Abstract
Background
Leverage of the femoral head against the acetabular rim may lead to posterior hip dislocation during sports activities in hips with femoroacetabular impingement (FAI) deformity. Abnormal concavity of the femoral head and neck junction has been well described in association with posterior hip dislocation. However, acetabular morphology variations are not fully understood.
Questions/purposes
The purpose of this study was to compare the acetabular morphology in terms of acetabular version and coverage of the femoral head in adolescents who sustained a posterior hip dislocation during sports and recreational activities with a control group of patients without a history of hip disease matched by age and sex.
Methods
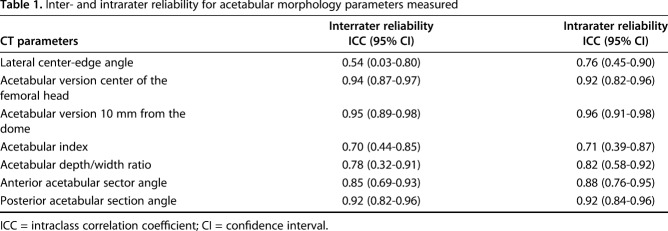
In this case-control study, we identified 27 adolescents with posterior hip dislocation sustained during sports or recreational activities who underwent a CT scan of the hips (study group) and matched them to patients without a history of hip disease being evaluated with CT for possible appendicitis (control group). Between 2001 and 2017, we treated 71 adolescents (aged 10-19 years old) for posterior hip dislocations. During the period in question, we obtained CT scans or MR images after closed reduction of a posterior hip dislocation. One patient was excluded because of a diagnosis of Down syndrome. Twenty-one patients who were in motor vehicle-related accidents were also excluded. Twelve patients were excluded because MRI was obtained instead of CT. Finally, three patients with no imaging after reduction and seven patients with inadequate CT reformatting were excluded. Twenty-seven patients (38%) had CT scans of suitable quality for analysis, and these 27 patients constituted the study group. We compared those hips with 27 age- and sex-matched adolescents who had CT scans for appendicitis and who had no history of hip pain or symptoms (control group). One orthopaedic surgeon and one pediatric musculoskeletal radiologist, not invoved in the care of the patients included in the study, measured the lateral center-edge angle, acetabular index, acetabular depth/width ratio, acetabular anteversion angle (10 mm from the dome and at the level of the center of the femoral heads), and the anterior and posterior sector angles in the dislocated hip; the contralateral uninvolved hip of the patients with hip dislocations; and both hips in the matched control patients. Both the study and control groups had 25 (93%) males with a mean age of 13 (± 1.7) years. Inter- and intrarater reliability of measurements was assessed with intraclass correlation coefficient (ICC). There was excellent reliability (ICC > 0.90) for the acetabular anteversion angle measured at the center of the femoral head, the acetabular version 10 mm from the dome, and the posterior acetabular sector angle.
Results
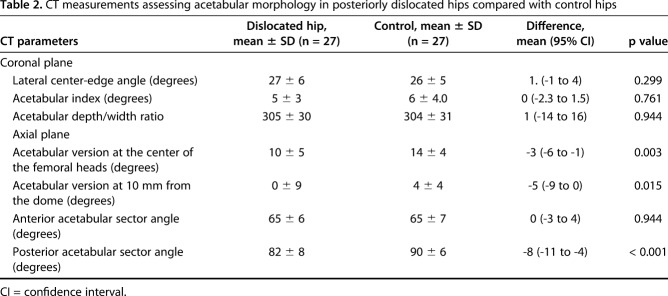
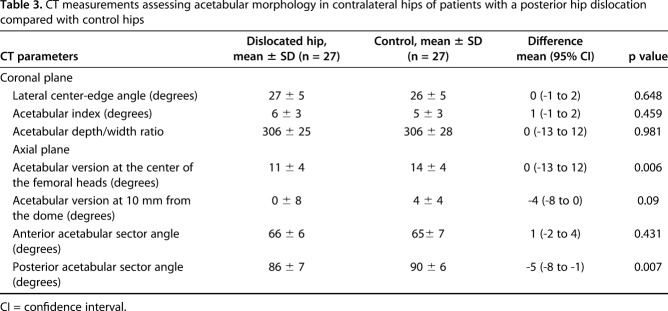
The mean acetabular anteversion angle (± SD) was lower in the study group at 10 mm from the acetabular dome (-0.4° ± 9° versus 4° ± 4°; mean difference -5°; 95% confidence interval [CI], -9 to -0.3; p = 0.015) and at the center of the femoral heads (10° ± 5° versus 14° ± 4°; mean difference -3°; 95% CI, -6 to -0.9; p = 0.003). A higher proportion of acetabula was severely retroverted in the study group (14 of 27 [52%]; 95% CI, 33%-71% versus four of 27 [15%]; 95% CI, 1%-28%; p = 0.006). The mean posterior acetabular sector angle was lower in the study group (82° ± 8° versus 90° ± 6°; mean difference -8°; 95% CI, -11 to -4; p < 0.001), whereas no difference was found for the anterior acetabular sector angle (65° ± 6° versus 65° ± 7°; mean difference 0.3°; 95% CI, -3 to 4; p = 0.944). There was no difference for the lateral center-edge angle (27° ± 6° versus 26° ± 5°; p = 0.299), acetabular index (5° ± 3° versus 6 ± 4°; p = 0.761), or acetabular depth/width ration (305 ± 30 versus 304 ± 31; p = 0.944) between groups. Acetabular anteversion angle at the center of the femoral heads (11° ± 4° versus 14° ± 4°; p = 0.006) and the posterior acetabular sector angle (86° ± 7 ° versus 91° ± 6°; p = 0.007) were lower in the contralateral uninvolved hips compared with control hips.
Conclusions
Decreased acetabular anteversion angle and posterior acetabular coverage of the femoral head were associated with posterior dislocation of the hip in adolescents with sports-related injury even in the absence of a high-energy mechanism. Further studies are necessary to clarify whether a causative effect exists between acetabular and femoral morphology and the dislocation of the hip in patients with sports-related injuries.
Level of Evidence
Level III, prognostic study.
Introduction
Traumatic posterior hip dislocation often results from high-energy trauma, including motor vehicle and pedestrian accidents. However, traumatic posterior hip dislocations also occur in athletes without the typical high-energy mechanism [4, 11, 19, 30]. Although patient-specific factors, including reduced femoral anteversion [27], have been reported in the past, in general the hip position at the time of the trauma has been thought to be the most important factor determining the hip dislocation. Higher hip flexion and adduction at the time of trauma are associated with simple dislocation, whereas less adduction or less internal rotation is associated with a fracture-dislocation of the posterior acetabular wall [12]. Recently, however, several studies described an association between femoral acetabular impingement (FAI) morphology and traumatic posterior dislocation of the hip [4, 5, 11, 13, 14, 16, 17, 19, 22, 30]. In hips with cam-type and pincer-type FAI morphology, the femoral head-neck junction impacts against the anterior acetabulum with hip flexion, adduction, and internal rotation. Impingement may predispose the femoral head to lever out the back over the fulcrum of the anterior acetabular rim with less force [4, 22]. Therefore, it is possible that the hip could dislocate without high-energy trauma because of the morphology of the proximal femur, the acetabulum, or a combination of both.
Accurate assessment of anatomic factors associated with posterior hip instability is essential to elucidate the etiology and for appropriate treatment and prognosis. Previous studies have reported abnormal concavity of the femoral head and neck junction as assessed by higher α angle and reduced head-neck offset in patients with traumatic hip dislocation [4, 5, 11, 14, 19, 22, 30]. One study reported that 42% and 58% of adolescents with posterior hip instability associated with sports injuries had a cam-type deformity at the 1 o’clock and 2 o’clock areas of the femoral head-neck junction, respectively [14]. Although the study reported reduced angle of acetabular version at the center of the femoral head in patients with hip dislocation, it remains unclear whether the femoral head is less covered by the acetabulum and what patterns of acetabular morphology may be associated with posterior hip dislocation in adolescents. Other studies reported the presence of acetabular retroversion based on the assessment of radiographs and the crossover sign, ischial spine sign, or posterior wall sign in patients who sustained a posterior hip dislocation [4, 11, 19, 22]. However, the application of those radiographic signs is limited in adolescents because the posterior acetabular wall is not fully ossified until approximately 14 years of age [8]. One study using CT in adolescents practicing sports who sustained a traumatic posterior dislocation of the hip demonstrated that acetabular anteversion angle was lower in the dislocation group compared with patients without hip disorders [14]. However, the study only included 12 patients with dislocation, and the assessment of acetabular morphology was limited by anteversion measurement only at the level corresponding to the center of the femoral head.
We therefore investigated the acetabular morphology in adolescents who sustained a traumatic posterior hip dislocation associated with a sports-related injury and compared those hips with the hips of age- and sex-matched patients with no known history of hip pain.
Patients and Methods
This retrospective, case-control study was approved by our institutional review board. We searched our institutional database for patients diagnosed with posterior dislocation of the hip between 2001 and 2017. Inclusion criteria were (1) age at the time of injury between 10 and 19 years old to be in compliance with the definition of adolescents as defined by the World Health Organization [29]; (2) posterior hip dislocation resulting from an injury occurring during recreational or competitive sports activities including team and individual sports such as American football and winter sports such as skiing; and (3) available CT image of the pelvis after closed reduction. The initial search identified 71 patients diagnosed with a traumatic posterior dislocation treated at our institution during the study period. During the period in question, we typically obtained CT scans after closed reduction of a posterior hip dislocation to assess for the quality of reduction, joint space symmetry, and to rule out any intraarticular osteochondral fracture. Recently, however, we have favored using MRI, which has been shown to improve the assessment of structural intraarticular pathologies including diagnosis of chondral and labral injuries [15, 24]. One patient was excluded because of a diagnosis of Down syndrome. Twenty-one patients involved in motor vehicle-related accidents were also excluded. Twelve patients were excluded because MR images were obtained instead of CT. Finally, three patients with no imaging after reduction and seven patients with inadequate CT reformatting were excluded. Twenty-seven patients (38%) had CT scans of suitable quality for analysis, and these 27 patients constituted the study group (Fig. 1).
Fig. 1.
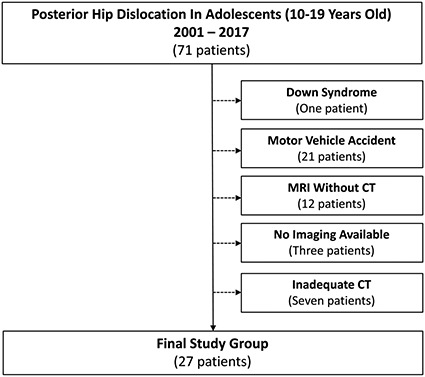
Algorithm representing the allocation criteria for the study group is shown. *Patients with high-energy injuries related to motor vehicle or pedestrian accidents were excluded because of injuries not related to sports or recreational activities. **Patients who did not have a CT scan of the pelvis including both hips or whose CT was of inadequate quality for reformatting were excluded.
The control group consisted of 27 patients without a history of hip disease or hip symptoms who had a pelvic CT scan as part of the evaluation for abdominal pain and suspected appendicitis. One of the authors (MGF) reviewed the medical records to confirm that each selected matched control patient had no history of hip disorders or symptoms. Each patient with a posterior dislocation was then matched to a control patient without hip disease or hip symptoms using a nearest neighbor approach [23]. Patients in the dislocation group were categorized based on sex and age, and the control patients were designated to each sex and age category. If there was more than one control patient in the sex and age category, the one with the closest body mass index (BMI) was selected.
The groups were well matched by age and sex. There were 25 (93%) males and two (7%) females in each cohort of 27 patients. Although the initial search was defined for patients aged 10 to 19 years at the time of injury, participants included in the study group ranged between 10 and 17 years old. The mean age was 13 years (± 2) in each group. Despite our efforts to match patients by BMI, BMI was slightly higher (p = 0.005) in the control group (23 ± 2 kg/m2) compared with the study group (19 ± 2 kg/m2). Although the difference in BMI could influence the femoral morphology and be a factor indirectly associated with the risk of a dislocation, BMI has no impact on the development of the acetabular morphology [18]. With the numbers available, no difference (p = 0.157) in skeletal maturity assessed by the status of the triradiate cartilage was observed between the groups. Eighteen of 27 patients (67%) in the posterior dislocation group had open triradiate cartilage compared with 16 (59%) patients in the control group. Fourteen of 27 patients (52%) sustained a traumatic posterior hip dislocation while playing football and eight (30%) patients while skiing. One patient was involved in each of the following activities: basketball, water trampoline, field hockey, sledding, and an unwitnessed fall while running.
CT Assessment of Acetabular Morphology
CT scan of the pelvis was acquired with the patients in a supine position on the table. All patients were scanned on a multidetector CT scanner at or less than 1.0 mm collimation. Given potential variations in pelvic tilt and pelvic rotation related to pain at the time of CT scan, axial CT images were subsequently reformatted into true axial and coronal planes based on a standardized technique using Synapse 3D software (Fujifilm Corp, Tokyo, Japan). In the true coronal plane, the acetabular index was measured by the technique described by Tönnis [25] and the lateral center-edge angle as described by Wiberg [28]. The status of the triradiate cartilage (closed, closing, or open) [20] was recorded. Acetabular depth/width ratio was also assessed in the coronal plane as described by Fujii et al. [9] (Fig. 2). In the true axial plane, we measured the acetabular anteversion angle cranially (at a level 10 mm distal to the highest point of the acetabular dome) and at the level of the center of the femoral heads as previously described by Fujii et al. [9]. Based on the Tönnis and Heinecke [26] criteria, patients were considered to have severe retroversion if the acetabular anteversion angle measured at the level of the center of the femoral heads was lower than 10°. Posterior and anterior acetabular support to the femoral head was also assessed in the true axial plane by measurement of the posterior and anterior acetabular sector angles at the level of the centers of the femoral heads as described by Anda et al. [2] (Fig. 3).
Fig. 2 A-C.
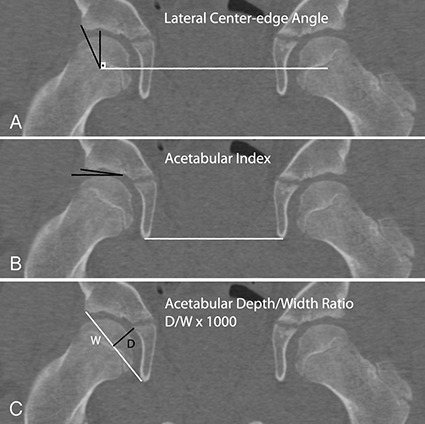
Measurements of acetabular morphology performed in the coronal plane are shown. (A) The lateral center-edge angle was measured between a perpendicular line to the line connecting the center of the femoral heads and a line connecting the center of the femoral head to the lateral aspect of the acetabular sourcil. (B) The acetabular index was measured by the angle formed between a line drawn from the lateral to the medial aspect of the acetabular sourcil and the transverse axis of the pelvis assessed by a line parallel to the line connecting the inferior aspect of the teardrops. (C) The acetabular width (w) was measured by a line connecting the lateral aspect of the sourcil and the medial inferior aspect of the teardrop. The acetabular depth (d) was measured from midpoint of the connecting width line to the deepest point of the acetabulum in a perpendicular fashion. The acetabular depth/width ratio was calculated as depth divided by the width multiplied by 1000.
Fig. 3 A-C.
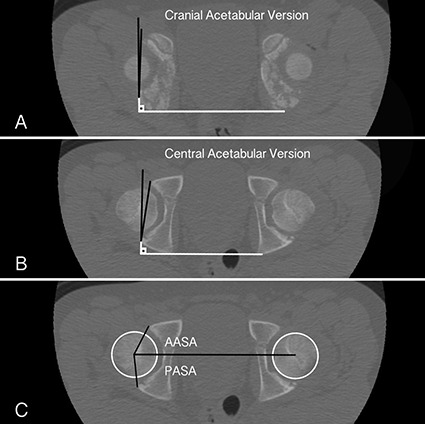
Measurements of acetabular morphology performed in the axial plane are shown. (A) To measure the acetabular version angle 10 mm below the acetabular dome, a line connecting the anterior and posterior rim of the acetabulum was drawn. An orthogonal line to the horizontal line connecting the posterior apex of the ischium was drawn and the angle formed corresponded to the acetabulum anteversion angle. (B) The acetabular anteversion angle was similarly measured at the level corresponding to the center of the femoral heads. (C) The anterior acetabular sector angle (AASA) is the angle formed between a horizontal line connecting the center of both femoral heads and a line connecting the anterior rim of the acetabulum to the center of the femoral head. The posterior acetabular sector angle (PASA) is the angle formed between the horizontal line and a line connecting the posterior acetabulum rim and the center of the femoral head.
These measurements were performed on both hips in each patient in the study and control cohorts. For all measurements, each hip in the dislocation group was compared with the same-sided hip in the control group. Measurements were performed independently by an orthopaedic surgeon not involved in the clinical care of the patients (MGF) and by a pediatric musculoskeletal radiologist (SDB). To assess intrareader variability, one reader (MGF) performed two sets of measurements on each patient cohort separated in time by a minimum of 4 weeks.
Statistical Analysis
Continuous variables were summarized using means, SDs, and confidence intervals (CIs) or medians and 25th and 75th percentiles as appropriate. Categorical variables were summarized using counts and percentages. For the primary outcome, the comparison between the acetabular version for the dislocated hips compared with matched controls was tested with a Wilcoxon signed rank test. For other secondary comparisons between the dislocated hips and the matched controls, measures were tested using a Wilcoxon signed rank test or a McNemar’s test as appropriate. For the comparison of the acetabular version categories as described by Tönnis [26], each of three levels was tested with a McNemar’s test and adjusted for multiple comparisons with Bonferroni adjustment.
Inter- and intrarater reliability of measurements was assessed with intraclass correlation coefficient (ICC). There was excellent reliability (ICC > 0.90) [6] for the acetabular anteversion angle measured at the center of the femoral head, the acetabular version 10 mm from the dome, and the posterior acetabular sector angle (Table 1). This reliability assessment resulted in three sets of measurements for each hip. All three measurements were used to reduce variability. To give equal weight to the two raters, the mean of the two measurements of Rater 1 was combined with the one measurement of Rater 2 to obtain the overall mean estimates.
Table 1.
Inter- and intrarater reliability for acetabular morphology parameters measured
All statistical calculations for this study were generated using SAS software 9.4 (SAS Institute Inc, Cary, NC, USA) and p values < 0.05 were considered statistically significant.
Results
The mean acetabular anteversion angle (± SD) was lower in the study group at 10 mm from the acetabular dome (-0.4° ± 9 versus 4 ± 4°; mean difference -5°; 95% CI, -9 to -0.3; p = 0.015) and at the center of the femoral heads (10° ± 5° versus 14° ± 4°; mean difference -3°; 95% CI, -6 to -0.9; p = 0.003) (Table 2). A higher proportion of acetabula was severely retroverted (anteversion angle < 10°) in the study group (14 of 27 [52%]; 95% CI, 33%-71% versus four of 27 [15%]; 95% CI, 1%-28%; p = 0.006). Patients with a posterior dislocated hip had decreased coverage of the femoral head posteriorly compared with control patients. The mean posterior acetabular sector angle was lower in the study group (82° ± 8° versus 90° ± 6°; mean difference -8°; 95% CI, -11 to -4; p < 0.001), whereas no difference was found for the anterior acetabular sector angle (65° ± 6° versus 65° ± 7°; mean difference 0.3°; 95% CI, -3 to 4; p = 0.944). With the numbers available, there was no difference for the lateral center-edge angle (27° ± 6° versus 26° ± 5°; p = 0.299), acetabular index (5° ± 3° versus 6 ± 4°; p = 0.761), or acetabular depth/width ration (305 ± 30 versus 304 ± 31; p = 0.944) between groups. Acetabular anteversion angle at the center of the femoral heads (11° ± 4° versus 14° ± 4°; p = 0.006) and the posterior acetabular sector angle (86° ± 7 ° versus 91° ± 6°; p = 0.007) were lower in the contralateral uninvolved hips compared with control hips.
Table 2.
CT measurements assessing acetabular morphology in posteriorly dislocated hips compared with control hips
The analysis of contralateral uninvolved hips in patients with posterior hip dislocation compared with hips in the control group showed lower acetabular anteversion angle at the level of the center of the femoral heads (11° ± 4° versus 14° ± 4°; mean difference 0; 95% CI, -13 to -12; p = 0.006) and decreased posterior coverage of the femoral head assessed by the posterior sector angle (86° ± 7° versus 90° ± 6°; mean difference -5°; 95% CI, -8 to -1; p = 0.007). No difference between the contralateral hip versus controls was observed for acetabular anteversion angle measured cranially at 10 mm from the acetabular dome (0° ± 8° versus 4° ± 4°; mean difference -4; 95% CI, -9 to 0; p = 0.09). Similarly, no difference was found for the anterior acetabular sector angle (66° ± 6° versus 65° ± 7°; mean difference 1°; 95% CI, -2 to 4; p = 0.431) (Table 3).
Table 3.
CT measurements assessing acetabular morphology in contralateral hips of patients with a posterior hip dislocation compared with control hips
Discussion
Posterior hip dislocation may occur during recreational and sports activities without the typical high-energy mechanism associated with dashboard injuries. FAI deformity may lead to an impact of the femoral head-neck junction against the anterior acetabular rim with the hip in flexion, adduction, and internal rotation [4, 22]. Although the association of FAI morphology and posterior hip dislocation has been described in adult athletes, less is known about this association in adolescents [14]. We found that patients with posterior hip dislocation had lower acetabular version and decreased posterior acetabular coverage in the dislocated hips and in the contralateral uninvolved hips when compared with control patients.
We acknowledge limitations of our study. First, the study was limited to the investigation of the acetabular morphology. Currently, it is accepted that other anatomic factors may predispose a hip that is abruptly moved into flexion with adduction and internal rotation moments to dislocate even in the absence of high-energy trauma. We believe that the influence of reduced femoral version [27] and abnormal femoral head and neck concavity [4, 5, 11, 14, 19, 22, 30] have been well established, and we purposely focus on the study of the acetabular morphology. Assessment of femoral version would have required axial imaging of the femoral condyles, which was not available as part of our institution CT protocol for abdominal pain and appendicitis and for CT imaging after closed reduction of hip dislocation. Further studies investigating the hip morphology in patients with posterior dislocation should look at femoral version to have a comprehensive analysis of the femur and acetabulum. Second, our matching methodology was not flawless. We could not match patients based on their activity level. Participants in the study group may have a higher level of activity than the control participants given the sports-related injury. Vigorous sports activities during adolescence are associated with the development of femoral cam FAI morphology [1, 21]. Therefore, a possible relationship among level activity, cam FAI morphology, and posterior dislocation could exist and should be further investigated. However, we are not aware of an association of sports participation with changes in the acetabular morphology, the main focus of our study.
Although we attempted to match patients based on BMI, BMI was slightly higher in the control group compared with the study group. However, higher BMI has been associated with cam morphology resembling a mild slipped capital femoral epiphysis deformity [18] and decreased femoral retroversion [10]. Notably, BMI has been shown to have no impact in the morphology of the acetabulum [18]. We believe that is unlikely that BMI difference observed between the groups would be related to the morphology of the acetabulum and to a higher risk of dislocation in the study group [18]. Third, our study included a wide range of ages (10-19 years old) to be compliant with the definition of adolescent age by the World Health Organization [29] with a risk of assessing patients with different stages of skeletal maturity. However, most patients in the dislocation cohort (18 of 27 [67%]) had open triradiate cartilage at the time of injury. The posterior acetabular wall does not completely ossify until age 13 or 14 years, after the triradiate cartilage has closed; posterior wall assessment has been proposed to be more reliable by using MRI [8]. It is possible that by using CT, we could have underestimated the cartilaginous portion of the posterior acetabular wall. To reduce the risk of underestimating the posterior wall assessment, we included a control group. We attempted to match participants by chronological age, and the overall distribution of triradiate cartilage status was not different between the groups. Notably, reliability measurements involving the posterior wall of the acetabulum were excellent, which reaffirmed that measuring off the posterior acetabular wall was reliable, even in the presence of a cartilaginous posterior wall. Fourth, the patients who met inclusion criteria for this study comprise a subset of patients diagnosed with a traumatic posterior hip dislocation during the study period, raising the potential risk of selection bias. During the period of the study, we typically obtained CT scans of the pelvis after closed reduction. However, in seven patients the CT was of poor quality or only included one hip and these patients could not be included. During the last years of the study period, MRI has been favored to evaluate the hip after reduction because it has been shown to improve the assessment of soft tissue pathology including an inverting or torn labrum. Notably, 12 patients were excluded from this study because MRI rather than CT was the image obtained. We believe that our sample is representative of the population of adolescents with sports and recreational-related traumatic hip dislocation seen in a tertiary children’s hospital. Finally, every study involving human measurements has a risk of assessment bias. In this study we had two observers: one orthopaedic surgeon not involved in the clinical treatment of patients (MGF) and a pediatric radiologist (SDB). The inter- and intrareliability of measurements was excellent for the acetabular version and posterior sector angles.
The findings of the current study expand the current knowledge about the hip morphology in hips with a posterior dislocation [5, 11, 14, 22, 30]. Mayer et al. [13] compared 12 male patients who had a posterior hip dislocation during sports to control hips and found a higher proportion of cam deformity in the dislocated group as well as lower values of acetabular anteversion at the center of the femoral head. Measurement of acetabular anteversion at the center of the femoral head is important but does not tell the whole history about the acetabular morphology because often in pincer-type FAI, acetabular retroversion may be restricted to the superior aspect of the joint. In this study we performed a rather comprehensive assessment of the acetabular morphology and we found that hips in the posteriorly dislocated group had lower mean acetabular anteversion in both levels measured. Moreover, we found that slightly more than half of patients in the dislocation cohort had severe retroversion of the acetabulum and this proportion was higher than that observed in control hips. Steppacher et al. [22] proposed that with flexion and internal rotation, the nonconcave head-neck area would impact against the prominent anterior rim in a retroverted acetabulum, which then acts as a fulcrum facilitating the posterior dislocation without a wall fracture. They postulated that the fulcrum mechanism is more important for dislocation than a coverage deficiency. However, we found that the posterior coverage of the femoral head as assessed by the posterior acetabular sector angle was lower in dislocated hips compared with the control hips without a difference in the anterior acetabular sector angle. Notably, the analysis of the contralateral uninvolved hip in patients with a posteriorly dislocated hip revealed a similar morphology to the dislocated hip with lower acetabular version angle at the center of the femoral heads and decreased posterior support to the femoral head. We believe that the findings of decreased acetabular anteversion and insufficient posterior coverage of the femoral head support the theory that an abnormal acetabulum morphology may predispose patients to a posterior hip dislocation even in the absence of a high-energy axial loading mechanism such as a dashboard injury. However, further studies are necessary to clarify whether there is a causal relationship between acetabular retroversion and posterior hip dislocation associated with sports activities.
We found no difference for measurements of acetabular dysplasia, including the lateral center-edge angle, acetabular index, and acetabular depth/width ratio, in hips with posterior dislocation and controls. Our findings are in line with previous studies suggesting that acetabular dysplasia is not a morphologic feature associated with traumatic posterior hip dislocation [11, 14, 22, 30]. The lateral center-edge angle and the acetabular index are surrogates for assessing lateral coverage of the femoral head by the acetabulum. Intuitively, the lateral coverage of the femoral head by the acetabulum should not influence the risk of posterior hip dislocation.
The findings of our study may help the treating orthopaedic surgeon understand the morphology of the hip when treating an adolescent with sports-related posterior dislocation. Although this study should not influence the management of a primary posterior hip dislocation, it may help in patients with the rare complication of recurrent posttraumatic posterior hip dislocation. In this setting, the morphology of the acetabulum should be investigated to include assessment of the acetabular version measured at the center of the femoral head and cranially and also the coverage of the femoral head anteriorly and posteriorly by the acetabular sector angles. In select patients, a periacetabular osteotomy to correct acetabular retroversion and improve the posterior coverage has been reported to provide joint stability [3, 7]. Our study showed an association between acetabular retroversion and decreased posterior coverage with sports-related posterior hip dislocation in adolescents. However, we caution that our findings do not prove that acetabular retroversion and decreased posterior acetabular coverage cause posterior dislocation of the hip. Future research will be needed to determine whether a causal relationship exists between acetabular morphology and posterior dislocation occurring during sports activities.
Acknowledgments
We thank Roya Dastjerdi MPH, MD, Department of Orthopedic Surgery, Boston Children’s Hospital, for her assistance with query and data acquisition.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Agricola R, Heijboer MP, Ginai AZ, Roels P, Zadpoor AA, Verhaar JA, Weinans H, Waarsing JH. A cam deformity is gradually acquired during skeletal maturation in adolescent and young male soccer players: a prospective study with minimum 2-year follow-up. Am J Sports Med. 2014;42:798-806. [DOI] [PubMed] [Google Scholar]
- 2.Anda S, Terjesen T, Kvistad KA. Computed tomography measurements of the acetabulum in adult dysplastic hips: which level is appropriate? Skeletal Radiol. 1991;20:267-271. [DOI] [PubMed] [Google Scholar]
- 3.Arpey NC, Holte AJ, Tofte JN, Willey MC. Acute periacetabular osteotomy for recurrent posttraumatic dislocation of the hip: a case report. JBJS Case Connect. 2018;8:e39. [DOI] [PubMed] [Google Scholar]
- 4.Berkes MB, Cross MB, Shindle MK, Bedi A, Kelly BT. Traumatic posterior hip instability and femoroacetabular impingement in athletes. Am J Orthop. 2012;41:166-171. [PubMed] [Google Scholar]
- 5.Canham CD, Yen YM, Giordano BD. Does Femoroacetabular impingement cause hip instability? A systematic review. Arthroscopy. 2016;32:203-208. [DOI] [PubMed] [Google Scholar]
- 6.Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic. 1981;86:127-137. [PubMed] [Google Scholar]
- 7.Crowther JD, Chudik SC, Dahners LE. Periacetabular osteotomy for stabilization of recurrent post-traumatic dislocation of the hip. J Orthop Trauma. 2002;16:433-436. [DOI] [PubMed] [Google Scholar]
- 8.Fabricant PD, Hirsch BP, Holmes I, Kelly BT, Lorich DG, Helfet DL, Bogner EA, Green DW. A radiographic study of the ossification of the posterior wall of the acetabulum: implications for the diagnosis of pediatric and adolescent hip disorders. J Bone Joint Surg Am. 2013;95:230-236. [DOI] [PubMed] [Google Scholar]
- 9.Fujii M, Nakamura T, Hara T, Nakashima Y, Iwamoto Y. Does radiographic coxa profunda indicate increased acetabular coverage or depth in hip dysplasia? Clin Orthop Relat Res. 2015;473:2056-2066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galbraith RT, Gelberman RH, Hajek PC, Baker LA, Sartoris DJ, Rab GT, Cohen MS, Griffin PP. Obesity and decreased femoral anteversion in adolescence. J Orthop Res. 1987;5:523-528. [DOI] [PubMed] [Google Scholar]
- 11.Krych AJ, Thompson M, Larson CM, Byrd JW, Kelly BT. Is posterior hip instability associated with cam and pincer deformity? Clin Orthop Relat Res. 2012;470:3390-3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Letournel E, Judet R. Fracture of the acetabulum. In: Elson R, ed. Fracture of the Acetabulum . Berlin, Germany: Springer-Verlag; 2014:23. [Google Scholar]
- 13.Manner HM, Mast NH, Ganz R, Leunig M. Potential contribution of femoroacetabular impingement to recurrent traumatic hip dislocation. J Pediatr Orthop B. 2012;21:574-578. [DOI] [PubMed] [Google Scholar]
- 14.Mayer SW, Abdo JC, Hill MK, Kestel LA, Pan Z, Novais EN. Femoroacetabular impingement is associated with sports-related posterior hip instability in adolescents: a matched-cohort study. Am J Sports Med. 2016;44:2299-2303. [DOI] [PubMed] [Google Scholar]
- 15.Mayer SW, Stewart JR, Fadell MF, Kestel L, Novais EN. MRI as a reliable and accurate method for assessment of posterior hip dislocation in children and adolescents without the risk of radiation exposure. Pediatr Radiol. 2015;45:1355-1362. [DOI] [PubMed] [Google Scholar]
- 16.Morris AC, Yu JC, Gilbert SR. Arthroscopic treatment of traumatic hip dislocations in children and adolescents: a preliminary study. J Pediatr Orthop. 2017;37:435-439. [DOI] [PubMed] [Google Scholar]
- 17.Novais EN, Heare TC, Hill MK, Mayer SW. Surgical hip dislocation for the treatment of intra-articular injuries and hip instability following traumatic posterior dislocation in children and adolescents. J Pediatr Orthop. 2016;36:673-679. [DOI] [PubMed] [Google Scholar]
- 18.Novais EN, Shefelbine SJ, Kienle KP, Miller PE, Bowen G, Kim YJ, Bixby SD. Body mass index affects proximal femoral but not acetabular morphology in adolescents without hip pathology. J Bone Joint Surg Am. 2018;100:66-74. [DOI] [PubMed] [Google Scholar]
- 19.Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:169-174. [DOI] [PubMed] [Google Scholar]
- 20.Popejoy D, Emara K, Birch J. Prediction of contralateral slipped capital femoral epiphysis using the modified Oxford bone age score. J Pediatr Orthop. 2012;32:290-294. [DOI] [PubMed] [Google Scholar]
- 21.Siebenrock KA, Behning A, Mamisch TC, Schwab JM. Growth plate alteration precedes cam-type deformity in elite basketball players. Clin Orthop Relat Res. 2013;471:1084-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steppacher SD, Albers CE, Siebenrock KA, Tannast M, Ganz R. Femoroacetabular impingement predisposes to traumatic posterior hip dislocation. Clin Orthop Relat Res. 2013;471:1937-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25:1-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thanacharoenpanich S, Bixby S, Breen MA, Kim YJ. MRI is better than CT scan for detection of structural pathologies after traumatic posterior hip dislocations in children and adolescents. J Pediatr Orthop. 2018. Jan 19. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 25.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer; 1987. [Google Scholar]
- 26.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747-1770. [DOI] [PubMed] [Google Scholar]
- 27.Upadhyay SS, Moulton A, Burwell RG. Biological factors predisposing to traumatic posterior dislocation of the hip. A selection process in the mechanism of injury. J Bone Joint Surg Br. 1985;67:232-236. [DOI] [PubMed] [Google Scholar]
- 28.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand. 1939:5-135. [Google Scholar]
- 29.World Health Organization. Adolescent Health. Available at: http://www.who.int/topics/adolescent_health/en/. Accessed August 10, 2018.
- 30.Wylie JD, Abtahi AM, Beckmann JT, Maak TG, Aoki SK. Arthroscopic and imaging findings after traumatic hip dislocation in patients younger than 25 years of age. J Hip Preserv Surg. 2015;2:303-309. [DOI] [PMC free article] [PubMed] [Google Scholar]