
Validation: yanxiang zhang.
Writing – original draft: Li Gong, yanxiang zhang.
Writing – review & editing: yanxiang zhang.
Footnotes
Abbreviations: BP = bodily pain, GH = general health, MCS = mental component summary, MH = mental health, PCS = physical component summary, PF = physical functioning, QOL = quality of life, RE = role limitations due to emotional problems, RP = role limitations due to physical problems, RTW = return to work, SF = social functioning, SF-36 = Short Form 36 Health Survey, VT = vitality.
The Institutional Review Board of The Affiliated Yantai Yuhuangding Hospital of Qingdao University Institution had approved this study. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent was obtained from all patients for inclusion in the study.
All authors declare that they have no financial or personal relationships with other people or organizations that could inappropriately influence this work.
References
- [1].Paradise MB, Shepherd CE, Wen W, et al. Neuroimaging and neuropathology indices of cerebrovascular disease burden: a systematic review. Neurology 2018;91:310–20. [DOI] [PubMed] [Google Scholar]
- [2].Jiang J, Chen Y, Shi J, et al. Population attributable burden of Helicobacter pylori-related gastric cancer, coronary heart disease, and ischemic stroke in China. Eur J Clin Microbiol Infect Dis 2017;36:199–212. [DOI] [PubMed] [Google Scholar]
- [3].Zhu L, He D, Han L, et al. Stroke research in China over the past decade: analysis of NSFC funding. Transl Stroke Res 2015;6:253–6. [DOI] [PubMed] [Google Scholar]
- [4].Cai SH, Lu SX, Liu LL, et al. Increased expression of hepatocyte nuclear factor 4 alpha transcribed by promoter 2 indicates a poor prognosis in hepatocellular carcinoma. Therap Adv Gastroenterol 2017;10:761–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ou H, Cai S, Liu Y, et al. A noninvasive diagnostic model to assess nonalcoholic hepatic steatosis in patients with chronic hepatitis B. Therap Adv Gastroenterol 2017;10:207–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ahmadi A, Tohidast SA, Mansuri B, et al. Acceptability, reliability, and validity of the Stroke and Aphasia Quality of Life Scale-39 (SAQOL-39) across languages: a systematic review. Clin Rehabil 2017;31:1201–14. [DOI] [PubMed] [Google Scholar]
- [7].Chabowski M, Grzebien A, Ziomek A, et al. Quality of life after carotid endarterectomy: a review of the literature. Acta Neurol Belg 2017;117:829–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].O’Keeffe F, Stark D, Murphy O, et al. Psychosocial outcome and quality of life following childhood stroke—a systematic review. Dev Neurorehabil 2017;20:428–42. [DOI] [PubMed] [Google Scholar]
- [9].Pulman J, Buckley E. Assessing the efficacy of different upper limb hemiparesis interventions on improving health-related quality of life in stroke patients: a systematic review. Top Stroke Rehabil 2013;20:171–88. [DOI] [PubMed] [Google Scholar]
- [10].Shan L, Shan J, Saxena A, et al. Quality of life and functional status after carotid revascularisation: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg 2015;49:634–45. [DOI] [PubMed] [Google Scholar]
- [11].van Middelaar T, Nederkoorn PJ, van der Worp HB, et al. Quality of life after surgical decompression for space-occupying middle cerebral artery infarction: systematic review. Int J Stroke 2015;10:170–6. [DOI] [PubMed] [Google Scholar]
- [12].Harris C. Return to work after stroke: a nursing state of the science. Stroke 2014;45:e174–6. [DOI] [PubMed] [Google Scholar]
- [13].Treger I, Shames J, Giaquinto S, et al. Return to work in stroke patients. Disabil Rehabil 2007;29:1397–403. [DOI] [PubMed] [Google Scholar]
- [14].Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med 2016;4:2103743725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yarlas A, Bayliss M, Cappelleri JC, et al. Psychometric validation of the SF-36((R)) Health Survey in ulcerative colitis: results from a systematic literature review. Qual Life Res 2018;27:273–90. [DOI] [PubMed] [Google Scholar]
- [16].Xue X, Cai S, Ou H, et al. Health-related quality of life in patients with chronic hepatitis B during antiviral treatment and off-treatment. Patient Prefer Adherence 2017;11:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cai SH, Lv FF, Zhang YH, et al. Dynamic comparison between Daan real-time PCR and Cobas TaqMan for quantification of HBV DNA levels in patients with CHB. BMC Infect Dis 2014;14:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Cai S, Cao J, Yu T, et al. Effectiveness of entecavir or telbivudine therapy in patients with chronic hepatitis B virus infection pre-treated with interferon compared with de novo therapy with entecavir and telbivudine. Medicine (Baltimore) 2017;96:e7021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wu X, Cai S, Li Z, et al. Potential effects of telbivudine and entecavir on renal function: a systematic review and meta-analysis. Virol J 2016;13:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Abu HO, Ulbricht C, Ding E, et al. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Qual Life Res 2018;27:2777–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Peng J, Yin J, Cai S, et al. Factors associated with adherence to nucleos(t)ide analogs in chronic hepatitis B patients: results from a 1-year follow-up study. Patient Prefer Adherence 2015;9:41–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Baatiema L, Chan C, Sav A, et al. Interventions for acute stroke management in Africa: a systematic review of the evidence. Syst Rev 2017;6:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Harpaz D, Eltzov E, Seet R, et al. Point-of-care-testing in acute stroke management: an unmet need ripe for technological harvest. Biosensors (Basel) 2017;7:E30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Shin AY, Porter PJ, Wallace MC, et al. Quality of life of stroke in younger individuals. Utility assessment in patients with arteriovenous malformations. Stroke 1997;28:2395–9. [DOI] [PubMed] [Google Scholar]
- [25].Wang R, Langhammer B. Predictors of quality of life for chronic stroke survivors in relation to cultural differences: a literature review. Scand J Caring Sci 2018;32:502–14. [DOI] [PubMed] [Google Scholar]
- [26].Cai S, Li Z, Yu T, et al. Serum hepatitis B core antibody levels predict HBeAg seroconversion in chronic hepatitis B patients with high viral load treated with nucleos(t)ide analogs. Infect Drug Resist 2018;11:469–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Cai S, Ou Z, Liu D, et al. Risk factors associated with liver steatosis and fibrosis in chronic hepatitis B patient with component of metabolic syndrome. United European Gastroenterol J 2018;6:558–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Xiao YB, Cai SH, Liu LL, et al. Decreased expression of peroxisome proliferator-activated receptor alpha indicates unfavorable outcomes in hepatocellular carcinoma. Cancer Manag Res 2018;10:1781–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Booth J, Connelly L, Lawrence M, et al. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC Neurol 2015;15:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kronenberg G, Schoner J, Nolte C, et al. Charting the perfect storm: emerging biological interfaces between stress and stroke. Eur Arch Psychiatry Clin Neurosci 2017;267:487–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Langhammer B, Sunnerhagen KS, Sallstrom S, et al. Return to work after specialized rehabilitation-An explorative longitudinal study in a cohort of severely disabled persons with stroke in seven countries: the Sunnaas International Network stroke study. Brain Behav 2018;8:e1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Peter R. One year follow-up after stroke. A preliminary feasibility study in the Jozsefvaros district of Budapest. Ideggyogy Sz 2012;65:113. [PubMed] [Google Scholar]
- [33].Endo M, Sairenchi T, Kojimahara N, et al. Sickness absence and return to work among Japanese stroke survivors: a 365-day cohort study. BMJ Open 2016;6:e9682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Cai S, Yu T, Jiang Y, et al. Comparison of entecavir monotherapy and de novo lamivudine and adefovir combination therapy in HBeAg-positive chronic hepatitis B with high viral load: 48-week result. Clin Exp Med 2016;16:429–36. [DOI] [PubMed] [Google Scholar]
- [35].Xue X, Cai S. Comment on “Assessment of Liver Stiffness in Pediatric Fontan Patients Using Transient Elastography”. Can J Gastroenterol Hepatol 2016;2016:9343960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Zeng J, Cai S, Liu J, et al. Dynamic changes in liver stiffness measured by transient elastography predict clinical outcomes among patients with chronic hepatitis B. J Ultrasound Med 2017;36:261–8. [DOI] [PubMed] [Google Scholar]


