Abstract
Background
The treatment of mild or borderline acetabular dysplasia is controversial with surgical options including both arthroscopic labral repair with capsular closure or plication and periacetabular osteotomy (PAO). The degree to which improvements in pain and function might be achieved using these approaches may be a function of acetabular morphology and the severity of the dysplasia, but detailed radiographic assessments of acetabular morphology in patients with a lateral center-edge angle (LCEA) of 18° to 25° who have undergone PAO have not, to our knowledge, been performed.
Questions/purposes
(1) Do patients with an LCEA of 18° to 25° undergoing PAO have other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum? (2) What is the survivorship free from revision surgery, THA, or severe pain (modified Harris hip score [mHHS] < 70) and proportion of complications as defined by the modified Dindo-Clavien severity scale at minimum 2-year followup? (3) What are the functional patient-reported outcome measures in this cohort at minimum 2 years after surgery as assessed by the UCLA Activity Score, the mHHS, the Hip disability and Osteoarthritis Outcome Score (HOOS), and the SF-12 mental and physical domain scores?
Methods
Between January 2010 and December 2014, a total of 91 patients with hip pain and LCEA of 18° to 25° underwent a hip preservation surgical procedure at our institution. Thirty-six (40%) of the 91 patients underwent hip arthroscopy, and 56 hips (60%) were treated by PAO. In general, patients were considered for hip arthroscopy when symptoms were predominantly associated with femoroacetabular impingement (that is, pain aggravated by sitting and hip flexion activities) and physical examination showed a positive anterior impingement test with negative signs of instability (negative anterior apprehension test). In general, patients were considered for PAO when symptoms suggested instability (that is, pain with upright activities, abductor fatigue now aggravated by sitting) and clinical examinations demonstrated a positive anterior apprehension test. Bilateral surgery was performed in six patients and only the first hip was included in the study. One patient was excluded because PAO was performed to address dysplasia caused by surgical excision of a proximal femoral tumor associated with multiple epiphyseal dysplasia during childhood yielding a total of 49 patients (49 hips). There were 46 of 49 females (94%), the mean age was 26.5 years (± 8), and the mean body mass index was 24 kg/m2 (± 4.5). Radiographic analysis of preoperative films included the LCEA, Tönnis acetabular roof angle, the anterior center-edge angle, the anterior and posterior wall indices, and the Femoral Epiphyseal Acetabular Roof index. Thirty-nine of the 49 patients (80%) were followed for a minimum 2-year followup (mean, 2.2 years; range, 2-4 years) and were included in the analysis of survivorship after PAO, complications, and functional outcomes. Kaplan-Meier modeling was used to calculate survivorship defined as free from revision surgery, THA, or severe pain (mHHS < 70) at minimum 2 years after surgery. Complications were graded according to the modified Dindo-Clavien severity. Patient-reported outcomes were collected preoperatively and at minimum 2 years after surgery and included the UCLA Activity Score, the mHHS, the HOOS, and the SF-12 mental and physical domain scores.
Results
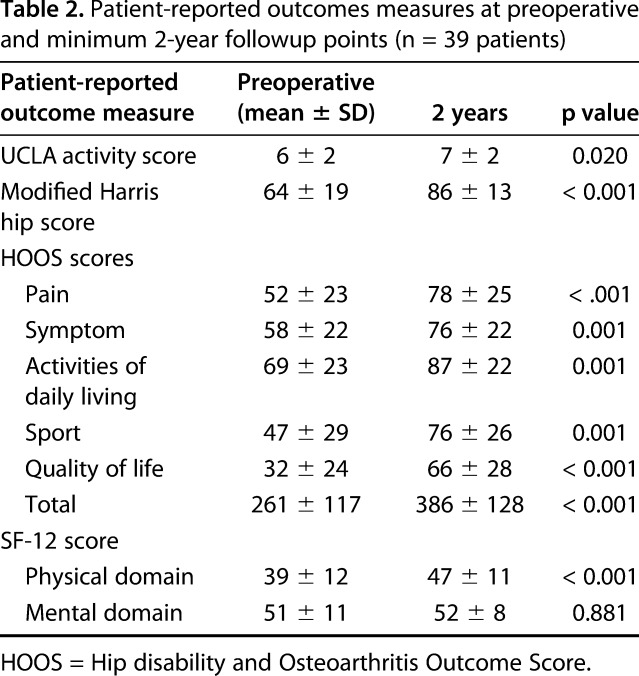
Forty-six of 49 hips (94%) had at least one other radiographic feature of dysplasia suggestive of abnormal femoral head coverage by the acetabulum. Seventy-three percent of the hips (36 of 49) had two or more radiographic features of hip dysplasia aside from a LCEA of 18° to 25°. The survivorship of PAO at minimum 2 years for the 39 of 49 (80%) patients available was 94% (95% confidence interval, 80%-90%). Three of 39 patients (8%) developed a complication. At a mean of 2.2 years of followup, there was improvement in level of activity (preoperative UCLA score 7 ± 2 versus postoperative UCLA score 6 ± 2; p = 0.02). Hip symptoms and function improved postoperatively, as reflected by a higher mean mHHS (86 ± 13 versus 64 ± 19; p < 0.001) and mean HOOS (386 ± 128 versus 261 ± 117; p < 0.001). Quality of life and overall health assessed by the physical domain of the SF-12 improved (47 ± 11 versus 39 ± 12; p < 0.001). However, with the numbers available, no improvement was observed for the mental domain of the SF-12 (52 ± 8 versus 51 ± 11; p = 0.881).
Conclusions
Hips with LCEA of 18° to 25° frequently have other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum. These hips may be inappropriately labeled as “borderline” or “mild” dysplasia on consideration of LCEA alone. A more comprehensive imaging analysis in these hips by the radiographic features of dysplasia included in this study is recommended to identify hips with abnormal coverage of the femoral head by the acetabulum and to plan treatment accordingly. Patients with LCEA of 18° to 25° showed improvement in hip pain and function after PAO with minimal complications and low proportions of persistent pain or reoperations at short-term followup. Future studies are recommended to investigate whether the benefits of symptomatic and functional improvement are sustained long term.
Level of Evidence
Level IV, therapeutic study.
Introduction
Acetabular dysplasia is defined as osseous deficiency of the acetabulum with abnormal coverage of the femoral head leading to overload of the rim and joint instability [14, 17]. Acetabular dysplasia may cause damage of the acetabular labrum and cartilage and ultimately lead to premature osteoarthritis [6, 27, 29, 36]. Several studies have demonstrated the success of the Bernese periacetabular osteotomy (PAO) described by Ganz et al. [12] in the treatment of classic acetabular dysplasia with lateral center-edge angle (LCEA) < 20° at both intermediate- and long-term followup [12, 20, 23, 42, 44]. However, to the best of our knowledge, only one prior study has focused specifically on outcomes of PAO in patients with an LCEA between 18° and 25° [37]. In that study, 27 patients demonstrated improvement in hip-specific outcomes and few complications at 1 year postoperatively. Further understanding of patient-reported outcomes, risk of reoperation, and complications of PAO in hips with LCEA of 18° to 25° is important because controversy surrounds the optimal treatment of these patients. For instance, hip arthroscopy with labrum repair and treatment of associated cam femoroacetabular impingement (FAI) morphology and capsular closure or plication have also been described for such patients with varying degrees of success [3, 4, 11, 16, 18, 25, 31].
Hip dysplasia has been historically identified by measurement of the LCEA described by Wiberg [45]. The original description considered hips with LCEA > 25° as normal hips and those with LCEA < 20° as pathologic. Wiberg considered hips with LCEA between 20° and 25° as uncertain. Subsequent studies have interchangeably described hips with LCEA between 18° and 25° as mild dysplastic [11, 25, 27, 38] or borderline dysplastic [4, 9, 11, 13, 16, 31]. Recent studies have suggested that the analysis of the hip based on a single measurement of the LCEA is limited [10, 15, 22, 33, 46]. Three-dimensional analysis has shown that hip dysplasia has a variety of forms with acetabular undercoverage patterns being found in anterior, lateral, and posterior acetabular regions [33, 46]. Furthermore, since the description of the LCEA, several other radiographic features of dysplasia including the anterior center-edge angle (ACEA) [19], the acetabular wall indices [39], the Femoral Epiphyseal Acetabular Roof (FEAR) index, and the Tönnis acetabualar roof angle [43] have been described to evaluate coverage of the femoral head by the acetabulum. To the best of our knowledge, a comprehensive radiographic assessment of acetabular morphology in patients with an LCEA of 18° to 25° undergoing PAO is lacking.
We therefore asked the following questions: (1) Do patients with an LCEA of 18° to 25° undergoing PAO have other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum? (2) What is the survivorship free from revision surgery, THA, or severe pain (modified Harris hip score [mHHS] < 70) and proportion of complications as defined by the modified Dindo-Clavien severity scale at minimum 2-year followup? (3) What are the functional patient-reported outcome measures (PROMs) in this cohort at minimum 2 years after surgery, as assessed by the UCLA Activity Score, the mHHS, the Hip disability and Osteoarthritis Outcome Score (HOOS), and the SF-12 mental and physical domain scores?
Patients and Methods
Institutional review board approval was obtained before this retrospective study. Between January 2010 and December 2014, a total of 91 patients with hip pain and LCEA of 18° to 25° underwent a hip preservation surgical procedure at our institution. The reference range of LCEA between 18° and 25° was chosen based on previous studies describing “mild” [11, 25, 27, 38] or “borderline” [4, 9, 11, 13, 16, 31] acetabular dysplasia. Thirty-six (40%) of the 91 patients underwent hip arthroscopy, and 56 hips (60%) were treated by PAO. In general, patients were considered for hip arthroscopy when symptoms were predominantly associated with FAI (that is, pain aggravated by sitting and hip flexion activities) and physical examination showed a positive anterior impingement test [17] with negative signs of instability (negative anterior apprehension test [21]). Conversely, patients were considered for PAO when symptoms suggested instability (that is, pain with upright activities, abductor fatigue now aggravated by sitting) and clinical examinations demonstrated a positive anterior apprehension test [21]. A contraindication to PAO was Tönnis Grade 2 osteoarthritis without remaining cartilage to correct into the weightbearing zone. Notably, all hips were classified as Tönnis arthritic Grade 0 preoperatively.
Three surgeons performed the operations (Y-JK, MBM, Y-MY). One surgeon performed both PAO and arthroscopic surgeries (Y-JK), one surgeon performed only hip arthroscopy (Y-MY), and one surgeon performed only PAO (MBM). Bilateral surgery was performed in six patients and only the first hip was included in the study. One patient was excluded because PAO was performed to address dysplasia caused by surgical excision of a proximal femoral tumor associated with multiple epiphyseal dysplasia during childhood yielding a total of 49 patients (49 hips) included in the study. For the radiographic analysis of other features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum, all 49 hips were included. There were 46 of 49 females (94%), the mean age was 26.5 years (± 8), and the mean body mass index (BMI) was 24 kg/m2 (± 4.5).
Thirty-nine of the 49 patients (80%) were followed for a minimum 2-year followup and were included in the analysis of survivorship after PAO, complications, and functional outcomes. There were 37 (95%) females, the mean age was 25.8 years (± 8.4 years), and mean BMI was 23.6 kg/m2 (± 4.3). The mean followup was 2.2 years and the range of followup was 2 to 4 years. Five patients (five of 39 [13%]) had undergone previous ipsilateral hip surgery. Hip arthroscopy with labral repair or débridement was the most frequent prior procedure (n = 4 [10%]), whereas one patient each had undergone an intertrochanteric osteotomy for pathologic femoral anteversion and a varus derotational osteotomy in childhood for developmental dysplasia of the hip (DDH). One patient was treated with abduction orthosis in infancy for DDH but required no other interventions until the PAO.
Surgical Technique
Surgery was performed following the surgical technique for PAO described by Ganz et al. [12] with a modified rectus femoris-sparing approach as described by Novais et al. [12, 24, 30, 34]. Arthroscopy before PAO or arthrotomy during PAO was performed for the treatment of intraarticular pathology including labral tear or associated abnormal femoral head-neck offset pathology as indicated on a patient-by-patient basis. At the time of PAO, two patients (two of 39 [5%]) underwent hip arthroscopy, and one patient underwent repair of a labral tear. Ten of 39 (26%) patients underwent arthrotomy after PAO was complete. In eight of those patients (eight of 39 [20%]), a femoral head-neck osteochondroplasty was performed for the treatment of associated asphericity leading to potential impingement. After correction of acetabular coverage, six patients (11%) underwent osteoplasty of the anteroinferior iliac spine (AIIS). Partial weightbearing was continued for 6 to 10 weeks (or until there was radiographic evidence of bone healing), and then progressive weightbearing and increased ROM were allowed. Low-dose aspirin was used for perioperative prophylaxis from deep venous thrombosis for 1 month postoperatively. Implant removal was typically offered 12 months postoperatively.
For the radiographic analysis of other features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum, all 49 hips were included. Aside from the LCEA, on the preoperative standing AP pelvic radiograph, we measured the acetabular roof angle as described by Tönnis [43], the anterior and posterior wall indices as described by Siebenrock et al. [39], and the FEAR index as described by Wyatt et al. [47]. The ACEA of Lequesne and de Seze was measured on the preoperative false profile radiograph [19] (Fig. 1). All measurements were performed by a fellowship-trained orthopaedic surgeon (MPM) using a validated software package specific to hip angle measurements [32]. We did not specifically assess reliability of the radiographic parameters of interest. A recent study reported that intrarater reliability for the acetabular index was 0.94 (95% confidence interval [CI], 0.91-0.96), for anterior acetabular wall index was 0.78 (95% CI, 0.54-0.92), and for FEAR index 0.93 (95% CI, 0.87-0.95) [7]. In the same study, interrater reliability was 0.90 for the acetabular index (95% CI, 0.84-0.93), 0.68 for the anterior acetabular wall index (95% CI, 0.43-0.84), and 0.83 (95% CI, 0.74-0.88) for the FEAR index.
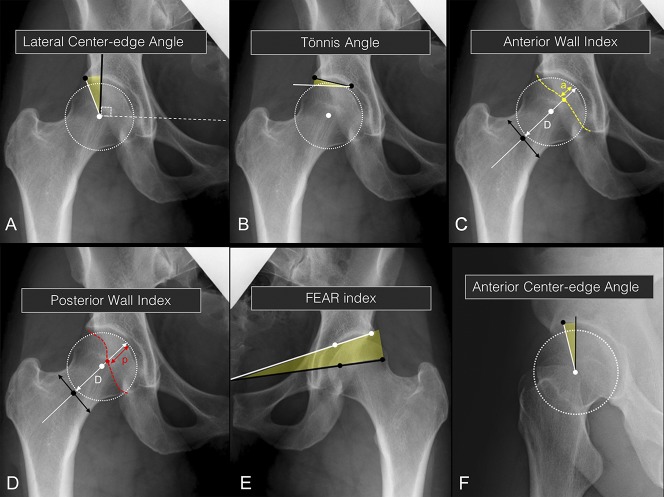
Fig. 1 A-F.
Radiographic measurements used to assess acetabular morphology and femoral head coverage by the acetabulum used in the study are shown. (A) The LCEA [45] is the angle formed between a perpendicular line (black line) to the line that connects the center of the femoral heads (white dashed lines) and a line (white line) that connects the center of the femoral head to the most lateral point (black circle) of the acetabular sourcil. (B) The Tönnis angle [43] is the angle formed between a line (black line) drawn between the most lateral and most medial points of the acetabular sourcil and a parallel line (white line) to the line connecting the center of the femoral heads that passes through the most medial point of the acetabular sourcil. (C) The anterior wall index [39] is measured after the diameter (D) of the femoral head is drawn (white arrow = distance D) in line with the axis of the femoral neck defined by the midpoint (black circle) of the neck. The yellow dot represents the point where the axis of the femoral neck passes through the anterior wall (yellow dashed line). The anterior wall index is calculated by dividing distance (a) by the diameter (D) of the femoral head. (D) The posterior wall index [39] is measured after the diameter (D) of the femoral head is drawn (white arrow = distance D) in line with the axis of the femoral neck defined by the midpoint (black circle) of the neck. The red dot represents the point where the axis of the femoral neck passes through the posterior wall (red dashed line). The posterior wall index is calculated by dividing distance (p) by the diameter (D) of the femoral head. (E) The FEAR index [47] is the angle formed between a line (black line) representing the physeal scar of the femoral head and a line (white line) connecting the most medial and lateral points of the acetabular sourcil. (F) The ACEA [19] is measured in the false profile radiograph by drawing a vertical longitudinal line (black line) passing through the center of the femoral head. The ACEA is the angle formed by the vertical line and a line (white line) connecting the center of the femoral head to the most anterior point (black dot) of the acetabular sourcil.
Kaplan-Meier modeling was used to calculate survivorship defined as free from revision surgery, THA, or severe pain (mHHS < 70) at minimum 2 years after surgery. All perioperative complications were recorded from a review of the electronic medical records performed by one of the authors not involved in the patients’ clinical care (MPM). Complications were graded following an adaptation of the Clavien-Dindo system [41] that has been previously validated for hip preservation surgery [41]. In brief, a Grade I complication is trivial and implies no treatment; a Grade II complication requires outpatient pharmacologic treatment or close monitoring; a Grade III complication requires surgical treatment as an inpatient; a Grade IV complication is life-threatening with high morbidity; and Grade V is death.
We collected activity, pain, and health-related quality-of-life outcomes preoperatively and postoperatively at 1 year and minimum 2-year followup with the use of a hip questionnaire that included the UCLA Activity Score, mHHS (pain, function, and activity sections), the HOOS which includes the WOMAC scores, and SF-12 mental and physical domain scores. Thirty-nine of the 49 patients (80%) were followed for a minimum 2-year followup and were included in the analysis of survivorship after PAO, complications, and functional outcomes.
Statistical Analysis
Continuous variables are reported as mean ± SD with a p value and 95% CI. Categorical variables are reported as percentages. Kaplan-Meier modeling was used to calculate survivorship defined as free from revision surgery, THA, or severe pain (mHHS < 70) at minimum 2 years after surgery. We tested changes between preoperative and postoperative values with paired-sample t-tests.
Results
Presenting Radiographic Measures in Patients With LCEA of 18°-25° Undergoing PAO
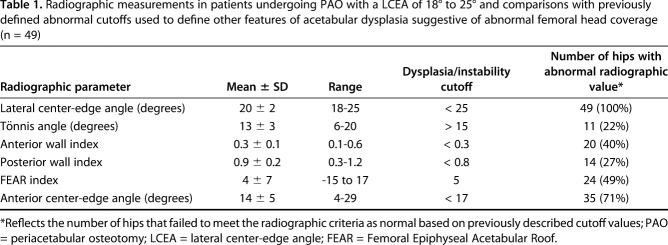
Patients with LCEA of 18° to 25° who underwent PAO often presented with other radiographic features of dysplasia. Of the 49 patients included in the radiographic analysis, 35 (71%) presented with an abnormally low ACEA suggesting insufficient anterior femoral head coverage by the acetabulum, whereas 20 (40%) had a low anterior wall index, which is another parameter used to assess anterior coverage. Twenty-four (49%) patients presented with an abnormal FEAR index, suggestive of hip pain associated with instability rather than impingement. The acetabular inclination assessed by the Tönnis angle was considered dysplastic in 11 (22%) of the patients. The mean ACEA (14° ± 5°) was below the 17° threshold considered for defining a hip as dysplastic (Table 1). Overall, 46 of 49 hips (94%) had at least one other radiographic feature of dysplasia suggestive of abnormal femoral head coverage by the acetabulum. Seventy-three percent of the hips (36 of 49) had two or more radiographic features of hip dysplasia aside from a LCEA of 18° to 25°. Only three of 49 (6%) patients had an LCEA of 18° to 25° as the single radiographic feature of dysplasia with all other parameters assessed being within normal range.
Table 1.
Radiographic measurements in patients undergoing PAO with a LCEA of 18° to 25° and comparisons with previously defined abnormal cutoffs used to define other features of acetabular dysplasia suggestive of abnormal femoral head coverage (n = 49)
Survival and Complication Profiles 2 Years After PAO
Kaplan-Meier survivorship free from revision surgery, THA, or severe pain (mHHS < 70) was 94% (95% CI, 80%-90%) at a mean followup of 2.2 years (range, 2-4 years). No patients underwent conversion to THA or revision surgery. Four patients had postoperative mHHS scores < 70 at latest followup and were classified as unsuccessful for the purpose of survival. Therefore, the total failure rate in the current study was 9%.
Three of 39 patients (8%) developed a complication after PAO. Two patients (5%) had neurapraxia of the lateral femoral cutaneous nerve (Grade II complication) requiring outpatient treatment but no major changes in their postoperative course. One patient (3%) developed a pulmonary embolism (Grade IV, major complication).
Patient-reported Outcome Measures After PAO in Hips With LCEA of 18°-25°
At a mean of 2.2 years of followup, there was an improvement in level of activity (preoperative UCLA score 7 ± 2 versus postoperative UCLA score 6 ± 2; p = 0.02). Hip symptoms and function improved postoperatively, as reflected by a higher mean mHHS (86 ± 13 versus 64 ± 19; p < 0.001) and mean HOOS (386 ± 128 versus 261 ± 117; p < 0.001). Quality of life and overall health assessed by the physical domain of the SF-12 improved (47 ± 11 versus 39 ± 12; p < 0.001). However, with the numbers available, no improvement was observed for the mental domain of the SF-12 (52 ± 8 versus 51 ± 11; p = 0.881; Table 2).
Table 2.
Patient-reported outcomes measures at preoperative and minimum 2-year followup points (n = 39 patients)
Discussion
Patients with an LCEA of 18° to 25° commonly are labeled as having “mild” or “borderline” dysplasia. However, the use of these terms based solely on the measurement of the LCEA is unspecific, controversial, and insufficient in determining the true degree of acetabular dysplasia. The location and severity of abnormal coverage of the femoral head by the dysplastic acetabulum are important factors to consider when deciding the best surgical treatment for these hips. Moreover, understanding the acetabular morphology is crucial for planning correction during PAO. In our radiographic review of patients with an LCEA of 18° to 25° undergoing PAO, we found that these patients have numerous radiographic features indicative of insufficient acetabular coverage aside from the LCEA. A low proportion of patients developed minor complications associated with the lateral femoral cutaneous nerve and only one patient had a serious complication (Grade IV, pulmonary embolism). In general, these patients achieved high PROM scores after PAO with no patients in this series having undergone revision surgery or THA at this short 2-year followup.
This study has several limitations. First, there is a potential risk of selection bias because during the study period, we treated symptomatic patients with an LCEA of 18° to 25° with either PAO or arthroscopic procedures and we only evaluated patients undergoing PAO in this study. However, in general, our indications for PAO versus arthroscopic procedures remained consistent and were based on differences in presenting symptoms and physical examination findings rather than acetabular morphology. In general, patients were considered for PAO when symptoms were suggestive of instability including pain with upright activities, abductor fatigue, and their examination showed a positive anterior apprehension test. Patients were considered for arthroscopic procedures when symptoms were predominantly the result of FAI (pain aggravated by sitting and hip flexion activities) and physical examination showed a positive anterior impingement test with negative signs of instability (anterior apprehension test). Second, our study lacks a control group of patients with LCEA 18° to 25°, which would allow for direct comparisons of indications, complications, survivorship, and PROMs. This is the logical next step and we plan to perform this in a prospective longitudinal comparative study. Third, our analysis does not include a three-dimensional (3-D) assessment of the hip morphology by CT, which would have provided a more robust evaluation of the hip morphology. A previous study of 50 patients with classic acetabular dysplasia (LCEA < 20°) suggested three patterns of acetabular deficiency in mild to severe dysplasia and highlighted the importance of 3-D analysis [33]. Although we obtained MRI on our patients preoperatively, we did not use CT imaging as routine, which limits our evaluation to plain film radiographic parameters. Nevertheless, we were able to show that patients with LCEA of 18° to 25° have several other features of dysplasia suggesting different patterns of acetabular insufficiency that may be better investigated in future studies using 3-D imaging. We also did not include in this study assessment of ligamentous laxity, hypermobility, and femoral version, which will be the focus of planned future investigations. Fourth, 10 (20%) patients were lost to the minimum followup of 2 years. All patients could be included in the radiographic analysis based on preoperative films; however, we limited the analysis of complications, survivorship, and PROMs to patients with minimum 2-year followup. This group could likely represent the best-case outcomes, so our results should be interpreted as such. Similarly, it is important to note that longer term followup of these patients is critical to truly evaluate the benefits of PAO for an LCEA of 18° to 25°. Fifth, although most patients in the study underwent an isolated PAO, approximately one-fourth of the patients had additional treatment during the PAO including osteochondroplasty of the femoral head-neck junction (10 of 39 [26%]), osteoplasty of the AIIS (six of 39 [15%]), and labral repair (one of 39 [2%]). The effect of these procedures on outcomes after PAO was not controlled for in this retrospective study. However, those procedures were often performed to prevent rather than to treat impingement after PAO, which has been recognized as an important predictive factor of worse prognosis [1].
On preoperative radiographic review of patients with an LCEA of 18° to 25°, numerous other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum were found. The ACEA, the Tönnis acetabular roof angle, the anterior and posterior wall indices, and the FEAR index were commonly dysplastic among these patients. Notably, only a small proportion (three of 49 [6%]) of patients had the LCEA as the only radiographic feature suggesting acetabular insufficiency with all other parameters assessed being within normal range. Our results suggest that preoperative evaluation of patients with an LCEA of 18° to 25° should include a more detailed evaluation of the acetabular morphology including a false profile view and measurement of radiographic parameters that assess the morphology of the anterior and posterior walls. Furthermore, our findings support the concept that hip dysplasia should be considered a spectrum of complex 3-D deformity that includes different degrees and locations of osseous acetabular insufficiency [10, 22, 33, 46]. Nepple et al. [33] described three patterns of acetabular dysplasia including anterosuperior deficiency, global deficiency, and posterosuperior deficiency in 50 patients (45 females) who underwent PAO for the treatment of classic (LCEA < 20°) hip dysplasia. Others have reported that 16% to 18% of patients with acetabular dysplasia have associated acetabular retroversion rather than the classic anterolateral insufficiency with acetabular anteversion [10, 22]. With this knowledge, use of the terms “borderline” or “mildly” dysplastic should perhaps be reconsidered and a more comprehensive evaluation of the acetabulum should be undertaken before making this distinction. Wilkin et al. [46] proposed a new classification system to differentiate the direction of acetabular insufficiency and instability in dysplastic hips. Anterior instability is recognized by a decreased anterior wall index with near normal LCEA, which may represent the range used in our study; posterior instability is associated with acetabular retroversion and a decreased posterior wall index, even with near normal LCEA; and lateral/global instability is recognized by LCEA lower than 25° and features of either anterior or posterior acetabular insufficiency, or both. To the best of our knowledge, the classifications proposed by Nepple et al. and Wilkin et al. are initial efforts to differentiate hips with acetabular dysplasia based on the severity and location of the acetabular insufficiency that may lead to joint instability. Future studies are necessary to validate these classifications and to investigate if they can be applied in the clinical setting, that is, if they could help surgeons identify patients who could benefit from PAO versus other surgical strategies such as arthroscopic intraarticular treatment of associated chondrolabral pathology.
Over the 2-year followup period, no patients underwent revision surgery or conversion to THA and only one major complication (pulmonary embolism; Grade IV) was observed. Our results mirror the findings by Ricciardi et al. [38], who reported a low proportion of complications and no conversion to THA at 1-year followup for hips with LCEA of 18° to 25°. Although our study suggests a high survivorship free of revision surgery, THA, and mHHS < 70 of PAO in the short term, prospective comparative studies will be necessary to help determine the best long-term surgical strategy for the treatment of symptomatic patients with an LCEA between 18° and 25°. However, the preliminary results suggesting a low proportion of complications and revision surgery with 94% survivorship reported here and those by Ricciardi et al. [38] are encouraging. In general, PAO is considered a major invasive procedure, which may discourage surgeons from recommending PAO in the setting of LCEA of 18° to 25° and instead favor an arthroscopic approach for the treatment of associated chondrolabral pathology. However, hip arthroscopy can also aggravate the instability of the hip, especially if preservation of the labrum with adequate repair and closure or even plication of the capsule is not performed [26, 28]. Notably, arthroscopic capsular plication and labral preservation in hips with LCEA of 18° to 25° has been reported to have 9% risk of revision arthroscopic surgery at minimum 2-year [9] and 19% at minimum 5-year followup [8]. Fukui et al. [11] reported improvement in hip-specific outcomes in 100 patients with LCEA of 20° to 25° at minimum 2 years with 5% conversion to THA and 7% revision hip arthroscopy. Although PAO for dysplasia has a proven track record of preserving hip function at both mid- and long-term followup, the long-term effect of both hip arthroscopy and PAO in these patients must be evaluated by future comparative prospective studies [12, 23, 42, 44].
Patients undergoing PAO for an LCEA of 18° to 25° in the current study showed improvements in selected PROMs at minimum 2-year followup. The degree of improvement in outcome scores between the preoperative and 2-year followup time points is comparable to several other studies describing positive improvement in PROMs after PAO in patients with varying degrees of acetabular dysplasia [2, 5, 21, 23, 35, 40, 44]. Notably, Ricciardi et al. [38] compared 27 patients with LCEA of 18° to 25° with 50 patients with hip dysplasia and LCEA < 17° and reported similar improvements for the mHHS, HOOS, and Hip Outcome Tool-33 at 1-year followup. Clohisy et al. [5], in a prospective study of patients undergoing PAO for hip dysplasia, found that patients with more severe dysplasia experienced greater improvement in mHHS and HOOS scores when compared with those with mild (LCEA > 15°) dysplasia. Our findings of improvement in PROMs at minimum 2 years after PAO in patients with LCEA of 18° to 25° should be compared with previous studies of arthroscopic treatment of intraarticular pathology in the setting of hip dysplasia with LCEA of 18° to 25° [4, 8, 9, 31]. Although those studies have found arthroscopic treatment provided good functional results at short-term followup, others have noted inferior results when comparing dysplastic hips with hips with normal acetabular coverage [16, 18, 25].
The current study found that patients with an LCEA of 18° to 25° undergoing PAO and concomitant procedures had an improvement in pain and function at 2 years postoperatively with a low proportion of complications or reoperations at short-term followup. Our radiographic evaluation stresses the importance of including a complete radiographic assessment to better understand the acetabular morphology in patients with an LCEA of 18° to 25°. A complete plain film radiographic evaluation should include measurements of the Tönnis acetabular roof angle, the anterior and posterior acetabular wall indices, the FEAR index on the AP pelvic radiograph, and the ACEA on the false profile view as well as assessment of femoral-head neck sphericity. Although we did not use 3-D imaging in this study, adding a low-dose CT of the pelvis including an axial view of the distal femur may allow for a more comprehensive analysis of the acetabular and femoral morphology in these hips, including assessment of femoral version. Because we found a high proportion of other radiographic features of dysplasia suggestive of abnormal femoral head coverage by the acetabulum in patients with an LCEA of 18° to 25°, we believe that grouping these patients under the same category is overly simplistic. Isolated reliance on the measurement of lateral femoral head coverage will continue to mislabel patients with deficient anterior and posterior head coverage and may hinder our ability to best treat the source of their hip pain. The treatment of hip pain in patients with acetabular dysplasia with LCEA of 18° to 25° remains controversial. Future studies should strive to more thoroughly define the spectrum of severity and location of acetabular undercoverage, which will enable meaningful comparative effectiveness studies between hip arthroscopy and PAO in the treatment of acetabular dysplasia in these patients.
Acknowledgments
We thank Yi-Meng Yen MD, PhD, Department of Orthopedic Surgery, Boston Children’s Hospital, for his contribution as one of the surgeons in the study.
Footnotes
One of the authors certifies that he (MBM) has received personal fees in an amount of less than USD 10,000 from Saunders/Mosby-Elsevier: Editorial (Saunders/Mosby-Elsevier Publishing, Atlanta, GA, USA). One author certifies that he (JDW) has received research support in an amount of USD 10,000 to USD 100,000 from Arthrex Inc (Naples, FL, USA) outside the submitted work and is a member of the Arthroscopy editorial board.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beaule PE, Dowding C, Parker G, Ryu JJ. What factors predict improvements in outcomes scores and reoperations after the Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2015;473:615-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055-1060. [DOI] [PubMed] [Google Scholar]
- 4.Chandrasekaran S, Darwish N, Martin TJ, Suarez-Ahedo C, Lodhia P, Domb BG. Arthroscopic capsular plication and labral seal restoration in borderline hip dysplasia: 2-year clinical outcomes in 55 cases. Arthroscopy. 2017;33:1332-1340. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Ackerman J, Baca G, Baty J, Beaule PE, Kim YJ, Millis MB, Podeszwa DA, Schoenecker PL, Sierra RJ, Sink EL, Sucato DJ, Trousdale RT, Zaltz I. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J Bone Joint Surg Am. 2017;99:33-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooperman D. What is the evidence to support acetabular dysplasia as a cause of osteoarthritis? J Pediatr Orthop. 2013;33(Suppl 1):S2-7. [DOI] [PubMed] [Google Scholar]
- 7.Davila-Parrilla AD, Wylie J, O'Donnell C, Maranho DA, Carry P, Novais EN. Reliability of and correlation between measurements of acetabular morphology. Orthopedics. 2018:1-7. [DOI] [PubMed] [Google Scholar]
- 8.Domb BG, Chaharbakhshi EO, Perets I, Yuen LC, Walsh JP, Ashberg L. Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med. 2018;46:305-313. [DOI] [PubMed] [Google Scholar]
- 9.Domb BG, Stake CE, Lindner D, El-Bitar Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591-2598. [DOI] [PubMed] [Google Scholar]
- 10.Fujii M, Nakashima Y, Yamamoto T, Mawatari T, Motomura G, Matsushita A, Matsuda S, Jingushi S, Iwamoto Y. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895-903. [DOI] [PubMed] [Google Scholar]
- 11.Fukui K, Briggs KK, Trindade CA, Philippon MJ. Outcomes after labral repair in patients with femoroacetabular impingement and borderline dysplasia. Arthroscopy. 2015;31:2371-2379. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26-36. [PubMed] [Google Scholar]
- 13.Hatakeyama A, Utsunomiya H, Nishikino S, Kanezaki S, Matsuda DK, Sakai A, Uchida S. Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med. 2018;46:135-143. [DOI] [PubMed] [Google Scholar]
- 14.Henak CR, Abraham CL, Anderson AE, Maas SA, Ellis BJ, Peters CL, Weiss JA. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage. 2014;22:210-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120-1129. [DOI] [PubMed] [Google Scholar]
- 16.Kalore NV, Jiranek WA. Save the torn labrum in hips with borderline acetabular coverage. Clin Orthop Relat Res. 2012;470:3406-3413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423-429. [DOI] [PubMed] [Google Scholar]
- 18.Larson CM, Ross JR, Stone RM, Samuelson KM, Schelling EF, Giveans MR, Bedi A. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44:447-453. [DOI] [PubMed] [Google Scholar]
- 19.Lequesne M, de Seze [False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies] [in French]. Rev Rhum Mal Osteoartic. 1961;28:643-652. [PubMed] [Google Scholar]
- 20.Lerch TD, Steppacher SD, Liechti EF, Tannast M, Siebenrock KA. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res. 2017;475:1154-1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001;50:229-238. [PubMed] [Google Scholar]
- 22.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245-253. [DOI] [PubMed] [Google Scholar]
- 23.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113-2123. [DOI] [PubMed] [Google Scholar]
- 24.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am. 2010;92(Suppl 1):115-129. [DOI] [PubMed] [Google Scholar]
- 25.Matsuda DK, Gupta N, Khatod M, Matsuda NA, Anthony F, Sampson J, Burchette R. Poorer arthroscopic outcomes of mild dysplasia with cam femoroacetabular impingement versus mixed femoroacetabular impingement in absence of capsular repair. Am J Orthop (Belle Mead NJ). 2017;46:E47-E53. [PubMed] [Google Scholar]
- 26.Matsuda DK, Khatod M. Rapidly progressive osteoarthritis after arthroscopic labral repair in patients with hip dysplasia. Arthroscopy. 2012;28:1738-1743. [DOI] [PubMed] [Google Scholar]
- 27.McWilliams DF, Doherty SA, Jenkins WD, Maciewicz RA, Muir KR, Zhang W, Doherty M. Mild acetabular dysplasia and risk of osteoarthritis of the hip: a case-control study. Ann Rheum Dis. 2010;69:1774-1778. [DOI] [PubMed] [Google Scholar]
- 28.Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440-445. [DOI] [PubMed] [Google Scholar]
- 29.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985-989. [DOI] [PubMed] [Google Scholar]
- 30.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92-98. [DOI] [PubMed] [Google Scholar]
- 31.Nawabi DH, Degen RM, Fields KG, McLawhorn A, Ranawat AS, Sink EL, Kelly BT. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44:1017-1023. [DOI] [PubMed] [Google Scholar]
- 32.Nepple JJ, Martell JM, Kim YJ, Zaltz I, Millis MB, Podeszwa DA, Sucato DJ, Sink EL, Clohisy JC; ANCHOR Study Group. Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med. 2014;42:2393-2401. [DOI] [PubMed] [Google Scholar]
- 33.Nepple JJ, Wells J, Ross JR, Bedi A, Schoenecker PL, Clohisy JC. Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res. 2017;475:1037-1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Novais EN, Kim YJ, Carry PM, Millis MB. The Bernese periacetabular osteotomy: is transection of the rectus femoris tendon essential? Clin Orthop Relat Res. 2014;472:3142-3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parry JA, Swann RP, Erickson JA, Peters CL, Trousdale RT, Sierra RJ. Midterm outcomes of reverse (anteverting) periacetabular osteotomy in patients with hip impingement secondary to acetabular retroversion. Am J Sports Med. 2016;44:672-676. [DOI] [PubMed] [Google Scholar]
- 36.Reijman M, Hazes JM, Pols HA, Koes BW, Bierma-Zeinstra SM. Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam study. Arthritis Rheum. 2005;52:787-793. [DOI] [PubMed] [Google Scholar]
- 37.Ricciardi BF, Fields KG, Wentzel C, Kelly BT, Sink EL. Early functional outcomes of periacetabular osteotomy after failed hip arthroscopic surgery for symptomatic acetabular dysplasia. Am J Sports Med. 2017;45:2460-2467. [DOI] [PubMed] [Google Scholar]
- 38.Ricciardi BF, Fields KG, Wentzel C, Nawabi DH, Kelly BT, Sink EL. Complications and short-term patient outcomes of periacetabular osteotomy for symptomatic mild hip dysplasia. Hip Int. 2017;27:42-48. [DOI] [PubMed] [Google Scholar]
- 39.Siebenrock KA, Kistler L, Schwab JM, Buchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012;470:3355-3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239-245. [PubMed] [Google Scholar]
- 41.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J; Academic Network for Conservational Hip Outcomes Research Group. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220-2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tönnis D. Normal values of the hip joint for the evaluation of x-rays in children and adults. Clin Orthop Relat Res. 1976;119:39-47. [PubMed] [Google Scholar]
- 44.Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169-2179. [DOI] [PubMed] [Google Scholar]
- 45.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939:7-38. [Google Scholar]
- 46.Wilkin GP, Ibrahim MM, Smit KM, Beaule PE. A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplasty. 2017;32:S20-S27. [DOI] [PubMed] [Google Scholar]
- 47.Wyatt M, Weidner J, Pfluger D, Beck M. The Femoroepiphyseal Acetabular Roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res. 2017;475:861-869. [DOI] [PMC free article] [PubMed] [Google Scholar]