Abstract
Background
Prophylactic pinning of the asymptomatic and normal-appearing contralateral hip in patients with unilateral slipped capital femoral epiphysis (SCFE) remains controversial. Understanding the minimal 10-year clinical, functional, and radiographic outcomes of the contralateral asymptomatic hip in unilateral SCFE may be helpful in the decision regarding whether the benefits associated with potentially preventing a SCFE are outweighed by the risk of additional surgery.
Questions/purposes
Among patients with SCFE treated with prophylactic pinning of the asymptomatic and contralateral hip, we sought (1) to determine the complications and reoperations; (2) to evaluate the development of cam deformities and the frequency and severity of osteoarthritis progression; and (3) to characterize hip pain and function as measured by the Harris hip score (HHS) and the Hip Disability and Osteoarthritis Outcome Score (HOOS) at minimal 10-year followup.
Methods
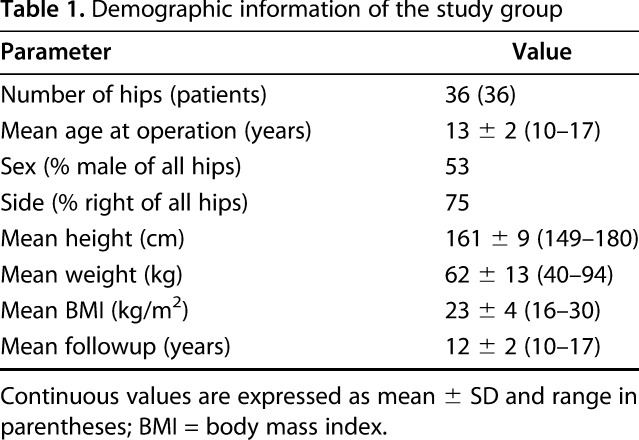
Between 1998 and 2005 all patients with SCFE seen at our institution were treated with the modified Dunn procedure and all were offered prophylactic pinning of the contralateral asymptomatic hip. Of the 41 patients who underwent the unilateral modified Dunn procedure and who had an asymptomatic contralateral hip, 37 patients (90%) underwent pinning of that contralateral hip. Of those, 33 patients (80%) were available for clinical and radiographic evaluation for this retrospective study at a minimum of 10 years (mean followup 12 ± 2 years) after surgery. Three patients of the 37 patients only had 10-year clinical followup, including questionnaires sent by mail and telephone, because they refused further radiographic followup and one patient was lost to followup. The group included 19 males and 17 females whose age at surgery was a mean of 13 ± 2 years. Medical charts were reviewed and patients were asked about complications and additional surgical procedures. Most recent postoperative radiographs were evaluated for measurement of the alpha angle, head-neck offset, epiphysis orientation, and osteoarthritis grading according to Tönnis classification and minimum joint space width. The presence of a cam deformity was defined by an alpha angle measurement > 60° on the AP radiograph and/or > 55° on the lateral radiograph. Hip function and pain were assessed by the HHS and HOOS outcome measures.
Results
No complications with prophylactic in situ pinning were recorded. Four of 36 (11%) patients underwent subsequent surgical treatment for cam-type femoroacetabular impingement (FAI), and hardware removal was performed in four hips (11%). The mean alpha angle was 53° ± 8° on the AP radiograph and 49° ± 8° on the lateral view at followup. In total, 10 of 33 hips (30%) had a cam morphology at the femoral head-neck junction and four (12%) were symptomatic and underwent FAI surgery. Six of 33 patients (18%) developed an asymptomatic cam morphology at the femoral head-neck junction; in three of 33 hips (9%), the cam deformity instead of lesion were visible only on the lateral projection, and 9% were visible on both the AP and lateral projections. The preoperative offset of the femoral head-neck junction was 10 ± 3 mm on the AP view and 11 ± 4 mm on the lateral view. At followup, the AP offset was 7 ± 3 mm and the lateral offset was 6 ± 3 mm, and on the lateral view, the offset was < 10 mm in eight hips (22%). No patient had radiographic signs of hip osteoarthritis (Tönnis Grade 0). The mean minimum joint space width was 4 ± 0.4 mm. The mean HHS for the 32 patients who did not undergo subsequent surgery was 97 ± 5 at latest followup. The mean postoperative HOOS was 94 ± 8 for the 32 patients at latest followup.
Conclusions
At a minimum followup of 10 years after prophylactic pinning of a contralateral asymptomatic hip, most patients achieve excellent hip scores; however, a substantial proportion will develop a symptomatic cam deformity despite prophylactic pinning. No patient had signs of osteoarthritis at a minimum of 10 years, but almost one-third of the patients who underwent prophylactic pinning developed a cam deformity.
Level of Evidence
Level IV, therapeutic study.
Introduction
Slipped capital femoral epiphysis (SCFE) is a relatively common hip disorder in adolescents with an overall incidence of 10.8 per 100,000 children in the United States [23] and an incidence of 11.6 per 100,000 children in Europe [46]. The prevalence of bilateral involvement has been reported to vary between 21% and 80% [4, 13–15, 19, 27, 32]. This variation is attributable in part to the fact that some patients have bilateral SCFE at the time of presentation [14, 18], whereas others develop asynchronous presentation, typically in the first 18 months after the primary slip [27]. Furthermore, the opposite hip may develop SCFE asymptomatically during adolescence leading to a later postslip deformity in adulthood [14, 19, 45]. Assessment of the contralateral hip in patients with unilateral SCFE followed for an average of 30 years have shown radiographic features of SCFE that had been underdiagnosed during adolescence in 40% of the patients [14]. Additionally, up to one-third of the contralateral hips with a postslip deformity develop signs of radiographic osteoarthritis at followup ranging from 16 to 66 years [14, 19]. There also is concerning evidence that even mild SCFE deformity can lead to femoroacetabular impingement (FAI) [10, 35] and articular cartilage damage that may increase the risk of later osteoarthritis development [17, 25, 38].
Although prophylactic pinning of the contralateral asymptomatic and normal-appearing hip in patients with unilateral SCFE is a well-known treatment method [43], it still remains controversial [5, 6, 13–15, 19, 22, 27, 31–33, 36, 45]. The high prevalence of bilateral involvement, the risks of a subsequent displaced SCFE with potential complications such as osteonecrosis, and the proportion of osteoarthritis in patients who developed an asymptomatic postslip deformity have all been reported as part of the rationale for prophylactic pinning [13, 14, 36, 37]. Although the risk of complications after prophylactic pinning with contemporary techniques has been reduced, some risk remains [5, 33]. Understanding the long-term outcome of the contralateral normal hip in unilateral SCFE is crucial to the decision regarding prophylactic fixation. Although a few long-term studies have reported up to a 30% incidence of osteoarthritis in the contralateral hips of patients treated for unilateral SCFE [13, 19], there are limited data about the mid- and long-term clinical, functional, and radiographic outcomes after prophylactic pinning [9].
In this retrospective study, we therefore evaluated patients with SCFE treated with prophylactic pinning of the contralateral and asymptomatic hip and sought (1) to determine the complications and reoperations; (2) to evaluate the development of cam deformities and the frequency and severity of osteoarthritis instead of arthritis progression; and (3) to characterize hip pain and function as measured by the Harris hip score (HHS) and the Hip Disability and Osteoarthritis Outcome Score (HOOS) at minimal 10-year followup.
Patients and Methods
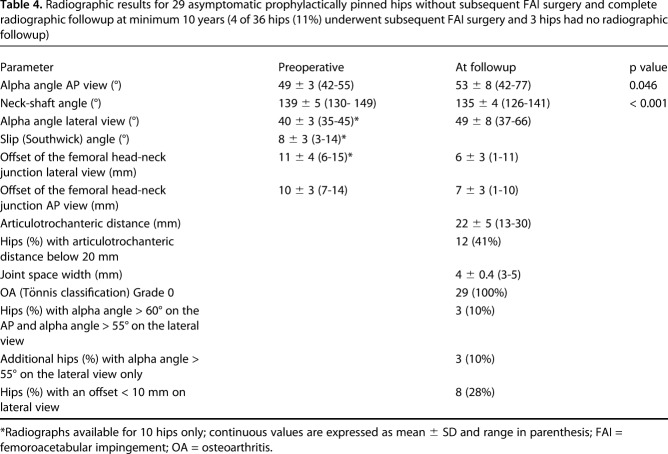
Between 1998 to 2005 a total of 42 patients (43 hips) were uniformly treated for SCFE with the modified Dunn procedure [40, 49, 50] at the University Hospital of Bern. During this period, we recommended prophylactic pinning of the asymptomatic contralateral hip (which showed no radiographic features of SCFE) in all patients. This series includes some of the first patients who underwent the modified Dunn procedure. This approach was applied regardless of whether the slips were mild or severe, acute or chronic, and all such patients were considered potentially eligible here. One patient (two hips) presented with bilateral symptomatic SCFE and was excluded. However, four patients did not undergo prophylactic pinning because the family refused after an informed discussion. Therefore, 37 patients underwent prophylactic pinning of the asymptomatic normal-appearing contralateral hip during the study period (Fig. 1). Minimum followup was set at 10 years; one patient who lived abroad was further excluded because of insufficient clinical and radiographic followup. A total of 36 patients with a minimum 10-year followup after prophylactic pinning were thus included. Three patients had only 10-year clinical followup, including questionnaires sent by mail and telephone, because they refused further radiographic followup (Fig. 1). This resulted in 33 hips of 33 patients with a complete clinical and radiographic minimum 10-year followup. There were 19 male patients (53%) and 17 female patients (47%) with a mean age of 13 ± 2 years at surgery and a mean body mass index (BMI) of 23 ± 4 kg/m2. This is above the 90th percentile. The BMI for males was 23 ± 4 kg/m2 and for females was 24 ± 5 kg/m2. The mean followup was 12 ± 2 years (Table 1).
Fig. 1.
The flowchart with exclusion criteria for the study group is shown.
Table 1.
Demographic information of the study group
We defined a normal contralateral hip at the time of the Dunn procedure as one that included a normal superior femoral neck line crossing the epiphysis (Klein’s line [21]), a normal alpha angle, and no tilt nor displacement of the epiphysis on the lateral view. Preoperative slip angle according to Southwick [39] was measured.
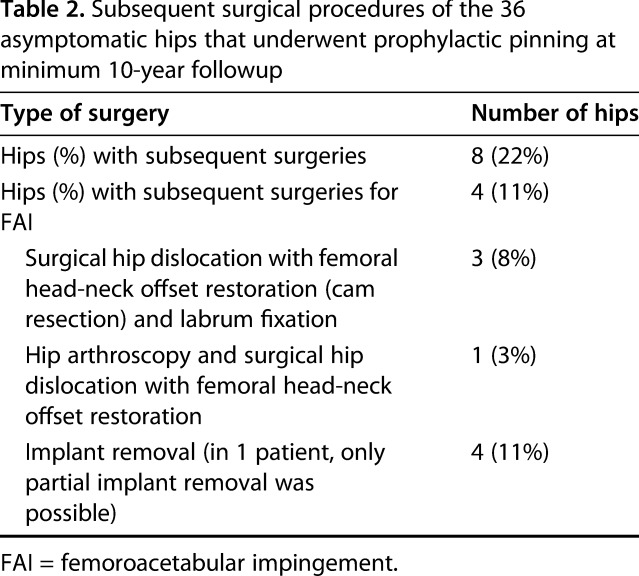
One of the authors (TDL) not involved in the surgical care of the patients reviewed the medical records for collection of preoperative demographic variables, including age at surgery, sex, and BMI. Data regarding intra- and postoperative complications were also collected along with any additional surgery during the study period (Table 2). The most recent clinical data including self-reported questionnaires, hip motion, and radiographs were assessed during a regular office visit by one of the authors (TDL) not involved in the surgical care of the patients.
Table 2.
Subsequent surgical procedures of the 36 asymptomatic hips that underwent prophylactic pinning at minimum 10-year followup
Description of Treatment/Operative Technique
For the prophylactic pinning, patients were positioned primarily in the supine position or occasionally in the lateral decubitus position, depending on the weight of the patient, on a radiolucent table. A small incision was made in the lateral aspect of the thigh and after dissection of the subcutaneous tissue, the fascia lata was split longitudinally. The vastus lateralis was split in line with its fibers by a scissor. A Hohmann retractor was placed anterior and posterior to the femur. A 2-mm Kirschner wire (not threaded) was placed on the anterior femoral neck to judge anteversion. Under fluoroscopic guidance, two fully threaded wires (size between 3.0 and 4.0 mm depending on the size of the patient) were introduced in the lateral cortex of the proximal femur and advanced into the proximal femoral epiphysis. Three wires were used in three patients because the position of two wires was deemed insufficient by the operating surgeon; in one patient, the fixation was performed with two 3.5-mm cortical screws. The rationale for using Kirschner wires was based on the relative simplicity of the procedure, their widespread availability, and our earlier excellent results using these implants. Adequate implant position was considered if the parallel or divergent placed Kirschner wires were crossing the physis in both AP and lateral projections. When proper positioning was seen on the image intensifier, the wires were cut 1 cm above the lateral cortex. The wound was closed in a standard fashion. All patients were allowed immediate full weightbearing on the side with prophylactic pinning.
Clinical Evaluation
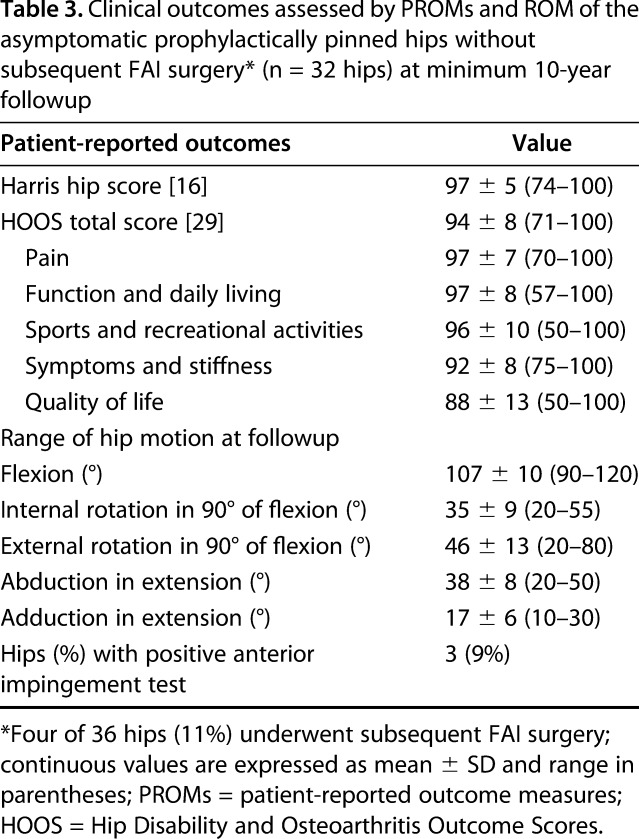
Self- or parent-reported reported outcome instruments were collected with questions regarding the left and right hips for the HHS [16] and the HOOS [20, 29]. The maximum HHS is 100 points; a score of 91 to 100 points corresponds to excellent hip function; 81 to 90 points is good function; 71 to 80 points means fair function; and ≤ 70 points equals poor hip function. The HOOS consists of 40 items assessing five dimensions: pain, function in activities of daily living, function in sport and recreation, hip-related quality of life, and other symptoms (Table 3). Each subscale has a score from 0 to 100, where 0 indicates extreme problem and 100 indicates no problem. The diagnosis of FAI during the followup period was based on a physical examination consistent with a painful (positive) impingement test [41] in association with limited internal rotation with the hip at 90o of flexion and abnormal femoral head-neck morphology on radiographs and MRI. Four patients with symptomatic cam-type FAI underwent direct MR arthrography for evaluation of the femoral head-neck junction, cartilage, and labrum damage. Any additional surgical treatment during the study period was recorded as part of the clinical outcome. Amplitudes of hip motion in flexion, abduction, adduction as well as internal and external rotation were assessed with the hip in 90° of flexion.
Table 3.
Clinical outcomes assessed by PROMs and ROM of the asymptomatic prophylactically pinned hips without subsequent FAI surgery* (n = 32 hips) at minimum 10-year followup
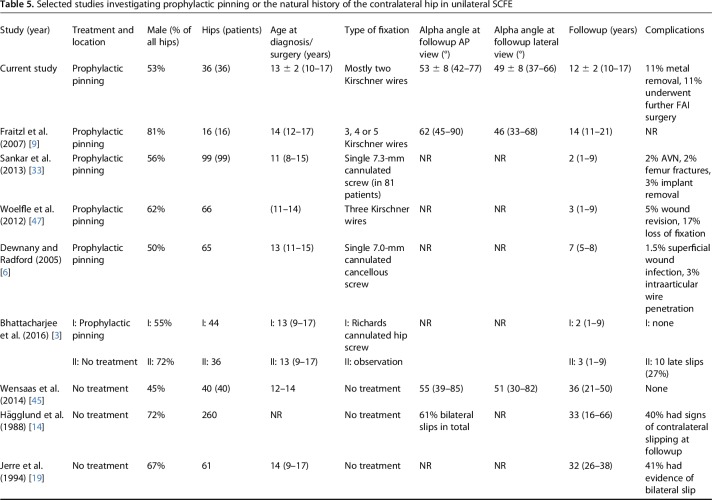
Radiographic Evaluation
Two authors (ENN, TDL) who were not involved in clinical care of the patients evaluated preoperative AP radiographs for the measurement of the femoral neck-shaft angle and the modified alpha angle for the AP view [11] to ascertain whether patients had coxa vara or cam morphology preoperatively (Table 4). Before surgery a lateral radiograph was often not feasible because of pain in the SCFE hip, which precluded frog-leg positioning. Postoperative radiographic variables of interest included the modified alpha angle for the AP view [11] and the alpha angle measured on the lateral (frog-leg or cross-table lateral) view [30]. The presence of a cam morphology was defined by an alpha angle measurement > 60° on the AP radiograph and/or > 55° on the lateral radiograph [1, 11, 30]. As secondary radiographic variables measured to assess the proximal femoral morphology, the neck-shaft angle and the articulotrochanteric distance were also measured. The normal reported mean values of the articulotrochanteric distance are 20 mm [7]. The normal reported slip angle is below 12° [26]. The normal reported offset of the femoral neck is 11.6 ± 0.7 mm, whereas hips with cam impingement have a decreased anterior offset of 7.2 ± 0.7 mm [8, 41]. Osteoarthritis was graded according to the classification of Tönnis [44] and joint space width was measured on AP pelvic radiographs with a film-focus distance of 1.2 m [41]. The central beam is directed to the midpoint between a line connecting both anterosuperior iliac spines and the superior border of the symphysis [41]. Three measurements of the joint space width were performed: medial, central, and lateral. The minimum of the three measurements was used as the outcome parameter.
Table 4.
Radiographic results for 29 asymptomatic prophylactically pinned hips without subsequent FAI surgery and complete radiographic followup at minimum 10 years (4 of 36 hips (11%) underwent subsequent FAI surgery and 3 hips had no radiographic followup)
Statistical Analysis and Reliability
Statistical analysis was performed using Winstat software (R. Fitch Software, Bad Krozingen, Germany). We tested normal distribution using the Kolmogorov-Smirnov test. Because all parameters were normally distributed, only parametric tests were used. We used the dependent t-test for continuous variables. To detect the reliability and reproducibility of three radiologic parameters (alpha angle, joint space width, and articulotrochanteric distance), 20 radiographs were randomly chosen from the image database of this patient cohort. Two independent observers (TDL, ENN) assessed the three radiologic parameters on AP radiographs on two separate occasions at least 2 weeks apart. Intraobserver agreement and interobserver agreement of the three radiologic parameters were calculated with the intraclass correlation coefficient (ICC). ICC was interpreted as moderate from 0.61 to 0.80 [28] and good from 0.81 to 1.0. The intraobserver agreement of the alpha angle was good for both observers (ICC of 0.71 for observer 1; ICC of 0.83 for observer 2). A good interobserver variability also was detected (ICC of 0.8 at both points).
Results
No intraoperative or postoperative complications with prophylactic in situ pinning were recorded. Four patients underwent symptomatic hardware removal and in one, the hardware was only able to be partially removed secondary to wire breakage (Table 2). Four of 36 (11%) patients (two males and two females) underwent subsequent additional surgery for symptomatic cam-type FAI during the followup period (Table 2). Three of these four patients underwent an open surgical hip dislocation with resection of the cam-type deformity and labrum refixation at 1, 4, and 8 years after the initial prophylactic pinning (Fig. 2). One patient had an unsuccessful hip arthroscopy for cam-type resection followed by an open surgical hip dislocation 11 years after the prophylactic pinning (Table 2). One patient developed asymptomatic Brooker Grade II heterotopic ossification around the trochanter that did not result in further surgery. No complications during subsequent FAI surgeries or hardware removals were recorded.
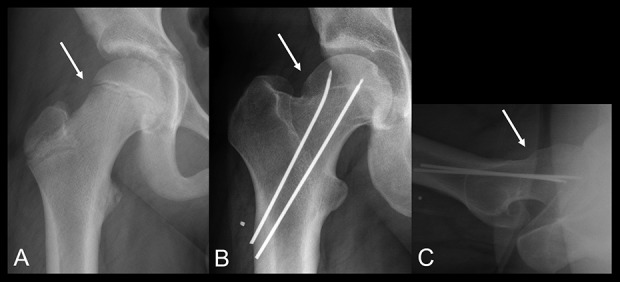
Fig. 2 A-D.
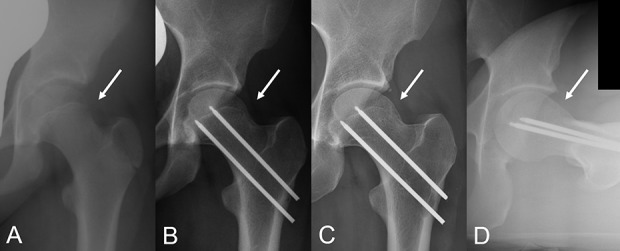
A 12-year-old female patient who initially presented with right hip pain underwent prophylactic pinning of the left asymptomatic hip. (A) The AP view of the left hip before surgery at age 12 years shows normal femoral head-neck junction (arrow). (B) The AP radiograph view obtained at 5 years postoperatively showing early signs of cam morphology development (arrow). (C) The AP radiograph obtained at 14 years after prophylactic pinning shows a clear abnormal femoral head and neck offset (arrow). (D) The lateral radiograph of the femur showing an aspherical femoral head-neck junction with a cam morphology anteriorly (arrow). The posterior aspect of the femoral neck is normal with no evidence of callus formation typical of SCFE. The cause of cam formation in this hip despite prophylactic pinning is unclear.
Overall, 10 of 33 hips (30% [seven males and three females]) had radiographic evidence of a cam-type morphology with an increased alpha angle at the femoral head-neck junction. As noted previously, four of 33 hips (12%) presented with a painful (symptomatic) cam-type FAI and underwent subsequent resection of the cam deformity (Table 2); the cam-type deformity was visible on the AP view in two patients (6%) and/or on the lateral view in two patients (6%). In the remaining six patients (18%), an abnormal alpha angle was seen on the AP view in three patients (9%) and on the AP and lateral views in three patients (9%). At most recent followup, 23 of 33 hips (70%) had a normal alpha angle on both the AP and lateral radiographic views. The mean alpha angle was 53° ± 8° on the AP radiograph and 49° ± 8° on the lateral view at followup in 29 hips (Table 4). The preoperative offset of the femoral head-neck junction was normal in all hips on both the AP and lateral radiographs (Table 4). At followup, the AP offset was 7 ± 3 mm and the lateral offset was 6 ± 3 mm (Table 4). Eight of 29 hips (28%) had an offset < 10 mm on the lateral view at followup. The preoperative Southwick angle (slip angle) averaged 8° ± 3°. No patient had radiographic signs of hip osteoarthritis (Tönnis Grade 0) at the latest followup of mean 12 ± 2 years. The mean minimum joint space width was 4 ± 0.4 mm. The articulotrochanteric distance showed a mean of 22 ± 5 mm and the neck-shaft angle averaged 135o ± 4° (Table 4). The articulotrochanteric distance represents the height of the greater trochanter and is considered normal above 20 mm. At final followup, 12 of 29 patients (41%) without subsequent surgery forcam FAI and complete radiographic followup had an articulotrochanteric distance below 20 mm.
The mean HHS for the 32 patients without subsequent FAI surgery (Fig. 3) for symptomatic cam FAI was 97 ± 5 (Table 3). Thirty-one patients (97%) who had not undergone subsequent FAI surgery (Fig. 4) had HHS equivalent to excellent function outcomes (> 91 points), whereas one patient (3%) had 74 points (fair function). The mean scores for the HOOS averaged 94 ± 8 (Table 3) for these 32 patients. The ROM for flexion averaged 107° ± 10° and for internal rotation in 90° of hip flexion 35° ± 9° (Table 1). Three of 32 patients (9%) presented with a positive anterior impingement test during the clinical examination at followup without having symptoms in daily life (Table 3).
Fig. 3 A-D.
A 14-year-old male patient with a preoperative (A) normal femoral head-neck junction (arrow), at 11 years (B) after prophylactic pinning of the asymptomatic right side and the lateral view (C) at 11-year followup are shown. (B) The AP radiograph and (C) the lateral view (C) at followup show a large cam morphology resembling a pistol grip deformity (arrows).
Fig. 4 A-C.
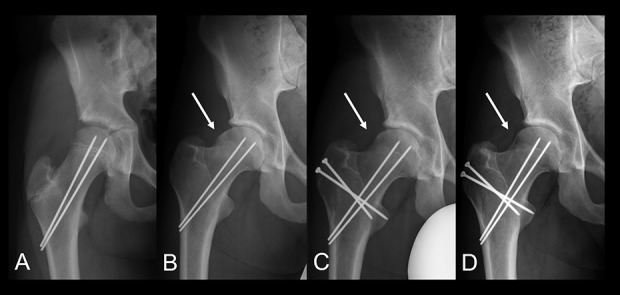
(A) A 14-year-old male patient underwent prophylactic pinning on the asymptomatic right side. The alpha angle was normal. (B) At 8-year followup, he presented with a symptomatic cam-type morphology (arrow) with an alpha angle of 62° on the lateral view and underwent surgical hip dislocation (C) for open cam resection (arrow). (D) At 10-year followup, he presented with a good clinical and radiographic outcome with an improved femoral head-neck junction (arrow) and normal alpha angle.
Discussion
The goals of prophylactic pinning are to prevent the development of SCFE, avoiding the risks of osteoarthritis associated with undiagnosed SCFE and the potential complications related to its treatment. These goals are based on the presumption that prophylactic fixation preserves the morphology of the proximal femur, preventing a postslip deformity that may be associated with FAI and hip osteoarthritis. However, long-term data supporting this assumption are lacking. In this small, retrospective study, we found no complications other than symptomatic hardware removal and high mean scores for hip-specific patient-reported outcomes and preservation of the normal femoral head and neck morphology in most patients at a minimum 10 years followup after prophylactic pinning. However, in 30% of patients (10 of 33), cam deformities developed, and in 11% (four of 36), they were symptomatic to undergo surgery for FAI. Although none have developed signs of osteoarthritis after minimal 10-year followup, these patients are still very young; most are in their third decade of life. The probability of developing degenerative changes of the hip in these patients thus persists.
This study had several limitations. The small sample size makes it likely that not all possible complications of these interventions would be observed here; this may be partially offset by the fact that at least this group was well surveyed: only one patient was completely lost to followup, and 33 of the remaining 36 were evaluated in person. Additionally, the lack of a control group makes it difficult to know with certainty whether prophylactic pinning in these patients would have improved the natural history of the condition. However, the fact that so many patients developed a cam deformity despite pinning makes us believe that perhaps more patients would have developed a cam deformity if they had not been pinned. The natural course of the asymptomatic and contralateral hip without prophylactic pinning in a patient with unilateral SCFE was investigated previously by others [45], and 10 years may be insufficient to determine whether osteoarthritis will develop in the group we treated; this is especially important to consider in light of the young age of these patients. Another potential limitation is related to the fact that an open subcapital realignment technique [40, 49, 50] was used for the treatment of the SCFE hip, and there was wide variation in the degree and severity of the slip among these patients. This could have impacted the functional outcomes of our patients. However, in our questionnaires, each item of the modified HHS and HOOS (Table 3) was collected for the left and right hip separately, allowing the patient to clearly differentiate between the hip that could be a source of dysfunction or pain. However, assessment of activity level is impossible to distinguish for each side and thus we did not report that specific score. In addition, we were not able to quantify femoral version because no CT or MRI scans were available for these patients. Abnormal femoral version could be an additional factor contributing to FAI and hip diseases resulting from the high prevalence of abnormal femoral version [24]. In addition, the measurement of the joint space width could theoretically be biased by magnification errors. We tried to minimize this bias with standardization of the projection of the AP pelvis radiograph and also utilizing the Tönnis grade. Furthermore, these patients with SCFE are thinner (BMI in Table 1) than most patients with SCFE reported in the orthopaedic literature. We believe that this factor may be more important for the symptomatic SCFE side rather than for the side undergoing prophylactic pinning. Finally, subgroup analysis for male and female patients was not possible because of the small sample size. This is important because of the known sex differences of development of cam-type FAI.
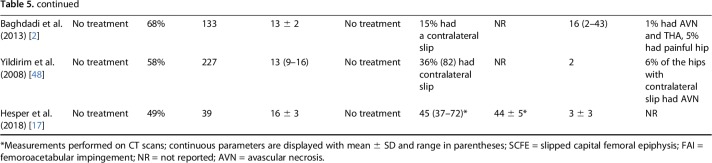
Prophylactic pinning of the contralateral radiographically normal-appearing side is associated with no complications, but additional procedures were performed in four patients (11%; Table 2) for symptomatic cam-type deformities and in another four patients for metal removal. Although Fraitzl et al. [9] reported no complications at 14-year followup after this procedure, others have reported complications associated with this procedure [33, 47]. Most frequently, these complications were symptomatic hardware, focal avascular necrosis, or proximal femur fractures at the entry point of screws [33]. The higher risk of complications in some of these studies could be caused by the larger study size or the larger number or size of implants such as screws or devices like a dynamic hip screw, which may promote these complications.
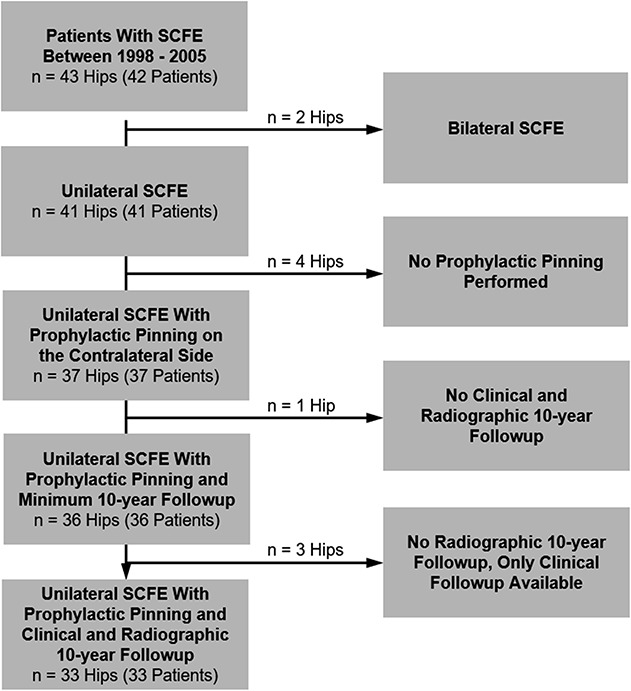
The contralateral and radiographically normal-appearing hips of patients with unilateral SCFE presented with cam-type deformities in 30% of hips at a mean followup of 12 years. Six of 33 patients (18%) developed a cam morphology of the femoral head-neck junction and remained asymptomatic at this time. However, an additional four hips (12%) with cam deformities became symptomatic and underwent surgical correction of the deformity (Table 2). Similar findings were reported by Fraitzl et al. [9] who found evidence of a cam deformity after prophylactic pinning in five of 16 patients (31%; Table 5). This is a relatively high prevalence in young patients and they are at high risk of having problems in the future. Fraitzl et al. [9] measured higher alpha angles (62°) on the AP view compared with our study (53°). However, the mean alpha angle of 53° ± 8° measured on the AP view at followup in our study is clearly higher (Table 4) than the 41° reported in a normative study in 200 asymptomatic participants [12]. Development of a cam deformity in the contralateral asymptomatic hip without prophylactic pinning in patients with unilateral SCFE has been reported with an even higher rate of approximately 40% [2, 3, 14, 19, 45, 48]. Thus, it seems clear that prophylactic pinning is not the cause of a later deformity. Prophylactic pinning may potentially decrease the rate of subsequent cam deformities through early stabilization of a potentially weak epiphysis. However, the benefit to prevent contralateral slip is clear but the benefit to prevent later cam-type FAI remains unclear. Hägglund et al. [14] reported that up to 40% had signs of contralateral slipping at followup ranging from 16 to 66 years (Table 5). Because prophylactic pinning could prevent a contralateral slip in our series, this seems to be a clear benefit to the authors. In the present series, there were no obvious signs of an abnormal orientation of the capital epiphysis (Fig. 3) or a previous silent capital slip of the femoral head at the time of surgery (Fig. 4). Because prophylactic pinning could prevent a contralateral slip, this would seem to justify the procedure to the authors, but we acknowledge that the prevention of later cam deformities requires further investigation.
Table 5.
Selected studies investigating prophylactic pinning or the natural history of the contralateral hip in unilateral SCFE
Development of osteoarthritis is an insidious process and our minimum 10-year followup is clearly too short to estimate the true incidence of hip osteoarthritis after prophylactic pinning. However, the fact that we did not identify any patient with radiographic osteoarthritis (Tönnis Grade 0) in this timeframe is encouraging. Previous long-term studies on the contralateral untreated hip reported osteoarthritic signs in approximately one-third of the hips that also developed an asymptomatic mild slip deformity over time. This was in contrast to osteoarthritic signs in 9% of the hips that did not develop signs of a mild slip over time [14, 19, 45]. Theoretically, prophylactic pinning might therefore reduce the number of later cam deformities and reduce the incidence of later osteoarthritis. Still, we need more refined diagnostic tools and/or more effective therapies to avoid growth abnormalities on the assumed normal-appearing hip. One-third of the patients in the epidemiologic cohort study of Agricola et al. [1] developed signs of hip osteoarthritis associated with a concomitant cam morphology after followup at 5 and 19 years. Hip arthroscopy for cam-type resection is increasingly performed without a complete understanding of the causes of the development of the cam deformity. An experimental ovine FAI model to simulate cam resection has been proposed recently and may help in understanding the development of the cam deformity using advanced MR techniques [34].
At an average 12-year followup after prophylactic pinning, the HHS and the HOOS assessing hip pain and function were good (Table 3) in all patients who did not undergo further FAI surgery, although it is important to remember that four patients did undergo this additional surgery. To compare the activity level is difficult because of the nature of the SCFE surgery here (modified Dunn procedure) and the fact that both hips underwent surgical procedures. We are aware of one intermediate-term study with a 14-year followup after prophylactic pinning. Fraitzl et al. [9] reported on 16 patients with prophylactic fixation of the contralateral (termed unaffected) hip. By assessing the Tegner and Lysholm activity scale [42], those authors found that most of their patients were generally not involved in athletic activities. Fraitzl et al. [9] reported that one of 16 patients (6%) had an activity level 3 of 10, eight of 16 (50%) had an activity level of 4 of 10, five of 16 patients (31%) had an activity level of 6 of 10, and two of 16 (13%) had an activity level of 9 of 10. In a 40-year followup study of patients treated for unilateral SCFE without prophylactic pinning of the contralateral hip, the mean modified HHS was rated good with 89 points, but 13% of the patients had a poor outcome [45]. In addition to the favorable clinical outcomes reported here, we also found that the hip ROM was normal (Table 3), which is in line with Fraitzl et al. [9]. Fraitzl et al. [9] found a positive impingement test in five of 16 (31%) patients. In our series, four of 36 patients (11%) underwent surgical treatment for symptomatic FAI (Fig. 2) and an additional three hips (9%) had a positive anterior impingement test [35] (Table 3). It is probable that the prevalence of a symptomatic positive anterior impingement test may have been underestimated in the past as a result of the lack of awareness of a potential underlying deformity or the absence of clinical tests and long-term radiographic studies after prophylactic pinning.
At minimum 10-year followup after prophylactic pinning of the contralateral radiographically normal hip in patients with a SCFE treated by the modified Dunn procedure, we detected no complications associated with the surgery in patients without further FAI surgery. Prophylactic pinning resulted in good clinical and functional outcomes without radiographic signs of osteoarthritis in this timeframe. However, 30% of the patients had radiographic evidence of a cam deformity and 11% of the patients underwent subsequent surgery for symptomatic cam impingement within the first 10 years after the initial pinning. Our findings in this small and retrospective study showed that prophylactic pinning does not guarantee a lifetime free of hip pain and hip impingement in all patients. Parents of patients with unilateral SCFE and physicians should be advised that there remains a risk for developing symptomatic FAI on the contralateral side, and patients should continue to be monitored in this regard.
Footnotes
The institution of one or more of the authors (MT) has received, during the study period, funding from the Swiss National Science Foundation.
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Bern, Bern, Switzerland.
References
- 1.Agricola R, Waarsing JH, Thomas GE, Carr AJ, Reijman M, Bierma-Zeinstra SMA, Glyn-Jones S, Weinans H, Arden NK. Cam impingement: defining the presence of a cam deformity by the alpha angle: data from the CHECK cohort and Chingford cohort. Osteoarthritis Cartilage . 2014;22:218–225. [DOI] [PubMed] [Google Scholar]
- 2.Baghdadi YMK, Larson AN, Sierra RJ, Peterson HA, Stans AA. The fate of hips that are not prophylactically pinned after unilateral slipped capital femoral epiphysis. Clin Orthop Relat Res . 2013;471:2124–2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhattacharjee A, Freeman R, Roberts AP, Kiely NT. Outcome of the unaffected contralateral hip in unilateral slipped capital femoral epiphysis: a report comparing prophylactic fixation with observation. J Pediatr Orthop B. 2016;25:454–458. [DOI] [PubMed] [Google Scholar]
- 4.Billing L, Severin E. Slipping epiphysis of the hip; a roentgenological and clinical study based on a new roentgen technique. Acta Radiol Suppl. 1959;174:1–76. [PubMed] [Google Scholar]
- 5.Crawford AH. Slipped capital femoral epiphysis. J Bone Joint Surg Am. 1988;70:1422–1427. [PubMed] [Google Scholar]
- 6.Dewnany G, Radford P. Prophylactic contralateral fixation in slipped upper femoral epiphysis: is it safe? J Pediatr Orthop B. 2005;14:429–433. [DOI] [PubMed] [Google Scholar]
- 7.Edgren W. Coxa plana. A clinical and radiological investigation with particular reference to the importance of the metaphyseal changes for the final shape of the proximal part of the femur. Acta Orthop Scand Suppl. 1965;Suppl 84:1-129. [PubMed] [Google Scholar]
- 8.Eijer H, Leunig M, Mahomed MN, Ganz R. Crosstable lateral radiograph for screening of anterior femoral head–neck offset in patients with femoro-acetabular impingement. Hip Int. 2001:37–41. [Google Scholar]
- 9.Fraitzl CR, Käfer W, Nelitz M, Reichel H. Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg Br. 2007;89:1592–1596. [DOI] [PubMed] [Google Scholar]
- 10.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res . 2003;417:112–120. [DOI] [PubMed] [Google Scholar]
- 11.Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89:1309–1316. [DOI] [PubMed] [Google Scholar]
- 12.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. [DOI] [PubMed] [Google Scholar]
- 13.Hägglund G. The contralateral hip in slipped capital femoral epiphysis. J Pediatr Orthop B. 1996;5:158–161. [DOI] [PubMed] [Google Scholar]
- 14.Hägglund G, Hansson LI, Ordeberg G, Sandström S. Bilaterality in slipped upper femoral epiphysis. J Bone Joint Surg Br. 1988;70:179–181. [DOI] [PubMed] [Google Scholar]
- 15.Hansson G, Nathorst-Westfelt J. Management of the contralateral hip in patients with unilateral slipped upper femoral epiphysis: to fix or not to fix--consequences of two strategies. J Bone Joint Surg Br. 2012;94:596–602. [DOI] [PubMed] [Google Scholar]
- 16.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 17.Hesper T, Bixby SD, Maranho DA, Miller P, Kim Y-J, Novais EN. Morphologic features of the contralateral femur in patients with unilateral slipped capital femoral epiphysis resembles mild slip deformity: a matched cohort study. Clin Orthop Relat Res . 2018;476:890–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jerre R, Billing L, Hansson G, Karlsson J, Wallin J. Bilaterality in slipped capital femoral epiphysis: importance of a reliable radiographic method. J Pediatr Orthop B. 1996;5:80–84. [DOI] [PubMed] [Google Scholar]
- 19.Jerre R, Billing L, Hansson G, Wallin J. The contralateral hip in patients primarily treated for unilateral slipped upper femoral epiphysis. Long-term follow-up of 61 hips. J Bone Joint Surg Br. 1994;76:563–567. [PubMed] [Google Scholar]
- 20.Klässbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score. An extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand J Rheumatol . 2003;32:46–51. [DOI] [PubMed] [Google Scholar]
- 21.Klein A, Joplin RJ, Reidy JA, Hanelin J. Slipped capital femoral epiphysis; early diagnosis and treatment facilitated by normal roentgenograms. J Bone Joint Surg Am. 1952;34:233–239. [PubMed] [Google Scholar]
- 22.Kocher MS, Bishop JA, Hresko MT, Millis MB, Kim Y-J, Kasser JR. Prophylactic pinning of the contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2004;86:2658–2665. [DOI] [PubMed] [Google Scholar]
- 23.Lehmann CL, Arons RR, Loder RT, Vitale MG. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop. 2006;26:286–290. [DOI] [PubMed] [Google Scholar]
- 24.Lerch TD, Todorski IAS, Steppacher SD, Schmaranzer F, Werlen SF, Siebenrock KA, Tannast M. Prevalence of femoral and acetabular version abnormalities in patients with symptomatic hip disease: a controlled study of 538 hips. Am J Sports Med. 2018;46:122–134. [DOI] [PubMed] [Google Scholar]
- 25.Leunig M, Casillas MM, Hamlet M, Hersche O, Nötzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. [DOI] [PubMed] [Google Scholar]
- 26.Loder RT. Slipped capital femoral epiphysis. Am Fam Physician. 1998;57:2135–2142, 2148–2150. [PubMed] [Google Scholar]
- 27.Loder RT, Aronson DD, Greenfield ML. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am. 1993;75:1141–1147. [DOI] [PubMed] [Google Scholar]
- 28.Montgomery AA, Graham A, Evans PH, Fahey T. Inter-rater agreement in the scoring of abstracts submitted to a primary care research conference. BMC Health Serv Res. 2002;2:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. [DOI] [PubMed] [Google Scholar]
- 31.Nowicki PD, Silva S, Toelle L, Strohmeyer G, Wahlquist T, Li Y, Farley FA, Caird MS. Severity of asynchronous slipped capital femoral epiphyses in skeletally immature versus more skeletally mature patients. J Pediatr Orthop. 2017;37:e23–e27. [DOI] [PubMed] [Google Scholar]
- 32.Riad J, Bajelidze G, Gabos PG. Bilateral slipped capital femoral epiphysis: predictive factors for contralateral slip. J Pediatr Orthop. 2007;27:411–414. [DOI] [PubMed] [Google Scholar]
- 33.Sankar WN, Novais EN, Lee C, Al-Omari AA, Choi PD, Shore BJ. What are the risks of prophylactic pinning to prevent contralateral slipped capital femoral epiphysis? Clin Orthop Relat Res . 2013;471:2118–2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmaranzer F, Arendt L, Lerch TD, Steppacher SD, Nuss K, Wolfer N, Dawson HE, von Rechenberg B, Kircher PR, Tannast M. Femoral osteochondroplasty can be performed effectively without the risk of avascular necrosis or femoral neck fractures in an experimental ovine FAI model. Osteoarthritis Cartilage . 2018;26:128–137. [DOI] [PubMed] [Google Scholar]
- 35.Schmaranzer F, Hanke M, Lerch T, Steppacher S, Siebenrock K, Tannast M. [Impingement of the hip] [in German]. Radiologe. 2016;56:825–838. [DOI] [PubMed] [Google Scholar]
- 36.Schultz WR, Weinstein JN, Weinstein SL, Smith BG. Prophylactic pinning of the contralateral hip in slipped capital femoral epiphysis: evaluation of long-term outcome for the contralateral hip with use of decision analysis. J Bone Joint Surg Am. 2002;84:1305–1314. [DOI] [PubMed] [Google Scholar]
- 37.Seller K, Raab P, Wild A, Krauspe R. Risk-benefit analysis of prophylactic pinning in slipped capital femoral epiphysis. J Pediatr Orthop B. 2001;10:192–196. [PubMed] [Google Scholar]
- 38.Sink EL, Zaltz I, Heare T, Dayton M. Acetabular cartilage and labral damage observed during surgical hip dislocation for stable slipped capital femoral epiphysis. J Pediatr Orthop. 2010;30:26–30. [DOI] [PubMed] [Google Scholar]
- 39.Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49:807–835. [PubMed] [Google Scholar]
- 40.Tannast M, Jost LM, Lerch TD, Schmaranzer F, Ziebarth K, Siebenrock KA. The modified Dunn procedure for slipped capital femoral epiphysis: the Bernese experience. J Child Orthop. 2017;11:138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. [DOI] [PubMed] [Google Scholar]
- 42.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res . 1985;198:43–49. [PubMed] [Google Scholar]
- 43.Thawrani DP, Feldman DS, Sala DA. Current practice in the management of slipped capital femoral epiphysis. J Pediatr Orthop. 2016;36:e27-37. [DOI] [PubMed] [Google Scholar]
- 44.Tönnis D. General radiography of the hip joint. In: Tönnis D, ed. Congenital Dysplasia, Dislocation of the Hip. New York, NY, USA: Springer; 1987. [Google Scholar]
- 45.Wensaas A, Gunderson RB, Svenningsen S, Terjesen T. Good long-term outcome of the untreated contralateral hip in unilateral slipped capital femoral epiphysis: forty hips with a mean follow-up of 41 years. J Child Orthop. 2014;8:367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Witbreuk M, Besselaar P, Eastwood D. Current practice in the management of acute/unstable slipped capital femoral epiphyses in the United Kingdom and the Netherlands: results of a survey of the membership of the British Society of Children’s Orthopaedic Surgery and the Werkgroep Kinder Orthopaedie. J Pediatr Orthop B. 2007;16:79–83. [DOI] [PubMed] [Google Scholar]
- 47.Woelfle JV, Fraitzl CR, Reichel H, Nelitz M. The asymptomatic contralateral hip in unilateral slipped capital femoral epiphysis: morbidity of prophylactic fixation. J Pediatr Orthop B. 2012;21:226–229. [DOI] [PubMed] [Google Scholar]
- 48.Yildirim Y, Bautista S, Davidson RS. Chondrolysis, osteonecrosis, and slip severity in patients with subsequent contralateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2008;90:485–492. [DOI] [PubMed] [Google Scholar]
- 49.Ziebarth K, Milosevic M, Lerch TD, Steppacher SD, Slongo T, Siebenrock KA. High survivorship and little osteoarthritis at 10-year followup in SCFE patients treated with a modified Dunn procedure. Clin Orthop Relat Res . 2017;475:1212–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim Y-J. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res . 2009;467:704–716. [DOI] [PMC free article] [PubMed] [Google Scholar]