Abstract
Background
The kinetic link among the lumbar spine, pelvic tilt, and the hip has been hypothesized, but this relationship requires further study in acetabular dysplasia. Anecdotal reports suggest that patients may compensate for acetabular dysplasia with an involuntary increase in anterior pelvic tilt; it is not known if this relationship is affected by acetabular reorientation.
Questions/purposes
(1) Does compensatory pelvic tilt decrease on preoperatively obtained standing AP pelvis radiographs compared with those obtained at a minimum of 6 months after bilateral periacetabular osteotomy (PAO)? (2) Does a modified surrogate measurement of pelvic tilt, the pubic symphysis to sacroiliac (PS-SI) index, correlate with a physical synthetic bones model in which pelvic tilt can be directly measured? (3) Can the PS-SI index demonstrate high interrater reliability?
Methods
We assessed the surgical records of one surgeon, who participates in the longitudinally maintained Academic Network of Conservational Hip Outcomes Research (ANCHOR) registry, for patients who had undergone the second side of a staged bilateral PAO between 2007 and 2016; there were 113 such patients. Of those, 70 (62%) were lost to followup within 6 months of the second PAO or did not have adequate imaging studies, and another three (3%) were excluded for prespecified reasons, leaving 40 (35%) for evaluation in this retrospective study. Standing preoperative and most recent postoperative AP pelvis radiographs were used to measure the Tönnis angle, anterior wall index, posterior wall index, lateral center-edge angle, pubis symphysis-to-sacrococcygeal junction distance, and the PS-SI index. The most recent radiographs were obtained at a mean of 16 ± 6 months after the second PAO. We chose 6 months as the minimum because at this time point, the majority of patients have reached their maximum clinical improvement and are no longer limited by postoperative muscle dysfunction. Statistical analysis was performed using the intraclass correlation coefficient (ICC) for interrater reliability and paired t-tests for assessing change in measurements from pre- to postoperative. Additionally, a model was created using a physical synthetic bones model in which pelvic tilt could be directly measured. This model was secured through bilateral acetabuli on a mount and rotated through 5° increases in pelvic tilt. AP pelvis radiographs were obtained at each point, the PS-SI index was measured, and a regression analysis performed to evaluate for trend.
Results
Overall, 37 of 40 patients (93%) had a decrease in pelvic tilt, as measured by the PS-SI index. The mean amount of pelvic tilt as measured by the PS-SI index decreased after surgery when comparing the preoperative with latest radiographs on this parameter (97 ± 14 mm versus 89 ± 13 mm, mean difference 8 ± 9 mm; 95% confidence interval, -11 to -5; range 17 increase to 24 decrease, p < 0.001). A linear relationship between pelvic tilt and PS-SI index (PS-SI index = 5.0° + 3.6° * tilt, R2 = 0.99) was identified in the synthetic bones validation model. Finally, the interrater reliability was found to be excellent for the PS-SI index preoperatively (ICC = 0.986) and postoperatively (ICC = 0.988).
Conclusions
We found a modest reduction in anterior pelvic tilt after bilateral PAO. This finding suggests that acetabular reorientation affects pelvic position. In clinical practice, patients with acetabular dysplasia may compensate with dynamic and reversible changes in pelvic tilt. The PS-SI index is a reproducible tool to measure the height of the pelvic inlet as an assessment of pelvic tilt. In the future, clinical studies should evaluate the clinical implications of these radiographic findings, including the assessment of back pain, which although multifactorial may be influenced by pelvic tilt.
Level of Evidence
Level III, therapeutic study.
Introduction
The kinetic link among the lumbar spine, acetabulum, and pelvic tilt is a subject of influence throughout the orthopaedic literature [20], particularly in the fields of arthroplasty [1, 3, 4] and the spine [17, 21]. To date, however, the role of the spine and pelvic tilt in patients with acetabular dysplasia requires further elucidation. Anecdotally, there is a speculative link between the lumbar spine and hip in acetabular dysplasia, because patients with dysplasia and hip pain may also present with low back pain. In acetabular dysplasia, the primary hip pathologic zone of deficiency can vary and involve the lateral, anterior, and posterior portions of the acetabulum [16]. When the acetabulum is deficient anteriorly, we speculate that patients attempt to compensate for this anterior deficiency by involuntarily increasing their anterior pelvic tilt. Recently, Fukushima et al. [8] evaluated radiographic parameters of sagittal alignment in patients with hip pathology and noted an increased lumbar lordosis and sacral slope in patients with acetabular dysplasia when compared with patients with symptomatic labral tears. Matsuyama et al. [14] observed a similar pattern with an increase in anterior pelvic tilt and a compensatory hyperlumbar lordosis in patients with bilateral congenital hip dislocation secondary to dysplasia.
However, the connection between pelvic tilt and acetabular position has not previously been described in patients with acetabular dysplasia. Furthermore, whether or not this compensation is reversible has not been characterized. We hypothesize that after bilateral periacetabular osteotomy (PAO) [9], the pelvic tilt can change with decreasing anterior pelvic tilt.
Before attempting to characterize the link between the hip and pelvic tilt in patients with acetabular dysplasia, reliable and reducible radiographic measurements of pelvic tilt and acetabular coverage must be identified. The standard measurements of pelvic tilt and acetabular coverage have poor interobserver reliability [7, 13] and are subject to variation in patient positioning and pelvic rotation [26]. Additionally, many of the measurements of sagittal alignment that are found on lateral lumbar spine or pelvis radiographs require additional radiation exposure for the patient beyond a standard hip radiograph series [6]. Lumbar lordosis is most commonly measured with Cobb’s angle. Pelvic incidence is measured as the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the axis of the femoral heads. Pelvic tilt is defined as the angle between the line connecting the pubic symphysis with the sacral promontory and a horizontal line [24] or the midpoint of the sacral plate to the femoral head axis and a vertical line [12] (Fig. 1). Previous studies attempted surrogate measurements of pelvic tilt on the AP pelvis radiograph and used varying distances and ratios, including the pubic symphysis to the midpoint of the sacrococcygeal joint, the pubic symphysis to a line connecting the center of both femoral heads, the vertical distance between the pubic symphysis and a line connecting the lower end of one sacroiliac joint, the ratio between the vertical and horizontal diameter of the pelvic foramen, the ratio between the vertical and horizontal extends of the obturator foramen, and the ratio between the vertical extend of the obturator foramen and the distance between the teardrops. In 2006, Tannast et al. [24] showed that these measurements demonstrated variable reliability. The strongest correlation was found between pelvic tilt and the distance between the sacrococcygeal junction and the pubic symphysis. This correlation was classified as “moderately strong” and the authors describe that with a probability of 65%, tilt can be estimated with an accuracy of 3.8° for men and 4.2° for women. This measure also has significant error that is likely the result of variation in sacral morphology and inconsistent visualization on radiographs [25]. Nepple et al. [15], utilizing a computer-assisted analysis of pelvic radiographs, found that although the inter- and intraobserver reliability for measurements of the landmarks of the sacrococcygeal joint and inferior coccyx was excellent, there was once again only moderate reliability between readers when the distances were classified as “normal” or “abnormal.”
Fig. 1.

This radiograph demonstrates standard radiographic measurements of sagittal balance that can be obtained from a lateral lumbar spine and pelvis radiograph. The blue lines represent lumbar spine Cobb angle, the red angle is pelvic incidence, and the yellow angle is pelvic tilt.
Although the distance between the sacrococcygeal junction and pubic symphysis is often utilized as the standard surrogate marker for pelvic tilt on the AP pelvis radiograph, multiple studies [15, 24, 25] have demonstrated that it has moderate reliability and is subject to variation. We propose the use of the pubic symphysis to sacroiliac index (PS-SI index) as a surrogate marker of pelvic tilt. This index is a modification of a technique described by Thorén and Sahlstedt [27] and can be measured on an AP pelvis radiograph without the need for additional views. It also is easily identified regardless of pelvic and sacral morphology.
We therefore asked: (1) Does compensatory pelvic tilt decrease on preoperatively obtained standing AP pelvis radiographs compared with those obtained at a minimum of 6 months after bilateral PAO? (2) Does a modified surrogate measurement of pelvic tilt, the PS-SI index, correlate with a physical synthetic bones model in which pelvic tilt can be directly measured? (3) Can the PS-SI index demonstrate high interrater reliability?
Patients and Methods
We obtained institutional review board approval to retrospectively evaluate a single-surgeon cohort of patients who underwent bilateral PAO according to the technique described by Ganz et al. [9]. All patients were enrolled in the longitudinally maintained, multicenter Academic Network of Conservational Hip Outcomes Research (ANCHOR) study group [5]. Initial analysis identified 113 patients who underwent bilateral PAO between 2007 and 2016. The range of time between surgeries was a minimum of 5 months 2 days to a maximum of 4 years 6 months. Exclusion criteria eliminated 33 patients (29%) because of insufficient followup, 37 (33%) because of inadequate imaging, and three (3%) for other medical comorbidities or previous hip surgery. We analyzed the remaining 40 patients (35%). There were 35 females (87.5%) and five males (12.5%). Mean age at first PAO was 21 ± 6 years (range, 12–41 years). Mean body mass index was 23 ± 3 kg/m2 (range, 18–35 kg/m2). Average followup from the time of the second PAO was 16 ± 6 months (range, 7–33 months).
To answer our first question about whether compensatory pelvic tilt decreases after PAO, we identified patients with preoperative AP pelvis radiographs and a minimum of 6 months of radiographic followup after the second PAO. We chose 6 months as the minimum because the majority of patients reach maximum clinical improvement at this time and are no longer limited by postoperative muscle dysfunction. This time point is likely a conservative estimate, because patients may continue to improve over time. The standardized technique for standing AP pelvis radiographs in our practice is performed with patients standing in stocking feet with bilateral patella pointing directly forward. The x-ray beam is centered midway between the anterosuperior iliac spine and the pubic symphysis. Any films that demonstrate > 2 mm of rotation between the coccyx and pubic symphysis are repeated by the x-ray technician (Fig. 2). These films were independently evaluated by two orthopaedic surgery residents (ED, NN) for the following variables: Tönnis angle [28], anterior wall index [22], posterior wall index, lateral center-edge angle (LCEA) [2], and the pubic symphysis to sacrococcygeal joint distance [25] [24]. The pubis symphysis to sacrococcygeal junction was measured as a surrogate for pelvic tilt.
Fig. 2.

This image illustrates the standardized technique for obtaining a standing AP pelvis radiograph. The patient is standing in stocking feet with bilateral patella pointing forward and the beam centered between the anterosuperior iliac spine and pubic symphysis.
Our modified technique for measuring a surrogate for pelvic tilt from the AP pelvis radiograph, which we called the PS-SI index, was performed as follows. Thorén and Sahlstedt [27] originally described the use of a line drawn from one sacroiliac joint to the pubic symphysis on an AP pelvis radiograph as a surrogate marker for pelvic tilt in 1990. This was modified to increase the reproducibility between examiners by drawing a horizontal line between bilateral sacroiliac joints. A vertical line from the pubic symphysis to the point of intersection with the sacroiliac line is drawn. The distance between the sacroiliac line and pubic symphysis is then measured to obtain the PS-SI index (Fig. 3).
Fig. 3.

This radiograph demonstrates the PS-SI index measurement.
To understand the relationship between the magnitude of change of the PS-SI index and degree of pelvic tilt, a model was created using a synthetic bone pelvis (Sawbones®, Vashon Island, WA, USA) mounted to a jig (Fig. 4) using a method similar to that described by Tannast et al. [23]. A three-dimensional vise with marked degrees was used to precisely and reproducibly tilt the pelvis. Standard AP plain radiographs of the Sawbones pelvis were obtained at varying degrees of pelvic tilt (0°, 5°, 10°, 15°, 20°, 25°, 30°) from neutral. The PS-SI index was measured at each known degree of pelvic tilt and a linear regression analysis performed to evaluate for trend.
Fig. 4.
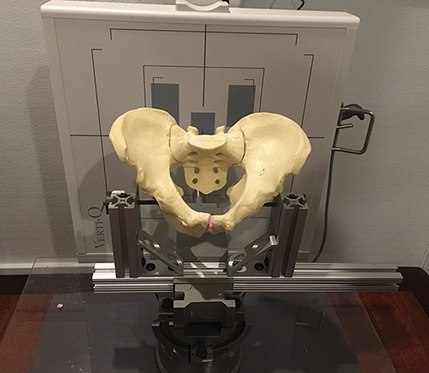
This image illustrates the experimental setup for comparison of the PS-SI relationship to pelvic tilt.
To assess the interrater reliability of the PS-SI index, we calculated an intraclass correlation coefficient (ICC) for measurements performed independently by two orthopaedic surgery residents (ED, NN). This calculation was based on a two-way random-effects analysis of variance and absolute agreement. An ICC < 0.50 indicated poor reliability, an ICC between 0.51 and 0.75 indicated moderate reliability, an ICC between 0.75 and 0.90 indicated good reliability, and an ICC > 0.90 indicated excellent reliability [11]. Because the raters demonstrated good-to-excellent reliability, we performed further analyses with the mean of the two raters’ measurements. We evaluated data distribution with the Shapiro-Wilk test. Differences between preoperative and postoperative values were evaluated with paired t-tests for normally distributed data and Wilcoxon signed-rank test for nonnormally distributed data. Pearson’s correlation was used to evaluate the relationship between change in the PS-SI index and the change in LCEA, Tönnis angle, posterior wall index, and anterior wall index. Data are presented as mean ± SD (95% confidence interval [CI]). A p value < 0.05 was considered statistically significant [19]. All statistical analysis was performed with SPSS (Version 22; IBM Corp, Armonk, NY, USA).
Results
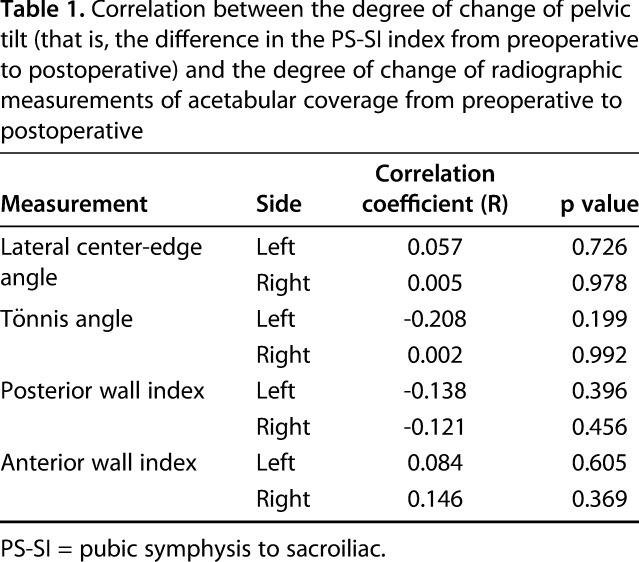
The compensatory anterior pelvic tilt, measured with the PS-SI index, decreased from standing AP pelvis radiographs obtained at a minimum of 6 months after bilateral PAO preoperatively compared with those obtained before surgery. We detected a change in the PS-SI index from preoperatively to postoperatively (p < 0.001). The mean change was a decrease of 8 ± 9 mm (95% CI, -11 to -5), and the change ranged from an increase of 17 mm to a decrease of 24 mm. The mean preoperative PS-IS index was 97 ± 14 mm (95% CI, 92-101) and the mean postoperative PS-SI index was 89 ± 13 mm (95% CI, 85-93). Overall, 37 patients (93%) had a decrease in the PS-SI index (Fig. 5). The pubic symphysis to sacrococcygeal junction distance demonstrated no difference from preoperative to postoperative (mean decrease of 4 ± 14 mm; 95% CI, -9 to 0.3) with a range from an increase of 26 mm to a decrease of 30 mm (p = 0.060). Intraobserver reliability was excellent for the preoperative (ICC = 0.928) and postoperative distance (ICC = 0.947). No correlation was found between the degree of change of pelvic tilt (that is, the difference in the PS-SI index from preoperative to postoperative) and the degree of change in anterior wall index, posterior wall index, LCEA, or Tönnis angle (Table 1). Further subgroup analysis based on age was also performed. In this analysis, we excluded patients with an increase in PS-SI index postoperatively. We identified no correlation between age at first PAO and decrease in PS-SI index (r = -0.0157; p = 0.384; n = 37).
Fig. 5.
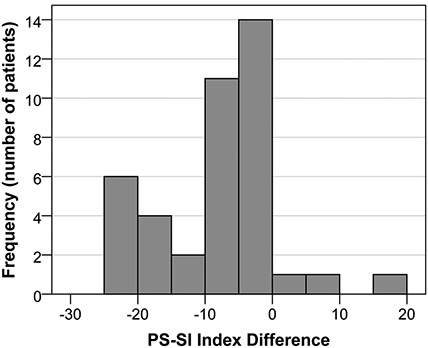
This histogram demonstrates the distribution of the difference in PS-SI index from preoperatively to postoperatively.
Table 1.
Correlation between the degree of change of pelvic tilt (that is, the difference in the PS-SI index from preoperative to postoperative) and the degree of change of radiographic measurements of acetabular coverage from preoperative to postoperative
The PS-SI index was found to correlate with pelvic tilt using the physical synthetic bone model in which pelvic tilt is directly measured. Linear regression analysis of the relationship between pelvic tilt and PS-SI index demonstrated a highly linear relationship (PS-SI index = 5.0° + 3.6° * pelvic tilt, R2 = 0.99). In the Sawbones model, for every 1° change in pelvic tilt, the PS-SI index increases by 3.6 mm (Fig. 6).
Fig. 6.
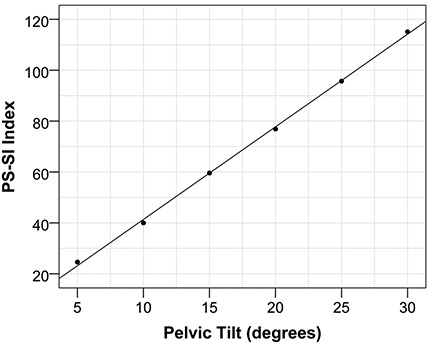
This figure is a regression analysis of PS-SI index and degree of pelvic tilt. It demonstrates a linear relationship.
Finally, our modified surrogate measurement for pelvic tilt, the PS-SI index, demonstrated excellent interrater reliability preoperatively (ICC = 0.990; 95% CI, 0.855–0.997) and postoperatively (ICC = 0.989; 95% CI, 0.851–0.997).
Discussion
Determining the role of pelvic tilt in compensation for acetabular deficiency is an important step in understanding the effects of treatment for patients with acetabular dysplasia. Although previous studies have identified a kinetic link among lumbar lordosis, pelvic tilt, and hip pathology, this has not been previously described in patients with acetabular dysplasia. Furthermore, the potential reversibility of the pelvic compensation for dysplasia has not been elucidated. Previously described surrogate markers of pelvic tilt such as the distance between the sacrococcygeal junction to pubic symphysis have been studied and found to correlate to pelvic tilt with moderate reliability. We choose to utilize this measurement of pelvic tilt as well as the PS-SI index, a surrogate modified marker of pelvic tilt that can be identified on an AP pelvis radiograph. The PS-SI index was further studied in a synthetic bone model to gain a sense of the size of the change of pelvic tilt that is seen. In this study, using a modified measurement called the PS-SI index, we demonstrated that anterior pelvic tilt decreases in patients after bilateral PAO. We found an excellent degree of interobserver reliability with this measurement and demonstrated that there is a measurable change in pelvic tilt using a synthetic bone model.
This study has several limitations. First, inherent variation in patient positioning for radiographs may influence the measurements of acetabular coverage, particularly the anterior and posterior wall [26] and pelvic tilt. To minimize this variation, all the radiographs used in this study were standing AP pelvis films. We utilized a standardized technique with all patients standing in stocking feet with bilateral patella facing the cassette and the beam centered between the pubic symphysis and the anterosuperior iliac spine. Second, because of the need to reduce variation in the radiographs, we had a significant loss of data. Of 113 initial patients who underwent bilateral PAO, 33 patients were excluded as a result of inadequate followup and 37 were excluded as a result of inadequate films. The patients with inadequate films were excluded because they had preoperative supine AP pelvis radiographs. This was common in early practice, before publication of research demonstrating the variation in positioning of the pelvis from supine to standing. This literature has demonstrated that apparent acetabular retroversion increases in supine films when compared with standing [29] and pelvic tilt increases approximately 5° posteriorly from supine to standing [10]. We felt that this degree of variability was significant and could result in a large confounding factor in our study. Therefore, we chose to exclude this large portion of patients. The patients who were excluded as a result of imaging concerns were treated by the same surgeon (IZ) utilizing a similar surgical technique and postoperative protocol, leading us to believe that there should not be a significant difference between the included and excluded patients. The patients who were lost as a result of inadequate followup are either surgeries that were performed within the past 6 months or patients who did not followup to a minimum of 6 months. Similarly, we felt that including patients who were only 1 to 2 months from surgery would result in a significant confounding factor, because patients are often limited by their postoperative muscular dysfunction at this time point. Patients continue to make significant gains in their core and hip stability through physical therapy between 2 and 6 months postoperatively. This muscular stability likely plays an important role in pelvic tilt and the lumbar spine and we felt that it would not be accurately assessed in the early postoperative period. Furthermore, we hypothesize that 6 months is likely an underestimate for the finding of decreased anterior pelvic tilt and changes likely continue to occur a year or more beyond the final surgery. This time point was chosen to maximize the number of eligible patients while allowing for a reasonable time of postoperative recovery to minimize confounding variables.
We found that compensatory pelvic tilt decreases after bilateral PAO, as measured on AP radiographs. We know of no other studies that describe the reversible changes in the pelvis after bilateral PAO. Previous work by Fukushima et al. [8] compared the sagittal vertical axis, pelvic tilt, pelvic incidence, sacral slope, and lumbar lordosis in patients with acetabular dysplasia (defined by LCEA < 20°) and patients with symptomatic labral tears. They found a higher sacral slope and lumbar lordosis in patients with dysplasia and no difference in pelvic tilt between the two study populations. This study supports, as we have seen, that there are changes to spinopelvic alignment as a result of acetabular dysplasia; however, it is significantly limited by its narrow definition of acetabular dysplasia and inclusion of only Asian female patients. Okuda et al. [18] evaluated pelvic inclination, sacral slope, lumbar lordosis, pelvic angle, and disc angle of L5/S1 in healthy volunteers and patients with varying stages of osteoarthritis secondary to dysplasia (defined as LCEA < 20°). They found an increase in anterior pelvic inclination without changes in the sacral slope and lumbar lordosis in the prearthritic group, but it was similar to age-matched control subjects. In the later-stage arthritic group, they found maintained lumbar lordosis and sacral slope, despite expected age-related decreases in lumbar lordosis and increase in sacral slope in the comparative healthy volunteer group. The authors hypothesize that in younger patients, accommodations are made through the sacroiliac joint to prevent changes to the lumbar and sacrum and in older patients, development of joint contracture may explain the lack of change to the lumbar spine. This study also presents interesting hypotheses about the potential role of the sacroiliac joint in compensation for dysplasia, but is similarly limited by its narrow definition of dysplasia and inclusion of only Asian female patients. Our study adds further support to previous work, which has demonstrated that pelvic tilt, inclination, and lumbar lordosis are altered in patients with dysplasia and is the first to suggest that these changes may be reversible. Tannast et al. [24] evaluated surrogate measurements for pelvic tilt and reported the sacrococcygeal junction to pubic symphysis measurement to have the strongest correlation to the actual pelvic tilt that can be measured on a lateral film. However, it is subject to measurement error as a result of variations in sacral morphology and radiographic factors such as positioning, presence of bowel gas, and difficult visualization of the sacrococcygeal junction. Our modified surrogate marker of pelvic tilt, the PS-SI index, relies on clearly identifiable landmarks, the sacroiliac joint and pubic symphysis. In this study we found a change in the PS-SI index from pre- to postoperative, but did not find a change in the sacrococcygeal junction to pubic symphysis measurement. There are several possible explanations for this discrepancy. There is much that is not well understood about pelvic morphology. These measurements may be affected by the size of the pelvis, pelvic incidence, or other anatomic factors that are not yet appreciated.
We found that our measurement of pelvic tilt, the PS-SI index, correlated well in a synthetic bones model of the pelvis under controlled imaging. The relative change in pelvic tilt from a neutrally positioned pelvis was linearly correlated with the change in PS-SI index measured on the corresponding AP pelvis radiograph. Although this model was not designed to determine a quantifiable, absolute pelvic tilt value from the PS-SI index, it does provide valuable information regarding the utility of this measurement. Tannast et al. and Thorens et al. [24, 27] previously described a similar measurement connecting one sacroiliac joint to the pubic symphysis rather than a tangent line connecting both sacroiliac joints as we present. Tannast et al. found a moderate correlation with pelvic tilt in a study of 104 human pelvic radiographs [24]. Future research, with a large sample size, would further validate this model and help to elucidate the quantitative relationship between the known PS-SI index and the absolute angle of pelvic tilt.
We found that our measure, the PS-SI index, was readily reproducible between observers. The excellent interrater reliability in both preoperative and postoperative measurements demonstrates that this is an easily reproducible measurement. Other measurements obtained from the AP pelvis film, including Tönnis angle and LCEA [13] as well as pelvic incidence, tilt, and sacral slope [7], have shown poor interrater reliability. In the future, research to compare this parameter with other commonly used surrogate measurements of pelvic tilt, including the distance from the pubic symphysis to sacrococcygeal junction, on both AP and lateral films is needed to assess for a correlation.
This study demonstrates a reduction in pelvic tilt after bilateral PAO, suggesting that acetabular reorientation affects pelvic orientation. This study further demonstrates that the compensation of the pelvis in acetabular dysplasia is dynamic and reversible. We have also identified a modified, easily reproducible surrogate measurement for pelvic tilt, the PS-SI index, which linearly correlates with changes in pelvic tilt on a synthetic bone model. This measurement will prove to be a valuable tool going forward as we further investigate the role of pelvic tilt in involuntary compensation for acetabular dysplasia. Future studies are needed to evaluate the clinical implications of these radiographic findings.
Footnotes
One of the authors certifies that he (IZ) has received or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from OrthoPediatrics (Warsaw, IN, USA), outside this submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Beaumont Health, Royal Oak, MI, USA.
References
- 1.An VVG, Phan K, Sivakumar BS, Mobbs RJ, Bruce WJ. Prior lumbar spinal fusion is associated with an increased risk of dislocation and revision in total hip arthroplasty: a meta-analysis. J Arthroplasty. 2018;33:297-300. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-1018. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Galim P, Ben-Galim T, Rand N, Haim A, Hipp J, Dekel S, Floman Y. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976). 2007;32:2099-2102. [DOI] [PubMed] [Google Scholar]
- 4.Blizzard DJ, Sheets CZ, Seyler TM, Penrose CT, Klement MR, Gallizzi MA, Brown CR. The impact of lumbar spine disease and deformity on total hip arthroplasty outcomes. Orthopedics. 2017;40:e520-e525. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Baca G, Beaule PE, Kim YJ, Larson CM, Millis MB, Podeszwa DA, Schoenecker PL, Sierra RJ, Sink EL, Sucato DJ, Trousdale RT, Zaltz I; ANCHOR Study Group. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41:1348-1356. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dimar JR, Carreon LY, Labelle H, Djurasovic M, Weidenbaum M, Brown C, Roussouly P. Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur Spine J. 2008;17:1373-1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukushima K, Miyagi M, Inoue G, Shirasawa E, Uchiyama K, Takahira N, Takaso M. Relationship between spinal sagittal alignment and acetabular coverage: a patient-matched control study. Arch Orthop Trauma Surg. 2018;138:1495-1499. [DOI] [PubMed] [Google Scholar]
- 9.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26-36. [PubMed] [Google Scholar]
- 10.Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph. A new computerized technique. J Bone Joint Surg Am. 1993;75:1318-1333. [DOI] [PubMed] [Google Scholar]
- 11.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mast NH, Impellizzeri F, Keller S, Leunig M. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res. 2011;469:188-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsuyama Y, Hasegawa Y, Yoshihara H, Tsuji T, Sakai Y, Nakamura H, Kawakami N, Kanemura T, Yukawa Y, Ishiguro N. Hip-spine syndrome: total sagittal alignment of the spine and clinical symptoms in patients with bilateral congenital hip dislocation. Spine (Phila Pa 1976). 2004;29:2432-2437. [DOI] [PubMed] [Google Scholar]
- 15.Nepple JJ, Martell JM, Kim YJ, Zaltz I, Millis MB, Podeszwa DA, Sucato DJ, Sink EL, Clohisy JC; ANCHOR Study Group. Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med. 2014;42:2393-2401. [DOI] [PubMed] [Google Scholar]
- 16.Nepple JJ, Wells J, Ross JR, Bedi A, Schoenecker PL, Clohisy JC. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res. 2017;475:1037-1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976). 1983;8:316-321. [DOI] [PubMed] [Google Scholar]
- 18.Okuda T, Fujita T, Kaneuji A, Miaki K, Yasuda Y, Matsumoto T. Stage-specific sagittal spinopelvic alignment changes in osteoarthritis of the hip secondary to developmental hip dysplasia. Spine (Phila Pa 1976). 2007;32:E816-819. [DOI] [PubMed] [Google Scholar]
- 19.Portney L, Watkins M. Foundations of Clinical Research: Applications in Practice. Boston, MA, USA: Prentice Hall; 2009. [Google Scholar]
- 20.Redmond JM, Gupta A, Nasser R, Domb BG. The hip-spine connection: understanding its importance in the treatment of hip pathology. Orthopedics. 2015;38:49-55. [DOI] [PubMed] [Google Scholar]
- 21.Shum GL, Crosbie J, Lee RY. Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine (Phila Pa 1976). 2005;30:1998-2004. [DOI] [PubMed] [Google Scholar]
- 22.Siebenrock KA, Kistler L, Schwab JM, Buchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012;470:3355-3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199-1205. [DOI] [PubMed] [Google Scholar]
- 24.Tannast M, Murphy SB, Langlotz F, Anderson SE, Siebenrock KA. Estimation of pelvic tilt on anteroposterior X-rays--a comparison of six parameters. Skeletal Radiol. 2006;35:149-155. [DOI] [PubMed] [Google Scholar]
- 25.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182-190. [DOI] [PubMed] [Google Scholar]
- 26.Tannast MM, Fritsch SM, Zheng GP, Siebenrock KM, Steppacher SM. Which radiographic hip parameters do not have to be corrected for pelvic rotation and tilt? Clin Orthop Relat Res . 2015;473:1255-1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thorén B, Sahlstedt B. Influence of pelvic position on radiographic measurements of the prosthetic acetabular component. An experimental study on a pelvic model. Acta Radiol. 1990;31:133-136. [PubMed] [Google Scholar]
- 28.Tönnis D, Legal H, Graf R. Congenital Dysplasia and Dislocation of the Hip in Children and Adults . Berlin, Germany: Springer-Verlag; 1987. [Google Scholar]
- 29.Troelsen A, Jacobsen S, Rømer L, Søballe K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res. 2008;466:813-819. [DOI] [PMC free article] [PubMed] [Google Scholar]


