Abstract
Objective:
Nasal surgeries (such as Functional Endoscopic Sinus Surgery, Rhinoplasty, and Septorhinoplasty) are popular procedures. But perioperative bleeding, eyelid edema, and periorbital ecchymosis remain problems. Tranexamic acid (TXA) is an antifibrinolytic, and it was used to reduce the perioperative bleeding. However, there is no enough evidence judging its safety and efficiency. Therefore, a meta-analysis is conducted by us to evaluate the role of TXA in patients undergoing nasal surgeries.
Method:
A search of the literature was performed until June 2018; the PubMed, Embase, Cochrane Central Register of Controlled Trials, and Google Scholar databases were searched for related articles using search strategy. Two authors independently assessed the methodological quality of the included studies and extracted data. Surgical information and postoperative outcomes were analyzed. Only randomized controlled trial (RCT) articles were included, and subgroup analysis was established to deal with heterogeneity. RevMan 5.3 software was selected to conduct the meta-analysis.
Result:
Eleven RCTs were included in our meta-analysis. There were significant differences in blood loss (P < .001), surgical field quality (P < .001), edema rating of upper (P < .001) and lower (P < .001) eyelid, ecchymosis rating of upper (P < .001) and lower eyelid (P < .001) when comparing the TXA group to the placebo group. However, the difference in operation time (P = .57) was not significant between the two groups.
Conclusion:
Perioperative TXA could reduce the blood loss and improve the quality of surgery field during nasal surgery, and it was helpful for reducing the edema and ecchymosis after nasal surgeries, but it has little influence in reducing the operation time.
Keywords: blood loss, meta-analysis, nasal surgery, tranexamic acid
1. Introduction
Nasal surgeries, such as rhinoplasty, septoplasty, and functional endoscopy sinus surgery (FESS) are common invasive nasal procedures, performed singly or in combination frequently. These procedures have drastically improved over time, although they were commonly performed by the mid-19th century.[1] Similar to other surgeries, these surgeries are not without complications, considering its performance for changing the physical appearance, and attending the satisfaction and confidence of patients. Therefore, it is necessary to prevent these complications.
The most common complications are intraoperative bleeding, eyelid edema, and periorbital ecchymosis after surgery.[2,3] The maxillofacial area is a blood-rich area,[4] so the bleeding is expected in most nasal surgeries and this has a negative impact on the quality of the surgery. The intraoperative bleeding will increase the operative risk and the consequent reduction in intraoperative visualization can hinder surgical progress, prolongs surgery, reduces success rates, and, in some cases, even prevent the surgeon from completing the procedure.[5] Sometimes, it may occur in the postoperative period when the packing is removed. In these cases, the doctor may need to add packing or to repack the nose, causing inconvenience to the patient. Edema can delay the healing process of the involved tissues, and ecchymosis may lead to permanent pigmentation of the skin.[6] Different kinds of osteotomies are needed in most cases of rhinoplasty and septoplasty, and it is the main cause of periorbital and paranasal edema and ecchymosis.[7] These sequelae may even cause potential candidates to dismiss the surgical treatment.
Tranexamic acid (TXA) is a synthetic derivative of lysine amino acid that exerts an antifibrinolytic effect via inhibits lysine-binding sites on plasminogen molecules.[8] TXA has been used to reduce bleeding digestive and urinary systems, thrombocytopenia, hemophilia, cardiac, and orthopedic surgeries, various types of nasal surgeries (rhinoplasty, septoplasty, turbinectomy, and FESS).[9,10] And systemic medication of TXA may cause some side effects such as dizziness, nausea, vomiting, blurred vision, and headache.[11]
In recent years, there have been some studies analyzed the efficacy of TXA on bleeding reduction, edema, ecchymosis, and other complications in nasal surgeries. However, different conclusions have been reached, and the efficacy of TXA in nasal surgery was not clear. Therefore, the aim of our study is to systematically review the existing research on the role of TXA in patients undergoing nasal surgery. This meta-analysis is conducted to determine whether perioperative TXA affect surgical field quality, operative time, and some operative complications (estimated blood loss, eyelid edema, and periorbital ecchymosis).
2. Materials and method
2.1. Search strategy
The PubMed (1980–June 2018), Embase (1980–June 2018), Cochrane Central Register of Controlled Trials, and Google Scholar databases were searched for related studies. To improve the sensitivity and specificity and sensitivity of searching, we used the following search terms in combination with Boolean operators “AND” or “OR”: “rhinoplasty OR septoplasty OR turbinectomy OR functional endoscopy sinus surgery OR nasal surgery” AND “tranexamic acid”. The search strategy is presented in Figure 1.
Figure 1.
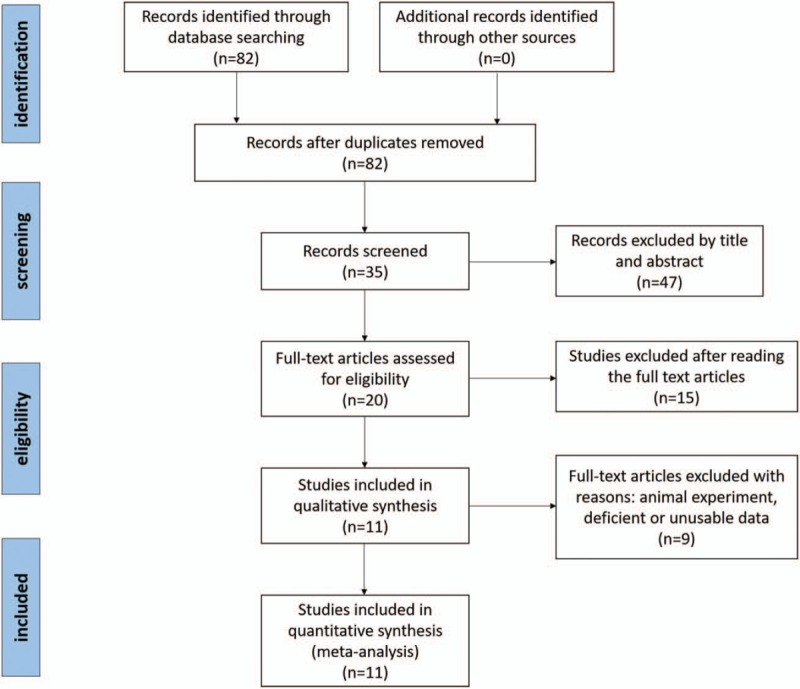
Search results and selection procedure.
2.2. Study selection
Included studies were considered eligible if they met the following criteria:
Study design: Interventional or observational studies
Population: Patients undergoing nasal surgery (rhinoplasty, septoplasty, and FESS)
Intervention: Tranexamic acid
Comparator: Placebo or nothing
Outcome:
Primary outcome: Blood loss, Surgical field quality.
Secondary outcome: Edema of upper and lower eyelid, Ecchymosis of upper and lower eyelid, operation time.
2.3. Quality assessment
Published RCTs comparing TXA with a control (placebo or nothing) in patients who underwent nasal surgery (rhinoplasty, septoplasty, and FESS) are included in this meta-analysis. Two reviewers (FL and WP) conducted the eligibility assessment, independently in an unblended standardized manner. And disagreements were resolved by discussion. According to the Cochrane Handbook for Systematic Reviews of Interventions,[12] the methodological quality, and risk basis of the included studies were evaluated as follows: (1) randomization method, (2) allocation concealment, (3) blind method of participant and outcome assessment, and (4) complete outcome data.
2.4. Data extraction
Data were extracted from the selected studies by two authors (WP and FL) independently. The extracted data included: publication data, title, first author's name, patient demographics, sample size, blood loss, surgical field quality, edema of upper and lower eyelid, ecchymosis of upper and lower eyelid, and operation time.
2.5. Data analysis and statistical methods
The data were analyzed by Review Manager Software for Windows (RevMan Version 5.3, Copenhagen, Denmark: The Nordic Cochrane Center, The Cochrane Collaboration, 2014). The means and standard deviations were applied to assess continuous variable outcomes with a 95% confidence interval [CI], and relative risks and 95% CIs were applied to assess dichotomous outcomes. Statistical heterogeneity was tested using the I2 value and chi-squared test. A P value <.05 was considered statistically significant, and the random effects model was used for analysis. If P values were <.05 or I2 > 50%, indicating significant heterogeneity, the random effects model was applied.
2.6. Ethical approval
This article is not involved in ethical requirements. This is a meta-analysis, so a ethical requirement is not necessary.
3. Result
3.1. Search result
The search strategy identified 82 relevant articles in the databases. Eleven RCTs[13–23] were selected after reading the abstracts and full text carefully. All of the documents are high quality articles. Finally, a total of 568 patients were included and reviewed for our meta-analysis, the sample sizes for each study ranged from 20 to 170. Theodore[23] studied the use of topical antifibrinolytic drugs in FESS, one part of the study was for TXA, the research designed two doses (100 mg and 1 g), so we divided them into two groups to extract data separately. The results of patient characteristics are summarized in Table 1. Risk of bias is represented in Figures 2 and 3. Seven studies[15,16,18,20–23] were for FESS, 3 studies[13,14,17] were for rhinoplasty, and 1 study[19] was for septorhinoplasty. There were 7 articles had been published in recent 3 years, and the longest article included was published in 2006.
Table 1.
The general characteristic of the included studies.
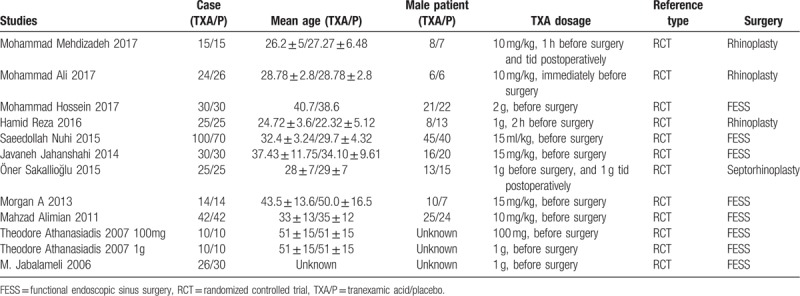
Figure 2.
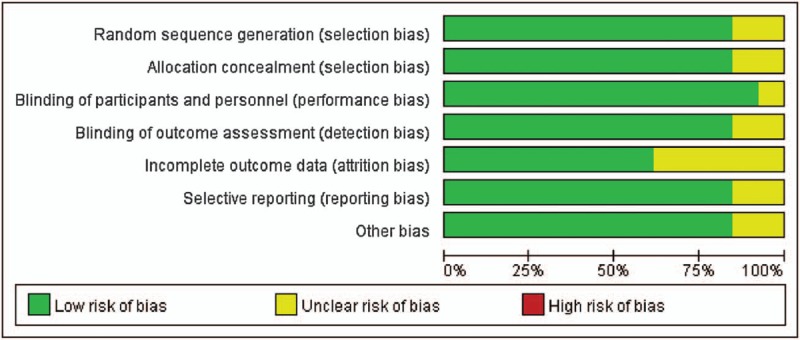
Risk of bias graph.
Figure 3.
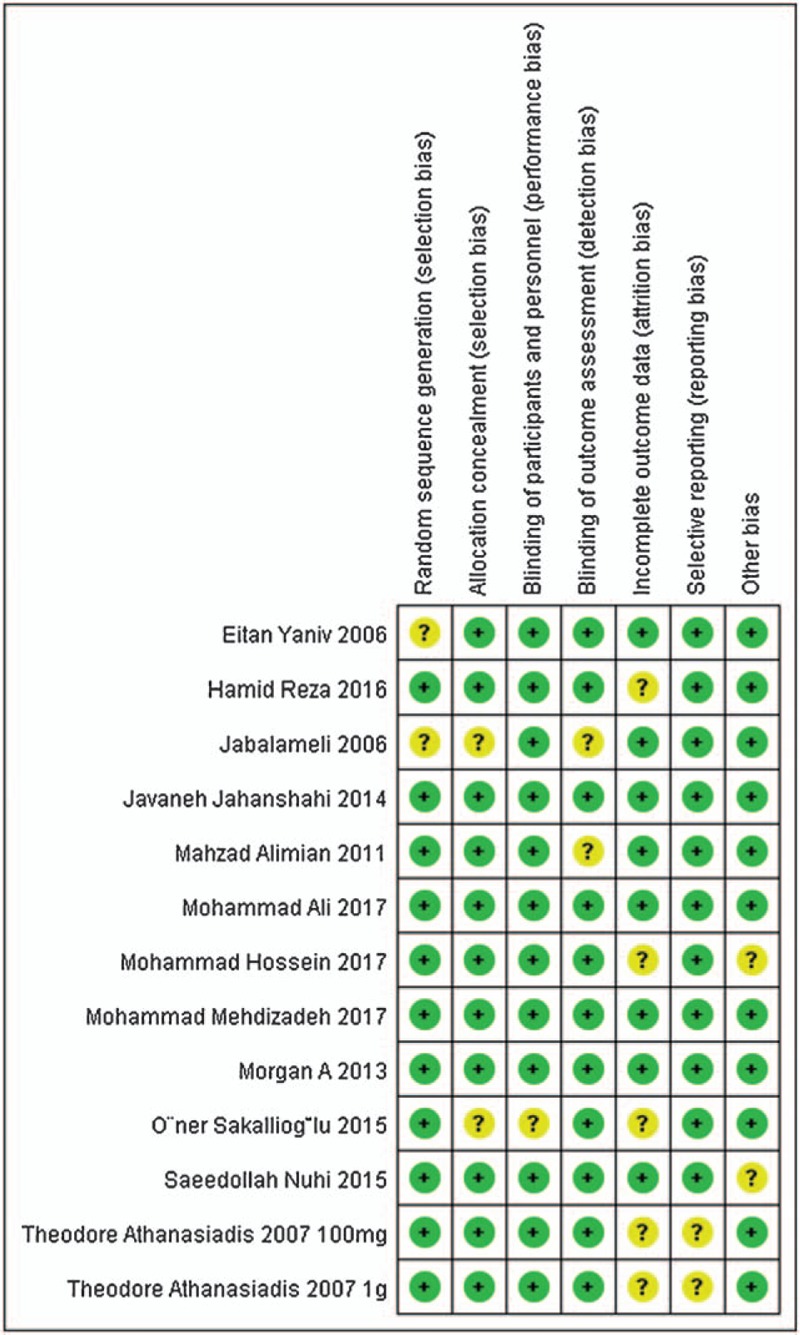
Risk of bias summary.
4. Meta-analysis results
4.1. Blood loss
Nine studies[14–22] in this meta-analysis provided the data of blood loss in nasal surgery. Three types of surgery were included in this result, so we established a subgroup analysis to deal with heterogeneity. Blood-loss volume was calculated by subtracting the volume of irrigation fluid from the total volume collected in the suction container, plus the estimated blood absorbed by the throat pack in each patient. The result showed a highly significant difference between TXA group and control group (MD = −72.65, 95% CI, [−100.42, −44.88], P < .001, Fig. 4). A random-effect model was used because the statistical heterogeneity was high (χ2 = 97.87, df = 8, P < .001, I2 = 92%).
Figure 4.
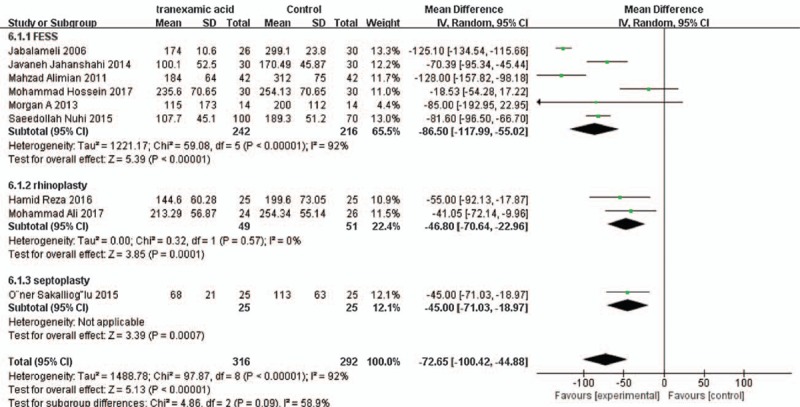
The effect of tranexamic acid illustrated by forest plot diagram on blood loss.
4.2. Surgical field quality
Based on seven component studies[15,20,21,23] with 388 patients providing available data, we found that TXA produced a better outcome compared to the placebo group in surgical field quality (MD = −0.63, 95% CI, [−0.83, −0.44], P < .001, Fig. 5). In the included studies of our meta-analysis, there are two validated scoring systems (Wormald grading scale[24] and Boezaart grading scale[25]) for surgical field quality. Both scoring systems are comparatively authoritative systems to evaluate the quality of the surgical field. A subgroup was established to survey the data of different scoring system and the reasons of heterogeneity. The statistical heterogeneity was low (χ2 = 5.90, df = 6, P = .43, I2 = 0%), so we used a fixed-effect model.
Figure 5.
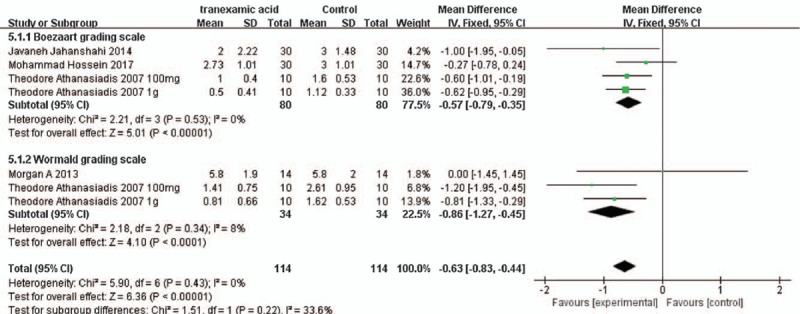
The effect of tranexamic acid illustrated by forest plot diagram on surgical field quality.
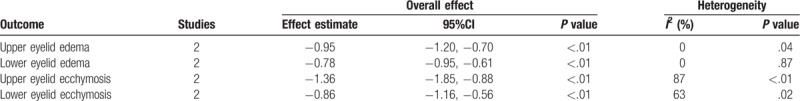
4.3. Edema and ecchymosis rating of upper and lower eyelid
Three studies[13,14,19] provided the data of edema and ecchymosis rating of upper and lower eyelid, two of them were rhinoplasty and one is about septorhinoplasty. The same evaluation index of eyelid edema and ecchymosis used in the three literatures (Fig. 6). We summarized the edema rating of upper and lower eyelid in Figure 7, and the ecchymosis rating of upper and lower eyelid in Figure 8. The results are presented in Table 2. We set up subgroups because the data from different days after surgery.
Figure 6.
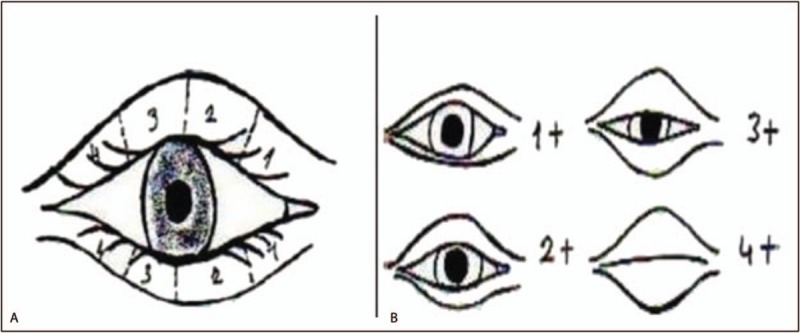
Rates of ecchymosis expansion (A) and periorbital edema (B) in upper and lower periorbital area.
Figure 7.
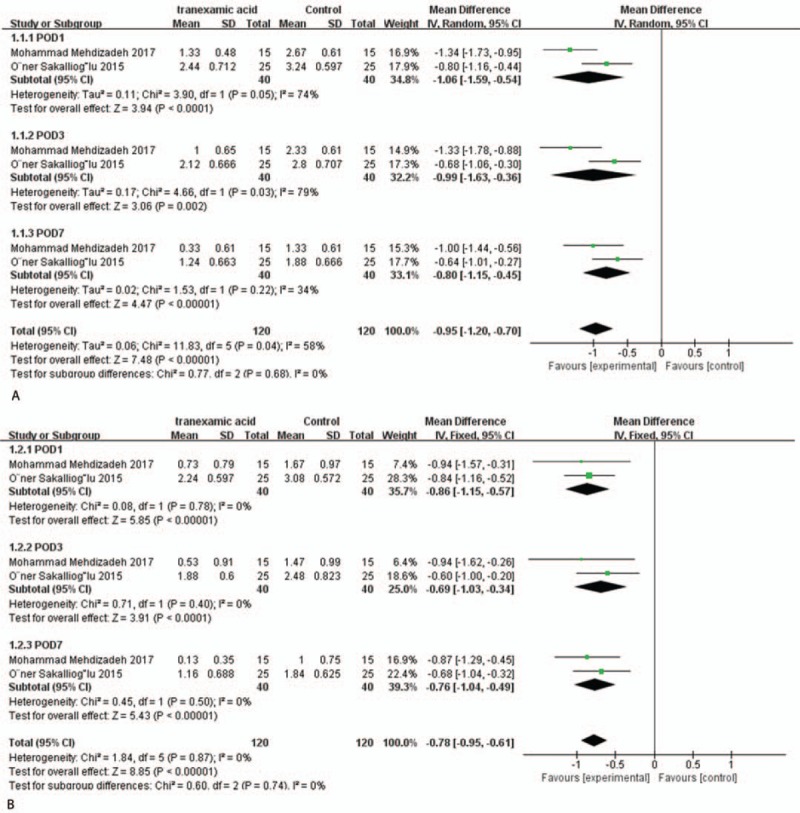
The effect of tranexamic acid illustrated by forest plot diagram on eyelid edema. (A) Edema of upper eyelid; (B) edema of lower eyelid.
Figure 8.
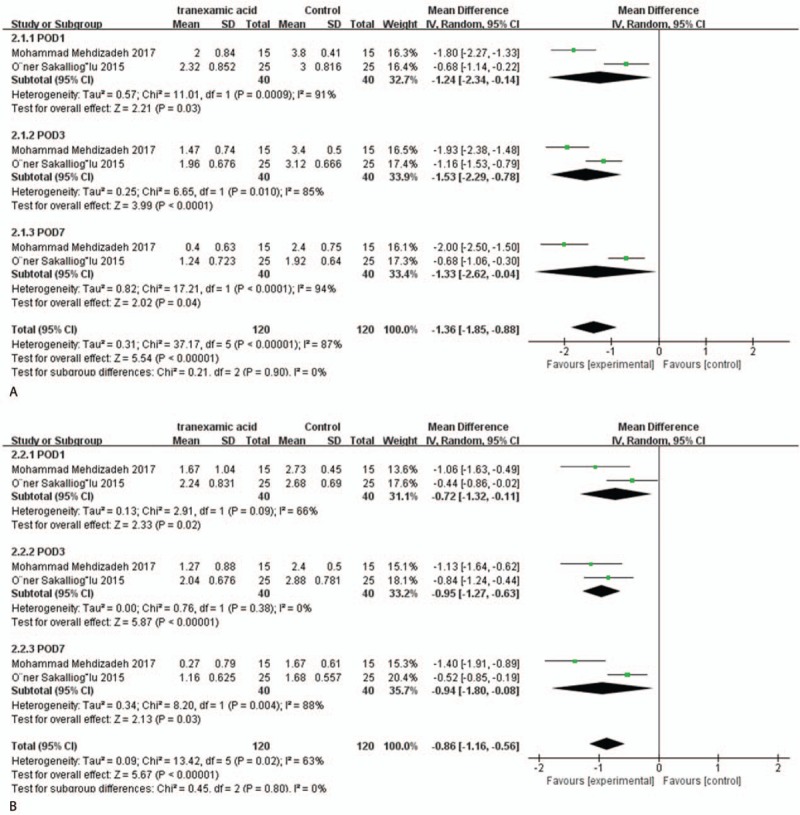
The effect of tranexamic acid illustrated by forest plot diagram on periorbital ecchymosis. (A) Ecchymosis of upper eyelid; (B) ecchymosis of lower eyelid.
Table 2.
Results of periorbital edema and ecchymosis.
4.4. Operation time
Seven studies[13–15,19–22] stated the operation time. Two types of surgery are included in this outcome, so we established a subgroup analysis. The available data revealed that there was no difference between the two groups (MD = −0.06, 95% CI, [−0.27, 0.15], P = .32, Fig. 9). A fixed-effect model was used, because the statistical heterogeneity was high (χ2 = 12.01, df = 6, P = .06, I2 = 50%).
Figure 9.
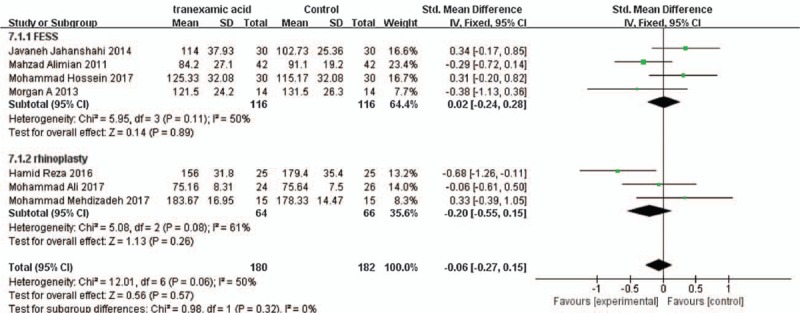
The effect of tranexamic acid illustrated by forest plot diagram on operation time.
5. Discussion
Nose surgeries (such as FESS, rhinoplasty, and septoplasty) are common procedure. However, patients under these surgeries often experience edema, ecchymosis, bleeding, and other complications. Because the nasal cavity is small, the blood vessels are abundant, and the routine hemostatic method is difficult to administer, therefore, the reasonable use of hemostatic drugs is an important measure to reduce the bleeding in the operation and provide clear field.[26] We summarized this meta-analysis to clear the efficacy of TXA during nose surgeries. The results indicated that the TXA have a positive effect in decrease intraoperative blood loss, improve the surgical field quality, and reducing periorbital edema and ecchymosis. No statistically significant difference was found in the operation time between the TXA group and the control group.
Blood loss was one of the primary outcomes in our research. Nine studies documented the data of blood loss, and the significant difference was found between the TXA group and the control group (P < .001). Bleeding is a common concern during nasal surgeries because of the rich blood supply of the nasal mucosa and sinuses. Although many nasal operations use local vasoconstrictor to treat nasal cavity and controlled hypotension anesthesia, the intraoperative oozing or bleeding still has a significant impact on operative field resolution and surgical procedures, even stop the operation. Our pooled data showed that TXA could effectively decrease the bleeding volume during nasal operation. It was reported that TXA was used for open-heart surgery under extracorporeal circulation, coronary artery bypass surgery, and hip arthroplasty, etc, which can significantly reduce the perioperative blood loss.[27–31] Another meta-analysis showed that TXA could reduce hemoglobin decline, volume of drainage, total blood loss, and transfusion requirements after total knee arthroplasty.[32] These results manifested that ideal hemostatic effect can be achieved when TXA is used perioperatively. This is very meaningful for the surgical procedure.
Surgical field quality was another primary outcome in our study. Good visibility during nasal surgeries is necessary, because the tiny structure of noses is filled with small blood vessels. In this case, even mild bleeding can cause the surgery to fail.[20] There two validated scoring systems (Wormald grading scale[24] and Boezaart grading scale[25]) for surgical field quality. Although the scoring scores are different, the scoring principles are the gradual changes in the quality of the surgical field from clear to vague. Therefore, we established a subgroup to survey the data of different scoring system and the reasons of heterogeneity. Our meta-analysis showed significant difference of surgical field quality between TXA group and placebo group, which indicates the TXA can improving the quality of operation field during nasal surgeries. This results in a response to the conclusion that TXA can reduce bleeding during nasal surgeries, because hemorrhage is the main reason affecting the quality of operative field.
The periorbital regions are particularly prone postoperative edema and ecchymosis during rhinoplasty, and it is hard to hide for patients. In the present meta-analysis, only two trials were identified and studied for postoperative edema and ecchymosis after perioperative TXA administration. There are four results respectively (edema of upper and lower eyelid, ecchymosis of upper and lower eyelid), and all the results displayed a significant difference between the two groups. This shows that the TXA in nasal surgery can effectively reduce postoperative edema and ecchymosis. Wang[33] thought systemic administration of TXA can reduce wound hematoma in minimally invasive total knee arthroplasty when rivaroxaban is used for thromboprophylaxis. And Chen[34] showed that TXA can reduce the incidence of extremity ecchymosis during total knee arthroplasty. According to these results, we concluded that perioperative TXA was helpful for reduce the edema and ecchymosis after nasal surgeries.
Operation time was one of the second outcomes in our meta-analysis. Seven RCTs were included in this index, and there was no significant difference in our pooled data (P = .57). In the included articles, the mean of operation times was range from 75 to 180 minutes. In our meta-analysis, we know that TXA can reduce the blood loss and improve the quality of surgery field, but this result shows that the use of TXA has no effect on operative time. The main reason may be the main determinant of the operative time is the complexity of surgery and surgeon's proficiency, although intraoperative bleeding may affect the operation process, the effect on the operation time is not very large. Therefore, we know that the perioperative TXA have little influence in operation time during nasal surgeries.
This systematic review has the following limitations:
-
(1)
Only eleven RCTs were selected in our meta-analysis; if more studies were included, statistical efficacy would increase.
-
(2)
Our meta-analysis included three types of surgery, although they were all nasal surgery, this improved the heterogeneity of the results.
-
(3)
The follow-up period of patients was too short in some of the trials. Most patients were followed up in the short term. This may lead to omission of some useful information.
-
(4)
There were not sufficient data, such as hemoglobin, hematocrit, and patient satisfaction.
-
(5)
Risk of bias cannot be avoided in this meta-analysis because only English publications were included.
-
(6)
The regimen or dosage of the drug is not fixed; this also improved the heterogeneity of the results. It is believed that all of these factors have the ability to change the efficacy of TXA during nasal surgeries and they need to be taken into account in the further study.
Although this article has some limitations, it is the first systemic review to evaluate the efficacy of TXA with placebo in nasal surgeries. We have rigorously selected the available articles, so the quality of the articles used after the final review is high. However, more high-quality literature should be included to improve statistical efficiency and increase sample size.
6. Conclusion
Our meta-analysis indicated that perioperative TXA could reduce the blood loss and improve the quality of surgery field during nasal surgery, and helpful for reduce the edema and ecchymosis after nasal surgeries, but it has little influence in reducing the operation time.
Author contributions
Conceptualization: Wei-dong Ping.
Data curation: Wei-dong Ping.
Formal analysis: Fei Li.
Methodology: Fei Li.
Project administration: Fei Li.
Resources: Qi-ming Zhao.
Software: Hua-feng Sun.
Supervision: Qi-ming Zhao.
Writing – original draft: Hua-feng Sun.
Writing – review & editing: Hai-shan Lu.
Footnotes
Abbreviations: CI = confidence interval, FESS = functional endoscopy sinus surgery, RCT = randomized controlled trial, TXA = tranexamic acid.
W-dP and Q-mZ contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Saif AM, Farboud A, Delfosse E, et al. Assessing the safety and efficacy of drugs used in preparing the nose for diagnostic and therapeutic procedures: a systematic review. Clin Otolaryngol 2016;41:546–63. [DOI] [PubMed] [Google Scholar]
- [2].Samman N, Cheung LK, Tong AC, et al. Blood loss and transfusion requirements in orthognatic surgery. J Oral Maxillofac Surg 1996;54:21–4. 25–6. [DOI] [PubMed] [Google Scholar]
- [3].Cochran CS, Landecker A. Prevention and management of rhinoplasty complications. Plast Reconstr Surg 2008;122:60e–7e. [DOI] [PubMed] [Google Scholar]
- [4].Choi WS, Irwin MG, Samman N. The effect of tranexamic acid on blood loss during orthognathic surgery: a randomized controlled trial. J Oral Maxillofac Surg 2009;67:125–33. [DOI] [PubMed] [Google Scholar]
- [5].Ragab SM, Hassanin MZ. Optimizing the surgical field in pediatric functional endoscopic sinus surgery: a new evidence-based approach. Otolaryngol Head Neck Surg 2010;142:48–54. [DOI] [PubMed] [Google Scholar]
- [6].Gutierrez S, Wuesthoff C. Testing the effects of long-acting steroids in edema and ecchymosis after closed rhinoplasty. Plast Surg (Oakv) 2014;22:83–7. [PMC free article] [PubMed] [Google Scholar]
- [7].Alajmi MA, Al-Abdulhadi KA, Al-Noumas HS, et al. Results of intravenous steroid injection on reduction of postoperative edema in rhinoplasty. Indian J Otolaryngol Head Neck Surg 2009;61:266–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Karimi A, Mohammadi SS, Hasheminasab M. Efficacy of tranexamic acid on blood loss during bimaxilary osteotomy: a randomized double blind clinical trial. Saudi J Anaesth 2012;6:41–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Later AF, Maas JJ, Engbers FH, et al. Tranexamic acid and aprotinin in low- and intermediate-risk cardiac surgery: a non-sponsored, double-blind, randomised, placebo-controlled trial. Eur J Cardiothorac Surg 2009;36:322–9. [DOI] [PubMed] [Google Scholar]
- [10].Lemay E, Guay J, Cote C, et al. Tranexamic acid reduces the need for allogenic red blood cell transfusions in patients undergoing total hip replacement. Can J Anaesth 2004;51:31–7. [DOI] [PubMed] [Google Scholar]
- [11].Herron J, French R, Gilliam AD. Civilian and military doctors’ knowledge of tranexamic acid (TXA) use in major trauma: a comparison study. J R Army Med Corps 2018;164:170–1. [DOI] [PubMed] [Google Scholar]
- [12].The Cochrane Collaboration; 2011;Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Available from www.cochrane-handbook.org. Accessed July 12, 2016. [Google Scholar]
- [13].Mehdizadeh M, Ghassemi A, Khakzad M, et al. Comparison of the effect of dexamethasone and tranexamic acid, separately or in combination on post-rhinoplasty edema and ecchymosis. Aesthetic Plast Surg 2018;42:246–52. [DOI] [PubMed] [Google Scholar]
- [14].Ghavimi MA, Taheri TK, Ghoreishizadeh A, et al. Efficacy of tranexamic acid on side effects of rhinoplasty: a randomized double-blind study. J Craniomaxillofac Surg 2017;45:897–902. [DOI] [PubMed] [Google Scholar]
- [15].Baradaranfar MH, Dadgarnia MH, Mahmoudi H, et al. The effect of topical tranexamic acid on bleeding reduction during functional endoscopic sinus surgery. Iran J Otorhinolaryngol 2017;29:69–74. [PMC free article] [PubMed] [Google Scholar]
- [16].Jabalameli M, Zakeri K. Evaluation of topical tranexamic acid on intraoperative bleeding in endoscopic sinus surgery. Iran J Med Sci 2006;31:221–3. [Google Scholar]
- [17].Eftekharian HR, Rajabzadeh Z. The efficacy of preoperative oral tranexamic acid on intraoperative bleeding during rhinoplasty. J Craniofac Surg 2016;27:97–100. [DOI] [PubMed] [Google Scholar]
- [18].Nuhi S, Goljanian TA, Zarkhah L, et al. Impact of intravenous tranexamic acid on hemorrhage during endoscopic sinus surgery. Iran J Otorhinolaryngol 2015;27:349–54. [PMC free article] [PubMed] [Google Scholar]
- [19].Sakallioğlu Ö, Polat C, Soylu E, et al. The efficacy of tranexamic acid and corticosteroid on edema and ecchymosis in septorhinoplasty. Ann Plast Surg 2015;74:392–6. [DOI] [PubMed] [Google Scholar]
- [20].Jahanshahi J, Hashemian F, Pazira S, et al. Effect of topical tranexamic acid on bleeding and quality of surgical field during functional endoscopic sinus surgery in patients with chronic rhinosinusitis: a triple blind randomized clinical trial. PLoS One 2014;9:e104477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Langille MA, Chiarella A, Cote DW, et al. Intravenous tranexamic acid and intraoperative visualization during functional endoscopic sinus surgery: a double-blind randomized controlled trial. Int Forum Allergy Rhinol 2013;3:315–8. [DOI] [PubMed] [Google Scholar]
- [22].Alimian M, Mohseni M. The effect of intravenous tranexamic acid on blood loss and surgical field quality during endoscopic sinus surgery: a placebo-controlled clinical trial. J Clin Anesth 2011;23:611–5. [DOI] [PubMed] [Google Scholar]
- [23].Athanasiadis T, Beule AG, Wormald PJ. Effects of topical antifibrinolytics in endoscopic sinus surgery: a pilot randomized controlled trial. Am J Rhinol 2007;21:737–42. [DOI] [PubMed] [Google Scholar]
- [24].Athanasiadis T, Beule A, Embate J, et al. Standardized video-endoscopy and surgical field grading scale for endoscopic sinus surgery: a multi-centre study. Laryngoscope 2008;118:314–9. [DOI] [PubMed] [Google Scholar]
- [25].Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth 1995;42(Pt 1):373–6. [DOI] [PubMed] [Google Scholar]
- [26].Zhang J. Effects of reptilase, tranexamic acid, carbazochrome sodium sulfonate on blood coagulation in patients undergoing endoscopy sinuses surgery. Chinese Journal Medicinal Guide 2008;10:234–6. 241. [Google Scholar]
- [27].Ren Z, Li S, Sheng L, et al. Topical use of tranexamic acid can effectively decrease hidden blood loss during posterior lumbar spinal fusion surgery: a retrospective study. Medicine (Baltimore) 2017;96:e8233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lostak J, Gallo J, Vecera M, et al. Local application of tranexamic acid in total hip arthroplasty decreases blood loss and consumption of blood transfusion. Acta Chir Orthop Traumatol Cech 2017;84:254–62. [PubMed] [Google Scholar]
- [29].Zabeeda D, Medalion B, Sverdlov M, et al. Tranexamic acid reduces bleeding and the need for blood transfusion in primary myocardial revascularization. Ann Thorac Surg 2002;74:733–8. [DOI] [PubMed] [Google Scholar]
- [30].Reid RW, Zimmerman AA, Laussen PC, et al. The efficacy of tranexamic acid versus placebo in decreasing blood loss in pediatric patients undergoing repeat cardiac surgery. Anesth Analg 1997;84:990–6. [DOI] [PubMed] [Google Scholar]
- [31].Ekback G, Axelsson K, Ryttberg L, et al. Tranexamic acid reduces blood loss in total hip replacement surgery. Anesth Analg 2000;91:1124–30. [DOI] [PubMed] [Google Scholar]
- [32].Wang C, Xu GJ, Han Z, et al. Topical application of tranexamic acid in primary total hip arthroplasty: a systemic review and meta-analysis. Int J Surg 2015;15:134–9. [DOI] [PubMed] [Google Scholar]
- [33].Wang JW, Chen B, Lin PC, et al. The efficacy of combined use of rivaroxaban and tranexamic acid on blood conservation in minimally invasive total knee arthroplasty a double-blind randomized, controlled trial. J Arthroplasty 2017;32:801–6. [DOI] [PubMed] [Google Scholar]
- [34].Chen X, Xie S, Wang K. Effectiveness of tranexamic acid in total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014;28:1338–41. [PubMed] [Google Scholar]


