Abstract
Background
The Bernese periacetabular osteotomy (PAO) continues to be a commonly performed nonarthroplasty option to treat acetabular dysplasia, but only a few short-term studies have evaluated complications rigorously after PAO.
Questions/purposes
(1) What complications are observed at 10-year mean followup of the Bernese PAO in patients with symptomatic acetabular dysplasia? (2) What factors are associated with these complications? (3) Do these complications affect clinical outcome scores?
Methods
We reviewed 238 hips in 206 patients treated with PAO from July 1994 to August 2008. Only PAOs performed for symptomatic acetabular dysplasia and those that had at a minimum 4-year followup were included. Patients who went on to THA before 4 years were included in the study. Patients with hip pain who presented with a clinical presentation of symptomatic acetabular dysplasia, radiographic evidence of femoral head uncovering, and a lateral center-edge angle < 25° were considered for PAO and no other juxtaacetabular osteotomy was offered other than PAO. Sixty-two hips had diagnoses other than acetabular dysplasia and 22 were lost to followup. The remaining 154 hips (129 patients) were evaluated by chart review at a mean of 10 years (range, 1.7–20.5 years) using the UCLA Activity Score, modified Harris hip score (mHHS), WOMAC, and radiographic analysis. The mean age at PAO was 26 years (range, 10-60 years) and consisted of 113 female patients (132 hips [86%]) and 16 male patients (22 hips [14%]). Complications were graded using the validated Clavien-Dindo system. Complications were assessed for each hip and the highest complication grade was assigned to the hip if multiple complications occurred. We divided complication grades into three groups for analysis: no complications, Grade 1 complications, and complications that deviated from the standard postoperative course (Grades 2, 3, and 4). There were no Grade 5 complications. Variables with significant (p < 0.05) univariable associations with complications were considered for inclusion in a multivariable model. Outcome variables (mHHS and WOMAC) at the most recent followup visit were analyzed using a generalized estimating equation approach. Analysis of variance was used to compare UCLA at the most recent followup among the complication classes.
Results
Major complications defined as Clavien-Dindo Grade 3/4 occurred in 14 hips (9%). After controlling for potential confounding variables, we found that increasing body mass index (BMI) (odds ratio [OR], 1.16; 95% confidence interval, 1.05-1.25; p = 0.004) was associated with increased risk of complication. In contrast, greater surgeon experience was associated with a decreased risk (OR, 0.3; p = 0.002). Complications were associated with postoperative pain and activity, WOMAC (mean ± SD: 0 complications = 1.5 ± 15.1, 1 complication = 4.3 ± 4.1, 2-3 complications = 3.8 ± 4.6; p = 0.020) and UCLA scores (mean ± SD: 0 complications = 7.8 ± 2, 1 complication = 6.7 ± 2.1, 2-3 complications = 6.5 ± 2; p = 0.003).
Conclusions
Most hips undergoing PAO have few complications. The most common major surgical complication is nonunion. Increasing BMI was a predictor of having a complication, and surgeon experience decreased complication risk. Having a complication adversely affected long-term pain and activity. To minimize complications and maximize outcomes, a patient’s BMI should be assessed preoperatively and those with excessive BMI should be counseled on the increased risk of complications. In an experienced surgeon’s hands, PAO has few complications at mean 10-year followup and a low risk of permanent disability.
Level of Evidence
Level III, therapeutic study.
Introduction
Developmental dysplasia of the hip (DDH) is a major cause of osteoarthritis in young adults that often results in THA at a young age [1, 15, 18, 24, 25, 36, 37]. Joint preservation surgery in DDH continues to be a desirable option because THA may be associated with early revision, and native joint preservation prevents the need for activity restrictions [10, 12, 13, 16, 17, 23]. Long-term outcome studies after periacetabular osteotomy (PAO) have indicated that most patients experience long-lasting pain relief and maintain an active lifestyle [38, 39]. PAO is a well-accepted procedure with an established learning curve and known short-term complications. However, to our knowledge, no studies have rigorously evaluated the complications that may accrue after PAO followup, the factors associated with those complications, and the effects of those complications on clinical outcomes [5, 8, 9, 28, 30, 41].
As PAO is becoming more widely used [3, 8, 20-22, 34], knowledge of complications that may accrue or persist over time is necessary. For example, there may exist late complications like acetabular osteonecrosis, delayed symptomatic nonunion, and manifestations of acetabular malreduction that are not appreciated at early followup but which become clinically important at longer term followup. There is a need to better define the late complications associated with PAO to educate providers and stratify patients who will benefit from surgery, but also to identify modifiable risk factors and prevent complications.
We therefore sought to answer the following questions: (1) What complications are observed at 10-year mean followup of the Bernese PAO in patients with symptomatic acetabular dysplasia? (2) What factors are associated with these complications? (3) Do these complications affect clinical outcome scores?
Materials and Methods
This is a retrospective study of 154 hips (129 patients) with DDH identified through review of a longitudinally maintained institutional hip database, which includes all patients treated with PAO. We obtained institutional review board approval for the present study. All patients who underwent PAO for symptomatic dysplasia of the hip from July 1994 to August 2008 were eligible for inclusion. We excluded patients with neuromuscular or connective tissue disorders, prior trauma, and additional diagnoses other than DDH such as Legg-Calvé-Perthes disease, slipped capital femoral epiphysis, and acetabular retroversion.
Patients who presented to the senior authors (JCC, PS) with symptomatic developmental dysplasia [29] of the hip, radiographic evidence of femoral head uncovering, and a lateral center-edge angle of < 25° were offered treatment with PAO; no other juxtaacetabular osteotomies were used or offered in this study period. In total, 238 PAOs were performed on 206 patients during the study period. Sixty-two hips were excluded because the patient underwent PAO for indications other than DDH or for additional diagnoses that did not meet the inclusion criteria, and another 22 hips were lost to followup or did not have greater than 4-year followup. Patients who went on to THA before 4 years were included in the study. The remaining 154 hips (129 patients) were retrospectively evaluated at a mean of 10 years (range, 1.7–20.5 years) (Fig. 1). The mean patient age was 26 years (range, 10-60 years). There were 113 female patients (132 hips [86%]) and 16 male patients (22 hips [14%]); the mean body mass index (BMI) was 24 kg/m2 (range, 17-34 kg/m2).
Fig. 1.
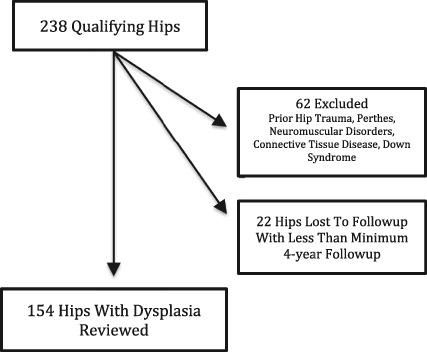
A flow diagram of the patient population is shown.
Surgical Technique
The surgical technique that has been previously reported [7] was performed according to Ganz et al. [14] and the abductor-sparing approach as described by Murphy and Millis was utilized [26]. Seventy-eight hips (51%) had concurrent procedures. Sixty-six underwent femoral head-neck osteochondroplasty using a Smith-Petersen approach, 21 underwent hip arthroscopy for labral resection or repair, and eight underwent a proximal femoral osteotomy (seven varus-producing and one valgus-producing). There were no concurrent cartilage repair techniques.
Clinical and Radiographic Analysis
Complications were graded and assessed for each hip according to the modified Clavien-Dindo classification system [11, 31, 41]. An orthopaedic surgeon (JW) performed a thorough chart review of all patients and complication grading was performed independent of the treating surgeons.
A Grade 1 complication needed no treatment and no deviation from a normal postoperative course. Grade 1 complications included transient lateral femoral cutaneous nerve dysesthesia, asymptomatic heterotopic ossification, and asymptomatic nonunions. A Grade 2 complication deviated from the normal postoperative course; patients underwent pharmacologic treatment or close monitoring as an outpatient. Grade 2 complications included superficial wound infections necessitating additional clinic visits and/or antibiotics and nerve palsy needing bracing and/or close observation with complete resolution. A Grade 3 complication resulted in surgical, endoscopic, or radiographic intervention and sometimes an unplanned hospital admission. Grade 3 complications included revision PAO, deep infection needing operative incision and débridement, open reduction and internal fixation of symptomatic nonunion, and heterotopic ossification excision. A Grade 4 complication was life-threatening and/or not treatable with potential for permanent disability, including permanent nerve injury, major vascular injury, and pulmonary embolism. A Grade 5 complication resulted in death.
Postoperative activity, pain, and quality-of-life outcomes were collected at latest followup with the use of a hip questionnaire that included the UCLA Activity Score, modified Harris hip score (mHHS), and the WOMAC pain subscale score. All of these are validated outcome scores for assessing patients with hip osteoarthritis [2, 4, 27, 33]. Patients who had undergone bilateral PAOs completed the series of questions for each hip individually.
Preoperative and latest followup radiographs were evaluated. Preoperative radiographs were evaluated for the lateral center-edge angle of Wiberg and measured on AP pelvis radiographs [40]. In addition, late postoperative radiographs were assessed for nonunion of osteotomy sites, osteonecrosis, and heterotopic ossification as described by Brooker et al. [6]. All patients with radiographs available were reviewed and none were excluded. An orthopaedic surgeon independent of the treating surgeons (JW) made all radiographic assessments.
Statistical Analysis
Our analysis focused on the modified Clavien-Dindo classification variable and we divided them into three groups according to the grade of complication: 0, 1, and 2 to 4. No Grade 5 complications occurred in our study. The Clavien-Dindo complication grade was assessed for each hip and the highest complication grade was assigned to the hip if multiple complications occurred. We analyzed this polytomous outcome variable using an ordinal logistic regression analysis, and we accounted for correlation among hips for patients undergoing bilateral surgery using a generalized estimating equation (GEE) approach independent correlation structure. Univariable analyses assessing the relationship between complications and sex, age, surgeon experience (≥ 75 case days), BMI, prior surgery, concurrent procedure, and severity of hip dysplasia were conducted. Variables with significant (p < 0.05) univariable associations with complication grade were considered for inclusion in a multivariable model. A forward selection approach was used to include variables in the multivariable model, and significant variables were retained. Outcome variables (mHHS and WOMAC) at the most recent followup visit were analyzed using a GEE approach (assuming normal distribution and a compound symmetric correlation structure). The UCLA Activity Score was considered a patient-level outcome, and for patients undergoing bilateral surgery, we only analyzed the UCLA score with the highest complication grade. An analysis of variance was used to compare UCLA at the most recent followup among the Clavien-Dindo complications grades. All analyses were conducted using SAS, Version 9.4 (SAS Institute Inc, Cary, NC, USA).
Results
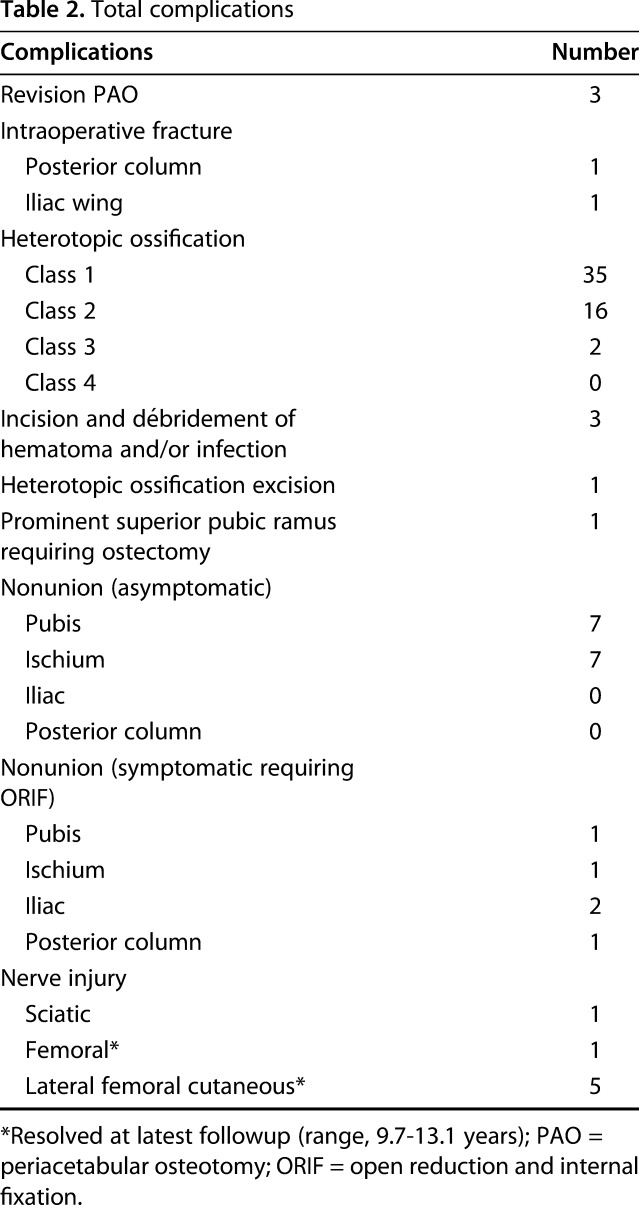
There were 66 hips with complications related to the PAO, and of those, 48 hips had complications classified as Grade 1, four as Grade 2, 13 as Grade 3, and one as Grade 4. Major complications as defined as Clavien-Dindo Grade 3/4 occurred in 14 hips (9%) (Table 1). There were five open reduction of nonunions, three incision and débridement of hematoma or deep infection, three revision PAOs, one heterotopic ossification excision, two intraoperative fractures needing open reduction and internal fixation, one ostectomy, and one residual sciatic nerve damage with residual foot pain (Table 2). There were no vascular injuries, no acetabular or femoral head osteonecrosis, and no complications that worsened over time.
Table 1.
Complications according to the modified Clavien-Dindo grading scheme
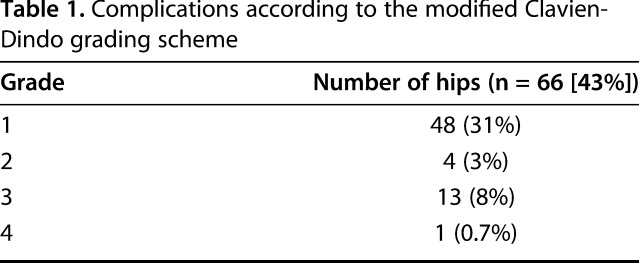
Table 2.
Total complications
Univariable analyses revealed that surgeon experience, concurrent osteochondroplasty, and labral repair were associated with decreased odds of complication, whereas preoperative BMI and age at surgery were associated with greater odds of a complication. In the multivariable model, we found that increased BMI was associated with being in a higher complication group, and surgeon experience of ≥ 75 days was associated with a decreased risk of being in a higher complication group. After adjusting for BMI and surgeon experience, none of the other factors considered for inclusion in the multivariable model (osteochondroplasty, age at surgery, scope/repair/resection) were associated with complication group and were not retained in the final multivariable model. In the multivariable model, for each unit of BMI increase, there was 17% higher odds of being in a higher complication group (odds ratio [OR], 1.16; 95% confidence interval [CI], 1.05-1.28; p = 0.004; see Fig. 2 for prediction plot of ≥ Grade 2). In contrast, 75 case days of experience was associated with a 70% decrease in the odds of being in a higher complication group (OR, 0.3; 95% CI, 0.14-0.64; p = 0.002).
Fig. 2.
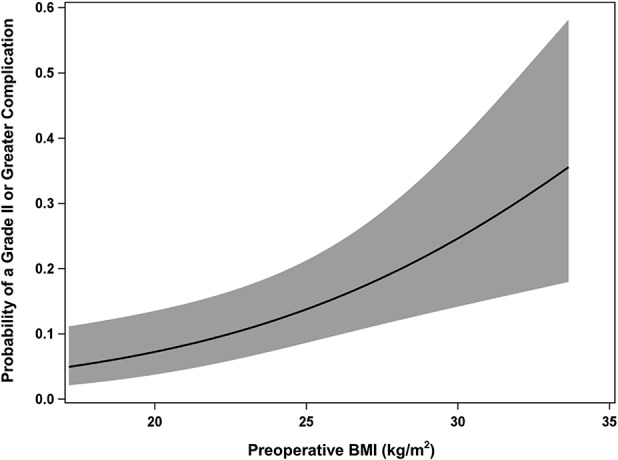
BMI versus probability of a Grade 2 or greater complication is shown. Shaded area shows 95% CIs.
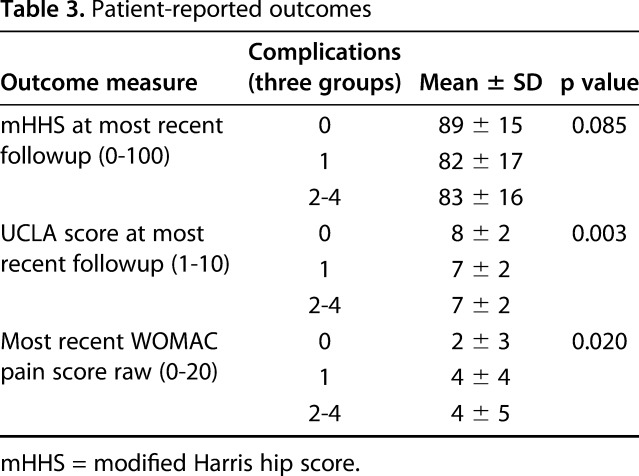
At higher complication grades, patients reported worse postoperative WOMAC pain subscale scores and worse UCLA activity levels. Patients who had no complications reported a higher mean UCLA score compared with patients who sustained a Grade 1 or higher complication (pairwise mean differences for Grade 1: -1.26; 95% CI, -2.05 to -0.48; p = 0.002; for Grade 2 or 3: -1.31; 95% CI, -2.45 to -0.16; p = 0.026). Also, patients who had no complications reported lower WOMAC pain scores compared with those who sustained a Grade 2 or higher complication (pairwise mean difference of 2.3; 95% CI, 0.7-3.9; p = 0.005) (Table 3).
Table 3.
Patient-reported outcomes
Discussion
As PAO is performed more frequently for symptomatic acetabular dysplasia, it is important to understand the full scope of complications and whether they are associated with functional outcomes. This is one of the largest followup studies analyzing complications and outcomes after the Bernese PAO, and to our knowledge, no other studies have reported a mean 10-year followup of complications with a standardized grading scheme [21, 32, 38]. We aimed to report the complications that accrue during followup of PAO, determine preoperative variables that may increase the likelihood of having a complication, and assess the effect of complications with that of patient-reported outcomes.
This study has limitations. First, this retrospective study represents two surgeons’ learning curves and experience. The results may not be representative of other surgeons or centers, which may limit the generalizability of the results, yet we had clear and consistent indications for PAO over the study period, and therefore surgeons with comparable backgrounds who follow these indications might expect similar results. This group includes the first PAOs done at our institution, which could overestimate the frequency of complications, because it has been shown even in highly trained surgeons, a learning curve may exist [9, 19, 30]. Second, this is a retrospective chart analysis, and although comprehensive, some complications could have been missed depending on documentation. This may have influenced some of the capture of Grade 1 complications, yet other more serious complications would still be captured. We also note 22 hips (22 patients [13%]) were lost to followup and postoperative survivorship and patient-reported outcomes were not available for these patients. We evaluated all patients who had at least 4-year minimum followup to address longer term followup and capture patients at their 5-year followup appointment and perhaps other complications have occurred since then. Patients lost to followup allow for transfer bias and, therefore, these results represent a best-case scenario; we cannot report the complications and outcomes in unaccounted for patients. Another limitation is that most Grade 1 complications have little if any clinical importance, yet are reported with our rigorous data collection methodology and grading scheme. This is why we divided our grading scheme to evaluate trivial Grade 1 complications separately from other complications that change a patient’s postoperative course. Hardware removal was not considered a complication. Next, only postoperative patient-reported outcome measures were utilized, which limits the efficacy of current results, because preoperative scores were not evaluated and although these postoperative patient-reported outcome measures were statistically significant, we are unsure if these results would be clinically significant.
We observed major complications in 9% (14 hips) in a select population of acetabular dysplasia. Zaltz et al. [41] reported on a prospective multicenter cohort and assessed the early complications of 205 patients who underwent PAO by trained PAO surgeons who were considered beyond their learning curve. All PAOs regardless of diagnosis were included. Within the first year of surgery, Zaltz et al. found a 6% proportion of major complications (Grade 3/4) but were unable to comment on the long-term consequences of these complications with only 1 year of followup. Davey and Santore reported the complications of their initial 75 PAOs. The patients were divided into two groups—the initial 35 PAOs and the next 35 PAOs. Although the initial 35 had increased complications, the overall observed major complication percentage was 10% [9]. Based on these studies, it appears that our major complication percentage is similar to these early-term results and do not seem to increase with time nor is there a substantial risk of permanent disability for these major complications.
In the current study, we found an association between increasing BMI and having a Grade 2 or greater complication. The odds of a patient developing a complication were 17% greater for each kg/m2 increase. BMI was treated as a continuous variable and was not dichotomized or graded as obese or nonobese. We have shown that although patients may not be classified as obese (BMI ≥ 30 kg/m2), complications may increase with each increased unit of BMI even in nonobese patients. Novais et al. [28] assessed the PAO complication risk and determined that obesity was an independent predictor of having a complication. For every 5-kg/m2 BMI increase, there was a 3.2 times greater chance of developing a complication, and patients who were classified as obese (BMI ≥ 30 kg/m2) had a 22.3% increase in complications. Our findings further clarify the increased risk of complications in patients with a larger BMI. We have also determined that complications impact postoperative outcomes. Future studies focusing on more comprehensive body composition rather than BMI may help further stratify patients who are at the highest risk for complications. Not to mention, patients with higher BMIs would benefit from nutritional evaluation and weight reduction before surgery to minimize risk of complications and optimize postoperative outcomes.
We also found that surgeon experience influences complications. In the current study, we assessed the learning curve as a potential variable and we found that 75 case days of experience was associated with a 70% decrease in the odds of complication. The concept of the PAO learning curve is well established [5, 8, 9, 14, 30, 35]. Peters et al. [30] reported on their learning curve and early experience. Their major complications for 73 patients undergoing PAO occurred in the first 30 cases. These results clarify the results of Peters et al. and further establish the PAO learning curve; further studies should investigate the impact of focused fellowship PAO training on the learning curve.
In our group, complications were adversely associated with pain (WOMAC) and activity (UCLA) scores. Patients who did not develop complications were more active and had less pain at most recent followup. Good long-term outcomes after the Bernese PAO have been reported [32, 38, 39] yet little is known about the effect of complications on outcomes. Biedermann et al. [5] reported on 50 patients with a mean followup of 7.4 years and assessed the association between outcomes and complications. They reported similar subjective outcome scores, SF-36 and WOMAC, with patients having a major or minor complication, except for those patients who had dysesthesia resulting from lateral femoral cutaneous nerve dysfunction. Patients who had lateral femoral cutaneous nerve dysesthesias had worse WOMAC scores at midterm followup. We have also verified that having a complication may affect postoperative outcomes, specifically WOMAC pain and UCLA Activity Score. Future direction should aim at minimizing complications to enhance longer term patient-reported outcomes.
In summary, this report is a comprehensive, retrospective mean 10-year evaluation of all complications associated with the Bernese PAO using a validated grading scheme. We report a relatively low percentage of complications. Increasing BMI and limited surgeon experience were associated with a greater complication risk and higher grade complications were associated with poorer WOMAC pain and UCLA Activity Scores. Complications do not appear to increase over time, and at long-term followup, the chance of permanent disability from a complication in our series was rare. To minimize complications and maximize outcomes, BMI should be assessed preoperatively and those patients with excessive BMI should be counseled on the increased risk of complications. In an experienced surgeon’s hands, PAO has few complications at mean 10-year followup and a low chance of permanent disability.
Footnotes
The institution of one or more of the authors (JCC) has received, during the study period, funding from the Curing Hip Disease Fund for research personnel salary support and statistical analysis consultation.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Washington University School of Medicine, St Louis, MO, USA.
References
- 1.Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986;35:119–128. [PubMed] [Google Scholar]
- 2.Ashby E, Grocott MPW, Haddad FS. Outcome measures for orthopaedic interventions on the hip. J Bone Joint Surg Br. 2008;90:545–549. [DOI] [PubMed] [Google Scholar]
- 3.Beaulé PE, Dowding C, Parker G, Ryu J-J. What factors predict improvements in outcomes scores and reoperations after the Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2015;473:615–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Biedermann R, Donnan L, Gabriel A, Wachter R, Krismer M, Behensky H. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop. 2007;32:611–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brooker AF, Bowerman JW, Robinson RA, Riley LH. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed] [Google Scholar]
- 7.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1):65–83. [DOI] [PubMed] [Google Scholar]
- 8.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davey JP, Santore RF. Complications of periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:33–37. [PubMed] [Google Scholar]
- 10.Devitt A, O'Sullivan T, Quinlan W. 16- to 25-year follow-up study of cemented arthroplasty of the hip in patients aged 50 years or younger. J Arthroplasty. 1997;12:479–489. [DOI] [PubMed] [Google Scholar]
- 11.Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg. 2004;240:205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dorr LD, Kane TJ, Conaty JP. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger. A 16-year follow-up study. J Arthroplasty. 1994;9:453–456. [DOI] [PubMed] [Google Scholar]
- 13.Duffy GP, Berry DJ, Rowland C, Cabanela ME. Primary uncemented total hip arthroplasty in patients < 40 years old. J Arthroplasty. 2001;16:140–144. [DOI] [PubMed] [Google Scholar]
- 14.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 15.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 2008;466:264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garellick G, Kärrholm J, Rogmark C, Rolfson O. Swedish Hip Arthroplasty Register: annual report 2012. 2013. Available at: https://registercentrum.blob.core.windows.net/shpr/r/Annual-report-2012-HJBqtLpig.pdf. Accessed September 5, 2017.
- 17.Georgiades G, Babis GC, Hartofilakidis G. Charnley low-friction arthroplasty in young patients with osteoarthritis: outcomes at a minimum of twenty-two years. J Bone Joint Surg Am. 2009;91:2846–2851. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 19.Howie DW, Beck M, Costi K, Pannach SM, Ganz R. Mentoring in complex surgery: minimising the learning curve complications from peri-acetabular osteotomy. Int Orthop. 2012;36:921–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim Y-J. Nonarthroplasty hip surgery for early osteoarthritis. Rheum Dis Clin North Am. 2008;34:803–814. [DOI] [PubMed] [Google Scholar]
- 21.Kralj M, Mavčič B, Antolič V, Iglič A, Kralj-Iglič V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840. [DOI] [PubMed] [Google Scholar]
- 22.Leunig M, Ganz R. The evolution and concepts of joint-preserving surgery of the hip. Bone Joint J. 2014;96:5–18. [DOI] [PubMed] [Google Scholar]
- 23.McAuley JP, Szuszczewicz ES, Young A, Engh CAS. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. [DOI] [PubMed] [Google Scholar]
- 24.Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. [DOI] [PubMed] [Google Scholar]
- 25.Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–223. [PubMed] [Google Scholar]
- 26.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98. [DOI] [PubMed] [Google Scholar]
- 27.Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Novais EN, Potter GD, Clohisy JC, Millis MB, Kim YJ, Trousdale RT, Carry PM, Sierra RJ. Obesity is a major risk factor for the development of complications after peri-acetabular osteotomy. Bone Joint J. 2015;97:29–34. [DOI] [PubMed] [Google Scholar]
- 29.Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011;93(Suppl 2):17–21. [DOI] [PubMed] [Google Scholar]
- 30.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. [DOI] [PubMed] [Google Scholar]
- 31.Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J; Academic Network for Conservational Hip Outcomes Research Group. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Terwee CB, Bouwmeester W, van Elsland SL, de Vet HCW, Dekker J. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis Cartilage. 2011;19:620–633. [DOI] [PubMed] [Google Scholar]
- 34.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179. [DOI] [PubMed] [Google Scholar]
- 35.Trousdale RT, Cabanela ME. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand. 2003;74:119–126. [DOI] [PubMed] [Google Scholar]
- 36.Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61:334–338. [DOI] [PubMed] [Google Scholar]
- 37.Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop Relat Res. 1987;225:62–76. [PubMed] [Google Scholar]
- 38.Wells J, Millis M, Kim Y-J, Bulat E, Miller P, Matheney T. Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res. 2017;475:396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wells J, Schoenecker P, Duncan S, Goss CW, Thomason K, Clohisy JC. Intermediate-term hip survivorship and patient-reported outcomes of periacetabular osteotomy: the Washington University experience. J Bone Joint Surg Am. 2018;100:218–225. [DOI] [PubMed] [Google Scholar]
- 40.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand Suppl. 1939;83:7–135. [Google Scholar]
- 41.Zaltz I, Baca G, Kim YJ, Schoenecker P, Trousdale R, Sierra R, Sucato D, Sink E, Beaule P, Millis MB, Podeszwa D, Clohisy JC. Complications associated with the periacetabular osteotomy: a prospective multicenter study. J Bone Joint Surg Am. 2014;96:1967–1974. [DOI] [PubMed] [Google Scholar]


