Abstract
Background
Hip microinstability has gained attention recently as a potential cause of hip pain. Currently there is a lack of evidence-based objective diagnostic criteria surrounding this diagnosis. Previous studies have shown translation of the femoral head during extreme hip positions. However, reliable assessment of femoral head translation is lacking.
Questions/purposes
(1) How precise is musculoskeletal ultrasound for measuring anterior femoral head translation during the hip anterior apprehension test? (2) What is the intra- and interrater reliability of dynamic ultrasonography in assessing anterior femoral head translation?
Methods
We recruited 10 study participants (20 hips) between the ages of 22 and 50 years with no history of hip pain or functional limitations. Test-retest methodology was used. Seven females and three males were enrolled. The mean age of study participants was 27 years (SD 8.7 years); mean body mass index was 22.6 kg/m2 (SD 2.2 kg/m2). All study participants underwent dynamic hip ultrasonography by three different physicians 1 week apart. Each hip was visualized in two neutral positions (neutral and neutral with the contralateral hip flexed [NF]) and two dynamic positions, which sought to replicate the apprehension test, although notably study participants had no known hip pathology and therefore no apprehension. The first maintained the hip in extension and external rotation off to the side of the examination table (EER1), and the second held the hip off of the bottom of the examination table (EER2). One hundred twenty ultrasound scans (480 images) were performed. Mean and SD were calculated using absolute values of the difference in ultrasound measurements (mm) between positions NF and EER1 and NF and EER2 calculated for each physician as well as an average of all three physicians. Intraclass correlation coefficient (ICC) analysis was used to examine intra- and interrater reliability.
Results
The mean absolute difference for NF and EER1 was 0.84 mm (SD 0.93 mm) and for NF and EER2 0.62 mm (SD 0.40 mm) on Study Day 1. Similarly, on Study Day 2, the mean absolute difference for NF and EER1 position was 0.90 mm (SD 0.74 mm) and for NF and EER2 1.03 mm (SD 1.18 mm). Cumulative values of ICC analysis indicated excellent intrarater reliability in all four positions: neutral 0.794 (95% confidence interval [CI], 0.494-0.918), NF 0.927 (95% CI, 0.814-0.971), EER1 0.929 (95% CI, 0.825-0.972), and EER2 0.945 (95% CI, 0.864-0.978). Similarly, interrater ICC analysis cumulative values were excellent for NF, EER1, and EER2 and fair to good for the neutral position: neutral 0.725 (95% CI, 0.526-0.846), NF 0.846 (95% CI, 0.741-0.913), EER1 0.812 (95% CI, 0.674-0.895), and EER2 0.794 (95% CI, 0.652-0.884).
Conclusions
This study offers the first ultrasound protocol of which we are aware for measuring anterior femoral head translation. Hip dynamic ultrasound may assist in providing precise objective clinical-based diagnostic evidence when evaluating complex hip pain and suspected microinstability. Musculoskeletal ultrasound is a reliable office-based method of measuring anterior femoral head translation that can be utilized by physicians with varying experience levels. Future studies are needed to investigate ultrasound anterior femoral head translation taking into account sex, prior hip surgery, hip osseous morphology, and ligamentous laxity.
Level of Evidence
Level III, diagnostic study.
Introduction
Microinstability of the hip has recently gained attention as a clinical entity [1, 22, 23], although there is a lack of evidence-based clinical objective diagnostic criteria surrounding this diagnosis. Hip microinstability is defined as painful supraphysiological mobility of the hip with associated architectural and functional abnormalities that impair joint stability [3, 9, 15, 17]. Ligamentous laxity and peripelvic muscle weakness can contribute to, and clinically present like, hip microinstability [5]. The healthy hip inherently has a large multiplanar ROM. Critical soft tissue-stabilizing structures include the acetabular labrum, ligamentum teres, iliofemoral, ischiofemoral and pubofemoral ligaments of the joint capsule [9, 11, 17, 24], and the iliocapsularis muscle [2, 13]. Furthering our understanding of hip microinstability is clinically important in that anterior femoral head translation is considered detrimental to hip health as a result of the resultant inherent lack of hip congruency [6].
The established physical examination maneuver to elicit symptoms of anterior instability when dynamically stressing the anterior soft tissue structures of the hip is the anterior apprehension test [25]. Clinically, the anterior apprehension test is designed to reproduce this stress and pain with hip extension and external rotation [17]. One study performed in cadavers has demonstrated that strain forces are maximally increased on the anterior labrum with abduction and external rotation when held in the extended position [10]. Another study showed that these motions were associated with anterior femoral head translation of 2 to 5 mm [17]. More recently, a study in cadaver models has demonstrated in hips with capsules that are normal, the components of femoral head translation were within 0.5 mm in positions close to neutral and increased femoral head translation and hip microinstability with surgical violation of the capsule up to 4 mm [14]. Translation of the femoral head in the acetabulum has been reported in extreme hip positions assessed by radiographs [23] and MRI [6]. However, to our knowledge, there is no existing technique that can reliably assess anterior femoral head translation to determine microinstability of the femoroacetabular joint.
We therefore asked: (1) How precise is ultrasound for measuring anterior femoral head translation during the hip anterior apprehension test? (2) What is the intra- and interrater reliability of dynamic ultrasonography in assessing anterior femoral head translation?
Patients and Methods
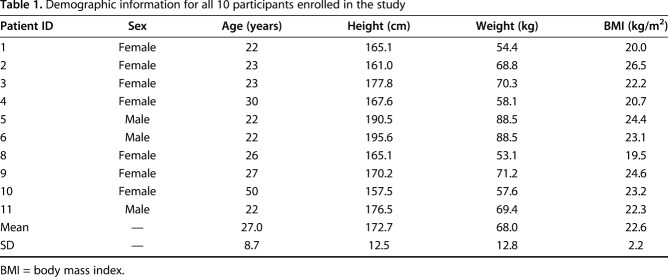
Patient recruitment and the study protocol were approved by the institutional review board at our institution before study commencement. A test-retest study design was used [18]. The study setting was a tertiary-level academic sports medicine musculoskeletal ultrasound program and pediatric and young adult hip preservation program. Seven females and three males were enrolled in the study. We did not attempt to enroll an equal number of males and females for this study, because no sex comparison analyses were required to answer the research questions. The mean age of the study participants was 27 years (SD ± 8.7 years), and the mean body mass index (BMI) was 22.6 kg/m2 (SD ± 2.2 kg/m2) (Table 1). A total of 120 ultrasound scans (480 images) were performed.
Table 1.
Demographic information for all 10 participants enrolled in the study
Ten study participants were recruited over a period of approximately 1 month through the hospital’s internal web page to undergo dynamic ultrasound hip evaluation. A total of 21 people was initially screened for participation in the study. One participant did not meet the study inclusion criteria and 10 participants could not participate in the study as a result of scheduling conflicts. The final study cohort included 10 individuals (20 hips). As a preliminary study, we decided to include bilateral hips from each participant for the initial data analysis. A secondary analysis was performed on one randomly selected hip per study participant (10 individuals, 10 hips). All participants were in good physical health and had no history of hip pathology or functional limitations. Participants between the ages of 22 and 50 years were eligible to participate provided they were able to attend the initial appointment as well as a followup appointment 1 week later.
Exclusion criteria included patients with hip pain, previous hip surgery, known hip pathology, or Ehlers-Danlos syndrome. Demographic information was collected on all study participants including height, weight, BMI, age, and sex. All participants met the inclusion criteria for the study and completed the experimental protocol as designed.
Three different ultrasound machines were utilized to perform the study: the GE Logiq E (Boston, MA, USA), Toshiba Xario™ 200 (Irvine, CA, USA), and the BK Flex Focus 400 (Peabody, MA, USA). Each of the three physicians (PAD, AS, SJ) was assigned to one of three ultrasound machines, which they used throughout the duration of the study. All study participants underwent dynamic hip ultrasonography by three attending-level nonoperative sports medicine physicians (PAD, AS, SJ) with varying levels of musculoskeletal ultrasound experience. The training levels of the three attending physicians include: Attending 1 = expert, 10 years of ultrasound experience; Attending 2 = intermediate, 7 years of ultrasound experience; Attending 3 = novice, recently completed nonoperative sports medicine fellowship training with 1 additional year focusing on musculoskeletal ultrasound. All three of the attending physicians perform a variety of ultrasound scans throughout the clinical day on all extremities. The novice physician has completed a sports medicine fellowship, which entails basic training in ultrasound only. The musculoskeletal ultrasound fellowship year entails performing scans 4 days/week and roughly six scans per day. The intermediate physician has been practicing musculoskeletal ultrasound for 7 years, roughly six to eight scans per day 4 days per week. This holds true for the expert-level attending with approximately 10 years of experience. Strict adherence to the protocol was maintained throughout the phases of data collection. The dynamic ultrasound examination of the hip was developed by the hip preservation team within our institution and utilized clinically as an adjunct to the care of patients with hip pain for the past 12 months.
The study consisted of two separate appointments 1 week apart. On Study Days 1 and 2, all 10 participants underwent ultrasound examination by each of the three physicians. Participants were encouraged to maintain a similar diet, physical activity, and other routine activities between the two appointments. By the end of the study day, each participant had undergone ultrasound examinations on each hip by each of the three physicians for a total of six examinations per patient. This study protocol allowed for testing of the reliability among the physicians at each time point (interrater reliability) as well as the reliability for each physician individually over time (intrarater reliability) [21].
Four different ultrasound positions were tested for each hip. The first two positions tested the neutral, or baseline, positions. For the first position, designated as the neutral position, the patient was placed in the supine position with both hips in extension (Fig. 1A). For the second position, neutral with the contralateral hip flexed (NF), the study participant again was placed in the supine position with the contralateral hip flexed and the lumbar spine flush to the examination table to stabilize the lumbar spine and pelvis (Fig. 1B).
Fig. 1 A-B.
(A) The first dynamic ultrasound position, termed neutral, shows the subject lying supine with both hips in the neutral position. (B) The second dynamic ultrasound position, termed neutral flexed (NF), shows the subject again lying supine with the contralateral hip held in flexion.
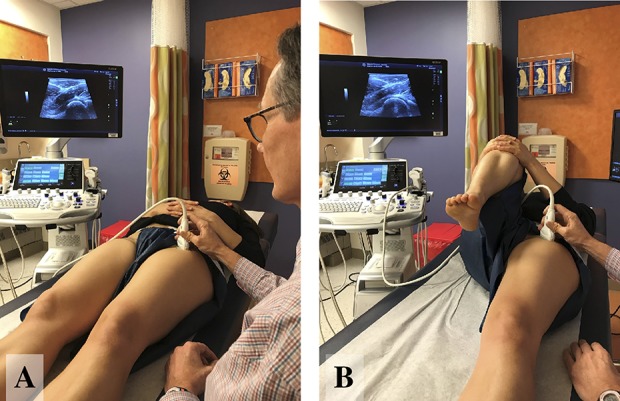
The following two positions were designed to test anterior femoral head translation in the apprehension positions [25]. The apprehension position was chosen because this position stresses the anterior structures of the hip and dynamically reproduces anterior femoral head translation. For both apprehension positions, the contralateral hip was flexed and held in place by the study participant. The patient was instructed again to stabilize the pelvis/lumbar spine by pressing the lower back flat to the examining table to promote lumbar and pelvic stabilization and minimize variability in pelvic tilt. The first position, EER1, involves the patient in the supine position with the ipsilateral hip dynamically maneuvered into extension and external rotation over the side of the bed by the examiner performing the ultrasound scan (Fig. 2A). For the final position, EER2, the patient again was placed in the supine position, and the hip was dynamically maneuvered into extension and external rotation at the bottom edge of the examining table, as opposed to the side (Fig. 2B).
Fig. 2 A-B.

(A) The third dynamic ultrasound position, termed EER1, shows the subject lying supine with the imaged hip held in extension and external rotation by the physician off to the side of the examination table while the contralateral hip is held in flexion. (B) The fourth dynamic ultrasound position, termed EER2, shows the subject again lying supine with the imaged hip held in extension and external rotation by the physician off of the end of the examination table while the contralateral hip is held in flexion.
In all positions, the probe was held in a sagittal oblique plane identifying the femoral head and acetabulum. The ultrasound linear high-frequency probe was used in all cases. The ultrasound probe was placed in the sagittal oblique position with the proximal end of the transducer positioned such that the acetabulum and femoral head were imaged at the head-neck junction of the proximal femur. The ultrasound examiner scanned the femoral acetabular junction from medial to lateral and located to the highest point, and midline, of the femoral head. Finally, an ultrasound image was obtained in each of these positions.
Measurements using the internal software of each machine were used to calculate the position of the femoral head as it relates to the acetabulum in millimeters (Fig. 3). In cases in which the femoral head was below the level of the acetabulum, a negative number (in millimeters) was designated, whereas femoral head position above the level of the acetabulum was considered positive. At any point during data collection, three participants were in rotation with three physicians; ideally each physician was performing an ultrasound examination at all times. On completion of an examination, the patients rotated to the next room for the ultrasound examination by a different physician. This rotation improved flow of patients throughout the data collection phase of the study.
Fig. 3.
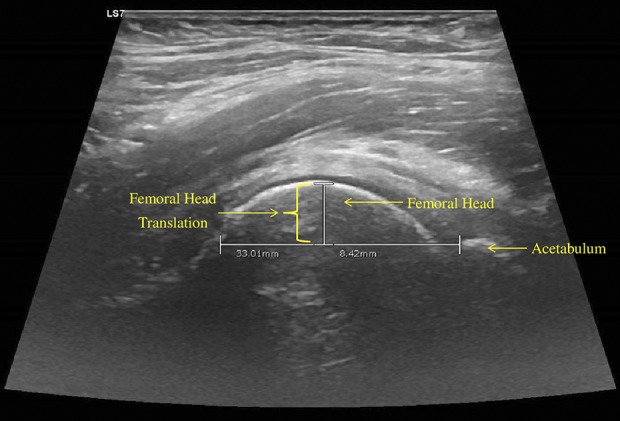
Measurement of anterior femoral head translation was performed using the internal software of the ultrasound machine to calculate the position of the femoral head as it relates to the acetabulum in millimeters; the vertical distance from the horizontal line to the sclerotic margin of the femoral head denotes the femoral head translation.
Main outcome measures include intrarater reliability for each of the three physician examiners and interrater reliability among each physician for four different ultrasound positions (neutral supine, NF, EER1, and EER2) measuring anterior femoral head translation for each hip.
Seven days after the initial appointment, patients underwent a second round of ultrasound examinations following the exact same protocol as Week 1. Every effort was made to keep the same schedule and rotation of patients; however, some patients needed to be moved earlier or later in the day as a result of scheduling complications. Strict adherence to the protocol again was maintained, and all measurements were taken and recorded a second time.
Statistical Analysis
Demographic information including age, height, weight, and BMI was descriptively analyzed using mean and SD. Additionally, raw data were used to express each participant’s four ultrasound hip images bilaterally on Study Day 1 and Study Day 2. The Shapiro-Wilk test was used to test and confirm normality of the data. The absolute difference between the NF and EER1 and EER2 positions was calculated using the average value for the three physicians. Intraclass correlation coefficient (ICC) analysis was used to examine intra- and interrater reliability. Specifically, intrarater reliability was tested for the three physicians, for four ultrasound positions, between Study Day 1 and Study Day 2. Additionally, the mean values of each ultrasound position performed by each physician between the two study time points were expressed as cumulative. Interrater reliability among the three physicians was calculated for Study Day 1 and Study Day 2 separately based on each ultrasound image. Again, cumulative values of the interrater reliability between Study Day 1 and Study Day 2 were expressed for each physician. For both intra- and interrater reliability measures, absolute agreement was used. Ninety-five percent confidence intervals were incorporated. Values of < 0.40 were considered poor. Values between 0.40 and 0.75 were defined as fair to good, whereas recorded values > 0.75 were classified as excellent reliability [7]. All analyses were performed by SPSS (SPSS Inc, Chicago, IL, USA).
Results
Femoral Head Translations
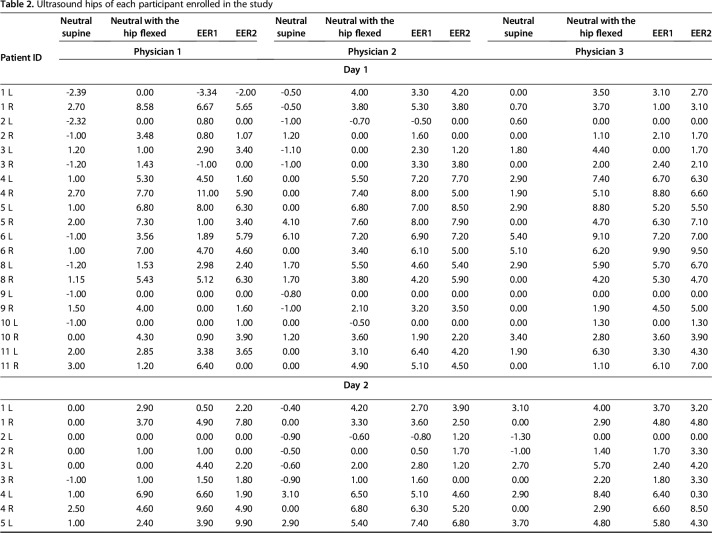
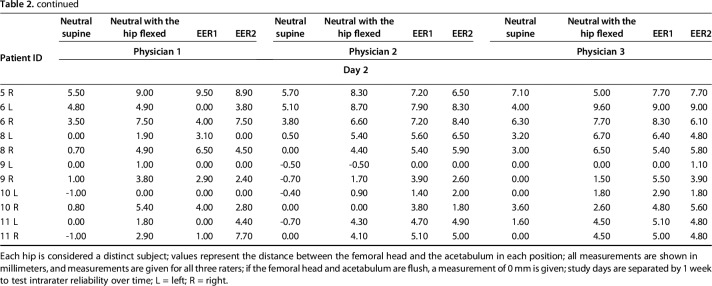
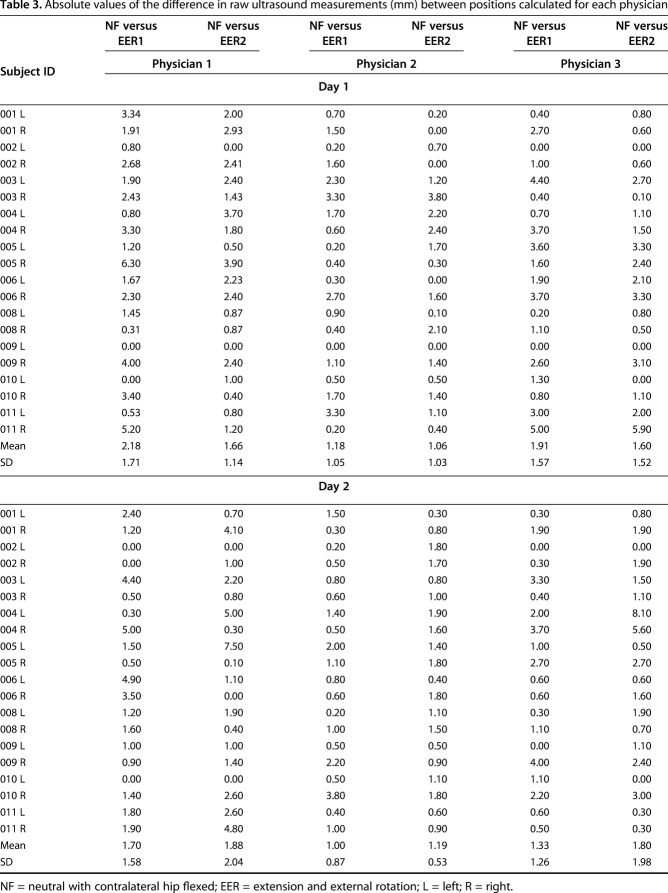
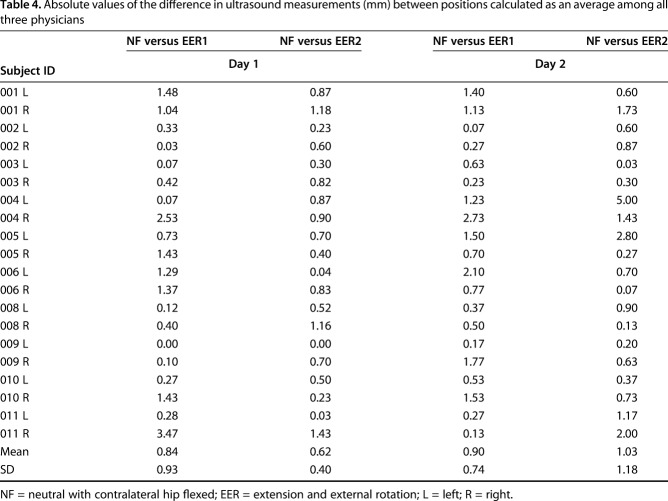
Dynamic ultrasound appears to be a precise method of measuring anterior femoral head translation in the neutral and apprehension positions (hip extension and external rotation). The mean absolute differences between positions, calculated from the anterior femoral head translation measurements (Table 2), for the three physicians individually ranged from 1.06 mm (SD 1.03 mm) to 2.18 mm (SD 1.71 mm) for Study Day 1 and from 1.00 mm (SD 0.87 mm) to 1.88 mm (SD 2.04 mm) for Study Day 2 (Table 3). When averaged among all three physicians, the mean absolute difference for NF and EER1 was 0.84 mm (SD 0.93 mm) and for NF and EER2 0.62 mm (SD 0.40 mm) on Study Day 1. Similarly, on Study Day 2, the mean absolute difference for NF and EER1 was 0.90 mm (SD 0.74 mm) and for NF and EER2 1.03 mm (SD 1.18 mm) (Table 4). These data show little deviation of measurements between positions, indicating high levels of precision.
Table 2.
Ultrasound hips of each participant enrolled in the study
Table 3.
Absolute values of the difference in raw ultrasound measurements (mm) between positions calculated for each physician
Table 4.
Absolute values of the difference in ultrasound measurements (mm) between positions calculated as an average among all three physicians
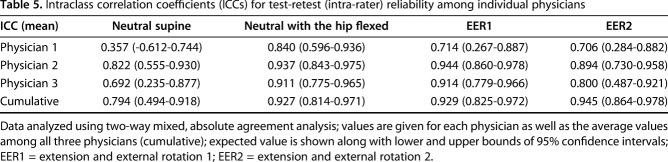
Intra- and Interrater Reliability
Using bilateral hips, we performed a series of ICC analyses. Cumulative values of ICC analysis indicated excellent intrarater reliability in all four ultrasound positions (Table 5). All three physicians demonstrated excellent intrarater reliability for the NF position (Table 5). In the EER1 and EER2 positions, two of the three physicians showed excellent intrarater reliability (Table 5) and one of the physicians had a fair to good level of intrarater reliability (Table 5). Intrarater reliability in the neutral position showed a wider range of reliability classifications, and the ICC value obtained by the expert physician was poor based on the predefined categorization (Table 5).
Table 5.
Intraclass correlation coefficients (ICCs) for test-retest (intra-rater) reliability among individual physicians
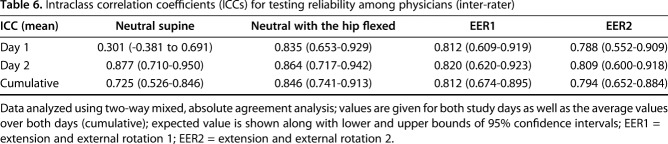
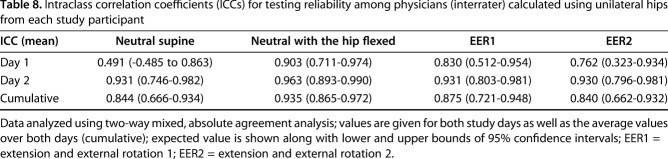
For the interrater ICC analysis, cumulative values showed excellent level measures for the NF, EER1, and EER2, but not the neutral position (Table 6). Interrater reliability for all three physicians was excellent in the same three ultrasound positions (NF, EER1, and EER2) on both Study Day 1 and Study Day 2. However, ICC values of interrater reliability in the neutral position were poor on Study Day 1, excellent on Study Day 2, and fair to good cumulatively (Table 6).
Table 6.
Intraclass correlation coefficients (ICCs) for testing reliability among physicians (inter-rater)
No difference in reliability testing was found between the apprehension positions when measured from the lateral side of the bed (EER1) versus the apprehension position performed at the foot of the bed (EER2) (Tables 5, 6).
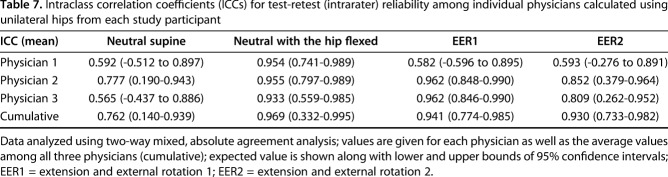
Secondary subgroup intra- and interrater ICC analyses for 10 randomly selected hips (one from each study participant) showed that all intrarater ICC classifications remained the same, except for an increase from poor to fair in the neutral supine position for one physician (Table 7). Similarly, all interrater ICC classifications remained the same except for an increase from poor to fair in the neutral supine position on Study Day 1 and an increase from fair to excellent in the neutral supine position cumulatively (Table 8).
Table 7.
Intraclass correlation coefficients (ICCs) for test-retest (intrarater) reliability among individual physicians calculated using unilateral hips from each study participant
Table 8.
Intraclass correlation coefficients (ICCs) for testing reliability among physicians (interrater) calculated using unilateral hips from each study participant
Discussion
Hip microinstability is defined as supraphysiological movement of the femoral head relative to the acetabulum; as a clinical entity, it is poorly understood. Objective diagnostic criteria may serve to guide treatment, but we lack objective clinical measures that can reliably assess anterior femoral head translation. Our findings support the notion that femoral head translation can be reliably measured using a simple office-based ultrasound examination.
Our research should be interpreted in light of the following limitations. The methodology for this research assumes each hip per study participant to be an independent data point, which could result in an overestimation of both the precision of the femoral head translation as well as the reliability of the measurements. To address this limitation, we randomly selected one hip per study participant and reran the reliability tests using half of the data points (Tables 7, 8). Interestingly, the reliability either stayed the same or increased for all positions, suggesting that our approach using bilateral hips does not overestimate the reliability of our measurements and, in fact, may underestimate those values. Furthermore, the research question simply investigates precision of the ultrasound measure in study participants and does not involve comparison analyses. The results may be difficult to generalize in that the physicians involved in this study are an inherent part of a large, high-volume hip preservation program with many years of hip ultrasound exposure and experience. To address this limitation, one of the physicians recruited to participate in the study recently completed a dedicated musculoskeletal ultrasound fellowship just 1 year before data collection. Notably, the different experience levels of three attending physicians did not affect the reliability results of the ultrasound measures. Ultrasound is user- and experience-dependent. Future training will be required for use and incorporation as the standard of care. To address this issue, the ultrasound physicians in this study are teaching national courses. More females were enrolled than males in this study cohort. Normal range of dynamic femoral head translation hip ultrasound measurements may vary by sex. Future research on dynamic hip ultrasonography is needed that controls for sex, ligamentous laxity, and the presence or absence of hip pathology. Although the number of study participants was low, the number of actual ultrasound scans was high, thereby providing ample data for statistical analysis and interpretation of results. Finally, this study did not investigate whether femoral head translation truly correlates with clinical hip microinstability.
The major finding of this study is that dynamic ultrasound examination of the hip to measure anterior femoral head translation showed excellent intra- and interrater reliability with the hip in both the neutral with the contralateral hip flexed and apprehension positions. This is the first study of which we are aware that has quantified anterior femoral head translation of the hip using dynamic ultrasound. Notably, it has been reported that the functional approach to evaluating hip motion is more accurate because it accounts for joint dynamics [27]. Siston and Delp [26] use a functional method to test hip center kinematics and a smallest error of 2.2 ± 0.2 mm is reported with a circumduction hip motion pattern. Studies using MRI three-dimensional (3-D) modeling [6, 12] and radiographs [23] have reported femoral head translation in select populations. Charbonnier et al. [6] measured femoral acetabular translation in dancers in multiple dance positions known to stress the femoral acetabular joint and reported femoroacetabular translations in the range of 0.93 to 6.35 mm using a validated virtual MRI 3-D modeling technique along with a motion capture system. The majority of our data reports a similar range of femoral head translation. Similarly, Gilles et al. [12] measured femoroacetabular translation in professional dancers during low-amplitude abductions and extreme flexions and report the best hip center computation method was the dynamic functional method that enforces interarticular distances from a neutral posture with measured hip center translations of 2.05 ± 0.74 mm. Dynamic ultrasound, in comparison to MR modeling and radiographs, provides real-time evaluation of femoral head translation and other provocative hip motions while also allowing for patient interaction during the examination to reproduce pain symptoms. Clinically, this is very helpful to the physician when trying to make an accurate diagnosis when evaluating complex hip pain. Future studies will aim to investigate the range of femoral head translations in patients with suspected hip microinstability related to prior surgery, ligamentous laxity, and acetabular dysplasia.
A comparable dynamic sonographic technique has been described [16, 19, 20] and validated [8, 28] in a similar fashion to assess inferior glenohumeral instability. Marquardt and Jerosch [20] studied AP translation of the humeral head as it relates to the bony glenoid utilizing dynamic ultrasound examination with the shoulder in 90° abduction and neutral rotation of the arm. This study revealed dorsal overhang of the humeral head in relation to the dorsal brim of the glenoid measurement to be 1.5 mm (± 3.5 mm) on the dominant side and 1.9 mm (± 3.4 mm) on the nondominant side. In comparison, patients with multidirectional shoulder instability were found to have increased AP translation of the humeral head of 2.9 mm (± 3.7 mm) on the dominant side and 0.7 mm (± 4.6 mm) on the opposite side. Yeap et al. [28] assessed anterior shoulder translation using ultrasound in the apprehension position of 90° of abduction and external rotation with applied external force of 60 N and reported the reliability of the measurements. The overall intraobserver variance ranged between 0% and 13% (mean 3.8% ± 2.5%) and 0.5% and 21% (mean 5.1% ± 3.9%) for the two observers, and the interobserver variance ranged between 0% and 30% (mean 9.3% ± 7.3%). In comparison, Cheng et al. [8] investigated intra- and interrater reliability of stress ultrasound of the shoulder performed by two observers. The authors found that dynamic ultrasound of the shoulder had good interrater reliability and excellent between-session repeatability coefficients. Borsa et al. [4] sought to quantify glenohumeral joint laxity in elite swimmers versus control athletes. This study found no significant differences in both anterior and posterior translation between the two groups with anterior translation measurements of 2.82 ± 1.7 mm and 2.74 ± 1.7 mm, respectively.
Clearly, further investigation of anterior femoral head translation using dynamic ultrasound is needed. Normative data and between-group comparison investigations (such as before and after hip arthroscopy) will be of great value in moving forward our understanding of hip microinstability in the future. In addition to the clinical benefits, including lack of radiation exposure and portability, dynamic ultrasound has the potential to reduce medical expenses. Cost-effectiveness analysis comparing other imaging modalities such as MRI and CT may be another intriguing project once the validity of dynamic ultrasound examination is established. We also note that the concept of hip microinstability currently lacks evidence-based clinical objective diagnostic criteria. This study offers the first ultrasound protocol for objectively measuring anterior femoral head translation. When excessive anterior femoral head translation or anterior hip microinstability is suspected, hip dynamic ultrasound may assist in providing objective clinical-based diagnostic evidence. In conjunction with a thorough history, physical examination, and other diagnostic modalities, this information can serve to provide objective measurements that will help determine the clinical diagnosis of hip microinstability in patients with hip pain. More generally, musculoskeletal ultrasound is a reliable and simple office-based method of measuring anterior femoral head translation.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Boston Children’s Hospital, Waltham, MA, USA.
References
- 1.Abrams GD, Luria A, Sampson J, Madding RA, Robinson WH, Safran MR, Sokolove J. Decreased synovial inflammation in atraumatic hip microinstability compared with femoroacetabular impingement. Arthroscopy. 2017;33:553–558. [DOI] [PubMed] [Google Scholar]
- 2.Babst D, Steppacher SD, Ganz R, Siebenrock KA, Tannast M. The iliocapsularis muscle: an important stabilizer in the dysplastic hip. Clin Orthop Relat Res. 2011;469:1728–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolia I, Chahla J, Locks R, Briggs K, Philippon MJ. Microinstability of the hip: a previously unrecognized pathology. Muscles Ligaments Tendons J. 2016;6:354–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borsa PA, Scibek JS, Jacobson JA, Meister K. Sonographic stress measurement of glenohumeral joint laxity in collegiate swimmers and age-matched controls. Am J Sports Med. 2005;33:1077–1084. [DOI] [PubMed] [Google Scholar]
- 5.Boykin RE, Anz AW, Bushnell BD, Kocher MS, Stubbs AJ, Philippon MJ. Hip instability. J Am Acad Orthop Surg. 2011;19:340–349. [DOI] [PubMed] [Google Scholar]
- 6.Charbonnier C, Kolo FC, Duthon VB, Magnenat-Thalmann N, Becker CD, Hoffmeyer P, Menetrey J. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med. 2011;39:557–566. [DOI] [PubMed] [Google Scholar]
- 7.Charter RA. A breakdown of reliability coefficients by test type and reliability method, and the clinical implications of low reliability. J Gen Psychol. 2003;130:290–304. [DOI] [PubMed] [Google Scholar]
- 8.Cheng SC, Hulse D, Fairbairn KJ, Clarke M, Wallace WA. Comparison of dynamic ultrasound and stress radiology for assessment of inferior glenohumeral laxity in asymptomatic shoulders. Skeletal Radiol. 2008;37:161–168. [DOI] [PubMed] [Google Scholar]
- 9.Dangin A, Tardy N, Wettstein M, May O, Bonin N. Microinstability of the hip: a review. Orthop Traumatol Surg Res. 2016;102:S301–S309. [DOI] [PubMed] [Google Scholar]
- 10.Dy CJ, Thompson MT, Crawford MJ, Alexander JW, McCarthy JC, Noble PC. Tensile strain in the anterior part of the acetabular labrum during provocative maneuvering of the normal hip. J Bone Joint Surg Am. 2008;90:1464–1472. [DOI] [PubMed] [Google Scholar]
- 11.Fukui K, Trindade CA, Briggs KK, Philippon MJ. Arthroscopy of the hip for patients with mild to moderate developmental dysplasia of the hip and femoroacetabular impingement: outcomes following hip arthroscopy for treatment of chondrolabral damage. Bone Joint J. 2015;97:1316–1321. [DOI] [PubMed] [Google Scholar]
- 12.Gilles B, Christophe FK, Magnenat-Thalmann N, Becker CD, Duck SR, Menetrey J, Hoffmeyer P. MRI-based assessment of hip joint translations. J Biomech. 2009;42:1201–1205. [DOI] [PubMed] [Google Scholar]
- 13.Haefeli PC, Steppacher SD, Babst D, Siebenrock KA, Tannast M. An increased iliocapsularis-to-rectus-femoris ratio is suggestive for instability in borderline hips. Clin Orthop Relat Res. 2015;473:3725–3734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han S, Alexander JW, Thomas VS, Choi J, Harris JD, Doherty DB, Jeffers JRT, Noble PC. Does capsular laxity lead to microinstability of the native hip? Am J Sports Med. 2018;46:1315–1323. [DOI] [PubMed] [Google Scholar]
- 15.Jackson TJ, Peterson AB, Akeda M, Estesss A, McGarry MH, Adamson GJ, Lee TQ. Biomechanical effects of capsular shift in the treatment of hip microinstability: creation and testing of a novel hip instability model. Am J Sports Med. 2016;44:689–695. [DOI] [PubMed] [Google Scholar]
- 16.Jerosch J, Marquardt M, Winkelmann W. [Ultrasound documentation of translational movement of the shoulder joint. Normal values and pathologic findings] [in German]. Ultraschall Med. 1991;12:31–35. [DOI] [PubMed] [Google Scholar]
- 17.Kalisvaart MM, Safran MR. Microinstability of the hip-it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg. 2015;2:123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karras DJ. Statistical methodology: II. Reliability and validity assessment in study design, Part B. Acad Emerg Med. 1997;4:144–147. [DOI] [PubMed] [Google Scholar]
- 19.Krarup AL, Court-Payen M, Skjoldbye B, Lausten GS. Ultrasonic measurement of the anterior translation in the shoulder joint. J Shoulder Elbow Surg. 1999;8:136–141. [DOI] [PubMed] [Google Scholar]
- 20.Marquardt M, Jerosch J. [Ultrasound evaluation of multidirectional instability of the shoulder] [in German]. Unfallchirurg. 1991;94:295–301. [PubMed] [Google Scholar]
- 21.Mc Auliffe S, Mc Creesh K, Purtill H, O'Sullivan K. A systematic review of the reliability of diagnostic ultrasound imaging in measuring tendon size: is the error clinically acceptable? Phys Ther Sport. 2017;26:52–63. [DOI] [PubMed] [Google Scholar]
- 22.McNeill W, Scott S. Treatment of hip microinstability and gluteal tendinopathies involves movement control and exercise. J Bodyw Mov Ther. 2016;20:588–594. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell RJ, Gerrie BJ, McCulloch PC, Murphy AJ, Varner KE, Lintner DM, Harris JD. Radiographic evidence of hip microinstability in elite ballet. Arthroscopy. 2016;32:1038–1044.e1031. [DOI] [PubMed] [Google Scholar]
- 24.Nepple JJ, Philippon MJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, Wijdicks CA. The hip fluid seal–Part II: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22:730–736. [DOI] [PubMed] [Google Scholar]
- 25.Shu B, Safran MR. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med. 2011;30:349–367. [DOI] [PubMed] [Google Scholar]
- 26.Siston RA, Delp SL. Evaluation of a new algorithm to determine the hip joint center. J Biomech. 2006;39:125–130. [DOI] [PubMed] [Google Scholar]
- 27.Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D'Lima DD, Cristofolini L, Witte H, Schmid O, Stokes I. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion–part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech. 2002;35:543–548. [DOI] [PubMed] [Google Scholar]
- 28.Yeap JS MA, Humphries L, Wallace AL. Ultrasonic evaluation of anterior shoulder translation in normal shoulders. J Musculoskelet Res. 2003;7:125–134. [Google Scholar]